Abstract
Objective
This study examined whether three-month outcomes of a brief image-based multiple behavior intervention on health habits and health-related quality of life of college students were sustained at 12-month follow-up without further intervention.
Methods
A randomized control trial was conducted with 303 undergraduates attending a public university in southeastern US. Participants were randomized to receive either a brief intervention or usual care control, with baseline, three-month, and 12-month data collected during fall of 2007.
Results
A significant omnibus MANOVA interaction effect was found for health-related quality of life, p=.01, with univariate interaction effects showing fewer days of poor spiritual health, social health, and restricted recent activity, p’s <.05, for those receiving the brief intervention. Significant group by time interaction effects were found for driving after drinking, p=.04, and moderate exercise, p=.04, in favor of the brief intervention. Effect sizes typically increased over time and were small except for moderate size effects for social health-related quality of life.
Conclusion
This study found that three-month outcomes from a brief image-based multiple behavior intervention for college students were partially sustained at 12-month follow-up.
Keywords: brief intervention, image, multiple behaviors, college students, long-term effects
Introduction
National longitudinal data indicate that the majority of health behaviors and health-related indicators worsen as adolescents’ age into young adulthood (Harris, Gordon-Larsen, Chantala, & Udry, 2006). Other national epidemiologic data indicate that the majority of adolescents (Eaton, et al., 2006) and adults (Fine, et al., 2004) are at risk for multiple, simultaneous health damaging behaviors associated with premature morbidity and mortality. In addition, studies show that various adolescent health behaviors are interrelated (Driskell, et al., 2008), and that potentially modifiable determinants may link multiple health risk and health promoting behaviors (Peters, et al., 2009). Together, these data support the need for, and potential utility of, targeting multiple health habits when developing and implementing behavioral interventions.
Typical prevention and intervention programs targeting individuals focus on single health behavior change, however, effective multiple behavior interventions may have a greater impact on public health (Nigg, Allegrante & Ory, 2002). There is increasing interest in developing and evaluating integrative interventions targeting multiple risk behaviors (Atkins & Clancy, 2004; Orleans, 2004; Prochaska, Spring, & Nigg, 2008). In addition, there are a growing number of studies showing that asset-based programs aimed at promoting healthy development involving positive identity and behaviors can improve multiple health habits among youth (Flay, 2003; Roth & Brooks-Gunn, 2003; Tebes, et al, 2007).
There are a lack of theoretical models for researchers and practitioners that directly address how to construct interventions targeting multiple health behaviors (Noar, Chabot, & Zimmerman, 2008; Orleans, 2004). One emerging framework for planning multiple behavior interventions is the Behavior-Image Model (BIM). BIM is based on two principles. First, that activating existing or creating new images of attractive others (i.e., social images or prototypes) and improved possible selves (i.e., future self-images) can integrate and motivate change across divergent health behaviors (Werch, 2007). Second, that BIM-based interventions should involve self-regulatory processes by providing feedback on participants’ health behaviors and self-images to increase commitment to goal setting aimed at reducing discrepancy between health behaviors and social/self-images. Several studies have demonstrated that brief interventions using positive social and self-images and health promoting behaviors, in addition to risk behaviors, may simultaneously improve multiple health behaviors among adolescents (Werch et al., 2003; 2005; 2008). Unfortunately, most brief interventions targeting college students have been singularly focused on problem alcohol consumption.
An initial study evaluating three BIM-influenced brief interventions for college students showed the interventions significantly improved a number of health promoting and health risk behaviors and health-related quality of life one-month post-intervention (Werch, et al., 2007). A second study of a BIM-influenced brief image-based intervention for college students found that undergraduates receiving the intervention showed improvements on frequency and heavy use of alcohol; driving after drinking; length, quantity and heavy use of marijuana; 30-day moderate exercise; sleep; and spiritual and social health-related quality of life three-months post-intervention, compared to students receiving usual care (Werch, et al., 2008). The current study examined whether initial three-month outcomes from the brief image-based multiple behavior intervention for undergraduates were sustained at 12-month follow-up without further intervention.
Methods
Participants
Students attending a mid-sized public university in southeastern US were recruited during fall of 2006 to participate in a randomized control trial of a brief health promotion program titled Project Fitness. Of 303 undergraduates recruited, 299 participants provided usable baseline data (99%), and of these 283 provided three-month data (95%), while 231 provided 12-month data (77%). The majority of participating students were female (59.5%). Average age of participants at baseline was 19.2 years old (SD=1.12). The majority were Caucasian (71.6%), followed by African American (12.7%). Nearly nine percent (8.7%) reported being Hispanic. Most participants lived in a co-ed residence hall (44.8%) or off-campus housing (38.5%), with the remaining proportion living in fraternity/sorority, single sex residence hall, co-op housing or other university housing (16.7 %).
Design and Procedures
Students attending the participating university aged 18-21 years were eligible to participate. Recruitment involved targeting students who visited the campus medical services center using posters and flyers, as well as through announcements made on the university’s student email, and by distributing flyers in selected undergraduate health courses and common areas throughout campus. Students were paid $20 for participating in each of three data collections.
After providing written consent, students completed a brief health behavior screen, and then the baseline survey via a secure online computer program in a quiet office on campus. Immediately after the collection of baseline data, participants were randomly assigned to receive either a brief tailored consultation and fitness goal plan, or usual care print materials, from a trained fitness specialist (i.e., bachelor’s level research staff). Participants were contacted and scheduled for a three-month data collection in the spring and a 12-month data collection during the following fall, 2007. The university’s institutional review board approved the research protocol prior to implementing the study.
Intervention
Brief Image Intervention
Participants assigned to receive the brief intervention were given a one-on-one consultation using a consultation protocol with scripted messages which lasted about 25 minutes. The consultation was based on BIM (Werch, 2007). Specifically, gain framed messages were used to illustrate how health promoting behaviors support positive social and self-images. In addition, loss framed messages were used to show how health risk behaviors interfere with positive image outcomes and achievement of health promoting habits. The consultation provided content tailored to current health behaviors and their relation to salient image achievement. Brief multiple behavior image types and examples are shown in Table 1. At the conclusion of the consult, participants received a one-page goal plan. The goal plan was also based on BIM. Research shows that the selection of image-based self-concordant goals facilitates behavioral change (Koestner, et al., 2002; Martin & Leary, 2001). Students were asked to select at least one goal from each of four behavior groups to improve in the next week, including: 1) increase physical activity and exercise, 2) decrease alcohol use, 3) decrease cigarette use, and 4) increase other fitness behaviors (i.e., nutrition, stress management, and sleep).
Table 1.
Brief multiple behavior intervention message types and examples
| Message Type | Example |
|---|---|
|
Tailored Feedback: Provides tailored information based on current health behaviors identified in the brief health behavior screen. |
I see that you engage in at least 30 minutes of moderate physical activity on most days of the week. Congratulations, you are physically active! |
|
Health Promotion Behavior Gain Framed (i.e., benefits): Illustrates that engaging in a health promoting behavior results in positive social and self-images. |
Young adults who engage in regular physical activity tend to feel energetic, sleep better, and look more attractive, slim and physically fit. Regular physical activity can reduce your stress level making you more relaxed, happy and unworried. |
|
Health Risk Behavior Loss Framed (i.e., costs): Shows that engaging in health risk behaviors interferes with favorable self-images and behaviors, and results in non-favorable images. |
Meanwhile, using too much alcohol and smoking cigarettes interferes with creating a physically active lifestyle. Alcohol misuse can get in the way of your fitness goals by decreasing your energy level, and directly harming your fitness level and compromising your goals of being in-shape, looking good and feeling strong. |
|
Tailored Behavior Coupling: Illustrates that simultaneously engaging in one or more health promoting behaviors while avoiding risk behaviors results in positive self-images. |
Regularly engaging in moderate physical activity, while avoiding too much alcohol and cigarettes, will help you continue to be a physically active young adult, and reach your fitness goals of keeping slim and trim. |
Usual Care Control
The usual care control consisted of a commercially available brochure titled “Fitness” (Krames, 2001). Participants assigned to this condition were asked to take their time and read the brochure in the same quiet, private office on campus where the brief interventions were conducted.
Measures
The revised Fitness & Health Survey (Werch, 2006) was used to collect data on targeted health behaviors and risk factors associated with BIM. Measures of interest for this study were those found to differ significantly between treatment and control groups at three-month post-intervention. All single item measures from significant multivariate analyses were also included in the current analysis. Measures selected for inclusion in this study were alcohol and marijuana consumption, driving after drinking, moderate exercise, sleep quantity, and health-related quality of life.
Substance use behaviors were measured with items adopted from standardized national youth substance use surveys and research (Botvin, Baker, & Renick, 1984; Eggert, et al., 1994; Ellickson & Hays, 1991; Johnson, et al., 1990). These items included measures of length of use, 30-day frequency, 30-day quantity, and 30-day heavy use for alcohol (Alpha=.85) and marijuana (Alpha=.93). Heavy use of alcohol was defined as 5 or more drinks in a row if a male and 4 or more drinks in a row if female, whereas heavy use of marijuana was “getting really high or stoned from marijuana.” Items measuring alcohol and marijuana frequency and heavy use in the past 30-days ranged from: 1 = 0 days, 2 = 1-2 days, to 7 = All 30 days. Quantity of alcohol use was assessed as how many alcoholic beverages usually drank per day in the past 30-days, and ranged from: 1 = I did not drink, 2 = 1 drink per day, to 12 = 11 or more drinks per day. Quantity of marijuana use was measured as how many times did you use any form of marijuana in the past 30-days, and ranged from: 1 = 0 times, 2 = 1-2 times, to 8 = 40 or more times.
Driving after drinking alcohol during the past 30-days was measured from an item adopted from prior epidemiologic studies, and ranged from: 1 = 0 times, 2 = 1 time, to 6 = 5 or more times (Gruenwald, Johnson, & Treno, 2002). Moderate exercise during the past 30-days was measured as how many days did you participate in physical activity for at least 30 minutes that did not make you sweat or breathe hard. This item was adopted from national epidemiologic surveys of physical activity among youth, and ranged from: 1 = 0 days, 2 = 1-2 days, to 7 = All 30 days (CDC, 2005). Sleep was measured by assessing the number of hours usually slept each night during the past 30-days, and ranged from: 1= 5 or fewer hours, 2 = 6 hours, to 5=9 or more hours (Groeger, Zijlstra, & Dijk, 2004; Wolfson, et al., 2003). Lastly, health-related quality of life was measured using five items which assessed the number of days during the past 30-days that physical health, mental health, spiritual health, and social health was not good, and the number of days that poor health of any kind kept one from doing their usual activities (Alpha=.73). The five items were adopted from research on health-related quality of life among adolescents, and ranged from: 1 = 0 days, 2 = 1-2 days, to 7 = All 30 days (Zullig, et al., 2004).
Statistical Analyses
All analyses were performed using SPSS version 17.0 (SPSS, Inc., 2008). Estimated marginal means and standard errors were displayed for all three data points for illustrative purposes, with three-month findings previously reported elsewhere (Werch, et al., 2008). Statistical analysis evaluated baseline and 12-month data to test whether positive outcomes at three-months were maintained at the 12-month follow-up. While tests of normality found some of the data to be skewed, we chose to use more powerful parametric tests instead of nonparametric analysis procedures. Specifically, MANOVA tests were employed as they are known to be robust in regard to violations of normality and homogeneity, particularly when larger sample sizes are examined like the one in this study (Bray & Maxwell, 1991; Meyers & Guarino, 2006).
Repeated measures MANOVAs were used to more efficiently address multiple-related health outcomes targeted by the intervention. This approach creates a new dependent variable maximizing group differences, while controlling for Type I error resulting from performing individual tests on multiple dependent variables. Repeated measures ANOVAs were used to examine temporal effects on single item health measures. Effect sizes of outcomes at both three- and 12-months were calculated using Cohen’s d statistic (Cohen, 1988). Procedures recommended for controlled pre- and posttest research designs were used (Morris, 2008), with effect sizes determined by obtaining within group post-intervention minus baseline difference scores and then subtracting experimental group scores.
A propensity scores approach was used to impute missing data at 12-months post-intervention. A model was developed for estimating missing values from multiple data sets using baseline scores and covariates to obtain the variability of imputed missing values. Specifically, we created five data sets and generated five separate logistic regressions from each imputed data set. A propensity score approach is used to estimate the probability of being in one group (missingness) versus another (no missingness) as a function of participants’ baseline scores, treatment assignment, and gender (Rosenbaum and Rubin, 1983). We imputed five complete data sets providing five imputed values for each participant. We then randomly selected one of the five imputed values for each participant to include in the final data set. This approach was motivated by Collins and colleagues (Collins, Schafer and Kam, 2001), and has the advantage of preserving the sample original variability while filling in the missing values. Outcome analyses were run with and without imputed values. Due to their similarity, only the more complete imputed data are presented here.
Results
Attrition Analysis
Twenty-three percent of participants (n=68) were lost to attrition at 12-month follow-up. No differences were found in the proportion of those who dropped out between experimental groups. Dropouts were more likely to have someone in their immediate family with an alcohol or drug problem (57.3%) than non-dropouts (40.2%), p=.01. No other baseline demographic or health behavior differences were found between dropouts and non-dropouts. Factorial ANOVA tests showed no dropout status by experimental group interaction effects on any of the demographic or health behaviors studied.
Outcome Analysis
Table 2 shows estimated marginal means and standard errors of health outcomes by experimental group and time. For substance use measures, neither of the omnibus MANOVA interaction effects were significant. In addition, none of the univariate interaction effects were significant for alcohol and marijuana consumption behaviors. Effect sizes at three- and 12-month follow-ups for alcohol use indicated that over time there were sustained small reductions on alcohol use frequency, and decreasing effects for heavy alcohol use for the brief intervention group.
Table 2.
Means (M) and standard errors of health outcomes among students in a southeastern university for experimental group by time, fall 2007 (n = 283)
| Intervention (n = 140) |
Control (n = 143) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
3MPosttest |
12MPosttest |
Baseline |
3MPosttest |
12MPosttest |
||||||||||
| Health Outcomes | M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | d1 | d2 | p |
| Alcohol | |||||||||||||||
| Length | 3.51 | .15 | 3.61 | .14 | 3.88 | .14 | 3.84 | .15 | 3.92 | .14 | 4.08 | .14 | -.01 | -.07 | .43 |
| Frequency | 2.56 | .12 | 2.36 | .12 | 2.60 | .12 | 2.57 | .12 | 2.72 | .12 | 2.90 | .12 | .24 | .20 | .08 |
| Quantity | 3.76 | .24 | 3.57 | .22 | 3.41 | .22 | 3.93 | .24 | 3.85 | .22 | 4.02 | .21 | .04 | .16 | .15 |
| Heavy use | 1.91 | .11 | 1.72 | .10 | 1.98 | .12 | 1.86 | .11 | 2.01 | .10 | 2.04 | .11 | .27 | .08 | .46 |
| Marijuana | |||||||||||||||
| Length | 1.90 | .14 | 1.70 | .13 | 1.89 | .14 | 1.95 | .13 | 2.06 | .13 | 2.04 | .14 | .19 | .06 | .52 |
| Frequency | 1.59 | .12 | 1.50 | .12 | 1.81 | .13 | 1.61 | .12 | 1.67 | .11 | 1.64 | .13 | .10 | -.13 | .20 |
| Quantity | 1.54 | .12 | 1.41 | .12 | 1.89 | .13 | 1.55 | .11 | 1.73 | .12 | 1.62 | .13 | .23 | -.20 | .12 |
| Heavy use | 1.46 | .10 | 1.33 | .10 | 1.59 | .11 | 1.48 | .10 | 1.58 | .10 | 1.49 | .11 | .19 | -.10 | .40 |
| Health Quality of Life | |||||||||||||||
| Physical health | 2.90 | .12 | 2.56 | .11 | 2.57 | .11 | 2.40 | .12 | 2.21 | .11 | 2.46 | .10 | .10 | .27 | .06 |
| Mental health | 3.11 | .13 | 2.71 | .11 | 3.09 | .12 | 2.90 | .13 | 2.63 | .10 | 3.00 | .12 | .09 | .08 | .51 |
| Spiritual health | 2.40 | .14 | 1.91 | .13 | 2.20 | .15 | 2.09 | .14 | 2.15 | .13 | 2.37 | .15 | .32 | .28 | .04 |
| Social health | 2.34 | .11 | 1.96 | .10 | 2.19 | .12 | 1.90 | .11 | 2.01 | .09 | 2.44 | .12 | .38 | .54 | .00 |
| Recent activity | 2.26 | .10 | 2.04 | .09 | 2.00 | .10 | 2.01 | .10 | 1.91 | .09 | 2.12 | .10 | .10 | .31 | .03 |
| Sleep | 2.71 | .09 | 3.17 | .08 | 2.96 | .08 | 2.80 | .09 | 2.92 | .08 | 3.01 | .08 | .32 | .04 | .85 |
| Driving after Drinking | .62 | .11 | .49 | .11 | .60 | .11 | .57 | .10 | .71 | .10 | .86 | .11 | .22 | .25 | .04 |
| Moderate Exercise | 4.32 | .15 | 4.52 | .15 | 4.44 | .15 | 4.72 | .15 | 4.46 | .14 | 4.32 | .15 | .25 | .29 | .04 |
Note: P values = Univariate treatment by 12-month interactions. d1 = Effect size for baseline to 3-month follow-up. d2 = Effect size for baseline tod 12-month follow-up.
Significant group by time interaction effects were found for driving after drinking, p=.04, with small effects at both three- and 12-month follow-ups for the brief intervention. A significant interaction was also found for moderate exercise in the past 30-days, p=.04, with small effects at both three- and 12-month follow-ups for the brief intervention. No differences were found for sleep behavior at 12-month follow-up.
A significant omnibus MANOVA interaction effect was found for health-related quality of life, p=.01, with significant univariate interaction effects showing fewer days of poor spiritual health, p=04, social health, p=.001, restricted recent activity, p=.03, and approaching significance on fewer days of poor physical health, p=.06 for those receiving the brief intervention. Effect sizes increased between three- and 12-month follow-ups for social health and restricted recent activity, and were small at 12-months except for moderate size effects for social health-related quality of life.
Figure 1 shows a graphical display of mean scores of significant health outcomes by experimental group and time. For participants receiving the brief intervention, most effects showed a curvilinear trend with improvements at 3-months weakening at 12-months, but remaining slightly improved over baseline scores, whereas most effects for participants receiving the control showed a linear pattern of worsening scores at both three- and 12-month follow-ups. The one exception was the number of days of poor health, which showed a linear trend of improvement at both three- and 12-month follow-ups for those receiving the brief intervention, and a curvilinear pattern for those in the control group.
Figure 1. Mean scores of significant health outcomes by treatment group and time.
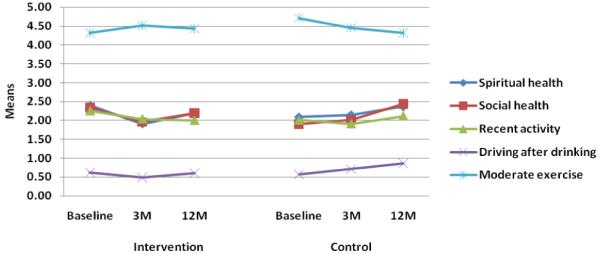
Note. Lower scores reflect improvement on all measures except moderate exercise.
Discussion
Few studies have examined the long-term effects of brief multiple behavior interventions. Such studies are critical to understanding the degree to which short-term brief intervention outcomes are sustained, and whether or not re-interventions may be needed to bolster specific behavioral degradations over time. Results from this study showed that a brief image-based multiple behavior intervention had sustained effects on some health outcomes, but not others. Evidence in favor of longer-term outcomes of the brief intervention was strongest for health-related quality of life, moderate exercise, and driving after drinking. Findings indicated effect sizes for these outcomes typically increased over time but remained small, with the exception of social health-related quality of life which reached a moderate effect size at 12-month follow-up.
Of particular note were the effects for various components of health-related quality of life, which were found to strengthen over time. These findings suggest that brief interventions can change not only various health habits, but important indicators of health. A post hoc analysis of associations among target health behaviors and health-related quality of life areas found that all correlations were low (r’s<.19), supporting the independence of health habits and health-related quality of life outcomes reported in this study. Previous research evaluating brief image-based multiple behavior interventions has supported their effects on increasing health-related quality of life of college students over time (Werch, et al., 2007). In the current study, these health indicators included quality of life associated with spiritual health, social health, and even one’s ability to conduct usual daily activities. Promoting the quality of healthy life is a major health goal in the US (USDHHS, 2000). Improving health-related quality of life is also a critical objective of health care (Kaplan, 2003), with evidence suggesting that it can be used as a measure to monitor the progression of health and improve provider-patient communication (Deyo & Carter, 1992). In addition, health-related quality of life is regularly assessed in health promotion and disease prevention interventions as a primary or secondary end point (Berra, 2003; Ravesloot, Seekins, & White, 2005).
However, initial effects from the brief intervention on other health behaviors, including alcohol and marijuana use and sleep, decayed at 12-month follow-up. Only one measure of alcohol use, alcohol frequency, showed a sustained small but non-significant effect over time. Interestingly, many of these degradations were due, in part to improvements among control students between the two follow-ups. Specifically, control participants showed increases in hours of sleep and decreases on all four measures of marijuana use between three- and 12-month data collections. While we are unaware of any unplanned activities or events which control students may have been exposed to, we can not rule out the possibility that some of the usual care control participants received additional health promotion or prevention communications between follow-up data collections.
Nevertheless, increases in alcohol and marijuana use among students receiving the brief intervention suggest the need to employ booster communications or re-interventions specifically designed to sustain alcohol and drug use outcomes. A previous study examining three- and 12-month effects of an image-based brief intervention for adolescents found similar weakening of alcohol and marijuana behavior outcomes over time (Werch, et al, 2005). There is a dearth of research evaluating different types of brief re-interventions targeting multiple health behaviors, which are designed to sustain and perhaps strengthen positive effects over time. In addition, further investigations are needed to determine if it is more efficacious or cost-effective to provide a booster intervention before or after positive outcomes begin to decline.
Study Limitations and Strengths
This study was limited to a sample of college students from a single university in the southeastern US. Additional research is needed to evaluate brief image-based interventions using students from diverse college and university settings, as well as for young adults not attending college. In addition, more participants who were lost to follow-up reported family alcohol or drug problems than those remaining in the study, thereby limiting the generalizability of the findings to certain student populations. By itself, this study should be viewed as an initial step toward examining the longitudinal effects of brief image-based multiple behavior interventions on health habits and health-related quality of life of college students. This investigation was also limited to three-month and 12-month post-intervention follow-ups. Studies are needed which include more frequent follow-up over longer periods of time to better understand the sustainability of multiple behavior and health indicator outcomes resulting from brief image-based interventions. Lastly, this study was limited to self-reported measures of health behavior and health-related quality of life. Nonetheless, all of measures in this study have been used in previous published research, and results from an item response analysis suggested little self-report bias due to social desirability or errors resulting from sloppy completion or deliberate falsification of reports.
This study also had a number of noteworthy strengths. One strength was the rigorous randomized control design with two post-intervention follow-up data collections. This study design allowed a rare look into the longer-term sustainability of early initial effects from a brief intervention (i.e., 12-months after intervention). Another strength was the examination of an innovative theory-based, brief intervention that targeted positive social and self-images to simultaneously address both health risk and health promoting behaviors using a brief format. Thus, this novel intervention linked health promotion and prevention goals within a single intervention, and addressed the epidemiologic reality of multiple and co-occurring risk behaviors common among adolescents and adults in the US. Multiple behavior interventions for individuals are rare, but hold greater likelihood to cost-effectively impact public health than those targeting single behaviors, particularly if they are brief in design. A final strength was the inclusion of effect sizes, in addition to significance testing. The addition of effect sizes at both three- and 12-month follow-ups provided key information, determining the degree to which initial positive outcomes were sustained over time.
Conclusions
In conclusion, this study found that initial three-month outcomes from a brief image-based multiple behavior intervention among college students were partially sustained at 12-month follow-up. In particular, health-related quality of life effects were maintained, as were moderate exercise and driving after drinking. However, effects on alcohol and marijuana use, along with the amount of sleep were not sustained over time. It is these later findings that indicate the need for research to assess re-interventions for prolonging selected behavioral outcomes resulting from brief multiple behavior interventions.
Acknowledgements
This manuscript would not have been possible without the financial support from the National Institute on Drug Abuse (Grant #DA018872 and #DA019172), and the National Institute on Alcohol Abuse and Alcoholism (Grant #AA9283). We also wish to also thank those college students who generously agreed to participate in this research and contribute their valuable time making this study possible.
Contributor Information
Chudley E. (Chad) Werch, Addictive & Health Behaviors Research Institute, Department of Health Education & Behavior, University of Florida, Jacksonville, Florida.
Michele J. Moore, Department of Public Health, University of North Florida, Jacksonville, Florida.
Hui Bian, Addictive & Health Behaviors Research Institute, Department of Health Education & Behavior, University of Florida, Jacksonville, Florida.
Carlo C. DiClemente, Department of Psychology, University of Maryland Baltimore County, Baltimore, Maryland.
I-Chan Huang, Department of Epidemiology and Health Policy Research, College of Medicine, University of Florida, Gainesville, Florida.
Steven C. Ames, Division of Hematology and Oncology, Mayo Clinic, Jacksonville, Florida.
Dennis Thombs, Department of Behavior Science and Community Health, College of Public Health and Health Professions, University of Florida, Gainesville, Florida.
Robert M. Weiler, Department of Health Education & Behavior, College of Health and Human Performance, University of Florida, Gainesville, Florida.
Steven B. Pokorny, Department of Health Education & Behavior, College of Health and Human Performance, University of Florida, Gainesville, Florida.
References
- Atkins D, Clancy C. Multiple Risk Factors Interventions: Are we up to the challenge? Am J Prev Med. 2004;27(2S):102–103. doi: 10.1016/j.amepre.2004.04.016. [DOI] [PubMed] [Google Scholar]
- Berra K. The effect of lifestyle interventions on quality of life and patient satisfaction with health and health care. J Cardiovasc Nurs. 2003;18(4):319–325. doi: 10.1097/00005082-200309000-00010. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Renick N, Filazzola AD, Botivn EM. A cognitive-behavioral approach to substance abuse prevention. Addict Behav. 1984;9:137–147. doi: 10.1016/0306-4603(84)90051-0. [DOI] [PubMed] [Google Scholar]
- Bray JH, Maxwell SE. Multivariate analysis of variance. Sage Publications; Newbury Park, CA: 1991. [Google Scholar]
- Centers for Disease Control and Prevention State and Local Youth Risk Behavior. 2008 June 2; 2005. Available: http://www.cdc.gov/HealthyYouth/YRBS/pdfs/2005highschoolquestionaire.pdf.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Earlbaum Associates; Hillsdale, NJ: 1998. [Google Scholar]
- Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6:330–351. [PubMed] [Google Scholar]
- Deyo RA, Carter WB. Strategies for improving and expanding the application of health status measures in clinical settings: A researcher-developer viewpoint. Med Care. 1992;30(S5):176–186. doi: 10.1097/00005650-199205001-00015. [DOI] [PubMed] [Google Scholar]
- Driskell MM, Dyment S, Mauriello L, Castle P, Sherman K. Relationships among multiple behaviors for childhood and adolescent obesity prevention. Prev Med. 2008;46:209–215. doi: 10.1016/j.ypmed.2007.07.028. [DOI] [PubMed] [Google Scholar]
- Eaton D, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Shanklin S, Lim C, Grunbaum J, Wechsler H. Youth Risk Behavior Surveillance - United States, 2005. J Sch Health. 2006;76:353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- Eggert L, Thompson E, Herting J, Nicholas L, Dicker B. Preventing adolescent drug abuse and high school dropout through an intensive school-based social network development program. Am J Health Promot. 1994;8(3):202–215. doi: 10.4278/0890-1171-8.3.202. [DOI] [PubMed] [Google Scholar]
- Ellickson P, Hays R. Beliefs about resistance self-efficacy and drug prevalence: Do they really affect drug use? Int J Addict. 1991;25(11A):1353–1378. doi: 10.3109/10826089009068468. [DOI] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. Am J Prev Med. 2004;27:18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Flay BR. Positive youth development is necessary and possible. In: Romer D, editor. Reducing adolescent risk: Toward an integrated approach. Sage Publications; Thousand Oaks, CA: 2003. pp. 347–354. [Google Scholar]
- Groeger JA, Zijlstra FRH, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some two thousand British adults. J Sleep Res. 2004;13(4):359–371. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- Gruenwald P, Johnson F, Treno A. Outlets, drinking and driving: A multilevel analysis of availability. J Stud Alcohol. 2002;63(4):460–468. doi: 10.15288/jsa.2002.63.460. [DOI] [PubMed] [Google Scholar]
- Harris KM, Gordon-Larsen P, Chantala K, Udry JR. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med. 2006;160:74–81. doi: 10.1001/archpedi.160.1.74. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Pentz MA, Weber MD, Dwyer JH, MacKinnon DP, Flay BR, Baer NA, Hansen WB. Relative effectiveness of comprehensive community programming for drug abuse prevention with high-risk and low-risk adolescents. J Consult Clin Psychol. 1990;58(4):447–456. doi: 10.1037//0022-006x.58.4.447. [DOI] [PubMed] [Google Scholar]
- Kaplan RM. The significance of quality of life in health care. Qual Life Res. 2003;12(S1):3–16. doi: 10.1023/a:1023547632545. [DOI] [PubMed] [Google Scholar]
- Koestner R, Lekes N, Powers TA, Chicoine E. Attaining personal goals: Self-concordance plus implementation intentions equals success. J Pers Soc Psychol. 2002;83(1):231–244. [PubMed] [Google Scholar]
- Krames . Fitness [Brochure] Krames; Yardley, PA: 2001. [Google Scholar]
- Morris SB. Estimating effect sizes from pretest-posttest-control group design. Organ Res Methods. 2008;11(2):364–386. [Google Scholar]
- Martin KA, Leary MR. Single, physically active, female: The effects of information about exercise participation and body weight on perceptions of young women. Soc Behav Personal. 2001;16(2):1–12. [Google Scholar]
- Meyers LS, Guarino AJ. Applied multivariate research: Design and interpretation. Sage Publications; Thousand Oaks, CA: 2006. [Google Scholar]
- Nigg CR, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: Common themes advancing health behavior research. Health Educ Res. 2002;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- Noar SM, Chabot M, Zimmerman RS. Applying health behavior theory to multiple behavior change: Considerations and approaches. Prev Med. 2008;46:275–280. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Orleans TC. Addressing multiple behavioral health risks in primary care. Am J Prev Med. 2004;27(2S):1–3. doi: 10.1016/j.amepre.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Peters LWH, Wiefferink CH, Hoekstra F, Buijs GJ, ten Dam GTM, Paulussen TGWM. A review of similarities between domain-specific determinates of four health behaviors among adolescents. Health Educ Res. 2009;24(2):198–223. doi: 10.1093/her/cyn013. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: An introduction and overview. Prev Med. 2008;46:181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth JL, Brooks-Gunn J. Youth development programs and healthy development. In: Romer D, editor. Reducing adolescent risk. Sage Publications; Thousand Oaks, CA: 2003. pp. 355–365. [Google Scholar]
- Ravesloot C, Seekins T, White G. Living Well With a Disability health promotion intervention: Improved health status for consumers and lower costs for health care policymakers. Rehabil Psychol. 2005;50(3):239–245. [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- SPSS Inc. SPSS 17.0 for Windows, Rel 17.0.0. [Computer software] SPSS Inc.; Chicago: 2008. [Google Scholar]
- Tebes JK, Feinn R, Vanderploeg JJ, Chinman MJ, Shepard J, Brabham T, Genovese M, Connell C. Impact of a positive youth development program in urban after-school settings on the prevention of adolescent substance use. J Adolesc Health. 2007;41:239–247. doi: 10.1016/j.jadohealth.2007.02.016. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- Werch C. The Behavior-Image Model: A paradigm for integrating prevention and health promotion in brief interventions. Health Educ Res. 2007;22(5):677–690. doi: 10.1093/her/cyl146. [DOI] [PubMed] [Google Scholar]
- Werch C, Moore M, DiClemente CC, Owen DM, Jobli E, Bledsoe R. A sport-based intervention for preventing alcohol use and promoting physical activity among adolescents. J Sch Health. 2003;73(10):380–388. doi: 10.1111/j.1746-1561.2003.tb04181.x. [DOI] [PubMed] [Google Scholar]
- Werch CE, Moore MJ, DiClemente CC, Bledsoe R, Jobli E. A multi-health behavior intervention integrating physical activity and substance use prevention for adolescents. Prev Sci. 2005;6(3):213–226. doi: 10.1007/s11121-005-0012-3. [DOI] [PubMed] [Google Scholar]
- Werch C, Moore MJ, Bian H, DiClemente CC, Ames SC, Weiler RM, Thombs D, Pokorny SB, Huang I-C. Efficacy of a brief image-based multiple behavior intervention for college students. Ann Behav Med. 2008;36(2):149–157. doi: 10.1007/s12160-008-9055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werch C, Bian H, Moore MJ, Ames S, DiClemente CC, Weiler RM. Brief multiple behavior interventions in a college student health care clinic. J Adolesc Health. 2007;41:577–585. doi: 10.1016/j.jadohealth.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werch C. Fitness & Health Survey 2006. University of Florida, Addictive and Health Behaviors Research Institute; Jacksonville, Florida: 2006. [Google Scholar]
- Wolfson A, Crowley S, Anwer U, Bassett JL. Changes in sleep patterns and depressive symptoms in first-time mothers: Last trimester to 1-year postpartum. Behav Sleep Med. 2003;1(1):54–67. doi: 10.1207/S15402010BSM0101_6. [DOI] [PubMed] [Google Scholar]
- Zullig KJ, Valois RF, Huebner ES, Drane JW. Evaluating the performance of the Center for Disease Control’s Health-related Quality of Life scales among adolescents. Public Health Rep. 2004;119:577–584. doi: 10.1016/j.phr.2004.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


