Abstract
Background
Abusive abdominal trauma may be difficult to diagnose, and even serious abdominal injury may be missed. Screening for occult abdominal trauma (OAT) has been recommended by child abuse experts. However, it is unclear how often screening occurs, and what factors are associated with screening.
Objectives
(1) To determine the prevalence of OAT in a sample of children with suspected physical abuse. (2) To assess the frequency of OAT screening. (3) To assess factors associated with screening.
Patients and Methods
Charts of children evaluated for abusive injury were identified via a search of hospital discharge codes. Identified charts were reviewed to determine whether OAT screening occurred. Data were collected regarding results of screening tests, abusive injuries identified, family demographics, and characteristics of the emergency department visit.
Results
Screening occurred in 51 of 244 eligible children (20%). Positive screens were identified in 41% of those screened, and 9% of the total sample. 5% of children aged 12–23 months had OAT identified by imaging studies. Screening occurred more often in children presenting with probable abusive head trauma [OR=20.4, 95% CI (3.6–114.6), p<0..01] compared to those presenting with other injuries. Subspecialty consultation from the Child Protection Team [OR=8.5, 95% CI (3.5–20.7), p<0.01] and other subspecialists [OR=24.3, 95% CI (7.1–83.3), p<0.01] also increased the likelihood that OAT screening would occur.
Conclusions
Our findings support OAT screening with liver and pancreatic enzymes for physically abused children. This study also supports the importance of subspecialty input, especially that of a Child Protection Team. Although many identified injuries may not require treatment, their role in confirming, or demonstrating increased severity of maltreatment can play a critical role in protecting children.
Keywords: Child abuse, abdominal trauma, screening
Introduction
Abusive abdominal trauma is the second leading cause of death among physically abused children, and may lead to significant morbidity among survivors.1,2 However, it may be difficult to diagnose and therefore even serious abdominal trauma may be missed.
In 1992, Coant and colleagues described a series of physically abused children who were screened for occult abdominal trauma by measuring transaminases and pancreatic enzymes.3 Of the 49 children screened, four had elevated transaminases, and three of the four had occult liver lacerations diagnosed by abdominal CT. Influenced in part by Coant’s findings, physicians evaluating children for suspected physical abuse increasingly began to screen children for occult abdominal trauma. Child abuse experts began recommending OAT screening, including a recommendation in an AAP policy statement on the evaluation of fractures suspicious for physical abuse.4–6
Ludwig, in a review of visceral injury in abuse, provided a strong justification for OAT screening. He described that abdominal injury may be overlooked due to young children’s limited verbal skills, delayed symptoms, low abdominal muscle tone and limited bruising, and physician focus on other, more overt injuries.4 Thus, he argued that even serious abdominal trauma may be overlooked.
Children with abusive abdominal injury appear to have higher mortality rates than children with similar severity, non-abusive injuries,7 and diagnostic delay may contribute to poor outcomes.8–12 In addition, delayed diagnosis of abusive abdominal injury may delay reporting to Child Protective Services (CPS) and police if other injuries are not clearly abusive. When the etiology of an injury is ambiguous, the presence of associated injury can help clarify the etiology as abuse. This, in turn, can lead to life-saving interventions, such as placing the child in a safe home environment.
Although child abuse experts have recommended OAT screening in children with suspected abuse,4–6 screening for OAT still appears to be sporadic. Further, the low incidence of overt abusive abdominal trauma (3 cases per million children) identified in a recent study has raised the question about whether the 6–8% rate of OAT in Coant’s study is generalizable to other populations of children.13 This retrospective study was therefore conducted in order to examine the rate of OAT among children with suspected physical abuse. A second objective was to identify characteristics of the child and family and the medical assessment that were associated with screening practice. Based on the epidemiology of other abusive injuries, we hypothesized that screening would occur more often among children who were young, minority, insured by Medicaid, and had more severe injuries. We also hypothesized that screening would occur less often when the emergency department was busy, and when subspecialty consultation was not provided.
Methods
Prior to initiating this research, the protocol was submitted to our Institutional Review Board and received an exemption from full IRB review. All medical records from the University of Maryland Medical Center were searched to identify children aged 0–5 years seen in the pediatric emergency department (ED) and diagnosed with definite or possible physical abuse, but without suggestion of abdominal trauma, between January 1, 1997 and December 31, 2005. Abusive injuries primarily included bruising, abrasions, burns, falls, fractures, and/or head trauma. Children were identified using International Classification of Disease version 9 (ICD-9) codes and External Cause of Injury (E)-codes for child abuse (ICD-9 code of 995.5 and E-code of 960–969).
In order to capture physically abused children who were not given child abuse diagnostic codes, all charts of children seen in the ED for injuries were also reviewed. If the ICD-9 code, E-code, or clinical diagnosis did not clearly indicate whether the injury was abusive vs. non-inflicted, the record was reviewed by at least one investigator to clarify the nature of the injury. Charts with any notation of reporting to Child Protective Services for suspected physical abuse were added to the sample. Children with a history and/or physical exam suggestive of abdominal trauma, regardless of etiology, were excluded. Also excluded were children who died in the ED, as an autopsy would obviate the need to screen for occult abdominal trauma.
Identified charts were reviewed to determine whether screening for occult abdominal trauma was conducted, and if so, the specific tests performed and the results of those tests. Additional data included all injuries, the history and symptoms at presentation, any studies obtained (e.g., skeletal survey and head CT, abdominal CT or ultrasound), and subspecialist consultations. The status of the ED attending (faculty or moonlighter) was noted, as was the time of day and year that the child presented. Demographic information, including age, race/ethnicity, sex, and insurance status was also collected.
OAT screening tests reviewed included liver transaminases (ALT and AST), pancreatic enzymes (amylase and lipase), urine for occult blood (dipstick and microscopic analysis), as well as stool for occult blood. Screening was considered to have occurred if at least one screening test was performed. So as not to miss any positive screening tests, we established somewhat low threshold values for positive screening tests. Tests considered positive included any ALT ≥70 IU/L, AST 80 ≥IU/L, amylase 90 ≥IU/L, lipase ≥50 IU/L, urine dipstick with ≥ 3+ blood, urine microscopic analysis with ≥ 20 red blood cells per high powered field, or a hemoccult positive stool.
Charts of children with positive OAT screening were examined to determine whether any additional testing (e.g. abdominal CT or ultrasound) had been performed to confirm or exclude abdominal trauma. Results of these tests were recorded.
Year of presentation was dichotomized into 1997–2001 and 2002–2005, as there was a large jump in the rate of screening between 2001 and 2002. Presentation time was dichotomized into evening presentation (4 – 11 pm) and non-evening presentation (all other times) as 4–11 pm is often the busiest time in the ED.
Data Analysis
OAT screening was the primary dependent variable, and was dichotomous – screening occurred if at least one screening test had been performed. Characteristics of the sample were described using means, medians, frequencies and proportions. Bivariate analyses included t-tests and chi-square tests, with Mann-Whitney U tests used for non-normal continuous variables.
Logistic regression was used for multivariate analysis to identify factors predictive of OAT screening. Independent variables included in the multivariate analysis were those that were significant in bivariate analyses. For multivariate analysis, a variable for subspecialty consultation was created and considered positive if any subspecialist (other than the Child Protection Team) had provided consultation. Child Protection Team (CPT) consultation was retained as a variable as we were interested in the specific effect of CPT consultation. Significant associations were identified between types of injuries (e.g. AHT and fractures), between injuries and CPT or other consultations, and between CPT and other consultations. Therefore separate models were developed for each injury variable and each consultation variable. Models were validated using the technique of Hosmer and Lemeshow.14
Results
A total of 244 children presented to the ED with possible abusive injuries during the time frame of the study. Of these, 65% were male, 42% were less than 1 year of age, 81% were African-American, and 87% were insured by Medicaid (Table 1). Half of the children (n=122) presented with bruises, although 30% of those also had other injuries. Seventy children presented with fractures, and 5% presented with probable abusive head trauma. Twenty percent of caregivers had no explanation for their child’s injuries.
Table 1.
Characteristics of the Sample with Suspected Physical Abuse (N=244)
| Characteristic | Number | Percent | |
|---|---|---|---|
| Demographics | Male | 156 | 65% |
| Age 0–11 months | 102 | 42% | |
| Age 12–35 months | 72 | 29% | |
| Age ≥36 months | 70 | 29% | |
| African American | 185 | 81% | |
| White | 42 | 18% | |
| Insured by Medicaid | 125 | 87% | |
| Symptoms at presentation |
Irritability | 36 | 15% |
| Lethargy | 9 | 4% | |
| Seizures | 10 | 4% | |
| Pain | 61 | 25% | |
| Not eating | 5 | 2% | |
| History at presentation |
No history of trauma | 49 | 20% |
| History does not fit with injury | 42 | 17% | |
| Fall | 38 | 16% | |
| History of child being abused | 37 | 15% | |
| Delay in seeking medical care | 25 | 10% | |
| Changing history | 19 | 8% | |
| Confessed abuse | 16 | 7% | |
| Self-inflicted injury | 12 | 5% | |
| Medical evaluation | Skeletal survey | 122 | 71% |
| Head CT | 83 | 34% | |
| Child Protection Team (CPT) consult | 68 | 28% | |
| Injuries | Bruise | 122 | 50% |
| Bruise only | 85 | 35% | |
| Burn | 37 | 15% | |
| Burn only | 30 | 12% | |
| Fracture | 70 | 29% | |
| Fracture only | 42 | 17% | |
| Probable abusive head trauma (subdural hemorrhage + retinal hemorrhage) |
13 | 5% | |
| Possible abusive head trauma (subdural hemorrhage +/− retinal hemorrhage) |
24 | 10% | |
| Other injury (abrasion, frenulum tear, oropharyngeal injury, etc.) |
16 | 7% | |
| Screening | Any screening for OAT | 51 | 21% |
| ALT and/or AST | 40 | 16% | |
| Amylase and/or lipase | 26 | 11% | |
| Urine dipstick | 28 | 12% | |
| Urine microscopic analysis | 21 | 9% | |
| Stool Hemoccult | 5 | 2% | |
| Screening occurred and positive | 21 | 41% | |
| Screening occurred, was positive and also identified by CT and/or ultrasound |
5 | 2% | |
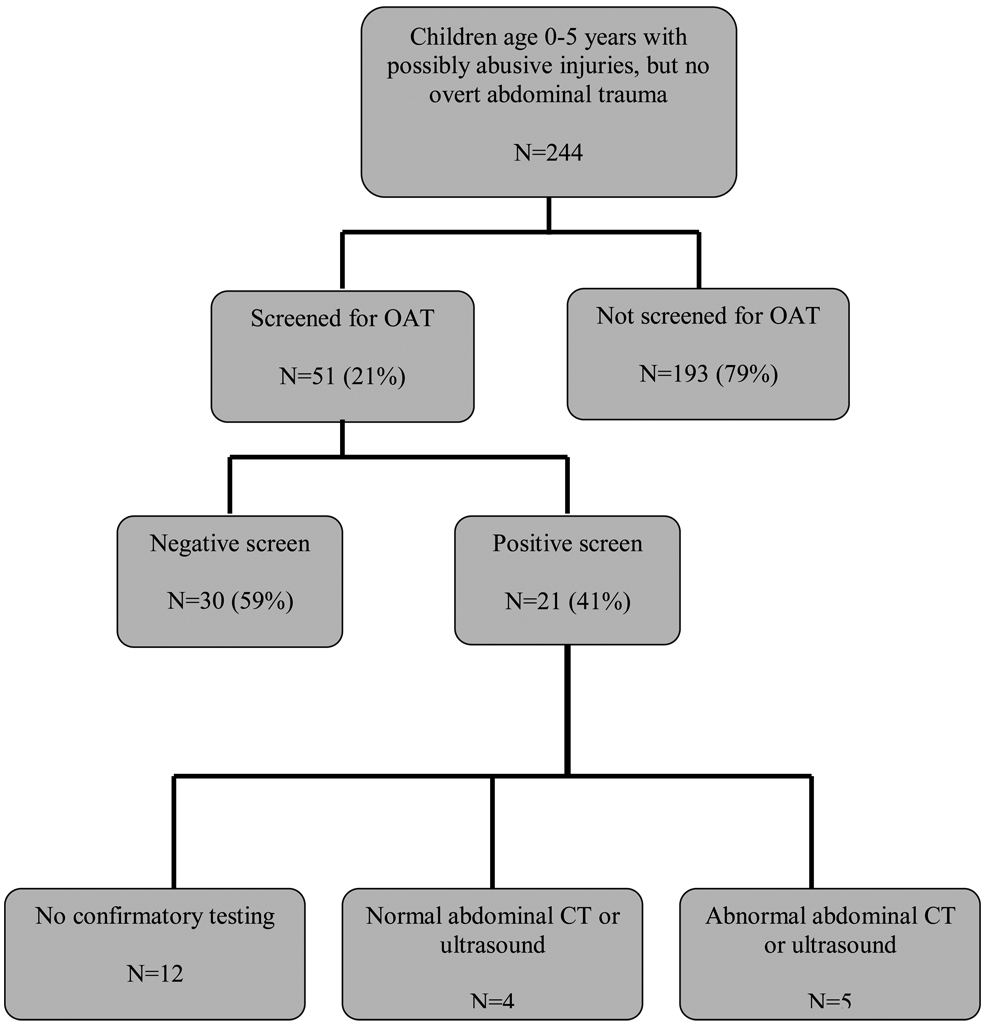
Approximately 20% (n=51) of children had at least one screening test for OAT performed (Table 1 and Figure). While 21 of the 51 children who were screened had positive screening tests, only 9 had confirmatory testing by abdominal CT and/or ultrasound. Five children (10% of those screened, 2% of the full sample) had injuries identified on abdominal CT and/or ultrasound; specific finding shown in Table 2. Among children aged 12–23 months, 5% of the total sample had injuries identified on abdominal imaging. Imaging findings often did not clearly indicate trauma, and several identified injuries were unrelated to the positive screening tests (Table 2). Possible splenic trauma was identified in two children, while an adrenal hemorrhage and possible lung contusion were found in two other children. Of the 5 children with ALT >250 IU/L and/or AST >450 IU/L, four had evidence of intra-abdominal injury on CT or ultrasound, and 3 others had evidence of liver injury, providing positive predictive values of 60–80%.
Figure.
Screening Procedure
Table 2.
Children Suspected of Having Been Physically Abused with Positive Screens for Occult Abdominal Trauma and Injury Identified on Abdominal CT or Ultrasound*
| Child | Clinical History | ALT | AST | Amy | Lip | CT or U/S |
Imaging Results |
|---|---|---|---|---|---|---|---|
| 1 | 1 month old found not breathing, unresponsive. Subdural hemorrhage, retinal hemorrhages |
347** | 326 | 30 | 10 | U/S | Fluid surrounding spleen, possible subcapsular collection. “Ascites surrounding liver” |
| CT | Large right sided pleural effusion Left sided rib fracture Left flank soft tissue swelling |
||||||
| 2 | 16 month old who “fell off the couch.” Bruises on wrists, head and neck. |
247 | 551 | 434 | 1070 | CT | “Density of lingula of lung” (contusion vs. infiltrate vs. atelectasis). |
| 3 | 18 month old with vague history of fall. Presented with vomiting, lethargy, seizures, and then respiratory failure. Subdural hemorrhage |
422 | 904 | 1761 | 3364 | CT | Dilated, fluid-filled segments of small bowel. Free fluid in intra- abdominal cavity. Possible splenic trauma. |
| 4 | 2 ½ year old with bruises and abrasions to arms, head, neck, and back. Mother’s boyfriend said he threw child in a trash can because a pit bull was chasing them. |
2695 | 1954 | 72 | 104 | CT and U/S |
Adrenal hemorrhage |
| 5 | 5 month old with vague history of fall, large head. Subdural hemorrhage, multiple healing rib fractures. |
29 | 66 | 120 | 387 | U/S | “Coarse echogenicity of liver.” Normal pancreas. |
Urine dipstick, urine micro and stool hemoccult not listed because the tests were either not performed, or were negative. All test results are measured in IU/L.
Numbers in bold indicate abnormal values.
Twelve children with positive screening tests did not have evaluation by CT or ultrasound. Eight of the twelve had only mildly elevated transaminases or lipase (ALT≤120, AST<130, and/or lipase ≤ 80). One child with significantly elevated transaminases and 3+ blood on urine dipstick had anoxic brain injury. Three additional children had microscopic hematuria – two of these children had specimens collected via urine bag. The method of collection for the third child was not documented in the chart.
Occurrence of OAT screening was not associated with most of the demographic variables examined, including race, gender, and insurance status. However, children <18 months of age were less likely to be screened compared to older children (11% vs. 30% screened, p<0.01). Children presenting in the evening, between 4 and 11 p.m., were screened less often than children presenting at other times of the day (10% vs. 25% screened, p<0.01).
Consultation from the CPT, surgery, neurosurgery, or ophthalmology all increased the likelihood of OAT screening. Children who had a skeletal survey or head CT performed were more likely to receive OAT screening than those who did not have these radiologic tests. Screening occurred more frequently after 2001 compared to before (39% vs. 14%, p<0.01).
On multivariate analysis, several variables predicted OAT screening (Table 4). Screening occurred more often in children presenting with probable abusive head trauma [OR=20.4, 95% CI (3.6–114.6), p<0.01] compared to those presenting with other injuries. Subspecialty consultation from the CPT [OR=8.4, 95% CI (3.5–20.8), p<0.01] and from other subspecialists [OR=24.3, 95% CI (7.1–83.3), p<0.01] also increased the likelihood that OAT screening would occur. Screening occurred more often in 2001–2005 compared to earlier years [OR=3.2, 95% CI(1.5–7.3), p<0.01], and occurred less often during peak ED activity [OR=0.4, 95% CI(0.1–0.9), p=0.03].
Table 4.
Predictors of OAT Screening on Multivariable Analysis.
| Predictor | Odds of OAT Screening (95% Confidence Interval) |
P value |
|---|---|---|
| Bruise (present vs. absent)* | 0.9 (0.4 – 2.1) | 0.88 |
| Fracture (present vs. absent)* |
1.2 (0.6 – 2.7) | 0.59 |
|
Probable abusive head trauma (present vs. absent)* |
20.4 (3.6– 114.6) | <0.01 |
| Burn (present vs. absent)* | 0.5 (0.2 – 2.0) | 0.36 |
|
Child Protection Team consultation (yes vs. no)* |
8.5 (3.5 – 20.8) | <0.01 |
|
Other subspecialty consultation (yes vs. no)* |
24.3 (7.1 – 83.3) | <0.01 |
|
Skeletal survey obtained (yes vs. no)*§ |
22.3 (4.3 – 115.4) | <0.01 |
|
Year of injury (2001–2005 vs. 1997–2001)*§ |
3.3 (1.5 – 7.3) | <0.01 |
|
Evening presentation (4–11 p.m. vs. other time)*§ |
0.4 (0.1 – 0.9) | 0.03 |
| Age (continuous)*§ | 1.0 (1.0 – 1.1) | 0.7 |
Covariates in model included age, year of injury, evening presentation, skeletal survey obtained, and insurance status.
Odds ratios obtained from model including probable abusive head trauma. Odds Ratios and significance were similar in other models.
Discussion
Of the 244 children with likely abusive injuries in our study, 51 (21%) were screened for OAT, and 21 had one or more positive screening tests for OAT. This represents 41% of all children screened and at least 9% of all children with abusive injuries. These are conservative estimates assuming that no OAT was present among those children who were not screened. Our rate of 9% is similar to findings in other studies. For example, Coant found positive screens in 8% of children with suspected child abuse, and Isaacman examined children with non-inflicted trauma and found occult abdominal injury in 6%.3,15 OAT is therefore hardly rare in the context of possible physical abuse.
When examining the rate of occult injury confirmed by abdominal CT or ultrasound, we found that 10% of children screened had OAT, accounting for 2% of all children with physical abuse and 5% of toddlers. These rates are comparable to those of other studies of children with both inflicted (6%) and non-inflicted (4.8%) trauma.3,15 Our findings indicate that at a minimum, 2 of every 100 children under 5 years of age presenting with possibly abusive injuries also have occult abdominal injury, and 1 in 20 toddlers may have occult abdominal injury.
For a number of reasons, our rates of occult abdominal trauma can only be considered estimates. First, our data and that of other researchers suggest that abdominal ultrasound and CT are not true gold standards, and may miss some abdominal injuries. Even if the radiologic testing were considered the gold standard, the majority of children did not have ultrasound or abdominal CT performed. Therefore, the sensitivity and specificity of the laboratory tests could not be determined. Further, some of the children with abnormal screening tests did not have radiologic testing; therefore, we were unable to confirm the presence of abdominal injury. While most children in this group had only mildly elevated laboratory results, this does not eliminate the possibility of abdominal injury. The utility of both screening and diagnostic tests varied according to the abdominal organ of interest, as discussed below.
While several authors have found liver transaminases to be an accurate predictor of hepatic injury,15–18 with sensitivity of 93–100%, and specificity of 53–100%, a more recent publication indicated a much lower sensitivity of only 53%.19 Although we could not calculate sensitivity or specificity, we did find these screening tests to have reasonable predictive value. Our positive predictive value of 60–80% is higher than that of 43% in Isaacman’s study.15 While we did not find any obvious liver lacerations, findings such as ascites surrounding the liver, and coarse echogenicity of the liver are strongly suggestive of trauma, particularly in the context of elevated transaminases.20 Our high positive predictive value supports the recommendation to perform screening in children being evaluated for suspected physical abuse.
While three children had markedly elevated pancreatic enzymes, and all had CT or ultrasound performed, we did not find any obvious pancreatic lacerations. This finding might be construed as pancreatic enzymes not being predictive of pancreatic injury. However, other studies indicate that identification of pancreatic trauma by CT may be particularly difficult.21–23 Therefore, it is likely that some pancreatic injuries were present despite negative CT scans. This finding suggests that our estimates of OAT may be higher than our conservative estimate of 2% noted above.
We had hoped that stool Hemoccult would adequately screen for intestinal injury. Unfortunately, testing was only performed in two children, making it impossible to assess its utility. Given the possibility of bowel trauma, it seems prudent to perform this easy screen although its sensitivity in other studies ranged only from 25–60%.24,25 Results from several previous studies indicated that hematuria might also be an accurate predictor of renal injury.15,26–28 Unfortunately, the three children identified with hematuria did not have radiologic testing to evaluate for possible renal or bladder injury. Optimal practice should include further evaluation. Given the ease and low cost of these two tests, it appears reasonable to include them in screening children with suspected physical abuse.
Several children in our study had traumatic injuries such as a lung contusion and splenic trauma that could not have been identified through any specific screening test. These findings indicate that many children with abusive injuries may also have occult injuries that cannot be identified through non-invasive screening tests. The decision to search for such occult injury must therefore balance the risks of missing an injury, (e.g. bleeding, sepsis, death, return to an abusive caregiver) with the risks of radiation, sedation, and oral contrast required for abdominal CT, as well as the cost of CT or ultrasound.
We did not identify disparities in OAT screening by race, gender or insurance status, findings that were reassuring given previous studies demonstrating differential screening for abusive head trauma and occult skeletal injury by race,29, 30 and differences in diagnosis of abuse by social class.31 However, limited racial and socioeconomic variability in our sample made it difficult to examine differences.
We expected rates of screening to be higher for more severe injuries such as fractures and abusive head trauma. This was the case for the most part in our bivariate analyses. However, only abusive head trauma remained a predictor of screening in our multivariate analysis. It is likely that physicians considered abusive head trauma to be a more severe form of abuse than the other abusive injuries.
Subspecialty input clearly played a role in the decision to perform OAT screening. This may have reflected the severity of children’s injuries; children with more severe injuries were more likely to have subspecialty and CPT consultation, and were more likely to be screened because of the severity of injury. However, it may also be because subspecialists were more aware of the possibility of occult abdominal injury compared to the emergency department physicians.
Screening occurred less often during peak ED hours (4–11 p.m.). This finding suggests that physicians screen more often when they have more time to think about patient evaluation and management, and forget to screen when they are busy. Development of management pathways or computerized order templates could prompt physicians to screen when they might otherwise forget.
There were a number of limitations to this study. As it was a retrospective chart review, we could not guarantee that children would be screened for OAT, nor that children with positive screens would have a CT or ultrasound performed. Therefore, it is probable that some children with OAT were missed. This was a particular problem for the 3 children with hematuria who did not have abdominal imaging, as several studies have shown that hematuria is a good marker for intra-abdominal trauma among children with non-inflicted injury.15,26–28 We have therefore presented conservative estimates of the percentage of positive screens, assuming that none of the unscreened children had OAT, and noting the minimum percentage of children with OAT. Even with these conservative estimates, the proportion of physically abused children with OAT is high enough to warrant screening, at least for children under 3 years of age.
A second limitation was the small number of children with positive OAT screens and/or findings on abdominal CT or ultrasound. The low numbers precluded identifying factors associated with the presence of occult abdominal injury. Future prospective studies may better identify these factors, and provide more specific criteria for OAT screening.
The abdominal injuries in our study were not associated with significant morbidity. However, the presence of multiple injuries is potentially a marker for more serious abuse, with important implications for children’s health and safety.
Conclusions and Implications
Our findings support Coant’s recommendation for OAT screening with liver and pancreatic enzymes for physically abused children. Additional studies are needed to establish the utility of screening with urinalysis and stool Hemoccult. This study also supports the importance of subspecialty input, especially that of a child protection team, in the medical evaluation of suspected physical abuse. Although many identified injuries may not require treatment, their role in confirming abuse, or demonstrating the increased severity of maltreatment can play a critical role in protecting children from further abuse.
Table 3.
Predictors of OAT Screening on Bivariate Analyses
| 3A: Demographic Characteristics | |||
|---|---|---|---|
| Characteristic | % Screened (N) | P value | |
| Race | White (N=42) | 29% (12) | 0.13 |
| African-American (N= 185) | 18% (34) | ||
| Gender | Male (N=156) | 22% (32) | 0.7 |
| Female (N=85) | 21% (19) | ||
| Age | <18 months (N=122) | 30% (37) | <0.01 |
| ≥18 months (N=122) | 11% (14) | ||
| Insurance | Medicaid (N=137) | 23% (31) | 0.1 |
| Private (N=21) | 38% (8) | ||
| 3B: Characteristics Related to Emergency Department Evaluation | |||
|---|---|---|---|
| Characteristic | % Screened if “Yes” (N) |
% Screened if “No” (N) |
P value |
| Evening presentation (4 –11 pm) (N=80) |
10% (8) | 26% (42) | <0.01 |
| Moonlighter in ED (N=102) | 23% (23) | 23% (18) | 0.99 |
| ED visit after 2001 (N=69) | 39% (27) | 14% (24) | <0.01 |
| Skeletal survey (N=131) | 37% (49) | 2% (2) | <0.01 |
| Head CT (N=84) | 42% (38) | 6% (12) | <0.01 |
| Child Protection Team consult (N=68) |
59% (40) | 6% (11) | <0.01 |
| Surgery consult (N=24) | 67% (16) | 16% (35) | <0.01 |
| Ophthalmology consult (N=67) | 55% (37) | 8% (14) | <0.01 |
| Neurosurgery consult (N=25) | 76% (19) | 15% (32) | <0.01 |
Acknowledgments
Support for this work was provided, in part, by the University of Maryland General Clinical Research Center Grant M01 RR16500 General Clinical Research Centers Program (NCRR), National Institutes of Health
Abbreviations
- OAT
Occult abdominal trauma
- ED
Emergency Department
- CPS
Child Protective Services
- CPT
Child Protection Team
- OR
Odds Ratio
Footnotes
Financial disclosure and Conflict of interest: The authors have nothing to disclose
Contributor Information
Wendy Gwirtzman Lane, Department of Epidemiology and Preventive Medicine, Department of Pediatrics, University of Maryland School of Medicine.
Howard Dubowitz, Department of Pediatrics, Division of Child Protection, University of Maryland School of Medicine.
Patricia Langenberg, Department of Epidemiology and Preventive Medicine, University of Maryland School of Medicine.
References
- 1.Schnitzer PG, Ewigman BG. Child deaths resulting from inflicted injuries: Household risk factors and perpetrator characteristics. Pediatrics. 2005;116:e687–e693. doi: 10.1542/peds.2005-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood J, Rubin DM, Nance ML, Christian CW. Distinguishing inflicted versus accidental abdominal injuries in young children. J Trauma. 2005;59:1203–1208. doi: 10.1097/01.ta.0000196437.07011.b1. [DOI] [PubMed] [Google Scholar]
- 3.Coant PN, Kornberg AE, Brody AS, Edwards-Holmes K. Markers for occult liver injury in cases of physical abuse in children. Pediatrics. 1992;89:274–278. [PubMed] [Google Scholar]
- 4.Ludwig S. Visceral manifestations of child abuse. In: Reece RM, Ludwig S, editors. Child Abuse: Medical Diagnosis and Management. 2nd Ed. Philadelphia: Lippincott, Williams and Wilkens; 2001. pp. 157–176. [Google Scholar]
- 5.Jenny C. for the Committee on Child Abuse and Neglect. Evaluation of infants and young children with multiple fractures. Pediatrics. 2006;118:1299–1303. doi: 10.1542/peds.2006-1795. [DOI] [PubMed] [Google Scholar]
- 6.Alexander RC, Levitt CJ, Smith WL. Abusive head trauma. In: Reece RM, Ludwig S, editors. Child Abuse: Medical Diagnosis and Management. 2nd Ed. Philadelphia: Lippincott, Williams and Wilkens; 2001. pp. 47–80. [Google Scholar]
- 7.Trokel M, DiScala C, Terrin NC, Sege RD. Blunt abdominal injury in the young pediatric patient: Child abuse and patient outcomes. Child Maltreatment. 2004;9:111–117. doi: 10.1177/1077559503260310. [DOI] [PubMed] [Google Scholar]
- 8.Canty TG, Canty TG, Jr., Brown C. Injuries of the gastrointestinal tract from blunt trauma in children: A 12-year experience at a designated pediatric trauma center. J Trauma. 1999;46:234–240. doi: 10.1097/00005373-199902000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Cooper A, Floyd T, Barlow B, Niemirska M, Ludwig S, Seidl T, et al. Major blunt abdominal trauma due to child abuse. J Trauma. 1988;28:1483–1487. doi: 10.1097/00005373-198810000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Sung CK, Kim KH. Missed injuries in abdominal trauma. J Trauma-Injury, Infection & Critical Care. 1996;41:276–282. doi: 10.1097/00005373-199608000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Olah A, Issekutz A, Haulik L, Makay R. Pancreatic transaction from blunt abdominal trauma: early versus delayed diagnosis and surgical management. Digestive Surgery. 2003;20:408–414. doi: 10.1159/000072708. [DOI] [PubMed] [Google Scholar]
- 12.Ozturk H, Onen A, Otcu S, Dokucu AI, Yagmur Y, Kaya M, Yucesan S. Diagnostic delay increases morbidity in children with gastrointestinal perforation from blunt abdominal trauma. Surg Today. 2003;33:178–182. doi: 10.1007/s005950300040. [DOI] [PubMed] [Google Scholar]
- 13.Barnes PM, Norton CM, Dunstan FD, Kemp AM, Yates DW, Sibert JR. Abdominal injury due to child abuse. Lancet. 2005;366:234–235. doi: 10.1016/S0140-6736(05)66913-9. [DOI] [PubMed] [Google Scholar]
- 14.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley & Sons; 1989. [Google Scholar]
- 15.Isaacman DJ, Scarfone RJ, Kost SI, et al. Utility of routine laboratory testing for detecting intra-abdominal injury in the pediatric trauma patient. Pediatrics. 1993;92:691–694. [PubMed] [Google Scholar]
- 16.Hennes HM, Smith DS, Schneider K, et al. Elevated liver transaminase levels in children with blunt abdominal trauma: a predictor of liver injury. Pediatrics. 1990;86:87–90. [PubMed] [Google Scholar]
- 17.Oldham KT, Guice KS, Kaufman RA, Martin LW, Noseworthy J. Blunt hepatic injury and elevated hepatic enzymes: A clinical correlation in children. J Ped Surg. 1984;19:457–461. doi: 10.1016/s0022-3468(84)80275-4. [DOI] [PubMed] [Google Scholar]
- 18.Puranik SR, Hayes JS, Long J, Mata M. Liver enzymes as predictors of liver damage due to blunt abdominal trauma in children. S Med J. 2002;95:203–206. [PubMed] [Google Scholar]
- 19.Karam O, La Scala G, Le Coultre C, Chardot C. Liver function tests in children with blunt abdominal traumas. Eur J Pediatr Surg. 2007;17:313–316. doi: 10.1055/s-2007-965533. [DOI] [PubMed] [Google Scholar]
- 20.Rathaus V, Zissin R, Werner M, Erez I, Shapiro M, Grunebaum M, Konen O. Minimal pelvic fluid in blunt abdominal trauma in children: The significance of this sonographic finding. J Ped Surg. 2001;36:1387–1389. doi: 10.1053/jpsu.2001.26377. [DOI] [PubMed] [Google Scholar]
- 21.Udekwu PO, Gurkin B. The use of computed tomography in blunt abdominal injuries. American Surgeon. 1996;62:56–60. [PubMed] [Google Scholar]
- 22.Benya EC, Lim-Dunham JE, Landrum O, Statter M. Abdominal sonography in examination of children with blunt abdominal trauma. AJR. 2000;174:1613–1616. doi: 10.2214/ajr.174.6.1741613. [DOI] [PubMed] [Google Scholar]
- 23.Tas F, Ceran C, Atalar MH, Bulut S, Selbes B, Isik AO. The efficacy of ultrasonography in hemodynamically stable children with blunt abdominal trauma: a prospective comparison with CT. Euro J Radiol. 2004;51:91–96. doi: 10.1016/S0720-048X(03)00145-1. [DOI] [PubMed] [Google Scholar]
- 24.Rosenthal P, Jennings MT. Comparison of fecal occult blood tests for detection of gastrointestinal bleeding in pediatric patients. Am J Gastroenterol. 1992;87:1575–1579. [PubMed] [Google Scholar]
- 25.Harewood GC, McConnell JP, Harrington JJ, Mahoney DW, Ahlquist DA. Detection of occult upper gastrointestinal tract bleeding: performance differences in fecal occult blood tests. Mayo Clin Proc. 2002;77:23–28. doi: 10.4065/77.1.23. [DOI] [PubMed] [Google Scholar]
- 26.Brown SL, Haas C, Dinchman KH, et al. Radiologic evaluation of pediatric blunt renal trauma in patients with microscopic hematuria. World Journal of Surgery. 2001;25:1557–1560. doi: 10.1007/s00268-001-0149-6. [DOI] [PubMed] [Google Scholar]
- 27.Holmes JF, Sokolove PE, Lane C, Kuppermann N. Identification of intra-abdominal injuries in children hospitalized following blunt abdominal trauma. Acad Emerg Med. 1999;6:799–806. doi: 10.1111/j.1553-2712.1999.tb01210.x. [DOI] [PubMed] [Google Scholar]
- 28.Taylor GA, Eichelberger MR, Potter BM. Hematuria. A marker of abdominal injury in children after blunt trauma. Ann Surg. 1988;208:688–693. doi: 10.1097/00000658-198812000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281(7):621–626. doi: 10.1001/jama.281.7.621. [DOI] [PubMed] [Google Scholar]
- 30.Lane WG, Rubin D, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288:1603–1609. doi: 10.1001/jama.288.13.1603. [DOI] [PubMed] [Google Scholar]
- 31.Lane, Dubowitz What factors affect the identification and reporting of child abuse related fractures? Clinical Orthopedics and Related Research. 2007;461:219–225. doi: 10.1097/BLO.0b013e31805c0849. [DOI] [PubMed] [Google Scholar]