Abstract
Staphylococci, in particular Staphylococcus aureus, are the predominant cause of bone infections worldwide. These infections are painful, debilitating and with the rise in antibiotic-resistant forms, increasingly difficult to treat. The growth in the number of prosthetic joint replacement procedures also provides new opportunities for these infections to take hold. Comprehending the mechanisms by which staphylococci interact with and damage bone is critical to the development of new approaches to meet this challenge. This review summarises current understanding of the mechanisms by which staphylococci infect and damage bone. We address the role of the inflammatory response to staphylococcal infection in disrupting the homeostatic balance of bone matrix deposition and resorption and thereby mediating bone destruction. A number of virulence factors that have been shown to contribute to bone infection and pathology are discussed, however no single factor has been defined as being specific to bone infections. Although traditionally considered an extracellular pathogen, there is increasing evidence that staphylococci are able to invade host cells, and that an intracellular lifestyle may facilitate long-term persistence in bone tissue, enabling evasion of antimicrobials and host immune responses. ‘Small colony variant’ strains, with mutations disabling the electron transport pathway appear particularly adept at invading and persisting within host cells, and exhibit enhanced antimicrobial resistance, and may represent a further complication in the treatment and management of staphylococcal bone disease.
Keywords: Staphylococcus aureus, Small colony variants, Bone infection, Osteoblasts, Osteoclasts, Signalling
Introduction
Bacteria of the genus Staphylococcus are the principal causative agents of two major types of infection affecting bone – septic arthritis and osteomyelitis, which involve the inflammatory destruction of joint and bone. These infections cause serious morbidity and are often difficult to manage (Berendt and Byren, 2004). The principal routes of infection for both osteomyelitis and septic arthritis are either haematogenous, resulting from bacteremia; contiguous, when the infection is transmitted from local tissue; or direct, resulting from infiltration of bone, often following injury, surgery or implantation of a foreign body, such as joint replacement (Berendt and Byren, 2004; Ciampolini and Harding, 2000; Goldenberg, 1998; Lazzarini et al., 2004; Lew and Waldvogel, 2004). Infections may be acute or chronic and affect native joints, especially the hip and knee, or prosthetic joints, long bones, vertebrae and almost any other bone. Osteomyelitis of the foot is particularly common in diabetic patients (Berendt and Byren, 2004; Nade, 2003).
Septic arthritis is a joint disease typified by bacterial colonisation and rapid articular destruction (Levine and Siegel, 2003). Infiltration and growth of bacteria within the synovium results in inflammation with infiltration of leukocytes into the joint fluid (Goldenberg, 1998; Nade, 2003). The production of reactive oxygen species and host matrix metalloproteinases (MMPs), lysosomal enzymes and bacterial toxins contribute to the destruction of cartilage. This starts with degradation of host proteoglycans followed by collagen breakdown within hours of infection, and is mediated by polymorphonuclear leukocytes (Goldenberg, 1998; Nade, 2003; Shirtliff and Mader, 2002; Stott, 2001). The containment of the inflammatory process within the joint results in increasing pressure, which impedes blood and nutrient supply to the joint exacerbating joint damage and facilitating destruction of cartilage and the synovium. Permanent destruction of articular cartilage and subchondral bone can occur rapidly, within just a few days (Shirtliff and Mader, 2002).
Osteomyelitis describes a range of infections in which bone is colonized with microorganisms, with associated inflammation and bone destruction. Acute osteomyelitic foci are characterised by pus-forming inflammation at the site of microbial colonisation. Damage to bone matrix and compression and destruction of vasculature is also observed as the infection spreads to surrounding soft tissues, which can further exacerbate bone necrosis (Lazzarini et al., 2004; Lew and Waldvogel, 2004) Sections of dead bone, known as sequestra, can form which may then detach to form separate infectious foci which, due to the lack of vasculature, are protected from immune cells and antibiotics (Lazzarini et al., 2004; Lew and Waldvogel, 2004). Such areas of dead, infected tissues that are inaccessible to antimicrobials or the immune response can lead to chronic persistence of the infection (Lazzarini et al., 2004).
The incidence of septic arthritis is between 2 and 10 in 100,000 in the general populace but may be as high as 30–70 per 100,000 in rheumatoid arthritis sufferers or recipients of prosthetic joints (Goldenberg, 1998; Nade, 2003; Stott, 2001) and is more common in children than adults, and in males rather than females (Levine and Siegel, 2003). Haematogenous osteomyelitis most frequently effects children and the elderly (Lew and Waldvogel, 2004) and in children, the incidence is typically between 1 in 5000 and 1 in 10,000 (Weichert et al., 2008). It has been argued that the incidence of haematogenous osteomyelitis is decreasing with an annual fall in childhood cases of 0.185 per 100,000 people recorded in Glasgow, Scotland between 1970 and 1997 (Blyth et al., 2001; Lazzarini et al., 2004; Weichert et al., 2008). Conversely, osteomyelitis resulting from direct infection is reportedly on the increase (Gillespie, 1990; Lazzarini et al., 2004). Local spread of infection from contiguous tissue to bone or direct infection can occur at any age, with foreign body implants a substantial risk factor (Lew and Waldvogel, 2004). The presence of an implant is particularly associated with chronic osteomyelitis, where antibiotic treatment is frequently ineffective, and removal of the implant and debridement are required (Ciampolini and Harding, 2000). Relapsing cases of osteomyelitis with several decades between episodes have been documented, and there are records of reactivation fifty or even eighty years after the initial infection (Ciampolini and Harding, 2000; Gallie, 1951; Greer and Rosenberg, 1993; Korovessis et al., 1991).
A broad range of bacterial species have been isolated in cases of septic arthritis and osteomyelitis. Pathogens cultured from septic joints include S. aureus, Streptococcus pyogenes, Streptococcus pneumoniae, Escherichia coli, Pseudomonas aeruginosa, Serratia marcescens, as well as Salmonella, Neisseria, Aerobacter, and Bacteroides species (Nade, 2003; Shirtliff and Mader, 2002). Staphylococcus and Streptococcus spp., Haemophilus influenzae, E. coli, P. aeruginosa, Salmonella and Mycobacterium spp. are all potential causes of osteomyelitis (Bennet and Bennet, 2006; Lazzarini et al., 2004; Lew and Waldvogel, 1997, 2004). S. aureus is the most commonly identified pathogen in both conditions, by a substantial margin, regardless of type or route of infection (Ciampolini and Harding, 2000; Goldenberg, 1998; Lew and Waldvogel, 2004).
Staphylococcus, principally S. aureus, accounts for between 37% and 67% of septic arthritis isolates in studies from a range of nations (Al Arfaj, 2008; Dubost et al., 2002; Goldenberg, 1998; Ryan et al., 1997). Coagulase-negative staphylococci are less commonly isolated from arthritic joints, representing between 3% and 16% of Staphylococcus cultures (Al Arfaj, 2008; Dubost et al., 2002; Ryan et al., 1997). Studies of osteomyelitis in several developed countries over the past decade have identified S. aureus in 38% to 67% of culture-positive cases. Coagulase-negative staphylococci were identified in 5% to 15% of culture-positive patients (Arnold et al., 2006; Blyth et al., 2001; Grammatico et al., 2008; Karwowska et al., 1998). Surveillance data from the Health Protection Agency on surgical site infections in the U.K. between 1997 and 2005 found S. aureus to be the causative agent in 41.4% of hip prosthesis, 33.5% of knee prosthesis, 53% of open reduction of bone fracture and 59.1% of hip hemiarthroplasty infections. Coagulase-negative staphylococci accounted for 15.1%, 20.7%, 7.5% and 6.3% of these infections, respectively (U.K. Health Protection Agency, 2008). S. epidermidis is the most common coagulase-negative Staphylococcus species in many types of infection, including osteomyelitis and infection of prosthetic joints, but other species, including Staphylococcus simulans, Staphylococcus hominis, Staphylococcus capitis, Staphylococcus caprae and Staphylococcus lugdunensis have all been reported (Greig and Wood, 2003; Lang et al., 1999; Murdoch et al., 1996; Vallianou et al., 2008).
Clearly S. aureus, and to a lesser extent other staphylococci, are pathogens of major importance in skeletal infections. The number of joint replacement procedures is increasing: 220,000 hip replacements were performed in the USA in 2003, a 38% rise from 1996, with numbers projected to rise to 572,000 by 2030. Total knee replacements reached 418,000 in 2003 and are expected to undergo a similar rise, especially in light of an aging population (Lee and Goodman, 2008). In cases of septic arthritis antibiotic therapy is frequently effective if applied rapidly, appropriately and in combination with joint drainage (Shirtliff and Mader, 2002). Osteomyelitis is, however, often refractory to antibiotic treatment, a problem exacerbated by the increasing levels of antibiotic resistance amongst Staphylococcus spp. This is complicated further by the emergence of particularly persistent, antibiotic-resistant ‘small colony variant’ forms that may be selected for by certain current treatment regimens (Ciampolini and Harding, 2000; Henderson and Nair, 2003; von Eiff et al., 1997a). Staphylococcal bone infections are thus likely to be a continuing and probably increasing problem, and understanding of the interaction of these pathogens with bone is central to development of the novel therapeutic strategies required to treat increasingly antibiotic-resistant and persistent infections.
Genomic features of staphylococci associated with bone infections
A number of studies have attempted to identify an association between the possession of certain virulence genes by S. aureus and invasive disease. Thus Peacock et al. (2002) suggested that the possession of certain combinations of virulence factor genes is associated with invasive disease, and increased severity of infection following examination of a panel of 334 S. aureus isolates by PCR. The isolates comprised those from 179 healthy patients, 94 hospital-acquired isolates and 61 community-acquired isolates. Seven putative virulence genes, including the adhesin genes fnbA and cna, the toxin genes sej, eta and hlg, and icaA, which is involved in biofilm production, were found to be associated with invasive isolates. The association with specific types of invasive infection was not examined and indeed the small number of isolates examined in this study would have precluded such an analysis (Peacock et al., 2002). The genes for the fibronectin-binding proteins fnbA and fnbB have been reported to be present in 98% and 99% of clinical isolates, respectively, from a range of orthopaedic associated infections, whereas the cna gene, encoding the collagen-binding protein was identified in just 46% of isolates (Arciola et al., 2005). Another study by Peacock et al. (2000) found the prevalence of both fnbA and fnbB genes, as opposed to just one of the two, to be significantly higher in invasive isolates than in ‘carriage’ strains in a panel of 163 strains, which included septic arthritis and osteomyelitis isolates. Genes encoding Panton-Valentine leukocidin were found to be present in 59 of 89 S. aureus isolates from cases of acute haematogenous osteomyelitis. The presence of pvl genes is associated with an increased risk of severe infection requiring intensive care, bacteremia and more severe systemic inflammation (Bocchini et al., 2006; Sdougkos et al., 2007). However, one of the problems with the above studies is that it is unclear how representative these strain collections are of those isolates carried in other establishments and regions across the world, since strain typing was not reported.
Strain typing studies of S. aureus, using multilocus sequence typing (MLST) and comparative genomic microarray hybridizations have so far failed to identify any specific clonal lineages associated with invasive disease (Feil et al., 2003; Lindsay et al., 2006). However, these studies did not use a collection of isolates from specific invasive diseases and therefore do not rule out the possibility that specific lineages or genes are associated with specific types of infection, such as osteomyelitis or septic arthritis. To date, the only genome comparison study relevant to S. aureus bone infections has been done using comparative genome microarray hybridisations of the S. aureus UAMS-1 strain, isolated from an osteomyelitis patient, with a range of genome sequenced strains (Cassat et al., 2005). These authors found variations in the complement of adhesin, toxin, exoenzyme and regulatory genes. Although it is not possible to draw general conclusions about association with bone infection from characterisation of a single strain, the presence of fnbA, but not fnbB or the bone sialoprotein-binding gene bbp, in UAMS-1 suggest that fnbB and bbp are dispensable for bone infection, at least in certain genetic backgrounds. Thus at this juncture there is a lack of evidence to support or disprove an association between specific S. aureus lineages or specific genomic features and the pathogenesis of bone infections.
Bone as a target organ
In terrestrial vertebrates mature bone is made up of dense surface plates of bone, known as the cortices, and within these is a network of bone struts oriented to oppose loading forces, known as trabecular bone. Trabecular bone is typically replaced every 3–4 years, with the denser cortical bone taking over a decade to replace in adults (Blair, 1998). This process of continual remodelling is required to remove old bone and microfractures to ensure bone integrity and mineral homeostasis (Vaananen and Laitala-Leinonen, 2008). The skeleton is a dynamic organ system, in a state of perpetual turnover which is continually remodelled by the actions of two cell types (Henderson and Nair, 2003). Osteoblasts are responsible for the deposition of bone matrix; they are found on bone surfaces and are derived from mesenchymal osteoprogenitor cells. These cells secrete osteoid, a mixture of bone matrix proteins primarily made up of type I collagen (over 90%), proteoglycans such as decorin and biglycan, glycoproteins such as fibronectin, osteonectin and tenascin-C, osteopontin, osteocalcin and bone sialoprotein, oriented along stress lines (Blair, 1998; Mackie, 2003). Osteoblasts are also thought to facilitate the mineralization of bone matrix, whereby hydroxyapatite, [Ca3(PO4)2]3·Ca[OH]2, crystals form, making up around 90% of bone matrix (Blair, 1998; Mackie, 2003). It is thought that ‘nucleators’ are required to instigate mineralisation, and phosphate-containing matrix proteins like bone sialoprotein and osteopontin are likely to play such a role (Henderson and Nair, 2003; Mackie, 2003; van de Lest and Vaandrager, 2007). Osteoblasts also produce tissue non-specific alkaline phosphatase (TNAP) which cleaves phosphate esters to liberate free inorganic phosphate, which is key to the process of mineralisation (van de Lest and Vaandrager, 2007). Osteoblasts are not terminally differentiated, and some may form osteocytes and become implanted in the bone matrix, eventually ceasing the secretion of osteoid, whilst others undergo apoptosis (Blair, 1998; Mackie, 2003). Osteocytes are also involved in bone maintenance, detecting stress within the bone through mechanosensitive mechanisms located in extensive cellular projections, called canaliculi, that interconnect osteocytes (van de Lest and Vaandrager, 2007). Osteocytes are thought to respond to mechanical stress by undergoing apoptosis, leading to osteoclast recruitment and differentiation, possibly by alterations in the levels of soluble factors produced by the osteocyte. Candidates include transforming growth factor β (TGF-β), which may suppress osteoclastogenesis when produced by healthy osteocytes (Henriksen et al., 2009; Matsuo and Irie, 2008).
The opposing action of bone matrix removal is performed by osteoclasts, multinucleate cells that are derived from the macrophage-monocyte lineage. These cells express large quantities of a vacuolar-type H+-ATPase on their cell surface, along with chloride channel 7 (ClC 7) enabling localised hydrochloric acid secretion into a closed compartment, known as the resorption lacuna, and subsequent solubilisation of bone mineral (Blair et al., 1989; Blair, 1998; Kornak et al., 2001; Vaananen and Laitala-Leinonen, 2008). The cell is attached to the bone matrix by a sealing zone membrane to create this compartment, and fusion of acidified vesicles with the plasma membrane contributes further to acid release (Vaananen and Laitala-Leinonen, 2008). Following mineral solubilisation, proteolysis of bone matrix proteins is then possible. Cathepsin K is centrally involved in degradation of bone matrix, it is highly expressed by osteoclasts and digests substrates such as collagen and osteonectin (Bossard et al., 1996; Drake et al., 1996). Evidence from knock-out mouse and selective inhibitor experiments indicates that cathepsin L, and MMPs also play a role in degrading bone matrix (Everts et al., 2006). Osteoclasts also secrete acid phosphatases, such as tartrate-resistant acid phosphatase (TRAcP), which is used as an osteoclast marker and is activated by cathepsin K cleavage (Blair et al., 1989; Blair, 1998; Ek-Rylander et al., 1991; Ljusberg et al., 2005). TRAcP is able to generate reactive oxygen species in addition to having phosphatase activity (Hayman and Cox, 1994). The exact cellular function of TRAcP in bone resorption is not well understood, but serum TRAcP levels correlate with bone-resorptive activity, and TRAcP-deficient mice exhibit reduced osteoclastic bone resorption and increased bone mineralization (Angel et al., 2000; Hayman et al., 1996; Nesbitt and Horton, 1997; Salo et al., 1997).
The balance of activity between these two cell types is crucial to maintaining the proper homeostasis of bone turnover, and any shift in the relative levels of osteoblast and osteoclast activity can result in bone pathology (Henderson and Nair, 2003). Infection with a pathogen such as S. aureus is capable of stimulating such a shift, mediated in part by induction of an inflammatory response. There is intimate interaction between the two cell types, with osteoblasts interpreting the majority of extracellular signals and subsequently modulating osteoclast differentiation and function (Henderson and Nair, 2003; Matsuo and Irie, 2008). Interaction between the RANK (receptor activator for nuclear factor κB) receptor, expressed by osteoclast precursors, and its cognate ligand, RANKL, expressed by osteoblasts is essential for osteoclastogenesis (Matsuo and Irie, 2008). RANKL is a homotrimeric protein displayed on the membrane of osteoblasts, although it may be secreted following cleavage by MMPs 7 or 14, or ADAM (a disintegrin and metalloprotease domain) (Boyce and Xing, 2008; Hikita et al., 2006; Lynch et al., 2005). Suppression of MMP 14-mediated secretion enhances osteoclastogenesis (Boyce and Xing, 2008; Hikita et al., 2006). The RANK receptor is a homotrimeric transmembrane protein belonging to the tumour necrosis factor (TNF) receptor superfamily. Following binding of RANKL to RANK, TRAF (TNF receptor-associated factor) adaptor proteins are recruited, with binding sites for TRAF2, TRAF5 and TRAF6 all present on RANK (Kim et al., 1999; Wada et al., 2006). TRAF6 seems to play a central role in RANK-mediated osteoclast formation, and mice deficient in TRAF6 are osteopetrotic (Lomaga et al., 1999) whereas TRAF2 and TRAF5 are relatively marginal players in osteoclastogenesis (Kanazawa et al., 2003; Kanazawa and Kudo, 2005). Signalling via RANK, and these adaptor proteins, activates a number of transcription factors, including NFκB (nuclear factor κ B), AP-1 (activator protein 1) and NFATc1 (nuclear factor of activated T-cells, cytoplasmic, calcineurin-dependent 1) which drive osteoclast differentiation (Matsuo and Irie, 2008; Wada et al., 2006). Osteoprotegrin (OPG) is an endogenous inhibitor of RANKL signalling, functioning as a decoy receptor that binds to RANKL and prevents its association with RANK (Wada et al., 2006; Yasuda et al., 1998).
Inflammation in bone infection
A number of host cytokines play a significant role in the pathogenesis of osteomyelitis, and there is strong evidence that production of these cytokines is induced by staphylococcal infection of bone, and that they directly contribute to bone destruction. In particular, the inflammatory cytokines tumour necrosis factor α (TNFα), interleukin 1 (IL-1) and IL-6 seem to be especially important in bone physiology and pathology (Kwan et al., 2004). In patients with acute osteomyelitis, plasma levels of TNFα, IL-1β (the secreted form of IL-1) and IL-6 are all elevated (Evans et al., 1998; Klosterhalfen et al., 1996). High levels of IL-1β, IL-6 and TNFα are also found in the synovial fluid of patients with septic arthritis (Osiri et al., 1998; Saez-Llorens et al., 1990). Interestingly, specific polymorphisms in the IL-1α and IL-6 genes have recently been found to be associated with an increased risk of osteomyelitis in the Greek population (Tsezou et al., 2008).
A number of animal models of S. aureus osteomyelitis reveal that bone infection can lead to elevated levels of these cytokines both locally and systemically. Increased levels of IL-1β have been measured in the tibiae of 22-month-old rats experimentally implanted with S. aureus-infected needles, and the same animals have increased circulating levels of IL-6 (Garcia-Alvarez et al., 2009). In a murine osteomyelitis model, bone levels of IL-1β and IL-6 are significantly increased in the early post-infection period, with TNFα rising later during the infection (Yoshii et al., 2002). The local source of these cytokines is not fully clear. Production of IL-1β can be induced in human osteoblast-like cell lines by a variety of stimuli, including TNFα (Pivirotto et al., 1995). However, infection of primary mouse osteoblasts with S. aureus results in increased transcription, but not increased protein synthesis or secretion of IL-1β (Marriott et al., 2002). TNFα is detectable only at low levels in human osteoblasts derived from mesenchymal stem cells and the osteosarcoma cell line MG63 (Bu et al., 2003). Infiltrating immune cells may therefore be a more likely source of IL-1β and TNFα in bone in response to infection (Bost et al., 1999; Ishimi et al., 1990; Marriott et al., 2002; Mundy, 1991; Robinson et al., 2007). IL-6 however, is produced by osteoblasts in response to a variety of signals, including infection with S. aureus (Bost et al., 1999; Ishimi et al., 1990).
These cytokines have potent effects on the process of bone remodelling, and are strongly implicated in the pathology of osteomyelitis. Cell culture models support the view that IL-1 and TNFα stimulate the proliferation and differentiation of osteoclast progenitors into mature osteoclasts in the presence of osteoblasts (Mundy, 1991; Pfeilschifter et al., 1989; Tokukoda et al., 2001). TNFα and IL-1β also stimulate osteoclast-mediated bone resorption, a process which may also require the presence of osteoblasts (Azuma et al., 2000; Taubman and Kawai, 2001; Thomson et al., 1987). Similarly, IL-6 increases bone resorption activity and osteoclast number in cultured mouse calvariae, and stimulates osteoclast differentiation in the presence of osteoblasts (Ishimi et al., 1990; Kotake et al., 1996). In vivo, local administration of IL-1 and TNF antagonists in a non-human primate model of periodontitis results in significant reduction of osteoclast formation and bone destruction (Assuma et al., 1998). Intravenous administration of TNFα and IL-1 in mice stimulates bone resorption in a dose-dependent fashion (Konig et al., 1988), and deletion of the murine IL-1R, TNF-R1 and TNF-R2 receptors and of caspase-1 significantly decreases osteoclast number and the area of bone resorption in calvariae following lipopolysaccharide (LPS) injection (Chiang et al., 1999).
IL-1β and TNFα also inhibit the differentiation of mesenchymal stem cells into osteoblast-like cells, and suppress the accompanying mineralisation and increased expression of alkaline phosphatase and procollagen I genes, although only TNFα inhibits osteonectin and osteopontin gene expression (Lacey et al., 2008). TNFα also decreases production of type I collagen and osteocalcin, and of alkaline phosphatase in a variety of osteoblast cell culture and bone tissue explant models, thereby reducing matrix deposition and mineralisation (Canalis, 1987; Centrella et al., 1988; Li and Stashenko, 1992; Nanes et al., 1989, 1991; Nanes, 2003; Smith et al., 1987).
Surface-associated material (SAM) from S. aureus stimulates bone resorption and osteoclast formation, and blockade of IL-1 or TNFα signalling completely abolishes this bone resorption activity. Neutralisation of TNFα and IL-6 fully abolishes SAM-stimulated osteoclastogenesis, with antagonism of IL-1 having only a partial effect (Meghji et al., 1998; Nair et al., 1995). The effect of this SAM on osteoclast formation and stimulation of resorption does not require co-culture with osteoblasts, and does not require RANKL signalling (Lau et al., 2006). S. epidermidis surface material can also induce bone resorption, by a mechanism that is strongly dependent on TNFα and, to a lesser extent, IL-1 (Meghji et al., 1997).
Induction and release of these cytokines in response to pathogen-associated molecules involves two main classes of pattern recognition receptors (PRRs), the Toll-like receptors (TLRs) and NOD-like receptors (NLRs). The production of TNFα and IL-6 by murine macrophages in response to S. aureus cell wall preparations is dependent on TLR2, and TLR2-deficient mice exhibit reduced survival of intravenous S. aureus infections compared to wild-type counterparts (Takeuchi et al., 1999, 2000). Signalling through TLRs, in response to microbial ligands such as LPS, ‘primes’ the cell for IL-1β production by inducing expression of the inactive, pro-form of the cytokine (Creagh and O'Neill, 2006; Kahlenberg et al., 2005). IL-1β is synthesised as a 31-kDa precursor molecule, and is processed to produce a 17-kDa active molecule by caspase-1. Caspase-1 activation, and subsequent processing and release of active IL-1β involves assembly of a multiprotein complex known as the inflammasome. This complex consists of caspase-1, the adaptor protein ASC (apoptosis-associated speck-like protein containing a caspase recruitment domain (CARD)) and one of several NLR proteins, of which four are known to associate with inflammasomes (Ting et al., 2008). Each NLR responds to different activating signals, and although the exact recognition steps remain to be elucidated, reported stimuli include flagellin, anthrax lethal toxin, and muramyl dipeptide (Boyden and Dietrich, 2006; Faustin et al., 2007; Franchi et al., 2006; Miao et al., 2006). A broad range of stimuli for NLRP3 (NLR family pyrin domain containing 3) have been reported, including S. aureus. Although NLRP3 and ASC are essential for IL-1β secretion by murine macrophages in response to S. aureus, the stimulating signal is as yet unknown, and deletion of the α-, β- and γ-toxins does not perturb production of the cytokine (Mariathasan et al., 2006; Ting et al., 2008). The inflammasome is involved in cell death in response to bacterial invasion (Marriott et al., 2002; McCall et al., 2008) and although invasion of murine osteoblasts by S. aureus induces apoptosis, it is not established whether the inflammasome is involved (Tucker et al., 2000).
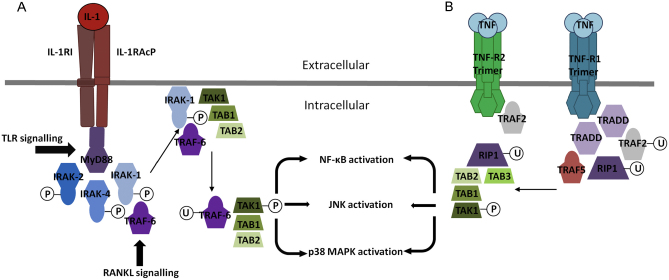
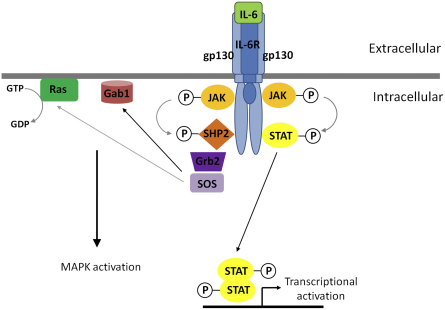
The major signal transduction events following binding of IL-1 and TNF to their respective receptors are shown in Fig. 1. Signalling in response to both cytokines leads to eventual activation of the NFκB transcription factor and JNK (c-Jun N-terminal kinase) and p38 MAPK (mitogen-activated protein kinase) signalling (Arend et al., 2008; Dinarello, 2009). Studies with knockout mice have shown that at least one of the p50 or p52 NFκB subunits is required for IL-1-induced osteoclast formation and resorptive activity, indicating that much of the osteoclastogenic activity of IL-1 is dependent on NFκB (Xing et al., 2003). TNFα binds to two receptors, TNF type I (TNF-R1) and type II (TNF-R2) receptor which differ in their signalling mechanisms although there is substantial signalling crosstalk between the two receptors (Aggarwal, 2003; Wajant et al., 2003). Interestingly, the S. aureus virulence factor protein A, in addition to possession of immunoglobulin G-binding activity, is able to bind to the TNF-R1 receptor and stimulates downstream signalling and inflammation (Gomez et al., 2004). TNFα mediates the osteoclastogenic activity of RANKL. TNFα production by osteoclast progenitors is induced by RANKL and stimulates osteoclast differentiation in an autocrine manner (Zou et al., 2001). Fig. 2 shows an overview of the signal transduction events following IL-6 binding to its receptor. Signal transduction involves the activation of Janus family (JAK) tyrosine kinases and subsequent phosphorylation and activation of STAT (signal transducers and activators of transcription) family transcription factors (Kwan et al., 2004). IL-6 mediates bone resorption indirectly, and has no effect on isolated osteoclasts and IL-6 induction of osteoclastogenesis is dependent on the expression of the IL-6 receptor by osteoblasts, but not osteoclast progenitors (Hattersley et al., 1988; Kwan et al., 2004; Udagawa et al., 1995).
Fig. 1.
Schematic diagram of IL-1 and TNF signal transduction events. (A) IL-1 binding to IL-1RI results in recruitment of the IL-1 receptor accessory protein IL-1RAcP, which form a complex that, via the intracellular Toll/IL-1 receptor (TIR) domains of the two receptor molecules, engages the MyD88 (myeloid differentiation factor 88) adaptor protein (Arend et al., 2008; Dinarello, 2009; Verstrepen et al., 2008). MyD88 binding initiates phosphorylation of IRAK-4 (interleukin-1 receptor-associated kinase 4), IRAK-2 and IRAK-1. IRAK-1 recruits TRAF6 and these two proteins localise to the cell membrane where they associate with TAK1 (TGF-β-activated kinase 1), TAB1 (TAK1-binding protein) and TAB2. The TAK1/TAB1/TAP2/TRAF6 complex translocates to the cytosol where TRAF-6 is poly-ubiquitinated and TAK1 is subsequently phosphorylated, and activates NF-κB, p38 MAPK and JNK. The MyD88 adaptor molecule and downstream signalling events are common to most Toll-like receptors (TLRs), and, via TRAF6, this pathway also converges with RANKL signalling. (B) Engagement of the homotrimeric TNF-R1 receptor by TNF enables recruitment of TRADD (TNF-R1 associated death domain protein) via homotypic death domain interactions. TRADD associates with itself, TRAF2 and RIP1 (receptor-interacting protein 1) and with TRAF5. TNF-R2 is able to directly associate with TRAF2, independently of TRADD. TRAF2 auto-poly-ubiquitinates and ubiquitinates RIP1. Poly-ubiquitination of RIP1 then leads to the recruitment of TAK1, through interactions with TAB1, TAB2 and TAB3, again leading to NF-κB, p38 MAPK and JNK activation (Bradley, 2008; Verstrepen et al., 2008).
Fig. 2.
Schematic diagram of IL-6 signalling events. IL-6 specifically binds to IL-6 receptor α (IL-6Rα), and recruits a homodimer of the gp130 signal-transducing protein (Naugler and Karin, 2008). This in turn leads to association of the JAK kinases JAK1, JAK2 and TYK2 with gp130, and the autophosphorylation of these kinases (Heinrich et al., 2003). JAK1 is of particular importance in IL-6 signalling, and cells deficient in this kinase exhibit substantial signalling impairment (Guschin et al., 1995; Heinrich et al., 2001; Rodig et al., 1998). Following JAK activation, gp130 is phosphorylated on multiple tyrosine residues, enabling recruitment and phosphorylation of STAT family transcripton factors. STAT3 is the major transcription factor acting downstream of IL-6 signalling, and dimerises upon phosphorylation and translocates to the nucleus to activate transcription of an array of target genes (Li et al., 2002; Naugler and Karin, 2008). IL-6 also activates the MAPK pathway, via JAK phosphorylation of SHP2 (SH2 domain-containing protein-tyrosine phosphatase). SHP2 is thought to recruit either the Grb2-SOS (growth factor receptor-bound protein/Son of Sevenless) complex and/or Gab1 (Grb2-associated binder 1) to gp130. Recruitment of SOS then enables activation of Ras and subsequently the MAPK (mitogen-associated protein kinase) pathway, although the importance of this pathway is currently unclear (Heinrich et al., 2003; Naugler and Karin, 2008).
It is clear that these cytokines have a prominent role in modulating bone turnover, and perturbation of their levels can have profound effects on this process. Although some mechanistic details are currently lacking, there is strong evidence that S. aureus infection of bone initiates local and systemic production of TNFα, IL-1 and IL-6 via host PRRs. Elevated levels of these cytokines then shift the homeostatic balance of bone turnover, increasing osteoclast differentiation and bone resorption and diminishing osteoblast-mediated bone matrix production and mineralisation, thereby driving bone destruction.
Staphylococcal invasion of bone cells
In addition to staphylococcal induction of inflammatory mediators that modulate the actions of osteoblasts and osteoclasts, bacteria of this genus are involved in more direct interactions with bone cells. Invasion and persistence of S. aureus in ‘non-professional phagocytic’ host cells in vitro has been described for many different cell types, including epithelial cells, endothelial cells and keratinocytes (Garzoni and Kelley, 2009; Kintarak et al., 2004). In cell culture systems, S. aureus is able to invade cultured osteoblasts from murine, human and embryonic chick sources, and S. epidermidis is also able to invade and grow within cultured osteoblasts (Ellington et al., 1999; Hudson et al., 1995; Jevon et al., 1999; Khalil et al., 2007; Reilly et al., 2000). Electron microscopy has demonstrated the presence of bacteria within osteoblasts and osteocytes of embryonic chicks following injection with S. aureus, indicating that internalisation by bone cells also occurs in vivo (Reilly et al., 2000). Intracellular bacteria inside osteoblasts and osteocytes in a patient with recurrent, long-term osteomyelitis of the fibula have been visualised by light and electron microscopy, although the species was unfortunately not determined (Bosse et al., 2005). More recently Stoodley et al. (2008), have demonstrated S. aureus biofilms in an infected total joint arthroplasty. Although not reported in this paper the authors also identified S. aureus within host cells (personal communications, Stoodley). Thus the suggestion that internalisation of S. aureus by bone cells in vivo provides a protective niche for the bacterium, where it is shielded from immune effector mechanisms and antibiotics, may help to explain persistent cases of osteomyelitis. However, the true importance of intracellular staphylococci in clinical osteomyelitis has yet to be established (Henderson and Nair, 2003).
S. aureus requires fibronectin-binding proteins (FnBPs) expressed on the surface of the bacterium to enable uptake by osteoblasts, and many other cell types (Ahmed et al., 2001; Garzoni and Kelley, 2009; Sinha et al., 1999). These proteins belong to a group of adhesins known as MSCRAMMs (microbial surface components recognising adhesive matrix molecules), which bind a range of extracellular matrix proteins including fibronectin, fibrinogen, collagen, elastin and bone sialoprotein (Hauck and Ohlsen, 2006). Mutants deficient in the two FnBPs, FnBPA and FnBPB invade host cells very poorly (Ahmed et al., 2001; Sinha et al., 1999). Invasion is dependent on fibronectin binding by these proteins, and on the host cell integrin α5β1 receptor (Dziewanowska et al., 1999; Fowler et al., 2000; Sinha et al., 1999). S. aureus binds to fibronectin via FnBPs displayed on the bacterial surface, and fibronectin serves as a bridging molecule to the integrin α5β1 which acts as a “phagocytic” receptor (Sinha et al., 1999). Alternative uptake mechanisms do exist in certain cell types, however, as S. aureus is still able to invade primary keratinocytes in the absence of FnBPs and uptake is not inhibited by blockade of integrin α5β1 binding to fibronectin (Kintarak et al., 2004). The mechanism of invasion also differs between S. aureus and S. epidermidis and the latter does not gain entry via the fibronectin-integrin α5β1 mechanism (Khalil et al., 2007). The level of expression of the alternative sigma factor, σB, affects fnbA expression and the fibronectin binding ability of S. aureus strains and correlates with the level of internalisation of bacteria by osteoblasts suggesting that σB-mediated up-regulation of FnBP expression may facilitate invasion (Mitchell et al., 2008; Nair et al., 2003).
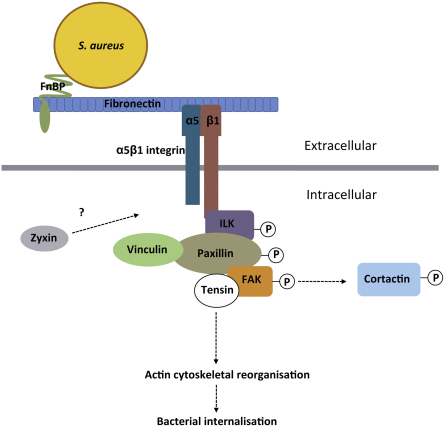
Integrin α5β1-mediated uptake of S. aureus requires remodelling of the actin cytoskeleton (Agerer et al., 2005). The integrin-linked kinase, ILK, provides a link between α5β1 and the cytoskeleton, and interacts with the cytoplasmic domains of β integrins and is subsequently activated. ILK activity is required for internalisation of S. aureus by epithelial cells (Wang et al., 2006). Recruitment of focal adhesion proteins, including the adaptor protein paxillin and the focal adhesion kinase, FAK, follows (Boulter and Van Obberghen-Schilling, 2006). Upon infection of HEK293T cells with S. aureus there is also recruitment of focal adhesion proteins, such as tensin, zyxin and vinculin to the site of bacterial attachment. FAK is recruited and tyrosine phosphorylated, and FAK-deficient cells are able to internalise S. aureus much less efficiently. Phosphorylation of downstream substrates of FAK, including cortactin, which is involved in actin cytoskeletal organisation, occurs during invasion, and interference with cortactin also reduces internalisation. So, signalling downstream of the integrin α5β1 receptor, involving ILK and FAK, is important for S. aureus invasion, at least in certain cell types (Agerer et al., 2005; Wang et al., 2006). Fig. 3 shows an overview of some of the events involved in the internalisation of S. aureus by host cells.
Fig. 3.
Schematic diagram of some of the signalling events involved in invasion of ‘non-professional phagocytic’ host cells by S. aureus. FnBPs expressed on the bacterial surface bind to fibronectin molecules in the extracellular matrix, which form a bridge with integrin α5β1 on the host cell membrane (Dziewanowska et al., 1999; Fowler et al., 2000; Sinha et al., 1999). Ligation of this complex to the integrin receptor causes receptor clustering and subsequent activation of ILK, via interaction with the β1 subunit (Wang et al., 2006). There is subsequent recruitment of paxillin and FAK and downstream phosphorylation of cortactin leading to remodelling of the actin cytoskeleton to enable bacterial uptake (Agerer et al., 2005). The focal adhesion proteins zyxin, vinculin and tensin are also recruited to the site of bacterial uptake, the latter two potentially via interactions with paxillin and FAK, respectively (Agerer et al., 2005).
Physical contact between S. aureus and osteoblasts induces host cell expression of tumour necrosis factor apoptosis inducing ligand (TRAIL) (Alexander et al., 2003). TRAIL is a member of the TNF cytokine family, and binds to two death domain-containing receptors, TRAIL receptors 1 and 2, which once activated recruit the FADD (Fas-associated protein with death domain) adaptor protein which in turn activates caspases 8 and −10 and commits the cell to an apoptotic pathway (Mahalingam et al., 2009). TRAIL produced by S. aureus-infected osteoblasts induces caspase-8 activation and apoptosis in cultured osteoblasts (Alexander et al., 2003). Uninfected osteoblasts cultured alongside infected cells also express TRAIL (Reott Jr., et al., 2008). TRAIL can induce apoptosis in human osteoclasts via TRAIL receptor 2, and also inhibits osteoclast differentiation (Colucci et al., 2007; Zauli et al., 2004). It is therefore possible that apoptosis of bone cells infected with S. aureus, and potentially of neighbouring uninfected cells may contribute to bone loss in osteomyelitis (Henderson and Nair, 2003).
Growing experimental support indicates that staphylococcal invasion of osteoblasts, most likely via the FnBP-fibronectin-integrin α5β1 bridging mechanism in the case of S. aureus, may play a role in the pathogenesis of bone infections. This intracellular location may provide a protected environment for bacteria, aiding prolonged persistence by enabling evasion of antimicrobials and host immune mechanisms and possibly contributing to bone damage by inducing apoptosis of infected cells.
Staphylococcal virulence determinants
A number of animal models of bone implant infection, osteomyelitis and septic arthritis have been developed which have enabled the role of specific virulence factors in infections to be determined. As mentioned at the outset there are a number of routes of bone infection, i.e. haematogenous, contiguous and direct infection of bone, and models have been developed to mimic each of these routes of infection. This is important since the range of environments experienced by the bacterium differs for each route and hence the virulence factors that are involved in pathology may be different for each route of infection. The septic arthritis model developed by Tarkowski and colleagues (Bremell et al., 1991, 1992; Tarkowski et al., 2001) in conjunction with defined isogenic mutants deficient in one or more virulence determinants, or with neutralising antibodies to virulence factors has proven to be particularly useful in elucidating the role of specific virulence determinants and host factors in bone infections. This model has shown that there is a plethora of virulence determinants involved in S. aureus septic arthritis (Table 1) some of which are also involved in osteomyelitis (Table 1). However, there is some controversy in this area because whilst the murine septic arthritis model is well established and standardised a number of different models have been developed for osteomyelitis and the relevance of specific virulence factors to bone implant infections or osteomyelitis appears to be dependent on the particular model used. For example the collagen adhesin Cna has been shown to contribute to osteomyelitis by some workers (Elasri et al., 2002) but not by others (Johansson et al., 2001) and has been reported not to be important in orthopaedic device infections (Darouiche et al., 1997). The role of FnBPs has not been directly assessed in a model of osteomyelitis, but comparison of S. aureus strains with and without fibronectin-binding activity in a mouse osteomyelitis model suggests that fibronectin-binding strains may give rise to more severe bone infections (Johansson et al., 2001). In the septic arthritis model, S. aureus fnbA fnbB mutants show no reduction in severity of arthritis, in contrast with clfA clfB mutants lacking the fibrinogen-binding clumping factors. However, the presence of the fnb genes results in greater weight loss and mortality, as well as higher serum levels of IL-6, indicating a role for FnBPs in the systemic inflammatory response (Palmqvist et al., 2005).
Table 1.
Virulence determinants which have been demonstrated to play a role in the pathology of experimental S. aureus bone infections. Most studies have utilised the murine model of septic arthritis.
| Virulence determinant | Model | Reference |
|---|---|---|
| Accessory gene regulator (agr) | A, O | Abdelnour et al., 1993; Blevins et al., 2003; Gillaspy et al., 1995 |
| Alpha-toxin and gamma-toxin | A | Gemmell et al., 1997; Nilsson et al., 1999 |
| Collagen adhesin (Cna) | A, O | Elasri et al., 2002; Nilsson et al., 1998; Patti et al., 1994; Xu et al., 2004 |
| Clumping factor (ClfA) | A | Josefsson et al., 2001; Palmqvist et al., 2004, 2005 |
| Capsular polysaccharide | A | Nilsson et al., 1997 |
| DltA (D-alanine modification of teichoic acid) | A | Collins et al., 2002 |
| Fibronectin-binding proteins | O | Johansson et al., 2001 |
| MgrA (a global regulator) | A | Jonsson et al., 2008 |
| MprF (L-lysine modification of membrane lipids) | A | Peschel et al., 2001 |
| Peptidoglycan | A | Liu et al., 2001 |
| Pls (plasmin-sensitive protein) | A | Josefsson et al., 2005 |
| Protein A | A | Gemmell et al., 1997; Palmqvist et al., 2002 |
| Ribonucleotide reductase class III | A | Kirdis et al., 2007 |
| Sigma factor B (σB) and sigma factor S (σs) | Jonsson et al., 2004; Shaw et al., 2008 | |
| Sortase SrtA (responsible for anchoring many adhesins to the bacterial cell wall) | A | Jonsson et al., 2002 |
| Small colony variant phenotype | A | Jonsson et al., 2003 |
| Staphylococcal accessory regulator | A, O | Blevins et al., 2003 |
| Staphylococcal DNA | A | Deng et al., 1999 |
| Staphylococcal superantigens | A | Abdelnour et al., 1994; Bremell and Tarkowski, 1995 |
| Two putative lytic transglycosylases, IsaA and SceD | A | Stapleton et al., 2007 |
A, arthritis; O, osteomyelitis.
One area of research that has received surprisingly little attention is that of the direct action of virulence factors on bone and bone cells. Work in our own laboratory has shown that S. aureus and S. epidermidis produce surface-associated proteins that can stimulate bone breakdown in an in vitro assay (Meghji et al., 1997; Nair et al., 1995). These surface-associated proteins and capsular material appear to promote the formation and activation of the bone-resorbing osteoclast (Lau et al., 2006; Meghji et al., 1998). Interestingly, a proportion of the population have antibodies that can block the action of the S. aureus proteins and prevent bone breakdown (Nair et al., 1997). The identity of the protein(s) in these mixtures which cause bone destruction has not been elucidated.
Small colony variants
Variant forms of S. aureus, known as small colony variants (SCVs), are associated with infections of bone and joint that may be particularly persistent, recurrent and refractory to antibiotic treatment (von Eiff et al., 2006). These bacteria are mutant forms of Staphylococcus that may have an adaptive advantage enabling persistent bone colonisation. SCV forms of coagulase-negative staphylococci, including S. epidermidis, S. lugdunensis and S. capitis have also been isolated from a range of infections (Adler et al., 2003; Seifert et al., 2005; von Eiff et al., 1999, 2006). The SCV phenotype is characterised by slow growth, with colonies around 10-fold smaller than wild-type forms, often with decreased pigmentation, increased aminoglycoside resistance and some reports of reduced haemolytic activity (Sendi and Proctor, 2009). The nature of these phenotypes can cause difficulty in detection and identification of the bacteria, and may contribute to an underestimation of the clinical prevalence of SCVs (von Eiff, 2008). These phenotypes usually result from auxotrophy for hemin, menadione or thymidine and can be reversed by supplementation with these molecules (Proctor et al., 1995, 2006). Mutations in the hemB and menD genes produce hemin and menadione auxotrophic strains with typical SCV phenotypes, and give rise to disruption of electron transport which is the basis of the growth deficiency, increased aminoglycoside resistance and other phenotypes (Bates et al., 2003; Proctor et al., 2006; von Eiff et al., 1997b). SCVs can be selected for with gentamicin in vitro, and there is evidence that antibiotic therapy, in particular use of gentamicin beads, which are used in addition to debridement and systemic antibiotic therapy for osteomyelitis may select for SCVs in clinical situations (Musher et al., 1977; von Eiff et al., 1997a). In a cohort of fourteen patients with confirmed S. aureus osteomyelitis, SCVs were isolated only from those four that had received gentamicin bead therapy, with the remaining ten patients harbouring normal S. aureus strains. Of the four SCVs, three were auxotrophic for hemin, and one for menadione. Only the patients harbouring SCVs had recurrent infections, although only patients whose gentamicin bead therapy had failed were included in the study (von Eiff et al., 1997a). SCVs have also been isolated from cases of infection of hip prostheses, and intracellular bacteria within host fibroblasts were identified in one of the five instances (Sendi et al., 2006).
Clinically isolated SCVs with hemin auxotrophy, and defined hemB mutants, show enhanced intracellular persistence in a range of human cell types (Moisan et al., 2006; Vaudaux et al., 2002; von Eiff et al., 1997b, 2001). The basis of this persistence is not established but may involve a number of possible mechanisms. S. aureus hemB mutants exhibit enhanced binding to fibrinogen and fibronectin, and transcribe and display more ClfA and FnBP on their surface, which may increase attachment and uptake by host cells (Vaudaux et al., 2002). Transcriptional profiling of clinical and defined mutant SCVs reveals increased transcription of genes regulated by σB, including adhesin genes, and down-regulation of exoprotein and toxin genes (Moisan et al., 2006). The effect of increased σB activity on MSCRAMM expression has been shown to correlate well with osteoblast invasion, adding weight to the argument that σB-mediated up-regulation of adhesins increases host cell invasion, at least in vitro, and that increased invasion by SCVs may be partially dependent on this mechanism (Moisan et al., 2006; Nair et al., 2003). It has been argued that reduced production of toxins, particularly haemolysins, by SCVs also contributes to intracellular persistence by reducing the cytotoxic effect on host cells (Moisan et al., 2006; Sendi and Proctor, 2009; von Eiff et al., 1997b).
In a murine septic arthritis model, a defined stable hemB mutant, exhibiting the SCV phenotype, elicited more frequent and severe arthritis than the parental strain despite a reduced bacterial load in the kidney and joints. It has been argued that SCVs are therefore more virulent on a ‘per organism’ basis and that enhanced protease production by hemB mutants may partially explain this (Jonsson et al., 2003). It may be that in clinical infections relatively small numbers of SCVs with enhanced virulence survive within tissues, possibly intracellularly, for extended periods and cause persistent infections. Clinically isolated SCVs are able to revert to the parent phenotype, although to what extent this may play a role in infections, and whether S. aureus may ‘switch’ between states in different in vivo situations is currently unclear.
Conclusions
Staphylococcus species are a major cause of debilitating bone disease globally, a situation that shows no sign of abating. The increasing antibiotic resistance of staphylococci, combined with the greater opportunity for infection afforded by escalating numbers of orthopaedic surgical procedures will only serve to exacerbate the problem. Furthermore, evidence is now emerging that staphylococci are facultative intracellular pathogens, and are able to exploit this protected niche during bone infection to enhance persistence. Spontaneously arising mutant forms, such as SCVs, may be particularly adapted to this lifestyle, complicating the treatment of these infections further. Although host factors involved in the inflammatory destruction of bone are increasingly well understood, the staphylococcal virulence determinants directly involved in skeletal colonisation and destruction are less well characterised. Continued focus on elucidating the complex interactions between host and pathogen in these invasive skeletal infections is required to develop more effective treatment regimes. Enhanced understanding of these interactions will not only inform improved clinical management of bone disease, but may well open up new avenues for therapeutic development.
Acknowledgement
We are grateful to the Arthritis Research Campaign for project grant funding (grant number 18294).
References
- Abdelnour A., Arvidson S., Bremell T., Ryden C., Tarkowski A. The accessory gene regulator (agr) controls Staphylococcus aureus virulence in a murine arthritis model. Infect. Immun. 1993;61:3879–3885. doi: 10.1128/iai.61.9.3879-3885.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdelnour A., Bremell T., Tarkowski A. Toxic shock syndrome toxin 1 contributes to the arthritogenicity of Staphylococcus aureus. J. Infect. Dis. 1994;170:94–99. doi: 10.1093/infdis/170.1.94. [DOI] [PubMed] [Google Scholar]
- Adler H., Widmer A., Frei R. Emergence of a teicoplanin-resistant small colony variant of Staphylococcus epidermidis during vancomycin therapy. Eur. J. Clin. Microbiol. Infect. Dis. 2003;22:746–748. doi: 10.1007/s10096-003-1029-9. [DOI] [PubMed] [Google Scholar]
- Agerer F., Lux S., Michel A., Rohde M., Ohlsen K., Hauck C.R. Cellular invasion by Staphylococcus aureus reveals a functional link between focal adhesion kinase and cortactin in integrin-mediated internalisation. J. Cell Sci. 2005;118:2189–2200. doi: 10.1242/jcs.02328. [DOI] [PubMed] [Google Scholar]
- Aggarwal B.B. Signalling pathways of the TNF superfamily: a double-edged sword. Nat. Rev. Immunol. 2003;3:745–756. doi: 10.1038/nri1184. [DOI] [PubMed] [Google Scholar]
- Ahmed S., Meghji S., Williams R.J., Henderson B., Brock J.H., Nair S.P. Staphylococcus aureus fibronectin binding proteins are essential for internalization by osteoblasts but do not account for differences in intracellular levels of bacteria. Infect. Immun. 2001;69:2872–2877. doi: 10.1128/IAI.69.5.2872-2877.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Arfaj A.S. A prospective study of the incidence and characteristics of septic arthritis in a teaching hospital in Riyadh, Saudi Arabia. Clin. Rheumatol. 2008;27:1403–1410. doi: 10.1007/s10067-008-0934-9. [DOI] [PubMed] [Google Scholar]
- Alexander E.H., Rivera F.A., Marriott I., Anguita J., Bost K.L., Hudson M.C. Staphylococcus aureus-induced tumor necrosis factor-related apoptosis-inducing ligand expression mediates apoptosis and caspase-8 activation in infected osteoblasts. BMC Microbiol. 2003;3:5. doi: 10.1186/1471-2180-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angel N.Z., Walsh N., Forwood M.R., Ostrowski M.C., Cassady A.I., Hume D.A. Transgenic mice overexpressing tartrate-resistant acid phosphatase exhibit an increased rate of bone turnover. J. Bone Miner. Res. 2000;15:103–110. doi: 10.1359/jbmr.2000.15.1.103. [DOI] [PubMed] [Google Scholar]
- Arciola C.R., Campoccia D., Gamberini S., Baldassarri L., Montanaro L. Prevalence of cna, fnbA and fnbB adhesin genes among Staphylococcus aureus isolates from orthopedic infections associated to different types of implant. FEMS Microbiol. Lett. 2005;246:81–86. doi: 10.1016/j.femsle.2005.03.035. [DOI] [PubMed] [Google Scholar]
- Arend W.P., Palmer G., Gabay C. IL-1, IL-18, and IL-33 families of cytokines. Immunol. Rev. 2008;223:20–38. doi: 10.1111/j.1600-065X.2008.00624.x. [DOI] [PubMed] [Google Scholar]
- Arnold S.R., Elias D., Buckingham S.C., Thomas E.D., Novias E., Arkader A., Howard C. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J. Pediatr. Orthop. 2006;26:703–708. doi: 10.1097/01.bpo.0000242431.91489.b4. [DOI] [PubMed] [Google Scholar]
- Assuma R., Oates T., Cochran D., Amar S., Graves D.T. IL-1 and TNF antagonists inhibit the inflammatory response and bone loss in experimental periodontitis. J. Immunol. 1998;160:403–409. [PubMed] [Google Scholar]
- Azuma Y., Kaji K., Katogi R., Takeshita S., Kudo A. Tumor necrosis factor-alpha induces differentiation of and bone resorption by osteoclasts. J. Biol. Chem. 2000;275:4858–4864. doi: 10.1074/jbc.275.7.4858. [DOI] [PubMed] [Google Scholar]
- Bates D.M., von E.C., McNamara P.J., Peters G., Yeaman M.R., Bayer A.S., Proctor R.A. Staphylococcus aureus menD and hemB mutants are as infective as the parent strains, but the menadione biosynthetic mutant persists within the kidney. J. Infect. Dis. 2003;187:1654–1661. doi: 10.1086/374642. [DOI] [PubMed] [Google Scholar]
- Bennet G.C., Bennet S.J. Infection of bone and joint. Surgery (Oxford) 2006;24:211–214. [Google Scholar]
- Berendt T., Byren I. Bone and joint infection. Clin. Med. 2004;4:510–518. doi: 10.7861/clinmedicine.4-6-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair H.C. How the osteoclast degrades bone. Bioessays. 1998;20:837–846. doi: 10.1002/(SICI)1521-1878(199810)20:10<837::AID-BIES9>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Blair H.C., Teitelbaum S.L., Ghiselli R., Gluck S. Osteoclastic bone resorption by a polarized vacuolar proton pump. Science. 1989;245:855–857. doi: 10.1126/science.2528207. [DOI] [PubMed] [Google Scholar]
- Blevins J.S., Elasri M.O., Allmendinger S.D., Beenken K.E., Skinner R.A., Thomas J.R., Smeltzer M.S. Role of sarA in the pathogenesis of Staphylococcus aureus musculoskeletal infection. Infect. Immun. 2003;71:516–523. doi: 10.1128/IAI.71.1.516-523.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blyth M.J., Kincaid R., Craigen M.A., Bennet G.C. The changing epidemiology of acute and subacute haematogenous osteomyelitis in children. J. Bone Joint Surg. Br. 2001;83:99–102. doi: 10.1302/0301-620x.83b1.10699. [DOI] [PubMed] [Google Scholar]
- Bocchini C.E., Hulten K.G., Mason E.O., Jr., Gonzalez B.E., Hammerman W.A., Kaplan S.L. Panton-Valentine leukocidin genes are associated with enhanced inflammatory response and local disease in acute hematogenous Staphylococcus aureus osteomyelitis in children. Pediatrics. 2006;117:433–440. doi: 10.1542/peds.2005-0566. [DOI] [PubMed] [Google Scholar]
- Bossard M.J., Tomaszek T.A., Thompson S.K., Amegadzie B.Y., Hanning C.R., Jones C., Kurdyla J.T., McNulty D.E., Drake F.H., Gowen M., Levy M.A. Proteolytic activity of human osteoclast cathepsin K. Expression, purification, activation, and substrate identification. J. Biol. Chem. 1996;271:12517–12524. doi: 10.1074/jbc.271.21.12517. [DOI] [PubMed] [Google Scholar]
- Bosse M.J., Gruber H.E., Ramp W.K. Internalization of bacteria by osteoblasts in a patient with recurrent, long-term osteomyelitis. A case report. J. Bone Joint Surg. Am. 2005;87:1343–1347. doi: 10.2106/JBJS.D.02649. [DOI] [PubMed] [Google Scholar]
- Bost K.L., Ramp W.K., Nicholson N.C., Bento J.L., Marriott I., Hudson M.C. Staphylococcus aureus infection of mouse or human osteoblasts induces high levels of interleukin-6 and interleukin-12 production. J. Infect. Dis. 1999;180:1912–1920. doi: 10.1086/315138. [DOI] [PubMed] [Google Scholar]
- Boulter E., Van Obberghen-Schilling E. Integrin-linked kinase and its partners: a modular platform regulating cell-matrix adhesion dynamics and cytoskeletal organization. Eur. J. Cell Biol. 2006;85:255–263. doi: 10.1016/j.ejcb.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Boyce B.F., Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch. Biochem. Biophys. 2008;473:139–146. doi: 10.1016/j.abb.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyden E.D., Dietrich W.F. Nalp1b controls mouse macrophage susceptibility to anthrax lethal toxin. Nat. Genet. 2006;38:240–244. doi: 10.1038/ng1724. [DOI] [PubMed] [Google Scholar]
- Bradley J.R. TNF-mediated inflammatory disease. J. Pathol. 2008;214:149–160. doi: 10.1002/path.2287. [DOI] [PubMed] [Google Scholar]
- Bremell T., Tarkowski A. Preferential induction of septic arthritis and mortality by superantigen-producing staphylococci. Infect. Immun. 1995;63:4185–4187. doi: 10.1128/iai.63.10.4185-4187.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremell T., Lange S., Yacoub A., Ryden C., Tarkowski A. Experimental Staphylococcus aureus arthritis in mice. Infect. Immun. 1991;59:2615–2623. doi: 10.1128/iai.59.8.2615-2623.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremell T., Abdelnour A., Tarkowski A. Histopathological and serological progression of experimental Staphylococcus aureus arthritis. Infect. Immun. 1992;60:2976–2985. doi: 10.1128/iai.60.7.2976-2985.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu R., Borysenko C.W., Li Y., Cao L., Sabokbar A., Blair H.C. Expression and function of TNF-family proteins and receptors in human osteoblasts. Bone. 2003;33:760–770. doi: 10.1016/j.bone.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Canalis E. Effects of tumor necrosis factor on bone formation in vitro. Endocrinology. 1987;121:1596–1604. doi: 10.1210/endo-121-5-1596. [DOI] [PubMed] [Google Scholar]
- Cassat J.E., Dunman P.M., McAleese F., Murphy E., Projan S.J., Smeltzer M.S. Comparative genomics of Staphylococcus aureus musculoskeletal isolates. J. Bacteriol. 2005;187:576–592. doi: 10.1128/JB.187.2.576-592.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centrella M., McCarthy T.L., Canalis E. Tumor necrosis factor-alpha inhibits collagen synthesis and alkaline phosphatase activity independently of its effect on deoxyribonucleic acid synthesis in osteoblast-enriched bone cell cultures. Endocrinology. 1988;123:1442–1448. doi: 10.1210/endo-123-3-1442. [DOI] [PubMed] [Google Scholar]
- Chiang C.Y., Kyritsis G., Graves D.T., Amar S. Interleukin-1 and tumor necrosis factor activities partially account for calvarial bone resorption induced by local injection of lipopolysaccharide. Infect. Immun. 1999;67:4231–4236. doi: 10.1128/iai.67.8.4231-4236.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciampolini J., Harding K.G. Pathophysiology of chronic bacterial osteomyelitis. Why do antibiotics fail so often? Postgrad. Med. J. 2000;76:479–483. doi: 10.1136/pmj.76.898.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins L.V., Kristian S.A., Weidenmaier C., Faigle M., van Kessel K.P., van Strijp J.A., Gotz F., Neumeister B., Peschel A. Staphylococcus aureus strains lacking D-alanine modifications of teichoic acids are highly susceptible to human neutrophil killing and are virulence attenuated in mice. J. Infect. Dis. 2002;186:214–219. doi: 10.1086/341454. [DOI] [PubMed] [Google Scholar]
- Colucci S., Brunetti G., Cantatore F.P., Oranger A., Mori G., Pignataro P., Tamma R., Grassi F.R., Zallone A., Grano M. The death receptor DR5 is involved in TRAIL-mediated human osteoclast apoptosis. Apoptosis. 2007;12:1623–1632. doi: 10.1007/s10495-007-0095-3. [DOI] [PubMed] [Google Scholar]
- Creagh E.M., O'Neill L.A. TLRs, NLRs and RLRs: a trinity of pathogen sensors that co-operate in innate immunity. Trends Immunol. 2006;27:352–357. doi: 10.1016/j.it.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Darouiche R.O., Landon G.C., Patti J.M., Nguyen L.L., Fernau R.C., McDevitt D., Greene C., Foster T., Klima M. Role of Staphylococcus aureus surface adhesins in orthopaedic device infections: are results model-dependent? J. Med. Microbiol. 1997;46:75–79. doi: 10.1099/00222615-46-1-75. [DOI] [PubMed] [Google Scholar]
- Deng G.M., Nilsson I.M., Verdrengh M., Collins L.V., Tarkowski A. Intra-articularly localized bacterial DNA containing CpG motifs induces arthritis. Nat. Med. 1999;5:702–705. doi: 10.1038/9554. [DOI] [PubMed] [Google Scholar]
- Dinarello C.A. Immunological and inflammatory functions of the interleukin-1 family. Annu. Rev. Immunol. 2009;27:519–550. doi: 10.1146/annurev.immunol.021908.132612. [DOI] [PubMed] [Google Scholar]
- Drake F.H., Dodds R.A., James I.E., Connor J.R., Debouck C., Richardson S., Lee-Rykaczewski E., Coleman L., Rieman D., Barthlow R., Hastings G., Gowen M. Cathepsin K, but not cathepsins B, L, or S, is abundantly expressed in human osteoclasts. J. Biol. Chem. 1996;271:12511–12516. doi: 10.1074/jbc.271.21.12511. [DOI] [PubMed] [Google Scholar]
- Dubost J.J., Soubrier M., De C.C., Ristori J.M., Bussiere J.L., Sauvezie B. No changes in the distribution of organisms responsible for septic arthritis over a 20 year period. Ann. Rheum. Dis. 2002;61:267–269. doi: 10.1136/ard.61.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziewanowska K., Patti J.M., Deobald C.F., Bayles K.W., Trumble W.R., Bohach G.A. Fibronectin binding protein and host cell tyrosine kinase are required for internalization of Staphylococcus aureus by epithelial cells. Infect. Immun. 1999;67:4673–4678. doi: 10.1128/iai.67.9.4673-4678.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ek-Rylander B., Bill P., Norgard M., Nilsson S., Andersson G. Cloning, sequence, and developmental expression of a type 5, tartrate-resistant, acid phosphatase of rat bone. J. Biol. Chem. 1991;266:24684–24689. [PubMed] [Google Scholar]
- Elasri M.O., Thomas J.R., Skinner R.A., Blevins J.S., Beenken K.E., Nelson C.L., Smeltzer M.S. Staphylococcus aureus collagen adhesin contributes to the pathogenesis of osteomyelitis. Bone. 2002;30:275–280. doi: 10.1016/s8756-3282(01)00632-9. [DOI] [PubMed] [Google Scholar]
- Ellington J.K., Reilly S.S., Ramp W.K., Smeltzer M.S., Kellam J.F., Hudson M.C. Mechanisms of Staphylococcus aureus invasion of cultured osteoblasts. Microb. Pathog. 1999;26:317–323. doi: 10.1006/mpat.1999.0272. [DOI] [PubMed] [Google Scholar]
- Evans C.A., Jellis J., Hughes S.P., Remick D.G., Friedland J.S. Tumor necrosis factor-alpha, interleukin-6, and interleukin-8 secretion and the acute-phase response in patients with bacterial and tuberculous osteomyelitis. J. Infect. Dis. 1998;177:1582–1587. doi: 10.1086/515313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everts V., Korper W., Hoeben K.A., Jansen I.D., Bromme D., Cleutjens K.B., Heeneman S., Peters C., Reinheckel T., Saftig P., Beertsen W. Osteoclastic bone degradation and the role of different cysteine proteinases and matrix metalloproteinases: differences between calvaria and long bone. J. Bone Miner. Res. 2006;21:1399–1408. doi: 10.1359/jbmr.060614. [DOI] [PubMed] [Google Scholar]
- Faustin B., Lartigue L., Bruey J.M., Luciano F., Sergienko E., Bailly-Maitre B., Volkmann N., Hanein D., Rouiller I., Reed J.C. Reconstituted NALP1 inflammasome reveals two-step mechanism of caspase-1 activation. Mol. Cell. 2007;25:713–724. doi: 10.1016/j.molcel.2007.01.032. [DOI] [PubMed] [Google Scholar]
- Feil E.J., Cooper J.E., Grundmann H., Robinson D.A., Enright M.C., Berendt T., Peacock S.J., Smith J.M., Murphy M., Spratt B.G., Moore C.E., Day N.P. How clonal is Staphylococcus aureus? J. Bacteriol. 2003;185:3307–3316. doi: 10.1128/JB.185.11.3307-3316.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler T., Wann E.R., Joh D., Johansson S., Foster T.J., Hook M. Cellular invasion by Staphylococcus aureus involves a fibronectin bridge between the bacterial fibronectin-binding MSCRAMMs and host cell beta1 integrins. Eur. J. Cell Biol. 2000;79:672–679. doi: 10.1078/0171-9335-00104. [DOI] [PubMed] [Google Scholar]
- Franchi L., Amer A., Body-Malapel M., Kanneganti T.D., Ozoren N., Jagirdar R., Inohara N., Vandenabeele P., Bertin J., Coyle A., Grant E.P., Nunez G. Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1[beta] in Salmonella-infected macrophages. Nat. Immunol. 2006;7:576–582. doi: 10.1038/ni1346. [DOI] [PubMed] [Google Scholar]
- Gallie W. First recurrence of osteomyelitis eighty years after infection. J. Bone Joint Surg. Br. 1951;33-B:110–111. doi: 10.1302/0301-620X.33B1.110. [DOI] [PubMed] [Google Scholar]
- Garcia-Alvarez F., Navarro-Zorraquino M., Castro A., Grasa J.M., Pastor C., Monzon M., Martinez A., Garcia-Alvarez I., Castillo J., Lozano R. Effect of age on cytokine response in an experimental model of osteomyelitis. Biogerontology. 2009;10:649–658. doi: 10.1007/s10522-008-9211-1. [DOI] [PubMed] [Google Scholar]
- Garzoni C., Kelley W.L. Staphylococcus aureus: new evidence for intracellular persistence. Trends Microbiol. 2009;17:59–65. doi: 10.1016/j.tim.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Gemmell C.G., Goutcher S.C., Reid R., Sturrock R.D. Role of certain virulence factors in a murine model of Staphylococcus aureus arthritis. J. Med. Microbiol. 1997;46:208–213. doi: 10.1099/00222615-46-3-208. [DOI] [PubMed] [Google Scholar]
- Gillaspy A.F., Hickmon S.G., Skinner R.A., Thomas J.R., Nelson C.L., Smeltzer M.S. Role of the accessory gene regulator (agr) in pathogenesis of staphylococcal osteomyelitis. Infect. Immun. 1995;63:3373–3380. doi: 10.1128/iai.63.9.3373-3380.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie W.J. Epidemiology in bone and joint infection. Infect. Dis. Clin. North Am. 1990;4:361–376. [PubMed] [Google Scholar]
- Goldenberg D.L. Septic arthritis. Lancet. 1998;351:197–202. doi: 10.1016/S0140-6736(97)09522-6. [DOI] [PubMed] [Google Scholar]
- Gomez M.I., Lee A., Reddy B., Muir A., Soong G., Pitt A., Cheung A., Prince A. Staphylococcus aureus protein A induces airway epithelial inflammatory responses by activating TNFR1. Nat. Med. 2004;10:842–848. doi: 10.1038/nm1079. [DOI] [PubMed] [Google Scholar]
- Grammatico L., Baron S., Rusch E., Lepage B., Surer N., Desenclos J.C., Besnier J.M. Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2008. Epidemiol. Infect. 2008;136:653–660. doi: 10.1017/S0950268807008850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer R.B., Rosenberg A.E. Case 6 – 1993 – A 69-year-old woman with a sclerotic lesion of the femur and pulmonary nodules. N. Engl. J. Med. 1993;328:422–428. doi: 10.1056/NEJM199302113280609. [DOI] [PubMed] [Google Scholar]
- Greig J.M., Wood M.J. Staphylococcus lugdunensis vertebral osteomyelitis. Clin. Microbiol. Infect. 2003;9:1139–1141. doi: 10.1046/j.1469-0691.2003.00777.x. [DOI] [PubMed] [Google Scholar]
- Guschin D., Rogers N., Briscoe J., Witthuhn B., Watling D., Horn F., Pellegrini S., Yasukawa K., Heinrich P., Stark G.R. A major role for the protein tyrosine kinase JAK1 in the JAK/STAT signal transduction pathway in response to interleukin-6. EMBO J. 1995;14:1421–1429. doi: 10.1002/j.1460-2075.1995.tb07128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattersley G., Dorey E., Horton M.A., Chambers T.J. Human macrophage colony-stimulating factor inhibits bone resorption by osteoclasts disaggregated from rat bone. J. Cell. Physiol. 1988;137:199–203. doi: 10.1002/jcp.1041370125. [DOI] [PubMed] [Google Scholar]
- Hauck C.R., Ohlsen K. Sticky connections: extracellular matrix protein recognition and integrin-mediated cellular invasion by Staphylococcus aureus. Curr. Opin. Microbiol. 2006;9:5–11. doi: 10.1016/j.mib.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Hayman A.R., Cox T.M. Purple acid phosphatase of the human macrophage and osteoclast. Characterization, molecular properties, and crystallization of the recombinant di-iron-oxo protein secreted by baculovirus-infected insect cells. J. Biol. Chem. 1994;269:1294–1300. [PubMed] [Google Scholar]
- Hayman A.R., Jones S.J., Boyde A., Foster D., Colledge W.H., Carlton M.B., Evans M.J., Cox T.M. Mice lacking tartrate-resistant acid phosphatase (Acp 5) have disrupted endochondral ossification and mild osteopetrosis. Development. 1996;122:3151–3162. doi: 10.1242/dev.122.10.3151. [DOI] [PubMed] [Google Scholar]
- Heinrich P.C., Bode J., Decker M., Graeve L., Martens A., Muller-Newen G., Pflanz S., Schaper F., Schmitz J. Termination and modulation of IL-6-type cytokine signaling. Adv. Exp. Med. Biol. 2001;495:153–160. doi: 10.1007/978-1-4615-0685-0_20. [DOI] [PubMed] [Google Scholar]
- Heinrich P.C., Behrmann I., Haan S., Hermanns H.M., Muller-Newen G., Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem. J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson B., Nair S.P. Hard labour: bacterial infection of the skeleton. Trends Microbiol. 2003;11:570–577. doi: 10.1016/j.tim.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Henriksen K., Neutzsky-Wulff A.V., Bonewald L.F., Karsdal M.A. Local communication on and within bone controls bone remodeling. Bone. 2009;44:1026–1033. doi: 10.1016/j.bone.2009.03.671. [DOI] [PubMed] [Google Scholar]
- Hikita A., Yana I., Wakeyama H., Nakamura M., Kadono Y., Oshima Y., Nakamura K., Seiki M., Tanaka S. Negative regulation of osteoclastogenesis by ectodomain shedding of receptor activator of NF-kappaB ligand. J. Biol. Chem. 2006;281:36846–36855. doi: 10.1074/jbc.M606656200. [DOI] [PubMed] [Google Scholar]
- Hudson M.C., Ramp W.K., Nicholson N.C., Williams A.S., Nousiainen M.T. Internalization of Staphylococcus aureus by cultured osteoblasts. Microb. Pathog. 1995;19:409–419. doi: 10.1006/mpat.1995.0075. [DOI] [PubMed] [Google Scholar]
- Ishimi Y., Miyaura C., Jin C.H., Akatsu T., Abe E., Nakamura Y., Yamaguchi A., Yoshiki S., Matsuda T., Hirano T. IL-6 is produced by osteoblasts and induces bone resorption. J. Immunol. 1990;145:3297–3303. [PubMed] [Google Scholar]
- Jevon M., Guo C., Ma B., Mordan N., Nair S.P., Harris M., Henderson B., Bentley G., Meghji S. Mechanisms of internalization of Staphylococcus aureus by cultured human osteoblasts. Infect. Immun. 1999;67:2677–2681. doi: 10.1128/iai.67.5.2677-2681.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson A., Flock J.I., Svensson O. Collagen and fibronectin binding in experimental staphylococcal osteomyelitis. Clin. Orthop. Relat. Res. 2001:241–246. doi: 10.1097/00003086-200101000-00032. [DOI] [PubMed] [Google Scholar]
- Jonsson I.M., Mazmanian S.K., Schneewind O., Verdrengh M., Bremell T., Tarkowski A. On the role of Staphylococcus aureus sortase and sortase-catalyzed surface protein anchoring in murine septic arthritis. J. Infect. Dis. 2002;185:1417–1424. doi: 10.1086/340503. [DOI] [PubMed] [Google Scholar]
- Jonsson I.M., vonEiff C., Proctor R.A., Peters G., Ryden C., Tarkowski A. Virulence of a hemB mutant displaying the phenotype of a Staphylococcus aureus small colony variant in a murine model of septic arthritis. Microb. Pathog. 2003;34:73–79. doi: 10.1016/s0882-4010(02)00208-5. [DOI] [PubMed] [Google Scholar]
- Jonsson I.M., Arvidson S., Foster S., Tarkowski A. Sigma factor B and RsbU are required for virulence in Staphylococcus aureus-induced arthritis and sepsis. Infect. Immun. 2004;72:6106–6111. doi: 10.1128/IAI.72.10.6106-6111.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonsson I.M., Lindholm C., Luong T.T., Lee C.Y., Tarkowski A. mgrA regulates staphylococcal virulence important for induction and progression of septic arthritis and sepsis. Microbes Infect. 2008;10:1229–1235. doi: 10.1016/j.micinf.2008.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josefsson E., Hartford O., O'Brien L., Patti J.M., Foster T. Protection against experimental Staphylococcus aureus arthritis by vaccination with clumping factor A, a novel virulence determinant. J. Infect. Dis. 2001;184:1572–1580. doi: 10.1086/324430. [DOI] [PubMed] [Google Scholar]
- Josefsson E., Juuti K., Bokarewa M., Kuusela P. The surface protein Pls of methicillin-resistant Staphylococcus aureus is a virulence factor in septic arthritis. Infect. Immun. 2005;73:2812–2817. doi: 10.1128/IAI.73.5.2812-2817.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlenberg J.M., Lundberg K.C., Kertesy S.B., Qu Y., Dubyak G.R. Potentiation of caspase-1 activation by the P2×7 receptor is dependent on TLR signals and requires NF-kappaB-driven protein synthesis. J. Immunol. 2005;175:7611–7622. doi: 10.4049/jimmunol.175.11.7611. [DOI] [PubMed] [Google Scholar]
- Kanazawa K., Azuma Y., Nakano H., Kudo A. TRAF5 functions in both RANKL- and TNF-induced osteoclastogenesis. J. Bone Miner. Res. 2003;18:443–450. doi: 10.1359/jbmr.2003.18.3.443. [DOI] [PubMed] [Google Scholar]
- Kanazawa K., Kudo A. TRAF2 is essential for TNF-alpha-induced osteoclastogenesis. J. Bone Miner. Res. 2005;20:840–847. doi: 10.1359/JBMR.041225. [DOI] [PubMed] [Google Scholar]
- Karwowska A., Davies H.D., Jadavji T. Epidemiology and outcome of osteomyelitis in the era of sequential intravenous-oral therapy. Pediatr. Infect. Dis. J. 1998;17:1021–1026. doi: 10.1097/00006454-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Khalil H., Williams R.J., Stenbeck G., Henderson B., Meghji S., Nair S.P. Invasion of bone cells by Staphylococcus epidermidis. Microbes Infect. 2007;9:460–465. doi: 10.1016/j.micinf.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Kim H.H., Lee D.E., Shin J.N., Lee Y.S., Jeon Y.M., Chung C.H., Ni J., Kwon B.S., Lee Z.H. Receptor activator of NF-kappaB recruits multiple TRAF family adaptors and activates c-Jun N-terminal kinase. FEBS Lett. 1999;443:297–302. doi: 10.1016/s0014-5793(98)01731-1. [DOI] [PubMed] [Google Scholar]
- Kintarak S., Whawell S.A., Speight P.M., Packer S., Nair S.P. Internalization of Staphylococcus aureus by human keratinocytes. Infect. Immun. 2004;72:5668–5675. doi: 10.1128/IAI.72.10.5668-5675.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirdis E., Jonsson I.M., Kubica M., Potempa J., Josefsson E., Masalha M., Foster S.J., Tarkowski A. Ribonucleotide reductase class III, an essential enzyme for the anaerobic growth of Staphylococcus aureus, is a virulence determinant in septic arthritis. Microb. Pathog. 2007;43:179–188. doi: 10.1016/j.micpath.2007.05.008. [DOI] [PubMed] [Google Scholar]
- Klosterhalfen B., Peters K.M., Tons C., Hauptmann S., Klein C.L., Kirkpatrick C.J. Local and systemic inflammatory mediator release in patients with acute and chronic posttraumatic osteomyelitis. J. Trauma. 1996;40:372–378. doi: 10.1097/00005373-199603000-00008. [DOI] [PubMed] [Google Scholar]
- Konig A., Muhlbauer R.C., Fleisch H. Tumor necrosis factor alpha and interleukin-1 stimulate bone resorption in vivo as measured by urinary [3H]tetracycline excretion from prelabeled mice. J. Bone Miner. Res. 1988;3:621–627. doi: 10.1002/jbmr.5650030607. [DOI] [PubMed] [Google Scholar]
- Kornak U., Kasper D., Bosl M.R., Kaiser E., Schweizer M., Schulz A., Friedrich W., Delling G., Jentsch T.J. Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001;104:205–215. doi: 10.1016/s0092-8674(01)00206-9. [DOI] [PubMed] [Google Scholar]
- Korovessis P., Fortis A.P., Spastris P., Droutsas P. Acute osteomyelitis of the patella 50 years after a knee fusion for septic arthritis. A case report. Clin. Orthop. Relat. Res. 1991:205–207. [PubMed] [Google Scholar]
- Kotake S., Sato K., Kim K.J., Takahashi N., Udagawa N., Nakamura I., Yamaguchi A., Kishimoto T., Suda T., Kashiwazaki S. Interleukin-6 and soluble interleukin-6 receptors in the synovial fluids from rheumatoid arthritis patients are responsible for osteoclast-like cell formation. J. Bone Miner. Res. 1996;11:88–95. doi: 10.1002/jbmr.5650110113. [DOI] [PubMed] [Google Scholar]
- Kwan T.S., Padrines M., Theoleyre S., Heymann D., Fortun Y. IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 2004;15:49–60. doi: 10.1016/j.cytogfr.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Lacey D.C., Simmons P.J., Graves S.E., Hamilton J.A. Proinflammatory cytokines inhibit osteogenic differentiation from stem cells: implications for bone repair during inflammation. Osteoarthritis Cartilage. 2008;17:735–742. doi: 10.1016/j.joca.2008.11.011. [DOI] [PubMed] [Google Scholar]
- Lang S., Livesley M.A., Lambert P.A., Elliott J., Elliott T.S. The genomic diversity of coagulase-negative staphylococci associated with nosocomial infections. J. Hosp. Infect. 1999;43:187–193. doi: 10.1053/jhin.1999.0245. [DOI] [PubMed] [Google Scholar]
- Lau Y.S., Wang W., Sabokbar A., Simpson H., Nair S., Henderson B., Berendt A., Athanasou N.A. Staphylococcus aureus capsular material promotes osteoclast formation. Injury. 2006;37(Suppl. 2):S41–S48. doi: 10.1016/j.injury.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Lazzarini L., Mader J.T., Calhoun J.H. Osteomyelitis in long bones. J. Bone Joint Surg. Am. 2004;86-A:2305–2318. doi: 10.2106/00004623-200410000-00028. [DOI] [PubMed] [Google Scholar]
- Lee K., Goodman S.B. Current state and future of joint replacements in the hip and knee. Expert Rev. Med. Devices. 2008;5:383–393. doi: 10.1586/17434440.5.3.383. [DOI] [PubMed] [Google Scholar]
- Levine M., Siegel L.B. A swollen joint: why all the fuss? Am. J. Ther. 2003;10:219–224. doi: 10.1097/00045391-200305000-00009. [DOI] [PubMed] [Google Scholar]
- Lew D.P., Waldvogel F.A. Osteomyelitis. N. Engl. J. Med. 1997;336:999–1007. doi: 10.1056/NEJM199704033361406. [DOI] [PubMed] [Google Scholar]
- Lew D.P., Waldvogel F.A. Osteomyelitis. Lancet. 2004;364:369–379. doi: 10.1016/S0140-6736(04)16727-5. [DOI] [PubMed] [Google Scholar]
- Li W., Liang X., Kellendonk C., Poli V., Taub R. STAT3 contributes to the mitogenic response of hepatocytes during liver regeneration. J. Biol. Chem. 2002;277:28411–28417. doi: 10.1074/jbc.M202807200. [DOI] [PubMed] [Google Scholar]
- Li Y.P., Stashenko P. Proinflammatory cytokines tumor necrosis factor-alpha and IL-6, but not IL-1, down-regulate the osteocalcin gene promoter. J. Immunol. 1992;148:788–794. [PubMed] [Google Scholar]
- Lindsay J.A., Moore C.E., Day N.P., Peacock S.J., Witney A.A., Stabler R.A., Husain S.E., Butcher P.D., Hinds J. Microarrays reveal that each of the ten dominant lineages of Staphylococcus aureus has a unique combination of surface-associated and regulatory genes. J. Bacteriol. 2006;188:669–676. doi: 10.1128/JB.188.2.669-676.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z.Q., Deng G.M., Foster S., Tarkowski A. Staphylococcal peptidoglycans induce arthritis. Arthritis Res. 2001;3:375–380. doi: 10.1186/ar330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljusberg J., Wang Y., Lang P., Norgard M., Dodds R., Hultenby K., Ek-Rylander B., Andersson G. Proteolytic excision of a repressive loop domain in tartrate-resistant acid phosphatase by cathepsin K in osteoclasts. J. Biol. Chem. 2005;280:28370–28381. doi: 10.1074/jbc.M502469200. [DOI] [PubMed] [Google Scholar]
- Lomaga M.A., Yeh W.C., Sarosi I., Duncan G.S., Furlonger C., Ho A., Morony S., Capparelli C., Van G., Kaufman S., van der H.A., Itie A., Wakeham A., Khoo W., Sasaki T., Cao Z., Penninger J.M., Paige C.J., Lacey D.L., Dunstan C.R., Boyle W.J., Goeddel D.V., Mak T.W. TRAF6 deficiency results in osteopetrosis and defective interleukin-1, CD40, and LPS signaling. Genes Dev. 1999;13:1015–1024. doi: 10.1101/gad.13.8.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch C.C., Hikosaka A., Acuff H.B., Martin M.D., Kawai N., Singh R.K., Vargo-Gogola T.C., Begtrup J.L., Peterson T.E., Fingleton B., Shirai T., Matrisian L.M., Futakuchi M. MMP-7 promotes prostate cancer-induced osteolysis via the solubilization of RANKL. Cancer Cell. 2005;7:485–496. doi: 10.1016/j.ccr.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Mackie E.J. Osteoblasts: novel roles in orchestration of skeletal architecture. Int. J. Biochem. Cell Biol. 2003;35:1301–1305. doi: 10.1016/s1357-2725(03)00107-9. [DOI] [PubMed] [Google Scholar]
- Mahalingam D., Szegezdi E., Keane M., Jong S., Samali A. TRAIL receptor signalling and modulation: Are we on the right TRAIL? Cancer Treat. Rev. 2009;35:280–288. doi: 10.1016/j.ctrv.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Mariathasan S., Weiss D.S., Newton K., McBride J., O'Rourke K., Roose-Girma M., Lee W.P., Weinrauch Y., Monack D.M., Dixit V.M. Cryopyrin activates the inflammasome in response to toxins and ATP. Nature. 2006;440:228–232. doi: 10.1038/nature04515. [DOI] [PubMed] [Google Scholar]
- Marriott I., Hughes F.M., Jr., Bost K.L. Bacterial infection of osteoblasts induces interleukin-1beta and interleukin-18 transcription but not protein synthesis. J. Interferon Cytokine Res. 2002;22:1049–1055. doi: 10.1089/107999002760624288. [DOI] [PubMed] [Google Scholar]
- Matsuo K., Irie N. Osteoclast–osteoblast communication. Arch. Biochem. Biophys. 2008;473:201–209. doi: 10.1016/j.abb.2008.03.027. [DOI] [PubMed] [Google Scholar]
- McCall S.H., Sahraei M., Young A.B., Worley C.S., Duncan J.A., Ting J.P., Marriott I. Osteoblasts express NLRP3, a nucleotide-binding domain and leucine-rich repeat region containing receptor implicated in bacterially induced cell death. J. Bone Miner. Res. 2008;23:30–40. doi: 10.1359/JBMR.071002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meghji S., Crean S.J., Nair S., Wilson M., Poole S., Harris M., Henderson B. Staphylococcus epidermidis produces a cell-associated proteinaceous fraction which causes bone resorption by a prostanoid-independent mechanism: relevance to the treatment of infected orthopaedic implants. Br. J. Rheumatol. 1997;36:957–963. doi: 10.1093/rheumatology/36.9.957. [DOI] [PubMed] [Google Scholar]
- Meghji S., Crean S.J., Hill P.A., Sheikh M., Nair S.P., Heron K., Henderson B., Mawer E.B., Harris M. Surface-associated protein from Staphylococcus aureus stimulates osteoclastogenesis: possible role in S. aureus-induced bone pathology. Br. J. Rheumatol. 1998;37:1095–1101. doi: 10.1093/rheumatology/37.10.1095. [DOI] [PubMed] [Google Scholar]
- Miao E.A., Puche-Aranda C.M., Dors M., Clark A.E., Bader M.W., Miller S.I., Aderem A. Cytoplasmic flagellin activates caspase-1 and secretion of interleukin 1[beta] via Ipaf. Nat. Immunol. 2006;7:569–575. doi: 10.1038/ni1344. [DOI] [PubMed] [Google Scholar]
- Mitchell G., Lamontagne C.A., Brouillette E., Grondin G., Talbot B.G., Grandbois M., Malouin F. Staphylococcus aureus SigB activity promotes a strong fibronectin-bacterium interaction which may sustain host tissue colonization by small-colony variants isolated from cystic fibrosis patients. Mol. Microbiol. 2008;70:1540–1555. doi: 10.1111/j.1365-2958.2008.06511.x. [DOI] [PubMed] [Google Scholar]
- Moisan H., Brouillette E., Jacob C.L., Langlois-Begin P., Michaud S., Malouin F. Transcription of virulence factors in Staphylococcus aureus small-colony variants isolated from cystic fibrosis patients is influenced by SigB. J. Bacteriol. 2006;188:64–76. doi: 10.1128/JB.188.1.64-76.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy G.R. Inflammatory mediators and the destruction of bone. J. Periodontal Res. 1991;26:213–217. doi: 10.1111/j.1600-0765.1991.tb01647.x. [DOI] [PubMed] [Google Scholar]
- Murdoch D.R., Everts R.J., Chambers S.T., Cowan I.A. Vertebral osteomyelitis due to Staphylococcus lugdunensis. J. Clin. Microbiol. 1996;34:993–994. doi: 10.1128/jcm.34.4.993-994.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musher D.M., Baughn R.E., Templeton G.B., Minuth J.N. Emergence of variant forms of Staphylococcus aureus after exposure to gentamicin and infectivity of the variants in experimental animals. J. Infect. Dis. 1977;136:360–369. doi: 10.1093/infdis/136.3.360. [DOI] [PubMed] [Google Scholar]
- Nade S. Septic arthritis. Best. Pract. Res. Clin. Rheumatol. 2003;17:183–200. doi: 10.1016/s1521-6942(02)00106-7. [DOI] [PubMed] [Google Scholar]
- Nair S., Song Y., Meghji S., Reddi K., Harris M., Ross A., Poole S., Wilson M., Henderson B. Surface-associated proteins from Staphylococcus aureus demonstrate potent bone resorbing activity. J. Bone Miner. Res. 1995;10:726–734. doi: 10.1002/jbmr.5650100509. [DOI] [PubMed] [Google Scholar]
- Nair S.P., Meghji S., Wilson M., Nugent I., Ross A., Ismael A., Bhudia N.K., Harris M., Henderson B. Clinical isolates of Staphylococcus aureus have osteolytic surface proteins and a proportion of the population have antibodies that block this activity: is this of prognostic significance? Br. J. Rheumatol. 1997;36:328–332. doi: 10.1093/rheumatology/36.3.328. [DOI] [PubMed] [Google Scholar]
- Nair S.P., Bischoff M., Senn M.M., Berger-Bachi B. The sigma B regulon influences internalization of Staphylococcus aureus by osteoblasts. Infect. Immun. 2003;71:4167–4170. doi: 10.1128/IAI.71.7.4167-4170.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanes M.S. Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene. 2003;321:1–15. doi: 10.1016/s0378-1119(03)00841-2. [DOI] [PubMed] [Google Scholar]
- Nanes M.S., McKoy W.M., Marx S.J. Inhibitory effects of tumor necrosis factor-alpha and interferon-gamma on deoxyribonucleic acid and collagen synthesis by rat osteosarcoma cells (ROS 17/2.8) Endocrinology. 1989;124:339–345. doi: 10.1210/endo-124-1-339. [DOI] [PubMed] [Google Scholar]
- Nanes M.S., Rubin J., Titus L., Hendy G.N., Catherwood B. Tumor necrosis factor-alpha inhibits 1,25-dihydroxyvitamin D3-stimulated bone Gla protein synthesis in rat osteosarcoma cells (ROS 17/2.8) by a pretranslational mechanism. Endocrinology. 1991;128:2577–2582. doi: 10.1210/endo-128-5-2577. [DOI] [PubMed] [Google Scholar]
- Naugler W.E., Karin M. The wolf in sheep's clothing: the role of interleukin-6 in immunity, inflammation and cancer. Trends Mol. Med. 2008;14:109–119. doi: 10.1016/j.molmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Nesbitt S.A., Horton M.A. Trafficking of matrix collagens through bone-resorbing osteoclasts. Science. 1997;276:266–269. doi: 10.1126/science.276.5310.266. [DOI] [PubMed] [Google Scholar]
- Nilsson I.M., Lee J.C., Bremell T., Ryden C., Tarkowski A. The role of staphylococcal polysaccharide microcapsule expression in septicemia and septic arthritis. Infect. Immun. 1997;65:4216–4221. doi: 10.1128/iai.65.10.4216-4221.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson I.M., Patti J.M., Bremell T., Hook M., Tarkowski A. Vaccination with a recombinant fragment of collagen adhesin provides protection against Staphylococcus aureus-mediated septic death. J. Clin. Invest. 1998;101:2640–2649. doi: 10.1172/JCI1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson I.M., Hartford O., Foster T., Tarkowski A. Alpha-toxin and gamma-toxin jointly promote Staphylococcus aureus virulence in murine septic arthritis. Infect. Immun. 1999;67:1045–1049. doi: 10.1128/iai.67.3.1045-1049.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osiri M., Ruxrungtham K., Nookhai S., Ohmoto Y., Deesomchok U. IL-1beta, IL-6 and TNF-alpha in synovial fluid of patients with non-gonococcal septic arthritis. Asian Pac. J. Allergy Immunol. 1998;16:155–160. [PubMed] [Google Scholar]
- Palmqvist N., Foster T., Tarkowski A., Josefsson E. Protein A is a virulence factor in Staphylococcus aureus arthritis and septic death. Microb. Pathog. 2002;33:239–249. doi: 10.1006/mpat.2002.0533. [DOI] [PubMed] [Google Scholar]
- Palmqvist N., Patti J.M., Tarkowski A., Josefsson E. Expression of staphylococcal clumping factor A impedes macrophage phagocytosis. Microbes Infect. 2004;6:188–195. doi: 10.1016/j.micinf.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Palmqvist N., Foster T., Fitzgerald J.R., Josefsson E., Tarkowski A. Fibronectin-binding proteins and fibrinogen-binding clumping factors play distinct roles in staphylococcal arthritis and systemic inflammation. J. Infect. Dis. 2005;191:791–798. doi: 10.1086/427663. [DOI] [PubMed] [Google Scholar]
- Patti J.M., Bremell T., Krajewska-Pietrasik D., Abdelnour A., Tarkowski A., Ryden C., Hook M. The Staphylococcus aureus collagen adhesin is a virulence determinant in experimental septic arthritis. Infect. Immun. 1994;62:152–161. doi: 10.1128/iai.62.1.152-161.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock S.J., Day N.P., Thomas M.G., Berendt A.R., Foster T.J. Clinical isolates of Staphylococcus aureus exhibit diversity in fnb genes and adhesion to human fibronectin. J. Infect. 2000;41:23–31. doi: 10.1053/jinf.2000.0657. [DOI] [PubMed] [Google Scholar]
- Peacock S.J., Moore C.E., Justice A., Kantzanou M., Story L., Mackie K., O'Neill G., Day N.P. Virulent combinations of adhesin and toxin genes in natural populations of Staphylococcus aureus. Infect. Immun. 2002;70:4987–4996. doi: 10.1128/IAI.70.9.4987-4996.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peschel A., Jack R.W., Otto M., Collins L.V., Staubitz P., Nicholson G., Kalbacher H., Nieuwenhuizen W.F., Jung G., Tarkowski A., van Kessel K.P., van Strijp J.A. Staphylococcus aureus resistance to human defensins and evasion of neutrophil killing via the novel virulence factor MprF is based on modification of membrane lipids with L-lysine. J. Exp. Med. 2001;193:1067–1076. doi: 10.1084/jem.193.9.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeilschifter J., Chenu C., Bird A., Mundy G.R., Roodman G.D. Interleukin-1 and tumor necrosis factor stimulate the formation of human osteoclast-like cells in vitro. J. Bone Miner. Res. 1989;4:113–118. doi: 10.1002/jbmr.5650040116. [DOI] [PubMed] [Google Scholar]
- Pivirotto L.A., Cissel D.S., Keeting P.E. Sex hormones mediate interleukin-1 beta production by human osteoblastic HOBIT cells. Mol. Cell. Endocrinol. 1995;111:67–74. doi: 10.1016/0303-7207(95)03549-m. [DOI] [PubMed] [Google Scholar]
- Proctor R.A., van L.P., Kristjansson M., Maslow J.N., Arbeit R.D. Persistent and relapsing infections associated with small-colony variants of Staphylococcus aureus. Clin. Infect. Dis. 1995;20:95–102. doi: 10.1093/clinids/20.1.95. [DOI] [PubMed] [Google Scholar]
- Proctor R.A., von Eiff C., Kahl B.C., Becker K., McNamara P., Herrmann M., Peters G. Small colony variants: a pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat. Rev. Microbiol. 2006;4:295–305. doi: 10.1038/nrmicro1384. [DOI] [PubMed] [Google Scholar]
- Reilly S.S., Hudson M.C., Kellam J.F., Ramp W.K. In vivo internalization of Staphylococcus aureus by embryonic chick osteoblasts. Bone. 2000;26:63–70. doi: 10.1016/s8756-3282(99)00239-2. [DOI] [PubMed] [Google Scholar]
- Reott M.A., Jr., Ritchie-Miller S.L., Anguita J., Hudson M.C. TRAIL expression is induced in both osteoblasts containing intracellular Staphylococcus aureus and uninfected osteoblasts in infected cultures. FEMS Microbiol. Lett. 2008;278:185–192. doi: 10.1111/j.1574-6968.2007.00988.x. [DOI] [PubMed] [Google Scholar]
- Robinson L.J., Borysenko C.W., Blair H.C. Tumor necrosis factor family receptors regulating bone turnover: new observations in osteoblastic and osteoclastic cell lines. Ann. NY Acad. Sci. 2007;1116:432–443. doi: 10.1196/annals.1402.025. [DOI] [PubMed] [Google Scholar]
- Rodig S.J., Meraz M.A., White J.M., Lampe P.A., Riley J.K., Arthur C.D., King K.L., Sheehan K.C., Yin L., Pennica D., Johnson E.M., Jr., Schreiber R.D. Disruption of the Jak1 gene demonstrates obligatory and nonredundant roles of the Jaks in cytokine-induced biologic responses. Cell. 1998;93:373–383. doi: 10.1016/s0092-8674(00)81166-6. [DOI] [PubMed] [Google Scholar]
- Ryan M.J., Kavanagh R., Wall P.G., Hazleman B.L. Bacterial joint infections in England and Wales: analysis of bacterial isolates over a four year period. Br. J. Rheumatol. 1997;36:370–373. doi: 10.1093/rheumatology/36.3.370. [DOI] [PubMed] [Google Scholar]
- Saez-Llorens X., Mustafa M.M., Ramilo O., Fink C., Beutler B., Nelson J.D. Tumor necrosis factor alpha and interleukin 1 beta in synovial fluid of infants and children with suppurative arthritis. Am. J. Dis. Child. 1990;144:353–356. doi: 10.1001/archpedi.1990.02150270103035. [DOI] [PubMed] [Google Scholar]
- Salo J., Lehenkari P., Mulari M., Metsikko K., Vaananen H.K. Removal of osteoclast bone resorption products by transcytosis. Science. 1997;276:270–273. doi: 10.1126/science.276.5310.270. [DOI] [PubMed] [Google Scholar]
- Sdougkos G., Chini V., Papanastasiou D.A., Christodoulou G., Tagaris G., Dimitracopoulos G., Spiliopoulou I. Methicillin-resistant Staphylococcus aureus producing Panton–Valentine leukocidin as a cause of acute osteomyelitis in children. Clin. Microbiol. Infect. 2007;13:651–654. doi: 10.1111/j.1469-0691.2007.01713.x. [DOI] [PubMed] [Google Scholar]
- Seifert H., Oltmanns D., Becker K., Wisplinghoff H., von E.C. Staphylococcus lugdunensis pacemaker-related infection. Emerg. Infect. Dis. 2005;11:1283–1286. doi: 10.3201/eid1108.041177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sendi P., Proctor R.A. Staphylococcus aureus as an intracellular pathogen: the role of small colony variants. Trends Microbiol. 2009;17:54–58. doi: 10.1016/j.tim.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Sendi P., Rohrbach M., Graber P., Frei R., Ochsner P.E., Zimmerli W. Staphylococcus aureus small colony variants in prosthetic joint infection. Clin. Infect. Dis. 2006;43:961–967. doi: 10.1086/507633. [DOI] [PubMed] [Google Scholar]
- Shaw L.N., Lindholm C., Prajsnar T.K., Miller H.K., Brown M.C., Golonka E., Stewart G.C., Tarkowski A., Potempa J. Identification and characterization of sigma, a novel component of the Staphylococcus aureus stress and virulence responses. PLoS One. 2008;3:e3844. doi: 10.1371/journal.pone.0003844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtliff M.E., Mader J.T. Acute septic arthritis. Clin. Microbiol. Rev. 2002;15:527–544. doi: 10.1128/CMR.15.4.527-544.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha B., Francois P.P., Nusse O., Foti M., Hartford O.M., Vaudaux P., Foster T.J., Lew D.P., Herrmann M., Krause K.H. Fibronectin-binding protein acts as Staphylococcus aureus invasin via fibronectin bridging to integrin alpha5beta1. Cell. Microbiol. 1999;1:101–117. doi: 10.1046/j.1462-5822.1999.00011.x. [DOI] [PubMed] [Google Scholar]
- Smith D.D., Gowen M., Mundy G.R. Effects of interferon-gamma and other cytokines on collagen synthesis in fetal rat bone cultures. Endocrinology. 1987;120:2494–2499. doi: 10.1210/endo-120-6-2494. [DOI] [PubMed] [Google Scholar]
- Stapleton M.R., Horsburgh M.J., Hayhurst E.J., Wright L., Jonsson I.M., Tarkowski A., Kokai-Kun J.F., Mond J.J., Foster S.J. Characterization of IsaA and SceD, two putative lytic transglycosylases of Staphylococcus aureus. J. Bacteriol. 2007;189:7316–7325. doi: 10.1128/JB.00734-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoodley P., Nistico L., Johnson S., Lasko L.A., Baratz M., Gahlot V., Ehrlich G.D., Kathju S. Direct demonstration of viable Staphylococcus aureus biofilms in an infected total joint arthroplasty. A case report. J. Bone Joint Surg. Am. 2008;90:1751–1758. doi: 10.2106/JBJS.G.00838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott N.S. Paediatric bone and joint infection. J. Orthop. Surg. (Hong Kong) 2001;9:83–90. doi: 10.1177/230949900100900116. [DOI] [PubMed] [Google Scholar]
- Takeuchi O., Hoshino K., Kawai T., Sanjo H., Takada H., Ogawa T., Takeda K., Akira S. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999;11:443–451. doi: 10.1016/s1074-7613(00)80119-3. [DOI] [PubMed] [Google Scholar]
- Takeuchi O., Hoshino K., Akira S. Cutting edge: TLR2-deficient and MyD88-deficient mice are highly susceptible to Staphylococcus aureus infection. J. Immunol. 2000;165:5392–5396. doi: 10.4049/jimmunol.165.10.5392. [DOI] [PubMed] [Google Scholar]
- Tarkowski A., Collins L.V., Gjertsson I., Hultgren O.H., Jonsson I.M., Sakiniene E., Verdrengh M. Model systems: modeling human staphylococcal arthritis and sepsis in the mouse. Trends Microbiol. 2001;9:321–326. doi: 10.1016/s0966-842x(01)02078-9. [DOI] [PubMed] [Google Scholar]
- Taubman M.A., Kawai T. Involvement of T-lymphocytes in periodontal disease and in direct and indirect induction of bone resorption. Crit. Rev. Oral Biol. Med. 2001;12:125–135. doi: 10.1177/10454411010120020301. [DOI] [PubMed] [Google Scholar]
- Thomson B.M., Mundy G.R., Chambers T.J. Tumor necrosis factors alpha and beta induce osteoblastic cells to stimulate osteoclastic bone resorption. J. Immunol. 1987;138:775–779. [PubMed] [Google Scholar]
- Ting J.P.Y., Willingham S.B., Bergstralh D.T. NLRs at the intersection of cell death and immunity. Nat. Rev. Immunol. 2008;8:372–379. doi: 10.1038/nri2296. [DOI] [PubMed] [Google Scholar]
- Tokukoda Y., Takata S., Kaji H., Kitazawa R., Sugimoto T., Chihara K. Interleukin-1beta stimulates transendothelial mobilization of human peripheral blood mononuclear cells with a potential to differentiate into osteoclasts in the presence of osteoblasts. Endocr. J. 2001;48:443–452. doi: 10.1507/endocrj.48.443. [DOI] [PubMed] [Google Scholar]
- Tsezou A., Poultsides L., Kostopoulou F., Zintzaras E., Satra M., Kitsiou-Tzeli S., Malizos K.N. Influence of interleukin 1alpha (IL-1alpha), IL-4, and IL-6 polymorphisms on genetic susceptibility to chronic osteomyelitis. Clin. Vaccine Immunol. 2008;15:1888–1890. doi: 10.1128/CVI.00209-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K.A., Reilly S.S., Leslie C.S., Hudson M.C. Intracellular Staphylococcus aureus induces apoptosis in mouse osteoblasts. FEMS Microbiol. Lett. 2000;186:151–156. doi: 10.1111/j.1574-6968.2000.tb09096.x. [DOI] [PubMed] [Google Scholar]
- U.K. Health Protection Agency, 2008. Surgical Site Infection – National aggregated data on Surgical Site Infections for hospitals that have participated in Surgical Site Infection Surveillance Scheme (SSISS) between October 1997 and December 2005. 〈http://www.hpa.org.uk/HPA/Topics/InfectiousDiseases/InfectionsAZ/1202115536296/〉.
- Udagawa N., Takahashi N., Katagiri T., Tamura T., Wada S., Findlay D.M., Martin T.J., Hirota H., Taga T., Kishimoto T., Suda T. Interleukin (IL)-6 induction of osteoclast differentiation depends on IL-6 receptors expressed on osteoblastic cells but not on osteoclast progenitors. J. Exp. Med. 1995;182:1461–1468. doi: 10.1084/jem.182.5.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaananen H.K., Laitala-Leinonen T. Osteoclast lineage and function. Arch. Biochem. Biophys. 2008;473:132–138. doi: 10.1016/j.abb.2008.03.037. [DOI] [PubMed] [Google Scholar]
- Vallianou N., Evangelopoulos A., Makri P., Zacharias G., Stefanitsi P., Karachalios A., Avgerinos P.C. Vertebral osteomyelitis and native valve endocarditis due to Staphylococcus simulans: a case report. J. Med. Case Reports. 2008;2:183. doi: 10.1186/1752-1947-2-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Lest C.H., Vaandrager A.B. Mechanism of cell-mediated mineralization. Curr. Opin. Orthop. 2007;18:434–443. [Google Scholar]
- Vaudaux P., Francois P., Bisognano C., Kelley W.L., Lew D.P., Schrenzel J., Proctor R.A., McNamara P.J., Peters G., von Eiff C. Increased expression of clumping factor and fibronectin-binding proteins by hemB mutants of Staphylococcus aureus expressing small colony variant phenotypes. Infect. Immun. 2002;70:5428–5437. doi: 10.1128/IAI.70.10.5428-5437.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verstrepen L., Bekaert T., Chau T.L., Tavernier J., Chariot A., Beyaert R. TLR-4, IL-1R and TNF-R signaling to NF-kappaB: variations on a common theme. Cell. Mol. Life Sci. 2008;65:2964–2978. doi: 10.1007/s00018-008-8064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Eiff C. Staphylococcus aureus small colony variants: a challenge to microbiologists and clinicians. Int. J. Antimicrob. Agents. 2008;31:507–510. doi: 10.1016/j.ijantimicag.2007.10.026. [DOI] [PubMed] [Google Scholar]
- von Eiff C., Bettin D., Proctor R.A., Rolauffs B., Lindner N., Winkelmann W., Peters G. Recovery of small colony variants of Staphylococcus aureus following gentamicin bead placement for osteomyelitis. Clin. Infect. Dis. 1997;25:1250–1251. doi: 10.1086/516962. [DOI] [PubMed] [Google Scholar]
- von Eiff C., Heilmann C., Proctor R.A., Woltz C., Peters G., Gotz F. A site-directed Staphylococcus aureus hemB mutant is a small-colony variant which persists intracellularly. J. Bacteriol. 1997;179:4706–4712. doi: 10.1128/jb.179.15.4706-4712.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Eiff C., Vaudaux P., Kahl B.C., Lew D., Emler S., Schmidt A., Peters G., Proctor R.A. Bloodstream infections caused by small-colony variants of coagulase-negative staphylococci following pacemaker implantation. Clin. Infect. Dis. 1999;29:932–934. doi: 10.1086/520462. [DOI] [PubMed] [Google Scholar]
- von Eiff C., Becker K., Metze D., Lubritz G., Hockmann J., Schwarz T., Peters G. Intracellular persistence of Staphylococcus aureus small-colony variants within keratinocytes: a cause for antibiotic treatment failure in a patient with Darier's disease. Clin. Infect. Dis. 2001;32:1643–1647. doi: 10.1086/320519. [DOI] [PubMed] [Google Scholar]
- von Eiff C., Peters G., Becker K. The small colony variant (SCV) concept – the role of staphylococcal SCVs in persistent infections. Injury. 2006;37(Suppl. 2):S26–S33. doi: 10.1016/j.injury.2006.04.006. [DOI] [PubMed] [Google Scholar]
- Wada T., Nakashima T., Hiroshi N., Penninger J.M. RANKL-RANK signaling in osteoclastogenesis and bone disease. Trends Mol. Med. 2006;12:17–25. doi: 10.1016/j.molmed.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Wajant H., Pfizenmaier K., Scheurich P. Tumor necrosis factor signaling. Cell Death Differ. 2003;10:45–65. doi: 10.1038/sj.cdd.4401189. [DOI] [PubMed] [Google Scholar]
- Wang B., Yurecko R.S., Dedhar S., Cleary P.P. Integrin-linked kinase is an essential link between integrins and uptake of bacterial pathogens by epithelial cells. Cell. Microbiol. 2006;8:257–266. doi: 10.1111/j.1462-5822.2005.00618.x. [DOI] [PubMed] [Google Scholar]
- Weichert S., Sharland M., Clarke N.M., Faust S.N. Acute haematogenous osteomyelitis in children: is there any evidence for how long we should treat? Curr. Opin. Infect. Dis. 2008;21:258–262. doi: 10.1097/QCO.0b013e3283005441. [DOI] [PubMed] [Google Scholar]
- Xing L., Carlson L., Story B., Tai Z., Keng P., Siebenlist U., Boyce B.F. Expression of either NF-kappaB p50 or p52 in osteoclast precursors is required for IL-1-induced bone resorption. J. Bone Miner. Res. 2003;18:260–269. doi: 10.1359/jbmr.2003.18.2.260. [DOI] [PubMed] [Google Scholar]
- Xu Y., Rivas J.M., Brown E.L., Liang X., Hook M. Virulence potential of the staphylococcal adhesin CNA in experimental arthritis is determined by its affinity for collagen. J. Infect. Dis. 2004;189:2323–2333. doi: 10.1086/420851. [DOI] [PubMed] [Google Scholar]
- Yasuda H., Shima N., Nakagawa N., Yamaguchi K., Kinosaki M., Mochizuki S., Tomoyasu A., Yano K., Goto M., Murakami A., Tsuda E., Morinaga T., Higashio K., Udagawa N., Takahashi N., Suda T. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. USA. 1998;95:3597–3602. doi: 10.1073/pnas.95.7.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshii T., Magara S., Miyai D., Nishimura H., Kuroki E., Furudoi S., Komori T., Ohbayashi C. Local levels of interleukin-1beta, −4, -6 and tumor necrosis factor alpha in an experimental model of murine osteomyelitis due to Staphylococcus aureus. Cytokine. 2002;19:59–65. doi: 10.1006/cyto.2002.1039. [DOI] [PubMed] [Google Scholar]
- Zauli G., Rimondi E., Nicolin V., Melloni E., Celeghini C., Secchiero P. TNF-related apoptosis-inducing ligand (TRAIL) blocks osteoclastic differentiation induced by RANKL plus M-CSF. Blood. 2004;104:2044–2050. doi: 10.1182/blood-2004-03-1196. [DOI] [PubMed] [Google Scholar]
- Zou W., Hakim I., Tschoep K., Endres S., Bar-Shavit Z. Tumor necrosis factor-alpha mediates RANK ligand stimulation of osteoclast differentiation by an autocrine mechanism. J. Cell. Biochem. 2001;83:70–83. doi: 10.1002/jcb.1202. [DOI] [PubMed] [Google Scholar]