Abstract
Objective
To study the effectiveness of planning and management interventions for ensuring children in India are immunized at the appropriate age.
Methods
The study involved children aged less than 18 months recruited from Haryana, India, in 2005–2006: 4336 in a pre-intervention cohort and 5213 in a post-intervention cohort. In addition, immunization of 814 hospitalized children from outside the study area was also assessed. Operational barriers to age-appropriate immunization with diphtheria, pertussis and tetanus (DPT) vaccine were investigated by monitoring vaccination coverage, observing immunization sessions and interviewing parents and health-care providers. An intervention package was developed, with community volunteers playing a pivotal role. Its effectiveness was assessed by monitoring the ages at which the three DPT doses were administered.
Findings
The main reasons for delayed immunization were staff shortages, non-adherence to plans and vaccine being out of stock. In the post-intervention cohort, 70% received a third DPT dose before the age of 6 months, significantly more than in the pre-intervention cohort (62%; P = 0.002). In addition, the mean age at which the first, second and third DPT doses were administered decreased by 17, 21 and 34 days, respectively, in the study area over a period of 18 months (P for trend < 0.0001). No change was observed in hospitalized children from outside the study area.
Conclusion
An intervention package involving community volunteers significantly improved age-appropriate DPT immunization in India. The Indian Government’s intention to recruit village-based volunteers as part of a health sector reform aimed at decentralizing administration could help increase timely immunization.
Résumé
Objectif
Étudier l’efficacité des interventions de planification et de gestion visant à garantir la vaccination des enfants à un âge approprié en Inde.
Méthodes
L’étude a porté sur des enfants de moins de 18 mois, recrutés dans l’Haryana en Inde, sur la période 2005-2006 : 4336 composant une cohorte pré-intervention et 5213 constituant une cohorte post-intervention. En outre, on a évalué la vaccination de 814 enfants hospitalisés, mais n’habitant pas la zone étudiée. On a étudié les obstacles opérationnels à l’administration à un âge approprié du vaccin antidiphtérique-anticoquelucheux-antitétanique (DTP) par une surveillance de la couverture vaccinale, une observation des sessions de vaccination et un entretien avec les parents et les prestataires de soins. On a mis au point un module d’intervention dans lequel des volontaires appartenant à la communauté jouaient un rôle central. L’efficacité de ce module a été évaluée en suivant les âges auxquels les doses de DPT étaient administrées.
Résultats
Les retards dans la vaccination étaient principalement imputables à des pénuries de personnel, au non-respect des plans et à des ruptures de stocks de vaccins. Parmi la cohorte post-intervention, 70 % des enfants avaient reçu une troisième dose de DTP avant l’âge de 6 mois, soit significativement plus que dans la cohorte pré-intervention (62 %, p = 0,002). De plus, l’âge moyen d’administration de la première, de la deuxième et de la troisième doses de DTP avait diminué respectivement de 17, 21 et 34 jours dans la zone étudiée, sur une période de 18 mois (probabilité de la tendance < 0,0001). Aucun changement n’a été observé chez les enfants hospitalisés ne provenant pas de la zone étudiée.
Conclusion
Un module d’intervention faisant appel à des volontaires communautaires a permis en Inde de rapprocher significativement l’âge d’administration du vaccin DPT de l’âge approprié. L’intention du Gouvernement indien de recruter des volontaires dans les villages dans le cadre de la réforme de décentralisation de l’administration pourrait favoriser la vaccination à un âge approprié.
Resumen
Objetivo
Estudiar la eficacia de intervenciones de planificación y gestión para garantizar que los niños de la India se vacunan a la edad apropiada.
Métodos
El estudio se realizó en 2005–2006 en menores de 18 meses de Haryana (India): 4336 en una cohorte preintervención y 5213 en una cohorte posintervención. Además también se investigó la vacunación de 814 niños hospitalizados que no pertenecían a la zona en estudio. Los obstáculos a la vacunación DTP (difteria, tétanos y tos ferina) a la edad apropiada se investigaron monitorizando la cobertura vacunal, observando las sesiones de vacunación y entrevistando a los padres y a los dispensadores de atención sanitaria. Se elaboró un conjunto de intervenciones en las que desempeñaron un papel destacado los voluntarios de la comunidad. La eficacia se evaluó en función de las edades a las que se administraron las tres dosis de la DTP.
Resultados
Las principales causas de retraso de la vacunación fueron la escasez de personal, el incumplimiento de los planes y el agotamiento de las existencias de la vacuna. En la cohorte posintervención, el 70% de los casos recibieron la tercera dosis de DTP antes de los 6 meses, porcentaje que fue significativamente mayor que en la cohorte preintervención (62%; P = 0,002). Además, en la zona estudiada el promedio de edad en el momento de la administración de la primera, segunda y tercera dosis de DTP disminuyó a lo largo de un periodo de 18 meses en 17, 21 y 34 días, respectivamente (P de la tendencia < 0,0001). En los niños hospitalizados que no pertenecían a la zona en estudio no se observaron cambios.
Conclusión
En la India, un conjunto de intervenciones en las que participaron voluntarios de la comunidad mejoró significativamente la vacunación con la DTP a edades apropiadas. La intención del Gobierno de la India de reclutar a voluntarios de los pueblos en el marco de la reforma del sector de la salud destinada a descentralizar la administración podría ayudar a incrementar la vacunación en el momento oportuno.
ملخص
الغرض
دراسة فعالية تخطيط وإدارة التدخلات لضمان تمنيع الأطفال في العمر المناسب.
الطريقة
اشتملت الدراسة على الأطفال أقل من عمر 18 شهراً المدرجين في منطقة هيريانا في الهند، خلال الفترة 2005-2006 وتضمن ذلك: 4336 طفلاً في مجموعة أترابية لم تتلق التدخل، و 5213 طفلاً في مجموعة أترابية بعد تلقيها التدخل، بالإضافة إلى تقييم تمنيع 814 طفلاً منومين في المستشفى من خارج منطقة الدراسة. وجرى تقصي العقبات الميدانية لتمنيع الأطفال في أعمارهم المناسبة بلقاح الخناق والسعال الديكي والكزاز عن طريق رصد التغطية باللقاح، ومشاهدة جلسات التمنيع، ومقابلة الآباء ومقدمي الرعاية الصحية. وأُعِدت حزمة من التدخلات، كان فيها للمتطوعين من المجتمع دور محوري. وجرى تقييم فعالية حزمة التدخلات عن طريق رصد أعمار الأطفال التي يعطى عندها لقاح (الخناق والسعال الديكي والكزاز).
الموجودات
كانت الأسباب الرئيسية لتأخر التمنيع هي قلة عدد العاملين، وعدم الالتزام بالخطط الموضوعة، ونفاذ كميات اللقاح المختزنة. وفي دراسة المجموعة الأترابية التي تلقت حزمة التدخلات، تبين أن 70% منهم تلقوا الجرعة الثالثة للقاح قبل عمر 6 شهور، وهذا نسبة أعلى ويعتد بها إحصائياً عن المجموعة الأترابية التي لم تتلق حزمة التدخلات (وبلغت نسبتها 62%؛ P= 0.002). بالإضافة إلى أن متوسط العمر الذي أعطيت عنده الجرعة الأولى والثانية والثالثة من لقاح (الخناق والسعال الديكي والكزاز) قد قل بمقدار 17 ، 21، 34 يوماً بالترتيب، في منطقة الدراسة خلال فترة 18 شهراً (P للتوجه أقل من 0.0001). ولم تلاحظ أي تغيرات بالنسبة للأطفال المنومين في المستشفيات من خارج منطقة الدراسة.
الاستنتاج
أدت حزمة التدخلات التي شارك فيها متطوعون من المجتمع إلى تحسين معدلات التمنيع بلقاح (الخناق والسعال الديكي والكزاز) في العمر المناسب للأطفال في الهند. ويمكن لتصميم حكومة الهند على توظيف متطوعين من القرى كجزء من إصلاح القطاع الصحي والسعي إلى تحقيق اللامركزية في الإدارة أن يساعد في رفع معدلات التمنيع في الأعمار المناسبة.
Introduction
Every year communicable diseases kill more than 14 million people throughout the world, predominantly in developing countries.1 At present, measles, pertussis and tetanus, diseases that affect children, are responsible for the majority of disability-adjusted life years lost.2 Measles accounts for 30 million cases and 888 000 deaths worldwide annually, 85% of them in south-east Asia and Africa.3 Outbreaks of diphtheria also occur, especially in countries with low vaccination coverage.4
Despite the availability of safe and effective vaccines, the coverage of immunization against the six main vaccine-preventable diseases is still variable across different regions of India.5 Although increasing immunization coverage is essential, it is also important that vaccines are administered when the child is at the appropriate age, as indicated in the national immunization schedule, because this will provide protection from disease when the risk is highest.6 Numerous studies have investigated immunization coverage and have recommended strategies for increasing it.7–12 However, few intervention studies have focused on administering vaccines at the appropriate age.13 The present study was conducted primarily to identify interventions that can increase timely vaccination by overcoming operational barriers to providing age-appropriate immunization.
Methods
Study population
The study was part of a pilot project that looked into the feasibility of estimating the burden of preventable Haemophilus influenzae type b (Hib) meningitis and pneumonia in India, with funding provided by the Indian Council of Medical Research, New Delhi, and the Johns Hopkins University Bloomberg School of Public Health in Baltimore, MD, United States of America. The study was approved by the Institutional Review Board of the Johns Hopkins University and the Institute Ethics Committee of the Post Graduate Institute of Medical Education and Research, Chandigarh, India. Written informed consent was obtained from the parents of all children taking part.
The intervention study was conducted in the rural community development block of Khizrabad in the Yamunanagar district of Haryana state, India, between July 2005 and December 2006. This district was chosen because immunization coverage for all currently administered vaccines in 1-year-old children was 78% in 2004,14 which was considered adequate for the introduction of the Hib vaccine. The national immunization schedule in India stipulates the administration of one dose of bacille Calmette–Guérin vaccine between birth and 6 weeks, three doses each of combined diphtheria, pertussis and tetanus (DPT) vaccine and oral poliovirus vaccine (OPV) at 6, 10 and 14 weeks, respectively, and measles vaccine at 9 months of age.15 In addition, the Khizrabad block was chosen from among four blocks in this district because its geographic location facilitated patients’ access to the study hospitals.
In the primary health-care system in India, community health centres provide specialist services for population groups of 100 000, while primary health centres provide health-care services for disease prevention and cure and health-care promotion to population groups of 30 000. Generally, individual primary health centres are associated with six subcentres, each of which covers a population group of 5000. In these subcentres, basic medical care for minor illnesses and disease prevention and health-care promotion activities are provided by male and female multipurpose health workers.
In the study block, a network of one community health centre, three primary health centres and 25 subcentres provided health care to a population of 170 000 in 204 villages. In addition to health service staff, 155 child care workers were also present in villages to promote nutritional and health interventions. These workers (roughly one for each 1000 population) belong to child-care and mother-care centres, or anganwadi, set up under the Indian Government’s Integrated Child Development Services Scheme.
The planning, implementation and monitoring of immunization services in Yamunanagar district is decentralized to the primary health centres. Vaccines are stored for up to 3 months at district headquarters, from where supplies are sent to the community health centre and to primary health centres that have facilities for storing vaccine for up to 1 month. Each subcentre holds an outreach session once a week, traditionally on a Wednesday, at anganwadis in the villages where vaccine storage facilities are not available.15
Pre-programme performance
To determine whether all eligible children at a particular subcentre had been registered at birth and thereby enrolled for vaccination, all children registered by the female multipurpose health worker as having been born between April 2004 and March 2005 were compared with the children registered by a trained community volunteer for the corresponding period. This was done in 13 subcentres (52%), where the same female multipurpose health worker had been present for at least two consecutive years. The details of the children registered by the community volunteers were validated in 10% of randomly selected households by one of five full-time field supervisors who had been recruited at primary health centres to supervise these volunteers.
The study investigators observed one village outreach session for each of the 25 subcentres using a standard World Health Organization supervisory checklist to identify problems in immunization service planning, implementation or monitoring.16
The mothers of children who had not attended the immunization session 1 month after the first DPT vaccine dose were interviewed to identify the reason for dropping out. All female multipurpose health workers in the community development block were interviewed to determine the number of sessions held during the preceding month as a proportion of the planned number of sessions, and the reasons for not holding a session as planned were recorded. The vaccine cold chain and logistics system were also reviewed.
Study intervention
Observations made during the assessment of the pre-intervention vaccination programme were discussed in separate meetings with district health authorities, medical officers from the community health centre and primary health centres and female multipurpose health workers. Subsequently, a strategy for improving the immunization programme was worked out jointly.
Data collection
Community volunteers enrolled all children under 18 months of age in the study, maintained a log of pregnant women and prospectively enrolled all children born to permanent residents during the study period. The past immunization status of children under 18 months of age at the time of initial enrolment was recorded. Subsequently, community volunteers recorded the date of immunization of children vaccinated in the immunization sessions and records were submitted each week. Each child was followed up until the age of 18 months. When the child reached 24 months, a follow-up form was completed detailing the dates when vaccines were administered after enrolment, as recalled by the mother. These follow-up forms were used to check the accuracy of data collected by community volunteers. Any disagreement was checked and a correct record was agreed upon by the field supervisors. In addition, immunization data on children under 2 years of age who were admitted to 15 paediatric private and government hospitals from the entire district were collected by medical officers as a part of pneumonia and meningitis surveillance.
Data analysis
Enrolment and follow-up data were entered into Epi Info version 3.0 statistical software (Centers for Disease Control and Prevention, Atlanta, GE, United States of America) for analysis. The overall effectiveness of the interventions was assessed by comparing the immunization coverage of children who had started or completed their immunization schedule at study enrolment (i.e. the pre-intervention cohort), reflecting the past performance of the immunization programme, with coverage of newborn children who had not been vaccinated before study enrolment (i.e. the post-intervention cohort), reflecting the impact of the interventions. The mean age at which different DPT doses were administered and the mean time difference between DPT doses in the two cohorts were also compared.
A similar analysis was performed using data from hospitalized children from all community development blocks except the study block. These children were divided into two groups: those immunized before July 2005 (the date at which the interventions were introduced in the study area) and those immunized after. The significance of the difference in categorical and continuous variables between the two groups was assessed using the χ² test and t test, respectively. The statistical significance for the trend was computed using the χ² test for trend and the ANOVA test for categorical and continuous variables, respectively.
Immunization data contained in the weekly reports provided by community volunteers were divided into six quarterly immunization cohorts covering the period from July 2005 to December 2006. An analysis of variance was used to determine whether there were any significant trends over the six quarters.
Results
The pre-intervention cohort comprised 4336 children aged less than 18 months who at the time of enrolment in the study had started or completed their immunization schedule; the post-intervention cohort comprised 5213 children who were registered prospectively at birth during the study. The majority (99.3%) of mothers consented to participation. The first, second and third DPT doses were administered during the study to 4810, 4775 and 4730 children, respectively. In addition, 814 children were admitted to the study hospitals from other blocks in Yamunanagar district. According to their parents’ reports, first, second and third DPT doses were administered to 477 (58.6%), 377 (46.3%) and 294 (36.1%) children, respectively.
Although nearly 92% of the children in the pre-intervention cohort had received a third DPT dose by the age of 12 months, only 19% had received it by the age of 4 months, the age by which they should have received it according to the Indian national immunization schedule.
Service delivery
The performance of the pre-intervention immunization programme was analysed to identify operational barriers that needed to be overcome to improve age-appropriate immunization coverage. It was found that female multipurpose health workers failed to register 7.5% of births on average. The percentage of missed births was less in villages with an anganwadi (0.5%) than in those without (17.2%). The accuracy of birth registration in villages was inversely related to their distance from a subcentre: the proportion of missed births was 0.02% in subcentre villages or villages within 2 km of a subcentre village, 9.5% in villages 2–5 km from a subcentre village and 8.2% in villages more than 5 km from a subcentre village.
A review of vaccine logistics revealed that ice-lined refrigerators and deep freezers were not functioning in two out of the three primary health centres. Moreover, only 1 months’ supply of vaccine could be stocked at the district store because storage space was inadequate. Overall, ice-lined refrigerators and deep freezers in the district could only store 80% of the 3 months’ stock. In 2 months of the preceding year (2004–2005), DPT vaccine was out of stock at district level.
Updated and comprehensive microplans were not available in primary health centres. Sixteen outreach sessions (13.9%) planned for the month preceding the performance analysis were not held. The main reasons were that a monthly staff meeting was scheduled at the primary health centre on an immunization day (50%); the female multipurpose health worker’s post was vacant (25%); the female multipurpose health worker decided to miss the session (12.5%), and the female multipurpose health worker was either on leave or away on training and there was no replacement (12.5%). Of the 99 sessions held, 23 (23.2%) did not take place on the planned day. In total, 527 children dropped out 1 month after the first DPT dose. The reasons given included: “child not at home on the day of immunization” (47.3%), “child not vaccinated due to minor illness” (27.3%), “mother busy and nobody to bring the child to the session” (7.0%) and “the session was not held on that day” (4.6%). In the remaining 13.8% of cases, either the vaccine was not available or the mother did not known that the session was taking place on that day.
Study intervention
Analysis of the immunization programme performance led to the development of the intervention package detailed in Table 1, which was designed to address the operational barriers identified above. The package was implemented by district health authorities.
Table 1. Details and timing of the interventions planned for increasing age-appropriate immunization coverage, India, 2005–2006.
| Timing | Intervention | |
|---|---|---|
| June 2005 | Recruitment and training of community volunteers and field supervisors | |
| August–October 2005 | Providing training and continuing education for medical officers at primary health centres, multipurpose health workers and anganwadia workers | |
| September–October 2005 | Analysing the performance of the pre-intervention immunization programme | |
| November 2005 | Presenting the analysis findings to district health authorities, and primary health centre and subcentre staff | |
| Drawing up an action plan using a participatory planning approach | ||
| November 2005–December 2006 | Microplanning at the primary health centre level | |
| Intensive monitoring of the immunization programme | ||
| Monthly feedback on performance | ||
| December 2005 | Recruitment of additional female multipurpose health workers and vaccinators by district health authorities to fill vacant positions |
a Village child-care and mother-care centre in India.
The presence of community volunteers who would act as community mobilizers was regarded as pivotal to the overall strategy and 25 community volunteers were recruited for the subcentres. The volunteers were educated to at least tenth grade (15 years of age) and were given an honorarium of 1000 Indian rupees (US$ 25)17 per month for part-time work. In addition, female multipurpose health workers were recruited to fill vacant positions at the subcentres. Part-time vaccinators were also hired to supplement immunization activity at any subcentre where the female multipurpose health worker was absent on a vaccination day. Comprehensive microplanning was carried out at primary health centre level to define the date, venue, vaccinator, number of clients, vaccine requirements and vaccine delivery mechanism for each outreach session. Continuing education sessions were held for doctors, health workers and anganwadi workers at the primary health centres to highlight the benefits of age-appropriate immunization. The study investigators participated in monthly meetings of programme officers and primary health centre medical officers held at the district level to review progress during the previous month and to resolve operational problems.
Effect of the intervention
The proportion of children who had received the third DPT dose by the ages of 4, 6 and 9 months was 22%, 70% and 88%, respectively, in the post-intervention cohort. This was significantly greater (P < 0.001) than in the pre-intervention cohort, where the proportions were 19%, 62% and 85%, respectively. There was no significant difference in coverage at 12 months.
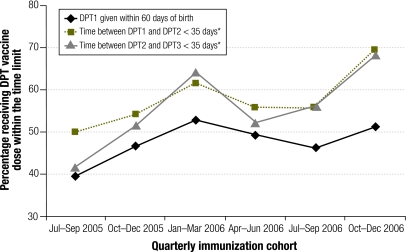
Findings in the six quarterly post-intervention cohorts are summarized in Table 2 and Fig. 1. The mean age at which the first, second and third DPT doses were administered decreased significantly (P for trend < 0.0001) from the first quarter of the study period (i.e. July–September 2005) to the sixth quarter (i.e. October–December 2006) (Table 2). In fact, the mean age at administration of the first, second and third DPT doses declined by 17, 21 and 34 days, respectively, in the study area (P < 0.0001). In contrast, this trend was not observed among children from the rest of the district admitted to study hospitals. In these children, the mean age at which the first DPT dose was administered varied from 65.8 to 68.9 days from the first to the sixth quarterly cohort. The corresponding variation for the second dose was from 94.3 to 129.7 days and, for the third dose, from 129.4 to 121.7 days.
Table 2. Age at DPT vaccination and time between DPT doses in the six quarterly immunization cohorts monitored after the introduction of the study interventions, India, 2005–2006.
| Date | No. of children vaccinated |
Mean (SD) age, in days, at vaccination |
Mean (SD) time, in days, between DPT doses |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DPT1 | DPT2 | DPT3 | DPT1* | DPT2* | DPT3* | DPT1 and DPT2* | DPT2 and DPT3* | |||
| July–September 2005 | 919 | 754 | 766 | 82.5 (58.4) | 129.9 (66.9) | 190.3 (86.2) | 52.5 (39.4) | 65.6 (54.8) | ||
| October–December 2005 | 1155 | 1107 | 1035 | 79 (62.6) | 129.2 (69.6) | 191.2 (91.2) | 50.2 (40.2) | 57.5 (51.1) | ||
| January–March 2006 | 978 | 1096 | 1174 | 71.4 (59.1) | 123.3 (81.8) | 164.3 (90.2) | 42.3 (43.3) | 55.5 (39.4) | ||
| April–June 2006 | 761 | 789 | 813 | 68.8 (44.4) | 116.9 (69.7) | 169.6 (89.6) | 50 (49.6) | 51.9 (41.1) | ||
| July–September 2006 | 822 | 822 | 888 | 73.4 (55.6) | 121.9 (58.8) | 175.9 (82.9) | 50.4 (38.8) | 52.9 (47.9) | ||
| October–December 2006 | 1035 | 979 | 855 | 65.2 (33.2) | 108.5 (52) | 156.1 (63.3) | 43.4 (37.2) | 42.3 (27.2) | ||
* P for trend < 0.0001 (ANOVA). DPT, diphtheria, pertussis and tetanus; DPT1, first DPT vaccine dose; DPT2, second DPT vaccine dose; DPT3, third DPT vaccine dose; SD, standard deviation.
Fig. 1.
Children who received DPT1 within 60 days of birth and who received DPT2 and DPT3 within 35 days of the preceding dose, in six quarterly immunization cohorts monitored after study interventions, India, 2005–2006
* P for trend < 0.0001 (χ² test for trend).
DPT, diphtheria, pertussis and tetanus; DPT1, first DPT vaccine dose; DPT2, second DPT vaccine dose; DPT3, third DPT vaccine dose.
Discussion
Previously, the immunization programme in the study area was being monitored by determining the proportion of children who were fully immunized at 1 year of age. Periodic surveys have also used this crude indicator to evaluate the performance of routine immunization programmes.18–20 This emphasis on 1-year-old children was evident in the figures on vaccination coverage before the study intervention: 92% of children aged 12 months had received the third DPT dose compared with only 19% of children aged 4 months. Since immunization is most beneficial when received at the recommended age, age-appropriate coverage should be the benchmark for assessing immunization programme performance.
Major operational lacunae in immunization programmes are related to programme planning and management. The findings of this study demonstrate that better microplanning can significantly improve programme performance. In particular, data provided by a management information system were found to be helpful for evaluating performance and finding solutions at monthly review meetings.
Implementation of the intervention programme was impeded by a higher-than-expected workload. In the study area, the average subcentre catered to a population of 6800, considerably above the national norm of 5000, and 12 subcentres (48%) catered to more than 8000. Moreover, there was a shortage of female multipurpose health workers. Similar observations were made in another local study.21 In our case, female multipurpose health workers, additional vaccinators and part-time community volunteers were recruited under the Reproductive and Child Health-II programme.22 In addition, the infrastructure for vaccine storage needs to be strengthened. This will become even more important when the Indian Government introduces newer vaccines, such as Hib and vaccine against hepatitis B.
One reason for the discrepancy between reported and actual routine immunization coverage often found in studies is underregistration of births.23,24 The completeness of birth registration can be improved by extending the Integrated Child Development Services programme to all areas of India and by better coordination with anganwadi workers.25 In the present study, birth registration by female multipurpose health workers was almost 100% in villages with an anganwadi.
The majority of previous studies of immunization performance have focused on overall coverage.7–12 We could not find any published research into age-appropriate immunization apart from one document in the grey literature.13 However, many authors have emphasized the importance of timely immunization for better protection against pertussis,26 measles27 and Hib.28
Other studies have noted that many children do not return for vaccination after the first dose of a multidose vaccine. One study from Delhi found a dropout rate similar to ours between the first and third DPT dose. The main reason given was a lack of information about the vaccination session.29 Dealing with this problem requires a change in focus from providing “universal coverage” to providing “universal timely coverage”. This new focus should be communicated to clients and highlighted in continuing education for health-care workers.
The present study identified operational barriers to providing immunization at an appropriate age in a developing country. However, it also showed that age-appropriate immunization coverage can be significantly increased (Table 2) by supervising workers in the community and by improving programme planning and monitoring.
Double-blind, randomized, controlled trials of programme management interventions are difficult to carry out. Comparable reference populations are hard to find and expenditure on data collection alone is difficult to justify. Hence, this study used hospitalized children from outside the study area as a reference population. It is possible that the parents of these children were more concerned about health than other parents. Nevertheless, the ages at which the DPT vaccine doses were administered to hospitalized children did not change during the study period, whereas the ages at which they were administered to children in the study area decreased. There were no sociodemographic or health infrastructure differences between these two groups. Moreover, selection bias was unlikely as only 0.7% of parents refused to participate.
Although the mean age at which the second and third DPT doses were administered in the post-intervention cohort decreased by several weeks (21 and 34 days, respectively) over the six study quarters. In the study area, there were cultural reasons for the delay in the first dose. A pregnant woman generally goes to her parents’ house to deliver her first baby and returns home when the baby is about 2 months old. Health workers usually administer vaccine only to the resident population. A change in state policy is required so that the baby can be vaccinated where it is delivered and mothers should be encouraged to ensure this happens.
Another barrier to providing age-appropriate immunization is that outreach sessions were held only once a month in each village. If a session was missed, the age at which the first and subsequent dose was given was increased by 1 month. Consequently, in this study, the intervention package was completely implemented by only the third quarter (Table 1) and the full impact of the intervention was seen in only the sixth quarter.
This study was conducted in an area that already had a high rate of immunization coverage in children 12 months of age. The findings may not be replicated in areas with low immunization rates. Nevertheless, the interventions implemented here may be helpful. Indeed, the World Health Organization and United Nations Children’s Fund Global Immunization and Vision Strategy recommends similar interventions30 in both low- and high-income settings.31–33
This study demonstrates that decentralization of planning and management can improve immunization programme performance. The role played by community volunteers is particularly relevant given that village-based volunteers, called accredited social health activists, are being introduced in India under the National Rural Health Mission34 as part of a health sector reform aimed at decentralizing and devolving administrative and financial power. Moreover, there is increasing interest worldwide in the impact of community-based health workers on child survival,35 particularly where there are few human resources. Community-based workers are cost-effective and can reduce inequity by targeting the poor.36 ■
Acknowledgements
We are grateful to Haryana Health Services, especially PK Jain, Vijay Atreja and Shivinder Singh for implementing the intervention package. We acknowledge assistance of Amandeep Kapoor, Dinesh Garg and Chandan Mago for data collection and supervision of community volunteers.
Footnotes
Funding: Funding was provided by the Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States of America, and the Indian Council of Medical Research, New Delhi, India.
Competing interests: None declared.
References
- 1.Heymann DL, editor. Control of communicable diseases manual 18th edn. Washington, DC: American Public Health Association; 2004. [Google Scholar]
- 2.Making every mother and child count: the world health report 2004 [statistical annex]. Geneva: World Health Organization; 2005. [Google Scholar]
- 3.National Institute of Communicable Diseases Measles continues to remain major public health problem. CD Alert. 2000;4:1. [Google Scholar]
- 4.National Institute of Communicable Diseases Diphtheria. CD Alert. 1999;3:1. [Google Scholar]
- 5.International Institute of Population Sciences and Ministry of Health and Family Welfare. India summary report: reproductive and child health district level household survey (2002-04) and facility survey (2003) Mumbai: IIPS and MHFW; 2006. [Google Scholar]
- 6.Expanded programme on immunization: immunization policy Geneva: World Health Organization;1995 (GPV/GEN/95.03 Rev.1).
- 7.Vaccine-preventable diseases monitoring systems Geneva: World Health Organization; 2009. Available from: http://whqlibdoc.who.int/hq/2008/WHO_IVB_2008_eng.pdf [accessed on 12 August 2009].
- 8.Jain SK, Chawla U, Gupta N, Gupta RS, Venketesh S, Lal S. Child survival and safe motherhood program in Rajasthan. Indian J Pediatr. 2006;73:43–7. doi: 10.1007/BF02758259. [DOI] [PubMed] [Google Scholar]
- 9.Bonu S, Rani M, Baker TD. The impact of the national polio immunization campaign on levels of equity in immunization coverage: evidence from rural north India. Soc Sci Med. 2003;57:1807–19. doi: 10.1016/S0277-9536(03)00056-X. [DOI] [PubMed] [Google Scholar]
- 10.de Timóteo Mavimbe JCT, Muquingue HN, Braa J, Bjune G. Immunization coverage in Mozambique: from concepts to decision-making. Health Policy. 2006;79:92–100. doi: 10.1016/j.healthpol.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Robertson SE, Valedez JJ. Global review of health-care surveys using lot quality assurance sampling (LQAS), 1984-2004. Soc Sci Med. 2006;63:1648–60. doi: 10.1016/j.socscimed.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal S, Bhanot A, Goindi G. Understanding and addressing childhood immunization coverage in urban slums. Indian Pediatr. 2005;42:653–63. [PubMed] [Google Scholar]
- 13.Bhanot A, Agarwal S, Srivastava K. Improving age-appropriate immunization among urban poor infants: possible options and approaches New Delhi: United States Agency for International Development, Urban Health Resource Centre; 2004. [Google Scholar]
- 14.India RG. Bulletin on rural health statistics in India 2005 New Delhi: Rural Health Division, Ministry of Health and Family Welfare; 2005. [Google Scholar]
- 15.India, Ministry of Health and Family Welfare. Manual on community needs assessment approach (CNAA) in family welfare programme New Delhi: MHFW; 1998.
- 16.India, Ministry of Health and Family Welfare. Immunization handbook for health workers New Delhi: MHFW; 2006.
- 17.Universal currency converter. Available from: http://www.xe.com/ucc/convert.cgi [accessed on 10 July 2009].
- 18.National family health survey 1 Mumbai and Calverton, MD: International Institute of Population Sciences and ORC Macro; 1993. [Google Scholar]
- 19.National family health survey 2 Mumbai and Calverton, MD: International Institute of Population Sciences and ORC Macro;1998. [Google Scholar]
- 20.International Institute for Population Sciences and Macro International. National Family Health Survey (NFHS-3), 2005–06: India Vol. 1. Mumbai: IIPS; 2007. [Google Scholar]
- 21.Murthy N, Barna A. Integrating reproductive health in health programmes in India. In: Krishnaraj M, Sudarshan RM, Sheriff A, eds. Gender, population and development Oxford: Oxford University Press; 1998. pp. 291-309. [Google Scholar]
- 22.India, Ministry of Health and Family Welfare Reproductive and child health program RCH-II New Delhi: MHFW; 2002.
- 23.Singh J, Kumar A, Rai RN, Khare S, Jain DS, Bhatia R, et al. Widespread outbreak of measles in rural Uttar Pradesh, India, 1996: high-risk areas and groups. Indian Pediatr. 1999;36:249–56. [PubMed] [Google Scholar]
- 24.Murray CJL, Shengelia B, Gupta M, Moussavi S, Tandon A, Thiereu M. Validity of reported immunization coverage in 45 countries. Lancet. 2003;362:1022–7. doi: 10.1016/S0140-6736(03)14411-X. [DOI] [PubMed] [Google Scholar]
- 25.Lal S. Functioning of subcentres in the system of primary health care. Indian Journal of Community Medicine. 2001;26:59–64. [Google Scholar]
- 26.Crowcroft NS, Stein C, Duclos P, Birmingham M. How best to estimate the global burden of pertussis? Lancet Infect Dis. 2003;3:413–8. doi: 10.1016/S1473-3099(03)00669-8. [DOI] [PubMed] [Google Scholar]
- 27.Dannetun E, Tegnell A, Hermansson G, Torner A, Giesecke J. Timeliness of MMR vaccination – influence on vaccination coverage. Vaccine. 2004;22:4228–32. doi: 10.1016/j.vaccine.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 28.von Kries R, Bohm O, Windfuhr A. Haemophilus influenzae b vaccination: the urgency for timely vaccination. Eur J Pediatr. 1997;156:282–7. doi: 10.1007/s004310050601. [DOI] [PubMed] [Google Scholar]
- 29.Sokhey J, Jain DC, Harit AK, Dhariwal AC. Moderate immunization coverage levels in East Delhi: implications for disease control programmes and introduction of new vaccines. J Trop Pediatr. 2001;47:199–203. doi: 10.1093/tropej/47.4.199. [DOI] [PubMed] [Google Scholar]
- 30.GIVS Global Immunization Vision and Strategy 2006-2015 Geneva: World Health Organization and United Nations Children’s Fund; 2005. Available from: http://www.who.int/vaccines-documents/DocsPDF05/GIVS_Final_EN.pdf [accessed on 10 July 200].
- 31.Dombkowski KJ, Lantz PM, Freed GL. The need for surveillance of delay in age-appropriate immunization. Am J Prev Med. 2002;23:36–42. doi: 10.1016/S0749-3797(02)00442-7. [DOI] [PubMed] [Google Scholar]
- 32.Akmatov MK, Kretzschmar M, Krämer A, Mikolajczyk RT. Timeliness of vaccination and its effect on fraction of vaccinated population. Vaccine. 2008;26:3805–11. doi: 10.1016/j.vaccine.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 33.Hull BP, McIntyre PB. Timeliness of childhood immunisation in Australia. Vaccine. 2006;24:4403–8. doi: 10.1016/j.vaccine.2006.02.049. [DOI] [PubMed] [Google Scholar]
- 34.India, Ministry of Health and Family Welfare. National rural health mission (2005-2012) New Delhi: MHFW; 2005.
- 35.Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369:2121–31. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- 36.Knippenberg R, Lawn JE, Darmstadt GL, Begkoyian G, Fogstad H. Systematic scaling up of neonatal care in countries. Lancet. 2005;365:1087–98. doi: 10.1016/S0140-6736(05)71145-4. [DOI] [PubMed] [Google Scholar]