Abstract
Objective
To investigate how sociocultural factors influence management of pain from sickle cell disease by comparing the experiences of those who usually manage their pain at home with those who are more frequently admitted to hospital for management of their pain.
Design
Qualitative analysis of semistructured individual interviews and focus group discussions.
Participants
57 participants with genotype SS or S/β-thal (44 subjects) or SC (9) (4 were unknown). 40 participants took part in focus groups, six took part in both focus groups and interviews, and nine were interviewed only. Participants were allocated to focus groups according to number of hospital admissions for painful crisis management during the previous year, ethnic origin, and sex.
Results
The relation between patients with sickle cell disease and hospital services is one of several major non-clinical dimensions shaping experiences of pain management and behaviour for seeking health care. Experiences of hospital care show a range of interrelated themes, which are common to most participants across variables of sex, ethnicity, and hospital attended: mistrust of patients with sickle cell disease; stigmatisation; excessive control (including both over- and undertreatment of pain); and neglect. Individuals respond to the challenge of negotiating care with various strategies. Patients with sickle cell disease who are frequently admitted to hospital may try to develop long term relationships with their carers, may become passive or aggressive in their interactions with health professionals, or may regularly attend different hospitals. Those individuals who usually manage their pain at home express a strong sense of self responsibility for their management of pain and advocate self education, assertiveness, and resistance as strategies towards hospital services.
Conclusions
The current organisation and delivery of management of pain for sickle cell crisis discourage self reliance and encourage hospital dependence. Models of care should recognise the chronic nature of sickle cell disorders and prioritise patients’ involvement in their care.
Key messages
The chronic nature of sickle cell disorders has been insufficiently recognised, with policy and services oriented towards the acute management of a minority of those affected
Experiences of pain and patterns of hospital admission for sickle cell crisis may be influenced by sociocultural and psychological factors as well as disease severity
The experiences of patients with sickle cell disease of hospital care are characterised by mistrust, stigmatisation, control, and neglect
Individuals who usually manage their pain at home show different attitudes and strategies towards hospital services from those who are frequently admitted to hospital
Models of care should acknowledge the diversity of the population with sickle cell disorders and prioritise the involvement and empowerment of patients
Introduction
The management of sickle cell disorders is of growing concern for health professionals and policymakers in the United Kingdom. Painful crises are the dominant feature of sickle cell disorders both for individual suffering and for service use.1 In the United States most painful episodes are managed at home,2,3 and many patients with sickle cell disease do not normally use health services for management of pain.2 Analysis of patterns of treatment seeking in the United Kingdom is hindered by the lack of coordinated information about the affected population.4 Ongoing analysis of data of hospital admissions and estimated population figures, however, suggest a similar pattern of service use to that in the United States, with a small percentage of the affected population consuming a disproportionate amount of resources. Most previous research has systematically excluded individuals with infrequent hospital contact5 assuming they experience little or no severe pain. Those who manage their pain at home have been similarly neglected by the organisation of health services, which have focused on acute management rather than primary and community care. Published research tends to ignore both the experiences of individuals who manage their pain in the community and the influence of non-clinical factors on treatment seeking behaviour.
Biomedical approaches to pain have traditionally conceptualised experiences of pain as fundamentally individual and purely biological.6 Our investigation draws upon the anthropological understanding that sociocultural factors influence the perception, response to, and communication of pain.7 Similarly, treatment seeking is a social action influenced by social context and individual meanings and experience, and not simply a straightforward individual response to the experience of physiological symptoms. We aimed to compare the experiences of pain and its management by patients with sickle cell disease with differing frequencies of hospital admissions, and to identify non-clinical factors contributing to patterns of service use. Given the lack of prior research on this issue we have used mainly qualitative methods8 to gain insight into the range of possible factors influencing experiences.
Participants and methods
We used focus group discussions and semistructured individual interviews as our main methods.
Participants
Overall, we recruited 57 subjects with sickle cell disease (haemoglobin type SS or S/β-thal or SC) across Greater London using theoretical sampling9 (systematic non-random sampling of participants possessing specific characteristics selected to aid the development of theory) via a wide range of channels (table 1). The main study groups comprised participants admitted to hospital with a painful crisis three or more times in the previous 12 months, and those admitted once or not at all.
Table 1.
Channels of recruitment
| Channel | No (%) of hospital admissions per year
|
|
|---|---|---|
| 3 or more (n=28) | 1 or fewer (n=29) | |
| Researcher visiting inpatients | 9 (32) | 0 (0) |
| Referral by counsellor or specialist nurse | 8 (29) | 9 (31) |
| Snowballing* | 3 (11) | 1 (3) |
| Participant in previous research | 2 (7) | 2 (7) |
| Researcher visiting outpatient clinic | 6 (21) | 11 (38) |
| Media | 0 (0) | 2 (7) |
| Mail-out | 0 (0) | 2 (7) |
| Referral by general practitioner | 0 (0) | 2 (7) |
Recruitment of further participants by networks of those already participating.
Ethical approval for the study was obtained from the research ethics committee of St Thomas’s Hospital. All participants completed consent forms before participating in interviews or focus groups.
Structured questionnaire
All participants completed a short structured questionnaire before taking part in an interview or focus group, or both, to collect sociodemographic data (table 2) and information on haemoglobin status, usual analgesic drugs, and current treatment (table 3). Participants were asked about frequency of hospital admissions and painful episodes. The definition of painful episodes was similar to that used in previous studies10: “pain which was in any part of your body, lasted at least two hours, you felt was caused by sickle cell, and may or may not have led you to go to hospital.”
Table 2.
Demographic characteristics of participants
| Characteristic | No (%) of participants (n=57) |
|---|---|
| Ethnic origin | |
| West African | 29 (51) |
| Afro-Caribbean | 26 (46) |
| Other African | 2 (4) |
| Sex | |
| Female | 32 (56) |
| Male | 25 (44) |
| Age group (years) | |
| 20-40 | 49 (86) |
| 41-60 | 6 (11) |
| Missing data | 2 (4) |
| Mean age | 34 |
Table 3.
Haemoglobin status and hospital treatment. Values are number (percentage)
| Variable | Participants (n=57)* | Hospital admissions per year
|
|
|---|---|---|---|
| 3 or more (n=28) | 1 or fewer (n=29) | ||
| Haemoglobin status | |||
| SS or S/β-thal | 44 (77) | 24 (42) | 20 (35) |
| SC | 9 (16) | 4 (7) | 5 (9) |
| Don’t know | 4 (7) | 0 (0) | 4 (7) |
| Transfusions and hydroxyurea | |||
| Transfusion ever | 43 (75) | 19 (33) | 24 (42) |
| Transfusion regimen currently | 4 (7) | 4 (7) | 0 (0) |
| Using hydroxyurea | 5 (9) | 5 (9) | 0 (0) |
| Missing data | 5 (9) | 0 (0) | 5 (9) |
| Usual drugs in hospital | |||
| Pethidine, diamorphine, or morphine, or a combination (strong analgesia) | 45 (79) | 27 (47) | 18 (32) |
| No pethidine, diamorphine, or morphine, or a combination (not strong analgesia) | 7 (12) | 0 (0) | 7 (12) |
| Missing data | 5 (9) | 1 (2) | 4 (7) |
| No of self reported painful episodes in previous 2 years | |||
| 1-2 | 2 (4) | 0 (0) | 2 (4) |
| 3-10 | 17 (30) | 5 (9) | 12 (21) |
| 11-20 | 12 (21) | 4 (7) | 8 (14) |
| 21-30 | 8 (14) | 4 (7) | 4 (7) |
| ⩾30 | 13 (23) | 11 (19) | 2 (4) |
| Missing data | 5 (9) | 4 (7) | 1 (2) |
Painful episodes do not total 100% owing to rounding up.
Interviews
We conducted 18 semistructured interviews with 15 individuals in settings chosen by the participants. Six pilot interviews were conducted before the focus groups to develop the topic guide. Ten interviews were conducted in parallel with the focus groups with individuals spending significant time in hospital who were unable to attend a focus group.
Focus groups
Participants were allocated to one of eight different focus groups on the basis of information provided in the questionnaires; the composition of each group was determined by ethnic origin (Afro-Caribbean or west African), sex, and number of hospital admissions in the previous year (three or more, or one or fewer). Each group met for two discussions of 1.5 to 2.5 hours. The main topics discussed in the focus groups were: diagnosis, childhood and adult experiences of pain, hospital experiences, primary care, analgesia, anatomy of a crisis, employment and education, support and relationships, and identity and lifestyle. All focus groups were facilitated by KM (the only non-participant present) whose role was to introduce the topics, to ask questions, and to encourage participation by all group members. The facilitator aimed to maintain a balance between covering the intended topics and allowing for the introduction of unanticipated issues that participants deemed relevant.
Statistical analysis
We analysed the data from the quantitative questionnaire using Epi-Info (version 6.0). The qualitative data consisted of the transcripts of focus group discussions and interviews. All qualitative data were professionally transcribed; the main researcher then corrected the transcripts against the original recordings for accuracy and inclusion of non-verbal detail (such as laughter, murmured assent, etc). Owing to the large volume of data AS did not listen to the recordings or participate in coding but read all transcripts and discussed the evolving coding framework at regular intervals. We used Nud*ist software for the analysis of the qualitative data (version 4, Qualitative Solutions and Research, Victoria, Australia). Coding categories were developed from the data rather than using a predetermined analytic framework. Text units (each uninterrupted segment of speech constitutes a unit) were grouped together according to perceived common underlying themes. As coding progressed each of these general themes was further subdivided as a greater understanding of the complexities of the data developed. The identification of horizontal relations between coding categories was a parallel process eventually leading to the development of an explanatory model, an aspect of which is presented here.
Validation
At the end of the study, information on the results of laboratory electrophoresis was obtained for most cases and compared with participants’ self reported haemoglobin status. The researcher also validated the accuracy of participants’ reported pattern of admissions in cases where there was any doubt by discussion with haemoglobinopathy counsellors and staff of outpatient clinics.
Questionnaire results
Twelve different London hospitals were named by participants as their base hospital; two participants reported regular attendance at several different hospitals. Patients admitted infrequently were less likely to use strong opioids and more likely to use mild analgesic in hospital (table 3). The proportion requiring strong analgesics was 100% for those admitted three or more times compared with 72% for those admitted less than three times (95% confidence interval for the difference of the proportions between groups 10% to 46%). There was considerable overlap in number of painful episodes between those admitted frequently and those who usually managed their pain at home (table 3): half of those who managed their pain at home had experienced 10 or more painful episodes during the previous 2 years. Of the 51 cases where self reported results were compared with laboratory results there was agreement in all cases of SS or S/β-thal (40 cases) and SC (9). Two (of a total of four) cases where participants did not report or did not know their haemoglobin status were identified as being SS (both of these were patients who managed their pain at home).
Qualitative results
We identified sociocultural and psychological factors which, along with differences in clinical severity, may contribute to variation in patterns of hospital use by individuals with sickle cell disorders. We focused on two main themes: experiences of hospital care, and strategies for management of pain and treatment seeking.
Experiences of hospital care
Our findings related to general aspects of hospital experience that were consistent for most participants, although a few individuals had very little experience of hospital care.
Mistrust
Participants gave accounts of mistrust by their professional carers. In all of the groups who were frequently admitted to hospital (groups 1-4) and two of the groups who managed their pain at home (groups 5-8) participants described being suspected by health professionals of exaggerating pain:
“The doctor will look at you, and he goes “I don’t think that you’re in a lot of pain.” (Focus group 1.1; text units 830.)
In contrast, some participants managing their pain at home described how health professionals seemed to suspect them of understating their pain levels:
“They get suspicious because they can’t believe you can be better in two days, but if I can look after myself, I don’t see why I should be there ... I feel better, I can stop taking [the painkillers] ... Once I didn’t have no more pain but they [were] giving me tablets which I didn’t know [were] painkillers.” (Focus group 7.2; text units 116-119.)
Stigmatisation
The perception of patients with sickle cell disease that they were treated differently from other inpatients was a prominent theme in all focus groups and interviews. Virtually all participants thought that patients with sickle cell disease were stigmatised as drug addicts—a stereotype which simultaneously feeds on and reinforces the mistrust of patients with sickle cell disease described above:
“The nurse turned around to me and said “It’s not because we don’t wanna give you the painkillers, it’s cos we’re scared that you’re gonna get hooked on it and we don’t wanna see you down on the street hustling drugs.” (Focus group 3.2; text units 274.)
Control
The issue of control related closely to mistrust and stigmatisation. Participants described various ways in which health professionals routinely exerted control over their care regimens and failed to involve them in decision making particularly in relation to giving drugs (overtreatment as well as undertreatment of pain), hospital admissions, and discharge.
P: “They give me diamorphine, but I try to take as small as I can—sometimes they push.”
KM: “They want you to take more?”
P: “Yes. They keep saying to me, “Oh the pain will come again.” And I say, “When the pain comes, I will tell you.” (Focus group 7.2; text units 195-199.)
P1: “You do tend to find certain nurses who like to overstep their bounds, they feel they know the best regime for your painkillers ...”
P2: “Absolutely.”
P1: “They feel that you should be having less than ... on the prescription ... and they will try and control your pain regime to the way they think it should go.” (Focus group 2.1; text units 434-442.)
“They kept saying, ‘I think we’re going to send you home,’ and yet I knew it was the sort of chest pain that I should be in ... So there was this debate ... in the end I was right—it was sickle lung.” (Focus group 5.2; text units 246-247.)
Neglect
Participants spoke of neglect of a range of needs including personal care and monitoring of vital signs. Some participants related such neglect to wider issues such as understaffing, whereas others interpreted it as further evidence that patients with sickle cell disease were a low priority for health professionals. Failure to provide adequate psychosocial support was also included as an example of neglect although this is a major issue that we can only refer to briefly here.
“[The nurses] just seem to concentrate on the pethidine injections and that’s it. I’ve been in days without having any assistance with my hygiene and personal care, and changing of the sheets and helping me with fluids—just basic stuff like that.” (Interview 11; text unit 122.)
“On [names ward] observations wasn’t done ... If they come round and you’re asleep then they leave you ... Sometimes they’ve already written in what your temperature is but the thermometer is still under your arm.” (Interview 3; text units 721-738.)
“You need to talk about what’s bothering you, but that is not an issue when you go in hospital—they see that you’ve got sickle cell and that’’s it ... I went into a state where I was practically suicidal and nobody recognised nothing except that I had sickle crisis.” (Focus group 1.2; text unit 1108.)
Strategies for management of pain and treatment seeking
The extent to which individual relations with pain had been shaped by these experiences was variable, and individuals responded differently to the challenges of negotiating management of pain and general care. Those who normally managed pain at home showed different strategies from those who were frequently admitted to hospital.
Strategies of patients managing pain at home
Strategies of patients managing pain at home were typified by two main characteristics: a sophisticated critical appraisal of hospital services, which acknowledged that spending time in hospital was often not in their own best interest, and a strong sense of self responsibility for the management of their condition, which included a recognition of the power of mental attitudes.
Assertiveness
“People think, ‘Oh the doctor knows best,’ but I think the patient knows best, because really if you don’t believe in yourself, no matter what the doctors do, it’s not gonna help you. You have to have that self power to say, ‘Look, enough’s enough.’ Because how long are you going to carry on taking all these different drugs, how long are you going to keep on dealing with the side effects?” (Focus group 7.2; text unit 220.)
Self education
“I think you do have to educate yourself because you’ll be in wards where nurses have never seen a sickler ... it didn’t come up in their training ... so I think it really comes down to you at the end of the day.” (Focus group 6.2; text unit 1346.)
Resistance
“I’d work during the day ... in agony, go home ... take the pethidine through the night, get up the next morning, go to work again without taking any drugs—in pain, agony—come home in the evening and repeat the same thing again. So you’re always trying to fight with it.” (Focus group 6.1; text unit 761.)
“It’s good to try and have a positive mind, not ‘Oh the pain’s here I’m gonna just let it take over me,’ not lie down in hospital for weeks on end, getting them to drug you up ’til God knows.” (Focus group 7.3; text unit 454.)
“Sometimes you want to fight it and you don’t want to go into hospital, because you know what hospital is and you know what staying out of hospital can do, and you know whether you’re going to be better within 2 or 3 days of staying at home, hopefully, or you may be in [hospital] a week or 10 days. So it’s all about mental toughness ...” (Focus group 8.2; text unit 737.)
Strategies of patients frequently admitted to hospital
Participants who were more frequently admitted to hospital commonly advocated the benefits of developing long term relationships with carers in one hospital to receive more individualised care. This strategy may be thwarted by the high turnover of ward nurses and junior doctors; some participants stressed the significance of their relationship with their consultant as a bulwark against mismanagement and unsympathetic attitudes of junior staff. A minority of patients frequently admitted to hospital may resort to verbal and occasionally physical aggression, sometimes provoked by undertreatment of pain and poor communication with health professionals, at other times as an expression of unresolved anger. Others reported that they maintained a passive attitude in their interactions with their carers, which necessarily extended to their attitude towards their condition. Self discharging from one hospital and going straight to another in response to unsatisfactory care was a strategy employed by a minority of patients.
Developing relationships
“If you’re in a regular hospital where they know you ... they tend to be able to build up some form of relationship because they’ve seen you before. So they know exactly how your crisis behaves, how you usually cope. They can work with you.” (Focus group 1.1; text unit 1078.)
Aggression
“Every time I come to casualty, he [junior doctor] will send me home ... one day ... he cancelled my painkiller and said I would have to go home, and I said, ‘Today I’m not going home.’ ... So I held him and I punched him.” (Interview 12.1; text units 503-506.)
Passivity
“Whenever they [doctors and nurses] say anything to me that I don’t like I just let it go by ... Whatever they want to do, they can just do it to me.” (Interview 10; text units 201-203.)
Use of multiple hospitals
“I’ve been in many hospitals [names five; laughter from group] ... If I go to the hospital and my pain’s not controlled, I don’t care if I die, I’ll get out of that hospital and go somewhere else to get pain free or to control my pain ...” (Focus group 3.1; text unit 380.)
Discussion
In our study we have used methods that facilitated the emergence of participants’ own accounts of their experiences, with minimal imposition of a predetermined analytical framework. Our findings suggest how individual management of pain may be affected by experiences of, and responses to, health services. The comparative approach found similar experiences of hospital care in London, across variables of sex, ethnicity, and hospital. We also highlight striking differences in attitude towards hospital services between those who usually manage their pain at home and those who are more frequently admitted to hospital.
Our investigation has been innovative in including individuals with sickle cell disorders previously excluded from research; those usually managing their pain at home. The knowledge that some individuals with sickle cell disorders rarely experience severe pain may suggest that those managing their pain at home fall into this category. In the absence of an objective measure of clinical severity, we have used self reported frequency of painful episodes to measure pain in participants infrequently admitted to hospital. This imperfect indicator relies on subjective recall over a significant period. We think, however, that taken with participants’ accounts and the fact that many of those who usually managed their pain at home were known to counsellors or attended outpatient clinics (table 1), these data provide evidence that home management is not simply a reflection of lesser disease severity. Although the patients more frequently admitted to hospital reported a greater overall number of painful episodes, there was sufficient overlap between the two groups to show that they are not two clinically discrete populations. In addition, the two groups seemed to have a similar distribution of genotypes. Validation of patients’ self reported haemoglobin status (where known by patients) showed complete agreement with laboratory records, suggesting that accurate information was provided by the study respondents.
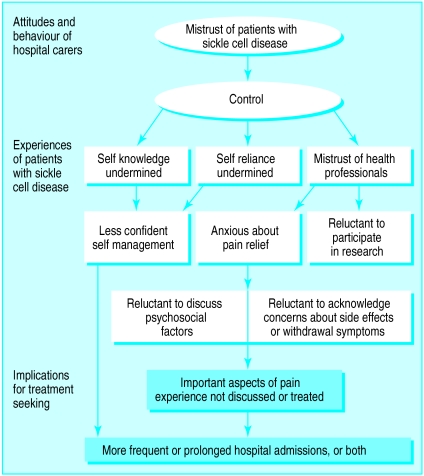
Hospital experiences and management of pain: explanatory model
Participants’ accounts of hospital care concord with previous research11–13 in highlighting issues of stigmatisation, lack of involvement in treatment decisions, and undertreatment of pain. Our findings, not previously described, suggest an explanatory model that illustrates the implications of health professional-patient relationships for individual management of pain (figure). A pervasive mistrust of patients with sickle cell disease leads health professionals to exert excessive control over their regimen for management of pain. Other studies have found that a significant proportion of health professionals may subscribe to the stereotype of patients with sickle cell disease as drug dependent.14,15 The undertreatment of pain from sickle cell disease has been described elsewhere11–13; our findings indicate that health professionals may also be overtreating pain particularly in those patients only rarely admitted to hospital. This observation suggests that the approach to treatment was not due solely to health professionals’ concerns about addiction, but also related to more fundamental issues of trust, control, and patient involvement. Failure to involve patients with sickle cell disease in making decisions about their care undermines self reliance and self knowledge, reducing capacity for self management. Repeated experiences of control and neglect erode patients’ trust in their professional carers leading to considerable anxiety about receiving adequate pain relief. Ballas16 has observed that “Patients with sickle cell disease often do not convey their true feelings about their management for fear of not receiving adequate treatment for pain.” Similarly, we found that patients may be reluctant to discuss certain issues—such as withdrawal symptoms and the influence of psychosocial factors on painful crises and hospital admissions—which they feared would diminish the validity of their entitlement to treatment in their carers’ eyes. This mistrust of health professionals seemed to have adversely influenced the recruitment to research and clinical trials17; difficulties experienced in recruiting patients for the current study who were frequently admitted to hospital were further evidence of this effect.
An understanding of the history of “race relations” in the United Kingdom prompts the question: to what extent do the experiences of mistrust and stigmatisation of patients with sickle cell disease mirror the healthcare experiences of London’s black population more generally? There is little basis for comparison owing to the paucity of published research on this issue, although alienation has been identified as a major theme in existing work.18 In contrast, black British people’s experiences of other public services such as education and policing have inspired far more published analyses, and it is reasonable to suppose that the healthcare experiences of black people might show parallel themes of institutional racism. We argue that any degree of alienation characterising the experience of a black person seeking treatment for a racially neutral condition is compounded in the case of a patient with sickle cell disease owing to the status of the disorder in the United Kingdom as a “black disease.” This racialisation has arguably contributed to an inadequate policy response, underdevelopment of services, and undercoverage of the condition in medical and nursing curricula (unpulished data19). All of these factors are probably significant determinants of the problems highlighted by our research.
Sickle cell disorder as a chronic condition
Recent models of chronic disease and disablement emphasise the role of social and political environments in perpetuating dependency.20 Experiences of hospital care for pain from sickle cell disease may disempower patients, inhibit self management, and actively contribute to dependence on acute services, as our model illustrates. The implications become salient when this model is considered in the context of the underprovision of public services for sickle cell disorders: lack of primary and community care and the failure of policy makers in social services, education, and housing to acknowledge the special needs associated with this condition.21,22 Thus the path of least resistance leads to hospital dependency. Although our findings indicate that many of those affected have resisted this route, further work is needed to understand the factors contributing to such resistance; greater insight may also be achieved by comparison with other chronic conditions.
The status of sickle cell disease as a chronic disorder is inadequately recognised by policymakers and service providers. Management of chronic disease demands that health professionals and patients work in partnership,23 whereas our findings indicate that management of pain from sickle cell disease is based on the acute care model. Recent discussion24,25 about models of care for sickle cell disorders has frequently degenerated into arguments about the use of opioids for pain. Commentators have failed to acknowledge either the complexity of the relationship between patients with sickle cell disease and health professionals, or the attendant implications for experiences of pain and treatment seeking. Principles of palliative care26 and models of care for other chronic conditions23,27 could enhance this discussion: issues of communication, continuity of care and home care, intersectoral collaboration, and a holistic understanding of pain, are of particular relevance. Models of care for patients with sickle cell disorders should also be informed by the recognition of this population’s diversity. The historical focus on the minority of the population with sickle cell disease who frequently use acute services perpetuates both the stigmatisation of service users by health professionals and bias in service organisation and research.
Figure.
How hospital experiences may adversely influence individual pain management in patients with sickle cell disease
Acknowledgments
We thank the individuals who took part in the research and the health professionals and others who assisted with recruitment, in particular: Marjorie Ferguson, Connie Harewood, Nadine Hay, Naheed Mir, Chioma Nwonkonkor, Comfort Okolo, Norman Parker, John Porter, Tom Pearson, Emma Prescott, Shirley Samuel, Beverly Smalling, Jenneh Soya-Bonga, Adrian Stevens, Nikki Thomas, Sharon Waller, Neill Westerdale, and Ann Yardumian. The study was overseen by a multidisciplinary steering group (including service user and voluntary sector representatives) whose members have provided expert assistance throughout the project. We also thank Nicola Low, Chris McKevitt, Rosie Denmark, and Graham Serjeant for useful comments, and Ruth Dundas for assistance with statistical analysis.
Footnotes
Funding: The King’s Fund and Marks and Spencer.
Competing interests: None declared.
References
- 1.Brozovic M, Davies SC, Brownell AI. Acute admissions of patients with sickle cell disease who live in Britain. BMJ. 1987;294:1206–1208. doi: 10.1136/bmj.294.6581.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Westerman MP, Bailey K, Freels S, Schlegel R, Williamson P. Assessment of painful episode frequency in sickle cell disease. Am J Haematol. 1997;54:183–188. doi: 10.1002/(sici)1096-8652(199703)54:3<183::aid-ajh2>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro BS, Dinges DF, Orne EC, Ohene-Frempong K, Orne MT. Recording of crisis pain in sickle cell disease. In: Tyler D, Krane E, editors. Advances in pain research therapy. New York: Raven; 1990. pp. 313–321. [Google Scholar]
- 4.Streetly A, Dick M, Layton M. Sickle cell disease: the case for coordinated information. BMJ. 1993;306:1491–1492. doi: 10.1136/bmj.306.6891.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serjeant GR. Natural history and determinants of clinical severity of sickle cell disease. Curr Opin Hematol. 1995;2:103–108. doi: 10.1097/00062752-199502020-00001. [DOI] [PubMed] [Google Scholar]
- 6.Good MJD, Brodwin PE, Good BJ, Kleinman A. Pain as human experience: an introduction. In: Good MJD, Kleinman A, editors. Pain as human experience: an anthropological perspective. Berkeley: University of California Press; 1992. pp. 169–197. [Google Scholar]
- 7.Helman CG. Culture health and illness. 3rd ed. Oxford: Butterworth-Heinemann; 1994. Pain and culture; pp. 171–193. [Google Scholar]
- 8.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311:42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glaser B, Strauss A. The discovery of grounded theory. Chicago: Aldine; 1967. [Google Scholar]
- 10.Platt OS, Thorington BD, Brambilla DJ, Milner PF, Rosse WF, Vichinsky E, et al. Pain in sickle cell disease—rates and risk factors. N Engl J Med. 1991;25:11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- 11.Alleyne J, Thomas VJ. The management of sickle cell crisis pain as experienced by patients and their carers. J Adv Nurs. 1994;19:725–732. doi: 10.1111/j.1365-2648.1994.tb01144.x. [DOI] [PubMed] [Google Scholar]
- 12.Murray N, May A. Painful crises in sickle cell disease—patients’ perspectives. BMJ. 1988;297:452–454. doi: 10.1136/bmj.297.6646.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Black J, Laws S. Living with sickle cell disease. London: Sickle Cell Society; 1986. [Google Scholar]
- 14.Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symp Manage. 1997;14:168–174. doi: 10.1016/S0885-3924(97)00019-5. [DOI] [PubMed] [Google Scholar]
- 15.Waldrop RD, Mandry C. Health professional perceptions of opioid dependence among patients with pain. Am J Emerg Med. 1995;13:529–531. doi: 10.1016/0735-6757(95)90163-9. [DOI] [PubMed] [Google Scholar]
- 16.Ballas SK. Sickle cell pain. Seattle: International Association for the Study of Pain; 1998. [Google Scholar]
- 17.Olujohungbe A, Cinkotai KI, Yardumian A. Hydroxyurea therapy for sickle cell disease in Britain. BMJ. 1998;316:1689. doi: 10.1136/bmj.316.7146.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donovan J. We don’t buy sickness, it just comes: health, illness and health care in the lives of black people in London. Aldershot: Gower; 1986. [Google Scholar]
- 19.Department of Health. Report of a working party of the Standing Medical Advisory Committee on sickle cell, thalassaemia and other haemoglobinopathies. London: HMSO; 1993. [Google Scholar]
- 20.Gignac MAM, Cott CA. Conceptual model of independence and dependence for adults with chronic physical illness and disability. Soc Sci Med. 1998;47:739–775. doi: 10.1016/s0277-9536(98)00149-x. [DOI] [PubMed] [Google Scholar]
- 21.Streetly A, Maxwell K, Mejia A. Sickle cell disorders in London: a needs assessment of screening and care services. Fair shares for London report. London: United Medical and Dental Schools, Department of Public Health Medicine; 1997. [Google Scholar]
- 22.Atkin K, Ahmad W, Anionwu E. Service support to families caring for a child with a sickle cell disorder or thalassaemia: the experience of health professionals, service managers and health commissioners. Health. 1998;2:305–327. [Google Scholar]
- 23.Lorig K. Chronic disease self-management—a model for tertiary prevention. Am Behav Scientist. 1996;39:676–683. [Google Scholar]
- 24.Konotey-Ahulu FID. Opiates for sickle-cell crisis? [Letter.] Lancet. 1998;351:1438. doi: 10.1016/S0140-6736(05)79487-3. [DOI] [PubMed] [Google Scholar]
- 25.Layton DM, Mufti GJ, Bevan DH, Gloth FM. Opiates for sickle-cell crisis? [Letters.] Lancet. 1998;351:1964–1965. doi: 10.1016/s0140-6736(05)78656-6. [DOI] [PubMed] [Google Scholar]
- 26.O’Neill B, Fallon M. Principles of palliative care and pain control. BMJ. 1997;315:801–804. doi: 10.1136/bmj.315.7111.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Layzell S, McCarthy M. Community-based health services for people with HIV/AIDS: a review from a health service perspective. AIDS Care. 1992;4:203–215. doi: 10.1080/09540129208253091. [DOI] [PubMed] [Google Scholar]