Abstract
The first target of the fifth United Nations Millennium Development Goal is to reduce maternal mortality by 75% between 1990 and 2015. This target is critically off track. Despite difficulties inherent in measuring maternal mortality, interventions aimed at reducing it must be monitored and evaluated to determine the most effective strategies in different contexts. In some contexts, the direct causes of maternal death, such as haemorrhage and sepsis, predominate and can be tackled effectively through providing access to skilled birth attendance and emergency obstetric care. In others, indirect causes of maternal death, such as HIV/AIDS and malaria, make a significant contribution and require alternative interventions. Methods of planning and evaluating maternal health interventions that do not differentiate between direct and indirect maternal deaths may lead to unrealistic expectations of effectiveness or mask progress in tackling specific causes. Furthermore, the need for additional or alternative interventions to tackle the causes of indirect maternal death may not be recognized if all-cause maternal death is used as the sole outcome indicator. This article illustrates the importance of differentiating between direct and indirect maternal deaths by analysing historical data from England and Wales and contemporary data from Ghana, Rwanda and South Africa. The principal aim of the paper is to highlight the need to differentiate deaths in this way when evaluating maternal mortality, particularly when judging progress towards the fifth Millennium Development Goal. It is recommended that the potential effect of maternity services failing to take indirect maternal deaths into account should be modelled.
Résumé
La première cible du cinquième objectif du Millénaire pour le développement fixé par les Nations Unies est de réduire des deux tiers, entre 1990 et 2015, le taux de mortalité maternelle. L’évolution actuelle s’écarte gravement de cet objectif. Malgré les difficultés inhérentes à la mesure de la mortalité maternelle, les interventions visant à réduire cette mortalité doivent être suivies et évaluées pour déterminer les stratégies les plus efficaces dans différentes situations. Dans certains contextes, les causes directes de décès maternels telles que les hémorragies et les accidents septiques, sont prédominantes et peuvent être contrées efficacement en permettant aux femmes de bénéficier d’une assistance à l’accouchement par du personnel qualifié et de soins obstétricaux d’urgence. Dans d’autres contextes, des causes indirectes de décès maternels telles que le VIH/sida et le paludisme contribuent notablement à la mortalité des mères et nécessitent d’autres types d’interventions. Les méthodes de planification et d’évaluation des interventions en faveur de la santé maternelle qui ne font pas la distinction entre décès maternels directs et indirects peuvent conduire à des attentes irréalistes quant à l’efficacité des interventions ou masquer les progrès dans la maîtrise de certaines causes. En outre, la nécessité d’interventions supplémentaires ou alternatives pour faire face aux causes indirectes de décès maternels peut ne pas être reconnue si le nombre de décès maternels toutes causes confondues est utilisé comme seul indicateur de résultat. Le présent article illustre l’importance de la différenciation entre décès maternels directs et indirects à travers l’analyse de données historiques provenant d’Angleterre et du Pays de Galle et de données contemporaines provenant du Ghana, du Rwanda et d’Afrique du Sud. Il vise principalement à attirer l’attention sur la nécessité de cette distinction lors de l’évaluation des décès maternels, notamment lorsqu’il s’agit de juger les progrès réalisés vers le cinquième objectif du Millénaire pour le développement. Il est recommandé de modéliser les effets potentiels de la non-prise en compte des décès maternels indirects par les services de maternité.
Resumen
La primera meta del quinto Objetivo de Desarrollo del Milenio de las Naciones Unidas, consistente en reducir la mortalidad materna en un 75% entre 1990 y 2015, parece cada día más inalcanzable. Pese a las dificultades inherentes a la medición de la mortalidad materna, es preciso vigilar y evaluar las intervenciones encaminadas a reducirla si se desea determinar las estrategias más eficaces en los diferentes contextos. En algunos entornos predominan las causas directas de defunción materna, como las hemorragias y la septicemia, que pueden abordarse eficazmente proporcionando acceso a atención de partería cualificada y atención obstétrica de urgencia. En otros casos, las causas indirectas, como el VIH/sida y la malaria, contribuyen de forma importante y exigen otro tipo de intervenciones. Los métodos de planificación y evaluación de las intervenciones de salud materna que no distinguen las defunciones maternas directas de las indirectas pueden dar lugar a expectativas poco realistas sobre la eficacia, o bien encubrir los progresos en relación con causas específicas. Además, a veces no se reconoce la necesidad de emprender intervenciones adicionales o alternativas para abordar las causas de mortalidad materna indirecta debido a que el único indicador de resultado empleado es la mortalidad materna por todas las causas. Este artículo muestra la importancia de diferenciar la mortalidad materna directa y la indirecta a partir de un análisis de datos históricos de Inglaterra y Gales y datos recientes de Ghana, Rwanda y Sudáfrica. El principal objetivo del artículo es subrayar la necesidad de distinguir las defunciones de ese modo al evaluar la mortalidad materna, sobre todo a la hora de calibrar los progresos hacia el quinto Objetivo de Desarrollo del Milenio. Se recomienda establecer modelos del efecto potencial de la no consideración de las defunciones maternas indirectas por los servicios de maternidad.
ملخص
الهدف الأول للمرمي الخامس من المرامي الإنمائية للألفية الصادرة عن الأمم المتحدة هو خفض وفيات الأمهات بنسبة 75% بين عامي 1990 و 2015. ومازال تحقيق هذا الهدف بعيداً عن المأمول. وبالرغم من الصعوبات المتأصلة في قياس وفيات الأمهات، فإنه يجب رصد وتقييم التدخلات الهادفة إلى خفض هذه الوفيات حتى يمكن تحديد أكثر الاستراتيجيات فعالية في مختلف المواقع. ففي بعض المواقع، تغلب الأسباب المباشرة لوفيات الأمهات، مثل النزف والإنتان، ومن الممكن معالجتها بفعالية من خلال توفير مشرفات ماهرات على الولادة، وتوفير الرعاية الطارئة للولادة. وفي مواقع أخرى، يكون للأسباب غير المباشرة لوفيات الأمهات، مثل مرض الإيدز والعدوى بفيروسه والملاريا، تأثير جسيم مما يتطلب تدخلات بديلة. وقد تؤدي الخطط والتقييم لتدخلات صحة الأمومة التي لا تراعي الفروق بين الأسباب المباشرة والأسباب غير المباشرة لوفيات الأمهات إلى توقعات غير حقيقية لفعاليتها، أو يمكن أن تخفي التقدم المحرز في معالجة الأسباب المعينة. بالإضافة إلى أنه قد يغيب التعرف على الحاجة إلى تدخلات إضافية أو بديلة لمعالجة الأسباب غير المباشرة لوفيات الأمهات عند استخدام جميع أسباب وفيات الأمهات كمؤشر وحيد لقياس النتائج. وتوضح هذه المقالة أهمية التفريق بين الأسباب المباشرة وغير المباشرة لوفيات الأمهات عن طريق تحليل البيانات التاريخية من إنكلترا و ويلز والبيانات المتزامنة لها من غانا، وروندا، وجنوب أفريقيا. والهدف الرئيس لهذا البحث هو إيضاح الحاجة إلى التفريق بين الوفيات بهذه الطريقة عند تقييم وفيات الأمهات، ولاسيما عند الحكم على التقدم المحرز في تحقيق المرمى الخامس من المرامي الإنمائية للألفية. ويوصى بتحديد نماذج للتأثير المحتمل لخدمات الأمومة التي تفشل في إيلاء الاهتمام بالأسباب غير المباشرة لوفيات الأمهات.
Introduction
Despite long-term efforts to reduce maternal mortality by providing antenatal care, emergency obstetric care and skilled attendance at delivery,1 the risk of dying during pregnancy or childbirth remains significant for women in developing countries. These countries accounted for 99% of the estimated 536,000 maternal deaths that occurred worldwide in 2005.2
The first target of the fifth United Nations Millennium Development Goal (MDG-5) is to reduce the maternal mortality ratio (MMR) worldwide by 75% between 1990 and 2015, with the proportion of births attended by skilled health personnel being used as a proxy indicator of progress. The second target for MDG-5 is to achieve universal access to reproductive health care, as judged using indicators such as the contraceptive prevalence rate and the unmet need for family planning. At present, progress towards MDG-5 is seriously off target.3,4 Between 1990 and 2005 there was a decline in maternal mortality across Latin America and the Caribbean, with the MMR decreasing from 179 maternal deaths per 100 000 live births to 132 per 100 000, and across Asia, with a decrease from 410 to 329 per 100 000. However, MMRs in sub-Saharan Africa have remained high, at over 900 maternal deaths per 100 000 live births.5
Given the current lack of progress in tackling maternal mortality, it is critical that effective interventions are implemented. Clearly, careful monitoring and evaluation of these interventions is crucial for determining what works and for ensuring that scarce resources are allocated effectively. This is particularly true for developing countries, where maternal mortality is highest and access to maternal health services is poor. As Graham et al. state, “[t]here is a need to show progress in terms of impact: reduced maternal mortality, complications and disabilities, and improved health”.6
There are a number of problems inherent in measuring maternal mortality: vital registration systems might be inadequate in developing countries, hospital records might be poor, maternal deaths occurring outside health facilities might not be registered, pregnancy status might not be disclosed, and maternal deaths might be misclassified.7 Nevertheless, various measurement tools are available for tracking trends, including censuses, household surveys and the examination of hospital records. Each has its own advantages and disadvantages, such as the cost of administration, a lack of statistical capacity and a requirement for large sample sizes.
However, even when maternal mortality is measured, the majority of aggregated information sources tend to group all maternal deaths together and there is a failure to differentiate between different categories of maternal death. According to the International Classification of Diseases (ICD), 10th revision, maternal death is classified using two main categories: direct and indirect maternal death.2
Direct obstetric deaths are those resulting from obstetric complications of the pregnant state (i.e. pregnancy, labour and the puerperium), from interventions, omissions or incorrect treatment, or from a chain of events resulting from any of the above. Indirect obstetric deaths are those resulting from a previously existing disease or a disease that developed during pregnancy and which was not due to direct obstetric causes but which was aggravated by the physiological effects of pregnancy.
In the context of developing countries, it is useful to use the direct–indirect dichotomy, even though the two terms are broad. Moreover, discriminating between them may be difficult at times and misclassification can occur. The only concrete way of determining the cause of death accurately is by autopsy. However, this is simply not a viable option for most cases in resource-poor settings.8 In addition, recent discussions about the ICD classification of maternal death recognize the difficulty of identifying a maternal deaths and it is recommended that new coding instructions are included in the next revision of the ICD.
In developing countries, the most common causes of direct maternal death are haemorrhage, sepsis, pregnancy-induced hypertension and complications of unsafe abortion, while the most common causes of indirect maternal death are anaemia, HIV/AIDS and malaria.9
While many of the problems associated with measuring maternal mortality have been discussed for a number of years, the classification of indirect maternal death was only included in the ICD, 9th revision, in 1975 and it is only recently that indirect maternal death has been attracting more attention as it becomes the leading cause of maternal death in developed countries.10 The earlier lack of attention to indirect maternal death may stem from a number of factors, such as the measurement difficulties previously mentioned and the fact that, until recently, indirect causes of maternal death were dwarfed by direct causes. This situation is changing with the increase in HIV/AIDS and the growing relative importance of noncommunicable diseases, such as cardiovascular disease, diabetes and respiratory disease.
The primary aim of this paper is to highlight the usefulness of differentiating between direct and indirect maternal deaths in ensuring the effective and reliable monitoring and evaluation of interventions for reducing mortality. Interventions such as the provision of skilled birth attendants and emergency obstetric care, while crucial in tackling the direct causes of maternal death, are unlikely to have a preventative or therapeutic effect on indirect causes unless a woman presents with a complication from an indirect cause during labour. Our hypothesis is that the failure to differentiate between direct and indirect maternal deaths may lead to inaccurate evaluations of interventions and underestimates of their effects because causes of death that are not targeted by a particular intervention may be included when measuring its effect. Furthermore, the need to provide additional or alternative interventions to combat indirect maternal death may remain obscured if the outcome being evaluated is only all-cause maternal death. In the following sections, we present examples supporting this hypothesis that have been taken from a number of sources, including data collected by the Initiative for Maternal Mortality Programme Assessment (Immpact).11
Evidence
Ghana 2003–2006
Between 2003 and 2006, Immpact conducted an evaluation of the waiving of official delivery fees in two regions of Ghana, referred to as the user fee exemption policy, to determine the effect on maternal health outcomes.12,13 A new method for identifying maternal deaths in institutions was developed, called the Rapid Ascertainment Process for Institutional Deaths.14 It involved screening hospital records to identify all deaths of women of reproductive age in 12 health-care facilities in the Volta region of Ghana and in 9 in the Central region. Maternal deaths that occurred before and after implementation of the user fee exemption policy were compared.
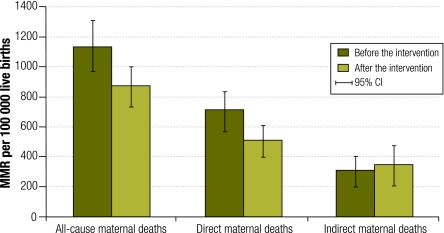
Overall, there was a statistically significant decrease in the institutional MMR from 1134 per 100 000 live births (95% confidence interval, CI: 964–1303) before implementation of the policy to 874 per 100 000 (95% CI: 741–1007) after (P < 0.02). While this decline suggests that the intervention was effective, the evidence becomes stronger when MMRs for direct and indirect maternal deaths are separated (Fig. 1). The MMR for direct deaths fell significantly by 29% from 714 per 100 000 live births (95% CI: 579–848) before the intervention to 506 per 100 000 (95% CI: 405–608) after (P < 0.02). In contrast, the MMR for indirect deaths rose, albeit not significantly, from 307 per 100 000 live births (95% CI: 218–395) to 341 per 100 000 (95% CI: 258–425), with infections unrelated to pregnancy (e.g. malaria and HIV) being the main causes of indirect maternal death. These findings suggest that the removal of official delivery fees had a substantial effect on direct maternal deaths but no impact on indirect maternal deaths, which is the pattern one would expect from an effective intervention targeting the delivery period.
Fig. 1.
MMRs before and after the introduction of a policy to waive official delivery fees, for all-cause, direct and indirect maternal deaths, Ghana, 2003–2006
CI, confidence interval; MMR, maternal mortality ratio.
Furthermore, when the results of this study were stratified by region, the fall in the all-cause institutional MMR in the Central region was not statistically significant: from 953 to 856 deaths per 100 000 births (P = 0.45). But when deaths were classified as direct or indirect maternal deaths, the reduction in the MMR for direct maternal deaths was of borderline statistical significance: from 615 to 444 deaths per 100 000 births (P = 0.08). This indicates that the effect of the intervention on direct maternal deaths would have been missed if the analysis had been confined to the all-cause MMR.
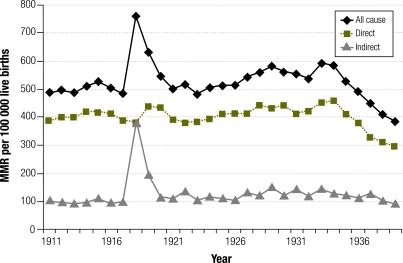
England and Wales 1918
Further evidence comes from historical data for England and Wales.15 Fig. 2 plots MMRs for all-cause, direct and indirect maternal deaths for England and Wales from 1911 to 1940. The prominent peak in indirect deaths in 1918 was due to a flu epidemic; the risk that a woman would die during pregnancy or childbirth from flu increased by a factor of 90 compared with the previous year. Over the same period, the direct maternal mortality rate remained fairly stable, thus the change in the MMR for all-cause maternal deaths primarily reflected the change in the MMR for indirect maternal deaths.
Fig. 2.
MMRs for all-cause, direct and indirect maternal deaths in England and Wales, 1911–1940
MMR, maternal mortality ratio.
The pattern described above is also likely to be found in modern-day outbreaks of infectious disease such as cholera or yellow fever. Approaches to monitoring and evaluating interventions aimed at reducing maternal mortality need to be configured so that they acknowledge the burden of epidemics on pregnant women and incorporate a mechanism for protecting these women, given their increased vulnerability. Methods of monitoring and evaluation that can disaggregate direct and indirect maternal deaths will be able to identify the effects of epidemics on maternal mortality more accurately and evaluate interventions aimed at reducing these effects more effectively.
South Africa 1998–2004
The proportion of maternal deaths classified as indirect could be increasing in areas with a high prevalence of HIV/AIDS. South Africa, one of the very few less-developed countries to have introduced a system of Confidential Enquiry into Maternal Deaths, provides an illustration of this apparent trend. Between 1998 and 2002–2004, the proportion of maternal deaths due to indirect causes rose from 33.4% to 43.4%.1 The overall estimated MMR in South Africa in 1998 was 84 maternal deaths per 100 000 live births; this increased to 124 per 100 000 in 2002–2004. Using the proportions of indirect maternal deaths identified by the Confidential Enquiry into Maternal Deaths, it can be shown that the MMR for indirect maternal deaths during the study period increased from 28 to 54 deaths per 100 000 live births, an increase of 93%, while the MMR for direct maternal deaths rose from 54 to 66 per 100 000, a far smaller increase of 22%.16 While the increase in the MMR for direct maternal deaths is smaller than that for indirect maternal deaths, it is still noteworthy. One factor that may have contributed to this increase is the misclassification of death due to HIV/AIDS that can occur in settings where there is a large number of undiagnosed HIV/AIDS cases, such as South Africa.17 In this situation, using only the MMR for all-cause maternal deaths masks the greater increase in, and the growing problem of, the indirect causes of maternal death.
In the 2002–2004 Confidential Enquiry into Maternal Deaths report, the leading cause of maternal death in South Africa was infection unrelated to pregnancy, with AIDS being not only the most common subcategory of non-pregnancy-related maternal deaths, but also the single most common subcategory of all maternal deaths.18 Bicego et al. also found a concomitant increase in the risk of maternal death with the increase in HIV prevalence in Malawi and Zimbabwe and concluded that, “maternal mortality measurements should separate direct obstetric from other causes”.19 A similar situation is likely to exist in other sub-Saharan African countries with a high prevalence of HIV/AIDS. However, this is not easy to confirm without appropriate monitoring systems in place.
Rwanda 1998
In 2002, Hammerich et al. conducted research into the impact of malaria on pregnancy in an area of unstable transmission in Rwanda.20 The authors found marked increases in maternal admissions for malaria to Byumba District Hospital, Rwanda during periods of heavy rainfall. One such period occurred in early 1998, when the annual number of maternal deaths more than tripled from 10 in 1997 to 35 in 1998, while maternal deaths related to malaria increased five-fold from 5 to 25 over the same period. Overall in 1998, 71% of maternal deaths recorded by the hospital were related to malaria. The researchers noted that even in nonepidemic years malaria can cause a large proportion of maternal deaths and that national and international responses dealing with malaria in pregnancy need strengthening. In particular, they advocate common action by all stakeholders within the framework of the World Health Organization’s Roll Back Malaria campaign and recommended wider initiatives aimed at addressing the sixth Millennium Development Goal.
Discussion
The examples of maternal death assessment in different countries presented in this paper make a compelling case for distinguishing between direct and indirect maternal deaths when planning, monitoring and evaluating interventions for improving maternal health and highlight the need for interventions to address both the direct and indirect causes of maternal death. Failure to differentiate between these two categories may lead to unrealistic expectations about the effect of an intervention on the total MMR, to misleading estimates of the success or failure of a particular intervention, to the neglect of major causes of death (i.e. those leading to indirect maternal deaths) and, consequently, to the misallocation of resources. For example, providing skilled birth attendance and emergency obstetric care may be effective in reducing direct maternal mortality in certain settings. However, this reduction can take place without there being a corresponding decline in the MMR for all-cause maternal deaths because of the failure to reduce, or even to prevent an increase in, indirect maternal deaths. We would suggest that the specific means of addressing the burden of maternal mortality in a particular context can only be identified by disaggregating direct and indirect maternal deaths. Consequently, when evaluating an intervention, evaluators must be explicit about the complications of pregnancy or delivery that the intervention is aiming to tackle and about the types of maternal death that may not be prevented by the intervention and that, therefore, need to be addressed by alternative mechanisms. After all, the main purposes of an evaluation are to determine whether or not resources are being used effectively and to identify those areas that require more attention.
The failure to include the indirect causes of maternal death in monitoring and evaluation may have significant knock-on effects on programme planning. In the Ghanaian example, the effects of the intervention in the Central region would have been missed if all-cause maternal mortality had been used as the sole indicator and no distinction had been made between direct and indirect maternal deaths. In addition, the examples from England and Wales, Rwanda and South Africa all illustrate situations in which an epidemic, that is an indirect cause of maternal death, might either mask or accentuate the effects of interventions.
Findings in other countries in western Africa21,22 similar to those reported above for Rwanda reinforce the message that malaria can have a significant impact on maternal mortality during the rainy season. In addition, McCaw-Binns et al.23 report data from Jamaica on an increase in HIV/AIDS-related maternal deaths that was associated with a rise in indirect maternal deaths overall while direct obstetric deaths were decreasing. The authors of the report state that,23 “[d]eclines in direct mortality may be associated with surveillance and related improvements in obstetric care. Increased indirect deaths from HIV/AIDS, cardiac disease, sickle cell disease and asthma suggests the need to improve collaboration with medical teams to implement guidelines to care for pregnant women with chronic diseases.” The authors also note that while improvements in the coverage and quality of obstetric care have contributed to a decline in direct maternal mortality, they have had a limited impact on indirect maternal mortality.
However, the accurate differentiation of direct and indirect maternal deaths requires the existence of specific mechanisms not only for identifying and counting maternal deaths, but also for collecting detailed information on the cause of death. This presents a considerably greater challenge than simply measuring and reporting all-cause maternal mortality, which, as previously discussed, is already difficult.24 The underreporting of maternal deaths, even in hospital settings, has been highlighted by findings from Immpact which show that many additional maternal deaths can be identified from case note reviews.25 Indirect maternal deaths were particularly likely to be missed because they often occurred in wards outside the maternity area and were frequently reported as non-maternal deaths.26,27
Given the underreporting observed in institutions where record-keeping is theoretically in place, it may be expected that direct and especially indirect maternal deaths in the community would be underreported to an even greater extent. Furthermore, in developing countries, where access to health-care services is limited, it is often the case that the majority of deaths occur in the community and not in a hospital or health centre.24 Verbal autopsy is still the main method used to collect information on the cause of death at the population level in countries where vital registration is inadequate and the level of professional birth attendance is low.28,29 Interviewing someone who is familiar with the circumstances of a death but who is highly likely to lack medical knowledge and then eliciting a cause of death from the signs, symptoms and circumstances of that death is prone to error. Research is currently being undertaken to develop more efficient methods for determining which deaths should be investigated30 and more efficient ways of analysing the data generated.31
In the limited number of developing countries that have sufficiently detailed data to differentiate between direct and indirect maternal deaths, programme planners are able to make use of the information to increase the accuracy and improve the targeting of maternal health programmes. In South Africa, the Confidential Enquiry into Maternal Deaths system has highlighted the fact that indirect causes of maternal death urgently need to be addressed by policy and planning initiatives, a situation that may not have been recognized had the system not been established.
Even though the importance of separating the direct and indirect causes of maternal death has been demonstrated, manuals available on the monitoring and evaluation of strategies for reducing maternal mortality and on the indicators used in such evaluations32–34 either fail to mention, or are extremely limited in their discussion of, the indirect causes of maternal death. The evidence presented here indicates that it is essential that current guidelines on the planning, monitoring and evaluation of maternal health interventions and programmes are updated to include indirect maternal deaths. As Bicego et al.19 comment in their study on the increase in maternal mortality associated with the HIV epidemic, “these observations have important implications for intervention strategies and monitoring in the context of safe motherhood programmes.”
Given the clear lack of progress towards achieving MDG-5, it is important that, if this goal is to become a reality, the best health-care interventions and strategies should be identified on the basis of sound evidence and should be put into practice. As AbouZahr has pointed out, “[a] comprehensive analysis of the burden of obstetric mortality and morbidity would need to address both direct and indirect causes of death and disabilities…”27 It also has to be acknowledged that, as a whole, maternal deaths result from health system failures at many levels.
Differentiating between direct and indirect maternal deaths will enable the monitoring and evaluation of interventions and programmes to be performed more accurately and will contribute to addressing failures and identifying what actually works in different contexts. Information on the relative importance of the direct–indirect dichotomy can then be used at the planning stage to ensure the optimum allocation of resources to areas in which the burden of maternal mortality is greatest. For future research, we recommend that maternal death data should be modelled to determine the influence of indirect maternal deaths on trends in direct maternal deaths and overall maternal mortality. This would give a more accurate measure of progress, which is essential for evaluating work towards MDG-5. ■
Acknowledgements
This work was undertaken as part of the Initiative for Maternal Mortality Programme Assessment (Immpact), which is funded by the Bill & Melinda Gates Foundation, the United Kingdom Department for International Development, the European Commission and the United States Agency for International Development (USAID). Immpact is an international research programme that also provides technical assistance through its consultancy arm, Ipact. The funders have no responsibility for the information provided or views expressed in this paper. The views expressed herein are solely those of the authors. We are grateful to our colleague Lucia D’Ambruoso and anonymous reviewers for their constructive comments on earlier versions of this paper.
Footnotes
Funding: Immpact, funded by the Bill & Melinda Gates Foundation, the UK Department for International Development, the European Commission and USAID.
Competing interests: None declared.
References
- 1.Campbell OM, Graham W. Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 2.Maternal mortality in 2000: estimates developed by WHO, UNICEF, UNFPA.2004 Available from: http://www.reliefweb.int/library/documents/2003/who-saf-22oct.pdf
- 3.Clemens M, Kenny C, Moss T. The trouble with the MDGs: confronting expectations of aid and development success. World Dev. 2007;35:735–51. doi: 10.1016/j.worlddev.2006.08.003. [DOI] [Google Scholar]
- 4.Hussein J, Braunholtz D, D’Ambruoso L. Maternal health in the year 2076. Lancet. 2008;371:203–4. doi: 10.1016/S0140-6736(08)60130-0. [DOI] [PubMed] [Google Scholar]
- 5.Hill K, Thomas K, AbouZahr C, Walker N, Say L, Inoue M, et al. Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet. 2007;370:1311–9. doi: 10.1016/S0140-6736(07)61572-4. [DOI] [PubMed] [Google Scholar]
- 6.Graham WJ, Ahmed S, Stanton C, Abou-Zahr C, Campbell OM. Measuring maternal mortality: an overview of opportunities and options for developing countries. BMC Med. 2008;6:12. doi: 10.1186/1741-7015-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Measuring maternal mortality: challenges, solutions and next steps Washington, DC: Population Reference Bureau; 2007. Available from: http://www.prb.org/pdf07/MeasuringMaternalMortality.pdf [accessed on 1 October 2009].
- 8.Kuo AM, Haukoos JS, Witt MD, Babaie ML, Lewis RJ. Recognition of undiagnosed HIV infection: an evaluation of missed opportunities in a predominantly urban minority population. AIDS Patient Care STDS. 2005;19:239–46. doi: 10.1089/apc.2005.19.239. [DOI] [PubMed] [Google Scholar]
- 9.Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 10.Centre for Maternal and Child Enquiries. Saving mothers lives: reviewing maternal deaths to make motherhood safer 2003–2005 2007. [DOI] [PubMed]
- 11.A global research initiative for the evaluation of safe motherhood intervention strategies. Immpact; 2008. Available from: http://www.immpact-international.org/ [accessed on 6 August 2008].
- 12.Bosu W, Bell J, Armar-Klemesu M, Ansong Tornui J. Effect of the delivery care user fee exemption policy on institutional maternal deaths in the Central and Volta regions of Ghana. Ghana Med J. 2007;41:118–24. doi: 10.4314/gmj.v41i3.55278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery fee exemption policy in Ghana: population estimates of changes in delivery service utilization in two regions. Ghana Med J. 2007;41:100–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Immpact toolkit: a guide and tools for maternal mortality programme assessment Immpact; 2008. Available from: http://www.immpact-international.org/toolkit/ [accessed on 6 August 2008].
- 15.Macfarlane A, Mugford M. Birth counts: statistics of pregnancy and childbirth United Kingdom: The Stationary Office; 2000. [Google Scholar]
- 16.United Nations. South Africa. Millennium development goals: country report2005 Available from: http://planipolis.iiep.unesco.org/upload/South%20Africa/South%20Africa%20MDG%20Report.pdf [accessed on 6 August 2008].
- 17.Ordi J, Ismail MR, Carrilho C, Romagosa C, Osman N, Machungo F, et al. Clinico-pathological discrepancies in the diagnosis of causes of maternal death in sub-Saharan Africa: retrospective analysis. PLoS Med. 2009;6:e1000036. doi: 10.1371/journal.pmed.1000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.PattisonB. Saving mothers: third report on confidential enquiries into maternal deaths in South Africa 2002–2004.
- 19.Bicego G, Boerma JT, Ronsmans C. The effect of AIDS on maternal mortality in Malawi and Zimbabwe. AIDS. 2002;16:1078–81. doi: 10.1097/00002030-200205030-00019. [DOI] [PubMed] [Google Scholar]
- 20.Hammerich A, Campbell OM, Chandramohan D. Unstable malaria transmission and maternal mortality: experiences from Rwanda. Trop Med Int Health. 2002;7:573–6. doi: 10.1046/j.1365-3156.2002.00898.x. [DOI] [PubMed] [Google Scholar]
- 21.Anya SE. Seasonal variation in the risk and causes of maternal death in the Gambia: malaria appears to be an important factor. Am J Trop Med Hyg. 2004;70:510–3. [PubMed] [Google Scholar]
- 22.Etard JF, Kodio B, Ronsmans C. Seasonal variation in direct obstetric mortality in rural Senegal: role of malaria? Am J Trop Med Hyg. 2003;68:503–4. [PubMed] [Google Scholar]
- 23.McCaw-Binns A, Alexander SF, Lindo JL, Escoffery C, Spence K, Lewis‑Bell K, et al. Epidemiologic transition in maternal mortality and morbidity: new challenges for Jamaica. Int J Gynaecol Obstet. 2007;96:226–32. doi: 10.1016/j.ijgo.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Graham WJ, Foster LB, Davidson L, Hauke E, Campbell OM. Measuring progress in reducing maternal mortality. Best Pract Res Clin Obstet Gynaecol. 2008;22:425–45. doi: 10.1016/j.bpobgyn.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Sombie I, Meda N, Hounton S, Bambara M, Ouedraogo T, Graham W. Missing maternal deaths: lessons from Souro Sanou University Hospital in Bobo-Dioulasso, Burkina Faso. Trop Doct. 2007;37:96–8. doi: 10.1258/004947507780609239. [DOI] [PubMed] [Google Scholar]
- 26.Qomariyah SN, Bell JS, Pambudi ES, Anggondowati T, Latief K, Achadi EL, et al. A practical approach to identifying maternal deaths missed from routine hospital reports: lessons from Indonesia. Global Health Action 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.AbouZahr C. Global burden of maternal death and disability. BMJ. 2003;67:1–11. doi: 10.1093/bmb/ldg015. [DOI] [PubMed] [Google Scholar]
- 28.Campbell OM, Ronsmans C. Verbal autopsies for maternal deaths: report of a WHO workshop, London, 10–13 January 1994 Geneva, World Health Organization, 1995. [Google Scholar]
- 29.Verbal autopsy. Maternal mortality measurement resource Available from: http://www.maternal-mortality-measurement.org/MMMResource_Tool_VerbalAutopsy.html [accessed on 7 May 2009].
- 30.Immpact toolkit. Maternal death from informants and maternal death follow-on review (MADE-IN / MADE-FOR) Available from: http://www.immpact-international.org/toolkit/module4/mimf/ [accessed on 7 May 2009].
- 31.Fottrell E, Byass P, Ouedraogo TW, Tamini C, Gbangou A, Sombie I, et al. Revealing the burden of maternal mortality: a probabilistic model for determining pregnancy-related causes of death from verbal autopsies. Popul Health Metr. 2007;5:1. doi: 10.1186/1478-7954-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maine D, Akalin M, Ward V, Kamara, A. The design and evaluation of maternal mortality programs 1997.
- 33.UNFPA. Programme manager’s planning, monitoring & evaluation toolkit. Tool number 6: programme indicators. Part II: indicators for reducing maternal mortality Available from: http://www.unfpa.org/monitoring/toolkit/Tool6_2.doc [accessed on 16 June 2008].
- 34.Maine D, Bailey P. Indicators for design, monitoring and evaluation of maternal mortality programs 2001.