Abstract
Objective
To examine the potential for reducing cardiovascular risk factors in the United States of America enough to cause age-adjusted coronary heart disease (CHD) mortality rates to drop by 20% (from 2000 baseline figures) by 2010, as targeted under the Healthy People 2010 initiative.
Methods
Using a previously validated, comprehensive CHD mortality model known as IMPACT that integrates trends in all the major cardiovascular risk factors, stratified by age and sex, we calculated how much CHD mortality would drop between 2000 and 2010 in the projected population of the United States aged 25–84 years (198 million). We did this for three assumed scenarios: (i) if recent risk factor trends were to continue to 2010; (ii) success in reaching all the Healthy People 2010 risk factor targets, and (iii) further drops in risk factors, to the levels already seen in the low-risk stratum.
Findings
If age-adjusted CHD mortality rates observed in 2000 remained unchanged, some 388 000 CHD deaths would occur in 2010. First scenario: if recent risk factor trends continued to 2010, there would be approximately 19 000 fewer deaths than in 2000. Although improved total cholesterol, lowered blood pressure in men, decreased smoking and increased physical activity would account for some 51 000 fewer deaths, these would be offset by approximately 32 000 additional deaths from adverse trends in obesity and diabetes and in blood pressure in women. Second scenario: If Healthy People 2010 cardiovascular risk factor targets were reached, approximately 188 000 CHD deaths would be prevented. Scenario three: If the cardiovascular risk levels of the low-risk stratum were reached, approximately 372 000 CHD deaths would be prevented.
Conclusion
Achievement of the Healthy People 2010 cardiovascular risk factor targets would almost halve the predicted CHD death rates. Additional reductions in major risk factors could prevent or postpone substantially more deaths from CHD.
Résumé
Objectif
Étudier les possibilités de réduire les facteurs de risque cardiovasculaire aux États-Unis d’Amérique de manière à ce que la mortalité par cardiopathie coronarienne (CC) ajustée pour l’âge baisse de 20 % d’ici à 2010 (par rapport aux données de mortalité de l’année 2000, servant de référence), objectif visé par l’Initiative Healthy People 2010.
Méthodes
En faisant appel à un modèle de mortalité détaillé et antérieurement validé appelé IMPACT, qui intègre les tendances des principaux facteurs de risque cardiovasculaire, stratifiées selon l’âge et le sexe, nous avons calculé de combien baisserait la mortalité par CC entre 2000 et 2010 dans la population projetée des États-Unis d’Amérique pour la tranche d’âges 25-84 ans (198 millions). Nous avons effectué ce calcul pour trois scénarios hypothétiques : (i) poursuite jusqu’en 2010 des tendances récemment observées pour les facteurs des risque ; (ii) réalisation de tous les objectifs relatifs aux facteurs de risque de l’Initiative Healthy People 2010 et (iii) diminutions supplémentaires des facteurs de risque jusqu’aux niveaux déjà relevés dans la strate de faible risque.
Résultats
Si les taux de mortalité par CC ajustés pour l’âge enregistrées en 2000 n’évoluent pas, quelque 388 000 décès par CC se produiront en 2010. Premier scénario : si les tendances récemment observées pour les facteurs de risque se poursuivent jusqu’en 2010, on devrait enregistrer environ 19 000 de moins qu’en 2000. La baisse de la mortalité qui devrait résulter de l’amélioration du taux de cholestérol total et de la baisse de la tension artérielle chez les hommes, ainsi que du recul du tabagisme et de l’augmentation de l’activité physique (quelque 51 000 décès en moins) devrait en effet être compensée par environ 32 000 décès supplémentaires dus aux tendances à la hausse de l’obésité et des diabètes chez les deux sexes et de la tension artérielle chez les femmes. Deuxième scénario : si les objectifs de l’Initiative Healthy People 2010 concernant les facteurs de risque cardiovasculaire sont réalisés, 188 000 décès par CC environ seront évités. Troisième scénario ; si les niveaux de risque cardiovasculaire de la strate à faible risque sont atteints, 372 000 décès par CC environ devraient pouvoir être évités.
Conclusion
La réalisation des objectifs relatifs aux facteurs de risque cardiovasculaire de l’Initiative Healthy People 2010 devrait presque réduire de moitié les taux de mortalité par CC prévus. Des réductions supplémentaires des principaux facteurs de risque pourraient prévenir ou différer substantiellement plus de décès par CC.
Resumen
Objetivo
Estudiar las posibilidades de reducir los factores de riesgo cardiovascular en los Estados Unidos en la medida necesaria para conseguir una caída del 20% (respecto a las cifras de 2000) de la mortalidad por cardiopatía coronaria (CC) ajustada por edad para 2010, conforme a la meta de la iniciativa Healthy People 2010.
Métodos
Utilizando un modelo detallado y previamente validado de mortalidad por CC conocido como IMPACT, que integra las tendencias de los principales factores de riesgo cardiovascular, estratificados por edad y sexo, calculamos cuánto disminuiría la mortalidad por CC entre 2000 y 2010 en la población de 25 a 84 años prevista para Estados Unidos (198 millones) en cada uno de los tres escenarios siguientes: (i) prolongación de las tendencias recientes de los factores de riesgo hasta 2010; (ii) logro de las metas de Healthy People 2010 respecto a los factores de riesgo, y (iii) caídas adicionales de los factores de riesgo hasta los niveles correspondientes al estrato de bajo riesgo.
Resultados
Si se mantienen las tasas de mortalidad por CC ajustadas por edad observadas en 2000, en 2010 se registrarán unas 388 000 muertes por CC. Primer escenario: si se prolongaran las tendencias recientes de los factores de riesgo hasta 2010, se registrarían aproximadamente 19 000 defunciones menos que en 2000. Pese a que las disminuciones del colesterol total y de la tensión arterial entre los hombres, unidas al menor consumo de tabaco y el aumento de la actividad física, reducirían en 51 000 el número de muertes, esa cifra se vería contrarrestada por las aproximadamente 32 000 defunciones provocadas por las tendencias adversas de la obesidad, la diabetes y la hipertensión entre las mujeres. Segundo escenario: si se alcanzan las metas de Healthy People 2010 referentes a los factores de riesgo cardiovascular, podrían prevenirse en torno a 188 000 defunciones por CC. Tercer escenario: si se generalizaran los niveles de riesgo cardiovascular del estrato de bajo riesgo, podrían prevenirse unas 372 000 defunciones por cardiopatía coronaria.
Conclusión
Si se alcanzaran las metas de Healthy People 2010 sobre los factores de riesgo cardiovascular, se reducirían casi a la mitad las tasas de mortalidad previstas por CC, y toda disminución adicional de los factores de riesgo principales podría tener aún un efecto considerable en ese sentido.
ملخص
الغرض
دراسة إمكانية خفض عوامل الخطر المتعلقة بالأمراض القلبية الوعائية في الولايات المتحدة الأمريكية بحيث تؤدي إلى خفض معدلات الوفيات المعدلة حسب العمر والناجمة عن المرض القلبي التاجي بنحو 20% (من الأرقام الأساسية لعام 2000)، وذلك بحلول عام 2010، وهو الغرض الذي استهدفته مبادرة السكان الأصحاء 2010.
الطريقة
باستخدام النموذج الشامل لوفيات المرض القلبي التاجي، والذي تم توثيقه مسبقاً، والمعروف باسم امباكت IMPACT، الذي يقوم بدمج جميع الاتجاهات في عوامل الخطر الرئيسية للأمراض القلبية الوعائية، مصنفة بحسب العمر والجنس، قام الباحثون بحساب حجم الوفيات الناجمة عن الأمراض القلبية التاجية التي قد تنخفض معدلاتها بين العامين 2000 و2010 في السكان المتوقعين في الولايات المتحدة والتي تتراوح أعمارهم ما بين 25-84 عاما (198 مليون). وأجرى الباحثون ذلك وفقاً لثلاثة سيناريوهات افتراضية هي: (1) عدم ملاحظة أي تغيير في معدلات الوفيات المعدلة بحسب العمر والناجمة عن المرض القلبي التاجي في عام 2000، (2) نجاح الوصول إلى جميع عوامل الخطر المستهدفة في مبادرة السكان الأصحاء 2010، (3) تحقيق المزيد من خفض عوامل الخطر إلى أن تصل إلى المستويات المشاهدة في أقل المجموعات المعرضة للخطر.
الموجودات
السيناريو االأول: إذا لم تتغير معدلات الوفيات المعدلة بحسب العمر والناجمة عن المرض القلبي التاجي في عام 2000، فهناك احتمال أن تحدث 388000 وفاة من جراء هذا المرض في عام 2010 (مما يعني 19000 وفاة تقريباً أقل من الوفيات التي وقعت في عام 2000). وعلى الرغم من أن التحسن في المستوى الإجمالي للكوليسترول، وانخفاض ضغط الدم في الرجال، مع انخفاض معدلات التدخين وزيادة النشاط البدني قد يكونوا جميعا وراء انخفاض معدلات الوفيات بحوالي 51000 وفاة، إلا أن هذا قد يضاهيه زيادة في الوفيات تبلغ 32000 ناجمة عن الاتجاهات الضائرة والتي تتمثل في السمنة والسكري وضغط الدم لدى النساء. السيناريو الثاني: إذا ما تحقق النجاح في بلوغ جميع عوامل الخطر المستهدفة في مبادرة السكان الأصحاء 2010، نكون قد نجحنا في تجنب حوالي 188000 وفاة ناجمة عن الأمراض القلبية التاجية. السيناريو الثالث: إذا ما تحقق خفض عوامل الخطر القلبية الوعائية إلى مرتبة المستويات المتدنية للخطر، سيمكن تجنب وقوع 372000 وفاة تقريباً من وفيات الأمراض القلبية التاجية.
الاستنتاج
إن تحقيق المرامي المستهدفة من مبادرة السكان الأصحاء 2010 والمتمثلة في الكشف عن عوامل الخطر القلبية الوعائية سيؤدي إلى خفض معدلات وفيات المرض القلبي التاجي إلى النصف. ومن شأن تحقيق المزيد من خفض عوامل الخطر أن يقي من أو يؤجل وقوع المزيد من الوفيات الناجمة عن المرض القلبي التاجي.
Introduction
Coronary heart disease (CHD) accounted for over 450 000 deaths in the United States of America in 2004.1,2 The burden of CHD in the United States is enormous; more than 13 million people are affected, and the costs of direct health care exceed US$ 150 billion annually.1,2
Since the late 1970s, age-adjusted CHD mortality rates have been halved in most industrialized countries, including the United States. However, between 1990 and 2000 this decrease diminished, and in younger age groups it nearly ceased.1,2 Many adults in the United States are still at high risk for cardiovascular disease. Total blood cholesterol levels exceed 200 mg/dl among more than 100 million adults; approximately 70 million have or are being treated for high blood pressure (systolic blood pressure 140 mmHg or diastolic blood pressure 90 mmHg), and over 50 million people still smoke.2–4
The Healthy People 2010 (HP2010) initiative promoted by the government of the United States contains targets for heart disease and stroke that explicitly address risk factor prevention, detection and management, along with prevention of recurrent events. HP2010 objectives include a 20% reduction in age-adjusted CHD mortality rates (from an overall rate of 203 per 100 000 population in 1998 to 162 per 100 000 in 2010).3 They also include specific targets for reducing mean total blood cholesterol (to 199 mg/dl), smoking (to 12% of the population), hypertension (to 16%), diabetes (to 6%), obesity (to 15%) and inactivity (to 20%).3 Inactivity was measured in the Behavioral Risk Factor Surveillance System of the United States Centers for Disease Control and Prevention as the proportion of adults engaging in no physical activity.5 If those targets are achieved, what reduction in CHD mortality might actually result by 2010?
Large meta-analyses and cohort studies have consistently demonstrated substantial reductions in CHD deaths related to decreases in each of the major cardiovascular risk factors among individuals covered by the studies.6–8 However, it is difficult to attribute a decline in the mortality rate for an entire population either to specific risk factor changes or to more effective medical interventions because favourable trends in both have often occurred simultaneously.9,10 Furthermore, risk factor improvements, such as lower blood pressure or total blood cholesterol, may be achieved through medications, lifestyle changes or a combination.1,2,8–10
A variety of CHD policy models have been developed to estimate the relative contributions and hence the population impact of medical and public health interventions. Good models are able to integrate and simultaneously consider large amounts of data on patient numbers, treatments and population risk factor trends.9–11 The CHD Policy Model developed in the United States was used successfully to examine risk factor trends in that country between 1980 and 19909 and later demonstrated the potential advantages of a population-based approach to prevention,12 consistent with European studies.13–15 Capewell et al. subsequently developed and refined a CHD mortality model called IMPACT and applied it in a variety of populations.10,16–19 Approximately 44% of the substantial CHD mortality decline in the United States between 1980 and 2000 was attributable to changes in major risk factors, and 47% to specific cardiological treatments.10 These findings resembled those from other industrialized countries.16,17,19,20
Three earlier analyses suggested that further modest reductions in major risk factors could halve CHD deaths in the United Kingdom.15,21–23 To determine if similar gains could be attained for the population of the United States or if they would be rendered unattainable by recent dramatic rises in obesity and diabetes, we used the previously calibrated IMPACT model10 for the United States to estimate the number of CHD deaths that could be prevented or postponed in 2010, compared with the number in 2000. The model was applied to three contrasting scenarios. In the third, most optimistic scenario, the prevalence of risk factors in the entire population was assumed to have reached the ideal levels already reported in “low-risk stratum” cohorts.24,25
Methods
The IMPACT model aims to explain the changes in CHD mortality rates observed in a population. It quantifies the contribution from temporal trends in the major population risk factors (smoking, high systolic blood pressure, elevated total blood cholesterol, obesity, diabetes and physical inactivity) and from medical and surgical treatments given to CHD patients.10,17,26 The model employs regression coefficients produced by large meta-analyses and cohort studies.6–8 Each coefficient quantifies the independent (log linear) relationship between the absolute change in a specific cardiovascular risk factor, such as high systolic blood pressure or total blood cholesterol, and the consequent change in population mortality rates from CHD (Table 1).6–8 For each risk factor, the subsequent reduction in deaths between base year 2000 and 2010 could then be estimated as the product of three variables:
Table 1. β regression coefficients and relative risk ratiosa for every 1-unit change in the level of major cardiovascular risk factors for CHD mortality, United States of America.
| Risk factor | Age group, in years |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 25–44 | 45–54 | 55–64 | 65–74 | 75–84 | ||||||
| Systolic blood pressure7 | ||||||||||
| Log hazard ratio per 1 mmHg change | ||||||||||
| Men | –0.036 | –0.035 | –0.032 | –0.027 | –0.021 | |||||
| Women | –0.046 | –0.046 | –0.035 | –0.032 | –0.026 | |||||
| Total blood cholesterol6 | ||||||||||
| Relative risk ratio per 1 mmol/l (38.6 mg/dl) change, both sexes | 0.900 | 0.650 | 0.450 | 0.333 | 0.317 | |||||
| Log β coefficient for change in mortality rate, both sexes | –1.2942 | –0.8238 | –0.5245 | –0.3719 | –0.3512 | |||||
| BMI8 | ||||||||||
| Relative risk ratio per 1 kg/m² change | 1.04 | 1.03 | 1.02 | 1.01 | 1.01 | |||||
| Log β coefficient for change in mortality rate, both sexes | 0.0363 | 0.0297 | 0.0165 | 0.0132 | 0.0099 | |||||
BMI, body mass index; CHD, coronary heart disease. a Calculated from relative risks used as input for the IMPACT model for the United States.
| Number of CHD deaths prevented = number of CHD deaths observed in 2000 × the risk factor reduction × the specific regression coefficient exponentiated10,22,23 |
All the coefficients and relative risk values were obtained from multivariate logistic regression analyses and were assumed to be independent, having been adjusted for potential confounding from the other major risk factors. The total deaths prevented could therefore be summed. Independent regression coefficients were not available for smoking, diabetes or physical inactivity. Thus, we used an alternative method that involved population-attributable risk fractions9,21,22 calculated for the INTERHEART study, a large, international multivariate analysis that included data from the United States27 (Table 2).
Table 2. ORsa for death from CHD for three cardiovascular risk factors, United States of America.
| Risk factor | OR (99% CI) |
||||
|---|---|---|---|---|---|
| Men |
Women |
||||
| Aged 55 years | Aged > 55 years | Aged 65 years | Aged > 65 years | ||
| Smoking | 3.33 (2.80– 3.95) | 2.52 (2.15– 2.96) | 4.49 (3.11– 6.47) | 2.14 (1.35– 3.39) | |
| Physical inactivity | 1.02 (0.83– 1.25) | 0.79 (0.66– 0.96) | 0.74 (0.49– 1.10) | 0.75 (0.46– 1.22) | |
| Diabetes | 2.66 (2.04– 3.46) | 1.93 (1.58– 2.37) | 3.53 (2.49– 5.01) | 2.59 (1.78– 3.78) | |
CHD, coronary heart disease; CI, confidence interval; OR, odds ratio. a Calculated from relative risks used as input for the IMPACT model for the United States. Based on data from the INTERHEART study.27
The original 1980–2000 IMPACT model10 was extended to 2010 using United States Census Bureau population projections and mortality data for men and women aged 25–84 years. The number of CHD deaths (International Classification of Diseases, ICD-10: I20–I25) expected in 2010 was then calculated under three contrasting risk factor scenarios.
Risk factor scenarios
In the first scenario, we assumed that recent risk factor trends would continue to 2010. Using data from the Third National Health and Nutrition Examination Survey (NHANES) 1988–1994, NHANES 1999–2002, and the Behavioral Risk Factor Surveillance System (1988–2002),3,4 we made linear projections from 1988–1994 through 1999–2002 to the country’s population in 2010 of recent trends in mean total blood cholesterol (mg/dl), population smoking prevalence (%), mean systolic blood pressure (mmHg), mean body mass index (BMI, in kg/m²), population prevalence of diagnosed and undiagnosed diabetes types 1 and 2 (%) and population prevalence of any leisure-time physical activity (%), all stratified by age and sex (Table 3).10,22,23
Table 3. Cardiovascular risk factor levels in base year 2000 and projections to 2010 under three cardiovascular risk factor change scenarios, United States of America.
| Risk factor scenario | Smoking prevalence, % |
Mean total blood cholesterol, mg/dl (mmol/l)a |
Mean systolic blood pressure, mmHg |
Mean BMI, kg/m² |
Diabetes prevalence, % |
Physical activityb prevalence, % |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | ||||||
| NHANES III (1988–1994) | 31.6 | 24.7 | 206 (5.32) | 210 (5.42) | 123.5 | 119.6 | 26.87 | 26.73 | 9.0 | 8.9 | 70.4 | 68.0 | |||||
| In 2000 (NHANES 1999–2002) | 27.3 | 21.9 | 205 (5.30) | 207 (5.35) | 124.4 | 123.9 | 27.86 | 28.51 | 11.7 | 9.5 | 75.1 | 70.5 | |||||
| In 2010, if recent trends continue | 22.6 | 18.7 | 204 (5.28) | 204 (5.28) | 125.3 | 128.5 | 29.18 | 30.16 | 15.2 | 10.1 | 80.8 | 74.1 | |||||
| In 2010, if HP2010 targets are achieved | 12.0 | 12.0 | 199 (5.15) | 199 (5.15) | 119.4c | 118.9c | 25.00d | 26.00d | 6.0e | 6.0e | 80 | 80 | |||||
| In 2010, if all in low-risk stratum | 0 | 0 | 176 (4.54) | 179 (4.64) | 115.7 | 114.7 | 25.50 | 23.60 | 0.0 | 0.0 | 100 | 100 | |||||
BMI, body mass index; HP2010, Healthy People 2010; NHANES, National Health and Nutrition Examination Survey. a Cholesterol conversion factor from mg/dl to mmol/l = 38.67. b Any leisure time activity. c Assuming a 5 mmHg decrease in mean value from 2000. d Assuming that obesity prevalence falls to 15%. e Total diabetes (diagnosed and undiagnosed), equivalent to HP2010 target of 25 diagnosed cases per 1000 population.
In the second scenario, we assumed that risk factor levels had dropped in accordance with the substantial but feasible reductions defined in the HP2010 objectives.3 In the absence of specific HP2010 targets for mean BMI, total diabetes prevalence and mean systolic blood pressure, we assumed that: (i) the 15% obesity target would equate to a population mean BMI of 25 kg/m² for men and 26 kg/m² for women; (ii) the 25 per 1000 population clinically diagnosed diabetes prevalence target would equate to a total (diagnosed and undiagnosed) type 1 and type 2 diabetes prevalence of 6%; and (iii) the 16% hypertension prevalence target would equate to a population mean systolic blood pressure of 119 mmHg, representing a 5 mmHg reduction from 2000 levels (Table 3).
In the third scenario, mean population risk factors were assumed to drop to the levels already observed in the “healthiest” stratum of cohorts in the United States, as defined by Stamler et al.24 and Daviglus et al.25 Levels for specific risk factors were as follows: (i) no smoking among men or women; (ii) mean total cholesterol of 175.6 mg/dl (4.54 mmol/l) for men and 179.6 mg/dl (4.64 mmol/l) for women; (iii) mean systolic blood pressure of 115.7 mmHg for men and 114.7 mmHg for women, representing a 10 mmHg reduction from 2000 levels; (iv) a mean BMI of 25.5 kg/m² for men and 23.6 kg/m² for women; and (v) zero prevalence of diabetes among both men and women.24,25 Physical activity was not specifically considered in these studies,24,25 so we defined the level in the lowest risk stratum as 100%, with everyone undertaking some leisure-time physical activity (Table 3).
To preserve the focus on risk factor changes, we assumed that the proportion of the population receiving medical and surgical treatments for CHD would remain constant.
Sensitivity analysis
Because of the uncertainties surrounding some of the estimates, a multi-way sensitivity analysis was performed using the analysis of extremes method.28 Minimum and maximum estimates of deaths prevented or postponed were generated using minimum and maximum plausible values for the main parameters: 95% confidence intervals (CIs) when available; otherwise, the best value ± 20%.10,22,23,28 Appendix A (available at: http://content.nejm.org/cgi/data/356/23/2388/DC1/1) provides worked examples of the calculations used in the model plus further details on the methods and data sources used.10
Results
Trends and estimates
Approximately 388 000 CHD deaths among people aged 25–84 years would be expected in 2010 if the same age-specific death rates recorded in 2000 (the base year) were also observed in 2010. This number would represent 15% more deaths than the 338 000 observed in 2000, a reflection of population ageing compounded by an increase in population size (Table 4).
Table 4. Age-specific CHD mortality ratesa and CHD deaths observed in 2000b and projections to 2010 under different cardiovascular risk factor scenarios, United States of America.
| Age group, in years | Population in 2010, 1000s | CHD mortality rate per 100 000 |
No. of CHD deaths |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Observed in 2000 | Per cent annual change, 1997–2002 | Expected in 2010 if recent risk trends continue | Expected in 2010 if recent risk trends continue | Expected in 2010 if risk rates for 2000 remain unchanged | In 2010 as a change from 2000 | Per cent change in 2010 from 2000 | ||||||||||||
| Men | ||||||||||||||||||
| 25–34 | 21 105 | 3.50 | –0.52 | 3.32 | 700 | 739 | –39 | –5.2 | ||||||||||
| 35–44 | 20 552 | 25.78 | –0.52 | 24.43 | 5 022 | 5 298 | –277 | –5.2 | ||||||||||
| 45–54 | 22 064 | 103.52 | –2.70 | 75.59 | 16 679 | 22 841 | –6 163 | –27.0 | ||||||||||
| 55–64 | 17 438 | 290.20 | –4.14 | 170.10 | 29 663 | 50 607 | –20 944 | –41.4 | ||||||||||
| 65–74 | 9 797 | 705.19 | –4.03 | 420.76 | 41 222 | 69 088 | –27 866 | –40.3 | ||||||||||
| 75–84 | 5 272 | 1736.85 | –3.20 | 1180.98 | 62 265 | 91 573 | –29 307 | –32.0 | ||||||||||
| Subtotal | 96 229 | 236.00 | –1.97 | 161.65 | 155 550 | 240 145 | –84 595 | –35.2 | ||||||||||
| Women | ||||||||||||||||||
| 25–34 | 20 541 | 1.17 | +2.16 | 1.42 | 292 | 240 | +52 | +21.6 | ||||||||||
| 35–44 | 20 568 | 7.63 | +2.16 | 9.28 | 1 909 | 1 569 | +339 | +21.6 | ||||||||||
| 45–54 | 22 763 | 29.93 | –1.56 | 25.25 | 5 749 | 6 813 | –1 065 | –15.6 | ||||||||||
| 55–64 | 18 747 | 110.39 | –4.15 | 64.57 | 12 104 | 20 696 | –8 591 | –41.5 | ||||||||||
| 65–74 | 11 473 | 340.32 | –3.69 | 214.61 | 24 621 | 39 044 | –14 423 | –36.9 | ||||||||||
| 75–84 | 7 578 | 1055.16 | –3.14 | 723.60 | 54 838 | 79 964 | –25 127 | –31.4 | ||||||||||
| Subtotal | 10 1670 | 146.90 | –1.12 | 97.88 | 99 515 | 148 325 | –48 815 | –32.9 | ||||||||||
| Total | 197 900 | 190.00 | –1.5 | 142.15 | 255 060 | 388 470 | –133 410 | –34.3 | ||||||||||
CHD, coronary heart disease. a Rounded to the nearest 100 b Data obtained from the American Heart Association.1
Between 1997 and 2002, the overall annual declines observed in CHD mortality rates were 2% for men and 1% for women. However, declines were minimal among men younger than 45 years of age, and increases were seen among women in that age group.
Three of the six major risk factors declined between 1988 and 2002, while obesity and diabetes increased. Systolic blood pressure rates rose among women and fluctuated among men. If the same trends continued, the overall result would be approximately 19 000 fewer deaths in 2010 than in 2000 (minimum estimate: 10 000; maximum estimate: 25 000). This represents some 51 000 fewer deaths because of improvements in mean total cholesterol and mean blood pressure in men, less the prevalence of smoking and of increased physical activity, minus approximately 32 000 additional deaths attributable to adverse trends in obesity, diabetes and mean blood pressure in women (Table 5).
Table 5. CHD deaths in 2010 as a change from 2000 baseline, by sex, under three cardiovascular risk factor scenarios, United States of America.
| Risk factor scenario | Risk factor value |
Fewer/additional CHD deaths in 2010a |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Both sexes |
Best estimate |
|||||||||||||
| Best estimate | Minimum estimate | Maximum estimate | Men | Women | ||||||||||||
| Smoking prevalence, in % | ||||||||||||||||
| In 2000 | 27.3 | 21.9 | – | – | – | – | – | |||||||||
| If recent trends continue to 2010 | 22.6 | 18.7 | –10 000 | –8 000 | –12 000 | –7 000 | –3 000 | |||||||||
| If HP2010 targets are achieved | 12.0 | 12.0 | –26 000 | –21 000 | –32 000 | –18 000 | –8 000 | |||||||||
| If all in low-risk stratum | 0 | 0 | –60 000 | –48 000 | –72 000 | –42 000 | –18 000 | |||||||||
| Mean total blood cholesterol, in mg/dl | ||||||||||||||||
| In 2000 | 205.0 | 206.9 | – | – | – | – | – | |||||||||
| If recent trends continue to 2010 | 204.2 | 204.3 | –28 000 | –17 000 | –41 000 | –15 000 | –14 000 | |||||||||
| If HP 2010 targets are achieved | 199.0 | 199.0 | –40 000 | –24 000 | –59 000 | –17 000 | –24 000 | |||||||||
| If all in low-risk stratum | 175.6 | 179.6 | –103 000 | –70 000 | –160 000 | –68 000 | –35 000 | |||||||||
| Mean systolic blood pressure, in mmHg | ||||||||||||||||
| In 2000b | 124.4 | 123.9 | – | – | – | – | – | |||||||||
| If recent trends continue to 2010 | 125.3 | 128.5 | +2 000 | +1 000 | +4 000 | –6 000 | +8 000 | |||||||||
| If HP2010 targets are achieved | 119.4 | 118.9 | –48 000 | –39 000 | –58 000 | –28 000 | –20 000 | |||||||||
| If all in low-risk stratum | 115.7 | 114.7 | –83 000 | –75 000 | –108 000 | –54 000 | –29 000 | |||||||||
| Mean BMI, in kg/m² | ||||||||||||||||
| In 2000 | 27.86 | 28.51 | – | – | – | – | – | |||||||||
| If recent upward trends continue to 2010 | 29.18 | 30.16 | +8 000 | +5 000 | +11 000 | +5 000 | +3 000 | |||||||||
| If HP2010 targets are achieved | 25.00 | 26.00 | –17 000 | –10 000 | –24 000 | –12 000 | –5 000 | |||||||||
| If all in low-risk stratum | 25.50 | 23.60 | –21 000 | –12 000 | –27 000 | –10 000 | –10 000 | |||||||||
| Diabetes prevalence, in % | ||||||||||||||||
| In 2000 | 11.7 | 9.5 | – | – | – | – | – | |||||||||
| If recent upward trends continue to 2010 | 15.2 | 10.1 | +16 000 | +5 000 | +22 000 | +11 000 | +5 000 | |||||||||
| If HP2010 targets are achieved | 6.0 | 6.0 | –44 000 | –26 000 | –66 000 | –24 000 | –20 000 | |||||||||
| If all in low-risk stratum | 0 | 0 | –72 000 | –49 000 | –100 000 | –38 000 | –34 000 | |||||||||
| Physical activity prevalence, in % | ||||||||||||||||
| In 2000 | 75.1 | 70.5 | – | – | – | – | – | |||||||||
| If recent trends continue to 2010 | 80.8 | 74.1 | –7 000 | –6 000 | –9 000 | –4 000 | –2 000 | |||||||||
| If HP2010 targets are achieved | 80 | 80 | –12 000 | –10 000 | –14 000 | –6 000 | –6 000 | |||||||||
| If all in low-risk stratum | 100 | 100 | –34 000 | –27 000 | –40 000 | –18 000 | –16 000 | |||||||||
| Totals | ||||||||||||||||
| If recent downward trendsb continue | – | – | –51 000 | –29 000 | –57 000 | –32 000 | –19 000 | |||||||||
| If recent upward trendsc continue | – | – | +32 000 | +10 000 | +32 000 | +16 000 | +16 000 | |||||||||
| Net effect if recent trends continue | – | – | –19 000 | –10 000 | –25 000 | –16 000 | –3 000 | |||||||||
| If HP2010 targets are achieved | – | – | –188 000 | –129 000 | –252 000 | –105 000 | –83 000 | |||||||||
| If all in low-risk stratum | – | – | –372 000 | –281 000 | –507 000 | –230 000 | –142 000 | |||||||||
| If only smoking, cholesterol and systolic blood pressure match low-risk stratum | – | – | –246 000 | –194 000 | –339 000 | –164 000 | –82 000 | |||||||||
| If only BMI, diabetes and physical activity match low-risk stratum | – | – | –126 000 | –87 000 | –167 000 | –66 000 | –60 000 | |||||||||
BMI, body mass index; CHD, coronary heart disease; HP2010, Healthy People 2010. a Rounded to nearest 1000. b In smoking prevalence, total blood cholesterol, physical inactivity prevalence, mean systolic blood pressure in men. c In systolic blood pressure in women, obesity prevalence, diabetes prevalence.
Approximately 188 000 fewer CHD deaths than in 2000 (minimum estimate: 129 000; maximum estimate: 252 000) could be achieved by reaching the specific reductions in cardiovascular risk factors called for in HP2010: (i) approximately 40 000 fewer deaths if population mean blood cholesterol levels declined to 199 mg/dl (5.15 mmol/l) among both men and women; (ii) approximately 26 000 fewer deaths if the smoking prevalence fell to 12% among both men and women; (iii) approximately 48 000 fewer deaths, mean systolic blood pressure were to drop to 119.4 mmHg among men and 118.9 mmHg among women (representing a 5 mmHg reduction in all age groups); (iv) approximately 12 000 fewer deaths, if physical activity rates rose to 80% among both men and women; (v) approximately 17 000 fewer deaths if mean BMI decreased substantially, to 25.0 kg/m² for men and 26.0 kg/m² for women; and (vi) approximately 44 000 fewer deaths if total diabetes prevalence dropped to 6% among both men and women.
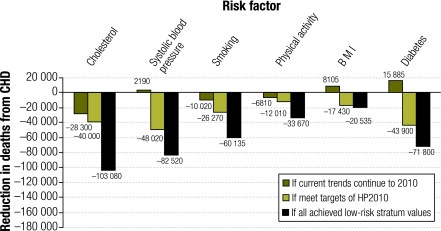
If the ideal scenario were achieved and mean population cardiovascular risk factors were reduced to the levels already observed in the healthiest stratum of cohorts,24,25 approximately 372 000 CHD deaths (minimum estimate: 281 000; maximum estimate: 507 000) could be prevented or postponed (Fig. 1). The 372 000 fewer deaths would be distributed as follows: (i) approximately 103 000 fewer deaths if population mean blood cholesterol levels declined to 175.6 mg/dl (4.54 mmol/l) among men and 179.6 mg/dl (4.64 mmol/l) among women; (ii) approximately 60 000 fewer deaths if smoking prevalence fell to zero; (iii) approximately 83 000 fewer deaths if mean systolic blood pressure dropped by 10 mmHg, to 115.7 mmHg for men and114.7 mmHg for women; (iv) approximately 34 000 fewer deaths if all men and women were physically active; (v) approximately 21 000 fewer deaths if mean BMI decreased to 25.5 in men and 23.6 in women; and (vi) approximately 72 000 fewer deaths if the prevalence of diabetes were zero (Table 5).
Fig. 1.
Estimated reduction in CHD deaths in 2010, by cardiovascular risk factor, under three different risk factor scenarios, United States of America
BMI, body mass index; CHD, coronary heart disease; HP2010, Healthy People 2010.
Estimated mortality benefits
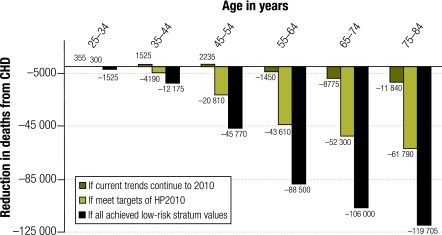
Under the scenario in which current trends continued, approximately 16 000 fewer deaths would occur among men and 3000 among women. In the two more optimistic scenarios, men would consistently benefit more than women, gaining 54% of the 188 000 fewer deaths under the HP2010 reductions scenario and 62% of the 372 000 fewer deaths if low-risk stratum levels are assumed (Table 5). Gains would predominantly occur among men aged 45–84 years and among women aged 65–84 years (Fig. 2). Of the 372 000 fewer deaths in the most optimistic scenario, 252 000 (68%) would represent premature deaths prevented or postponed, that is, deaths among those under 75 years of age (Table 6).
Fig. 2.
Estimated reduction in CHD deaths in 2010, by age group, under three different cardiovascular risk factor scenarios, United States of America
CHD, coronary heart disease; HP2010, Healthy People 2010.
Table 6. Number of CHD deathsa in 2010 as a change from 2000 baseline, by sex and age group, under three cardiovascular risk factor scenarios, United States of America.
| Age group, in years | Scenario |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recent trends continue |
HP2010 targets are achieved |
All achieve low-risk stratum values |
||||||||||||||||||
| Men | Women | Both sexes | Men | Women | Both sexes | Men | Women | Both sexes | ||||||||||||
| 25–34 | +55 | +305 | +355 | –225 | –75 | –300 | –1 000 | –1 000 | –2 000 | |||||||||||
| 35–44 | +380 | +1 000 | +2 000 | –3 000 | –2 000 | –4 000 | –8 000 | –4 000 | –12 000 | |||||||||||
| 45–54 | +2 000 | +115 | +2 000 | –16 000 | –5 000 | –20 000 | –35 000 | –11 005 | –46 000 | |||||||||||
| 55–64 | –2 000 | –1 000 | –1 000 | –27 000 | –16 000 | –44 000 | –57 000 | –31 000 | –89 000 | |||||||||||
| 65–74 | –10 000 | +1 000 | –9 000 | –28 000 | –25 000 | –52 000 | –62 000 | –44 000 | –106 000 | |||||||||||
| 75–84 | –7 000 | –5 000 | –12 000 | –25 000 | –37 000 | –62 000 | –67 000 | –53 000 | –120 000 | |||||||||||
| Total | –16 000 | –3 000 | –19 000 | –105 000 | –83 000 | –188 000 | –230 000 | –142 000 | –372 000 | |||||||||||
CHD, coronary heart disease; HP2010, Healthy People 2010. a Rounded to nearest 1000.
Using extensive sensitivity analyses, we examined the impact of higher and lower values for model parameters.28 Changing the values influenced the number of deaths postponed or prevented but did not alter the relative contribution of each risk factor (Table 5, columns 5 and 6). Thus, regardless of whether best, minimum or maximum estimates were considered, the most substantial contributions came from the changes in blood cholesterol, blood pressure and smoking (Table 5).
Discussion
Success in achieving the HP2010 targets could almost halve predicted CHD deaths in 2010, or indeed in 2015. Our findings are reassuringly consistent with earlier studies in England,23 Scotland22 and the United States.12 In the United Kingdom, a modest reduction in mean population blood cholesterol level from 225 mg/dl to 200 mg/dl could reduce CHD deaths by approximately half.14,15,24 In contrast, a rather optimistic 25% reduction in the prevalence of obesity would probably prevent just 2% of CHD deaths.15,24 A corresponding 25% reduction in the prevalence of inactivity might prevent 1% of CHD deaths.15,29
Although CHD death rates have been falling in the United States for four decades, they are now levelling off in young men and women.2 Recent declines in total blood cholesterol have been modest, blood pressure is now rising among women and obesity and diabetes are rising steeply in both sexes. Furthermore, population ageing will increase the numbers of CHD deaths in the United States and elsewhere.30
There is no room for complacency. If recent risk factor trends continue, there should be approximately 20 000 fewer deaths from CHD in 2010 than in 2000. This reflects some 50 000 fewer deaths expected from improvements in total blood cholesterol, smoking, physical activity and blood pressure in males, but more than half of this gain would be offset by approximately 30 000 additional deaths owing to higher obesity and diabetes rates, plus a rise in systolic blood pressure among women. Increasing treatments could not compensate for these worsening risk factors. In 2000, barely 40% of eligible patients received appropriate therapies.10 Even raising this proportion to an optimistic 50% would only postpone approximately 60 000 additional deaths in 2010.31
Successfully achieving the specific risk factor reduction targets proposed in the HP2010 could prevent or postpone approximately 190 000 CHD deaths. This would potentially halve the CHD mortality burden seen in 2000. The HP2010 objectives for blood cholesterol and physical activity remain potentially attainable. However, attaining the targets for blood pressure among women, obesity and diabetes appears more challenging because recent adverse trends would have to be reversed.3
Successfully reducing population risk factor levels to those already seen in the healthiest (low-risk) stratum could result in approximately 370 000 fewer CHD deaths among people aged 25–84 years in the United States. This figure would represent a 96% decrease in the 388 000 CHD deaths observed in 20001,3 and is somewhat larger than the 85% reduction predicted by other studies.24,25 Although probably an overestimate, the results for this third scenario show an aspirational ideal to highlight potential future gains. However, the low-risk stratum in the population of the United States remains frustratingly small, even when defined only by smoking, blood pressure and blood cholesterol: 6% in the 1970s32 and, even now, only 7.5% among whites and 4% among African Americans.33
Achieving reductions
Although fashionable, screening and treating high-risk individuals would necessitate medicating 15–25% of all adults.34,35 Furthermore, the key goal is not intervention but sustained risk factor reductions.35 The whole population approach described by Rose13 appears both more effective and cost-effective.13–15 Similar conclusions have been reported previously in Dutch, Finnish and American cohorts.12,35
Lowering total blood cholesterol should therefore remain a priority in the United States, as every 1 mg/dl decrease in cholesterol offers a potentially powerful 1% reduction in mortality.6 Large blood cholesterol declines have already been achieved by comprehensive national policies elsewhere (20% in Finland18 and 15% in Mauritius36). In contrast, the United States mean total blood cholesterol fell a mere 3% in adults (from 206 to 201 mg/dl) between 1988 and 2004.37 Furthermore, these levels remain well above the optimal, prompting recent national dietary policies to further reduce total blood cholesterol levels.2,3,38
Smoking prevalence remains above 20% overall in the United States and is even higher in specific groups. This represents substantial room for improvement. Success in reducing tobacco use requires two comprehensive strategies: preventing young people from starting to smoke, and promoting cessation among smokers.39 Success has been attained with intensive anti-smoking programmes in California (United States);40 advertising bans in Finland, Iceland and Norway; and smoke-free environment legislation in Ireland, Italy, Scotland and New York City in the United States,41 to cite some examples. It is encouraging that many more states in the United States are now passing laws requiring smoke-free environments.41
The recent blood pressure trends in women are alarming. High blood pressure is a powerful risk factor; every 1 mmHg reduction in the mean population systolic blood pressure could prevent approximately 10 000 CHD deaths each year in the United States.7 Furthermore, mean population blood pressure has been decreasing in most industrialized countries in recent decades as a result of dietary trends rather than use of medications.42–44 The American Public Health Association has called on industry to reduce the salt content of processed foods over the next decade, and this may contribute to meeting the dietary guidelines for daily sodium intake of < 2300 mg.44,45
As our analysis suggests, current adverse trends in the United States in obesity and diabetes prevalence and blood pressure in women will probably cause approximately 30 000 additional CHD deaths in 2010. Obese individuals with pre-diabetes can benefit from a combination of diet, exercise counselling and behaviour therapy,46 but prevention is preferable. Yet today’s obesogenic environment is reinforced by powerful commercial, political, economic and social factors,47 and reversing these trends is a daunting task that will require substantial efforts.2,3,32
In the United States, recent increases in physical activity, echoing trends in Canada, Finland and elsewhere, are encouraging.5,18,48 Although engaging in adequate physical activity confers many health benefits, we found that in the United States, as elsewhere, reductions in CHD mortality would be modest.15,23 Interventions promoting physical activity among individuals seldom show long-term sustainability.48 However, physical activity in populations may be increased by 4% to 9% through multiple interventions.23,49
The IMPACT model
For our current analyses we used the validated IMPACT model for the United States.10 Recent high-quality data from NHANES and other large national studies reflect many events in a very large population. The model is comprehensive and transparent; it uses recent, reliable and reasonably precise age-specific regression coefficients from substantial meta-analyses6,7 and relative risk values obtained from the large INTERHEART study.27 Every key assumption is addressed and justified in Appendix A (available at: http://content.nejm.org/cgi/data/356/23/2388/DC1/1).
All models are simplifications of reality, with clear limitations. First, this model considered only mortality, not morbidity. However, our estimates of fewer deaths can easily be translated into a 12-fold increase in life-years gained.50 Second, the model only explained 91% of the mortality decrease, leaving 9% unexplained. Third, several assumptions were necessary, one of them being that any delay in mortality reduction (lag time) would be relatively unimportant over a 10-year scenario.10,17,23 However, extending the projections from 2000–2010 to 2000–2015 would generate very similar results. Although all coefficients were independent, coming from multivariate logistic regression analyses,6,7,27 some may not have been fully adjusted and thus “residual confounding” may remain, along with some imprecision.10 Furthermore, the population-attributable risk approach may have slightly overestimated the contributions of diabetes, smoking and physical activity. Some net overestimation of benefits is thus possible, particularly for the ideal scenario. Conversely, underestimation was also possible because the model assumed similar change across the population. Larger reductions among older, more motivated individuals with higher mortality rates might generate greater benefits.
Model development and comparisons with other models may be useful, along with consideration of “novel” risk factors, such as high levels of C-reactive protein.2,3,51 For future studies, it may also be useful to perform economic and ethnic analyses and to validate the model using 2010 data when they become available. However, our rigorous sensitivity analyses were reassuring, for they suggest that the key findings are unlikely to change substantially.10,17,23 Moreover, even crude estimates are potentially valuable for planners and policy-makers.
Conclusion
In conclusion, implementing evidence-based policies to better control tobacco use and achieve a healthier diet across the population could potentially halve future CHD deaths in the United States. ■
Acknowledgements
We thank Wayne H Giles, Umed A Ajani and Thomas E Kottke for their helpful comments on the original model.
Footnotes
Funding: This study was supported by investigator salaries only – Higher Education Funding Council for England (SC, JAC) and United States Centers for Disease Control and Prevention (ESF, JBC, KJG, DRL).
Competing interests: None declared.
References
- 1.Heart disease and stroke statistics: 2008 update Dallas, TX: American Heart Association; 2008. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the US from 1980 through 2002: concealed levelling of mortality rates. J Am Coll Cardiol. 2007;50:2128–32. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health and Human Services. Healthy people 2010: understanding and improving health and objectives for improving health Washington, DC: Government Printing Office; 2000. Available from: http://www.cdc.gov/nchs/hphome.htm [accessed on 5 October 2009].
- 4.Public health action plan to prevent heart disease and stroke Atlanta, GA: Centers for Disease Control and Prevention; 2008. Available from: http://www.cdc.gov/dhdsp/library/action_plan/index.htm [accessed on 5 October 2009].
- 5.Centers for Disease Control and Prevention Prevalence of no leisure-time physical activity – 35 states and the District of Columbia, 1988–2002. MMWR Morb Mortal Wkly Rep. 2004;53:82–6. [PubMed] [Google Scholar]
- 6.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–72. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 8.Bogers RP, Bemelmans WJ, Hoogenveen RT, Boshuizen HC, Woodward M, Knekt P, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167:1720–8. doi: 10.1001/archinte.167.16.1720. [DOI] [PubMed] [Google Scholar]
- 9.Hunink MG, Goldman L, Tosteson AN, Mittleman MA, Goldman PA, Williams LW, et al. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535–42. doi: 10.1001/jama.277.7.535. [DOI] [PubMed] [Google Scholar]
- 10.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in mortality from coronary heart disease in the United States between 1980 and 2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices – Modeling Studies. Value Health. 2003;6:9–17. doi: 10.1046/j.1524-4733.2003.00234.x. [DOI] [PubMed] [Google Scholar]
- 12.Goldman L, Phillips KA, Coxson P, Goldman PA, Williams L, Hunink MG, et al. The effect of risk factor reductions between 1981 and 1990 on coronary heart disease incidence, prevalence, mortality and cost. J Am Coll Cardiol. 2001;38:1012–7. doi: 10.1016/S0735-1097(01)01512-1. [DOI] [PubMed] [Google Scholar]
- 13.Rose G. The strategy of preventive medicine Oxford: Oxford University Press; 1992. [Google Scholar]
- 14.Emberson J, Whincup P, Morris R, Walker M, Ebrahim S. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur Heart J. 2004;25:484–91. doi: 10.1016/j.ehj.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 15.McPherson K, Britton A, Causer L. Coronary heart disease: estimating the impact of changes in risk factors London: National Heart Forum; 2002. pp. 1-60 [Google Scholar]
- 16.Capewell S, Beaglehole R, Seddon M, McMurray J. Explanation for the decline in coronary heart disease mortality in Auckland, New Zealand, between 1982 and 1993. Circulation. 2000;102:1511–6. doi: 10.1161/01.cir.102.13.1511. [DOI] [PubMed] [Google Scholar]
- 17.Unal B, Critchley JA, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation. 2004;109:1101–7. doi: 10.1161/01.CIR.0000118498.35499.B2. [DOI] [PubMed] [Google Scholar]
- 18.Laatikainen T, Critchley J, Vartiainen E, Salomaa V, Ketonen M, Capewell S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol. 2005;162:764–73. doi: 10.1093/aje/kwi274. [DOI] [PubMed] [Google Scholar]
- 19.Critchley J, Liu J, Zhao D, Wei W, Capewell S. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation. 2004;110:1236–44. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]
- 20.Bots ML, Grobbee DE. Decline of coronary heart disease mortality in the Netherlands from 1978 to 1985: contribution of medical care and changes over time in presence of major cardiovascular risk factors. J Cardiovasc Risk. 1996;3:271–6. doi: 10.1097/00043798-199606000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Vartiainen E, Puska P, Pekkanen J, Tuomilehto J, Jousilahti P. Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. BMJ. 1994;309:23–7. doi: 10.1136/bmj.309.6946.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Critchley JA, Capewell S. Substantial potential for reductions in coronary heart disease mortality in the UK through changes in risk factor levels. J Epidemiol Community Health. 2003;57:243–7. doi: 10.1136/jech.57.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unal B, Critchley JA, Capewell S. Small changes in UK cardiovascular risk factors could halve coronary heart disease mortality. J Clin Epidemiol. 2005;58:733–40. doi: 10.1016/j.jclinepi.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282:2012–8. doi: 10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 25.Daviglus ML, Stamler J, Pirzada A, Yan LL, Garside DB, Liu K, et al. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292:1588–92. doi: 10.1001/jama.292.13.1588. [DOI] [PubMed] [Google Scholar]
- 26.Unal B, Critchley J, Capewell S. IMPACT, a validated comprehensive coronary heart disease model: overview and technical appendices Liverpool: Liverpool University; 2007. Available from: http://www.liv.ac.uk/PublicHealth/sc/bua/impact.html [accessed on 5 October 2009].
- 27.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 28.Briggs A, Sculpher M, Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health Econ. 1994;3:95–104. doi: 10.1002/hec.4730030206. [DOI] [PubMed] [Google Scholar]
- 29.Naidoo B, Thorogood M, McPherson K, Gunning-Schepers LJ. Modelling the effects of increased physical activity on coronary heart disease in England and Wales. J Epidemiol Community Health. 1997;51:144–50. doi: 10.1136/jech.51.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Capewell S. Predicting future coronary heart disease deaths in Finland and elsewhere. Int J Epidemiol. 2006;35:1253–4. doi: 10.1093/ije/dyl158. [DOI] [PubMed] [Google Scholar]
- 31.Capewell S, Unal B, Critchley JA, McMurray JJ. Over 20 000 avoidable coronary deaths in England and Wales in 2000: the failure to give effective treatments to many eligible patients. Heart. 2006;92:521–3. doi: 10.1136/hrt.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daviglus ML, Liu K. Today’s agenda: we must focus on achieving favorable levels of all risk factors simultaneously. Arch Intern Med. 2004;164:2086–7. doi: 10.1001/archinte.164.19.2086. [DOI] [PubMed] [Google Scholar]
- 33.Hozawa A, Folsom AR, Sharrett R, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: comparison of African American with white subjects - Atherosclerosis Risk in Communities Study. Arch Intern Med. 2007;167:573–9. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 34.Manuel DG, Kwong K, Tanuseputro P, Lim J, Mustard CA, Anderson GM, et al. Effectiveness and efficiency of different guidelines on statin treatment for preventing deaths from coronary heart disease: modelling study. BMJ. 2006;332:1419–24. doi: 10.1136/bmj.38849.487546.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Capewell S. Will screening individuals at high risk of cardiovascular events deliver large benefits? No. BMJ. 2008;337:a1395. doi: 10.1136/bmj.a1395. [DOI] [PubMed] [Google Scholar]
- 36.Dowse GK, Gareeboo H, Alberti KG, Zimmet P, Tuomilehto J, Purran A, et al. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non-communicable disease intervention programme in Mauritius. Mauritius Non-communicable Disease Study Group. BMJ. 1995;311:1255–9. doi: 10.1136/bmj.311.7015.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, et al. Trends in serum lipids and lipoproteins of adults, 1960. JAMA. 2005;294:1773–81. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 38.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S.American Heart Association Nutrition Committee, et alDiet and lifestyle recommendations revision 2006: a scientific statement from the AHA Nutrition Committee. Circulation 200611482–96. 10.1161/CIRCULATIONAHA.106.176158 [DOI] [PubMed] [Google Scholar]
- 39.Framework Convention for Tobacco Control [internet site]. Geneva: World Health Organization; 2004. Available from: http://www.who.int/fctc/en/ [accessed on 5 October 2009].
- 40.Fichtenberg CM, Glantz SA. Association of the California Tobacco Control Program with declines in cigarette consumption and mortality from heart disease. N Engl J Med. 2000;343:1772–7. doi: 10.1056/NEJM200012143432406. [DOI] [PubMed] [Google Scholar]
- 41.Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359:482–91. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 42.Tunstall-Pedoe H, Connaghan J, Woodward M, Tolonen H, Kuulasmaa K. Pattern of declining blood pressure across replicate population surveys of the WHO MONICA project, mid-1980s to mid-1990s, and the role of medication. BMJ. 2006;332:629–35. doi: 10.1136/bmj.38753.779005.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension. 2003;42:1093–9. doi: 10.1161/01.HYP.0000102864.05174.E8. [DOI] [PubMed] [Google Scholar]
- 44.Havas S, Roccella EJ, Lenfant C. Reducing the public health burden from elevated blood pressure levels in the United States by lowering intake of dietary sodium. Am J Public Health. 2004;94:19–22. doi: 10.2105/AJPH.94.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dietary guidelines for Americans Washington, DC: United States Department of Health and Human Services,/Department of Agriculture; 2005.
- 46.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jain A. Treating obesity in individuals and populations. BMJ. 2005;331:1387–90. doi: 10.1136/bmj.331.7529.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Craig CL, Russell SJ, Cameron C, Bauman A. Twenty-year trends in physical activity among Canadian adults. Can J Public Health. 2004;95:59–63. doi: 10.1007/BF03403636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tudor-Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi-experimental comparison of results from Wales and a matched reference area. BMJ. 1998;316:818–22. doi: 10.1136/bmj.316.7134.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Unal B, Critchley J, Fidan D, Capewell S. Life-years gained from modern cardiological treatments and population risk factor changes in England and Wales, 1981–2000. Am J Public Health. 2005;95:103–8. doi: 10.2105/AJPH.2003.029579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brotman DJ, Walker E, Lauer MS, O’Brian RG. In search of fewer independent risk factors. Arch Intern Med. 2005;165:138–45. doi: 10.1001/archinte.165.2.138. [DOI] [PubMed] [Google Scholar]