Abstract
Objective
To evaluate the cost-effectiveness of topical emollients, sunflower seed oil (SSO) and synthetic Aquaphor, versus no treatment, in preventing mortality among hospitalized preterm infants (< 33 weeks gestation) at a tertiary hospital in Bangladesh.
Methods
Evidence from a randomized controlled efficacy trial was evaluated using standard Monte Carlo simulation. Programme costs were obtained from a retrospective review of activities. Patient costs were collected from patient records. Health outcomes were calculated as deaths averted and discounted years of life lost (YLLs) averted. Results were deemed cost-effective if they fell below a ceiling ratio based on the per capita gross national income of Bangladesh (United States dollars, US$ 470).
Findings
Aquaphor and SSO were both highly cost-effective relative to control, reducing neonatal mortality by 26% and 32%, respectively. SSO cost US$ 61 per death averted and US$ 2.15 per YLL averted (I$ 6.39, international dollars, per YLL averted). Aquaphor cost US$ 162 per death averted and US$ 5.74 per YLL averted (I$ 17.09 per YLL averted). Results were robust to sensitivity analysis. Aquaphor was cost-effective relative to SSO with 77% certainty: it cost an incremental US$ 26 more per patient treated, but averted 1.25 YLLs (US$ 20.74 per YLL averted).
Conclusion
Topical therapy with SSO or Aquaphor was highly cost-effective in reducing deaths from infection among the preterm neonates studied. The choice of emollient should be made taking into account budgetary limitations and ease of supply. Further research is warranted on additional locally available emollients, use of emollients in community-based settings and generalizability to other geographic regions.
Résumé
Objectif
Évaluer le rapport coût/efficacité d’émollients topiques, à savoir l’huile de tournesol et l’Aquafor synthétique, par rapport à l’absence de traitement, dans la prévention de la mortalité chez les nourrissons prématurés (moins de 33 semaines de gestation) hospitalisés dans un hôpital tertiaire du Bangladesh.
Méthodes
Les éléments fournis par un essai d’efficacité contrôlé et randomisé ont été évalués à l’aide d’une simulation de Monte Carlo classique. Les coûts programmatiques ont été déterminés à partir d’une revue rétrospective des activités. Les coûts pour les patients ont été relevés dans les dossiers des patients. Les résultats sanitaires ont été calculés sous forme de décès évités et d’années de vie perdues (YLL) évitées. Les résultats ont été jugés comme offrant un bon rapport coût/efficacité s’ils restaient inférieurs à un taux plafond déterminé à partir du revenu national brut par habitant du Bangladesh (en dollars des États-Unis d’Amérique, US $ 470).
Résultats
L’Aquafor et l’huile de tournesol présentaient l’un et l’autre un rapport coût/efficacité nettement supérieur à la valeur de référence, réduisant la mortalité néonatale de 26 % et 32 % respectivement. Le coût de l’huile de tournesol était de US $ 61 par décès évité et de US $ 2,15 par YLL évitée (6,39 dollars internationaux par YLL évitée). Celui de l’Aquafor était de US $ 162 par décès évité et de US $ 5,74 par YLL évitée (I$ 17,09 par YLL évitée). Ces résultats n’ont pas été remis en question par l’analyse de sensibilité. L’Aquafor présentait un meilleur rapport coût/efficacité que l’huile de tournesol avec une certitude de 77% : il coûtait US $ 26 de plus par patient traité, mais permettait d’éviter 1,25 YLL (US $ 20,74 par YLL évitée).
Conclusion
Le traitement topique par l’huile de tournesol ou l’Aquafor s’est révélé d’un très bon rapport coût/efficacité pour réduire la mortalité par infection chez les nouveau-nés prématurés étudiés. Il faut choisir l’émollient en prenant en compte les contraintes budgétaires et la facilité d’approvisionnement. Il serait justifié d’entreprendre des recherches supplémentaires sur d’autres émollients disponibles localement, sur l’utilisation d’émollients dans un contexte communautaire et sur les possibilités de généralisation à d’autres zones géographiques.
Resumen
Objetivo
Evaluar la costoeficacia de los emolientes tópicos a base de aceite de girasol y del producto sintético Aquaphor en comparación con la ausencia de tratamiento como medida de prevención de la mortalidad de los lactantes prematuros (< 33 semanas de gestación) en un hospital terciario de Bangladesh.
Métodos
Los datos, obtenidos en un ensayo aleatorizado controlado de la eficacia, fueron evaluados mediante el método estándar de simulación de Montecarlo. Los costos de los programas se determinaron mediante una revisión retrospectiva de las actividades, y los costos para los pacientes se determinaron a partir de su historia clínica. Los resultados sanitarios se calcularon como el número de defunciones evitadas y de años de vida perdidos (AVP) descontados evitados. Se consideraron costoeficaces los resultados inferiores a un límite máximo basado en el ingreso nacional bruto por habitante de Bangladesh, 470 dólares estadounidenses (US$).
Resultados
Tanto el Aquaphor como el aceite de girasol fueron muy costoeficaces en comparación con la situación de control, pues redujeron la mortalidad neonatal en un 26% y un 32%, respectivamente. El costo del aceite de girasol fue de US$ 61 por muerte evitada, y de US$ 2,15 por AVP evitado (6,39 dólares internacionales, I$, por AVP evitado). El costo del Aquaphor fue de US$ 162 por muerte evitada y US$ 5,74 (I$ 17,09) por AVP evitado. Los resultados demostraron ser robustos en el análisis de sensibilidad. El Aquaphor fue costoeficaz en comparación con el aceite de girasol con un grado de certidumbre del 77%: cuesta US$ 26 más por paciente tratado, pero evita 1,25 AVP (US$ 20,74 por AVP evitado).
Conclusión
La administración tópica de aceite de girasol o Aquaphor fue muy costoeficaz como medida de reducción de las muertes por infección entre los recién nacidos prematuros estudiados. La elección del emoliente debería hacerse teniendo en cuenta las limitaciones presupuestarias y la agilidad del suministro. Se requieren nuevas investigaciones sobre otros emolientes disponibles a nivel local, sobre el uso de emolientes en entornos comunitarios y sobre la generalización a otras regiones geográficas.
ملخص
الغرض
تقييم مردود تكلفة المُطرّيات الموضعية، وزيت بذرة دوار الشمس، والأكوافور المُصنّع، مقارنة بعدم المعالجة، في توقي الوفيات بين الولدان الخدج المنومين في المستشفى (وكان عمرهم الحملي أقل من 33 أسبوعاً) في أحد المستشفيات الثالثية في بنغلاديش.
الطريقة
جرى تقييم البيّنات الخاصة بتجربة معشاة ذات شواهد باستخدام محاكاة مونت كارلو المعيارية. جمعت تكاليف البرنامج عن طريق المراجعة الاستعادية للأنشطة. وجمعت تكاليف المرضى من سجلات المرضى. وجرى حساب النتائج الصحية مثل تفادي الوفيات وسنوات العمر المفقودة التي تم خفضها. واعتُبِرَت النتائج ذات مردود مقابل التكلفة إذا كانت أقل من معدل الحد الأقصى وذلك اعتماداً على نصيب الفرد من الناتج القومي الإجمالي في بنغلاديش (والبالغ 470 دولار أمريكي).
الموجودات
كان لكل من الأكوافور وزيت بذرة دوار الشمس مردوداً عالياً مقابل التكلفة مقارنة بالشواهد، وخفضا وفيات الولدان بنسبة 26% و 32% بالترتيب. وبلغتت تكلفة زيت بذرة دوار الشمس 61 دولاراً أمريكياً لكل وفاة يمكن تفاديها، و2.15 دولار مقابل كل سنة مفقودة من العمر أمكن تفاديها (أي 6.39 دولار دولي، لكل سنة مفقودة من العمر أمكن تفاديها). وبلغت تكلفة الأكوافور 162 دولاراً أمريكياً لكل وفاة أمكن تفاديها و 5.74 دولارات أمريكية لكل سنة مفقودة من العمر أمكن تفاديها (أي 17.09 دولار دولي لكل سنة مفقودة من العمر أمكن تفاديها). وكانت النتائج صامدة أمام تحليل الحساسية. وكانت تكلفة الأكوافور فعالة مقارنة بزيت بذرة دوار الشمس بنسبة تأكيد 77%: وتكلفته تزيد بمقدار 26 دولاراً أمريكياً مقابل معالجة المريض الواحد، ولكنه يؤدي إلى تجنب 1.25 سنة مفقودة من العمر (أي 20.74 دولار أمريكي لكل سنة مفقودة من العمر أمكن تفاديها).
الاستنتاج
المعالجة الموضعية بزيت بذرة دوار الشمس أو الأكوافور لها مردوداً عالياً مقابل التكلفة في خفض الوفيات الناجمة عن العدوى بين الولدان الخدج قيد الدراسة. وعند اختيار المُطرّيات يجب الأخذ في الحسبان قيود الميزانية وسهولة الإمدادات.وهناك مبررات لإجراء المزيد من الدراسات على المُطرّيات الإضافية المتاحة محلياً، واستخدامها في المواقع المجتمعية المرتكز وإمكانية تعميمها في المناطق الجغرافية الأخرى.
Introduction
An estimated 4 million children worldwide die each year during the neonatal period, three fourths of them within the first 7 days.1 The overwhelming majority (99%) of neonatal deaths occur in low- and middle-income settings and are caused directly by infections and complications due to prematurity and birth asphyxia and indirectly by low birth weight (< 2500 g).1 Infants born very preterm (i.e. gestational age < 32 weeks) and with very low birth weight (< 1500 g) have mortality rates of over 50% in many low-resource settings2–5 and are at high risk for long-term disabilities and impairments.6
Premature infants have compromised skin barrier function, which increases their risk of infection7–9 and of hypothermia due to transepidermal water and heat loss.10,11 Undernutrition further impairs skin barrier function and compromises the immune system, increasing the risk of morbidity and mortality.12,13
Application of topical emollients has been practised traditionally in South Asia and sub-Saharan Africa for generations. It has a variety of perceived benefits, although some of the emollients used may be detrimental, depending on their composition and mode of application.14–16 Mustard seed oil is the most widely used emollient in South Asia owing to its fragrance, warming sensation and availability; however, it may be toxic to keratinocytes of the skin.15–17 Research on the impact of four natural oils and of Aquaphor, a synthetic emollient, on epidermal barrier function in mice has shown that mustard seed oil has deleterious effects on the epidermal barrier.14 By contrast, sunflower seed oil (SSO) and Aquaphor significantly accelerate barrier recovery.14
Aquaphor and SSO were tested in randomized controlled trials in Bangladesh and Egypt.4 In Bangladesh, massage with SSO resulted in a 41% reduction in sepsis and a 26% reduction in mortality,5,18 while Aquaphor treatment resulted in 32% lower mortality among treated infants relative to controls.5
The efficacy of this trial highlights the potential for low-cost, culturally acceptable alternatives to replace mustard seed oil for treating preterm, low-birth-weight infants in South Asia.5 The Disease Control Priorities Project (DCP2) has identified research on emollients as a global priority.19 In particular, evidence is needed to inform decision-making about how the use of emollients should be prioritized in health policy. This paper presents data on the cost-effectiveness of SSO and Aquaphor therapy versus standard care for preterm neonates at a tertiary hospital in Bangladesh.
Methods
Study site and population
Bangladesh is characterized by high rates of maternal and neonatal undernutrition, prematurity (gestational age < 37 weeks) (19%),20 low birth weight (30%) and neonatal mortality (42 per 1000 live births).21 A prospective randomized controlled trial was conducted to ascertain the impact of topical emollients on rates of sepsis and mortality in preterm infants admitted to Dhaka Shishu Hospital in Dhaka, Bangladesh, between December 1998 and July 2003. With a total of 320 paediatric beds, Dhaka Shishu is the largest tertiary-level paediatric hospital in the country. It has extensive laboratory capabilities in addition to a 20-bed special care nursery, which generally operates at full capacity.5,18
A total of 497 preterm, low-birth-weight neonates were randomly assigned to one of three treatment groups: SSO (n = 159 141 < 1500 g), Aquaphor (n = 157; 138 < 1500 g) and control (n = 181; 154 < 1500 g). Eligibility for enrolment in the trial was limited to preterm infants (< 33 weeks gestational age) presenting to hospital for care within 72 hours of birth. Infants were excluded if they had major congenital abnormalities, hydrops fetalis, conditions requiring major surgery, clinically evident skin infections, generalized skin disease or structural epidermal defects covering over 5% of the body, or if they were expected to die within 48 hours. This trial has been registered (MS# 2007-0213 Clinical Trials.gov #98-04-21-03-2) and additional information on the trial is detailed elsewhere.5,7,18,22
Description of interventions
The emollients tested in this trial were high-linoleate SSO (Omega Nutrition, Bellingham, WA, USA) and Aquaphor, a synthetic emollient consisting of petroleum, mineral oil, mineral wax and lanolin alcohol (Beiersdorf, Norwalk, CT, USA). Control infants received standard care without any oil or massage and were managed on an intention-to-treat basis. Study nurses applied 4 g of emollient per kilogram of body weight (in 100 g graduations) three times daily for 14 days, then two times daily for every day thereafter. Risk factors for nosocomial infections were minimized through infection control practices,23 and blood cultures were obtained from infants suspected of systemic infection. Health complications were treated appropriately. Physicians were masked to treatment group assignment, although distinct differences in emollient consistency made complete assurance of masking uncertain.
Health outcomes
The primary health outcome measured was 28-day survival, adjusted according to hazard ratios between intervention and control groups.5 Deaths averted were translated to discounted years of life lost (YLL) averted,24 consistent with cost-effectiveness analyses of other neonatal care interventions.19 Reference case assumptions included an average life expectancy at birth of 62.6 years25 and a discount rate of 3%, in keeping with standard practice in economic evaluation for low- and middle-income countries.26 However, empirical evidence from developing country settings suggests that 6% may better represent social preferences, and this was tested in sensitivity analysis.27 Age-weighting was excluded from reference case calculations for consistency with the analyses presented in DCP2,26 but was also tested in sensitivity analysis.
Costing
Economic costs for the 20-bed nursery staffed with 6 physicians, 4 nurses and 1 laboratory technician were calculated from a provider and programme perspective through a retrospective review of individual patient records and project activities. Programme costs included activities required to initiate and implement the study and were distributed evenly across intervention arms. One-time start-up activities included administrative time required to prepare for the study, identification of emollient supply, investigator time to develop a manual on emollient application, and nurse orientation and training in emollient application and data collection. Implementation costs for the remainder of the project included costs associated with refresher training of nurses (half a day three times each year). Provider costs included emollient treatments, antibiotics and other medications, blood transfusions, medical supplies, laboratory tests, bed costs and food.
Cost per bed-day was 300 Bangladeshi taka (US$ 5.95), calculated on the basis of hospital charges to patients; shadow prices were used for patients treated free of charge. Costs per day charged to patients were validated through costing by the health facility, including capturing of actual electricity and overhead costs. These costs were comparable to figures reported by the World Health Organization (WHO) Choosing Interventions that are Cost-Effective (WHO-CHOICE) project.28 All costs associated with research components of the trial were excluded, as were opportunity costs incurred by household members for lost wages and transportation. Costs were converted to 2006 base-year dollars using local consumer price indices. Start-up costs were expected to be amortized over two years and were annualized and discounted at 3%. All costs were converted from Bangladeshi taka to United States dollars (US$) using a 2006 exchange rate29 and were also converted to international dollars (I$) to make them comparable to WHO-CHOICE figures.28 International dollars have the same purchasing power as a US dollar in the United States. International dollar values were determined by dividing taka by the 2006 purchasing power parity (PPP) conversion factor.
Cost-effectiveness
The cost-effectiveness of each pair of strategies (SSO versus control, Aquaphor versus control, SSO versus Aquaphor) was evaluated according to incremental cost-effectiveness ratios (ICERs). Reference case calculations included all costs and YLLs calculated with a 3% discount rate and no age–weighting (3,0). The impact of uncertainty regarding patient-level costs and health outcome data was accounted for through probabilistic sensitivity analysis, using standard Monte-Carlo simulation resampling.30 In this method, data points were randomly sampled from original data, with replacement, and ICERs were calculated. This process was repeated to represent what results might arise if a large number of similar trials were performed. These calculations were performed in Excel (Microsoft, Redmond, WA, USA), using a Visual Basic-based macro to perform the resample automatically.
In total, 10 000 iterations were generated for each simulation and plotted on two-dimensional cost-effectiveness planes.30 In accordance with precedent from the Commission on Macroeconomics and Health, outputs were evaluated against a ceiling ratio based on the per capita gross national income of Bangladesh (US$ 470).31 Results were presented as cost-effectiveness acceptability curves, which are standardized tools for summarizing the probability of cost-effectiveness based on variations in the ceiling ratio.32 Additional sensitivity analyses were conducted on total costs by increasing and decreasing estimates by 25%. Finally, sensitivity analyses were also performed on the assumptions underpinning YLLs averted.24,26
Results
Results are presented in terms of 100 premature neonates, a number that approximates the number of premature neonates who might be treated at a similar facility per year.
Costs
Table 1 outlines programme costs for initiating study activities and maintain training (US$ 917 per arm). These costs were equal to 5% and 4% of total costs in the SSO and Aquaphor arms, respectively. Annualized start-up costs were US$ 1014.01 and implementation phase costs were US$ 810.67.
Table 1. Intervention programme costs for a 20-bed nursery in Dhaka Shishu Hospital, a tertiary facility with 320 paediatric beds, Dhaka, Bangladesh, 1998–2003.
| Activity | Total annualized cost in US$ (%) |
|---|---|
| Start-up | 1023.15 (55.8) |
| Administrative set-up | 9.14 (0.5) |
| Orientation for neonatal unit physicians and staff | 178.45 (9.7) |
| Identification of emollient supplier | 137.30 (7.5) |
| Manual on emollient application | 274.59 (15) |
| Training of nurses | 423.67 (23.1) |
| Implementation | |
| Refresher training of nurses | 810.67 (44.2) |
| Total cost | 1833.82 |
US$, United States dollar.
Table 2 shows the distribution of provider costs per patient by study arm and component. Hospital stays were the most expensive component; costs were similar for all three treatment groups, with an average length of stay in days of 11.54 (SSO), 11.76 (Aquaphor) and 11.48 (control). Overall, Aquaphor cost about 20 times as much as SSO, with an average per patient cost of US$ 29 and a unit cost of US$ 0.76 for a single application of 4 g of emollient, or US$ 1.14 for each treatment of a neonate weighing 1500 g. SSO, by comparison, cost an average of US$ 1.55 per patient and had a unit cost of US$ 0.04 for 4 g, or US$ 0.06 for each treatment of an infant weighing 1500 g. All other costs were comparable across arms. The average total cost per patient in the SSO arm was US$ 99.47, compared to US $125.35 in the Aquaphor arm and US$ 93.39 in the control arm.
Table 2. Provider costs per patient, by study arm and component, in clinical trial comparing two topical emollients in preterm infants, Dhaka Shishu Hospital, Dhaka, Bangladesh, 1998–2003.
| Distribution of provider costs in US$ (%) |
|||
|---|---|---|---|
| SSO | Aquaphor | Control | |
| (n = 159) | (n = 157) | (n = 181) | |
| Emollient | 1.55 (1.56) | 29.00 (21.13) | None |
| Druga | 8.02 (8.06) | 7.40 (5.90) | 7.90 (8.46) |
| Medical suppliesb | 4.59 (4.61) | 4.60 (3.67) | 4.53 (4.85) |
| Laboratory testsc | 6.12 (6.15) | 5.62 (4.48) | 5.70 (6.10) |
| Hospital stayd | 68.89 (69.26) | 69.60 (55.53) | 66.57 (71.28) |
| Maternal meals | 6.99 (7.03) | 7.04 (5.62) | 6.75 (7.23) |
| Blood transfusion | 3.32 (3.34) | 2.08 (1.66) | 1.95 (2.08) |
| Total | 99.47e | 125.35e | 93.39e |
SSO, sunflower seed oil; US$, United States dollar. a Injections of antibiotics, intravenous saline, syrups and other medications. b Catheters, intravenous tubing, syringes, needles, gauze and other medical supplies. c All laboratory exams: blood cultures, blood urea, bilirubin, serum electrolytes and other laboratory tests. d Derived by taking the 300 taka (US$ 5.95 per day) charged by the hospital per day, inclusive of staff time, capital, facility administrative and overhead costs, and multiplying that by the duration of stay. Shadow prices were used for patients treated at no charge. e Inconsistencies arise due to rounding.
Health outcomes
The 26% reduction in mortality with SSO treatment corresponded to an adjusted probability of death of 52%,5 and translated to 19 deaths averted per 100 neonates, or 523 YLLs averted given an average lifespan in Bangladesh of 62.6 years (discounted to 28.24 YLLs (3,0) (Table 3). Aquaphor reduced mortality by 32%; this outcome was associated with an adjusted probability of death of 48% and 23 deaths averted, or 649 YLLs per 100 neonates (Table 3).5
Table 3. Deaths and YLLs averted and associated costs per 100 neonates, by study arm, in clinical trial comparing two topical emollients in preterm infants, Dhaka Shishu Hospital, Dhaka, Bangladesh, 1998–2003.
| Deaths averted | YLLs averted | Incremental cost (US$) | Cost per death averted (US$) | Cost per YLL averted (US$) | |
|---|---|---|---|---|---|
| SSO vs control | 19 | 523 | 1124 | 61 | 2.15 |
| Aquaphor vs control | 23 | 649 | 3725 | 162 | 5.74 |
| Aquaphor vs SSO | 4 | 125 | 2600 | 586 | 20.74 |
SSO, sunflower seed oil; US$, United States dollar, YLL, year of life lost.
Cost-effectiveness
Per 100 neonates, the total cost of each arm was US$ 10 517 (95% confidence interval, CI: 10 138–10 878) for SSO, US$ 13 117 (95% CI: 12 722–13 509) for Aquaphor and US$ 9393 (95% confidence interval, CI: 9079–9699) for control (confidence intervals bootstrapped from Monte Carlo simulations). Reference case calculations for SSO relative to control found an incremental cost of US$ 1124 for 19 deaths or 523 YLLs averted. This translated to a cost-effectiveness of US$ 61 per death averted, or US$ 2.15 per YLL averted (I$ 6.39 per YLL averted) (Table 3). Aquaphor cost US$ 3725 and averted 649 YLLs relative to control conditions, giving an ICER of US$ 162 per death averted, or US$ 5.74 per YLL averted (I$ 17.09 per YLL averted). Comparison of the two emollients reveals that Aquaphor was more costly but more effective than SSO, with an ICER of US$ 586 per death averted, or US$ 20.74 per YLL averted (I$ 94.35 per YLL averted). Confidence intervals were not determined for ICERs because results extended beyond zero for two of the three comparisons, rendering results not meaningful.
Sensitivity analysis
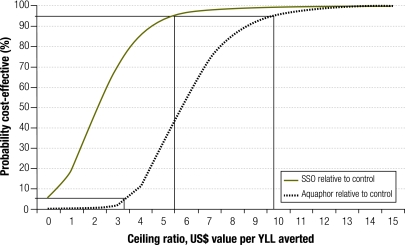
The cost-effectiveness acceptability curves shown in Fig. 1 and Fig. 2 illustrate the degree of uncertainty around each comparison according to different valuations of YLLs. If YLLs are valued above US$ 5.33 (i.e. above the point at which the 95% probability of cost-effectiveness line intersects the x-axis), decision-makers can be 95% certain that using SSO was cost-effective relative to control. The certainty that SSO was cost-effective never fell below 6% at any YLL valuation as there remains a probability that it improves health at a lower cost. Aquaphor was also highly cost-effective relative to the control arm. Above US$ 9.55 per YLL averted it was 95% certain that Aquaphor was cost-effective; below US$ 3.45 per YLL averted, it was 95% certain that it was not. All of these results are well below the per capita gross national income in Bangladesh (US$ 470).25
Fig. 1.
Cost-effectiveness acceptability curves: topical emollient interventions relative to control in a clinical trial in preterm infants, Dhaka Shishu Hospital, Dakha, Bangladesh, 1998–2003
SSO, sunflower seed oil; US$, United States dollar; YLL, years of life lost.
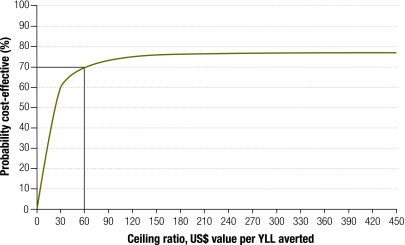
Fig. 2.
Cost-effectiveness acceptability curve in a clinical trial of preterm infants treated with Aquaphor versus SSO, Dhaka Shishu Hospital, Dhaka, Bangladesh, 1998–2003
SSO, sunflower seed oil; US$, United States dollar; YLL, years of life lost.
When the two intervention strategies are compared, Aquaphor is more cost-effective, although a decision-maker can never be more than 77% certain of this result (Fig. 2). This finding is explained by the 21% chance that Aquaphor is more costly and less effective than SSO, coupled with a 2% chance that its cost-effectiveness is above the threshold YLL valuation.
If total arm costs are 25% higher than those found in the trial, the cost-effectiveness of each emollient relative to control remains below US$ 10/YLL (Table 4). Sensitivity analyses on YLL assumptions recommended by Fox-Rushby and Hanson (2001)24 have no effect on the interpretation of ICERs – all remain highly cost-effective.
Table 4. Cost-effectiveness of SSO versus control per YLL averted in a clinical trial comparing two topical emollients in preterm infants,a Dhaka Shishu Hospital, Dhaka, Bangladesh, 1998–2003.
| YLL (3,0)b | YLL (3,1)b | YLL (0,0)b | YLL (6,0)b | |
|---|---|---|---|---|
| YLLs averted | 523 | 587 | 1160 | 302 |
| ICER (US$) | 2.15 | 1.92 | 0.97 | 3.73 |
ICER, incremental cost-effectiveness ratio; SSO, sunflower seed oil; US$, United States dollar; YLL, years of life lost. a Sensitivity analysis per 100 neonates. b YLL (r,K); r = discount rate (3% or 0% or 6%) per year; K = age-weighting present (1) or absent (0).
Discussion
Repeated, gentle massage of neonates’ skin with SSO or Aquaphor was highly cost-effective in reducing neonatal mortality in the intervention groups relative to the control group, even at very low valuations of YLLs. Both emollients substantially improve neonatal survival, owing at least in part to marked reductions in risk of sepsis,4,5,18 although our results may be underestimates as costs associated with the treatment of complications following the neonatal period were not considered and are likely to have been higher in the control group.6 The choice between Aquaphor and SSO is more complicated because each is highly cost-effective, and there is not a significant difference between their efficacies (P = 0.2163). While the Arrow-Lind theorem advocates decision-making using expected values when results are uncertain,33 decision-making depends on a variety of economic and ethical factors, particularly available budget to reach target coverage levels.26
Public financing of emollient treatment may be warranted for both economic and ethical reasons. In addition to being cost-effective, it has notable externalities: it can prevent infectious disease from spreading to others and may also prevent disabilities that require lifelong medical treatment and support from caregivers. The expense of Aquaphor would presumably be catastrophic for most Bangladeshi households, which earn on average US$ 38.63 per month;25 at US $29 per patient, Aquaphor treatment would amount to 75% of the average monthly salary, which is well above the WHO definition for catastrophic cost (more than 40% of monthly income after subsistence needs have been met).34 From an ethical perspective, 50% of Bangladeshis live below the poverty line,35 and would not be able to afford contributory insurance. With mortality rates in the intervention groups of 48% (Aquaphor) and 52% (SSO) relative to 71% percent in the control group, this intervention is clearly life-saving for a cohort with high mortality, meets the “rule of rescue” criterion and is vertically equitable.36
Many of the same arguments apply to SSO. However, since SSO costs only US$ 1.55 per patient, or 4% of monthly household income, there is greater probability that it could be supported by the private market, which means that smaller incremental policy changes would be required. In Bangladesh and much of the developing world, patients often independently buy medicines recommended for inpatients from pharmacies. Asking already underresourced public health systems to provide additional interventions is difficult, particularly when an estimated US$ 37 million would be needed to provide Aquaphor to 1.3 million low-birth-weight infants per year37 – a sum that amounts to slightly less than 3% of total national health expenditure.38
On one hand, investment by high-income countries in developing country health systems is increasing;39 however, sustainable change can be expected to occur gradually, and investors generally shun environments with high disease burdens. It could be argued that national governments have the capacity to determine how much revenue they raise through taxation and should finance all interventions deemed cost-effective,40 but experience shows that revenue targets are not always achieved in reality.41 While the choice of emollient will depend on the ease of maintaining a reliable supply and on local preference,16,17 Aquaphor will become more attractive when single-use ointment tubes are manufactured – which will avoid bedside contamination of the product42 – and when the cost falls through bulk purchasing.
Comparison to other studies
This is the first study on the cost-effectiveness of emollients to protect premature neonates in low-resource settings. The efficacy data generated by the clinical trial underlying this analysis5,18 are corroborated by a smaller study conducted in Egypt, which documented a 54% reduction in sepsis and found a trend in reduction in mortality, although statistical power was insufficient.4 Neither of these trials found adverse outcomes from the intervention, such as skin reactions, injuries, infections or phototherapy burns.4,5,18 Both studies suggest that with careful monitoring it is appropriate for these interventions to be replicated in comparable tertiary-care environments.
Justification for use of YLLs
The limitations of disability-adjusted life years (DALYs) are described elsewhere.43 However, some of the assumptions underlying the DALY can be justified, as some degree of modelling is a “fact of life” in clinical trial-based economic evaluation.44 Defining health outcomes as YLLs facilitates comparison with a wide spectrum of evaluations in large-scale evidence bases such as DCP2.26 There is precedent in the neonatal survival chapter of DCP219 for excluding the years of life with disability (YLD) component of the DALY, which is difficult to observe scientifically; moreover, data from low- and middle-income countries on disabilities stemming from neonatal conditions is lacking.45 However, the Global Burden of Disease study recognizes perinatal illness as the sixth largest contributor to YLDs in low- and middle-income countries.46 In further work, evidence from our trial will be used to inform a calculation framework useful for economic evaluation of neonatal health interventions, although such an analysis is not expected to have a significant effect on our already highly cost-effective results.
Generalizability of findings
The high prevalence of low birth weight (31%)21 and prematurity (16%) and the widespread traditional use of emollients in South Asia2 make it a priority area for research to evaluate the generalizability of our findings.47 Among the interventions recommended by DCP2 for South Asia, estimates of the cost per DALY averted range from US$ 8.00 for childhood immunizations to US$ 260.50 for a package of maternal and neonatal care services.26 SSO and Aquaphor both achieve better cost-effectiveness than all the interventions evaluated in DCP2 for this region. Converted into international dollars, the cost effectiveness of Aquaphor and SSO is I$ 17 and I$ 6 per YLL averted, respectively. These estimates compare favourably with maternal and neonatal interventions for South Asia evaluated by WHO-CHOICE, which range in cost effectiveness from I$ 6 for support for breastfeeding at 50% coverage to I$ 16 930 for a comprehensive package of maternal and neonatal care services at 95% coverage.28
Further research is warranted for other regions of the world with high burdens of neonatal mortality. In both Africa and Asia, the potential benefits of emollient therapy for neonates, regardless of gestational age or birthweight, should be studied, as should its use for babies born at primary care facilities and at home. When costs from the tertiary hospital nursery in this study are scaled up, expected economies of scale in variable costs should be taken into account.
As the majority of neonatal deaths in low-resource settings occur outside the formal health care sector, it is important to understand the sociocultural and contextual factors that affect treatment-seeking behaviour. In many South Asian societies, new mothers enter a period of seclusion from society after delivery, which means that they often do not seek care from the formal health sector for themselves or for their babies.48 As community health workers (CHWs) have been shown to be effective providers in such circumstances,3,49–52 and community-based care has been shown to improve the equity of care distribution,53 research on community-based delivery of emollients is recommended. However, the limitations of the CHW model should be recognized, and the sustainability of behaviour change in non-facility settings should be explored.
Conclusion
The perception exists that hospital care of premature infants is expensive and requires high technology and specialized medical attention. This study suggests that topical treatment with Aquaphor or SSO is highly cost-effective, resulting in significant health improvements among preterm infants, and can be integrated into existing hospital treatment protocols at low cost. This policy change would address two of three intervention objectives outlined by the Lancet Neonatal Survival Series for neonatal care by reducing the need for emergency care and strengthening care for low-birth-weight infants.11 Further research should be conducted on the impact of emollients in community settings so that they can be considered for inclusion in priority packages of community-based neonatal interventions.49,54 The high proportion of births occurring outside the formal health care sector in many high-mortality settings provides further impetus for expanding research on emollients to the community level; however, strategies are needed to address the use of potentially toxic emollients (e.g. use of mustard oil, mixing the emollient with potentially harmful additives) and harmful application techniques, such as too vigorous massage, which can damage the skin barrier, especially in preterm infants.17 Successful implementation of emollient therapy is anticipated to improve health outcomes among neonates in South Asia, and also in sub-Saharan Africa, pending further research, and to facilitate the achievement of the fourth Millennium Development Goal. ■
Acknowledgements
The authors wish to thank Dr Abdullah Baqui for his support of this analysis. In addition, we wish to express our gratitude to AKM Dawlat Khan and Md. Khalid Hassan, whose exhaustive efforts in collecting the data in Bangladesh made this analysis and paper possible. We also thank Sally Schippert for her work on data cleaning during the early stages of analysis and Jacob Allen for designing the Visual Basic macro that facilitated Monte Carlo simulation. Lastly, we are indebted to Kim Mulholland, Barbara Stoll and William Blackwelder for their guidance as members of the parent study’s Data and Safety Monitoring Board.
Gary L Darmstadt is currently Director, Family Health and Strategic Project Team Leader, Maternal, Neonatal and Child Health, Global Health Program, Bill & Melinda Gates Foundation, PO Box 23350, Seattle, WA, 98102, USA.
Footnotes
Funding: This study was supported by the Thrasher Research Fund; the Office of Health, Infectious Diseases and Nutrition, Global Health Bureau, United States Agency for International Development (award HRN‑A-00-96-90006-00); Save the Children-US through a grant from the Bill & Melinda Gates Foundation; and the Society for Pediatric Dermatology.
Competing interests: None declared.
References
- 1.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 2.Yasmin S, Osrin D, Paul E, Costello A. Neonatal mortality of low-birth-weight infants in Bangladesh. Bull World Health Organ. 2001;79:608–14. [PMC free article] [PubMed] [Google Scholar]
- 3.Bang AT, Bang RA, Reddy HM. Home-based neonatal care: summary and applications of the field trial in rural Gadchiroli, India (1993 to 2003). J Perinatol. 2005;25(Suppl 1):S108–22. doi: 10.1038/sj.jp.7211278. [DOI] [PubMed] [Google Scholar]
- 4.Darmstadt GL, Badrawi N, Law PA, Ahmed S, Bashir M, Iskander I, et al. Topically applied sunflower seed oil prevents invasive bacterial infections in preterm infants in Egypt: a randomized, controlled clinical trial. Pediatr Infect Dis J. 2004;23:719–25. doi: 10.1097/01.inf.0000133047.50836.6f. [DOI] [PubMed] [Google Scholar]
- 5.Darmstadt GL, Saha SK, Ahmed AS, Ahmed S, Chowdhury MA, Law PA, et al. Effect of skin barrier therapy on neonatal mortality rates in preterm infants in Bangladesh: a randomized, controlled, clinical trial. Pediatrics. 2008;121:522–9. doi: 10.1542/peds.2007-0213. [DOI] [PubMed] [Google Scholar]
- 6.Khan NZ, Muslima H, Parveen M, Bhattacharya M, Begum N, Chowdhury S, et al. Neurodevelopmental Outcomes of Preterm Infants in Bangladesh. Pediatrics. 2006;118:280. doi: 10.1542/peds.2005-2014. [DOI] [PubMed] [Google Scholar]
- 7.Darmstadt GL, Saha SK, Ahmed AS, Choi Y, Chowdhury MA, Islam M, et al. Effect of topical emollient treatment of preterm neonates in Bangladesh on invasion of pathogens into the bloodstream. Pediatr Res. 2007;61:588–93. doi: 10.1203/pdr.0b013e3180459f75. [DOI] [PubMed] [Google Scholar]
- 8.Darmstadt G, Saha S, Ahmed A, Khatun M, Chowdhury M. The skin as a potential portal of entry for invasive infections in neonates. Perinatology. 2003;5:205–12. [Google Scholar]
- 9.Darmstadt GL, Dinulos JG. Neonatal skin care. Pediatr Clin North Am. 2000;47:757–82. doi: 10.1016/S0031-3955(05)70239-X. [DOI] [PubMed] [Google Scholar]
- 10.Kalia YN, Nonato LB, Lund CH, Guy RH. Development of Skin Barrier Function in Premature Infants. J Invest Dermatol. 1998;111:320–6. doi: 10.1046/j.1523-1747.1998.00289.x. [DOI] [PubMed] [Google Scholar]
- 11.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–88. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 12.Darmstadt GL. The skin and nutritional disorders in the newborn. Eur J Pediatr Dermatol. 1998;8:221–8. [Google Scholar]
- 13.Osendarp SJ, van Raaij JM, Darmstadt GL, Baqui AH, Hautvast JG, Fuchs GJ. Zinc supplementation during pregnancy and effects on growth and morbidity in low birthweight infants: a randomised placebo controlled trial. Lancet. 2001;357:1080–5. doi: 10.1016/S0140-6736(00)04260-4. [DOI] [PubMed] [Google Scholar]
- 14.Darmstadt GL, Mao-Qiang M, Chi E, Saha SK, Ziboh VA, Black RE, et al. Impact of topical oils on the skin barrier: possible implications for neonatal health in developing countries. Acta Paediatr. 2002;91:546–54. doi: 10.1080/080352502753711678. [DOI] [PubMed] [Google Scholar]
- 15.Darmstadt GL, Saha SK. Traditional practice of oil massage of neonates in Bangladesh. J Health Popul Nutr. 2002;20:184–8. [PubMed] [Google Scholar]
- 16.Mullany LC, Darmstadt GL, Khatry SK, Tielsch JM. Traditional massage of newborns in Nepal: implications for trials of improved practice. J Trop Pediatr. 2005;51:82–6. doi: 10.1093/tropej/fmh083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed AS, Saha SK, Chowdhury MA, Law PA, Black RE, Santosham M, et al. Acceptability of massage with skin barrier-enhancing emollients in young neonates in Bangladesh. J Health Popul Nutr. 2007;25:236–40. [PMC free article] [PubMed] [Google Scholar]
- 18.Darmstadt GL, Saha SK, Ahmed AS, Chowdhury MA, Law PA, Ahmed S, et al. Effect of topical treatment with skin barrier-enhancing emollients on nosocomial infections in preterm infants in Bangladesh: a randomised controlled trial. Lancet. 2005;365:1039–45. doi: 10.1016/S0140-6736(05)71140-5. [DOI] [PubMed] [Google Scholar]
- 19.Lawn JE, Zupan J, Begkoyian G, Knippenberg R. Newborn survival. In: Jamison D, Breman J, Measham A, Alleyne G, Cleason M, Evans DB et al., eds. Disease control priorities in developing countries, 2nd ed. Washington, DC: The World Bank and Oxford University Press; 2006. pp. 531-549. [Google Scholar]
- 20.Hosain GM, Chatterjee N, Begum A, Saha SC. Factors associated with low birthweight in rural Bangladesh. J Trop Pediatr. 2006;52:87–91. doi: 10.1093/tropej/fmi066. [DOI] [PubMed] [Google Scholar]
- 21.Save the Children. State of the world’s newborns Washington, DC: Save the Children; 2001. [Google Scholar]
- 22.Choi Y, Saha SK, Ahmed AS, Law PA, Chowdhury MA, Islam M, et al. Routine skin cultures in predicting sepsis pathogens among hospitalized preterm neonates in Bangladesh. Neonatology. 2008;94:123–31. doi: 10.1159/000119722. [DOI] [PubMed] [Google Scholar]
- 23.Darmstadt GL, Nawshad Uddin Ahmed AS, Saha SK, Azad Chowdhury MA, Alam MA, Khatun M, et al. Infection control practices reduce nosocomial infections and mortality in preterm infants in Bangladesh. J Perinatol. 2005;25:331–5. doi: 10.1038/sj.jp.7211283. [DOI] [PubMed] [Google Scholar]
- 24.Fox-Rushby JA, Hanson K. Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis. Health Policy Plan. 2001;16:326–31. doi: 10.1093/heapol/16.3.326. [DOI] [PubMed] [Google Scholar]
- 25.The World Bank. World Development Indicators Data Query website. [Internet site]. Available at: devdata.worldbank.org/data-query. [accessed on 9 November 2009].
- 26.Musgrove P, Fox-Rushby J. Cost-effectiveness analysis for priority setting. In: Jamison D, Breman J, Measham A, Alleyne G, Cleason M, Evans D, eds. Disease control priorities in developing countries, 2nd ed. Washington, DC: The World Bank and Oxford University Press; 2006. pp. 271-285. [Google Scholar]
- 27.Robberstad B. Estimation of private and social time preferences for health in northern Tanzania. Soc Sci Med. 2005;61:1597–607. doi: 10.1016/j.socscimed.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization Choosing interventions that are cost-effective (WHO-CHOICE) [Internet site]. Available at: http://www.who.int/choice/en/ [DOI] [PMC free article] [PubMed]
- 29.International Monetary Fund World Economic Outlook Database [Internet site]. Available at: http://www.imf.org/external/pubs/ft/weo/2009/02/weodata/weorept.aspx?s [accessed on 17 November 2009].
- 30.Drummond M, Sculpher M. Methods for the economic evaluation of health care 3rd Edn. Oxford, Oxford University Press; 2005. [Google Scholar]
- 31.Sachs J. Macroeconomics and health: investing in health for economic development Geneva: World Health Organization; 2001. [Google Scholar]
- 32.Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves – facts, fallacies and frequently asked questions. Health Econ. 2004;13:405–15. doi: 10.1002/hec.903. [DOI] [PubMed] [Google Scholar]
- 33.Arrow KJ, Lind RC. Uncertainty and the evaluation of public investment decisions. Am Econ Rev. 1970;60:364–78. [Google Scholar]
- 34.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 35.United Nations Development Programme. Human development indices New York: United Nations Development Programme; 2008. Available from: http://hdr.undp.org/en/media/HDI_2008_EN_Tables.pdf [accessed on 17 November 2009].
- 36.Musgrove P. Public spending on health care: how are different criteria related? Health Policy. 1999;47:207–23. doi: 10.1016/S0168-8510(99)00024-X. [DOI] [PubMed] [Google Scholar]
- 37.UNICEF. Low birthweight: country, regional and global estimates Geneva: World Health Organization; 2004. [Google Scholar]
- 38.Data International Ltd. Bangladesh National Health Accounts, 1999‑2001 Dhaka, Bangladesh: Health Economics Unit, Ministry of Health and Family Welfare; 2003. Available from: http://www.who.int/nha/docs/en/BangladeshNHA_1999-2001.pdf [accessed on 17 November 2009].
- 39.Schieber G, Gottret P. Health financing revisited: a practitioner’s guide Washington DC: World Bank: 2006. Available from: http://siteresources.worldbank.org/INTHSD/Resources/topics/Health-Financing/HFRFull.pdf [accessed on 27 October 2009].
- 40.Jack W. Public spending on health care: how are different criteria related? a second opinion. Health Policy. 2000;53:61–7. doi: 10.1016/S0168-8510(00)00093-2. [DOI] [PubMed] [Google Scholar]
- 41.Musgrove P. Cost-effectiveness as a criterion for public spending: a reply to William Jack’s ’second opinion’. Health Policy. 2000;54:229–33. doi: 10.1016/S0168-8510(00)00115-9. [DOI] [PubMed] [Google Scholar]
- 42.Ramsey KM, Malone SG, Fey PD. Aquaphor as a source of colonization and subsequent blood stream infections among very low birthweight neonates. [Abstract 53]. Abstracts from the Eighth Annual Scientific Meeting of the Society for Healthcare Epidemiology of America, Orlando, FL, April 1998. Infect Control Hosp Epidemiol. 1998;19:689. [Google Scholar]
- 43.Anand S, Hanson K. Disability-adjusted life years: a critical review. J Health Econ. 1997;16:685–702. doi: 10.1016/S0167-6296(97)00005-2. [DOI] [PubMed] [Google Scholar]
- 44.Buxton MJ, Drummond MF, Van Hout BA, Prince RL, Sheldon TA, Szucs T, et al. Modelling in economic evaluation: an unavoidable fact of life. Health Econ. 1997;6:217–27. doi: 10.1002/(SICI)1099-1050(199705)6:3<217::AID-HEC267>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 45.Maulik PK, Darmstadt GL. Childhood disability in low and middle income countries: overview of screening, prevention, services, legislation and epidemiology. Pediatrics. 2007;120(Suppl 1):S1–55. doi: 10.1542/peds.2007-0043B. [DOI] [PubMed] [Google Scholar]
- 46.Mathers CD, Lopez AD, Murray CJL. The burden of disease and mortality by condition: data, methods, and results for 2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, eds. Global burden of disease and risk factors: data, methods and results for 2001 New York: Oxford University Press; 2006. pp. 45-234. [Google Scholar]
- 47.UNICEF. State of the world’s children 2008: child survival New York: United Nations Children’s Fund; 2008. [Google Scholar]
- 48.Winch PJ, Alam MA, Akther A, Afroz D, Ali NA, Ellis AA, et al. Local understandings of vulnerability and protection during the neonatal period in Sylhet District, Bangladesh: a qualitative study. Lancet. 2005;366:478–85. doi: 10.1016/S0140-6736(05)66836-5. [DOI] [PubMed] [Google Scholar]
- 49.Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed AS, Williams EK, Seraji HR, et al. Effect of community-based newborn-care intervention package implemented through two service delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371:1936–44. doi: 10.1016/S0140-6736(08)60835-1. [DOI] [PubMed] [Google Scholar]
- 50.Darmstadt GL, Baqui AH, Choi Y, Bari S, Rahman SM, Mannan I, et al. Validation of community health workers’ assessment of neonatal illness in rural Bangladesh. Bull World Health Organ. 2009;87:12–9. doi: 10.2471/BLT.07.050666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baqui A, Williams EK, Rosecrans AM, Agrawal PK, Ahmed S, Darmstadt GL, et al. Impact of an integrated nutrition and health programme on neonatal mortality in rural northern India. Bull World Health Organ. 2008;86:796–804. doi: 10.2471/BLT.07.042226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumar V, Mohanty S, Kumar A, Mishra RP, Santosham M, Baqui AH, et al. Impact of community-based behavior change management on neonatal mortality: a cluster-randomized, controlled trial in Shivgarh, Uttar Pradesh, India. Lancet. 2008;372:1151–62. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 53.Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, et al. NGO facilitation of a government’s community-based maternal and neonatal health programme in rural India: Improvements in equity. Health Policy Plan. 2008;23:234–43. doi: 10.1093/heapol/czn012. [DOI] [PubMed] [Google Scholar]
- 54.Haws RA, Thomas AL, Bhutta ZA, Darmstadt GL. Impact of packaged interventions on neonatal health: a review of the evidence. Health Policy Plan. 2007;22:193–215. doi: 10.1093/heapol/czm009. [DOI] [PubMed] [Google Scholar]