Abstract
Background:
There is a need for simple imaging parameters capable of predicting therapeutic outcome.
Methods:
This retrospective study analysed 50 patients with locally advanced carcinoma of the cervix who underwent dynamic contrast-enhanced MRI before receiving potentially curative radiotherapy. The proportion of enhancing pixels (EF) in the whole-tumour volume post-contrast agent injection was calculated and assessed in relation to disease-free survival (DFS).
Results:
Tumours with high EF had a significantly poorer probability of DFS than those with low EF (P=0.011).
Interpretation:
EF is a simple imaging biomarker that should be studied further in a multi-centre setting.
Keywords: enhancing fraction, dynamic contrast-enhanced MRI, cervix cancer, radiotherapy, imaging biomarkers
Carcinoma of the cervix is the second most common cancer in women and a significant cause of mortality worldwide (Monk et al, 2009). Outcome of patients with locally advanced disease has improved in recent years with the adoption of concurrent chemoradiotherapy (Green et al, 2001). However, the overall 5-year survival rate is still only around 60% and the use of concurrent chemotherapy may increase the risk of late toxicity (Spensley et al, 2009). Consequently, there is a need to predict, before treatment, those patients likely to respond to radiotherapy alone and those who might benefit from combination therapy and/or the addition of novel targeted therapeutic agents.
There is interest in developing imaging biomarkers that predict cancer treatment outcome. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) can be used to estimate microvascular parameters such as tissue perfusion and capillary permeability. Some of the parameters have been shown to correlate with histological measurements of angiogenesis (Mayr et al, 1996; Hawighorst et al, 1999) and tumour oxygenation (Cooper et al, 2000) and have had some success in predicting treatment outcome (Loncaster et al, 2002). Although tracer kinetic analysis of DCE-MRI data results in the estimation of physiologically relevant parameters, the requirement for high-temporal resolution data – enabling an arterial input function (Parker et al, 2006) to be obtained – and pre-contrast T1 measurements make DCE-MRI studies difficult to implement. There is interest, therefore, in developing simple imaging biomarkers of tumour physiology.
Enhancing fraction (EF) assessed using DCE-MRI or CT has been presented as a simple method of assessing whole-tumour vascularity. Enhancing fraction is the proportion of tissue within a tumour that enhances and has been shown to predict treatment outcome in ovarian (O’Connor et al, 2007) and other solid tumours (Mullamitha et al, 2007) and has been used to assess treatment efficacy of an anti-angiogenic agent (Jayson et al, 2005). The aim of this study was to investigate whether EF measured with DCE-MRI was able to predict treatment outcome in patients with carcinoma of the cervix.
Materials and methods
Patients
Approval from a local ethics committee was obtained and all patients gave informed consent. Fifty patients with locally advanced carcinoma of the cervix underwent pre-treatment MRI scans. Patients subsequently received 40–45 Gy external beam radiotherapy (EBRT) to the pelvis – 20 fractions over 28 days – followed by low dose rate intracavitary brachytherapy (22.5−32.5 Gy). Disease-free survival (DFS) was calculated from the date of start of radiotherapy to date of disease recurrence or latest follow-up date where no recurrence occurred.
MR protocol
MRI scans were performed on a 1 T Siemens Magnetom Impact (Siemens Healthcare, Frimley, UK). Staging scans were carried out as previously described (Cooper et al, 2000; Loncaster et al, 2002). Dynamic scans used a sagittal 2D T1-weighted FLASH sequence (TR/TE=130/6.5 ms, FOV=290 × 290 × 5 mm, matrix=256 × 256, NSA=1, α=70°) with a temporal resolution of 25 s. One sequence of nine contiguous slices covering the whole-tumour volume was obtained before and seven after injection of 0.1 mmol kg−1 body weight Gd-DTPA.
Data analysis
Regions of interest (ROIs) encompassing the whole tumour were defined by an experienced radiologist on the pre-contrast T2-weighted images. Regions of interest were transferred to the dynamic data series. Data analysis was carried out using IDL (Research Systems Inc., Boulder, CO, USA). Tumour volumes were calculated by multiplying the number of pixels in the ROI by the voxel dimensions. A threshold for enhancing pixels was defined as a signal change greater than three times the standard deviation (s.d.) of signal values over the whole-tumour volume calculated in the pre-contrast image. The number of pixels that exceeded this threshold at 25 and 50 s post-contrast agent injection was calculated and divided by the total number of pixels in the tumour ROI to obtain EF at 25 and 50 s, respectively.
Pearson correlations between tumour volume and EF at 25 and 50 s were investigated using SPSS (SPSS Inc., Chicago, IL, USA). Spearman correlations between tumour stage and tumour volume, EF at 25 and 50 s were assessed. Tumours were stratified into two groups – those with tumour volume, stage and EF above or below the median. Kaplan–Meier curves were produced and a log-rank test performed to investigate significant differences in DFS. A significance level of 0.05 with a Bonferroni correction for multiple comparisons was used. A Fisher's exact test was used to assess differences in EF at 25 s in tumours of different size, stage, nodal status and age of the patient.
Results
Patient details are shown in Table 1. The median age of the 50 women was 63 years (range 29–82 years). The median tumour volume was 49.9 cm3 (range 6.8–184.2 cm3); 46 tumours were squamous cell carcinomas, 3 were adenosquamous cell carcinomas and 1 was adenocarcinoma; 26 and 24 patients had negative and positive nodal status, respectively. The median follow-up time in surviving patients was 105 months (range 86–128 months). A total of 32 patients had recurrence of their disease at the time of writing – 8 patients had local recurrence only, 9 patients had distant recurrence only, 13 had local and distant recurrence and 2 had residual disease after treatment.
Table 1. Summary of the distribution of patients as stratified by median EF at 25 s (28.4%).
| Parameter | n | Low EF at 25 s (n) | High EF at 25 s (n) | P-valuea |
|---|---|---|---|---|
| Stage | 0.047 | |||
| I | 1 | 1 | 0 | |
| II | 25 | 13 | 12 | |
| III | 23 | 10 | 13 | |
| IVA | 1 | 1 | 0 | |
| Tumour volume | <0.01b | |||
| Less than median | 25 | 17 | 8 | |
| Greater than median | 25 | 8 | 17 | |
| Age (years) | 0.157 | |||
| ⩽62 | 25 | 11 | 14 | |
| >62 | 25 | 14 | 11 | |
| Nodal status | 0.018 | |||
| Negative | 26 | 17 | 9 | |
| Positive | 24 | 8 | 16 |
Assessed by Fisher's exact test.
Significant at the 0.05 level with Bonferonni correction applied for multiple comparisons.
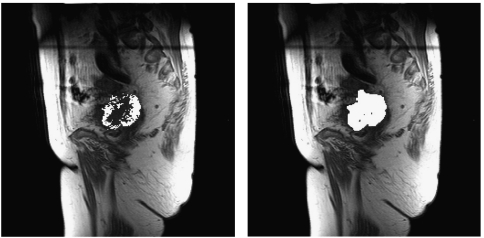
Figure 1 shows the distribution of enhancing pixels for EF calculated at 25 and 50 s, respectively, for one patient. Enhancing fraction at 25 s post-contrast was higher in larger tumours (P<0.01). The results of correlations are shown in Table 2. There was a weak positive correlation between tumour volume and EF at 25 s (r=0.37, P<0.01). There were no associations between EF at 50 s post-contrast and any clinicopathological parameter.
Figure 1.
EF in a cervix tumour (squamous cell carcinoma, stage IIIB) at 25 (36.5%) and 50 s (95.9%), respectively. The pre-treatment EF at 25 s was greater than the median and the patient subsequently developed local recurrence and metastases and died from their disease 17 months after diagnosis.
Table 2. Results of correlations between parameters.
| EF at 25 s | EF at 50 s | Tumour volume | Tumour stage | |
|---|---|---|---|---|
| EF at 25 s | — | 0.596a | 0.374a | −0.025 |
| EF at 50 s | 0.596a | — | 0.296 | −0.011 |
| Tumour volume | 0.374a | 0.296 | — | 0.148 |
| Tumour stage | −0.025 | −0.011 | 0.148 | — |
Pearson correlations are presented in all cases except for correlations between parameters with tumour stage that used a Spearman's test.
Significant at 0.05 level with Bonferroni correction applied for multiple comparisons.
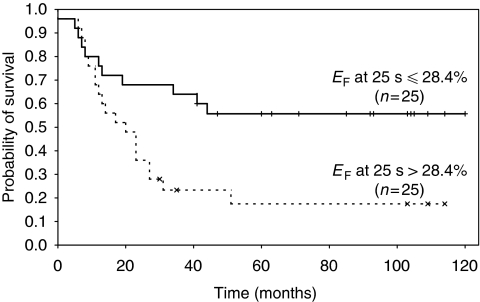
Figure 2 shows the Kaplan–Meier curves for patients stratified by median EF at 25 s (28.4%). There was a significant difference between DFS in patients with high and low tumour EF at 25 s (P=0.011). Enhancing fraction calculated at 50 s was not associated with DFS. In this cohort of patients neither baseline tumour volume (P=0.88) nor disease stage (P=0.09) had prognostic significance.
Figure 2.
Kaplan–Meier curves showing the relationship between disease-free survival (DFS) and EF measured at 25 s post-contrast agent injection using an enhancement threshold of three times the s.d. in the baseline signal measured over the whole-tumour volume. Patients were stratified by the median EF at 25 s that was 28.4%. Numbers of patients in each arm and statistical significance are indicated.
Discussion
A total of 50 patients with carcinoma of the cervix underwent DCE-MRI scans before receiving EBRT. We calculated EF at two time points to examine the prognostic significance of EF in this patient group. Patients with tumours with an EF at 25 s greater than the median had a significantly poorer DFS than those with low EF, concurring with a similar study in ovarian cancer (O’Connor et al, 2007). This finding is consistent with high EF reflecting more vascular and angiogenic tumours that are more likely to recur than those with low EF. The observation is consistent with work (Hawighorst et al, 1998) in which high kep – a rate constant describing the transfer of contrast agent between the vascular and the interstitial space – was indicative of a poor prognosis.
Other studies in cervical cancer have shown that high amplitude of enhancement is related to improved patient survival. Previous work involving a subset of this patient group (Loncaster et al, 2002) showed that high AH – a parameter dependent on the size of the interstitial space (Hoffman et al, 1995) – was associated with improved patient survival. Similarly, Mayr et al (1996) showed that high relative signal intensity (rSI) – the ratio of post- to pre-contrast signal – resulted in improved prognosis. These results suggest that EF measured early in the dynamic time series provides different physiological information from AH and rSI. We postulate that EF at 25 s is likely to relate to tissue perfusion whereas AH and rSI are associated with the size of the interstitial space. A low EF may also be consistent with a large hypoxic fraction; however, further work is needed to characterise the precise relationship, if any, between EF and hypoxic fraction. Recent work (Zahra et al, 2009) showed a weak correlation between kep and tumour regression measured at 5 weeks after radiotherapy, with high enhancement being associated with better tumour regression; however, the results of long-term follow-up were not presented.
This study involved the retrospective analysis of data collected between July 1997 and August 2000. Few dynamic data points were acquired and the 25-s temporal resolution precluded accurate tracer kinetic analysis. The MRI signal threshold above which pixels are said to have enhanced was calculated using the s.d. of the baseline signal in the whole-tumour ROI due to the lack of multiple baseline (pre-contrast) data points. Despite this limitation, we showed a significant relationship between EF and patient outcome. This finding agrees with other studies (Mullamitha et al, 2007; O’Connor et al, 2007) where the precise method of defining enhancement varied, showing that only a few dynamic data points and an accurate assessment of baseline tumour volume are required for calculation of EF. Although EF is simple to calculate when compared with tracer kinetic analysis, precise definitions of enhancement will vary with the MR protocol being used, magnet strength, contrast agent dose and rate of administration. These factors may affect the precision of the measurement but EF at 25 s should still reflect tissue perfusion, as hypothesised, and be capable of predicting DFS. Studies with more baseline signal data have used statistical techniques (O'Connor et al, 2009) to define enhancing pixels. Further work in larger prospective studies is therefore required to establish how best to define a threshold; however, our results add weight to the development of EF as an imaging biomarker applicable to routine clinical use.
The patients included in this study were treated up to 10 years ago, when radiotherapy alone was commonly prescribed as treatment of choice. Current best practice recommends concurrent chemoradiotherapy for patients with carcinoma of the cervix, so it is important to test whether EF has the same prognostic potential in this patient group. However, patients with locally advanced disease still receive radiotherapy alone if they have inadequate renal function for chemotherapy.
In conclusion, the results of this retrospective study suggest that EF measured using DCE-MRI is capable of predicting DFS in patients with carcinoma of the cervix. High EF was associated with poor prognosis. Enhancing fraction is a simple imaging biomarker and does not rely on sophisticated MRI techniques or data analysis. Confirmation in further datasets should be carried out to validate EF as a biomarker of prognosis in locally advanced carcinoma of the cervix.
Acknowledgments
We thank the MR radiographers at the Christie for scanning the patients in this study, Mrs Rita Hannon and Mr Ric Swindell for help with patient follow-up and statistics. This work was supported by a Christie Endowment grant. Professor Catharine West was supported by Experimental Cancer Medicine Centre and Cancer Research UK funding.
References
- Cooper RA, Carrington BM, Loncaster JA, Todd SM, Davidson SE, Logue JP, Luthra AD, Jones AP, Stratford I, Hunter RD, West CML (2000) Tumour oxygenation levels correlate with dynamic contrast-enhanced magnetic resonance imaging parameters in carcinoma of the cervix. Radiothe Oncol 57: 53–59 [DOI] [PubMed] [Google Scholar]
- Green JA, Kirwan JM, Tierney JF, Symonds P, Fresco L, Collingwood M, Williams CJ (2001) Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet 358: 781–786 [DOI] [PubMed] [Google Scholar]
- Hawighorst H, Knapstein PG, Knopp MV, Vaupel P, van Kaick G (1999) Cervical carcinoma: standard and pharmacokinetic analysis of time-intensity curves for assessment of tumor angiogenesis and patient survival. Magn Reson Mater Phys Biol Med 8: 55–62 [DOI] [PubMed] [Google Scholar]
- Hawighorst H, Weikel W, Knapstein PG, Knopp MV, Zuna I, Schoenberg SO, Vaupel P, van Kaick G (1998) Angiogenic activity of cervical carcinoma: assessment by functional magnetic resonance imaging-based parameters and a histomorphological approach in correlation with disease outcome. Clin Cancer Res 4: 2305–2312 [PubMed] [Google Scholar]
- Hoffman U, Brix G, Knopp MV, Hess T, Lorenz WJ (1995) Pharmacokinetic mapping of the breast: a new method for dynamic MR mammography. Magn Reson Med 33: 506–514 [DOI] [PubMed] [Google Scholar]
- Jayson GC, Parker GJM, Mullamitha S, Valle JW, Saunders M, Broughton L, Lawrence J, Carrington B, Roberts C, Issa B, Buckley DL, Cheung S, Davies K, Watson Y, Zinkewich-Peotti K, Rolfe L, Jackson A (2005) Blockade of platelet-derived growth factor receptor-beta by CDP860, a humanized, PEGylated di-Fab’, leads to fluid accumulation and is associated with increased tumor vascularised volume. J Clin Oncol 23: 973–981 [DOI] [PubMed] [Google Scholar]
- Loncaster JA, Carrington BM, Sykes JR, Jones AP, Todd SM, Cooper RA, Buckley DL, Davidson SE, Logue JP, Hunter RD, West CML (2002) Prediction of radiotherapy outcome using dynamic contrast enhanced MRI of carcinoma of the cervix. Int J Radiat Oncol Biol Phys 54: 759–767 [DOI] [PubMed] [Google Scholar]
- Mayr NA, Yuh WTC, Magnotta VA, Ehrhardt JC, Wheeler JA, Sorosky JI, Davis CS, Wen BC, Martin DD, Pelsang RE, Buller RE, Oberley LW, Mellenberg DE, Hussey DH (1996) Tumor perfusion studies using fast magnetic resonance imaging technique in advanced cervical cancer: a new noninvasive predictive assay. Int J Radiat Oncol Biol Phys 36: 623–633 [DOI] [PubMed] [Google Scholar]
- Monk BJ, Sill MW, Burger RA, Gray HJ, Buekers TE, Roman LD (2009) Phase II trial of bevacizumab in the treatment of persistent or recurrent squamous cell carcinoma of the cervix: a gynecologic oncology group study. J Clin Oncol 27: 1069–1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullamitha SA, Ton NC, Parker GJ, Jackson A, Julyan PJ, Roberts C, Buonaccorsi GA, Watson Y, Davies K, Cheung S, Hope L, Valle JW, Radford JA, Lawrance J, Saunders MP, Munteanu MC, Nakada MT, Nemeth JA, Davis HM, Jiao Q, Prabhakar U, Lang Z, Corringham RE, Beckman RA, Jayson GC (2007) Phase I evaluation of a fully human anti-alphav integrin monoclonal antibody (CNTO 95) in patients with advanced solid tumors. Clin Cancer Res 13: 2128–2135 [DOI] [PubMed] [Google Scholar]
- O’Connor JP, Jayson GC, Jackson A, Ghiorghiu D, Carrington BM, Rose CJ, Mills SJ, Swindell R, Roberts C, Mitchell CL, Parker GJ (2007) Enhancing fraction predicts clinical outcome following first-line chemotherapy in patients with epithelial ovarian carcinoma. Clin Cancer Res 13: 6130–6135 [DOI] [PubMed] [Google Scholar]
- O'Connor JPB, Carano RAD, Clamp AR, Ross J, Ho CCK, Jackson A, Parker GJM, Rose CJ, Peale FV, Friesenhahn M, Mitchell CL, Watson Y, Roberts C, Hope L, Cheung S, Reslan HB, Go MAT, Pacheco GJ, Wu X, Cao TC, Ross S, Buonaccorsi GA, Davies K, Hasan J, Thornton P, del Puerto O, Ferrara N, van Bruggen N, Jayson GC (2009) Quantifying antivascular effects of monoclonal antibodeies to vascular endothelial growth factor: insights from imaging. Clin Cancer Res 15: 6674–6682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker GJ, Roberts C, Macdonald A, Buonaccorsi GA, Cheung S, Buckley DL, Jackson A, Watson Y, Davies K, Jayson GC (2006) Experimentally-derived functional form for a population-averaged high-temporal-resolution arterial input function for dynamic contrast-enhanced MRI. Magn Reson Med 56: 993–1000 [DOI] [PubMed] [Google Scholar]
- Spensley S, Hunter RD, Livsey JE, Swindell R, Davidson SE (2009) Clinical outcome for chemoradiotherapy in carcinoma of the cervix. Clin Oncol (R Coll Radiol) 21: 49–55 [DOI] [PubMed] [Google Scholar]
- Zahra MA, Tan LT, Priest AN, Graves MJ, Arends M, Crawford RA, Brenton JD, Lomas DJ, Sala E (2009) Semiquantitative and quantitative dynamic contrast-enhanced magnetic resonance imaging measurements predict radiation response in cervix cancer. Int J Radiat Oncol Biol Phys 74: 766–773 [DOI] [PubMed] [Google Scholar]