Abstract
Outcomes in depression treatment research include both changes in symptom severity and functional impairment. Symptom measures tend to be the standard outcome but we argue that there are benefits to considering functional outcomes. An exhaustive literature review shows that the relationship between symptoms and functioning remains unexpectedly weak and often bidirectional. Changes in functioning often lag symptom changes. As a result, functional outcomes might offer depression researchers more critical feedback and better guidance when studying depression treatment outcomes. The paper presents a case for the necessity of both functional and symptom outcomes in depression treatment research by addressing three aims–1) review the research relating symptoms and functioning, 2) provide a rationale for measuring both outcomes, and 3) discuss potential artifacts in measuring functional outcomes. The three aims are supported by an empirical review of the treatment outcome and epidemiological literatures.
Keywords: Depression, Social functioning, Occupational functioning, Physical functioning, Outcome measurement
1. Introduction
Mental disorders create societal problems because they produce functional impairment. These impairments may either cause or be caused by the disorder (see Barnett & Gotlib, 1988); regardless of the causal properties, there must be a link between impairment and disorder for researchers, policy-makers, and health care professionals to pay attention1. If functional impairment potentially drives our attention then functional impairment ought to be a prominent outcome for evaluating treatments. A cursory review of psychological and psychiatric treatment outcome literature suggests otherwise. A systematic search of over 90 depression treatment outcome meta-analyses indicates that less than 5% of the clinical trials measure and report functional outcomes. That cursory review corroborates a systematic review of more than 150 published depression clinical trials where an even lower proportion reported any functional outcomes. The most prominent outcomes consist of symptoms, symptom profiles, or diagnostic endpoints. Measuring symptom outcomes makes sense; symptoms are the most proximal indicators of a disorder. Unfortunately, these indicators only take us so far. We can examine whether people with disorders possess different symptom scores or profiles before and after treatment. What remains unanswered is whether these measures provide us with an understanding of functional change – that is, whether people are more functionally capable after treatment.
Symptom measures somewhat reflect functional impairment but lack domain-specific functional information. As a result, depression researchers acknowledge the need for multidimensional outcomes when trying to capture treatment effectiveness (Booth et al., 1997) or routine clinical outcomes (Möller, Demyttenaere, Sacchetti, Rush, & Montgomery, 2003). The same logic has been argued for the definition of remission (Zimmerman, Ruggero, et al., 2006; Zimmerman, Chelminski, McGlinchey, & Young, 2006; Zimmerman, McGlinchey, Posternak, et al., 2006) since both symptoms and functioning indicate a depressive episode.
The depression literature provides various estimates relating depressive symptoms and functioning. Most researchers examining the relationship use adjectives (e.g., strong, weak, etc.) rather than provide exact correlations. To address this shortcoming, we present a literature review relating depressive symptoms and functional outcomes.
We chose to study depression because depression is one of the three most prevalent and burdensome psychological disorders that affects us all in some way. Latest US estimates show that depressive disorders affect approximately 16% of the population (lifetime prevalence) (Kessler et al., 1994, 2003) and leads to considerable personal, social and economic loss. Cross-sectionally, survey evidence (Kessler et al., 2003) suggests that roughly 60% of depressed people reported substantial (i.e., severe or very severe) impairment. Furthermore, roughly half (51.6%) received depression treatment but only 2 out of 5 patients (41.9%) responded–only 20% of depressed respondents were successfully treated–and most indicated substantial daily life functional impairment even after treatment. Thus, following treatment, many people continue to live with fewer depressive symptoms that adversely affect functioning. Functional impairment affects not only the depressed person but families, friends, and general society as well. A recent US estimate of depression’s economic burden indicates direct costs (diagnosis and treatment) of $2.1 billion and indirect costs (impact on occupational, long-term disability, premature mortality, etc.) of $4.2 billion (Jones & Cockrum, 2000; Baldwin, 2001); cost estimates that rank depression as one of the most costly US health care problems (Wells et al., 1989). The high prevalence, direct impact, and serious society implications gave us the best case scenario for relating symptoms and impairment.
To support prior research initiatives and to provide a deeper understanding of the relationship between symptoms and functioning, we aimed to 1) review the research relating symptoms and functioning, 2) provide a rationale for measuring both outcomes, and 3) discuss potential measurement artifacts. We reviewed the literature to summarize and examine the relationship between symptoms and functioning.
Reviews of social (e.g., social alienation (Coyne & Downey, 1991; Joiner & Katz, 1999; Joiner, 2000; Coyne, Thompson, & Palmer, 2002), marital discord (Coyne et al., 2002), and social interactions (Coyne, 1976; Segrin & Abramson, 1994; Nezlek, Hampton, & Shean, 2000; Wildes, Harkness, & Simons, 2002; Petty, Sachs-Ericsson, & Joiner, 2004)), behavioral (e.g., physical activity (Allgöwer, Wardle, & Steptoe, 2001), engagement in pleasant activities (Lewinsohn & Graf, 1973), and engagement in high risk activities (Allögwer et al., 2001)), biological (e.g., adrenergic system changes (Dubini, Bosc, & Polin, 1997) and prefrontal cortex activity (Fu et al., 2001; Davidson, Pizzagalli, Nitschke, & Putnam, 2002; Stone, Quartermain, Lin, & Lehmann, 2007)), and economic (Chisholm, Sanderson, Ayuso-Mateos, & Saxena, 2004) indicators of depression converge on the same conclusion–depression adversely affects human functioning. These reviews, however, contain no specific information about the magnitude of the relationship. Regardless, depression experts hold that the relationship exists and most consider it to be common knowledge today. Mental health experts, for example, acknowledge the relationship in both diagnostics (American Psychiatric Association, 1994) and treatment planning (Kramer, Smith, & Maruish, 2004). We have all come to accept that depression interferes with daily independent living and leads to great suffering for patient, family, and society; the relationship strength, however, remains unclear.
While most researchers and clinicians recognize these implications, severity of depression is almost solely expressed by phenomenological (i.e., symptoms) assessments that fail to address the effects of depression. Furthermore, major depression episodes require functional impairment or distress in “social, occupational, or other important area[s] of functioning” (American Psychiatric Association, 1994). Researchers and clinicians devote considerable resources to understanding and treating depression; measuring both functional and symptom outcomes may only serve to help those efforts. Our intentions are to demonstrate that symptoms and functioning hold a tenuous relationship requiring both to be measured routinely.
2. Methods
We conducted several comprehensive literature searches of PubMed, Cochran Collaboration Archives, PSYCInfo, Google, and relevant article reference lists. There was no time constraint used for the search; we used all articles meeting our search terms on June 30th, 2007. The first search focused on identifying symptom and functional outcome measures used in depression research. Our aim was to identify every relevant general and domain-specific measure used with depressed samples. An initial search using the keywords “major depression” and “function[ing]” produced more than 700 articles that were reduced by searching specific functional domain keywords (e.g., “social functioning”) and instrument names (e.g., “SAS-SR” and “SOFAS”) to ensure adequate coverage. We focused on major depression to ensure our search addressed pathology in the vein of the DSM system (Coyne, 1994). Results from this search were used for the second search that focused on identifying articles reporting the relationship between depression symptom measures and functional outcome measures with depressed samples. Keywords “major depression”, “symptoms”, and “function[ing]” produced over 500 articles that were reduced by searching for specific symptom measures (e.g., “BDI”) and functioning measures (e.g., “SAS-SR”). The final search results included articles containing correlations between depression symptom measures and functional outcome measures (Narticles=10 for global functioning; Narticles=21 for social functioning; Narticles=3 for occupational functioning; and Narticles=2 for physical functioning) for subjects with either current major depressive disorder (MDD) or a current major depressive episode (MDE). We chose to exclude any non-correlational studies to avoid any possible confound due to potential conversion problems from other statistics. Furthermore, our choice to exclude non-clinical samples stem from the fact that depression scales are not well-suited for measuring depressive symptomatology in non-depressed samples (Watson et al., 1995).
2.1. Analyses
We used summary statistics (means and standard deviations) for the published correlations from each functional domain. Additionally, hierarchical regression models were used to predict absolute values of the correlations reported. Correlations from each functional domain served as the dependent variable while sample size, respondent similarity, and administration time served as the predictors. Specifically, predictors included sample size (N), similarity of respondent (binary variable coded as 1 for similar respondent and 0 for dissimilar respondent), and dummy-coded contrasts of administration time (post-treatment compared to both baseline and during treatment). Sample size was included simply as a proxy for the stability of the correlation whereas the other predictors were theoretically justifiable from the literature. Similarity of respondent served to disentangle response bias from symptom and functioning covariation. Finally, administration time allowed us to assess the stability of the correlations over time within and between studies. We excluded symptom and function measures as predictors due to the imbalance in most models Instead of modeling those predictors, we present figures that show the mean correlations observed by instrument. For each significant predictor, we reported unstandardized regression coefficients (b) along with the t value and p-value associated with the coefficient. Due to space limitations, we only reported significant predictor results but noted non-significant results in cases where the non-significance might be meaningful. Since multiple models were used for the regression analysis–one for each functional domain–we countered alpha inflation due to multiple tests using a conservative Bonferroni correction procedure and report p-values well below the .05. The regression models helped us determine the best predictors of those correlations. These predictive models were not meant to affect policy but rather to stimulate future research efforts in this area.
3. Results
3.1. The association between depressive symptoms and global functioning
Many functional outcomes relate to depressive symptomatology; global functioning serves as the best starting point. Most of the work directly relating depressive symptoms to global functioning focuses on mean differences. These mean differences, however, do not convey the relationship between the two outcomes. Some research, however, offers correlations (e.g., Shelton et al., 2001)2. We list the predominant global functioning measures (see Table 1) and depressive symptom measures (see Table 2) to show the depth and breadth of our search. We also included relative citation rates for the measures to show the extent to which each was used in depression research.
Table 1.
Global functioning measures used in depression research
| Measure | Source | Respondent | Nitems | NDepStudies | Psychometrics |
|
|---|---|---|---|---|---|---|
| ᾱ | rxx’ | |||||
| SF-36 | Ware and Sherbourne (1992) | Patient | 36 | > 1000 | .79 | .42 |
| CGI-S | American Psychiatric Association (1994) | Clinician | 1 | > 700 | NA | .2–.81 |
| CGI-C | American Psychiatric Association (1994) | Clinician | 1 | > 700 | NA | .15–.78 |
| GAF | American Psychiatric Association (1994) | Clinician | 1 | > 150 | NA | .83 |
Measure abbreviations: SF-36: Short-form Health Survey, CGI-S: Clinical Global Impression-Current State, CGI-C: Clinical Global Impression-Clinical Improvement, GAF: Global Assessment of Functioning.
The psychometrics include measures of internal consistency (α) and test-retest reliability (rxx’).
Table 2.
Depression symptom measures
| Measure | Source | Respondent | Nitems | NDepStudies | Psychometrics |
|
|---|---|---|---|---|---|---|
| ᾱ | rxx’ | |||||
| BDI | Beck, Ward, Mendelson, Mock, and Erbaugh (1961) | Patient | 21 | > 1500 | .86 | .66 |
| CES-D | Radloff (1977) | Patient | 20 | > 1200 | .85 | .57 |
| HAM-D | Hamilton (1960) | Clinician | 17 | > 1200 | .89 | |
| Zung | Zung (1965) | Patient | 20 | > 800 | .83 | |
| MADRS | Montgomery and Asberg (1979) | Clinician | 10 | > 800 | .90 | |
| HADS-D | Zigmond and Snaith (1983) | Patient | 14 | ≈ 800 | .85 | .86 |
| SCL-90 | Derogatis, Lipman, and Covi (1973) | Patient | 90 | > 600 | .86 | .81 |
| CIDI | Kessler, Andrews, Mroczek, Ustun, and Wittchen (1998) | Patient | Varies | ≈ 350 | .95 | |
| SCIDIII | Spitzer, Williams, Gibbon, and First (1992) | Clinician | Varies | ≈ 350 | .64–.93 | |
| SCIDIV | American Psychiatric Association (1994) | Clinician | varies | ≈ 350 | .61–.80 | |
| MDI | Bech (1998) | Clinician | 12 | ≈ 30 | .90 | |
| IDS-SR | Rush, Gullion, Basco, Jarrett, and Trivedi (1996) | Patient | 30 | ≈ 30 | .92 | |
| IDS-CR | Rush et al. (1986) | Clinician | 30 | ≈ 25 | .90 | |
| SCL-20 | Derogatis et al. (1974a,b) | Patient | 90 | ≈ 20 | .92 | |
| QIDS-SR | Rush et al. (2003) | Patient | 18 | ≈ 20 | .86 | |
| QIDS-C | Rush et al. (2003) | Clinician | 18 | ≈ 10 | .85 | |
Measure abbreviations: BDI: Beck Depression Inventory, CES-D: Center for Epidemiological Studies Depression Scale, HAM-D: Hamilton Depression Rating Scale, Zung: Zung Self-Rating Depression Scale, MADRS: Montgomery–Asberg Depression Rating Scale, HADS-D: Hospital Anxiety and Depression Scale-Depression, SCL-90: Symptom Check List-90 items, CIDI: Composite International Diagnostic Interview, SCIDIII: Structured Clinical Interview (DSM-III), SCIDIV: Structured Clinical Interview (DSM-IV), MDI: Major Depression Inventory, IDS-SR: Inventory of Depressive Symptoms-Self-Rated, IDS-CR: Inventory of Depressive Symptoms-Clinician Rated, SCL-20: Symptom Check List-20 items, QIDS-SR: Quick Inventory of Depressive Symptomatology-Self-Rated, QIDS-C: Inventory of Depressive Symptoms-Clinician.
The psychometrics include measures of internal consistency (ᾱ) and test-retest reliability (rxx’).
Table 3 lists the correlations (sorted in descending absolute value order) found from our search. Patients report fewer functional limitations as depression remits–a finding throughout the depression treatment literature but not necessarily communicated via the correlations listed in our table. Concurrent measures of depressive symptoms and global functioning show moderate to strong correlations (X̄Abs(r)=.50, σ=.25) across clinical samples of all ages. The strongest correlations exist for concurrent, end-of-treatment administrations with homogeneous respondents (i.e., clinicians or patients completed both instruments). Regression model results accounted for 75% (Radj2=.75) of the variance in these correlations. When comparing treatment administration times, post-treatment (b=.34; t=6.03, p<.00001) and during treatment (b=.32; t=4.99, p<.00001) correlations were higher than those assessed at baseline; no other treatment time comparisons were significant. Finally, the same respondent produces significantly higher correlations than dissimilar respondents (b=.25; t=4.51, p<.0002). Figs 1 and 2 show the absolute correlations observed by measure and by administration time, respectively.
Table 3.
Correlations between depressive symptom and global functioning measures
Post-treatment assessment.
6-year follow-up.
HAM-D was shortened to 10 items.
Baseline assessment.
DSM-IV symptoms were measured by a combination of rating scales including the Hamilton Depression Rating Scale (HAM-D), Montgomery-Asberg Rating Scale, and the Brief Psychiatric Rating Scale.
Fig. 1.
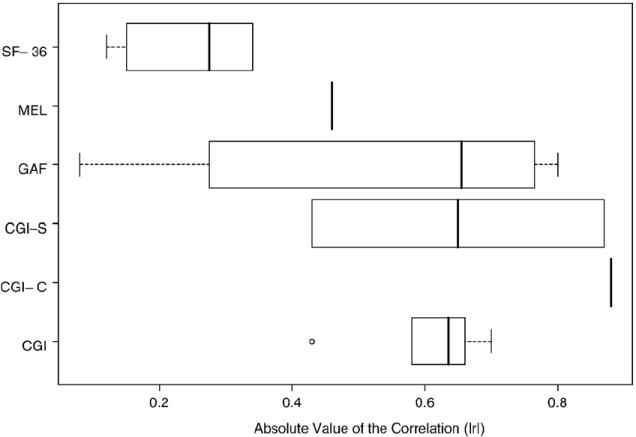
Absolute value of correlations obtained for each global functioning measure.
Fig. 2.
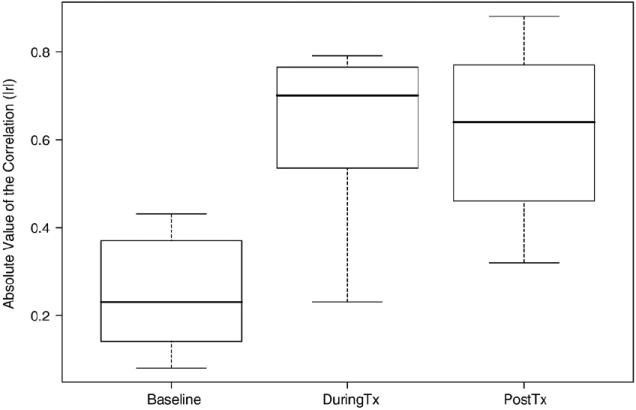
Absolute values of global functioning correlations by administration time.
Clinicians and clinical researchers ought to be interested in functional improvement, decline, and impairment across specific domains affected by depression. The clinician’s role is to reduce both symptoms and impairment (Möller et al., 2003). Clinical researchers aim to develop better interventions that ameliorate patient suffering. Relying on global measures of functional impairment does little to advance this initiative because residual functional impairment may persist after symptoms remit (Zimmerman et al., 2008).
3.2. Functional domains
The evidence suggests depressive symptoms are related to functioning across many domains. We covered the relationship between symptoms and global functioning but we have not addressed the nature of that relationship across specific functional domains. Depression results in household strain, social irritability, financial strain, physical limitations, occupational disruption, and restricted activity days, bed days, health status (Judd, Paulus, Wells, & Rapaport, 1996). The questions remain whether these outcomes are affected uniformly and, if not, what might account for the differences. If clinicians and clinical researchers are to use both symptom and function outcome measures, they ought to be clear about the state and nature of the relationship. In the following sections, we document the available evidence linking depressive symptoms with three specific functional domains–social, occupational, and physical. We begin each section below with a summary of a) theoretical perspectives linking symptoms and functioning, b) functional outcome measures and c) empirical results from our literature review.
3.3. Social functioning
3.3.1. Theoretical ties between depression and social functioning
Many theories relate depressive symptoms and social functioning. One theory–interpersonal theory–provides a mechanistic framework where emotions guide social interactions throughout the formation and maintenance of interpersonal relationships (Keltner & Kring, 1998). People are social animals; they strive to maintain relationships with others and emotions help us navigate those relationships (Myers & Diener, 1995; Diener & Seligman, 2002). When emotions no longer function normally, the guidance offered by them deteriorates and our social functioning suffers (Hatfield, Cacioppo, & Rapson, 1994; Joiner & Katz, 1999; Zauszniewski & Rong, 1999). Other theories suggest similar linkages but specify different mechanisms. Information processing (Leppnen, 2006), for example, suggests that depression results from an inability to process emotionally relevant social interaction cues. People with major depression have abnormal cognitive and neural processing of emotional information (Goeleven, Raedt, Baert, & Koster, 2006). The abnormal processing may not only be indicative of depression vulnerability (Leppänen, 2006) but also may cause the lasting social impairment often observed following depressive treatment (Hirschfeld et al., 2002). Furthermore, poor social functioning may lead to lasting depression due to rejection (Coyne, 1976). These divergent theories suggest different causal mechanisms and causal direction; a troubling result for both clinicians and researchers.
From one perspective, depression causes social impairment–but not a simple linear causal relationship. For causal direction, treatment outcome studies show improved social functioning for patients who respond to treatment (Agosti, 1999b; Airaksinen, Wahlin, Larsson, & Forsell, 2006; Buist-Bouwman, Ormel, Graaf, & Vollebergh, 2004; Judd et al., 2000; Spijker et al., 2004) and fully recover (Agosti & Stewart, 1998; Papakostas et al., 2004). Observational studies show modest prediction of social adjustment with depression symptom scores (Agosti & Stewart, 1998; Agosti, 1999a,b). Retrospective studies (e.g., Bromberger et al., 2005) show similar results where past depression predicted current social functioning. Regardless of this evidence, social functioning as an end-point may be more difficult to change than depressive symptoms (Judd et al., 2004).
Not all treatment outcome studies support these improvements. Bech (2005) documented statistical but non-clinically significant social functioning change for various scales. Social functioning improvement depends on characteristics of the treatment (e.g., duration; Kocsis et al., 2002, strength; Nickel et al., 2005, and modality; Weissman, Klerman, Prusoff, Sholomskas, & Padian, 1981; Kasper, 1999; Papakostas et al., 2004) and patient (e.g., personality disorders; Tyrer, 1990; Seivewright, Tyrer, & Johnson, 2004; Skodol et al., 2005, comorbid medical conditions; Simon, Korff, & Lin, 2005, comorbid mental health conditions; Spijker et al., 2004, physical fitness Stewart et al., 2003, cognitive functioning Airaksinen et al., 2006, and coping style; Sherbourne, Hays, & Wells, 1995). Furthermore, social functioning change lags behind depression symptom change; impairment lingers–persisting much longer (up to 4 years longer; Bothwell & Weissman, 1977) than depressive symptoms (Hirschfeld et al., 2000, 2002; Scott et al., 2000). Patients who presented with symptoms and functional impairment before treatment showed clinically meaningful change in symptoms but relatively little change in social functioning afterwards. Thus, social functioning changes are said to lag symptom changes. The lingering social impairment appears context dependent, lingering longer in marital and interpersonal relationships (Moos, Cronkite, & Moos, 1998) where certain symptoms (e.g., low mood, fatigue, sexual disinterest, cognitive problems, and suicidal ideation) persist (Tweed, 1993). Finally, social functioning tends to change at a complex, non-linear rate (Tweed, 1993) dependent upon specific symptoms. That is, the nature of the relationship and the length of lingering depended upon a subset of symptoms. Despite the complexities of the relationship, there is one clear finding from the literature–social functioning changes follow depressive symptom changes.
An alternative perspective of social functioning causing depression gains far less support. Theoretically, depression may cause social skill deficits (Segrin & Abramson, 1994) that create socially uncomfortable situations that perpetuate negative cognitions (Abramson, Metalsky, & Alloy, 1989). In a longitudinal study with elderly (60+ years old), for example, Kivelä (1994) found that poor spousal relations tended to adversely impact the mood for men. The social or familial strain caused elevated depressive symptoms. These findings indicate the potential for a bidirectional relationship.
3.3.2. Social functioning measures
Researchers use many social functioning scales in depression outcome studies (Bech, 2005). Table 4 presents a measure summary listing each by name, length, and relative use in depression outcome research. Several notable findings jump out. First, few of these social functioning measures have citation rates comparable to any depression symptom measure; most depression symptom measures have over 500 citations where only one social functioning measure has over 100. Second, only one social functioning measure tends to be widely used with the rest relegated to specific research programs. Development date is another subtle distinction between depression symptom measures and social functioning measures. Most symptom measures were developed in the 1960’s (40+ years ago) whereas most social functioning measures were developed within the last 20 years. Development date has an obvious influence on use; if the measure did not exist in the 1970’s, it was not going to be used in research. Finally, instruments using patient self-report have substantially higher citations in depression research.
Table 4.
Social functioning measures
| Abbreviation | Source | Respondent | Social domains | Nitems | NDepStudiesa | Psychometrics |
|
|---|---|---|---|---|---|---|---|
| α | rxx’ | ||||||
| SF-36 | Ware and Sherbourne (1992) | Patient | General | 2 | >200 | .79 | .44 |
| DAS | Spanier (1976) | Patient | Relationships | 32 | 41 | .81 | |
| IIP | Horowitz et al. (1988) | Patient | Relationships | 127 | 31 | .93 | .80 |
| SDS | Sheehan et al. (1996) | Patient | General | 3 | 29 | .89 | .73 |
| SASS | Bosc Dubini and Polin (1997) | Patient | Multiple | 21 | 24 | .81 | |
| SAS-SR | Weissman and Bothwell (1976) | Patient | Multiple | 42 | 23 | .74 | .80 |
| DID | Weissman and Bothwell (2004) | Patient | Multiple | 6 | 16 | .89 | .82 |
| WSAS | Marks (1986) | Patient | Leisure and Relationships | 5 | 14 | .81 | .73 |
| SOFAS | Goldman, Skodol, and Lave (1992) | Clinician | General | 1 | 11 | .89 | |
| SIS | Clare and Cairns (1978) | Clinician | Multiple | 13 | 3 | .90 | |
| IPS | Davidson et al. (1989) | Clinician | Sensitivity | 6 | 2 | ||
| LFQ* | Davidson et al. (1989) | Patient | General | 14 | 2 | .84 | .77 |
| SFQ | Tyrer (1990) | Patient | Multiple | 8 | 2 | ||
| SAS-II | Schooler et al. (1979) | Clinician | Multiple | 52 | 1 | ||
Abbreviations: SF-36: Short-Form Health Survey, DAS: Dyadic Adjustment Scale, IIP: Inventory of Interpersonal Problems, SDS: Sheehan Disability Scale, SASS: Social Adaptation Self-evaluation Scale, SAS-SR: Social Adjustment Scale-Self-Report; DID, Diagnostic Inventory for Depression, WSAS, Work and Social Adjustment Scale, SOFAS: Social and Occupational Functioning Assessment Scale for the DSM-IV, SIS: Social Interview Schedule, IPS: Interpersonal Sensitivity Scale, LFQ: Life Functioning Questionnaire,SFQ: Social Functioning Questionnaire, and the SAS-II, Social functioning measures included the Social Adjustment Scale II. Notes: *LFQ contains mostly social functioning items but also contains items relevant to occupational functioning. The psychometrics includes measures of internal consistency (α) and test–retest reliability (rxx’).
These numbers represent the frequency each measure was used in depression research as of 8/31/2008 in PubMed.
We sorted the instruments in Table 4 according to relative use and discuss them in that order. Each measure assesses somewhat different aspects of social functioning. A brief and widely used social functioning scale–the SF-36 social functioning subscale–consists of two self-report items contained in Short-Form Health Survey (SF-36) (Ware & Sherbourne, 1992; McHorney, Ware, Lu, & Sherbourne, 1994). The two items represent general social functioning and relate well with depression remission (e.g., Korff et al., 2003). The second most used instrument is the Dyadic Adjustment Scale (DAS) (Spanier, 1976). While not specifically a social adjustment scale per se, the DAS assesses adjustment, satisfaction, and general relationship quality in dyadic relationships (e.g., marital, friends, etc.). Similarly, the Inventory of Interpersonal Problems (IIP) (Horowitz, Rosenberg, Baer, Ureo, & Villaseor, 1988) assesses the extent to which depressive symptoms affect significant relationships. The Sheehan Disability Scale (SDS) (Sheehan, Harnett-Sheehan, & Raj, 1996)–a broad, self-report measure of social functioning–consists of just three items with each assessing work/study, social life, and family life functioning. Only one item specifically addresses social functioning, however, most researchers use all three items together to reflect overall disability (Sheehan & Sheehan, 2008). Another self-report instrument, the Social Adaptation Self-Evaluation Scale (SASS) (Paykel, 1999) consists of 21 items of which 16 assess relationships in, attitudes of and sensitivity to social situations. Developed primarily as a clinical trial outcome measure, the SASS can be found also in epidemiological studies and cross-sectional designs. The Social Adjustment Scale–Self Report (SAS-SR) (Paykel, Weissman, Prusoff, & Tonks, 1971; Weissman, Prusoff, Thompson, Harding, & Myers, 1978); a 42 items patient self-report scale covers a wide spectrum of social contexts including work, home, school, leisure, family, and marital, and parental domains. All contexts are combined to form four general categories of social adjustment–performance at expected tasks, friction with others, interpersonal relations, and feelings/satisfaction. The six-item Diagnostic Interview for Depression (DID) psychosocial functioning subscale (Zimmerman, Sheeran, & Young, 2004) assesses the impact of depressive symptoms on daily responsibilities, relationships with significant others, relationships with close family members, relationships with friends, participation in leisure activities, and overall level of function. Three of the five items on the Work and Social Ajustment Scale (WSAS) (Marks, 1986) assess social functioning directly. These relevant items assess leisure (both social and private) and relationship contexts while the other items assess home and work functioning. A single item that combines both social and occupational functioning comes from the Diagnostic and Statistical Manual (IV-TR) (American Psychiatric Association, 1994) and is commonly referred to as the Social and Occupational Functioning Assessment Scale (SOFAS). Clinicians rate patients according to impairment due to both mental and physical health problems thus introducing a potential for less interpretable scores. Another clinician administered scale is the Social Interview Schedule (SIS) (Clare & Cairns, 1978; Hecht & Wittchen, 1988) that assesses a patient’s management and satisfaction across 13 social domains. Shifting away from more general social functioning toward a mechanistic level is the Interpersonal Sensitivity Scale (IPS) (J. Davidson, Zisook, Giller, & Helms, 1989)–consisting of a subset of items from the Hopkins Symptom Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974a,b). The IPS assesses the extent to which a person is (overly) sensitive to social situations. An instrument that shows high convergent validity with the SAS-SR (.56<r<.85) is the Life Functioning Questionnaire (LFQ) (Altshuler, Mintz, & Leight, 2002)–a 14-item self-report instrument. Altshuler and colleagues developed the LFQ to accomodate the complex social roles adopted by most contemporary patients. While consisting of mainly work-relevant functioning items, several items assess domain specific social functioning. The Social Functioning Questionnaire (SFQ) (Tyrer, 1990) is even shorter than the SASS and consists of just 8 self-report items. Several studies showed that the SFQ had a modest but significant relationship with symptom scores (Tyrer et al., 2005) and that relationship persisted even after 12 years of follow-up with patients suffering from comorbid personality disorders (Seivewright et al., 2004). Finally the Social Adjustment Scale (SAS-II) (Schooler, Hogarty, & Weissman, 1979) is a widely used self-report instrument in schizophrenia research but several depression researchers use the instrument to assess social functioning.
Only a few studies report convergent validity between social functioning instruments. The few that do indicate a strong correlation suggesting substantial overlap between measures. The subscales on the LFQ, for example, correlate roughly .70 with the subscales on the SAS-SR (Altshuler et al., 2002) and the IIP correlates about .65 with the SAS-SR (Vittengl, Clark, & Jarrett, 2003). Other social functioning instruments likely correlate just as high but some researchers (e.g., Bech, 2005) hold that certain measures are more sensitive to treatment changes than others. Direct comparison studies between instruments for treatment outcomes–taking into account the psychometric properties–need to be done before we can be confident that some measures are preferable to others.
3.3.3. Empirical relationship between depressive symptoms and social functioning measures
There are many choices in social functioning outcome instruments and all show a relatively modest relationship with depressive symptoms. Table 5 summarizes the relationship between depressive symptom and social functioning measures. The mean correlation across all studies was just as strong as the mean global functioning correlation (X̄Abs(r)=.51, σ=.18) with slightly less variability (see Fig. 3 for the correlations by social functioning measure). Predicting those correlations with sample size, respondent, and administration time yielded a moderately strong prediction model accounting for less than half of the variance (Radj2=.40). The correlations between social functioning and depressive symptoms were best predicted by sample size and administration time. While sample size predicted the absolute magnitude of the correlation (b=.0007; t=3.36, p<.002), the effect was incredibly small. A much larger effect (see Fig. 4) was observed for administration time where post-treatment (b=.27; t=4.87, p<.00001) and during treatment (b=.24; t=4.22, p<.00001) administrations yielded the largest absolute value correlations compared to baseline. Neither lagged administration (b=−.34; t=−1.04, p<.30) nor pooled (b=−.10; t=−0.77, p<.44) differed from baseline or non-concurrent (b=−.39; t=−3.75, p<.0005) administrations.
Table 5.
Social functioning effect sizes by study
Authors reported Spearman ρ instead of Pearson r.
r computed for 12 week data.
r computed for 30 week data.
r computed on 6-year follow-up data.
r computed for 4 week data.
Sertraline treatment group only at 76 weeks into the treatment.
The HAM-D, IDS-SR, IDS-CR, and the BDI were combined to form a composite measure and r was computed based upon a longitudinal change score.
r computed between AUC scores for both measures.
r computed on baseline measures.
r computed for 8 week data.
r represents relationship between past depression and 12-year follow-up of social functioning.
r computed on longitudinal data.
Symptoms measured by first principal component of the SCL-90, the BDI, and the mental health/vitality scales from the SF-36.
Social functioning was measured by first principal component of the Groning’s List of Protracted Difficulties (Hendriks et al., 1990) and the Hostility scale of the SCL-90).
Placebo treatment group only at 76 weeks into the treatment.
Fig. 3.
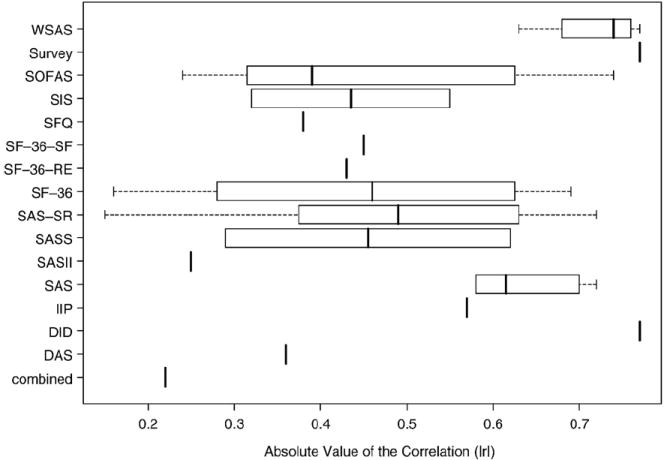
Absolute values of social functioning correlations by measure.
Fig. 4.
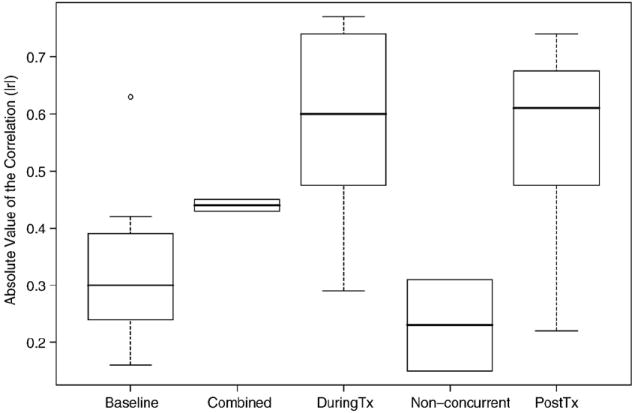
Absolute values of social functioning correlations by administration time.
3.4. Occupational functioning
3.4.1. Theoretical ties between depression and occupational functioning
A depressed person values social functioning while everyone–the depressed person and society–values occupational functioning. Depression affects worker productivity by reducing cognitive processing (Pardo, Pardo, Humes, & Posner, 2006), memory (Bearden et al., 2006; Rose & Ebmeier, 2006), attention and concentration (Zimmerman, McGlinchey, Young, & Chelminski, 2006; Levin, Heller, Mohanty, Herrington, & Miller, 2007), and energy levels (Christensen & Duncan, 1995) as much if not more than most other physical illnesses (Burton, Conti, Chen, Schultz, & Edington, 1999). At the surface level, depression affects three areas related to occupational functioning–education, absenteeism, presenteeism, and employment (Lerner et al., 2004). Depression affects educational attainment (Berndt et al., 2000) thus affecting employment opportunities. If employed, depressed people miss work more than other employees (Stoudemire, Frank, Hedemark, Kamlet, & Blazer, 1986; Rice & Miller, 1995; Stewart et al., 2003; Rost, Smith, & Dickinson, 2004; Zhang, Rost, & Fortney, 1999; Zhang, Rost, Fortney, & Smith, 1999; Kessler et al., 1999; Leon, Walkup, & Portera, 2002; Druss, Rosenheck, & Sledge, 2000; Collins et al., 2005); –including workers with debilitating medical conditions such as heart disease (Druss et al., 2000) and rheumatoid arthritis (Lerner et al., 2004). Depressed workers are less productive (i.e., lower presenteeism) than non-depressed workers; they operate at slower rates (Wang, 2004) and produce more errors (Greenberg et al., 2003). As depressive symptoms increase, work productivity decreases further (Thompson & Richardson, 1999) independent of comorbid medical conditions (Adler et al., 2006). Furthermore, depressed workers work report more conflict (Smith et al., 2002) at work leading to even greater loss of productivity. All of these effects combined lead to unemployment or underemployment (Greenberg, Stiglin, Finkelstein, & Berndt, 1993; Greenberg et al., 2003; Kassam & Patten, 2006)–negative social outcomes to be sure. Depression may have the highest impact on total work impairment of any disorder (Collins et al., 2005). It is important to note that no research to date suggests a bidirectional relationship between depression and occupational functioning.
3.4.2. Occupational functioning measures
Unlike social functioning where context differentiates most measures, occupational functioning can be measured by many different approaches and each captures a separate facet (e.g., employment status, absenteeism, presenteeism) of occupational function. Table 6 lists the available occupational functioning measures used with depressed patients. Some measures listed are single items that pertain only to the patient’s current status.
Table 6.
Occupational functioning measures
| Measure | Source | Respa | Facetsb | Nitems | NDepStudies | Psychometrics |
|
|---|---|---|---|---|---|---|---|
| α | rxx’ | ||||||
| Employment | NA | Any | E | 1 | >250 | NA | |
| Absenteeism | NA | Any | A | 1 | >250 | NA | |
| SAS-SRc | Weissman and Bothwell (1976) | P | P | 6 | 23 | ||
| WHO-DAS II | Rehm et al. (1999) | Any | P | 32d | 17 | .86 | |
| WAI | Tuomi, Ilmarinen, Jahkola, Katajarinne, and Tulkki (1998) | P | A,P | 2 | 4 | .72 | |
| EWPS | Endicott and Nee (1997) | P | P | 25 | 3 | ||
| SPS | Lynch and Riedel (2001)e | P | P | 32 | 2 | ||
| SPS | Turpin et al. (2004) | P | P | 13 | 2 | .82 | |
| WPI | Burton et al. (1999) | Many | A,P | 2 | 1 | ||
| SPS | Koopman et al. (2002) | P | P | 3 | 1 | .80 | |
| WLQ | Lerner et al. (2001) | P | P | 48 | 1 | .89–.96 | |
| WPAI | Reilly, Zbrozek, and Dukes (1993) | P | E,A,P | 6 | 1 | .71–.75 | |
| OFS | Hannula et al. (2006) | C | E,A,P | 1 | 1 | NA | .91 |
Measure abbreviations: SAS-SR: Social Adjustment Scale-Self-Report, WHO-DAS II: World Health Organization-Disability Assessment Scale, WAI: Work Ability Index, EWPS: Endicott Work Productivity Scale, SPS: Stanford Presenteeism Scale, WPI: Work Productivity Index, WLQ: Work Limitation Questionnaire, WPAI: Work Productivity and Activity Impairment Questionnaire, OFS: Occupational Functioning Scale The psychometrics include measures of internal consistency (α) and test-retest reliability (rxx’).
Respondent of the instrument: P (Patient), C (Clinician), Any (for anyone) and Many (for multiple respondents).
Facets include E (employment), A (absenteeism) and P (presenteeism).
The SAS-SR work subscale.
12 or 32 item versions for either clinician administered, self-report, or proxy respondents.
The original Stanford Presenteeism Scale was developed in 2001 but several shorter versions came afterwards and are listed below.
Capturing occupational functioning may be as simple as recording current employment status or employment history and as complex as monitoring the workplace environment. Employment status merely reflects a person’s current state of employment. Some researchers (e.g., Coryell et al., 1993) use a rating scale to assess employment status to provide a fuller picture of current, past, and potential future status. Employment history, in contrast, provides more depth about a person’s ability to maintain a single job, focus on a career, or even tolerate the demands of long-term employment. These crude measures often provide enough evidence to show that a person is not functioning or cannot function well within an occupational setting. For those who are gainfully employed, however, the crude employment and employment history measures miss functional deficiencies that may better predict long-term occupational functioning and even continued employment. There are a number of self-report instruments available that capture occupational functioning. Each of those discussed here were evaluated with a depressed sample at some point during development; needless to say there are countless instruments from other research areas that may be just as suitable.
Two general domains tend to be the focus of most occupational functioning measures–presenteeism and absenteeism. Presenteeism reflects the person’s ability to be productive when present at work. There are two newer and more widely used instruments of presenteeism; the Work Limitations Questionnaire (WLQ) (Lerner et al., 2001, 2003, 2004) and the Stanford Presenteeism Scale (SPS) (Koopman et al., 2002). The WLQ is a 25 item self-report measure that covers four dimensions of work including time, physical, mental-interpersonal, and output demands. Research using the WLQ showed that patients with mental health concerns (especially depression) tended to be far more work impaired than patients with known physical health concerns. A second presenteeism instrument–the Stanford Presenteeism Scale (SPS)–comes in multiple lengths as brief as 6 items (Koopman et al., 2002) or 13 items (Turpin et al., 2004) but may be administered as a full-scale 32-item (Lynch & Riedel, 2001) self-report. The SPS focuses on the last month of work and covers two general domains (completing work and avoiding distractions). All versions tend to show strong psychometric properties with depressed samples. Other instruments are available for assessing presenteeism but they are not widely used with depression and therefore do not have the empirical support that the instruments above possess.
Presenteeism reflects a worker’s ability to get work done while absenteeism reflects the person’s tendency to avoid or miss work. There are many different ways to assess absenteeism but most of the instruments tend to be far less complicated than the presenteeism scales. The reason for the simpler measurement model stems from the fact that absenteeism is an easier, more available construct than presenteeism. What complicates matters for measuring absenteeism is the context; a person may miss work for many reasons but it is important to distinguish missed work due to mental health problems from missed work due to other circumstances. The presenteeism scales mentioned previously typically provide some data for assessing absenteeism but the researcher must be sure that the absence is due to depression. Linking employee records (if available) with self-reports attributing the nature of the absence is likely to be the best method for capturing the full context of worker attendance.
Both absenteeism and presenteeism may be assessed using alternative methods including daily record techniques (Zohar, 1999), informant reports (Wright, 1992; Wright & Bonett, 1993), or objective performance records (Bommer, Johnson, Rich, Podsakoff, & MacKenzie, 1995) that all use some form of behaviorally anchored rating scales (Smith & Kendall, 1963). These methods have a long history in industrial and organizational (IO) psychology and each approach offers reasonably strong predictive validity to worker turnover and retention. Furthermore, the relationship between more objective measures and subjective measures tends to be stable but weak, suggesting a unique contribution from both perspectives.
The IO literature also distinguishes between normal (inadvertent) functioning and deviant (deliberate) functioning. A recent meta-analysis by Berry, Ones, and Sackett (2007) provides clear definitions of deviant worker habits including the distinction between individual and organizational deviance. Individual deviance refers to acts directed at other people whereas organization deviance refers to acts directed at the organization. Both of these deviant acts may be relevant to poor occupational functioning but neither tends to be found in the clinical outcome literature. Researchers studying workplace deviant behavior tend to use a single, self-report instrument of workplace deviance (Bennett, Torrance, Boyle, & Guscott, 2000) with a minority of the research using similar but distinct self-report scales (e.g., Marcus, Schuler, Quell, & Hmpfer, 2002); alternative methods appear to absent in the literature.
Distinguishing between normal and deviant functioning may be helpful in measuring occupational functioning in future clinical contexts by stressing that occupational functioning is more than just the execution of tasks at work (Arvey & Murphy, 1998); occupational functioning includes both the nature of the work, the workplace setting, and the person’s ability and state to carry out the requisite work without causing problems at the organizational level. Measuring occupational functioning at multiple levels will help us better understand the nature and extent that depression affects a person’s functioning.
3.4.3. Empirical relationship between depressive symptoms and occupational functioning measures
While the implications of depression on occupational functioning seem clear, the research support is wanting. Some studies suggest a strong relationship (e.g., Aluoja, Leinsalu, Shlik, Vasar, & Luuk, 2004) while others suggest a weak relationship (e.g., Adler et al., 2006; Hannula, Lahtela, Jrvikoski, Salminen, & Mkel, 2006) but neither side has much direct support. Table 7 lists the empirical support linking depressive symptom measures to occupational functioning measures. Due to the lack of variability in respondent and sample size, we restricted our regression analysis to just administration time as a predictor. The prediction model, even though restricted, accounted for more than half the variance in the correlations (Radj2=.56). Also, just as the previous functional domains showed, post-treatment (b=.33; t=4.16, p<.002) and during treatment (b=.22; t=3.27, p<.008) administration produced significantly greater correlations compared to baseline assessments.
Table 7.
Occupational functioning correlations by study
| Source | Symptom measure | Functional measure | N | r |
|---|---|---|---|---|
| Hirschfeld et al. (2002) | HAM-D | EWPS | 175 | .57a |
| Aikens et al. (2008) | SCL-20 | WLQ | 511 | .57 |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 172 | .48a |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 172 | .47b |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 170 | .46a |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 175 | .40b |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 172 | .40c |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 175 | .39c |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 170 | .39b |
| Hannula et al. (2006) | SCL-90 | OFS | 150 | −.26 |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 175 | .24d |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 170 | .21c |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 172 | .18d |
| Hirschfeld et al. (2002) | HAM-D | EWPS | 170 | .08d |
r computed for 12 week data.
r computed for 8 week data.
r computed for 4 week data.
r computed on baseline measures.
A complex relationship between depressive symptoms and occupational functioning may exist but the epidemiological research focus obscures the phenomenology. Specifically, epidemiologists frequently compare depressed and non-depressed people with respect to their occupational functioning. A recent review (Simon, Barber, et al., 2001) documented the relationship between major depression and occupational functioning in four different research designs–cross-sectional naturalistic, longitudinal naturalistic, uncontrolled treatment, and controlled treatment studies. With few exceptions, the reviewed studies provided occupational functioning outcomes with depressed and non-depressed subjects. We lose the ability to estimate the degree to which symptoms affect occupational functioning with group mean comparisons. Depressive symptom increases result in greater occupational impairment (Rytsälä et al., 2005; Sasso, Rost, & Beck, 2006); although only a few studies directly examined this relationship. Depression decreases worker productivity during depressive episodes and even after symptoms remit (Adler et al., 2006).
Epidemiological studies are not the only source linking depressive symptoms and occupational functioning; another method of examining the relationship is through treatment outcome studies. Treatment studies frequently show dramatic changes in occupational functioning during (Mauskopf, Simeon, Miles, Westlund, & Davidson, 1996) and after (Katzelnick, Kobak, Greist, Jefferson, & Henk, 1997) treatment. Those changes are not always clearly documented in the literature. Some studies show more rapid improvement in vocational functioning compared to social functioning (Lisio et al., 1986), however, the overall treatment impact is not always present (Adler et al., 2006) and may require further information about the patients (Jansen, Kant, & Brandt, 2002) to fully understand the relationship. The problem of lingering effects still complicate the relationship; symptoms often abate far earlier than vocational impairments and thus create the same problem of lingering functional impairment after treatment as seen with social impairment (Adler et al., 2006). The longitudinal modeling of social functioning has yet to be done with occupational functioning so there is no direct evidence to the nature and extent of change in occupational functioning during or after treatment.
On a more positive note, depression treatment leads to significant occupational functioning (Rost et al., 2004; Sasso et al., 2006) improvements and social cost reductions (Thompson, 1995). Since occupational functioning can be expressed in terms of monetary value, many studies justify the costs of depression treatment as a cost-savings alternative to no treatment (e.g., Donohue & Pincus, 2007). Cost savings are used to justify the use of both low-cost antidepressants (Hylan, Buesching, & Tollefson, 1998) and high-cost intensive treatment (Leon et al., 2002). Treatment, in general, offers a strong return on investment for most employers (Sasso et al., 2006). Simon, Barber, et al. (2001) reviewed the literature on worker productivity and concluded that depression treatment costs (Simon, Katon, et al., 2001) were far less than the productivity gains observed in workers. Taken together, it appears that the relationship between depressive symptomatology and vocational impairment becomes clearer and more consistent when both are converted into a common metric–money.
3.5. Physical functioning
3.5.1. Theoretical ties between depression and physical functioning
Depressive symptoms relate to physical functioning in many ways. The postulated relationship between depression and physical functioning outcomes remains quite simple; as depressive symptoms increase, physical functioning deteriorates and vice versa (Goodwin, 2006). It is not clear, however, that a causal relationship holds for depression affecting physical functioning. Physical functioning, in general, deteriorates with any medical comorbidity (Cesari et al., 2006) and declines in physical functioning may even bring on depression. The precise relationship remains difficult to disentangle. Moreover, the relationship gets confounded by comorbid conditions and age. Where possible, we present research that take these factors into consideration.
Physical activity likely changes during depressive episodes. The relationship between depressive symptoms and physical activity can be attributed to the fact that depressive episodes are defined by three symptoms relevant to physical activity including 1) diminished interest or pleasure in (almost) all activities throughout the day, 2) psycho-motor agitation or retardation nearly every day, and 3) fatigue or loss of energy nearly every day. If a person were to meet any one of these criteria, we might expect that person to be less physically active. Restlessness or agitation might seem to be a compelling reason to expect an increase in physical activity–thus complicating the relationship. A person, however, must be interested in physical activity and able to participate–even if participation is merely purposeful walking (e.g., to get to work, run errands, etc.). Interest gets affected by definition (first criteria) while ability gets affected by agitation/retardation and fatigue. Few prospective studies exist that directly examine the relationship between activity and depressive symptoms; one exception (Brown, Ford, Burton, Marshall, & Dobson, 2005) showed a negative relationship between symptoms and physical activity in middle-aged women. Recently, Kawada, Katsumata, Suzuki, and Shimizu (2007) reported significant correlations (all r’s >.5) between the morning and afternoon daytime activity but found no significant correlations between activity and reported depressive symptoms. So if people are active in the morning, they tend to be active in the evening, however, general activity does not seem to be related to symptoms in older (Kawada et al., 2007) or younger people (Desha, Ziviani, Nicholson, Martin, & Darnell, 2007). The conflicting results indicate that activity levels may be difficult to compare directly with depressive symptoms.
3.5.2. Physical functioning measures
Physical functioning may be viewed from many perspectives including physical limitations, physical ability, or physical activity with each perspective relevant to fully capturing physical functioning. Depression researchers tend to focus on physical limitations and use a single, self-report instrument–the MOS SF-36 physical function subscale (Ware & Sherbourne, 1992; A. Stewart & Kamberg, 1992). The SF-36 subscale consists of 10 items that assess a person’s general physical functioning ranging from limited instrumental activities of daily living (e.g., bathing or dressing) to vigorous daily activity (e.g., participating in strenuous sports) (Ware & Sherbourne, 1992). Researchers also use questions pertaining to general physical functioning such as visual analog scales.
There are a few studies that provide empirical results for physical ability. In those studies, two measures of physical ability consist of walking speed (e.g., Penninx et al., 1998, 2002) or hand grip strength (e.g., Russo et al., 2007). Both approaches indicate the same result–depression is inversely related to physical ability. The direct measures tend to be more widely used with geriatric populations since comorbid medical conditions affect ability perhaps as much if not more than depression.
With respect to physical activity, there are many ways to measure physical activity including self-report (e.g., the 68-item Arizona Activity Frequency Questionnaire (AAFQ); Staten et al., 2001; Swanson, 2002) or direct measurement (e.g., pedometers; Fukukawa et al., 2004). Physical activity measures assess total energy expenditure by converting self-reported or directly measured values into common caloric or metabolic equivalent units (METS); greater expenditures indicate more physical activity. Direct measures tend to be more intrusive but yield important behavioral data not readily available in depression research. Exercise researchers typically use pedometers (O’Hara & Rehm, 1979) or accelerometers (Todder, Caliskan, & Baune, 2006; Kawada et al., 2007) and often supplemented by exercise logs or diaries to assess physical activity. Both approaches have proven valuable in assessing physical activity across many different samples and contexts.
3.5.3. Empirical relationship between depressive symptoms and physical functioning measures
There is a vast literature on physical functioning in depression with the majority of the work pertaining to sleep, disability, and comorbid medical conditions. Empirical findings suggest that as depression decreases, physical limitations abate but the changes in physical functioning tend to plateau in treatment outcome studies (e.g., Greco, Eckert, & Kroenke, 2004). The findings consistently suggest that physical functioning is negatively related to depressive symptoms. As physical functioning deteriorates, depressive symptoms tend to worsen. These findings suggest a bi-directional relationship.
Our search of physical functioning included physical activity, physical ability and physical illness. Many studies do not distinguish these areas and, instead, combine together as “physical functioning”. Coulehan, Schulberg, Block, Madonia, and Rodriguez (1997), for example, showed that physical functioning at the global level was related to changes in depressive symptomatology but no correlation or regression was reported.
While some evidence exists for physical activity, there is little research directly examining the relationship between depressive symptoms and physical ability. Only two studies reported correlations. One study reported a correlation of −.39 between combined symptom measures and the SF-36 physical functioning scale (Conradi, Jonge, & Ormel, 2008) while the other study (Aikens, Kroenke, Nease, Klinkman, & Sen, 2008) reported a lower correlation (.27) between the SCL-20 and the Patient Health Questionnaire.
Other indirect results exist but did not meet our inclusion criteria. Some studies failed to provide correlations while others focused on non-depressed samples. Russo et al. (2007), for example, found that older people with depression performed significantly worse on walking tasks and instrumental activities of daily living; no correlations were provided. Whether the number of symptoms predicts physical ability remains unclear with those results. Yanagita et al. (2006) found that depressive symptoms predicted the outcomes of several upper and lower extremity performance measures in a sample of roughly 3000 elderly men–none clinically depressed during the study. In both studies cited above, deficits in physical ability may be attributable to general physical decline or mood disturbance.
The research linking depression and physical illness tends to gain the most attention. Stroke, for example, tends to be associated with depression onset and the extent of depression predicts mortality (Robinson, 1997). A similar effect was observed with reports of general health. Han and Jylha (2006) showed that as depressive symptoms declined, an older adult sample tended to have a lower likelihood of reporting declines in health. Conversely, Rutledge et al. (2006) found that depression adversely affects cardiac functioning in a sample of already symptomatic patients with coronary artery disease (CAD). These findings support the known relationship between depression and disease severity. Depression tends to be present with approximately one-fifth (coronary heart disease) to one third (congestive heart failure) of the patients with heart disease (Whooley, 2006) and the relationship between the two problems is small but significant (Frasure-Smith & Lesprance, 2006). Thus, symptoms and self-reported health appear correlated but the magnitude of the relationship remains unclear in the physically healthy depressed population. The studies cited above represent only the latest additions to a long list of research linking disease severity to depression.
One final link between depressive symptoms and physical functioning comes from the treatment literature. According to some accounts (e.g., Lenze et al., 2001) the relationship between self-reported ratings of general health predict response to depression treatment in older adults. Self-reported health independently accounts for treatment response (dropout and improvement) beyond other common predictors (e.g., demographic measures, depression severity, physical functioning, social functioning, medical comorbidities, personality factors, hopelessness, medication use, treatment side-effects, or treatment non-compliance). As health declines, older people are less responsive to depression treatment. Previous areas of functioning show a bi-directional effect; as depressive symptoms increase, functioning declines and as functioning improves, depressive symptoms decrease. Other variables such as perceptions of general health may be necessary to account for when delving into the relationship between depressive symptoms and physical functioning. That is, how a person feels about his/her health may be more important than actual health when we look further into the relationship.
4. Discussion
The current study is the first study to review and document the relationship between depressive symptoms and functional outcomes. We found that administration time had a statistically significant prediction of those correlations, however, we interpret these results with caution. Correlations present many methodological complications and likely result in weak inferences. Nevertheless, the overall modest correlations may be indicative of two things: 1) depressive symptom and functional outcome measures capture some common variance and 2) the unshared variance may indicate the importance of both measures. These results ought to be interpreted for their heuristic value and not as firm conclusions.
4.1. Artifacts affecting the relationship between symptom and function measures
Several methodological artifacts might help us better understand these correlations. First, a correlation is only meaningful if the scores possess a logical, psychometrically sound structure. Neither symptom nor functional outcome measure scores meet that criteria. Symptom measures typically produce non-unidimensional scores (i.e., factor analyses fail to find a single factor; Ruscio & Ruscio, 2000); functional outcome measures have the same problem (Bech, Lunde, & Unden, 2002). Thus, correlations of non-unidimensional scores are difficult to interpret and perhaps even less predictable.
Second, that difficulty may not just be a product of the instrument properties but also of the measured constructs and samples. Depressed samples are not always depressed; some may be suffering from loss or unabated sadness (Wakefield, Schmitz, First, & Horwitz, 2007). Combining depressed and non-depressed samples creates another opportunity to obscure the relationship. Comorbid medical conditions obscure it even further.
Third, response biases may artificially increase the correlations. Some argue (Morgado, Smith, Lecrubier, & Widlcher, 1991; Spielmans & McFall, 2006) that depressed people tend to respond negatively to most questions–symptom or function. That negative response bias would inflate the correlation between any measures. Multiple informants across all measures would help clarify the relationship (Möller, 2000).
Floor and ceiling effects may also inflate the correlation. A person can only respond affirmatively to depressive or negative symptoms–never a strong positive symptom that may indicate a buffer from depression. Thus, depressive symptom scores have a floor effect. Functional measures have the same but opposite effect. We only ask questions about mundane functioning (e.g., instrumental activities of daily living) as opposed to superior functioning (e.g., running marathons). Thus, a ceiling effect exists for functional measures. Those two effects combined lead to inflated correlations due simply to scaling properties (Torgerson, 1958).
Another scaling problem exists when converting continuous measures to binary values. Cut scores for symptom measures are routinely analyzed to determine optimal cut points that may indicate remission (e.g., Nemeroff, 2007). These binary scores–remitted versus unremitted–decrease statistical power (Cohen, 1983) and may introduce effects non-existent in the continuous scores (Maxwell & Delaney, 1993).
Sampling and research design may also affect the correlations summarized here. Most researchers focus on the already depressed; none study normal adults and follow them over long periods to assess both symptoms and functioning. One study (Tweed, 1993) analyzed from depression onset to long-term follow-up but that still conditions on these people being depressed at the onset. Thus, all studies begin with samples of depressed individuals. If we always condition on the consequence of depression then it will remain difficult to determine the nature of the relationship.
Finally, the correlation between symptoms and functioning may be affected by the scope of both measures. Broad measures capturing all aspects of depressive symptomatology or functional ability/impairment may produce stronger correlations than specific measures. This point may seem counter-intuitive since most of us think that broad measures might produce greater error variance, however, it is not error variance that necessarily gets inflated. As we mentioned previously, most symptom and functioning measures are multi-dimensional. The greater number of dimensions results in more variance–reliable variance related to many constructs. We capitalize on chance correlations when we have more constructs being measured. Hence, broader measures likely capture chance relationships rather than specific, interpretable relationships.
We acknowledge these artifacts and recognize that the summary correlations presented above may suffer from any or all. With that being said, we also recognize that all analyses suffer from these and other artifacts. Thus, our summary statistics are useful for heuristic purposes and ought to guide future clinical research.
According to our analyses, administration time predicted the relationship between depressive symptoms and functional outcomes. We want to emphasize that these results merely reflect a summary of the findings and not definitive, policy-guiding implications. For reasons that may stem from the artifacts above, administration time seems to be related to the magnitude of the correlation between symptom and functional measures. Correlations, however, indicate a relationship and so we caution readers to avoid over-interpreting those findings. What these relationships may imply is the potential for both direct and indirect paths leading from symptoms to functional impairment. We encourage researchers to look further into these relationships so we may better understand the change process.
4.2. Implications of potential bi-directional and lagged effects
No result from our study directly addresses either bi-directional or lagged effects but both effects require some attention because they may be relevant to our findings. The correlations we reported above reflect associations–not causes. Underlying those associations, however, may be a myriad of causal pathways. Specifically, the causal pathways likely lead from symptoms to impairment and vice versa (i.e., bi-directional). The bulk of the evidence for the bi-directional effect come from the social functioning literature but it is not unreasonable to expect a similar bi-directional effect for the other functional domains. Bi-directional effects would have little influence on our summary correlations since correlations have no inherent direction. In contrast, if the causal pathways underlying these correlations reflect more complicated effects such as lagged or indirect effects then these correlations merely scratch the surface of a complex web of causal effects. The correlations may mask the most important information about the relationship between symptoms and functioning. A lagged effect–if present–would likely attenuate the correlation between symptoms and functioning. Furthermore, if the effect between symptom change and functional change indeed lags then we might reconsider outcome measures in clinical trials. Symptom changes would represent the first opportunity to see change but not the most important aspect. Greater patience (i.e., long-term follow-up) would yield greater information about intervention effectiveness in changing patient functioning.
We acknowledge the potential for complex effects and maintain that there is greater promise for the combination of functional and symptom outcomes in clinical depression research. Both may be instrumental in our detailed understanding of the change process. In fact, meta-analyses might provide greater information for treatment assessment if they included functional outcomes along with symptom outcomes. Symptoms provide an early sign of treatment response where, perhaps, functional outcomes provide an indicator of meaningful change. Understanding which treatments produce changes in both may lead to greater discoveries in treatment development and evaluation.
4.3. Premorbid functioning
Another important aspect to consider with these correlations is premorbid functioning. Patients, for example, who have poor social functioning prior to depression onset may not show much functional improvement at all after treatment. Premorbid functioning, thus, may affect the correlations in unpredictable and, perhaps sample specific ways. To be confident our summarized correlations are not greatly affected by premorbid functioning, we would need to know the normative functioning for each domain–at a minimum–and the sample representativeness of those norms. A more preferable situation would be to have premorbid functioning recorded for each patient so that true changes may be correlated between symptoms and functioning. If there were a true bi-directional effect between functioning and symptoms then premorbid functioning would likely strengthen the correlations at baseline. We did not see that strengthening effect but the effect may still be present if there exists a lag between changes in functioning and depressive symptom. Thus, premorbid functioning stands as a relevant but omitted variable in our analysis and with that variable we might better untangle the underlying causal pathways.
Our collective understanding of the sequelae of functional impairment does not reach into the realm of depression. Thus, without that knowledge, we are unable to appreciate the role of premorbid functioning on depressive symptoms or post-treatment functioning. Most studies focus on depressive symptomatology and the consequences but few studies look at the precursors to depression. An exception to that statement is the ongoing work of Alloy, Abramson and colleagues (e.g., Alloy et al., 2000) who study cognitive vulnerabilities to depression. Perhaps there are vulnerabilities to depression that are not cognitive but rather functional. Future research ought to focus on assessing the potential vulnerabilities or predictive role pre-depression functioning may have on both depressive symptomatology as well as post-treatment functioning.
5. Conclusion
We focused on correlations between depressive symptom and functional outcome measures. While the results indicated a moderate correlation, other non-correlational work (e.g., Hays, Wells, Sherbourne, Rogers, & Spritzer, 1995) shows the impact of depression is equal to or worse than the impact of other chronic medical conditions (e.g., diabetes, hypertension, heart attack, and congestive heart failure) on general functional impairment. This review stepped through three specific aims to systematically analyze the current science supporting the measurement of functional impairment in depression outcome research. Accordingly, we documented the relationship between three functional domains and showed that these domains related moderately well with measures of depressive symptoms but not so well as to be seen as redundant. The relationship between symptoms and functioning is complicated, and we acknowledge the complications of including functional measures along with symptom measure when no clear model exists to indicate the underlying relationship. What might be clear from most of the previous research comparing symptoms and functioning is that the latter tends to be less responsive to treatment; thus, functional outcomes might lag behind symptom outcomes. We extended our discussion to advocate for more inclusion of functional outcome measures to improve clinical research. In summary, we encourage researchers to consider re-prioritizing their measure selection to ensure that the focus shifts away from mere symptom reduction in clinical outcomes research and more toward a comprehensive measurement model that includes functional outcomes. While the present article focuses on depression, the general points should apply to other mental disorders.
Acknowledgments
Patrick E. McKnight was supported by the National Institute of Arthritis, Musculoskeletal, and Skin Diseases R01-AR-047595. Todd B. Kashdan was supported by National Institute of Mental Health grant MH-73937.
Footnotes
The Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 1994) even explicitly states that most disorders must affect normal functioning in social, occupational, or other domains.
Correlations do not communicate the nature of the relationship between symptoms and functioning. Barnett and Gotlib (1988) distinguish between causal, concomitant and consequential variables to depression. These are difficult to distinguish in correlational studies so to ensure accuracy and precision in our language, we restrict our discussion to associations–correlations rather than causes. While our decision might weaken our argument, we hold that given the evidence to date, few relationships may be clearly defined. We work with the available data and provide an argument for what is missing and provide suggestions for future scientific inquiry.
References
- Abramson L, Metalsky G, Alloy L. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. The American Journal of Psychiatry. 2006 Sep;163(9):1569–1576. doi: 10.1176/appi.ajp.163.9.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agosti V. Predictors of persistent social impairment among recovered depressed outpatients. Journal of Affective Disorders. 1999 Oct;55(2–3):215–219. doi: 10.1016/s0165-0327(98)00200-6. [DOI] [PubMed] [Google Scholar]
- Agosti V. Residual symptoms and social functioning over six-months in recovered outpatients with chronic depression. Journal of Affective Disorders. 1999;52(1–3):251–255. doi: 10.1016/s0165-0327(98)00041-x. [DOI] [PubMed] [Google Scholar]
- Agosti V, Stewart JW. Social functioning and residual symptomatology among outpatients who responded to treatment and recovered from major depression. Journal of Affective Disorders. 1998 Jan;47(1–3):207–210. doi: 10.1016/s0165-0327(97)00119-5. [DOI] [PubMed] [Google Scholar]
- Aikens JE, Kroenke K, Nease DE, Klinkman MS, Sen A. Trajectories of improvement for six depression-related outcomes. General hospital psychiatry. 2008;30(1):26–31. doi: 10.1016/j.genhosppsych.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Airaksinen E, Wahlin A, Larsson M, Forsell Y. Cognitive and social functioning in recovery from depression: Results from a population-based three-year follow-up. Journal of Affective Disorders. 2006 Nov;96(1–2):107–110. doi: 10.1016/j.jad.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Allgöwer A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association. 2001 May;20(3):223–227. [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Hogan ME, Whitehouse WG, Rose DT, Robinson MS, et al. The Temple–Wisconsin Cognitive Vulnerability to Depression Project: Lifetime history of axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2000 Aug;109(3):403–418. [PubMed] [Google Scholar]
- Altshuler LL, Gitlin MJ, Mintz J, Leight KL, Frye MA. Subsyndromal depression is associated with functional impairment in patients with bipolar disorder. The Journal of Clinical Psychiatry. 2002 Sep;63(9):807–811. doi: 10.4088/jcp.v63n0910. [DOI] [PubMed] [Google Scholar]
- Altshuler L, Mintz J, Leight K. The Life Functioning Questionnaire (LFQ): A brief, gender-neutral scale assessing functional outcome. Psychiatry research. 2002 Oct;112(2):161–182. doi: 10.1016/s0165-1781(02)00180-4. [DOI] [PubMed] [Google Scholar]
- Aluoja A, Leinsalu M, Shlik J, Vasar V, Luuk K. Symptoms of depression in the Estonian population: Prevalence, sociodemographic correlates and social adjustment. Journal of Affective Disorders. 2004 Jan;78(1):27–35. doi: 10.1016/s0165-0327(02)00179-9. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR. 4. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- Arvey RD, Murphy KR. Performance evaluation in work settings. Annual Review of Psychology. 1998;49:141–168. doi: 10.1146/annurev.psych.49.1.141. [DOI] [PubMed] [Google Scholar]
- Baldwin DS. Unmet needs in the pharmacological management of depression. Human psychopharmacology. 2001 Dec;16(S2):S93–S99. doi: 10.1002/hup.337. [DOI] [PubMed] [Google Scholar]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: Distinguishing among antecedents, concomitants, and consequences. Psychological Bulletin. 1988 Jul;104(1):97–126. doi: 10.1037/0033-2909.104.1.97. [DOI] [PubMed] [Google Scholar]
- Bearden CE, Glahn DC, Monkul ES, Barrett J, Najt P, Villarreal V, et al. Patterns of memory impairment in bipolar disorder and unipolar major depression. Psychiatry Research. 2006 Jun;142(2–3):139–150. doi: 10.1016/j.psychres.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Bech P. Quality of life in the psychiatric patient. London: Mosby-Wolfe; 1998. [Google Scholar]
- Bech P. Social functioning: Should it become an endpoint in trials of antidepressants? CNS drugs. 2005;19(4):313–324. doi: 10.2165/00023210-200519040-00004. [DOI] [PubMed] [Google Scholar]
- Bech P, Lunde M, Unden M. Social Adaptation Self-Evaluation Scale (SASS): Psychometric analysis as outcome measure in the treatment of patients with major depression in the remission phase. International Journal of Psychiatry in Clinical Practice. 2002;6(3):141–146. doi: 10.1080/136515002760276063. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961 Jun;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benazzi F. A 10-item Hamilton Depression Rating Scale to measure major depressive episode severity in outpatients. International journal of geriatric psychiatry. 1998 Aug;13(8):570–571. doi: 10.1002/(sici)1099-1166(199808)13:8<570::aid-gps813>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Bennett KJ, Torrance GW, Boyle MH, Guscott R. Cost–utility analysis in depression: The Mcsad utility measure for depression health states. Psychiatric Services (Washington, D.C) 2000 Sep;51(9):1171–1176. doi: 10.1176/appi.ps.51.9.1171. [DOI] [PubMed] [Google Scholar]
- Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Kornstein SG, Miller IM, et al. Lost human capital from early-onset chronic depression. The American Journal of Psychiatry. 2000 Jun;157(6):940–947. doi: 10.1176/appi.ajp.157.6.940. [DOI] [PubMed] [Google Scholar]
- Berry C, Ones D, Sackett P. Interpersonal deviance, organizational deviance, and their common correlates: A review and meta-analysis. Journal of Applied Psychology. 2007;92:410–424. doi: 10.1037/0021-9010.92.2.410. [DOI] [PubMed] [Google Scholar]
- Bommer W, Johnson J, Rich G, Podsakoff P, MacKenzie S. On the interchangeability of objective and subjective measures of employee performance: A meta-analysis. Personnel Psychology. 1995;48:587–605. [Google Scholar]
- Booth BM, Zhang M, Rost KM, Clardy JA, Smith LG, Smith GR. Measuring outcomes and costs for major depression. Psychopharmacology Bulletin. 1997;33(4):653–658. [PubMed] [Google Scholar]
- Bosc M, Dubini A, Polin V. Development and validation of a social functioning scale, the social adaptation self-evaluation scale. European neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology. 1997 Apr;7(Suppl 1):S57–S70. doi: 10.1016/s0924-977x(97)00420-3. discussion S71-3. [DOI] [PubMed] [Google Scholar]
- Bothwell S, Weissman MM. Social impairments four years after an acute depressive episode. The American Journal of Orthopsychiatry. 1977 Apr;47(2):231–237. doi: 10.1111/j.1939-0025.1977.tb00978.x. [DOI] [PubMed] [Google Scholar]
- Bromberger JT, Kravitz HM, Wei H-L, Brown C, Youk AO, Cordal A, et al. History of depression and women’s current health and functioning during midlife. General Hospital Psychiatry. 2005;27(3):200–208. doi: 10.1016/j.genhosppsych.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Bronisch T, Hecht H. Major depression with and without a coexisting anxiety disorder: Social dysfunction, social integration, and personality features. Journal of Affective Disorders. 1990 Nov;20(3):151–157. doi: 10.1016/0165-0327(90)90138-x. [DOI] [PubMed] [Google Scholar]
- Brown WJ, Ford JH, Burton NW, Marshall AL, Dobson AJ. Prospective study of physical activity and depressive symptoms in middle-aged women. American Journal of Preventive Medicine. 2005 Nov;29(4):265–272. doi: 10.1016/j.amepre.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Buist-Bouwman MA, Ormel J, de Graaf R, Vollebergh WAM. Functioning after a major depressive episode: Complete or incomplete recovery? Journal of Affective Disorders. 2004 Nov;82(3):363–371. doi: 10.1016/j.jad.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Burton WN, Conti DJ, Chen CY, Schultz AB, Edington DW. The role of health risk factors and disease on worker productivity. Journal of Occupational and Environmental Medicine / American College of Occupational and Environmental Medicine. 1999 Oct;41(10):863–877. doi: 10.1097/00043764-199910000-00007. [DOI] [PubMed] [Google Scholar]
- Cesari M, Onder G, Russo A, Zamboni V, Barillaro C, Ferrucci L, et al. Comorbidity and physical function: Results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study) Gerontology. 2006;52(1):24–32. doi: 10.1159/000089822. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Sanderson K, Ayuso-Mateos JL, Saxena S. Reducing the global burden of depression: Population-level analysis of intervention cost-effectiveness in 14 world regions. British Journal of Psychiatry: The Journal of Mental Science. 2004 May;184:393–403. doi: 10.1192/bjp.184.5.393. [DOI] [PubMed] [Google Scholar]
- Christensen L, Duncan K. Distinguishing depressed from nondepressed individuals using energy and psychosocial variables. Journal of Consulting and Clinical Psychology. 1995 Jun;63(3):495–498. doi: 10.1037//0022-006x.63.3.495. [DOI] [PubMed] [Google Scholar]
- Clare AW, Cairns VE. Design, development and use of a standardized interview to assess social maladjustment and dysfunction in community studies. Psychological Medicine. 1978 Nov;8(4):589–604. doi: 10.1017/s0033291700018808. [DOI] [PubMed] [Google Scholar]
- Cohen J. The cost of dichotomization. Applied Psychological Measurement. 1983;7:249–253. [Google Scholar]
- Collins J, Baase C, Sharda C, Ozminkowski R, Nicholson S, Billotti G, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine. 2005 Jun;47(6):547–557. doi: 10.1097/01.jom.0000166864.58664.29. [DOI] [PubMed] [Google Scholar]
- Conradi HJ, de Jonge P, Ormel J. Prediction of the three-year course of recurrent depression in primary care patients: Different risk factors for different outcomes. Journal of Affective Disorders. 2008 Jan;105(1–3):267–271. doi: 10.1016/j.jad.2007.04.017. [DOI] [PubMed] [Google Scholar]
- Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. The American Journal of Psychiatry. 1993 May;150(5):720–727. doi: 10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodriguez E. Treating depressed primary care patients improves their physical, mental, and social functioning. Archives of Internal Medicine. 1997 May;157(10):1113–1120. [PubMed] [Google Scholar]
- Coyne JC. Depression and the response of others. Journal of Abnormal Psychology. 1976 Apr;85(2):186–193. doi: 10.1037//0021-843x.85.2.186. [DOI] [PubMed] [Google Scholar]
- Coyne JC. Self-reported distress: Analog or Ersatz depression? Psychological Bulletin. 1994 Jul;116(1):29–45. doi: 10.1037/0033-2909.116.1.29. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Downey G. Social factors and psychopathology: Stress, social support, and coping processes. Annual Review of Psychology. 1991;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Thompson R, Palmer SC. Marital quality, coping with conflict, marital complaints, and affection in couples with a depressed wife. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2002 Mar;16(1):26–37. doi: 10.1037//0893-3200.16.1.26. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K. Depression: Perspectives from affective neuroscience. Annual review of psychology. 2002;53:545–574. doi: 10.1146/annurev.psych.53.100901.135148. [DOI] [PubMed] [Google Scholar]
- Davidson J, Zisook S, Giller E, Helms M. Symptoms of interpersonal sensitivity in depression. Comprehensive Psychiatry. 1989;30(5):357–368. doi: 10.1016/0010-440x(89)90001-1. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale–preliminary report. Psychopharmacology Bulletin. 1973 Jan;9(1):13–28. [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974 Jan;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels R, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist, a measure of primary symptom dimensions. In: Pichot P, editor. Psychological measurements in psychopharmacology: Problems in pharmacopsychiatry. 7. Basel, Switzerland: Kargerman; 1974. pp. 79–110. [DOI] [PubMed] [Google Scholar]
- Desha LN, Ziviani JM, Nicholson JM, Martin G, Darnell RE. Physical activity and depressive symptoms in American adolescents. Journal of sport & exercise psychology. 2007 Aug;29(4):534–543. doi: 10.1123/jsep.29.4.534. [DOI] [PubMed] [Google Scholar]
- Diener E, Seligman MEP. Very happy people. Psychological Science: A Journal of the American Psychological Society / APS. 2002 Jan;13(1):81–84. doi: 10.1111/1467-9280.00415. [DOI] [PubMed] [Google Scholar]
- Donohue JM, Pincus HA. Reducing the societal burden of depression: A review of economic costs, quality of care and effects of treatment. PharmacoEconomics. 2007;25(1):7–24. doi: 10.2165/00019053-200725010-00003. ILL requested. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a major U.S. corporation. The American Journal of Psychiatry. 2000 Aug;157(8):1274–1278. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- Dubini A, Bosc M, Polin V. Do noradrenaline and serotonin differentially affect social motivation and behaviour? European neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology. 1997 Apr;7(Suppl 1):S49–S55. doi: 10.1016/s0924-977x(97)00419-7. discussion S71-3. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J. Endicott Work Productivity Scale (EWPS): A new measure to assess treatment effects. Psychopharmacology bulletin. 1997;33(1):13–16. [PubMed] [Google Scholar]
- Faravelli C, Servi P, Arends JA, Strik WK. Number of symptoms, quantification, and qualification of depression. Comprehensive Psychiatry. 1996;37(5):307–315. doi: 10.1016/s0010-440x(96)90011-5. [DOI] [PubMed] [Google Scholar]
- Frasure-Smith N, Lespérance F. Recent evidence linking coronary heart disease and depression. Canadian Journal of Psychiatry Revue Canadienne de Psychiatrie. 2006 Oct;51(12):730–737. doi: 10.1177/070674370605101202. [DOI] [PubMed] [Google Scholar]
- Fu CH, Reed LJ, Meyer JH, Kennedy S, Houle S, Eisfeld BS, et al. Noradrenergic dysfunction in the prefrontal cortex in depression: An [15O] H2O PET study of the neuromodulatory effects of clonidine. Biological Psychiatry. 2001 Feb;49(4):317–325. doi: 10.1016/s0006-3223(00)01050-7. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Akechi T, Azuma H, Okuyama T, Higuchi T. Evidence-based guidelines for interpretation of the Hamilton Rating Scale for Depression. Journal of Clinical Psychopharmacology. 2007 Oct;27(5):531–534. doi: 10.1097/JCP.0b013e31814f30b1. [DOI] [PubMed] [Google Scholar]
- Fukukawa Y, Nakashima C, Tsuboi S, Kozakai R, Doyo W, Niino N, et al. Age differences in the effect of physical activity on depressive symptoms. Psychology and Aging. 2004 Jun;19(2):346–351. doi: 10.1037/0882-7974.19.2.346. [DOI] [PubMed] [Google Scholar]
- Günther OH, Roick C, Angermeyer MC, König H-H. The responsiveness of EQ-5D utility scores in patients with depression: A comparison with instruments measuring quality of life, psychopathology and social functioning. Journal of Affective Disorders. 2008 Jan;105(1–3):81–91. doi: 10.1016/j.jad.2007.04.018. [DOI] [PubMed] [Google Scholar]
- Goeleven E, Raedt RD, Baert S, Koster EHW. Deficient inhibition of emotional information in depression. Journal of Affective Disorders. 2006 Jul;93(1–3):149–157. doi: 10.1016/j.jad.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: A review of measures of social functioning. The American Journal of Psychiatry. 1992 Sep;149(9):1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. Depression and associated physical diseases and symptoms. Dialogues in Clinical Neuroscience. 2006;8(2):259–265. doi: 10.31887/DCNS.2006.8.2/mgoodwin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. Journal of General Internal Medicine : Official Journal of the Society for Research and Education in Primary Care Internal Medicine. 2004 Aug;19(8):813–818. doi: 10.1111/j.1525-1497.2004.30531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, et al. The economic burden of depression in the United States: How did it change between 1990 and 2000? The Journal of Clinical Psychiatry. 2003 Dec;64(12):1465–1475. doi: 10.4088/jcp.v64n1211. requested through ILL. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Stiglin LE, Finkelstein SN, Berndt ER. The economic burden of depression in 1990. The Journal of Clinical Psychiatry. 1993 Nov;54(11):405–418. [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960 Feb;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Jylha M. Improvement in depressive symptoms and changes in self-rated health among community-dwelling disabled older adults. Aging & Mental Health. 2006 Nov;10(6):599–605. doi: 10.1080/13607860600641077. [DOI] [PubMed] [Google Scholar]
- Hannula JA, Lahtela K, Järvikoski A, Salminen JK, Mäkelä P. Occupational Functioning Scale (OFS)–An instrument for assessment of work ability in psychiatric disorders. Nordic Journal of Psychiatry. 2006;60(5):372–378. doi: 10.1080/08039480600937140. [DOI] [PubMed] [Google Scholar]
- Hatfield E, Cacioppo J, Rapson R. Emotional contagion. New York: Cambridge University Press; 1994. [Google Scholar]
- Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Archives of General Psychiatry. 1995 Jan;52(1):11–19. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- Hecht H, Wittchen HU. The frequency of social dysfunction in a general population sample and in patients with mental disorders. A comparison using the social interview schedule (sis) Social Psychiatry and Psychiatric Epidemiology. 1988 Jan;23(1):17–29. doi: 10.1007/BF01788438. [DOI] [PubMed] [Google Scholar]
- Hecht H, von Zerssen D, Krieg C, Pössl J, Wittchen HU. Anxiety and depression: Comorbidity, psychopathology, and social functioning. Comprehensive Psychiatry. 1989;30(5):420–433. doi: 10.1016/0010-440x(89)90008-4. [DOI] [PubMed] [Google Scholar]
- Hecht H, von Zerssen D, Wittchen HU. Anxiety and depression in a community sample: The influence of comorbidity on social functioning. Journal of Affective Disorders. 1990 Feb;18(2):137–144. doi: 10.1016/0165-0327(90)90070-o. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R, Dunner D, Keitner G, Klein D, Koran L, Kornstein S, et al. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biological Psychiatry. 2002 Jan;51(2):123–133. doi: 10.1016/s0006-3223(01)01291-4. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R, Montgomery S, Keller M, Kasper S, Schatzberg A, Moller H, et al. Social functioning in depression: A review. The Journal of Clinical Psychiatry. 2000 Apr;61(4):268–275. doi: 10.4088/jcp.v61n0405. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988 Dec;56(6):885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Hylan TR, Buesching DP, Tollefson GD. Health economic evaluations of antidepressants: A review. Depression and anxiety. 1998;7(2):53–64. [PubMed] [Google Scholar]
- Jansen NWH, Kant IJ, van den Brandt PA. Need for recovery in the working population: Description and associations with fatigue and psychological distress. International Journal of Behavioral Medicine. 2002;9(4):322–340. doi: 10.1207/s15327558ijbm0904_03. [DOI] [PubMed] [Google Scholar]
- Joiner T. Depression’s vicious scree: Self-propagatory and erosive factors in depression chronicity. Clinical Psychology: Science & Practice. 2000;7:203–218. [Google Scholar]
- Joiner T, Katz J. Contagion of depressive symptoms and mood: Meta-analytic review and explanations from cognitive, behavioral, and interpersonal viewpoints. Clinical Psychology: Science and Practice. 1999;6:149–164. [Google Scholar]
- Jones MT, Cockrum PC. A critical review of published economic modelling studies in depression. PharmacoEconomics. 2000 Jun;17(6):555–583. doi: 10.2165/00019053-200017060-00003. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ, Paulus M, Leon AC, Maser JD, et al. Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry. 2000 Apr;57(4):375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. The American Journal of Psychiatry. 1996 Nov;153(11):1411–1417. doi: 10.1176/ajp.153.11.1411. [DOI] [PubMed] [Google Scholar]
- Judd LL, Rapaport MH, Yonkers KA, Rush AJ, Frank E, Thase ME, et al. Randomized, placebo-controlled trial of fluoxetine for acute treatment of minor depressive disorder. The American Journal of Psychiatry. 2004 Oct;161(10):1864–1871. doi: 10.1176/ajp.161.10.1864. [DOI] [PubMed] [Google Scholar]
- Kasper S. From symptoms to social functioning: differential effects of antidepressant therapy. International clinical psychopharmacology. 1999 May;14(Suppl 1):S27–S31. doi: 10.1097/00004850-199905001-00006. [DOI] [PubMed] [Google Scholar]
- Kassam A, Patten SB. Major depression, fibromyalgia and labour force participation: A population-based cross-sectional study. BMC Musculoskeletal Disorders. 2006;7:4. doi: 10.1186/1471-2474-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzelnick DJ, Kobak KA, Greist JH, Jefferson JW, Henk HJ. Effect of primary care treatment of depression on service use by patients with high medical expenditures. Psychiatric Services (Washington, D.C) 1997 Jan;48(1):59–64. doi: 10.1176/ps.48.1.59. [DOI] [PubMed] [Google Scholar]
- Kawada T, Katsumata M, Suzuki H, Shimizu T. Actigraphic predictors of the depressive state in students with no psychiatric disorders. Journal of Affective Disorders. 2007 Feb;98(1–2):117–120. doi: 10.1016/j.jad.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Keltner D, Kring A. Emotion, social function, and psychopathology. Review of General Psychology. 1998;2:320–342. [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7:171–185. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, et al. Depression in the workplace: Effects on short-term disability. Health Affairs (Project Hope) 1999;18(5):163–171. doi: 10.1377/hlthaff.18.5.163. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA : the journal of the American Medical Association. 2003 Jun;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994 Jan;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kivelä SL. Depression and physical and social functioning in old age. Acta Psychiatrica Scandinavica Supplementum. 1994;377:73–76. doi: 10.1111/j.1600-0447.1994.tb05806.x. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Schatzberg A, Rush AJ, Klein DN, Howland R, Gniwesch L, et al. Psychosocial outcomes following long-term, double-blind treatment of chronic depression with sertraline vs placebo. Archives of General Psychiatry. 2002 Aug;59(8):723–728. doi: 10.1001/archpsyc.59.8.723. [DOI] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Tuovinen T, Honkalampi K, Antikainen R, Hintikka J, Haatainen K, et al. Mental health and well-being in a 6-year follow-up of patients with depression : Assessments of patients and clinicians. Social Psychiatry and Psychiatric Epidemiology. 2008;43(9):688–696. doi: 10.1007/s00127-008-0353-x. [DOI] [PubMed] [Google Scholar]
- Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, et al. Stanford presenteeism scale: Health status and employee productivity. Journal of Occupational and Environmental Medicine / American College of Occupational and Environmental Medicine. 2002 Jan;44(1):14–20. doi: 10.1097/00043764-200201000-00004. [DOI] [PubMed] [Google Scholar]
- Korff MV, Katon W, Rutter C, Ludman E, Simon G, Lin E, et al. Effect on disability outcomes of a depression relapse prevention program. Psychosomatic Medicine. 2003;65(6):938–943. doi: 10.1097/01.psy.0000097336.95046.0c. [DOI] [PubMed] [Google Scholar]
- Kramer TL, Smith GR, Maruish ME. Major depressive disorder: Assessing the spectrum of symptoms and functional impairment at treatment entry and follow-up. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment, 3rd ed Instruments for adults, Vol. 3. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2004. pp. 293–311. [Google Scholar]
- Lenze EJ, Miller MD, Dew MA, Martire LM, Mulsant BH, Begley AE, et al. Subjective health measures and acute treatment outcomes in geriatric depression. International Journal of Geriatric Psychiatry. 2001 Dec;16(12):1149–1155. doi: 10.1002/gps.503. [DOI] [PubMed] [Google Scholar]
- Leon AC, Walkup JT, Portera L. Assessment and treatment of depression in disability claimants: A cost–benefit simulation study. The Journal of Nervous and Mental Disease. 2002 Jan;190(1):3–9. doi: 10.1097/00005053-200201000-00002. [DOI] [PubMed] [Google Scholar]
- Leppänen JM. Emotional information processing in mood disorders: A review of behavioral and neuroimaging findings. Current Opinion in Psychiatry. 2006 Jan;19(1):34–39. doi: 10.1097/01.yco.0000191500.46411.00. [DOI] [PubMed] [Google Scholar]
- Lerner D, Adler DA, Chang H, Lapitsky L, Hood MY, Perissinotto C, et al. Unemployment, job retention, and productivity loss among employees with depression. Psychiatric Services (Washington, D.C) 2004 Dec;55(12):1371–1378. doi: 10.1176/appi.ps.55.12.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner D, Amick BC, Lee JC, Rooney T, Rogers WH, Chang H, et al. Relationship of employee-reported work limitations to work productivity. Medical Care. 2003 May;41(5):649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- Lerner D, Amick BC, Rogers WH, Malspeis S, Bungay K, Cynn D. The work limitations questionnaire. Medical Care. 2001 Jan;39(1):72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- Levin R, Heller W, Mohanty A, Herrington J, Miller G. Cognitive deficits in depression and functional specificity of regional brain activity. Cognitive Therapy and Research. 2007;31:211–233. [Google Scholar]
- Lewinsohn PM, Graf M. Pleasant activities and depression. Journal of Consulting and Clinical Psychology. 1973 Oct;41(2):261–268. doi: 10.1037/h0035142. [DOI] [PubMed] [Google Scholar]
- Lisio GD, Maremmani I, Perugi G, Cassano GB, Deltito J, Akiskal HS. Impairment of work and leisure in depressed outpatients. A preliminary communication. Journal of Affective Disorders. 1986;10(2):79–84. doi: 10.1016/0165-0327(86)90029-7. [DOI] [PubMed] [Google Scholar]
- Lynch W, Riedel J. Measuring employee productivity: A guide to self-assessment tools. Scottsdale, AZ: Institute for Health and Productivity Management; 2001. [Google Scholar]
- Marcus B, Schuler H, Quell P, Hömpfer G. Measuring counterproductivity: Development and initial validation of a German self-report questionnaire. International Journal of Selection and Assessment. 2002;10(1):18–35. [Google Scholar]
- Marks I. Behavioural psychotherapy: Maudsley pocketbook of clinical management. Bristol, UK: John Wright; 1986. [Google Scholar]
- Mauskopf JA, Simeon GP, Miles MA, Westlund RE, Davidson JR. Functional status in depressed patients: The relationship to disease severity and disease resolution. The Journal of Clinical Psychiatry. 1996 Dec;57(12):588–592. doi: 10.4088/jcp.v57n1207. [DOI] [PubMed] [Google Scholar]
- Maxwell S, Delaney H. Bivariate median splits and spurious statistical significance. Psychological Bulletin. 1993;113:181–190. [Google Scholar]
- McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical care. 1994 Jan;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Konarski JZ, Mancini DA, Zurowski M, Giacobbe P, Soczynska JK, et al. Improving outcomes in depression: A focus on somatic symptoms. Journal of Psychosomatic Research. 2006 Mar;60(3):279–282. doi: 10.1016/j.jpsychores.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Möller HJ. Rating depressed patients: Observer- vs self-assessment. European psychiatry : The Journal of the Association of European Psychiatrists. 2000 May;15(3):160–172. doi: 10.1016/s0924-9338(00)00229-7. [DOI] [PubMed] [Google Scholar]
- Möller H-J, Demyttenaere K, Sacchetti E, Rush AJ, Montgomery SA. Improving the chance of recovery from the short- and long-term consequences of depression. International Clinical Psychopharmacology. 2003 Jul;18(4):219–225. doi: 10.1097/00004850-200307000-00004. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. The British Journal of Psychiatry : The Journal of Mental Science. 1979 Apr;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Moos RH, Cronkite RC, Moos BS. Family and extrafamily resources and the 10-year course of treated depression. Journal of Abnormal Psychology. 1998 Aug;107(3):450–460. doi: 10.1037//0021-843x.107.3.450. [DOI] [PubMed] [Google Scholar]
- Morgado A, Smith M, Lecrubier Y, Widlöcher D. Depressed subjects unwittingly overreport poor social adjustment which they reappraise when recovered. The Journal of Nervous and Mental Disease. 1991 Oct;179(10):614–619. doi: 10.1097/00005053-199110000-00005. [DOI] [PubMed] [Google Scholar]
- Mulder RT, Joyce PR, Frampton C. Relationships among measures of treatment outcome in depressed patients. Journal of Affective Disorders. 2003 Sep;76(1–3):127–135. doi: 10.1016/s0165-0327(02)00080-0. [DOI] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, Greist JH. The work and social adjustment scale: A simple measure of impairment in functioning. The British Journal of Psychiatry : The Journal of Mental Science. 2002 May;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Myers D, Diener E. Who is happy? Psychological Science. 1995;6:10–19. [Google Scholar]
- Nemeroff CB. The burden of severe depression: A review of diagnostic challenges and treatment alternatives. Journal of Psychiatric Research. 2007;41(3–4):189–206. doi: 10.1016/j.jpsychires.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Nezlek J, Hampton C, Shean G. Clinical depression and day-to-day social interaction in a community sample. Journal of Abnormal Psychology. 2000 Feb;109(1):11–19. doi: 10.1037//0021-843x.109.1.11. [DOI] [PubMed] [Google Scholar]
- Nickel M, Nickel C, Lahmann C, Mitterlehner F, Tritt K, Leiberich PK, et al. Recovering the ability to function socially in elderly depressed patients: A prospective, controlled trial. Archives of Gerontology and Geriatrics. 2005;41(1):41–49. doi: 10.1016/j.archger.2004.11.001. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Rehm LP. Self-monitoring, activity levels, and mood in the development and maintenance of depression. Journal of Abnormal Psychology. 1979 Aug;88(4):450–453. [PubMed] [Google Scholar]
- Papakostas GI, Petersen T, Denninger JW, Tossani E, Pava JA, Alpert JE, et al. Psychosocial functioning during the treatment of major depressive disorder with fluoxetine. Journal of Clinical Psychopharmacology. 2004 Oct;24(5):507–511. doi: 10.1097/01.jcp.0000138761.85363.d5. [DOI] [PubMed] [Google Scholar]
- Pardo JV, Pardo PJ, Humes SW, Posner MI. Neurocognitive dysfunction in antidepressant-free, non-elderly patients with unipolar depression: Alerting and covert orienting of visuospatial attention. Journal of Affective Disorders. 2006 May;92(1):71–78. doi: 10.1016/j.jad.2005.12.037. [DOI] [PubMed] [Google Scholar]
- Parker G, Roussos J, Hadzi-Pavlovic D, Wilhelm K, Mitchell P, Austin MP. Plumbing the depths: Some problems in quantifying depression severity. Journal of Affective Disorders. 1997 Jan;42(1):49–58. doi: 10.1016/s0165-0327(96)00097-3. [DOI] [PubMed] [Google Scholar]
- Paykel E. Social functioning and the depressed patient. International Journal of Psychiatry in Clinical Practice. 1999;3(1):S9–S11. [Google Scholar]
- Paykel E, Weissman M, Prusoff B, Tonks C. Dimensions of social adjustment in depressed women. The Journal of Nervous and Mental Disease. 1971 Mar;152(3):158–172. doi: 10.1097/00005053-197103000-00002. [DOI] [PubMed] [Google Scholar]
- Penninx B, Guralnik J, Ferrucci L, Simonsick E, Deeg D, Wallace R. Depressive symptoms and physical decline in community-dwelling older persons. JAMA : The Journal of the American Medical Association. 1998 Jun;279(21):1720–1726. doi: 10.1001/jama.279.21.1720. [DOI] [PubMed] [Google Scholar]
- Penninx B, Rejeski W, Pandya J, Miller M, DiBari M, Applegate W, et al. Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2002 Mar;57(2):P124–P132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- Petty SC, Sachs-Ericsson N, Joiner TE. Interpersonal functioning deficits: temporary or stable characteristics of depressed individuals? Journal of Affective Disorders. 2004 Aug;81(2):115–122. doi: 10.1016/S0165-0327(03)00158-7. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ranjith G, Farmer A, McGuffin P, Cleare AJ. Personality as a determinant of social functioning in depression. Journal of Affective Disorders. 2005 Jan;84(1):73–76. doi: 10.1016/j.jad.2004.10.008. [DOI] [PubMed] [Google Scholar]
- Rehm J, Ustun T, Saxena S, Nelson CB, Chatterji S, Ivis F, et al. On the development and psychometric testing of the WHO screening instrument to assess disablement in the general population. International Journal of Methods in Psychiatric Research. 1999;8:110–123. [Google Scholar]
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993 Nov;4(5):353–365. doi: 10.2165/00019053-199304050-00006. ILL request. [DOI] [PubMed] [Google Scholar]
- Rice DP, Miller LS. The economic burden of affective disorders. The British journal of psychiatry(Supplement(27)) 1995 Apr;:34–42. [PubMed] [Google Scholar]
- Robinson RG. Neuropsychiatric consequences of stroke. Annual review of medicine. 1997;48:217–229. doi: 10.1146/annurev.med.48.1.217. [DOI] [PubMed] [Google Scholar]
- Rose EJ, Ebmeier KP. Pattern of impaired working memory during major depression. Journal of Affective Disorders. 2006 Feb;90(2–3):149–161. doi: 10.1016/j.jad.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Rost K, Smith JL, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity. A randomized trial. Medical Care. 2004 Dec;42(12):1202–1210. doi: 10.1097/00005650-200412000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio J, Ruscio AM. Informing the continuity controversy: A taxometric analysis of depression. Journal of Abnormal Psychology. 2000 Aug;109(3):473–487. [PubMed] [Google Scholar]
- Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C. The Inventory for Depressive Symptomatology (IDS): Preliminary findings. Psychiatry Research. 1986 May;18(1):65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine. 1996 May;26(3):477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003 Sep;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Russo A, Cesari M, Onder G, Zamboni V, Barillaro C, Pahor M, et al. Depression and physical function: Results from the aging and longevity study in the sirente geographic area (ilSIRENTE study) Journal of Geriatric Psychiatry and Neurology. 2007 Sep;20(3):131–137. doi: 10.1177/0891988707301865. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, et al. Depression is associated with cardiac symptoms, mortality risk, and hospitalization among women with suspected coronary disease: The NHLBI-sponsored WISE study. Psychosomatic medicine. 2006;68(2):217–223. doi: 10.1097/01.psy.0000195751.94998.e3. [DOI] [PubMed] [Google Scholar]
- Rytsälä HJ, Melartin TK, Leskelä US, Lestelä-Mielonen PS, Sokero TP, Isometsä ET. Determinants of functional disability and social adjustment in major depressive disorder: A prospective study. The Journal of nervous and mental disease. 2006 Aug;194(8):570–576. doi: 10.1097/01.nmd.0000230394.21345.c4. [DOI] [PubMed] [Google Scholar]
- Rytsälä HJ, Melartin TK, Leskelä US, Sokero TP, Lestelä-Mielonen PS, Isometsä ET. Functional and work disability in major depressive disorder. The Journal of Nervous and Mental Disease. 2005 Mar;193(3):189–195. doi: 10.1097/01.nmd.0000154837.49247.96. [DOI] [PubMed] [Google Scholar]
- Sasso ATL, Rost K, Beck A. Modeling the impact of enhanced depression treatment on workplace functioning and costs: A cost-benefit approach. Medical Care. 2006 Apr;44(4):352–358. doi: 10.1097/01.mlr.0000204049.30620.1e. [DOI] [PubMed] [Google Scholar]
- Schooler N, Hogarty G, Weissman M. Social adjustment scale II. In: Hargreaves W, Attkisson C, Sorenson J, editors. Resource materials for community mental health program evaluators (publication no adm 79-328) Washington, DC: US Departmtne of Health, Education, and Welfare; 1979. pp. 290–330. [Google Scholar]
- Scott J, Teasdale JD, Paykel ES, Johnson AL, Abbott R, Hayhurst H, et al. Effects of cognitive therapy on psychological symptoms and social functioning in residual depression. The British Journal of Psychiatry: The Journal of Mental Science. 2000 Nov;177:440–446. doi: 10.1192/bjp.177.5.440. [DOI] [PubMed] [Google Scholar]
- Segrin C, Abramson LY. Negative reactions to depressive behaviors: A communication theories analysis. Journal of Abnormal Psychology. 1994 Nov;103(4):655–668. doi: 10.1037//0021-843x.103.4.655. [DOI] [PubMed] [Google Scholar]
- Seivewright H, Tyrer P, Johnson T. Persistent social dysfunction in anxious and depressed patients with personality disorder. Acta psychiatrica Scandinavica. 2004 Feb;109(2):104–109. doi: 10.1046/j.1600-0447.2003.00241.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. International Clinical Psychopharmacology. 1996 Jun;11(Suppl 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- Sheehan KH, Sheehan DV. Assessing treatment effects in clinical trials with the Discan metric of the Sheehan disability scale. International Clinical psychopharmacology. 2008 Mar;23(2):70–83. doi: 10.1097/YIC.0b013e3282f2b4d6. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Keller MB, Gelenberg A, Dunner DL, Hirschfeld R, Thase ME, et al. Effectiveness of St John’s wort in major depression: A randomized controlled trial. JAMA : The Journal of the American Medical Association. 2001 Apr;285(15):1978–1986. doi: 10.1001/jama.285.15.1978. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Hays RD, Wells KB. Personal and psychosocial risk factors for physical and mental health outcomes and course of depression among depressed patients. Journal of Consulting and Clinical Psychology. 1995 Jun;63(3):345–355. doi: 10.1037//0022-006x.63.3.345. [DOI] [PubMed] [Google Scholar]
- Simon GE, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, et al. Depression and work productivity: The comparative costs of treatment versus nontreatment. Journal of Occupational and Environmental Medicine /American College of Occupational and Environmental Medicine. 2001 Jan;43(1):2–9. doi: 10.1097/00043764-200101000-00002. [DOI] [PubMed] [Google Scholar]
- Simon GE, Katon WJ, VonKorff M, Unützer J, Lin EH, Walker EA, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. The American Journal of Psychiatry. 2001 Oct;158(10):1638–1644. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]
- Simon GE, Korff MV, Lin E. Clinical and functional outcomes of depression treatment in patients with and without chronic medical illness. Psychological Medicine. 2005 Feb;35(2):271–279. doi: 10.1017/s0033291704003071. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Grilo CM, Pagano ME, Bender DS, Gunderson JG, Shea MT, et al. Effects of personality disorders on functioning and well-being in major depressive disorder. Journal of Psychiatric Practice. 2005 Nov;11(6):363–368. doi: 10.1097/00131746-200511000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P, Kendall L. Retranslation of expectations: An approach to the construction of unambiguous anchors for rating scales. Journal of Applied Psychology. 1963;47:149–155. [Google Scholar]
- Smith J, Rost K, Nutting P, Libby A, Elliott C, Pyne J. Impact of primary care depression intervention on employment and workplace conflict outcomes: is value added? The Journal of Mental Health Policy and Economics. 2002 Mar;5(1):43–49. [PubMed] [Google Scholar]
- Spanier G. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spielmans GI, McFall JP. A comparative meta-analysis of clinical global impressions change in antidepressant trials. The Journal of Nervous and Mental Disease. 2006 Nov;194(11):845–852. doi: 10.1097/01.nmd.0000244554.91259.27. [DOI] [PubMed] [Google Scholar]
- Spijker J, Graaf R, Bijl RV, Beekman ATF, Ormel J, Nolen WA. Functional disability and depression in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (nemesis) Acta psychiatrica Scandinavica. 2004 Sep;110(3):208–214. doi: 10.1111/j.1600-0447.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992 Aug;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Staten LK, Taren DL, Howell WH, Tobar M, Poehlman ET, Hill A, et al. Validation of the Arizona Activity Frequency Questionnaire using doubly labeled water. Medicine and Science in Sports and Exercise. 2001 Nov;33(11):1959–1967. doi: 10.1097/00005768-200111000-00024. [DOI] [PubMed] [Google Scholar]
- Stewart A, Kamberg C. Physical functioning measures. In: Stewart A, Ware J, editors. Measuring functioning and well-being: The medical outcomes study approach. Durham, NC: Duke University Press; 1992. pp. 86–101. [Google Scholar]
- Stewart K, Turner K, Bacher A, De Regis J, Sung J, Tayback M, et al. Are fitness, activity, and fatness associated with health-related quality of life and mood in older persons? Journal of Cardiopulmonary Rehabilitation. 2003;23(2):115–121. doi: 10.1097/00008483-200303000-00009. [DOI] [PubMed] [Google Scholar]
- Stone EA, Quartermain D, Lin Y, Lehmann ML. Central alpha1-adrenergic system in behavioral activity and depression. Biochemical Pharmacology. 2007 Apr;73(8):1063–1075. doi: 10.1016/j.bcp.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Stoudemire A, Frank R, Hedemark N, Kamlet M, Blazer D. The economic burden of depression. General Hospital Psychiatry. 1986 Nov;8(6):387–394. doi: 10.1016/0163-8343(86)90018-6. [DOI] [PubMed] [Google Scholar]
- Swanson GD. The Arizona Activity Frequency Questionnaire using doubly labeled water. Medicine and Science in Sports and Exercise. 2002 Jul;34(7):1217. doi: 10.1097/00005768-200207000-00028. author reply 1217. [DOI] [PubMed] [Google Scholar]
- Thompson C. Economics of treatment of depression. The British Journal of Psychiatry : The Journal of Mental Science. 1995 Jul;167(1):112. doi: 10.1192/bjp.167.1.112b. [DOI] [PubMed] [Google Scholar]
- Thompson D, Richardson E. Current issues in the economics of depression management. Current Psychiatry Reports. 1999 Dec;1(2):125–134. doi: 10.1007/s11920-999-0021-1. [DOI] [PubMed] [Google Scholar]
- Todder D, Caliskan S, Baune BT. Night locomotor activity and quality of sleep in quetiapine-treated patients with depression. Journal of Clinical Psychopharmacology. 2006 Dec;26(6):638–642. doi: 10.1097/01.jcp.0000239798.59943.77. [DOI] [PubMed] [Google Scholar]
- Torgerson W. Theory and methods of scaling. New York: Wiley; 1958. [Google Scholar]
- Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A. Work ability index:Helsinki 1998 [Google Scholar]
- Turpin RS, Ozminkowski RJ, Sharda CE, Collins JJ, Berger ML, Billotti GM, et al. Reliability and validity of the Stanford Presenteeism Scale. Journal of Occupational and Environmental Medicine / American College of Occupational and Environmental Medicine. 2004 Nov;46(11):1123–1133. doi: 10.1097/01.jom.0000144999.35675.a0. [DOI] [PubMed] [Google Scholar]
- Tweed DL. Depression-related impairment: Estimating concurrent and lingering effects. Psychological Medicine. 1993 May;23(2):373–386. doi: 10.1017/s0033291700028476. [DOI] [PubMed] [Google Scholar]
- Tyrer P. Personality disorder and social functioning. In: Peck D, Shapiro C, editors. Measuring human problems: A practical guide. Chichester: John Wiley & Son; 1990. pp. 119–142. [Google Scholar]
- Tyrer P, Nur U, Crawford M, Karlsen S, McLean C, Rao B, et al. The Social Functioning Questionnaire: A rapid and robust measure of perceived functioning. The International Journal of Social Psychiatry. 2005 Sep;51(3):265–275. [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Interpersonal problems, personality pathology, and social adjustment after cognitive therapy for depression. Psychological Assessment. 2003 Mar;15(1):29–40. doi: 10.1037/1040-3590.15.1.29. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Improvement in social-interpersonal functioning after cognitive therapy for recurrent depression. Psychological Medicine. 2004 May;34(4):643–658. doi: 10.1017/S0033291703001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield JC, Schmitz MF, First MB, Horwitz AV. Extending the bereavement exclusion for major depression to other losses: Evidence from the National Comorbidity Survey. Archives of General Psychiatry. 2007 Apr;64(4):433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
- Wang J. A longitudinal population-based study of treated and untreated major depression. Medical Care. 2004 Jun;42(6):543–550. doi: 10.1097/01.mlr.0000128001.73998.5c. [DOI] [PubMed] [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995 Feb;104(1):3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976 Sep;33(9):1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Prusoff BA, Sholomskas D, Padian N. Depressed outpatients. Results one year after treatment with drugs and/or interpersonal psychotherapy. Archives of General Psychiatry. 1981 Jan;38(1):51–55. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. The Journal of Nervous and Mental Disease. 1978 May;166(5):317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Wells KB, Hays RD, Burnam MA, Rogers W, Greenfield S, Ware JE. Detection of depressive disorder for patients receiving prepaid or fee-for-service care. results from the medical outcomes study. JAMA : The Journal of the American Medical Association. 1989 Dec;262(23):3298–3302. [PubMed] [Google Scholar]
- Whooley MA. Depression and cardiovascular disease: Healing the broken-hearted. JAMA : The Journal of the American Medical Association. 2006 Jun;295(24):2874–2881. doi: 10.1001/jama.295.24.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Harkness KL, Simons AD. Life events, number of social relationships, and twelve-month naturalistic course of major depression in a community sample of women. Depression and Anxiety. 2002;16(3):104–113. doi: 10.1002/da.10048. [DOI] [PubMed] [Google Scholar]
- Wright T. Work satisfaction, work performance, and organization tenure considered as predictors of employee turnover. The Journal of Applied Business Research. 1992;8:83–88. [Google Scholar]
- Wright T, Bonett D. The role of employee coping and performance in voluntary employee withdrawal: A research refinement and elaboration. Journal of Management. 1993;19:147–161. [Google Scholar]
- Yanagita M, Willcox BJ, Masaki KH, Chen R, He Q, Rodriguez BL, et al. Disability and depression: Investigating a complex relation using physical performance measures. The American Journal of Geriatric Psychiatry Official Journal of the American Association for Geriatric Psychiatry. 2006 Dec;14(12):1060–1068. doi: 10.1097/01.JGP.0000224364.70515.12. [DOI] [PubMed] [Google Scholar]
- Zauszniewski JA, Rong JR. Depressive cognitions and psychosocial functioning: A test of Beck’s cognitive theory. Archives of psychiatric nursing. 1999 Dec;13(6):286–293. doi: 10.1016/s0883-9417(99)80060-0. [DOI] [PubMed] [Google Scholar]
- Zhang M, Rost KM, Fortney JC. Earnings changes for depressed individuals treated by mental health specialists. The American Journal of Psychiatry. 1999 Jan;156(1):108–114. doi: 10.1176/ajp.156.1.108. [DOI] [PubMed] [Google Scholar]
- Zhang M, Rost KM, Fortney JC, Smith GR. A community study of depression treatment and employment earnings. Psychiatric services (Washington, D.C) 1999 Sep;50(9):1209–1213. doi: 10.1176/ps.50.9.1209. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983 Jun;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, McGlinchey JB, Young D. Diagnosing major depressive disorder VI: Performance of an objective test as a diagnostic criterion. The Journal of Nervous and Mental Disease. 2006 Aug;194(8):565–569. doi: 10.1097/01.nmd.0000230393.19478.d5. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, McGlinchey JB, Posternak MA, Friedman M, Boerescu D, Attiullah N. Discordance between self-reported symptom severity and psychosocial functioning ratings in depressed outpatients: Implications for how remission from depression should be defined. Psychiatry Research. 2006 Feb;141(2):185–191. doi: 10.1016/j.psychres.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, McGlinchey JB, Posternak MA, Friedman M, Boerescu D, Attiullah N. Remission in depressed outpatients: More than just symptom resolution? Journal of Psychiatric Research. 2008 Aug;42(10):797–801. doi: 10.1016/j.jpsychires.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, McGlinchey JB, Young D, Chelminski I. Diagnosing major depressive disorder I: A psychometric evaluation of the DSM-IV Symptom Criteria. The Journal of Nervous and Mental Disease. 2006 Mar;194(3):158–163. doi: 10.1097/01.nmd.0000202239.20315.16. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Posternak MA, Chelminski I. Defining remission on the Montgomery–Asberg Depression Rating Scale. The Journal of Clinical Psychiatry. 2004 Feb;65(2):163–168. doi: 10.4088/jcp.v65n0204. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Ruggero CJ, Chelminski I, Young D, Posternak MA, Friedman M, et al. Developing brief scales for use in clinical practice: the reliability and validity of single-item self-report measures of depression symptom severity, psychosocial impairment due to depression, and quality of life. The Journal of Clinical Psychiatry. 2006 Oct;67(10):1536–1541. doi: 10.4088/jcp.v67n1007. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Sheeran T, Young D. The diagnostic inventory for depression: A self-report scale to diagnose DSM-IV major depressive disorder. Journal of Clinical Psychology. 2004 Jan;60(1):87–110. doi: 10.1002/jclp.10207. [DOI] [PubMed] [Google Scholar]
- Zohar D. When things go wrong: The effect of daily work hassles on effort, exertion and negative mood. Journal of Occupational and Organizational Psychology. 1999;72(3):265–283. [Google Scholar]
- Zung WW. A self-rating depression scale. Archives of General Psychiatry. 1965 Jan;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]


