Abstract
Total parenteral nutrition (TPN), or the complete absence of enteral nutrients, is commonly used in a clinical setting. However, a major consequence of TPN administration is the development of mucosal atrophy and a loss of epithelial barrier function (EBF); and this loss may lead to an increase in clinical infections and septicemia. Our laboratory has investigated the mechanism of this TPN-associated loss of EBF using a mouse model. We have demonstrated that the mucosal lymphoid population significantly changes with TPN, and leads to a rise in IFN-γ and decline in IL-10 expression – both of which contribute to the loss of EBF. Associated with these cytokine changes is a dramatic decline in the expression of tight junction and adherens junction proteins. This article discusses the potential mechanisms responsible for these changes, and potential strategies to alleviate this loss in EBF.
Keywords: epithelial barrier function, tight junction, Intraepithelial lymphocyte, Interleukin-7 (IL-7), interferon gamma (IFN-γ), IL-10, Mouse, epithelial cells
Introduction
The intestinal epithelium undergoes both morphological and functional changes during total parenteral nutrition (TPN) administration. Many patients, because of either gastrointestinal dysfunction or a lack of intestinal length, are unable to tolerate enteral feedings. These patients are confined to a prolonged course of TPN. It is estimated that over 250,000 patients receive TPN in the United States alone on a yearly basis 1, resulting in over 11.5 million patient days of care per year. Increasingly, investigators have found that the intestine undergoes significant changes during the administration of TPN with an absence of enteral nutrition. In several TPN animal models, the intestinal epithelium shows a loss of villus height and a decline in epithelial growth 2, 3. Further analysis of the mucosa shows a loss of epithelial barrier function (EBF) during the administration of TPN 4. This loss of barrier function may result in endotoxins and even bacteria entering the systemic circulation.
Clinical Consequences of a Loss of Epithelial Barrier Function with TPN
Loss of EBF with TPN may well be a potential mechanism for the observed higher rates of septicemia and other clinical infectious processes. Significantly higher rates of sepsis and infection have been strongly associated with TPN in the clinical settings of surgery and trauma 5, 6. The etiology of these increased rates of infection is controversial. Systemic immunologic changes are quite common during the administration of TPN, and include both a decrease in absolute lymphocyte counts and a depression in lymphocyte function 7-9.
Use of a TPN Mouse Model to Study Mucosal Atrophy and Epithelial Barrier Function
The mouse model of TPN has yielded valuable insights, and may actually more closely resemble clinical TPN administration than other animal models. Previous studies with TPN in rat models showed a rapid progression of villus atrophy within a matter of 3 days 10. Such changes do not occur as rapidly in humans receiving TPN, and thus must be carefully interpreted. Mouse models of TPN show the development of villus atrophy and formation of an epithelial barrier leak in a delayed period of onset (twice as long as rats), and more similar (although still more rapid) to humans.
TPN administration results in a loss of mucosal barrier function
Loss of EBF has been identified both in experimental models of TPN 3, 10, 11 and in humans 12. The mechanism by which TPN leads to a loss of epithelial integrity has only recently been approached. In vitro cultures of intestinal epithelial cells (EC) have given critical insights into these mechanisms. A number of cytokines influence EBF. This was first shown in human intestinal EC (T84 cell line) incubated with interferon gamma (IFN-γ) 13. Using a similar in vitro model, others have shown that pretreatment with transforming growth factor beta 1 (TGF-β1) can prevent the effects of IFN-γ 14. A number of other cytokines have also been shown to affect EBF. Similar to TGF-β1, IL-10 can attenuate the loss of epithelial barrier in T84 monolayers caused by IFN-γ 15. IL-4, however, can lead to a loss of EBF in a similar in vitro model 16. Other cytokines which have been associated with a loss of EBF include IL-6 and tumor necrosis factor alpha (TNF-α) 17. Loss of barrier function with TPN appears to be closely associated with the increased expression of IFN-γ by intraepithelial lymphocytes (IEL) 11, 18.
Gut-Associated Lymphoid Tissue (GALT)
The gastrointestinal tract is exposed to a number of foreign antigens on a daily basis, including toxins, bacteria, viruses and a number of diverse enteral nutrients. A critical part of protecting the host from these factors is the GALT. The GALT is a complex immunologic organ which contains several layers within the intestinal tract 19-21. The layer of the GALT closest to the lumen is the intraepithelial lymphocytes (IEL). The IEL has a unique T-cell phenotype, and plays a critical role in both proliferative and cytotoxic T-lymphocyte actions 22, 23. The IEL phenotype predominately consists of CD4-,CD8+ (70-85%, for mice, single positive), with other less frequent sub-populations: CD4-,CD8- (5-10%, double negative); CD4+,CD8- (5-12%, single positive); and CD4+,CD8+ (4-10%, double positive) 24, 25. The IEL also has a large number of γδ-TCR+ cells (30-70% compared to less than 2% in peripheral blood lymphocytes of mice) 26. The IEL is thought to be derived from both a thymic-dependent and a thymic-independent source. Although still controversial 27, studies suggest that the IEL originate from both the intestinal tract as well as the thymus 27, 28. RAG2-/- mice injected with bone marrow of nude mice failed to develop peripheral T-cells – but did develop a nearly normal IEL population which contained CD8+ T-cells with both γδ– or αβ-TCR+ phenotype 29. Although still controversial, the thymic-independent portion of the IEL is best defined by the CD8αα homodimeric T-cell population. In contrast, CD8αβ (heterodimeric) cells are believed to be of thymic origin. The function of the IEL has not been completely determined. Using a redirected cytotoxic functional assay without in vitro activation, the IEL shows considerable activity 30. The actual significance of these actions has not been completely defined, but suggests a role in protecting the organism from harmful intraluminal pathogens. The IEL is also a rich source of cytokines, including: IFN-γ 31, IL-2 32, IL-4 33, IL-6 34, TNF-α 35, and TGF-β1 36. TGF-β1 has been detected in both αβ-TCR+ and γδ–TCR+ IEL subsets 37. IL-10 has recently been shown to be expressed in the IEL, and may closely relate to the modulation and function of T-regulatory cells 38. Cytokine production in the αβ-TCR+ fraction of the IEL has been extensively studied, and the CD4+,CD8- population expresses IFN-γ, IL-4 and IL-5 37, 39. The CD4+,CD8+ population expresses greater amounts of IFN-γ and IL-5. The CD4-,CD8+ population produces IFN-γ, IL-5 and some IL-6. It appears that a major aspect of IEL regulatory function is achieved by specific cytokine production. It is hypothesized that IEL cytokine production leads to modulation in epithelial cell function 40, as well as to a down-regulation of immunologic sensitization to foreign antigen 33.
IEL Closely Interact with Mucosal Epithelial Cells
Because of the close physical association of the IEL with mucosal EC, interactions between the two populations have been examined. EC express essential ligands which are needed for IEL to adhere and reside within the mucosal epithelium 41. Interestingly, these ligands are expressed along the basolateral surface of the EC, in juxtaposition to IEL. Perhaps the best characterized of these is the integrin αEβ7 on the IEL and E-cadherin on the surface of the epithelial cells 42. Another important manner in which the IEL and EC intercommunicate is via the large number of cytokines, growth factors and chemokines which are expressed by EC. One such example is that EC-derived IL-7 strongly influences the development, growth and phenotype of the adjacent IEL 43. IL-7-/- or IL-7R-/- mice show distinct declines in absolute numbers of thymocytes and IEL, with a virtual absence of the γδ– TCR+ population, and fewer αβ-TCR+ T cells than wild-type mice 44.
Changes in the IEL with TPN Administration
Phenotypic changes
A number of IEL phenotypic alterations occur with TPN, and include a marked decline in the CD4+, CD44+ and CD8αβ+ populations (Table 1). The CD4+ population is known to be very responsive to exogenous stimulation, and its loss may explain an observed loss of IEL proliferative responsiveness with TPN 31. The loss of the CD8αβ+ population with TPN may represent a loss of the thymic-dependent population of the IEL 29, and the loss of CD44+ cells suggests a shift to a less mature IEL 45. Interestingly, the alteration in IEL phenotype did not correlate with enteral anaerobic or aerobic bacterial cultures, in that the number and strain of these bacteria did not significantly change with TPN 31. An additional group is shown in Table 1, that of TPN mice allowed small amounts of enteral food (TPN+Food group; comprising 25% of caloric needs). Interestingly, IEL phenotype changes were significantly influenced by the loss of enteral nutrition; most of the observed IEL changes with TPN were reversed with the addition of this small amount of enteral nutrition. The mechanism by which enteral food prevents the observed IEL changes has not been determined.
Table 1.
Small bowel IEL phenotype in Control and TPN mice. Column on right are mice maintained on TPN and allowed ad lib chow. Results are from flow cytometry studies after gating on the IEL population. CD4,CD44 results not shown because of the marked loss of the CD4+ population with TPN. Results are expressed as mean % gated IEL (ranges) and represents an N=6 mice for each group.
| IEL Phenotypes | Description | Control (range) |
TPN (range) |
TPN+Food (range) |
|---|---|---|---|---|
| CD4 and CD8α | ||||
| CD4+CD8- | single positive | 4.7 (3.9-6.1) | 0.6 (0.2-0.7)* | 2.5 (1.9-2.8) |
| CD4+CD8+ | double positive | 2.8 (2.5-4.3) | 0.6 (0.1-1)* | 5.4 (3.8-12.1) |
| CD4-CD8- | double negative | 28 (23-34) | 35 (19-64) | 16 (12-28) |
| CD4-CD8+ | single positive | 65 (58-70) | 64 (37-79) | 72 (67-77) |
| CD8αα and CD8αβ | ||||
| CD8αα+ | thymic-independent | 64 (59-71) | 52 (40-63) | 72 (66-78) |
| CD8αβ+ | thymic-dependent | 4.8 (3.0-6.5) | 0.4 (0.1-0.8)* | 7.4 (5.6-8.6) |
| TCR-αβ vs. TCR-γδ | ||||
| TCR-αβ+ | T-cell receptor | 39 (33-43) | 22 (21-31) | 24 (18-28) |
| TCR-γδ+ | T-cell receptor | 62 (53-68) | 70 (57-76) | 57 (51-62) |
| CD44 | T-cell maturity | |||
| CD8+,CD44+ | 29 (28-37) | 10 (1.0-18)* | 40 (38-46) |
P<0.01, by ANOVA.
Cytokine expression
Table 2 shows changes in cytokine expression with TPN 31, 36, 46. This panel of cytokines was chosen because each of these has been shown to alter either barrier function or apoptotic signaling in the intestine 15, 16, 47-51. Our laboratory reported a rise in IFN-γ expression with TPN, and this could well impact both the observed increase of EC apoptosis 52 as well as a loss of EBF (see below). In addition to IFN-γ, other cytokines may also have relevance to EC physiology, including IL-4, IL-6 and IL-10 (Table 2). As mentioned above, each of these cytokines can contribute to changes in EBF. It is possible that the decline in IL-10 mRNA expression and the rise in IL-4 and IL-6 may all contribute to the development of the TPN-associated epithelial leak and increased rates in EC apoptosis. The administration of 25% enteral nutrition to TPN mice prevented these cytokine changes. As mentioned earlier, EC-derived IL-7 is another important cytokine within the intestinal mucosa. Our laboratory has shown a close physical relation between EC which express IL-7 and IEL 53. Subsequently, we showed that the administration of TPN results in a significant decline in IL-7 expression 54. With the administration of exogenous IL-7, much of the IEL phenotypic changes associated with TPN can be prevented 54, suggesting that IL-7 may have an important role in the mediation of the changes to the mucosa with TPN administration.
Table 2.
mRNA expression of IEL cytokines in control, TPN and TPN+Food groups. Note the significant alterations in all measured cytokines with administration of TPN, and the prevention of these changes with the addition of enteral feedings to TPN mice. N=6,
| Groups | IL-4 | IL-6 | IL-10 | IFN-γ |
|---|---|---|---|---|
| Control | 0.10±0.1 | 0.02±0.0 | 0.55±0.2 | 0.15±0.1 |
| TPN | 0.73±0.3** | 0.95±0.3** | 0.23±0.1** | 0.29±0.1* |
| TPN+Food | 0.11±0.1 | 0.05±0.0 | 0.65±0.2 | 0.14±0.0 |
P <0.05,
P<0.01 TPN vs. Control and TPN+Food; using ANOVA. In general a Bonferonni post hoc t test is used for remaining Preliminary results. Results are the mean (±SD) mRNA expression of cytokine from purified IEL (via magnetic beads) samples, and expressed as the ratio of cytokine expression to beta actin. Abbreviations: IFN-γ: interferon gamma. (Data submitted to J Surg Res).
Impact of IEL-derived Cytokines and Epithelial Barrier Function
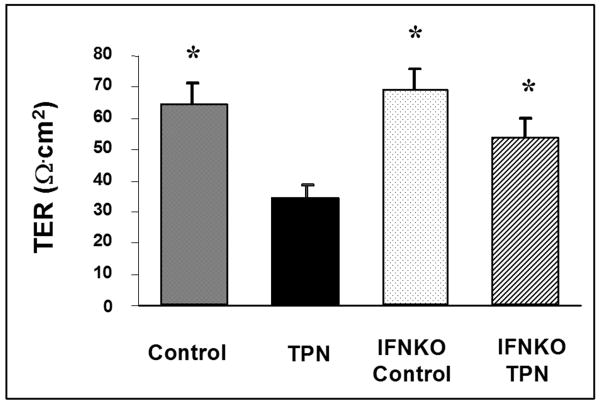
TPN-associated increases in IEL-derived IFN-γ and decline in IL-10 expression have both been associated with a loss of EBF 11, 18, 55. A significant decline in transepithelial resistance (TER) of full-thickness ileum is noted in the TPN group. In order to determine the influence that increased expression of IFN-γ had on this change in EBF, a series of IFN-γ knockout mice underwent TPN administration. In the absence of IFN-γ, the degree of TPN-associated epithelial barrier breakdown, as measured by either the permeability coefficient (Papp) or by transepithelial resistance (TER) (Figure 1), was significantly lessened 46. The fact that permeability levels did not completely return to normal suggested that other mediators of this breakdown exist. Whether this is a direct action of IFN-γ on the EBF, or if acts to prime tumor necrosis factor receptors remains to be determined 56. Subsequently, our group then determined the influence of the decline in IL-10 with TPN administration. Sun, et al demonstrated that the additional administration of exogenous IL-10 to mice receiving TPN resulted in a return of EBF toward normal 55. Similar to the IFN-γ mice, exogenous IL-10 partially prevented this barrier loss; however, the effect was only about 50% effective. This suggests that the cytokine changes with TPN administration account for a substantial degree of EBF loss.
Figure 1.
Transepithelial resistance (TER) in mice was measured in Ussing chambers after a 30 min equilibration period. Results (mean ± SD) in 6 mice per group. TPN significantly decreased intestinal TER in wild-type mice. Elimination of IFN-γ was achieved using knockout mice (IFNKO). Significance was found between the TPN and all other study groups; the other groups were not significantly different between themselves. ANOVA was used for statistical analysis. *P<0.05 comparing TPN group to other groups, with a Bonferonni post hoc analysis.
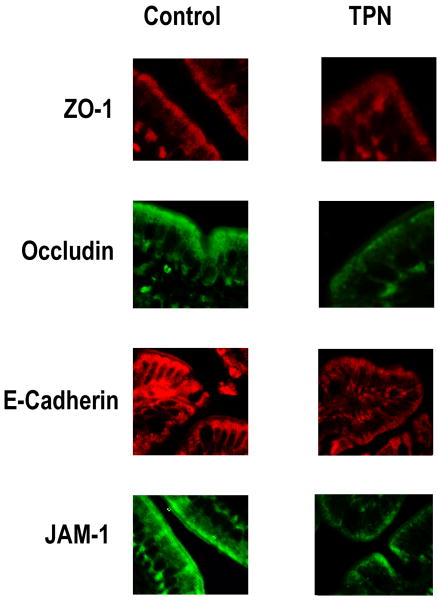
Alteration in the Tight Junction with TPN
The etiology of this loss of EBF was further investigated. Our laboratory detected a substantial decline in the expression of a number of tight junction molecules 55, including ZO-1, occluden, several claudins and JAM-1, as well as the adherens molecule E-cadherin. Figure 2 shows immunofluorescent images of some of these factors. In addition to a loss of expression, internalization (endocytosis) of some of these factors can be seen – a finding similarly observed in vitro with cytokine exposure to epithelial monolayers, as well as other clinical disease processes where EBF is lost such as in inflammatory bowel disease 50, 57, 58.
Figure 2.
Immunofluorescent images of representative portions of mid-small bowel mucosa in Control (enterally fed) and TPN study groups. Note the loss of junctional and adherens proteins with TPN. Additionally, note the movement of some of these proteins (occludens) into the cytoplasm with TPN administration.
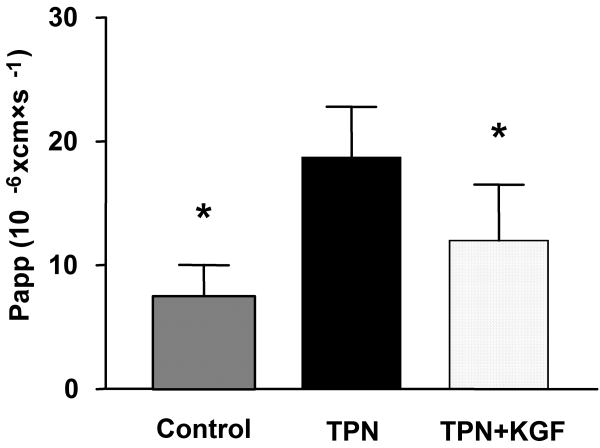
Therapeutic Options to Prevent Barrier Loss with TPN
The IEL not only expresses a number of cytokines, but the γδ-TCR sub-population has been shown to express keratinocyte growth factor (KGF, or fibroblast growth factor-7) 59. Our group has subsequently demonstrated that with TPN administration, there is a marked decline in KGF expression by this IEL sub-population 60. Further, the exogenous administration of KGF to mice receiving TPN was able to significantly prevent loss of villus height, crypt depth and restored EBF (Figure 3) 61. This suggests that the use of KGF may have a therapeutic potential for patients on long-term TPN, and may prevent many of the complications associated with EBF loss.
Figure 3.
Effect of TPN on the permeability coefficient (Papp) of tritiated mannitol as measure in Ussing chambers of full-thickness ileal specimens with TPN administration (*P<0.05). Note also the return of permeability to control levels when TPN mice are given exogenous keratinocyte growth factor (KGF) (5mg/kg/day) 62.
Conclusions
TPN results in a loss of villus height, loss of EC proliferation, rise in EC apoptosis, and a marked decline in EBF. Using a mouse model of TPN, the IEL has been shown to undergo significant changes. Such changes may partially account for the mechanism of EBF loss with TPN, and may contribute to the increased incidence of septicemia with TPN administration. The mechanisms by which IEL change with TPN are not known, but data suggest that such changes are due to a lack of enteral nutrition and may be mediated by a decline in EC-derived IL-7. Understanding the mechanisms which are responsible for such changes may lead to the potential for therapeutic options in patients receiving TPN. Further, understanding the changes in the IEL with TPN administration may also yield important information in how EC-IEL interactions take place. Such interactions appear to directly influence observed alterations in the physiology of the intestinal mucosa. Thus, these cell-cell interactions may have important applications in other processes such as gut adaptation after bowel resection, or during autoimmune processes such as inflammatory bowel disease.
Acknowledgments
This research was supported by NIH grant 2R01-AI044076-10 (to DHT), and the ASPEN Rhoads Research Foundation Maurice Shils Grant (to HY), and the University of Michigan DNA Core, University of Michigan Transgenic Core. National Cancer Institute through the University of Michigan's Cancer Center Support Grant (5 P03 CA46592).
References
- 1.Anderson G, Steinberg E. DRG's and specialized nutritional support: the need for reform. J Paren Enter Nutr. 1986;10:3–10. doi: 10.1177/014860718601000103. [DOI] [PubMed] [Google Scholar]
- 2.Shou J, Lappin J, Minnard EA, Daly JM. Total parenteral nutrition, bacterial translocation, and host immune function. American Journal of Surgery. 1994;167(1):145–50. doi: 10.1016/0002-9610(94)90065-5. [DOI] [PubMed] [Google Scholar]
- 3.Kansagra K, Stoll B, Rognerud C, et al. Total parenteral nutrition adversely affects gut barrier function in neonatal piglets. Am J Physiol Gastrointest Liver Physiol. 2003 doi: 10.1152/ajpgi.00243.2003. [DOI] [PubMed] [Google Scholar]
- 4.Peterson CA, Carey HV, Hinton PL, et al. GH elevates serum IGF-I levels but does not alter mucosal atrophy in parenterally fed rats. American Journal of Physiology. 1997;272(5 Pt 1):G1100–8. doi: 10.1152/ajpgi.1997.272.5.G1100. [DOI] [PubMed] [Google Scholar]
- 5.Moore F, Moore E, Jones T. TEN vs TPN following major abdominal trauma: reduced septic morbidity. J Trauma. 1989;29:916–923. doi: 10.1097/00005373-198907000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kudsk K, Croce M, Fabian T, et al. Enteral versus parenteral feeding. Effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992;215(5):503–511. doi: 10.1097/00000658-199205000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dominioni L, Gnes F, Dionigi R, et al. Histopathological studies on dog lymphoid structures during malnutrition and total parenteral nutrition. Bollettino dell Istituto Sieroterapico Milanese. 1976;55(4):311–6. [PubMed] [Google Scholar]
- 8.Renegar KB, Johnson CD, Dewitt RC, et al. Impairment of mucosal immunity by total parenteral nutrition: requirement for IgA in murine nasotracheal anti-influenza immunity. Journal of Immunology. 2001;166(2):819–25. doi: 10.4049/jimmunol.166.2.819. [DOI] [PubMed] [Google Scholar]
- 9.Kudsk KA, Li J, Renegar KB. Loss of upper respiratory tract immunity with parenteral feeding. Annals of Surgery. 1996;223(6):629–35. doi: 10.1097/00000658-199606000-00001. discussion 635-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ney DM. Effects of insulin-like growth factor-I and growth hormone in models of parenteral nutrition. Jpen: Journal of Parenteral & Enteral Nutrition. 1999;23(6 Suppl):S184–9. doi: 10.1177/014860719902300603. [Review] [41 refs] [DOI] [PubMed] [Google Scholar]
- 11.Yang H, Finaly R, Teitelbaum DH. Alteration in epithelial permeability and ion transport in a mouse model of total parenteral nutrition. Critical Care Medicine. 2003;31(4):1118–1125. doi: 10.1097/01.CCM.0000053523.73064.8A. [DOI] [PubMed] [Google Scholar]
- 12.Buchman A, Moukarzel A, Bhuta S, et al. Parenteral nutrition is associated with intestinal morphologic and functional changes in humans. J Paren Enter Nutr. 1995;19:453–460. doi: 10.1177/0148607195019006453. [DOI] [PubMed] [Google Scholar]
- 13.Madara J, Stafford J. Interferon-γ directly affeccts barrier function of cultured intestinal epithelial monolayers. J Clin Invest. 1989;83:724–727. doi: 10.1172/JCI113938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Planchon S, Martins C, Guerrant R, Roche J. Regulation of intestinal epithelial barrier function by TGF-β1. J Immunol. 1994;153:5730–5738. [PubMed] [Google Scholar]
- 15.Madsen KL, Lewis SA, Tavernini MM, et al. Interleukin 10 prevents cytokine-induced disruption of T84 monolayer barrier integrity and limits chloride secretion. Gastroenterology. 1997;113(1):151–9. doi: 10.1016/s0016-5085(97)70090-8. [DOI] [PubMed] [Google Scholar]
- 16.Colgan SP, Resnick MB, Parkos CA, et al. IL-4 directly modulates function of a model human intestinal epithelium. J Immunol. 1994;153(5):2122–9. [PubMed] [Google Scholar]
- 17.Spies M, Chappell VL, Dasu MR, et al. Role of TNF-alpha in gut mucosal changes after severe burn. Am J Physiol Gastrointest Liver Physiol. 2002;283(3):G703–8. doi: 10.1152/ajpgi.00149.2001. [DOI] [PubMed] [Google Scholar]
- 18.Yang H, Kiristioglu I, Y F, et al. Interferon-gamma expression by intraepithelial lymphocytes results in a loss of epithelial barrier function in a mouse model of total parenteral nutrition. Ann Surg. 2002;236(2):226–234. doi: 10.1097/00000658-200208000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iijima H, Takahashi I, Kiyono H. Mucosal immune network in the gut for the control of infectious diseases. Reviews in Medical Virology. 2001;11(2):117–33. doi: 10.1002/rmv.307. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi I, Kiyono H. Gut as the largest immunologic tissue. Jpen: Journal of Parenteral & Enteral Nutrition. 1999;23(5 Suppl S):S7–S12. doi: 10.1177/014860719902300503. [DOI] [PubMed] [Google Scholar]
- 21.Hershberg RM, Mayer LF. Antigen processing and presentation by intestinal epithelial cells - polarity and complexity. Immunology Today. 2000;21(3):123–128. doi: 10.1016/s0167-5699(99)01575-3. [DOI] [PubMed] [Google Scholar]
- 22.Probert CS, Saubermann LJ, Balk S, Blumberg RS. Repertoire of the alpha beta T-cell receptor in the intestine. Immunol Rev. 2007;215:215–25. doi: 10.1111/j.1600-065X.2006.00480.x. [DOI] [PubMed] [Google Scholar]
- 23.Kronenberg M, Havran WL. Frontline T cells: gammadelta T cells and intraepithelial lymphocytes. Immunol Rev. 2007;215:5–7. doi: 10.1111/j.1600-065X.2006.00489.x. [DOI] [PubMed] [Google Scholar]
- 24.Beagley KW, Husband AJ. Intraepithelial lymphocytes: origins, distribution, and function. Crit Rev Immunol. 1998;18(3):237–54. doi: 10.1615/critrevimmunol.v18.i3.40. [DOI] [PubMed] [Google Scholar]
- 25.Mosley RL, Klein JR. A rapid method for isolating murine intestine intraepithelial lymphocytes with high yield and purity. J Immunol Methods. 1992;156(1):19–26. doi: 10.1016/0022-1759(92)90006-f. [DOI] [PubMed] [Google Scholar]
- 26.Ishiguro Y, Kanazawa H, Munakata A. Approaches to intestinal gamma delta T cells. Molecular Medicine: Novel Findings Of Gene Diagnosis, Regulation Of Gene Expression, and Gene Therapy. 1999;1172:131–136. [Google Scholar]
- 27.Lefrancois L, Puddington L. Extrathymic intestinal T-cell development: virtual reality? Immunol Today. 1995;16(1):16–21. doi: 10.1016/0167-5699(95)80065-4. [DOI] [PubMed] [Google Scholar]
- 28.Rocha B, Vassalli P, Guy-Grand D. Thymic and extrathymic origins of gut intraepithelial lymphocyte populations in mice. J Exp Med. 1994;180(2):681–6. doi: 10.1084/jem.180.2.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rocha B, Guy-Grand D, Vassalli P. Extrathymic T cell differentiation. Curr Opin Immunol. 1995;7(2):235–42. doi: 10.1016/0952-7915(95)80008-5. [DOI] [PubMed] [Google Scholar]
- 30.Ebert E. Intra-epithelial lymphocytes: interferon-gamma production and suppressor/cytotoxic activities. Clin Exp Immunol. 1990;82:81–85. doi: 10.1111/j.1365-2249.1990.tb05407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kiristioglu I, Antony P, Fan Y, et al. Total parenteral nutrition-associated changes in mouse intestinal intraepithelial lymphocytes. Digestive Diseases and Sciences. 2002;47(5):1147–1157. doi: 10.1023/a:1015066813675. [DOI] [PubMed] [Google Scholar]
- 32.Fujihashi K, Kawabata S, Hiroi T, et al. Interleukin 2 (IL-2) and interleukin 7 (IL-7) reciprocally induce IL-7 and IL-2 receptors on gamma delta T-cell receptor-positive intraepithelial lymphocytes. Proceedings of the National Academy of Sciences of the United States of America. 1996;93(8):3613–8. doi: 10.1073/pnas.93.8.3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebert EC, Roberts AI. IL-4 down-regulates the responsiveness of human intraepithelial lymphocytes. Clinical & Experimental Immunology. 1996;105(3):556–60. doi: 10.1046/j.1365-2249.1996.d01-782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Q, Fang C, Hasselgren P. Intestinal permeability is reduced and IL-10 levels are increased in septic IL-6 knockout mice. American Journal of Physiology - Regulatory Integrative & Comparative Physiology. 2001;281(3):R1013–23. doi: 10.1152/ajpregu.2001.281.3.R1013. [DOI] [PubMed] [Google Scholar]
- 35.Lundqvist C, Melgar S, Yeung MM, et al. Intraepithelial lymphocytes in human gut have lytic potential and a cytokine profile that suggest T helper 1 and cytotoxic functions. J Immunol. 1996;157(5):1926–34. [PubMed] [Google Scholar]
- 36.Kiristioglu I, Teitelbaum DH. Alteration of the intestinal intraepithelial lymphocytes during total parenteral nutrition. Journal of Surgical Research. 1998;79(2):91–96. doi: 10.1006/jsre.1998.5408. [DOI] [PubMed] [Google Scholar]
- 37.Fujihashi K, Yamamoto M, McGhee JR, et al. Function of alpha beta TCR+ intestinal intraepithelial lymphocytes: Th1- and Th2-type cytokine production by CD4+CD8- and CD4+CD8+ T cells for helper activity. Int Immunol. 1993;5(11):1473–81. doi: 10.1093/intimm/5.11.1473. [DOI] [PubMed] [Google Scholar]
- 38.Kamanaka M, Kim S, Wan Y, et al. Expression of interleukin-10 in intestinal lymphocytes detected by an interleukin-10 reporter knockin tiger mouse. Immunity. 2006;25(6):941–52. doi: 10.1016/j.immuni.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 39.Fujihashi K, Yamamoto M, McGhee JR, Kiyono H. alpha beta T cell receptor-positive intraepithelial lymphocytes with CD4+, CD8- and CD4+, CD8+ phenotypes from orally immunized mice provide Th2-like function for B cell responses. J Immunol. 1993;151(12):6681–91. [PubMed] [Google Scholar]
- 40.Croitoru K, Ernst P. Intraepithelial lymphocyte lineage and function. The interactions between the intestinal epithelium and the intraepithelial lymphocyte. In: Kiyono H, McGhee J, editors. Mucosal Immunology: Intraepithelial Lymphocytes. Vol. 9. New York: Raven Press Ltd.; 1993. pp. 79–88. [Google Scholar]
- 41.Shaw S, Hermanowski-Vosatka A, Shibahara T, et al. Migration of intestinal intraepithelial lymphocytes into a polarized epithelial monolayer. American Journal of Physiology. 1998;275(3 Pt 1):G584–91. doi: 10.1152/ajpgi.1998.275.3.G584. [DOI] [PubMed] [Google Scholar]
- 42.Benmerah A, Badrichani A, Ngohou K, et al. Homotypic aggregation of CD103 (alpha E beta 7)+ lymphocytes by an anti-CD103 antibody, HML-4. European Journal of Immunology. 1994;24(9):2243–9. doi: 10.1002/eji.1830240946. [DOI] [PubMed] [Google Scholar]
- 43.Laky K, Lefrancois L, Lingenheld E, Puddington L. Enterocyte expression of interleukin 7 induces development of gamma delta T cells and Peyer's patches. J Exp Med. 2000;191:1569–80. doi: 10.1084/jem.191.9.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laky K, Lefrancois L, von Freeden-Jeffry U, et al. The role of IL-7 in thymic and extrathymic development of TCR gamma delta cells. Journal of Immunology. 1998;161:707–713. [PubMed] [Google Scholar]
- 45.Dozmorov IM, Miller RA. Regulatory interactions between virgin and memory CD4 T lymphocytes. Cell Immunol. 1996;172(2):141–8. doi: 10.1006/cimm.1996.0226. [DOI] [PubMed] [Google Scholar]
- 46.Yang H, Kiristioglu I, Fan Y, et al. Interferon-gamma expression by intraepithelial lymphocytes results in a loss of epithelial barrier function in a mouse model of total parenteral nutrition. Annals of Surgery. 2002;236(2):226–234. doi: 10.1097/00000658-200208000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ciacci C, Mahida YR, Dignass A, et al. Functional interleukin-2 receptors on intestinal epithelial cells. J Clin Invest. 1993;92(1):527–32. doi: 10.1172/JCI116598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang WY, Smail N, Wang P, Chaudry IH. Increased Gut Permeability After Hemorrhage Is Associated With Upregulation Of Local and Systemic Il-6. Journal of Surgical Research. 1998;79(1):39–46. doi: 10.1006/jsre.1998.5385. [DOI] [PubMed] [Google Scholar]
- 49.Planchon SM, Martins CA, Guerrant RL, Roche JK. Regulation of intestinal epithelial barrier function by TGF-beta 1. Evidence for its role in abrogating the effect of a T cell cytokine. J Immunol. 1994;153(12):5730–9. [PubMed] [Google Scholar]
- 50.Schmitz H, Fromm M, Bentzel CJ, et al. Tumor necrosis factor-alpha (TNFalpha) regulates the epithelial barrier in the human intestinal cell line HT-29/B6. Journal of Cell Science. 1999;112(Pt 1):137–46. doi: 10.1242/jcs.112.1.137. [DOI] [PubMed] [Google Scholar]
- 51.Yang H, Fan Y, Teitelbaum DH. Intraepithelial lymphocyte-derived interferon-gamma evokes enterocyte apoptosis with parenteral nutrition in mice. Am J Physiol Gastrointest Liver Physiol. 2003;284(4):G629–37. doi: 10.1152/ajpgi.00290.2002. [DOI] [PubMed] [Google Scholar]
- 52.Yang H, Teitelbaum DH. Intraepithelial lymphocyte-derived interferon-gamma evokes enterocyte apoptosis with parenteral nutrition in mice. Am J Physiol Gastrointest Liver Physiol. 2003;284:G629–G637. doi: 10.1152/ajpgi.00290.2002. [DOI] [PubMed] [Google Scholar]
- 53.Yang H, Spencer A, Teitelbaum DH. Interleukin-7 administration alters intestinal intraepithelial lymphocyte phenotype and function in vivo. Cytokine. 2005 doi: 10.1016/j.cyto.2005.06.014. e-published ahead of print. [DOI] [PubMed] [Google Scholar]
- 54.Yang H, Sun X, Haxhija EQ, Teitelbaum DH. Intestinal epithelial cell-derived interleukin-7: A mechanism for the alteration of intraepithelial lymphocytes in a mouse model of total parenteral nutrition. Am J Physiol Gastrointest Liver Physiol. 2007;292(1):G84–91. doi: 10.1152/ajpgi.00192.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun X, Yang H, Nose K, et al. Decline in Intestinal Mucosal IL-10 Expression and Decreased Intestinal Barrier Function in a Mouse Model of Total Parenteral Nutrition. Amer J Physiol Gastrointestinal and Liver Physiology. 2007 doi: 10.1152/ajpgi.00386.2007. E-pub in advance. [DOI] [PubMed] [Google Scholar]
- 56.Wang F, Schwarz B, Graham W, et al. IFN-gamma-induced TNFR2 expression is required for TNF-dependent intestinal epithelial barrier dysfunction. Gastroenterology. 2006;131(4):1153–63. doi: 10.1053/j.gastro.2006.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Turner JR. Molecular Basis of Epithelial Barrier Regulation From Basic Mechanisms to Clinical Application. Am J Pathol. 2005;169(6):1901–1909. doi: 10.2353/ajpath.2006.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zeissig S, Bojarski C, Buergel N, et al. Downregulation of epithelial apoptosis and barrier repair in active Crohn's disease by tumour necrosis factor alpha antibody treatment. Gut. 2004;53(9):1295–302. doi: 10.1136/gut.2003.036632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boismenu R, Havran WL. Modulation of epithelial cell growth by intraepithelial gamma delta T cells. Science. 1994;266(5188):1253–5. doi: 10.1126/science.7973709. [DOI] [PubMed] [Google Scholar]
- 60.Yang H, Antony PA, Wildhaber BE, Teitelbaum DH. Intestinal intraepithelial lymphocyte gammadelta-T cell-derived keratinocyte growth factor modulates epithelial growth in the mouse. J Immunol. 2004;172(7):4151–8. doi: 10.4049/jimmunol.172.7.4151. [DOI] [PubMed] [Google Scholar]
- 61.Yang H, Wildhaber B, Tazuke Y, Teitelbaum DH. 2002 Harry M. Vars Research Award. Keratinocyte growth factor stimulates the recovery of epithelial structure and function in a mouse model of total parenteral nutrition. JPEN J Parenter Enteral Nutr 2002. 2002;26(6):333–40. doi: 10.1177/0148607102026006333. discussion 340-1. [DOI] [PubMed] [Google Scholar]
- 62.Yang H, Wildhaber BE, Teitelbaum DH. 2003 Harry M. Vars Research Award. Keratinocyte growth factor improves epithelial function after massive small bowel resection. JPEN J Parenter Enteral Nutr. 2003;27(3):198–206. doi: 10.1177/0148607103027003198. discussion 206-7. [DOI] [PubMed] [Google Scholar]