Abstract
Purpose:
To test the hypothesis that keratoconus and pellucid patients who have glaucoma or are suspected of having glaucoma have lower corneal hysteresis (CH) and/or corneal resistance factor (CRF) measurements compared to controls.
Methods:
A prospective study at a tertiary eye center of keratoconus and pellucid patients with glaucoma or suspected of having glaucoma, and age-matched keratoconus and pellucid controls, was performed. After informed consent was obtained, corneal topography, ocular response analyzer measurements, pachymetry, intraocular pressure, A-scan measurements, Humphrey visual fields (VFs), and disc photos were done. Analyses compared cases to controls on primary (CH and CRF) and secondary variables. Disc photos and VFs were rated in a masked fashion.
Results:
The mean CH (8.2, SD=1.6, vs 8.3, SD=1.5) and CRF (7.3, SD=2.0, vs 6.9, SD=2.1) were low and did not differ significantly between 20 study patients (29 eyes) and 40 control patients (61 eyes), respectively. CH had a negative, significant correlation with maximum corneal curvature by topography (P < .002) and positive, significant correlation with central corneal thickness (P < .003). The mean cup-disc ratio was larger among cases than controls (0.54, SD=0.20, vs 0.38, SD=0.20; P = .003). VFs were suggestive of glaucoma more often among the study eyes than controls (11 of 29, 37.9%, vs 8 of 60, 13.3%; P =.019).
Conclusions:
CH was low in study and control patients and was correlated with severity of keratoconus/pellucid, but not with glaucoma/suspected glaucoma or control status. Evidence of glaucoma was more common in study eyes than controls, but was present in both.
INTRODUCTION
Keratoconus and pellucid marginal corneal degeneration (pellucid) are conditions typically associated with low normal intraocular pressure (IOP) and are not thought to be associated with glaucoma. However, in a large cornea referral practice with a special interest in the treatment of keratoconus, a number of patients have developed glaucomatous optic neuropathy or have been diagnosed as “glaucoma suspects,” despite having normal or minimally elevated IOPs. It is important that ophthalmologists be aware of this possible association so that keratoconus patients with abnormal or suspicious-appearing optic nerves get visual field (VF) testing and treatment for glaucoma when needed.
Patients with keratoconus and pellucid have corneal thinning and are usually myopic. As both of these findings are associated with glaucoma, pachymetry and axial length need to be measured and analyzed in any study investigating a possible association of ectatic disorders with glaucoma. Central corneal thinning is associated with undermeasurement of IOP by Goldmann applanation tonometry (GAT). Since the Ocular Hypertension Treatment Study (OHTS) results were published, it has been recognized that reduced central corneal thickness (CCT) is a risk factor for glaucoma in patients with ocular hypertension.1 Previous research of these ectatic disorders revealed that GAT was an average of 2 mm Hg lower than the IOP measured by Pascal dynamic contour tonometry (DCT) (Ziemer, Zurich, Switzerland), a finding that was statistically significant but not clinically significant.2 The problem in keratoconus is not primarily one of undermeasurement of IOP, as finger pressures are typically low. Central corneal thickness may relate to more fundamental properties affecting ocular biomechanical properties and the risk for glaucoma.
One hypothesis to account for the development of normal-tension glaucoma in patients with ectatic diseases is that abnormal scleral biomechanical properties are risk factors. It is known clinically that the sclera tends to collapse in these patients during penetrating keratoplasty, suggesting that the whole eye has altered mechanical properties. These biomechanical abnormalities may result in reduced support for the optic nerve at the level of the lamina cribrosa, increasing its susceptibility to glaucomatous damage. This finding may have relevance to understanding the pathogenesis of normal-tension glaucoma in other patients.
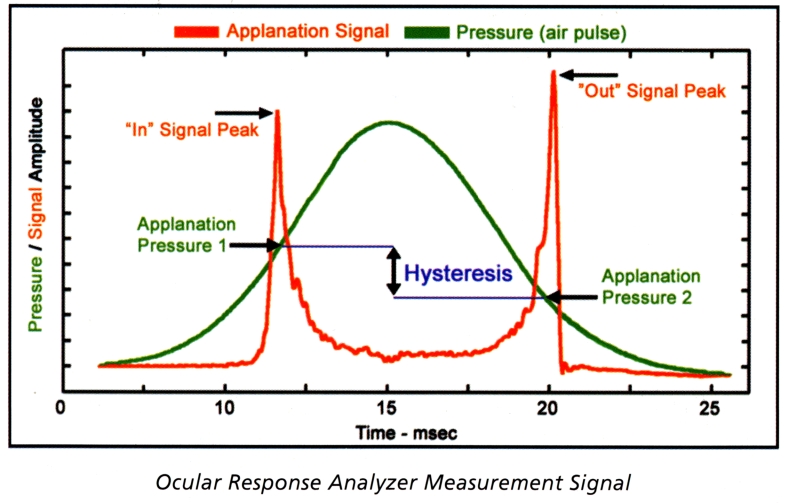
Recently, it has become possible to better measure ocular biomechanics noninvasively using the noncontact ocular response analyzer (ORA; Reichert, Buffalo, New York).3 Prior to the availability of this instrument, only measurements requiring mathematical calculations were possible in normal and keratoconic eyes.4–8 The ORA uses an air puff to cause inward, followed by outward, corneal movement. It provides two applanation measurements within 20 msec, one when the cornea is flat on the way in and the other on the way out (Figure). The difference between these pressures is the corneal hysteresis (CH), which is thought to reflect corneal viscoelasticity, a property related to corneal rigidity and thickness. In addition, a corneal resistance factor (CRF) is calculated by the instrument, which is thought to measure the elastic properties of the cornea. The IOPg is the average of the two pressure measurements, which is intended to correspond to GAT. An IOPcc is also reported, which is said to be compensated for corneal properties, such as thickness and hysteresis.
FIGURE.
Ocular response analyzer measurement signal.
The purpose of this study was to evaluate CH and CRF in keratoconus and pellucid patients who were diagnosed as having suspected or confirmed glaucoma and to compare them to age-matched keratoconus and pellucid control patients in order to test the hypothesis that low CH and/or CRF is associated with glaucomatous optic neuropathy. Previous studies have shown that keratoconus is associated with low CH compared to normal controls.9,10 However, a possible association between ectatic disorders and normal-tension glaucoma has not been previously reported. In addition, the association between CH and CRF and severity of ectatic disorders, as indicated by maximal corneal curvature and degree of central corneal thinning, was also explored.
CASE REPORT
A 66-year-old white man with keratoconus had undergone follow-up examinations on the Cornea Service since 1988. His IOPs as measured by GAT had ranged from 8 to 15 mm Hg in each eye. On repeated examinations with dilated pupils, the optic nerves were considered to appear healthy, although mild cup-disc (C/D) asymmetry was noted, with a slightly increased C/D ratio in the right eye of 0.55 vs 0.45 in the left eye in 2006. The patient was on the list of potential control patients for this study. However, on examination with dilated pupils prior to cataract surgery in the right eye in 2007, C/D ratios of 0.65 in the right eye and 0.40 in the left eye were noted. Glaucoma consultation was obtained. IOPs by GAT were 9 mm Hg OD and 8 mm Hg OS. C/D ratios as measured by the glaucoma specialist were 0.85 vertical and 0.70 horizontal in the right eye and 0.70 vertical with superior thinning and 0.55 horizontal in the left eye. Humphrey VF testing using the central 24-2 and Swedish Interactive Thresholding Algorithm (SITA) standard strategy was performed. VF testing had good reliability with findings of generalized field depression in each eye and an inferior arcuate scotoma in the left eye. A diagnosis of primary open-angle glaucoma, greater in the left than the right eye, was made as a result of the superior thinning of the optic nerve rim in the left eye and associated inferior field loss in the left eye, despite the larger C/D ratio in the right eye. Since the patient had a history of asthma and was to undergo cataract surgery, brimonidine ophthalmic solution 0.15%, one drop twice daily in each eye, was begun. When the patient developed an allergy to it after 7 months, therapy was switched to latanoprost.
METHODS
Institutional Review Board (IRB) approval was obtained from the Wills Eye Institute IRB for the study protocol. Study patients included patients with keratoconus and pellucid marginal degeneration who were diagnosed as having glaucoma or suspected of having glaucoma. Keratoconus and pellucid were diagnosed by a cornea specialist by slit-lamp biomicroscopy findings of localized corneal thinning and ectasia and confirmed by corneal topography. In keratoconus the location of maximal thinning and ectasia coincided, whereas in pellucid the location of the maximal thinning was inferior, or peripheral, to the area of maximal ectasia. Criteria for suspected glaucoma included maximum IOP by GAT of greater than or equal to 22 mm Hg or suspicious-appearing optic nerves with C/D ratios of greater than or equal to 0.65, or C/D asymmetry. Glaucoma was diagnosed by glaucoma specialists on the basis of typical optic nerve abnormalities, with or without corresponding Humphrey VF defects. Control patients had maximum Goldmann IOP of less than 22 mm Hg and normal-appearing optic nerves on routine examinations with dilated pupils with C/D ratios of less than or equal to 0.6. Control patients were age-matched to study patients. The goal was 2 control patients per study patient. Exclusion criteria for both study and control patients consisted of prior ocular surgery, including corneal transplantation, laser phototherapeutic keratectomy, and trabeculectomy, or a history of hydrops.
Potential study patients were identified by a computer search of all keratoconus and pellucid patients examined during 2006 with a second diagnosis of suspected glaucoma or primary open-angle glaucoma. Potential control patients were identified through a computer search of keratoconus and pellucid patients examined in 2006, which included 446 patients aged 35 or older. Most study and control patients were invited to participate during a routine office visit, given an informed consent to read, and asked to return for a study visit on another day. Four potential study patients identified by the computer search who were not seen for routine follow-up care during the first 6 months of the study were sent a letter inviting them to participate and a copy of the informed consent to review and were asked to contact the principal investigator.
At the study visit the IRB-approved informed consent was signed and the IRB-approved study protocol was completed. The number of eligible eyes was determined, and the reason, if any, for exclusion of one eye was recorded. Demographic information recorded included the date of birth, sex, race, height, and weight. Patients were asked about a history of sleep apnea. The number of years since the diagnosis of keratoconus or pellucid and of glaucoma or suspected glaucoma was noted. The maximum IOP (Tmax) by GAT and year it occurred were recorded for each eye. Current ocular medications were listed. An allergy history was obtained, including seasonal and perennial allergies, asthma, eczema, and drug allergies. Snellen visual acuity was measured, and the method of correction was specified. Slit-lamp biomicroscopy was performed. Blepharitis, floppy eyelids, papillary reaction of the superior tarsus (graded 1 to 4), location of the cone, and scarring, if present, were recorded.
Tests were performed in the same order. Corneal topography (Humphrey Atlas Topography system; Carl Zeiss Meditec Inc, Dublin California) was performed, and the maximum curvature, as determined by inspection of topography, was recorded. ORA readings were obtained, and CH, IOPcc, IOPg, and CRF were recorded. The principal investigator tried to obtain 3 ORA measurements per eye with a consistent wave pattern, but sometimes fewer consistent measurements were possible with a maximum of 6 readings per eye. Topical anesthetic drops were then instilled, and ultrasound measurement of CCT was performed (Accutome ultrasonic pachymeter; Accutome Inc, Malvern, Pennsylvania). Three readings per eye were averaged. Central TonoPen (T tono) (TonoPen XL; Mentor, Jacksonville, Florida) IOP measurements were done. Goldmann applanation tonometry was performed. The dial was twisted without the examiner looking, and then the GAT was measured. Patients who wore contact lenses reinserted them prior to having Humphrey VF testing using the central 24-2 and SITA standard strategy. Lenses were then removed, and tropicamide 1% and phenylephrine 2.5% drops were instilled. Noncontact axial length measurements were determined (Innovative Imaging V3; Ellix Inc, Sacramento, California), including the anterior chamber depth. Stereo disc photographs were taken. In some cases contact lenses were reinserted to try to improve the quality of the disc photographs.
Study patients and control patients were compared with regard to age, duration of keratoconus or pellucid marginal degeneration, maximum IOP by GAT in the medical record prior to study visit, allergies, scarring and maximal curvature by corneal topography, and CCT. The primary outcome was the comparison of CH and CRF between cases and controls. Specific correlations among demographic and clinical variables were also examined.
The stereo disc photographs and Humphrey VFs were analyzed by one glaucoma specialist masked as to whether the tests were from study or control patients. The quality of the disc photographs was rated good, fair, or poor on the basis of the reliability of the determination of the neuroretinal rim margin. Disc photographs were judged as to whether or not quality was adequate to diagnose glaucoma. The presence of a notch, peripapillary changes, disc hemorrhage, and/or anomalous tilt of the optic nerve in the disc photos was recorded and analyzed. Visual fields were considered reliable if false negatives and false positives were less than 25%. Evidence of glaucoma included the presence of a definite notch due to focal thinning, or an increased C/D ratio of 0.8 relative to the size of the optic nerve, or a typical pattern of glaucomatous loss on VF testing. Evidence of glaucoma by disc photos was graded in 2 ways: 2 categories of yes/no and 3 categories of yes/no/maybe. Evidence of glaucoma on VFs was similarly graded yes/no and yes/no/maybe. The diagnosis of glaucoma was based on clinical judgment of a combination of the disc photos and visual fields.
Statistical analyses compared cases vs controls on the primary end points of CH and CRF. The normality of the data was tested before using parametric statistical tests. A generalized estimating equations (GEE) approach to linear models using SAS PROC GENMOD was used to account for correlated measures between eyes for bilateral patients for continuous measures (such as CH).11 Conditional logistic regression determined by the Hosmer-Lemeshow method for paired data was used for the analysis of nominal variables such as scarring and sleep apnea.12 In addition, systemic variables (sleep apnea and floppy eyelids) were analyzed on a “per patient” basis. Finally, correlation analysis was used to look at the relationships among primary and secondary variables.
Secondary analyses were performed using a series of multivariable modes testing the difference in CH between cases and controls, controlling for potential moderating variables (candidate variables were analyzed one at a time).
The masked ratings of the disc photos and visual fields of study cases vs controls were analyzed for statistically significant differences using the GEE model for C/D ratio and conditional regression for nominal variables.
RESULTS
Twenty study patients and 40 age-matched controls completed the study (Tables 1A, 1B, 2A, and 2B). One control patient developed a small abrasion after ultrasound pachymetry, did not complete the study, and was replaced by another control. The age of most controls (32 of 40, 80%) was within 3 years of the study patient, but 5 controls were within 4 years of the study patient, and 3 were within 5 years of the study patient (Table 1A and 2A). There were 9 female and 11 male study patients, and 20 female and 20 male control patients. Three study patients and one control patient had pellucid and the remainder had keratoconus. Four study patients had a diagnosis of glaucoma associated with VF loss typical of glaucomatous optic neuropathy. The remaining 16 study patients were suspected of having glaucoma on the basis of suspicious-appearing optic nerves and/or borderline IOP. Twelve had an increased C/D ratio and normal IOPs, one had an increased C/D ratio and borderline IOP, one had borderline IOP and corticosteroid-induced glaucoma in the other eye, and 2 had borderline IOPs only. The diagnosis of suspected glaucoma was confirmed by a glaucoma specialist prior to the study in most patients (13 of 16, 81.2%). Three suspected of having glaucoma who were not evaluated by a glaucoma specialist had IOP by GAT of 22 mm Hg OU or C/D asymmetry of 0.3 and 0.15 with suspicious-appearing discs (1 case each). Nine study patients were receiving glaucoma medication, including 4 patients with glaucoma and 5 with suspected glaucoma. All were using topical medication, except for one receiving oral methazolamide because of corticosteroid-induced glaucoma in the other eye after penetrating keratoplasty.
TABLE 1A.
HISTORY OF STUDY PATIENTS
| NO. | DOB | EYE | SEX | RACE | HEIGHT (in.) | WEIGHT (lb) | SLEEP APNEA | KC/P | YEARS KC/P | YEARS GL/GL SUSP | TMAX (mm Hg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1942 | OD | M | C | 67 | 175 | No | KC | 32 | 9 gl | 16 |
| 2 | 1950 | OD | F | AA | 63 | 200 | No | KC | 2 | 2 gl susp | 16 |
| 4 | 1941 | OS | M | C | 67 | 198 | ND | KC | 44 | 0.1 gl | 15 |
| 5 | 1948 | OS | M | C | 70 | 270 | No | KC | 27 | 4 gl susp | 20 |
| 9 | 1951 | OD | M | C | 71 | 220 | Yes | P | 1.5 | 1.5 gl | 22 |
| OS | 23 | ||||||||||
| 10 | 1952 | OD | F | AA | 65 | 186 | ND | KC | 44 | 0.25 gl susp | 15 |
| OS | 17 | ||||||||||
| 17 | 1949 | OD | M | C | 74 | 205 | Snores | KC | 22 | 2 gl susp | 21 |
| OS | 19 | ||||||||||
| 21 | 1943 | OS | F | C | 61 | 129 | No | KC | 23 | 5 gl susp | 19 |
| 25 | 1956 | OS | M | C | 69 | 185 | No | P | 13 | 3 gl susp | 20 |
| 26 | 1947 | OS | M | C | 70 | 175 | No | KC | 37 | 8 gl susp | 18 |
| 27 | 1960 | OD | F | C | 65 | 275 | Yes | KC | 1 | 1 gl susp | 22 |
| OS | 22 | ||||||||||
| 28 | 1945 | OD | F | C | 67 | 150 | No | KC | 13 | 4 gl susp | 17 |
| OS | 16 | ||||||||||
| 32 | 1941 | OS | F | C | 65 | 120 | No | KC | 25 | 1 gl susp | 10 |
| 33 | 1950 | OD | M | C | 68 | 209 | Yes | P | 16 | 3 gl susp | 21 |
| OS | 21 | ||||||||||
| 39 | 1941 | OS | F | C | 61 | 190 | Snores | KC | 49 | 3 gl | 26 |
| 40 | 1948 | OS | M | AA | 77 | 320 | ND | KC | 19 | 2.5 gl susp | 16 |
| 42 | 1949 | OD | M | C | 70 | 200 | No | KC | 16 | 4 gl susp | 18 |
| OS | 22 | ||||||||||
| 43 | 1942 | OD | F | C | 63 | 128 | No | KC | 18 | 3 gl susp | 17 |
| OS | 17 | ||||||||||
| 50 | 1948 | OD | F | C | 64.5 | 135 | Snores | KC | 1 | 1 gl susp | 20 |
| OS | 20 | ||||||||||
| 52 | 1960 | OS | M | C | 69 | 190 | Yes | KC | 26 | 2.5 gl susp | 16 |
AA, African American; C, Caucasian; DOB, date of birth; KC, keratoconus; P, pellucid marginal degeneration; GL, glaucoma; GL SUSP, glaucoma suspected; ND, no data; Tmax, maximum intraocular pressure.
TABLE 1B.
RESULTS WITH STUDY PATIENTS
| NO. | VA/CORR | FLOPPY EYELIDS | SCAR | MAX TOPO K (D) | CH | IOPg | IOPcc | CRF | CCT (μm) | GAT (mm Hg) | T TONO (mm Hg) | AXIAL LENGTH (mm) | ACD (mm) | AL-ACD (mm) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 6/9 rgp | No | Yes | 63.5 | 7.1 | 8.4 | 13.4 | 5.5 | 368 | 11.5 | 12 | 24.36 | 3.45 | 20.91 |
| 2 | 6/12 hybrid | Yes | Yes | 53.0 | 6.3 | 10.6 | 16.1 | 5.5 | 439 | 14 | 14 | 24.75 | 3.59 | 21.16 |
| 4 | 6/7.5 rgp | Yes | Yes | 59.5 | 6.1 | 9.7 | 15.7 | 5.0 | 188 | 11 | 14 | 24.35 | 3.4 | 20.95 |
| 5 | 6/9 rgp | Yes | No | 52.0 | 6.7 | 8.2 | 13.7 | 5.1 | 475 | 12 | 12 | 24.40 | 3.64 | 20.76 |
| 9 | 6/9 hybrid | Yes | No | None | 8.2 | 11.8 | 15.2 | 8.2 | 596 | 17 | 12 | 26.78 | 3.88 | 22.90 |
| 6/9 rgp | Yes | No | 53.0 | 7.4 | 15.5 | 19.3 | 7.4 | 538 | 18 | 15 | 22.85 | 22.90 | 22.85 | |
| 10 | 6/18 rgp | N | Yes | 62.5 | 5.6 | 9 | 15.6 | 4.4 | ND | 10 | 15 | 27.47 | 4.84 | 22.63 |
| 6/12 rgp | N | Yes | 66.5 | 6.4 | 9.6 | 15.2 | 5.2 | 388 | 12 | 14 | 27.09 | 4.64 | 22.45 | |
| 17 | 6/18 rgp | N | Yes | 54.5 | 9.4 | 15.4 | 16.9 | 9.6 | 553 | 20 | 18 | 26.68 | 3.69 | 22.99 |
| 6/15 rgp | N | Yes | 53.0 | 8.1 | 10.1 | 13.8 | 6.9 | 552 | 19 | 13 | 26.64 | 3.78 | 22.86 | |
| 21 | 6/12 rgp | Y | Yes | 58.0 | 9.3 | 15.7 | 17.3 | 9.5 | 516 | 15 | 13 | 23.60 | 3.73 | 19.87 |
| 25 | 6/12 rgp | Y | No | 50.75 | 6.6 | 14.7 | 19.4 | 6.9 | 525 | 18 | 19.5 | 30.24 | 4.31 | 25.93 |
| 26 | 6/18 rgp | N | Yes | 55.0 | 9.8 | 14.2 | 15.6 | 9.5 | 499 | 10 | 16 | 25.56 | 4.24 | 22.32 |
| 27 | 6/6 gl | Yes | No | 45.0 | 13 | 15.2 | 13.3 | 12.2 | 553 | 12 | 11 | 23.23 | 3.57 | 19.66 |
| 6/12 gl | Yes | No | 52.0 | 7.3 | 11.7 | 16.0 | 6.7 | 523 | 16 | 11 | 23.49 | 3.76 | 19.73 | |
| 28 | 6/7.5 rgp | No | No | 50.0 | 9.4 | 7.5 | 10.1 | 7.2 | 444 | 10 | 14 | 25.15 | 3.35 | 21.80 |
| 6/7.5 rgp | No | No | 49.0 | 8.8 | 7.9 | 11.1 | 6.8 | 478 | 10 | 12 | 24.82 | 3.4 | 21.42 | |
| 32 | 6/18 rgp | Yes | Yes | 49.0 | 8.3 | 4 | 8.4 | 5.2 | None | 8 | None | 24.51 | 3.9 | 20.61 |
| 33 | 6/9 rgp | No | Yes | 48.0 | 8.3 | 9.5 | 13.1 | 6.8 | 595 | 12 | 16 | 24.69 | 4.02 | 20.67 |
| 6/18 rgp | No | No | 47.5 | 8 | 10.1 | 13.9 | 6.8 | 588 | 17.5 | 12 | 24.60 | 3.76 | 20.84 | |
| 39 | 6/18 rgp | No | Yes | 50.5 | 7.1 | 11.9 | 16.4 | 6.6 | 483 | 16 | 17 | 26.35 | 2.80 | 23.55 |
| 40 | 6/15 rgp | Yes | Yes | 51.0 | 8.1 | 8.3 | 12.3 | 6.3 | 595 | 10 | None | 28.06 | 4.05 | 24.01 |
| 42 | 6/12 rgp | No | Yes | 48.5 | 6.4 | 6.4 | 12.5 | 4.2 | None | 11 | 11 | 26.1 | 3.83 | 22.27 |
| 6/9 rgp | No | No | 46.5 | 8.7 | 15.4 | 17.5 | 9.0 | 540 | 14 | 12 | 26.50 | 3.9 | 22.60 | |
| 43 | 6/7.5 rgp | No | No | 52.5 | 8.5 | 11.5 | 14.6 | 7.5 | 492 | 13 | 6 | 23.18 | 3.49 | 19.69 |
| 6/7.5 rgp | No | No | 50.5 | 7.4 | 12.3 | 16.4 | 6.9 | 453 | 14 | 6 | 23.12 | 3.45 | 19.67 | |
| 50 | 6/9 rgp | No | No | 46.5 | 11 | 17.3 | 17.4 | 11.0 | 474 | 17 | 14 | 25.01 | 3.09 | 21.92 |
| 6/9 rgp | No | No | 46.5 | 9.1 | 14.3 | 16.3 | 9.0 | 461 | 16 | 12 | 24.63 | 3.02 | 21.61 | |
| 52 | 6/12 rgp | No | No | 48.5 | 10.7 | 11.1 | 11.9 | 9.4 | 523 | 12 | 11 | 25.96 | 3.78 | 22.18 |
ACD, anterior chamber depth; AL-ACD, axial length minus anterior chamber depth; CCT, central corneal thickness; CH, corneal hysteresis; CRF, corneal resistance factor; GAT, Goldmann applanation tonometry; IOP, intraocular pressure; IOPcc, cornea compensated IOP; IOPg, IOP correlated with Goldmann applanation tonometry (by ORA); MAX TOPO K, maximum curvature by corneal topography; ND, no data; rgp, rigid gas permeable lens; T TONO, tonometry by Tono-Pen.
TABLE 2A.
HISTORY OF CONTROL PATIENTS
| NO.* | DOB | EYE | SEX | RACE | HEIGHT (in.) | WEIGHT (lb) | SLEEP APNEA | KC/P | YEARS KC/P | Tmax (mm Hg) |
|---|---|---|---|---|---|---|---|---|---|---|
| 3 | 1957 | OD | M | C | 73 | 195 | No | KC | 10 | 18 |
| OS | 18 | |||||||||
| 6 | 1946 | OD | F | C | 65 | 196 | ND | KC | 12 | 15 |
| 7 | 1949 | OD | M | C | 71 | 185 | No | KC | 24 | 13 |
| OS | 14 | |||||||||
| 8 | 1965 | OD | F | C | 67 | 235 | No | KC | 1 | 12 |
| OS | 13 | |||||||||
| 13 | 1958 | OS | M | C | 73 | 172 | ND | KC | 19 | 16 |
| 12 | 1960 | OS | M | C | 70 | 170 | No | KC | 26 | 15 |
| 14 | 1967 | OD | F | C | 66 | 127 | No | KC | 3 | 11 |
| OS | 11 | |||||||||
| 15 | 1949 | OD | F | C | 62 | 149 | No | KC | 36 | 14 |
| 16 | 1943 | OD | M | C | 70 | 190 | No | KC | 20 | 16 |
| 18 | 1948 | OD | F | C | 67 | 136 | Snores | KC | 24 | 10 |
| OS | 12 | |||||||||
| 19 | 1956 | OD | M | C | 72.5 | 205 | Snores | KC | 22 | 16 |
| OS | 16 | |||||||||
| 20 | 1946 | OD | M | C | 68 | 250 | N | KC | 14 | 11 |
| OS | 11 | |||||||||
| 22 | 1942 | OD | M | C | 68 | 178 | N | P | 46 | 18 |
| OS | 16 | |||||||||
| 23 | 1942 | OD | M | C | 76 | 220 | Snores | KC | 34 | 12 |
| OS | 13 | |||||||||
| 24 | 1936 | OD | F | C | 65 | 120 | No | KC | 29 | 17 |
| OS | 12 | |||||||||
| 29 | 1956 | OD | F | C | 62 | 165 | Snores | KC | 27 | 21 |
| 30 | 1947 | OD | F | AA | 65.6 | 203 | Snores | KC | 38 | 18 |
| 35 | 1955 | OD | M | C | 72 | 195 | No | KC | 22 | 16 |
| OS | 16 | |||||||||
| 37 | 1949 | OD | F | C | 62.5 | 120 | N | KC | 32 | 20 |
| 41 | 1946 | OD | F | C | 63 | 230 | N | KC | 14 | 16 |
| OS | 16 | |||||||||
| 44 | 1949 | OD | F | C | 64 | 150 | N | KC | 26 | 18 |
| OS | 18 | |||||||||
| 45 | 1955 | OD | M | C | 70 | 205 | No | KC | 20 | 16 |
| OS | 16 | |||||||||
| 34 | 1956 | OD | M | C | 71 | 185 | No | KC | 7 | 14 |
| OS | 16 | |||||||||
| 46 | 1951 | OD | M | C | 67 | 180 | ND | KC | 4 | 19 |
| 47 | 1951 | OD | M | C | 72 | 200 | ND | KC | 31 | 15 |
| OS | 13 | |||||||||
| 51 | 1945 | OD | M | C | 66 | 180 | Snores | KC | 37 | 17 |
| OS | 16 | |||||||||
| 54 | 1947 | OD | F | C | 60 | 140 | ND | KC | 40 | 15 |
| OS | 16 | |||||||||
| 55 | 1946 | OD | F | C | 64 | 130 | No | KC | 30 | 15 |
| OS | 15 | |||||||||
| 56 | 1949 | OS | M | C | 73 | 259 | Yes | KC | 27 | 17 |
| 57 | 1944 | OD | M | C | 66 | 150 | Yes | KC | 36 | 12 |
| 58 | 1947 | OS | M | C | 71 | 216 | Snores | KC | 45 | 14 |
| 48 | 1948 | OD | F | C | 64 | 150 | Snores | KC | 44 | 13 |
| OS | 14 | |||||||||
| 36 | 1945 | OD | M | C | 69 | 201 | Snores | KC | 15 | 18 |
| OS | 20 | |||||||||
| 59 | 1947 | OD | F | C | 67 | 172 | No | KC | 10 | 11 |
| OS | 11 | |||||||||
| 61 | 1941 | OS | F | C | 64 | 205 | No | KC | 25 | 14 |
| 62 | 1946 | OS | F | C | 66 | 142 | No | KC | 40 | 14 |
| 64 | 1938 | OS | F | C | 64 | 112 | Snores | KC | 52 | 13 |
| 60 | 1951 | OS | M | C | 70 | 182 | Snores | KC | 30 | 16 |
| 65 | 1942 | OS | F | C | 65 | 220 | No | KC | 45 | 20 |
| 63 | 1937 | OD | F | AA | 64 | 185 | Yes | KC | 43 | 18 |
| 66 | 1951 | OS | F | C | 66 | 145 | No | KC | 24 | 20 |
AA, African American; C, Caucasian; DOB, date of birth; KC, keratoconus; ND, no data; P, pellucid marginal degeneration; Tmax, maximum intraocular pressure.
No case number assigned when study appointment scheduled; out of order when patient rescheduled.
TABLE 2B.
RESULTS WITH CONTROL PATIENTS
| NO.* | VA/CORR | FLOPPY EYELIDS | SCAR | MAX TOPO K (D) | CH | IOPg | IOPcc | CRF | CCT (μm) | GAT | T TONO (mm Hg) | AXIAL LENGTH (mm) | ACD (mm) | AL-ACD (mm) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | 6/9 rgp | No | No | 46.0 | 7.2 | 13.9 | 18.1 | 7.2 | 459 | 14 | 16 | 28.77 | 3.83 | 24.94 |
| 6/18 rgp | No | Yes | 60.5 | 9.1 | 8.4 | 11.2 | 7.2 | 13 | 15 | 29.81 | 4.12 | 25.69 | ||
| 6 | 6/30 rgp | Y | Yes | 78.0 | 9.6 | 13.9 | 15.4 | 9.3 | 592 | 13 | 15 | 25.77 | 4.17 | 21.6 |
| 7 | 6/9 hybrid | No | Yes | 51.0 | 7.9 | 4.3 | 9.1 | 4.9 | 216 | 10 | 8 | 27.54 | 3.64 | 23.9 |
| 6/9 rgp | No | No | 52.0 | 8.4 | 6.1 | 10.1 | 5.9 | 446 | 10 | 14 | 26.96 | 3.49 | 23.97 | |
| 8 | 6/12 gl | Yes | No | 48.5 | 8.7 | 11.4 | 14.3 | 7.7 | 484 | 8 | 8 | 24.25 | 3.73 | 20.52 |
| 6/18 gl | Yes | No | 53.0 | 7.0 | 7.0 | 13.1 | 5.3 | 468 | 8 | 6 | 24.13 | 3.54 | 20.59 | |
| 13 | 6/7.5 gl | No | No | 51.0 | 8.0 | 8.2 | 12.4 | 6.2 | 518 | 8 | 7 | 22.03 | 3.45 | 19.58 |
| 12 | 6/9 rgp | No | Yes | 52.0 | 6.2 | 6.4 | 12.7 | 4.1 | 444 | 10 | 11 | 24.90 | 4.02 | 20.88 |
| 14 | 6/7.5 scl | No | No | 46.5 | 8.9 | 10.9 | 13.7 | 7.8 | 533 | 10 | 10 | 24.58 | 3.59 | 20.99 |
| 6/7.5 scl | No | No | 46.5 | 8.6 | 10.0 | 13.2 | 7.2 | 535 | 10 | 11 | 24.30 | 3.59 | 20.71 | |
| 15 | 6/7.5 rgp | No | No | 57.0 | 8.3 | 10.5 | 14.0 | 7.1 | 405 | 12 | 14 | 24.45 | 3.93 | 20.52 |
| 16 | 6/9 rgp | Yes | No | 46.0 | 10.0 | 7.5 | 9.6 | 7.6 | 509 | 6 | 8 | 26.45 | 3.49 | 22.96 |
| 18 | 6/9 rgp | Yes | Yes | 60.0 | 8.3 | 2.9 | 7.4 | 4.8 | 477 | 6 | 4 | 23.78 | 3.4 | 20.38 |
| 6/9 rgp | Yes | No | 53.0 | 7.0 | 2.4 | 8.4 | 3.6 | 466 | 7 | 7 | 23.64 | 3.4 | 20.24 | |
| 19 | 6/7.5 hybrid | Yes | No | 57.0 | 7.4 | 6.4 | 11.4 | 5.1 | 506 | 7 | 9 | 24.88 | 4.17 | 20.71 |
| 6/7.5 hybrid | Yes | Yes | 56.0 | 6.8 | 4.5 | 10.4 | 4.1 | 424 | 7 | 9 | 25.45 | 4.5 | 20.95 | |
| 20 | 6/7.5 rgp | Yes | Yes | 52.0 | 6.0 | 9.4 | 15.5 | 4.8 | 486 | 10 | 14 | 25.88 | 3.73 | 22.15 |
| 6/9 rgp | Yes | Yes | 72.5 | 4.4 | 6.6 | 14.8 | 2.6 | 427 | 8 | 18 | 25.98 | 3.83 | 22.15 | |
| 22 | 6/9 rgp | Yes | No | 53.0 | 7.5 | 14.5 | 18.3 | 7.6 | 574 | 16 | 18 | 25.54 | 4.5 | 21.04 |
| 6/9 rgp | Yes | Yes | 51.0 | 5.2 | 16.8 | 22.7 | 6.4 | 560 | 16 | 16 | 25.28 | 4.45 | 20.83 | |
| 23 | 6/12 rgp | No | No | 58.0 | 7.4 | 7.5 | 12.3 | 5.4 | 469 | 12 | 11 | 24.59 | 3.4 | 21.19 |
| 6/15 sc (J1) | No | No | 47.0 | 6.8 | 8.4 | 13.7 | 5.2 | 511 | 12 | 13 | 24.43 | 3.49 | 20.94 | |
| 24 | 6/18 rgp | No | Yes | 59.0 | 10.3 | 3.5 | 5.8 | 6.7 | 439 | 8 | 9 | 23.77 | 3.18 | 20.59 |
| 6/21 rgp | No | No | 55.0 | 10.9 | 2.6 | 4.3 | 7.0 | 446 | 6 | 9 | 23.93 | 3.21 | 20.72 | |
| 29 | 6/7.5 gl | Yes | No | 47.5 | 10.4 | 15.1 | 15.6 | 10.3 | 475 | 14 | 16 | 25.52 | 3.76 | 21.76 |
| 30 | 6/18 rgp | No | Yes | >60.0 | 6.0 | 18.4 | 23.3 | 7.5 | 526 | 14 | 12 | 26.24 | 3.66 | 22.58 |
| 35 | 6/5 scl | No | No | 46.5 | 8.1 | 13.3 | 17.1 | 8.0 | 519 | 17 | 20 | 25.77 | 3.64 | 22.13 |
| 6/7.5 rgp | No | No | 55.0 | 6.8 | 8.1 | 13.5 | 5.2 | 464 | 16 | 18 | 25.87 | 3.73 | 22.14 | |
| 37 | 6/6 gl | No | Yes | 53.0 | 9.3 | 13.1 | 15.2 | 8.8 | 536 | 10 | 15 | 24.88 | 4.28 | 20.60 |
| 41 | 6/15 rgp | No | Yes | 61.5 | 9.5 | 15.0 | 16.5 | 9.5 | 538 | 14 | 11 | 25.0 | 4.12 | 20.88 |
| 6/12 rgp | No | No | 53.5 | 8.9 | 11.7 | 14.3 | 8.9 | 493 | 14 | 12 | 25.36 | 4.14 | 21.22 | |
| 44 | 6/9 rgp | No | Yes | 55.0 | 8.0 | 15.2 | 18.3 | 8.3 | 472 | 18 | 15 | 23.04 | 2.94 | 20.10 |
| 6/12 rgp | No | Yes | 53.5 | 9.2 | 12.6 | 14.8 | 8.5 | 465 | 14 | 12 | 22.89 | 3.06 | 19.83 | |
| 45 | 6/12 hybrid | No | Yes | 54.5 | 7.2 | 4.2 | 9.2 | 4.2 | 519 | 8 | 7 | 23.88 | 3.54 | 20.34 |
| 6/12 hybrid | No | Yes | 51.5 | 7.6 | 6.1 | 10.9 | 5.2 | 564 | 10 | 7 | 23.57 | 3.42 | 20.15 | |
| 34 | 6/6 rgp | Yes | No | 44.0 | 10.2 | 13.2 | 14.2 | 9.6 | 553 | 14 | 10 | 27.03 | 3.45 | 23.58 |
| 6/7.5 rgp | Yes | No | 44.5 | 10.2 | 12.4 | 13.5 | 9.4 | 548 | 14 | 11 | 27.59 | 3.54 | 24.05 | |
| 46 | 6/12 rgp | No | No | 50.5 | 7.9 | 10.9 | 14.5 | 6.9 | 489 | 15 | 13 | 24.84 | 3.66 | 21.18 |
| 47 | 6/12 rgp | No | No | 50.5 | 7.8 | 6.0 | 10.6 | 5.3 | 478 | 9 | 12 | 24.75 | 3.66 | 21.09 |
| 6/12 gp | No | Yes | 50.5 | 7.2 | 7.4 | 12.5 | 5.3 | 437 | 10 | 17 | 24.99 | 3.76 | 21.23 | |
| 51 | 6/9 rgp | No | Yes | 52.0 | 9.1 | 7.8 | 10.8 | 7.0 | 527 | 12 | 6 | 23.4 | 3.49 | 19.91 |
| 6/12 rgp | No | Y | 52.0 | 7.3 | 8.5 | 13.3 | 5.7 | 452 | 10 | 7 | 23.91 | 3.54 | 20.37 | |
| 54 | 6/15 rgp | No | Yes | 55.0 | 10.4 | 7.6 | 9.2 | 8.0 | 535 | 10 | 8 | 24.86 | 3.61 | 21.25 |
| 6/15 rgp | No | Yes | 55.0 | 9.4 | 9.4 | 11.8 | 7.7 | 527 | 11 | 11 | 24.87 | 3.69 | 21.28 | |
| 55 | 6/9 rgp | No | Yes | 52.0 | 7.2 | 6.5 | 11.7 | 5.0 | 416 | 10 | 9 | 25.87 | 3.61 | 22.26 |
| 6/7.5 rgp | No | No | 50.0 | 9.2 | 9.6 | 12.2 | 7.7 | 525 | 11 | 10 | 25.22 | 3.54 | 21.68 | |
| 56 | 6/7.5 rgp | Yes | No | 48.5 | 10.5 | 11.2 | 9.2 | 9.2 | 496 | 16 | 13 | 23.71 | 3.52 | 20.19 |
| 57 | 6/15 rgp | No | Yes | 64.0 | 6.1 | 4.0 | 10.8 | 3.3 | 481 | 14 | 8 | 26.87 | 4.36 | 22.51 |
| 58 | 6/12 rgp | Yes | Yes | 55.5 | 6.6 | 8.1 | 13.7 | 5.0 | 467 | 10 | 9 | 25.9 | 3.52 | 22.38 |
| 48 | 6/12 rgp | No | No | 55.0 | 9.0 | 12.4 | 14.9 | 8.3 | 519 | 14 | 12 | 28.23 | 3.97 | 24.26 |
| 6/15 rgp | No | No | 47.0 | 10.1 | 14.6 | 15.5 | 9.9 | 524 | 14 | 12 | 27.85 | 4.0 | 23.85 | |
| 36 | 6/9 rgp | No | No | 47.0 | 8.7 | 14.8 | 17.2 | 8.7 | 498 | 18 | 18 | 27.33 | 3.42 | 23.91 |
| 6/12 rgp | No | No | 48.25 | 8.5 | 12.8 | 15.9 | 7.9 | 471 | 20 | 18 | 26.96 | 3.4 | 23.55 | |
| 59 | 6/9 rgp | No | No | 48.0 | 9.7 | 13.3 | 14.9 | 9.1 | 520 | 12 | 14 | 25.23 | 3.85 | 21.38 |
| 6/9 rgp | No | No | 52.0 | 8.9 | 11.4 | 14.1 | 7.9 | 495 | 12 | 16 | 25.04 | 3.81 | 21.23 | |
| 61 | 6/12 rgp | No | No | 47.5 | 9.8 | 11.6 | 13.2 | 8.8 | 515 | 11 | 12 | 24.5 | 4.05 | 20.45 |
| 62 | 6/15 rgp | No | Yes | 66.0 | 7.1 | 6.0 | 11.4 | 4.7 | 446 | 12 | 10 | 23.2 | 3.57 | 19.63 |
| 64 | 6/12 rgp | No | Yes | 59.0 | 9.3 | 9.6 | 12.1 | 7.7 | 458 | 11 | 12 | 23.76 | 3.52 | 20.24 |
| 60 | 6/12 rgp | No | Yes | 60.5 | 5.5 | 8.6 | 15.3 | 4.2 | 456 | 13 | 13 | |||
| 65 | 6/12 rgp | N | No | 47.0 | 10.5 | 22.1 | 21.5 | 12.5 | 533 | 20 | 19 | 26.2 | 3.16 | 23.04 |
| 63 | 6/12 rgp | N | Yes | 60.5 | 10.7 | 12.6 | 13.2 | 9.8 | 525 | 12 | 19 | 24.35 | 4.02 | 20.33 |
| 66 | 6/9 rgp | N | No | 48.0 | 10.4 | 10.9 | 12.0 | 9.0 | 534 | 12 | 15 | 25.45 | 3.3 | 22.15 |
ACD, anterior chamber depth; AL-ACD, axial length minus anterior chamber depth; CCT, central corneal thickness; CH, corneal hysteresis; CRF, corneal resistance factor; GAT, Goldmann applanation tonometry; IOP, intraocular pressure; IOPcc, cornea compensated IOP; IOPg, IOP correlated with Goldmann applanation tonometry (by ORA); MAX TOPO K, maximum curvature by corneal topography; ND, no data; rgp, rigid gas permeable lens; scl, soft contact lens; T TONO, tonometry by Tono-Pen.
No case number assigned when study appointment scheduled; out of order when patient rescheduled.
The demographic variables were similar in both groups (Table 3). Specifically, there were no statistically significant differences between the groups for age, sex, years of keratoconus or pellucid, height, weight, or body mass index (BMI) (Table 2). The mean age was 59 years (range, 47–67 years) for study cases and 58.9 years (range, 42–72 years) for controls. The mean duration of keratoconus was 19.4 years for cases and 25.9 years for controls (P = .111). When data were analyzed separately for males and females, there was a significant difference between groups in years of keratoconus for females, with a mean of 17.7 years for female cases vs 27.9 years for female controls (P = .051, Table 3). Three study and two control patients were African American, and the rest of the patients were Causcasian. The mean BMI was 29.6 for the cases and 27.9 for the controls. Floppy eyelids were present in 7 of 20 study patients (35%) and 11 of 40 controls (27.5%). Sleep apnea had been diagnosed in 4 of 20 study patients (20%) and 3 of 40 controls (7.5%) (P = .171).
TABLE 3.
DEMOGRAPHIC CHARACTERISTICS AND BASELINE FUNCTION IN CASE AND CONTROL PATIENTS
| VARIABLE | CASES | CONTROLS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. eyes | 29 | 61 | |||||||||
| No. patients | 20 | 40 | |||||||||
| Males | 10 | 20 | |||||||||
| Females | 10 | 20 | |||||||||
| Males (N=10) | Mean | Median | SD | Min | Max | Mean | Median | SD | Min | Max | P<* |
| Age (yr) | 58.9 | 59.0 | 4.4 | 47.0 | 66.0 | 57.4 | 58.0 | 5.6 | 47.0 | 66.0 | .117 |
| Years of KC | 21.1 | 20.5 | 11.9 | 1.5 | 44.0 | 24.1 | 22.0 | 11.4 | 4.0 | 46.0 | .353 |
| Height (in.) | 70.4 | 70.0 | 2.9 | 67.0 | 77.0 | 70.5 | 71.0 | 2.6 | 66.0 | 76.0 | .948 |
| Weight (lb) | 214.0 | 205.0 | 38.2 | 175.0 | 329.0 | 197.4 | 195.0 | 23.6 | 150.0 | 259.0 | .212 |
| BMI (kg/m2) | 30.2 | 29.7 | 4.0 | 25.1 | 38.7 | 27.9 | 27.1 | 3.4 | 22.7 | 38.0 | .172 |
| Females (N=10) | Mean | Median | SD | Min | Max | Mean | Median | SD | Min | Max | P< |
| Age (yr) | 59.0 | 60.0 | 6.4 | 48.0 | 67.0 | 60.4 | 61.0 | 6.8 | 42.0 | 72.0 | .204 |
| Years of KC | 17.7 | 13.0 | 16.6 | 1.0 | 49.0 | 27.9 | 29.0 | 13.4 | 1.0 | 52.0 | .051 |
| Height (in.) | 64.5 | 65.0 | 2.2 | 61.0 | 69.0 | 64.4 | 64.0 | 2.0 | 60.0 | 67.0 | .853 |
| Weight (lb) | 171.5 | 150.0 | 50.0 | 120.0 | 275.0 | 164.4 | 150.0 | 38.8 | 112.0 | 235.0 | .898 |
| BMI (kg/m2) | 29.0 | 24.4 | 8.4 | 20.0 | 45.8 | 27.9 | 26.9 | 6.4 | 19.2 | 40.7 | .978 |
| All (N=20) | Mean | Median | SD | Min | Max | Mean | Median | SD | Min | Max | P< |
| Age (yr) | 59.0 | 59.0 | 5.4 | 47.0 | 67.0 | 58.9 | 60.0 | 6.3 | 42.0 | 72.0 | .406 |
| Years of KC | 19.4 | 18.0 | 14.4 | 1.0 | 49.0 | 25.9 | 26.0 | 12.5 | 1.0 | 52.0 | .111 |
| Height (in.) | 67.4 | 67.0 | 3.9 | 61.0 | 77.0 | 67.6 | 67.0 | 3.8 | 60.0 | 76.0 | .772 |
| Weight (lb) | 192.0 | 190.0 | 48.9 | 120.0 | 320.0 | 181.7 | 185.0 | 35.6 | 112.0 | 259.0 | .364 |
| BMI (kg/m2) | 29.6 | 28.7 | 6.6 | 20.0 | 45.8 | 27.9 | 27.1 | 5.0 | 19.2 | 40.7 | .352 |
BMI, body mass index; KC, keratoconus.
For interval variables, P values are from generalized estimating equations (GEE) regression for paired data using SAS PROC GENMOD. Hypothesis tests per patient.
There were a total of 29 eyes in 20 study cases and 61 eyes in 40 controls. Eleven study patients had one eye excluded because of a corneal transplant (8 eyes), no recordable ORA measurement (2 eyes), or suspected keratoconus, defined as a normal slit-lamp examination and abnormal topography consistent with keratoconus (1 eye). Nineteen control patients had one eye excluded because of a corneal transplant (11 eyes), a history of laser phototherapeutic keratectomy for nodular scar (2 eyes), no recordable ORA measurement (3 eyes), suspected keratoconus (1 eye), unilateral keratoconus (1 eye), or patient preference (1 eye). ORA measurements could not be obtained in 5 eyes, all with scarring and 4 with maximal curvature by topography greater than or equal to 59.5 D. Approximately half of the study eyes (14 of 29, 48.3%) and control eyes (29 of 61, 47.5%) had scarring due to keratoconus. One control patient was unable to wait to have VF, A-scan, and disc photos.
PRIMARY END POINT
The purpose of the present study was to test the hypothesis that low CH and/or CRF would be a significant risk factor for glaucoma or suspected glaucoma with normal IOP in patients with keratoconus and pellucid. As can be seen in Table 4, there was not a statistically significant difference between study cases and controls for measurements of CH (P = .734), with a mean for study cases of 8.2 (SD = 1.6) and a mean for controls of 8.3 (SD = 1.5). The mean difference was −0.15 (95% confidence interval [CI], −1.02 to 0.72). This represents a small effect size of 0.03.13 There was no significant difference between cases and controls on the measurement of CRF, 7.3 vs 6.9 for controls (P = .639). The mean difference was 0.29 (95% CI, −0.90 to 1.46), with a small effect size of 0.04. The lack of greater numbers of available study patients precluded a more highly powered study.
TABLE 4.
PRIMARY OUTCOME VARIABLES FOR CASE AND CONTROL PATIENTS
| INTERVAL VARIABLES | CASES (N=29) | CONTROLS (N=61) | P<* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MEAN | MEDIAN | SD | MIN | MAX | MEAN | MEDIAN | SD | MIN | MAX | ||
| CH | 8.2 | 8.1 | 1.6 | 5.6 | 12.6 | 8.3 | 8.3 | 1.5 | 4.4 | 10.9 | .734 |
| Tmax | 18.7 | 19.0 | 3.2 | 10.0 | 26.0 | 15.3 | 16.0 | 2.6 | 10.0 | 21.0 | <.0001 |
| Max topo K | 52.2 | 50.9 | 5.4 | 45.0 | 66.5 | 53.5 | 52.0 | 6.4 | 44.0 | 78.0 | .443 |
| IOPg | 11.3 | 11.1 | 3.3 | 4.0 | 17.3 | 9.8 | 9.4 | 4.1 | 2.4 | 22.1 | .175 |
| IOPcc | 14.8 | 15.2 | 2.6 | 8.4 | 19.4 | 13.3 | 13.3 | 3.6 | 4.3 | 23.3 | .047 |
| CRF | 7.3 | 6.9 | 2.0 | 4.2 | 12.2 | 6.9 | 7.2 | 2.1 | 2.6 | 12.5 | .639 |
| GAT | 13.7 | 13.0 | 3.2 | 8.0 | 20.0 | 11.8 | 12.0 | 3.4 | 6.0 | 20.0 | .102 |
| Pach | 493.8 | 507.5 | 86.6 | 188.0 | 596.0 | 488.7 | 491.0 | 54.9 | 216.0 | 592.0 | .848 |
| T tono | 13.1 | 13.0 | 3.0 | 6.0 | 19.5 | 12.1 | 12.0 | 3.9 | 4.0 | 20.0 | .332 |
| Axial length | 25.4 | 24.8 | 1.7 | 22.9 | 30.2 | 25.3 | 25.0 | 1.5 | 22.0 | 29.8 | .844 |
| ACD | 4.4 | 3.8 | 3.6 | 2.8 | 22.9 | 3.7 | 3.6 | 0.4 | 2.9 | 4.5 | .288 |
| AL-ACD | 21.8 | 21.8 | 1.5 | 19.7 | 25.9 | 21.6 | 21.2 | 1.4 | 19.6 | 25.7 | .712 |
| Papillae | 0.6 | 0.0 | 0.7 | 0.0 | 2.0 | 0.3 | 0.0 | 0.6 | 0.0 | 3.0 | .256 |
| Nominal variables | N | % | N | % | P<* | ||||||
| Floppy eyelids† | 7 | 35.0 | 11 | 27.5 | .829 | ||||||
| Scarring | 14 | 48.3 | 29 | 47.5 | .865 | ||||||
| Sleep apnea† | 4 | 21.1 | 3 | 8.1 | .171 | ||||||
ACD, anterior chamber depth; AL-ACD, axial length minus anterior chamber depth; CH, corneal hysteresis; CRF, corneal resistance factor; GAT, Goldmann applanation tonometry; IOP, intraocular pressure; IOPcc, cornea compensated IOP; IOPg, IOP correlated with Goldmann applanation tonometry (by ORA); Max Topo K, maximum curvature by corneal topography; Pach, pachymetry; T tono, tonometry by Tono-Pen; Tmax, maximum GAT in medical record;
*For interval variable P values are from generalized estimating equations (GEE regression) for paired data using SAS PROC.GENMOC. For nominal variable P values are from conditional logistic regression for paired data using SAS PROC LOGISTIC.
Hypothesis tests are per patient.
SECONDARY END POINTS
Cases and controls were also compared with regard to a number of secondary end points (Table 4). These included Tmax, as determined by retrospective chart review, maximum corneal curvature (K) by corneal topography, IOPg and IOPcc measured by ORA, GAT, T tono, CCT, axial length, and axial length minus anterior chamber depth, measured by A-scan. There were no significant differences between cases and controls except for measures of Tmax (P < .0001) and IOPcc (P = .047). For Tmax, the mean for cases was higher than that for controls: 18.7 mm Hg (SD = 3.2) vs 15.3 mm Hg (SD = 2.6). Measurements of IOPcc were also higher for cases relative to controls: 14.8 mm Hg (SD = 2.6) vs 13.3 mm Hg (SD = 3.6). The mean maximum K by topography was 52.2 (SD = 5.4) for the cases compared to 53.5 (SD = 6.4) for the controls (P = .443). The mean CCT was 493.8 μm for the cases compared to 488.7 μm for the controls (P = .848). The mean axial length and axial length minus anterior chamber depth were 25.5 mm and 21.8 mm, respectively, for the cases compared to 25.3 and 21.6, respectively, for the controls (P = .844, P = .712, respectively).
CORRELATION ANALYSIS
The relationship between CH measurements of both the study and control patients with age, duration of keratoconus, maximal K as determined by topography, and CCT was analyzed by Pearson correlation coefficients. Table 5 summarizes the correlation coefficient (and concomitant P value) for each pairwise comparison. Results showed that CH had a moderate negative correlation with maximum K by corneal topography (r = −0.33, P < .002) and a moderate positive correlation with pachymetry (r = 0.32, P < .003). These findings are consistent with CH decreasing in association with increasing keratoconus disease severity as measured by increased curvature and thinner corneas.
TABLE 5.
CORRELATIONS AMONG MEASURES
| VARIABLE | WITH | R* | P< |
|---|---|---|---|
| Corneal hysteresis | Age | 0.09 | .412 |
| Duration KC | −0.13 | .235 | |
| Max K topo | −.0.33 | .002 | |
| Pachymetry | 0.32 | .003 | |
| IOPg | GAT | 0.74 | <.001 |
| Pachymetry | 0.38 | <.001 | |
| IOPcc | GAT | 0.70 | <.001 |
| Pachymetry | 0.22 | .044 | |
| T tono | GAT | 0.57 | <.002 |
| GAT | Pachymetry | 0.29 | .006 |
IOPcc, corneal compensated intraocular pressure; IOPg, IOP correlated with GAT (by ORA); KC, keratoconus; Max K topo, maximum curvature by corneal topography; GAT, Goldmann applanation tonometry; T tono, tonometry by Tono-Pen.
Pearson correlation coefficients.
In addition, there was a strong positive correlation of IOPg measured by the ORA with GAT (r = 0.74, P < .001) as well as a moderate correlation of IOPg with pachymetry (r = 0.38, P < .001). Similarly, there was a strong positive correlation of IOPcc with GAT (r = 0.70, P < .001) as well as a modest correlation of IOPcc with pachymetry (r = 0.22, P = .044). There was also a moderate correlation of T tono with GAT (r = 0.57, P < .001) and a small correlation of GAT with pachymetry (r = 0.29).
A series of secondary analyses were also performed to determine whether or not there was a difference in CH between the study patients and controls after accounting for potential confounding variables such as disease severity, as indicated by maximum topographic K, CCT, and scarring. No significant confounding variables were found. Because of the small number of patients (4 cases) with a diagnosis of definite glaucoma, excluding those with suspected glaucoma, it was not possible to compare these patients with the controls.
Analysis of the results of the masked rating of the optic nerve photos of study and control patients indicated that the only significant difference was that the mean C/D ratio of the study cases was larger (0.54, SD = 0.20) than that of the controls (0.38, SD = 0.20) (P = .003; Tables 6A and 6B). The quality of the photos was poor in almost half of the study cases (13 of 29, 44.8%) and controls (28 of 59, 47.5%) due to corneal irregular astigmatism and scarring associated with keratoconus. In over half of the study cases (15 of 29, 51.7%) and controls (31 of 59, 52.5%), the quality of the disc photos was rated inadequate to diagnose glaucoma. (Disc photos were not rated in 2 eyes.) Over 70% of the discs were rated normal among both the study cases (16 of 22, 72.7%) and controls (39 of 49, 79.6%). (Discs were rated in as many eyes as possible, including some with poor-quality disc photos.)
TABLE 6A.
AGREEMENT WITH INDEPENDENT RATER CASE AND CONTROL PATIENTS
| CASES | CONTROLS | P< | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| PHOTO | |||||
| Photo quality | N=29 | N=59 | |||
| Good | 11 | 37.9 | 13 | 22.0 | 0.252 |
| Fair | 5 | 17.2 | 18 | 30.5 | |
| Poor | 13 | 44.8 | 28 | 47.5 | |
| Adequate to diagnose | N=29 | N=59 | |||
| Yes | 14 | 48.3 | 28 | 47.5 | 0.981 |
| No | 19 | 82.6 | 45 | 90.0 | |
| Glaucoma | N=23 | N=50 | |||
| Yes | 4 | 17.4 | 5 | 10.0 | 0.443 |
| No | 19 | 82.6 | 45 | 90.0 | |
| GSN | N=22 | N=49 | |||
| Normal | 16 | 72.7 | 39 | 79.6 | 0.306 |
| Suspect | 5 | 22.7 | 10 | 20.4 | |
| Glaucoma | 1 | 4.5 | 0 | 0.0 | |
| Notch | N=17 | N=39 | |||
| Yes | 2 | 11.8 | 3 | 7.7 | 0.385 |
| No | 15 | 88.2 | 36 | 92.3 | |
| PPP changes | N=24 | N=41 | |||
| Yes | 13 | 54.2 | 20 | 48.8 | 0.838 |
| No | 11 | 45.8 | 21 | 51.2 | |
| Disc Heme | N=20 | N=35 | |||
| Yes | 0 | 0.0 | 0 | 0.0 | N/A |
| No | 20 | 100.0 | 35 | 100.0 | |
| Anomalous | N=19 | N=41 | |||
| Yes | 0 | 0.0 | 6 | 14.6 | 0.995 |
| No | 19 | 100.0 | 35 | 85.4 | |
| Tilt | N=19 | N=38 | |||
| Yes | 8 | 42.1 | 4 | 10.5 | 0.259 |
| No | 11 | 57.9 | 34 | 89.5 | |
| Large | N=5 | N=6 | |||
| Yes | 5 | 100.0 | 6 | 100.0 | N/A |
| No | 0 | 0.0 | 0 | 0.0 | |
| Small | N=4 | N=16 | |||
| Yes | 4 | 100.0 | 16 | 100.0 | N/A |
| No | 0 | 0.0 | 0 | 0.0 | |
GSN, glaucoma/suspect/normal appearance of optic nerve; N/A, not applicable; Photo, disc photo; PPP, peripapillary.
TABLE 6B.
AGREEMENT WITH INDEPENDENT RATER CASE AND CONTROL PATIENTS*
| CASES† | CONTROLS‡ | P< | |||
|---|---|---|---|---|---|
| n | % | N | % | ||
| Cup-disc ratio | N=23 | N=51 | .003 | ||
| Mean | 0.54 | 0.38 | |||
| SD | 0.20 | 0.20 | |||
| Median | 0.55 | 0.30 | |||
| Min | 0.10 | 0.10 | |||
| Max | 0.80 | 0.85 | |||
| HVF | |||||
| Reliable (Y/N) | N=29 | N=60 | |||
| Yes | 29 | 100.0 | 60 | 100.0 | N/A |
| No | 0 | 0.0 | 0 | 0.0 | |
| Glaucoma (Y/N) | N=29 | N=60 | |||
| Yes | 3 | 10.3 | 4 | 6.7 | .612 |
| No | 26 | 89.7 | 56 | 93.3 | |
| GSN | N=29 | N=60 | |||
| Normal | 18 | 62.1 | 52 | 86.7 | .019 |
| Suspect | 10 | 34.5 | 7 | 11.7 | |
| Glaucoma | 1 | 3.4 | 1 | 1.7 | |
| Best guess glaucoma | N=29 | N=60 | |||
| Yes | 4 | 13.8 | 5 | 8.3 | .433 |
| No | 13 | 44.8 | 44 | 73.3 | |
| Any glaucoma (per eye) | N=29 | N=60 | |||
| Yes | 16 | 55.2 | 16 | 26.7 | .010 |
| No | 13 | 44.8 | 44 | 73.3 | |
| Any glaucoma (per patient) | N=20 | N=40 | |||
| Yes | 13 | 65.0 | 13 | 32.5 | .027 |
| No | 7 | 35.0 | 27 | 67.5 | |
GSN, glaucoma/suspect/normal appearance of optic nerve; HVF, Humphrey visual field; N/A, not applicable.
Analysis per patient (based on N=20 cases and N=40 controls).
From N=29 observations for cases (20 patients).
From N=60 observations for controls (40 patients).
Analysis of the results of the masked rating of the VFs of the study and control patients showed that the fields were reliable in all patients (Table 6B). Study cases were significantly more likely than controls to be suggestive of glaucoma (10 of 29, 34.5% of cases; 7 of 60, 11.7% of controls; P = .019). Taking into account both the disc photos and fields, study cases, analyzed by eye and patient, were significantly more likely than controls to have any evidence of glaucoma, (P = .10 per eye, P = .027 per patient).
Nine eyes were judged by overall impression to have glaucoma, including 2 study eyes (2 patients) with the clinical diagnosis of glaucoma, 2 study eyes (1 patient) suspected of having glaucoma, and 5 control eyes (5 patients). The 9 eyes in 8 patients with evidence of glaucoma were compared to the other eyes and patients and found to have significantly longer duration of keratoconus (mean, 36.8 years vs 22.5 years, P < .001), steeper corneas (mean maximum K by topography 60.2 D vs 52.3 D, P < .001), and more scarring (P = .01). Mean CH was similar (7.5 vs 8.3, P = .237).
The masked reader of the discs and fields reviewed the results of the 5 control eyes and recommended that the patients be contacted for examination, with pupil dilation, of the optic nerves and VF testing. Evidence of possible glaucoma was found in 3 eyes of 2 control patients on VFs on repeated testing, confirming the masked evaluation of 2 eyes, and adding concern about the second eye of one patient. Repeated VFs and glaucoma consultations have been requested in all these control patients. The data was reanalyzed 2 ways: first, by removing the controls with possible evidence of glaucoma, and second, by adding them to the study cases. The results did not change, and CH and CRF did not differ significantly between the controls (first reanalysis, CH 8.3, CRF 6.8; second reanalysis, CH 8.3, CRF 6.8) and the study patients (first reanalysis, CH 8.1, CRF 7.3; second reanalysis, CH 8.2, CRF 7.3). P values were as follows: CH, P = .746; CRF, P = .517 (controls removed), and CH, P = .970; CRF, P = .498 (controls added to study cases).
DISCUSSION
Normal-tension glaucoma has developed in keratoconus and pellucid patients who have been followed for many years. In other keratoconus patients, glaucoma is suspected, more often because of suspicious-appearing optic nerves than borderline IOP. This is notable given an expected prevalence of open-angle glaucoma of 1% in the adult population in the United States, with only 20% of them expected to have low-tension glaucoma. Keratoconus occurs in 1 in 200 of the population (0.5%). It is important to be aware of this possible association between keratoconus and normal-tension glaucoma, since keratoconus patients usually have low normal IOP and are thought to be at lower than average risk for glaucoma. In the chart review of both the study patients and controls, it was noted that frequently finger pressures were done because patients were wearing contact lenses, and since the eyes were soft, quantitative IOP pressure measurements were often not done. Evaluation of the optic nerve in keratoconus patients is challenging because of irregular astigmatism and scarring, which limit the view. Suspicious-appearing nerves may be considered physiologic due to myopia in the setting of low IOPs. Our experience suggests that suspicious-appearing nerves require follow-up with VF testing, which should be repeated regularly, even if initially normal.
Both keratoconus and pellucid patients were included in this study because these are very closely related ectactic diseases. Corneal topography is similar in low sagging cones and pellucid, with both having a butterfly pattern of steepening at 4-and 8-o’clock positions. Pellucid has more peripheral inferior corneal thinning, with less decrease in CCT, compared to keratoconus. The altered biomechanical properties associated with both keratoconus and pellucid are not limited to decreased CCT.
The results of this study do not support the hypothesis that the keratoconus study patients who are suspected of having glaucoma or who have glaucoma would have lower CH and/or CRF than the control patients, as both groups had similar low mean measurements of 8.2 and 8.2 for CH and 7.3 and 6.9 for CRF for the cases and controls, respectively. Although the power of the study was limited because of the number of patients, given the similar findings in the two groups, it is unlikely that a larger study would have obtained different results. If low CH proves to be a risk factor for glaucoma, then all keratoconus and pellucid patients should be considered at increased risk for glaucoma. The limited quality of disc photos due to corneal disease makes the diagnosis of glaucoma prior to visual field loss especially difficult in this patient population. The diagnosis of glaucoma in the masked evaluation of disc photos and visual fields in both study and control patients suggests that glaucoma is being missed in these patients. Despite a high index of suspicion in this practice setting, some of the eyes (5 of 60, 8.3%) considered to have glaucoma were controls.
Corneal hysteresis was correlated with keratoconus disease severity in both the study and control patients as indicated by moderate negative correlation with maximum K by corneal topography and positive correlation with CCT, meaning the CH decreases with increasing corneal steepening and thinning. Longitudinal studies would be necessary to determine cause and effect and whether or not keratoconus patients with lower CH are more likely to have progressive keratoconus or if CH decreases along with advancing disease.
The mean Tmax by GAT was significantly higher, 18.7 mm Hg for the study patients compared to 15.3 mm Hg for the controls. Both average measurements are within normal limits but are higher than the usual IOPs of 12 mm Hg recorded in keratoconus patients, who are also generally younger (David Varssanno, unpublished data). Study and control patients had similar keratoconus disease severity, as indicated by mean maximal corneal K and corneal thinning. They also were similarly myopic, as indicated by axial length measurements with and without taking into account anterior chamber depth.
Study cases and control patients were similarly overweight with average BMI of 29.6 and 27.9, respectively. A nonsignificant increased percentage of study patients (21%) vs controls (8.1%) had a diagnosis of sleep apnea (P = .171). Sleep apnea may be underdiagnosed, as a number of study and control patients have not been formally evaluated despite a history of snoring.
Analysis of IOP measurements by various instruments determined that the IOPg by the ORA was strongly correlated with GAT, as expected, and moderately correlated with CCT. IOPcc was also strongly correlated with GAT, but only modestly correlated with CCT. IOPcc is intended to be less affected by CCT than IOPg. In this study, there was only a small correlation between GAT and CCT, which is not surprising given the additional influence of altered corneal biomechanics in keratoconus. The modest or small correlation of IOPcc and GAT with CCT suggests that corneal thinning did not have a large effect on IOP measurement. The recent Meiktila Eye Study of CCT and IOP in a nonglaucomatous Asian population14 showed that CCT was significantly, but weakly, associated with IOP, with an increase of 100 μm in CCT predicting an increase in IOP of only 1.3 mm Hg. This is of interest, since patients in the current study had thinner corneas than seen in people without corneal disease, and confirms the limited role of CCT in IOP undermeasurement. However, results in an Asian population14 may be different from ours, and glaucoma specialists think that low CCT and IOP underestimation are correlated.
Our study population is different from typical keratoconus patients in that our patients were older, with study cases averaging 59 years old and age-matched controls 58.9 years old, and had long-standing disease (mean, 19.4 years for cases and 25.9 years for controls). Keratoconus is thought of as a disease of young adults. However, in a practice with a special interest in all aspects of medical and surgical management of keratoconus, 40% of patients are 50 years old or older (unpublished data). The possible association of keratoconus with normal-tension glaucoma that we have observed would be less evident in practices treating only young keratoconus patients, because of the later onset of glaucoma.
Evaluation of the disc photos determined that they were of inadequate quality to diagnose glaucoma in over half the study cases (51.7%) and controls (52.5%). Although the average C/D ratio was greater among study cases (0.54) than controls (0.38) (P = .003), most nerve heads appeared normal. Disc photos are the standard way to evaluate optic nerves when glaucoma is suspected or present, but have limited usefulness in patients with keratoconus or pellucid. Clinical examination of the disc is possible, although difficult, in cases with poor-quality photos, since the examiner can try to look around the area of maximal corneal pathology. Devices used to evaluate the optic nerve depend on the clarity of the media, which is reduced in these patients. We have found it even more challenging to obtain good-quality optical coherence tomography and Heidelberg retinal tomography images in these patients. Since changes in the disc precede visual field changes in glaucoma, difficulty in evaluating the disc makes the early diagnosis of glaucoma prior to visual field changes problematic in this patient population. A low threshold for obtaining glaucoma consultations in keratoconus and pellucid patients is necessary, since glaucoma specialists are more used to evaluating the optic nerve under difficult circumstances.
Visual fields were reliable in all patients and were suggestive of glaucoma more frequently among study cases than controls (P = .019). One should have a low threshold for obtaining VFs in this patient population.
It is of considerable interest and concern that 8.3% of control eyes (5 of 60) were judged to have glaucoma by the overall impression of the independent rater. Additional examination of these patients showed evidence of glaucoma in 3 eyes on the basis of the VFs. This suggests that normal-tension glaucoma may be even more common than appreciated in keratoconus and pellucid patients. Corneal thinning and low corneal hysteresis may be risk factors for normal-tension glaucoma not only in these patients, but perhaps in other patients as well. Further study of these parameters in patients with normal-tension glaucoma without keratoconus or pellucid could be worthwhile in elucidating the importance of biomechanical properties in normal-tension glaucoma in general.
Keratoconus is associated with localized corneal thinning, and corneal thinning is recognized as a risk factor for glaucoma progression. Patients in this study had corneal thinning with a mean CCT of 493 μm among the study patients and 489 μm in the controls. However, pellucid is associated with inferior corneal thinning, and the average CCT in the 5 eyes of 3 pellucid study patients, including one with definite glaucoma, was 568 μm (range, 525–596 μm). The OHTS determined that thin CCT was a significant risk for the progression from ocular hypertension to primary open-angle glaucoma with CCTs less than 555 μm associated with a 3-fold increased risk compared to CCTs greater than 588 μm.1 In addition, CCT less than 545 μm in patients with preperimetric (without visual field loss) glaucomatous optic neuropathy is associated with the development of visual field abnormalities.15
The relationship between corneal thinning and glaucoma is not fully understood. There is strong evidence that CCT measurement should be included in the examination of patients with ocular hypertension.16 GAT determination assumes a CCT of 520 μm. With a thinner cornea, less force is needed to flatten the (central 3.06 mm) cornea, so a falsely lower IOP may result. Correcting IOP measurements for CCT cannot be done with a simple linear correction.17 Measurements of IOP considered less influenced by corneal thickness, including use of the Pascal DCT in previous studies2 and the Reichert ORA IOPcc in this study, have yielded IOP measurements averaging 1 to 2 mm Hg higher in keratoconus patients. In addition, finger pressures are low in keratoconus. Undermeasurement of IOP due to corneal thinning does not appear to be the key clinical issue in keratoconus patients. They appear to be susceptible to glaucomatous optic nerve damage at normal pressures.
It is also recognized that the association of thin corneas with glaucoma may not be through the effect on IOP measurement, but rather that CCT may be a surrogate for increased susceptibility to optic nerve damage.18 It is thought that CCT may be related to biomechanical properties of the lamina cribrosa, which affect the optic nerve.19 It is likely that altered biomechanical properties in keratoconus are important in its apparent association with normal-tension glaucoma, and understanding this may be relevant to normal-tension glaucoma in patients without keratoconus.
The ORA is a relatively new instrument that enables one to study biomechanical properties of the eye. The ORA uses an air jet, similar to a noncontact tonometer, to generate a force on the cornea. The air pulse causes the cornea to move inward past a first applanation (flattening), P1, into a concave shape, and then within milliseconds the air pulse turns off and the pressure decreases symmetrically (Figure). The maximum air pressure varies depending on P1. The cornea passes through a second applanation, P2, while returning to its normal convex curvature. An electro-optical detector monitors the shape of the central 3.0 mm of the cornea during the 20-msec measurement and detects applanation. Two applanation times correspond to 2 peaks when the light reflection is maximal produced by the inward and outward applanations. Two pressures are at the intersection of a vertical line through the peak of the applanation curve and the pressure curve. The 2 pressures are different owing to viscoelastic properties of the cornea. The difference of the 2 pressures is corneal hysteresis (CH). The average of the 2 pressures is IOPg, which is correlated with Goldmann tonometry.3 IOPcc is a corneal-compensated IOP obtained from the difference of the 2 pressures (P1-kP2) where k is a constant (0.43) determined by Reichert, the manufacturer of ORA.17 It is intended to be independent of CCT and corneal curvature. A corneal resistance factor (CRF) is also generated by the ORA. It is also derived from the difference of P1 and P2 (P1-kP2), where k takes into account the relationship of P1, P2, and CCT. It is intended to be more strongly associated with CCT than CH is. CRF is intended to be a measurement of corneal resistance that is relatively unaffected by IOP changes.20
Corneal hysteresis is a measurement of corneal viscoelasticity, a biomechanical property. In elastic materials, such as springs, the strain, or deformation (change in length), is directly proportional to the stress, or force, applied and is independent of the duration or speed of the force applied.21 Viscosity describes the tendency of liquids to resist flow so that after deformation by stress, they do not regain their original shape.19 High-viscosity materials, likened to shock absorbers, move slowly in response to stress, and low-viscosity materials move quickly. Viscoelastic materials have both properties. They recover their original shape after the stress is removed, but the relaxation path is different than the deformation path. This is called hysteresis, and it is due to dissipation of energy in the material as heat.19 Corneal hysteresis is thought to measure viscosity or viscoelasticity, and CRF is thought to measure elastic properties, but there is some uncertainty about this.22 Low CH indicates less viscous dampening by the cornea.
In 2005, Liu and Roberts23 used a mathematical model of the cornea to determine the influence of corneal thickness, curvature, and biomechanics on GAT. The model predicted that variations in corneal elasticity would have a much greater impact on IOP readings (17.26 mm Hg) compared to CCT (2.87 mm Hg for CCT 443–629 μm) and curvature (1.76 mm Hg for radius of curvature 7.0–8.6 mm). In addition, elasticity affected the impact of CCT, so that an increase in stiffness (decrease in elasticity) increased the effect of CCT on IOP. Their study looked forward to the possibility of measuring corneal biomechanical properties in vivo with the availability of new instruments including the ORA. At the Ocular Biomechanics Symposium at the Association for Research in Vision and Ophthalmology (ARVO) meeting in April 2008, the marked increased importance of elasticity over CCT and curvature in IOP measurement error was considered accurate (C.J. Roberts, ARVO Meeting, 2008, Symposium).
Since the ORA is a relatively new instrument, available since 2005, only beginning in 2006 have a number of studies been published about its use for various purposes.20 Medieros and Weinreb17 evaluated the influence of CCT, corneal curvature, and axial length on IOP measurements by GAT and ORA. They found that GAT was significantly associated with CCT and corneal curvature, but not axial length, and that IOPcc was not affected by any of these measurements. It is worth noting that more force is necessary to flatten a steeper cornea, and therefore the GAT is higher in steeper corneas.23 On the basis of this, higher GAT would be expected in keratoconus patients because of corneal steepening, which is not the case. In a mathematical model the influence of corneal curvature on IOP measurements is less than the influence of corneal thickness.23 Axial length is a measure of myopia, which is a risk factor for glaucoma. Our study measured axial length and axial length minus anterior chamber depth (which eliminates the contribution of corneal steepening, due to keratoconus, to axial length) and determined that the study and control patients were similar with regard to myopia (average, 25.5 mm for study cases and 25.3 mm for controls) and that CH was not correlated with axial length in this population.
Shah and associates22 used the ORA to study the relationship between CH, CRF, and CCT in over 200 normal eyes in patients with an average age of 62.1 years (SD 18.1, range 18–87 years). They reported the CH to average 10.7 (SD = 2.0) and the CRF to average 10.3 (SD = 2.0). In a large study of twins by Carbonaro and associates,24 the mean CH was 10.24 (SD = 1.54). The average CH in both our study and control keratoconus patients was lower than normal (8.2 vs 8.3, SD = 1.6 vs 1.5). In the series of Shah and coworkers,22 there was a wide range in normal CH, from 6.1 to 17.6. Both CH and CRF had a positive, but only moderate, correlation with CCT (average CCT, 545 μm, SD = 36.4, range 471–650 μm).
Kotecha and associates25 used the ORA to evaluate the association between CH and both age and CCT, among other things, in complex studies done using a prototype of the machine in 2002–2003 and determined that CH increased with CCT and decreased with age, indicating that thicker corneas have greater dampening properties and that older corneas are stiffer. Because of age-related changes in corneal biomechanical properties, it was decided in our study to age-match the study patients and controls.
Laiquzzaman and associates26 studied the diurnal variation of CH in normal subjects and determined that they were almost constant throughout the day. Kida and associates27 also reported that the change in CH over 24 hours was insignificant. Due to the reported lack of diurnal variation, the time of our study visits varied between 9 AM and 3 PM and depended on the convenience of the patient and the availability of visual field, disc photo, and A-scan testing.
In a review article by Brown and Congdon,18 there is an analysis of the literature regarding possible mechanisms by which corneal measurements could be associated with glaucoma. The thickness of the lamina cribrosa has been reported to be less in highly myopic eyes with glaucoma.28 It is hypothesized that a thin lamina cribrosa may be associated with the development of glaucoma. Studies on the optic nerve as a biomechanical structure susceptible to IOP changes are ongoing.29
Congdon and associates18 studied the impact of CCT and CH on glaucoma damage and determined that lower CH, but not CCT, was associated with progressive visual field loss in a series of 230 patients examined on a Glaucoma Service. Thin CCT, but not CH, was associated with a higher C/D ratio at the last examination. It was unclear if CCT was a risk factor for glaucoma via an effect on IOP measurement or if CCT is a surrogate for increased susceptibility to damage. Thinner CCT and lower CH were associated with glaucoma damage, but related to different outcomes. There may be pressure-independent risk factors for glaucoma related to the composition of the eye wall. The study by Congdon and associates18 is relevant to the current study. Their definition of glaucoma was based on abnormal, reliable visual fields by the OHTS criteria and optic nerve damage consistent with visual field damage as judged by fellowship-trained glaucoma specialists. C/D ratios were based on photos, when available, and description in the medical record, when photos were not available. We also found a significant correlation between CH and CCT. It is somewhat unexpected that different corneal properties were associated with optic nerve vs visual field damage, since optic nerve damage precedes visual field loss.
Broman and associates30 studied the relationship between various ocular parameters, including CCT, axial length, corneal curvature, and corneal astigmatism, with IOP measurements and CH in a large series of glaucoma patients. They found that GAT was less affected by CCT, changing by only 0.66 mm Hg per 10 μm in untreated eyes, compared to TonoPen and IOPg by ORA. Corneal hysteresis was significantly correlated with CCT, consistent with findings of our study. Corneal hysteresis was significantly associated with average corneal curvature, but not with GAT, axial length, or astigmatism. Their findings with regard to corneal curvature were different from our results, especially for steeper corneas, with average curvature over 45 diopters, which were associated with higher CH in Broman and associates’ study, but not in our patients. It is unclear how many glaucoma patients had steep corneas in their study. It is to be expected that the biomechanical properties of steep corneas with keratoconus would not be the same as normal steep corneas. Most CCTs in their study of glaucoma patients were between 500 and 600 μm, in contrast to our keratoconus patients with a mean CCT of 494 μm. In glaucoma patients, CCT and corneal curvature are usually within the normal range, whereas keratoconus by definition is associated with abnormal corneal thinning and steepening.
In a large study, Song and associates31 evaluated the association between CH and axial length among Chinese middle school students and found that longer axial length was significantly associated with lower CH and higher IOP. A prospective study would be necessary to test their hypothesis that low CH puts eyes at risk for axial elongation and myopia. Corneal hysteresis may contribute to the association of myopia with glaucoma. In addition, thin CCT and low CH may be indicators of a more readily deformable eye providing less support to the optic nerve in response to IOP, resulting in glaucoma. If this proves to be the case, CH, in addition to CCT, could identify those eyes with suspected glaucoma that are more likely to progress to glaucoma, which would benefit from early treatment. Our keratoconus patients had axial myopia with a mean axial length greater than 25 mm. They also had lower CH, were much older, and were predominantly Caucasian. The onset of keratoconus is heralded by increasing myopia in teenagers, and it would be worth investigating whether or not low CH in middle schoolers is a risk factor for the development of keratoconus.
Shah and associates9 studied the biomechanical properties of the cornea with the ORA in 207 normal and 93 keratoconic eyes and found a mean CH of 10.7 (SD = 2.0, range 6.1–17.6) among normals compared to a mean CH of 9.6 (SD = 2.2, range 4.7–16.7) among keratoconus patients. The CH was significantly lower in keratoconus patients. CH and CCT were moderately correlated. The mean age was 30 years greater in the normal patients (62.1 years) than in the keratoconus patients (32.3 years). Severity of keratoconus was graded using various Orbscan II (Bausch & Lomb Surgical, Rochester, New York) measurements, including anterior curvature, according to which K 45.1 to 46.9 D was considered mild and K > 50 D was severe. The difference in CH between mild and severe keratoconus (mean 10.3 vs 9.0) was significant. The difference in CH between normal patients and mild keratoconus (mean 10.7 vs 10.3) was not significant. Decreasing CH was associated with increasing keratoconus disease severity. CH was not able to distinguish between normals and mild keratoconus, as there was a wide range of CH with considerable overlap, limiting the usefulness of this test in screening patients for forme fruste or mild keratoconus prior to refractive surgery.
The study of Shah and associates9 is the largest published series evaluating CH in keratoconus patients. The number of keratoconus eyes is similar to the number in our study. The investigators did not age-match study and control patients; the mean age of their keratoconus patients (32.3 years) was around 30 years younger than the mean age of their normals (62.1 years) and of our keratoconus patients (59 years). Mean CCT in keratoconus was similar in both series. Increased severity of keratoconus, manifest by increased corneal curvature, is associated with decreased CH in both studies. The mean CH in our study (8.3) was lower than in Shah and associates’ study (9.6 overall, and 9.0 for severe keratoconus). Our keratoconus patients had an average maximum K by topography of over 52 D compared to less than half of the eyes (41 of 93, 44.1%) with severe disease associated with anterior K greater than 50 D in Shah and associates’ series. Our patients had more advanced keratoconus, as measured by maximum corneal curvature, and lower CH.
Ortiz and associates10 studied biomechanical properties in normal, post-LASIK, and keratoconic eyes and reported that CH and CRF were significantly lower in keratonconic eyes (mean, 7.5 and 6.2, respectively) than post-LASIK eyes (mean, 9.3 and 8.13, respectively). This was a large series of 251 eyes, including 165 normal eyes, 65 eyes 1 month post-LASIK, but only 21 keratoconic eyes. The mean CH in normal controls was similar in this series (10.8) to that in previous reports by Shah and associates (10.7.).9,22 Corneal hysteresis was reported to be lower in the oldest age bracket (60 to 80 years) compared to the youngest (9 to 14 years) normal control group, evidence that it is a good idea to age-match patients, but probably not necessary to do so very closely. No difference was observed between men and women, suggesting that it is not necessary to sex-match patients. The mean CH (7.5) and CRF (6.2) in keratoconic eyes was lower than in our series (8.3 and 7.1, respectively) and Shah and associates’study (CH 9.6).9 It is unclear why the CH was lower in the study by Ortiz and associates,10 as the keratoconus patients were young, averaging 30 years of age, similar to Shah and associates’ patients, and the mean K was 47.7 D and CCT was 498 μm, suggesting that keratoconus was not more severe in this small series. The severity of keratoconus was graded in the series by Ortiz and associates10 and found to significantly negatively correlate with CH and CRF, indicating that more advanced disease was associated with lower measurements. Despite the low average CH among keratoconus patients, there was still overlap in the CH of normal and keratoconus eyes, limiting the usefulness of the test in screening patients prior to refractive surgery.
Regarding the structural integrity of the optic nerve head, at the Ocular Biomechanics Symposium, ARVO 2008, the lamina cribrosa was described as a weak spot in the sclera with a complicated, variable anatomy and blood supply that could be a factor in the variable susceptibility of eyes to similar IOPs (Downs J, ARVO Meeting, 2008, Symposium). Scleral mechanics were described as driving optic nerve head biomechanics (McBrien NA, ARVO Meeting, 2008, Symposium). Increased stiffness (decreased elasticity) of the sclera with age is associated with increased collagen cross-linking.32 Structural properties of the cornea may be related to both the sclera and optic nerve.
An important study by Wells and associates33 investigated prospectively the relationship between acute IOP-induced optic nerve head deformation with CH and CCT in glaucomatous and control human eyes by raising the IOP with a modified LASIK suction ring to 64 mm Hg for less than 30 seconds and mapping the optic nerve head surface before and during IOP elevation using a Heidelberg retina tomograph II. Both CH and CCT were lower in the glaucoma patients (8.8 and 532 μm, respectively). Controlling for age and sex, by multiple variable analysis, in glaucoma patients but not controls, only CH was significantly correlated with mean cup depth increase, CCT, and axial length. This research tests the hypothesis that eyes with a more deformable cornea, with less viscous damping and lower CH, have optic discs that are more susceptible to glaucoma damage from increased IOP. The results suggest that CH represents properties of the eye and not just the cornea and that glaucoma patients have altered ocular biomechanics.
In a case report by Kerautret and associates34 of a patient who developed unilateral corneal ectasia after bilateral LASIK, it was observed that the 2 eyes had similar postoperative CH and CRF values, but that the affected eye had different waveform morphology of the ORA signals, with lower amplitude of the applanation peaks. In addition to the lower amplitudes, the width of peak 2 was greater in the ectatic eye. In keratoconus, it is typical that the peak amplitudes are lower and the signals are wider. Additional studies of the waveforms of our keratoconus patients are ongoing with recently available software, which may reveal differences not observed in the CH and CRF measurements. Software is now available from the manufacturer that will make it possible to study many waveform parameters.
A recent study of the cost-effectiveness of treating ocular hypertension35 determined that the cost of preventing one case of glaucoma decreased if risk factors were taken into account, including CCT of 533 μm (40 μm less than the average in the OHTS study) and vertical C/D ratio of 0.6 (0.2 wider than the average). Keratoconus patients suspected of having glaucoma usually are at risk by virtue of thin corneas and an increased C/D ratio, not borderline IOP, as in the OHTS study. If low CH proves to be an independent risk factor for glaucoma, that may further increase the value of treating keratoconus patients with suspected glaucoma. The findings of the Collaborative Normal-Tension Glaucoma Study36 that a 30% reduction in IOP significantly prevented or delayed disease progression in 80% of patients after 5 years follow-up may apply to keratoconus patients with normal-tension glaucoma.
CONCLUSIONS
The ORA is a relatively new device that improves our ability to study ocular biomechanics directly and noninvasively. Future studies may increase our understanding of exactly what the ORA measures and determine how important its results are in evaluating patients’ risk of developing glaucoma, including normal-tension glaucoma, and in predicting risk of progression of glaucoma. Longitudinal studies are needed to determine if altered ocular biomechanics, as measured by the ORA, precede and/or follow glaucoma.
Keratoconus and pellucid patients can develop normal-tension glaucoma. The diagnosis of glaucoma is challenging in these patients because of the difficulty of optic nerve evaluation in the setting of irregular astigmatism and corneal scarring in these ectatic corneal diseases. However, this study found visual fields to be reliable and useful in patients with keratoconus and pellucid. A low threshold for performing visual field tests is necessary in this patient population. It is important that ophthalmologists be aware of the possible association of keratoconus with normal-tension glaucoma so that appropriate testing is done and treatment given. In this study, keratoconus and pellucid patients who had glaucoma or suspected glaucoma and control keratoconus and pellucid patients all had lower than normal CH and CRF measured by the ORA. The results of this study indicate that all older patients with keratoconus and pellucid may be at risk for normal-tension glaucoma. It would be of interest to study biomechanical properties in normal-tension glaucoma patients without keratoconus or pellucid to determine if low CH and CRF are risk factors. Our study suggests that normal-tension glaucoma may be associated with abnormal biomechanical properties predisposing the optic nerve to glaucomatous damage at normal pressures.
ACKNOWLEDGMENTS
Funding/Support: This research was made possible by funding from Kenneth B. Gray, Jr, and the Gray Corneal Research Fund at Wills Eye Institute.
Financial Dislosures: None.
Conformity With Author Information: The Wills Eye Institute Institutional Review Board approved this research.
Other Acknowledgements: Statistical assistance was provided by Jacqueline R. Cater, PhD, Senior Associate Biostatistician at Biomedical Statistical Consulting, Wynnewood, Pennsylvania. The author acknowledges the contributions of Jonathan S. Myers, MD, and Louis W. Schwartz, MD, of the Glaucoma Service, Wills Eye Institute; and Kristin M. Hammersmith, MD, Christopher J. Rapuano, MD, and Peter R. Laibson, MD, of the Cornea Service, Wills Eye Institute.
REFERENCES
- 1.Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–720. doi: 10.1001/archopht.120.6.714. [DOI] [PubMed] [Google Scholar]
- 2.Ozbek Z, Cohen EJ, Hammersmith KM, Rapuano CJ. Dynamic contour tonometry: a new way to assess intraocular pressure in ectatic corneas. Cornea. 2006;25:890–894. doi: 10.1097/01.ico.0000224649.12214.33. [DOI] [PubMed] [Google Scholar]
- 3.Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31:156–162. doi: 10.1016/j.jcrs.2004.10.044. [DOI] [PubMed] [Google Scholar]
- 4.Friedenwald JS. Contribution to the theory and practice of tonometry. Am J. Ophthalmol. 1937;20:985–1024. [Google Scholar]
- 5.Edmund C. Assessment of an elastic model in the pathogenesis of keratoconus. Acta Ophthalmol. 1987;65:545–550. doi: 10.1111/j.1755-3768.1987.tb07038.x. [DOI] [PubMed] [Google Scholar]
- 6.Edmund C. Corneal rigidity and ocular rigidity in normal and keratoconic eyes. Acta Ophthalmol. 1988;66:134–140. doi: 10.1111/j.1755-3768.1988.tb04000.x. [DOI] [PubMed] [Google Scholar]
- 7.Brooks AMV, Robertson IF, Mahoney A. Ocular rigidity and intraocular pressure in keratoconus. Aust J Ophthalmol. 1984;12:317–324. doi: 10.1111/j.1442-9071.1984.tb01175.x. [DOI] [PubMed] [Google Scholar]
- 8.Foster CS, Yamamoto GK. Ocular rigidity in keratoconus. Am J Ophthalmol. 1978;86:802–806. doi: 10.1016/0002-9394(78)90125-3. [DOI] [PubMed] [Google Scholar]
- 9.Shah S, Laiquzzaman M, Bhojwani R, Mantry S, Cunliffe I. Assessment of the biomechanical properties of the cornea with the Ocular Response Analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci. 2007;48:3026–3031. doi: 10.1167/iovs.04-0694. [DOI] [PubMed] [Google Scholar]
- 10.Ortiz D, Pinero D, Shabayek MH, Arnalich-Montiel F, Alio JL. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg. 2007;33:1371–1375. doi: 10.1016/j.jcrs.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 11.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. New York: John Wiley & Sons; 2004. pp. 291–321. [Google Scholar]
- 12.Hosmer DW, Lemeshow S. Logistic regression for matched case-control studies. New York: John Wiley & Sons; 1989. pp. 187–215. [Google Scholar]
- 13.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. pp. 1–40. [Google Scholar]
- 14.Casson RJ, Abraham LM, Newland HS, et al. Corneal thickness and intraocular pressure in a nonglaucomatous Burmese population. Arch Ophthalmol. 2008;126:981–985. doi: 10.1001/archopht.126.7.981. [DOI] [PubMed] [Google Scholar]
- 15.Medieros FA, Sample PA, Zangwill LM, et al. Corneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous topic neuropathy. Am J Ophthalmol. 2003;136:805–813. doi: 10.1016/s0002-9394(03)00484-7. [DOI] [PubMed] [Google Scholar]
- 16.Dueker DK, Singh K, Lin SC, et al. Corneal thickness measurement in the management of primary open-angle glaucoma. Ophthalmology. 2007;114:1779–1787. doi: 10.1016/j.ophtha.2007.04.068. [DOI] [PubMed] [Google Scholar]
- 17.Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the Ocular Response Analyzer. J Glaucoma. 2006;15:364–370. doi: 10.1097/01.ijg.0000212268.42606.97. [DOI] [PubMed] [Google Scholar]
- 18.Congdon NG, Broman AT, Bandeen-Roche K, Grover V, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006;141:868–875. doi: 10.1016/j.ajo.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Brown KE, Congdon NG. Corneal structure and biomechanics: impact of the diagnosis and management of glaucoma. Curr Opin Ophthalmol. 2006;17:338–343. doi: 10.1097/01.icu.0000233951.01971.5b. [DOI] [PubMed] [Google Scholar]
- 20.Kotecha A. What biomechanical properties of the cornea are relevant for the clinician? Surv Ophthalmol. 2007;52:S109–114. doi: 10.1016/j.survophthal.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Dupps WJ. Hysteresis: new mechanospeak for the ophthalmologist. J Cataract Refract Surg. 2007;31:156–162. doi: 10.1016/j.jcrs.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Shah S, Laiquzzaman M, Cunliffe I, Mantry S. The use of the Reichert ocular response analyser to establish the relationship between ocular hysteresis, corneal resistance factor and central corneal thickness in normal eyes. Contact Lens Anterior Eye. 2006;29:257–262. doi: 10.1016/j.clae.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement. J Cataract Refract Surg. 2005;31:146–155. doi: 10.1016/j.jcrs.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 24.Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ. The heritability of corneal hysteresis and ocular pulse amplitude. Ophthalmology. 2008;115:1545–1549. doi: 10.1016/j.ophtha.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Kotecha A, Elsheikh A, Roberts CR, Zhu H, Garway-Heath DF. Corneal thickness and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Invest Ophthalmol Vis Sci. 2006;47:5337–5347. doi: 10.1167/iovs.06-0557. [DOI] [PubMed] [Google Scholar]
- 26.Laiquzzaman M, Bhojwani R, Cunliffe I, Shah S. Diurnal variation of ocular hysteresis in normal subjects: relevance in clinical context. Clin Exp Ophthalmol. 2006;34:114–118. doi: 10.1111/j.1442-9071.2006.01185.x. [DOI] [PubMed] [Google Scholar]
- 27.Kida T, Liu JHK, Weinreb RN. Effects of aging on corneal biomechanical properties and their impact on 24-hour measurement of intraocular pressure. Am J Ophthalmol. 2008;146:567–572. doi: 10.1016/j.ajo.2008.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jonas JB, Berenshtein E, Holbach L. Lamina cribrosa thickness and spatial relationships between intraocular space and cerebrospinal fluid space in highly myopic eyes. Invest Ophthalmol Vis Sci. 2004;45:2660–2665. doi: 10.1167/iovs.03-1363. [DOI] [PubMed] [Google Scholar]
- 29.Burgoyne CF, Downs JC, Bellezza AJ, et al. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage Prog Retin Eye Res. 2005;24:39–73. doi: 10.1016/j.preteyeres.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Broman AT, Congdon NG, Bandeen-Roche K, Quigley HA. Influence of corneal structure, corneal responsiveness, and other ocular parameters on tonometric measurement of intraocular pressure. J Glaucoma. 2007;16:581–588. doi: 10.1097/IJG.0b013e3180640f40. [DOI] [PubMed] [Google Scholar]
- 31.Song Y, Congdon N, Li L, et al. Corneal hysteresis and axial length among Chinese secondary school children: the Xichang pediatric refractive error study (X-PRES) report No. 4. Am J Ophthalmol. 2008;145:819–826. doi: 10.1016/j.ajo.2007.12.034. [DOI] [PubMed] [Google Scholar]
- 32.Schultz DS, Lotz JC, Lee SM, Trinidad ML, Stewart JM. Structural factors that mediate scleral stiffness. Invest Ophthalmol Vis Sci. 2008;49:4232–4236. doi: 10.1167/iovs.08-1970. [DOI] [PubMed] [Google Scholar]
- 33.Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KCY, Sachdev N. Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci. 2008;49:3262–3268. doi: 10.1167/iovs.07-1556. [DOI] [PubMed] [Google Scholar]
- 34.Kerautret J, Colin J, Touboul D, Roberts Biomechanical characteristics of the ectatic cornea. J Cataract Refract Surg. 2008;34:510–513. doi: 10.1016/j.jcrs.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 35.Stewart WC, Stewart JA, Nassar QJ, Mychaskiw MA. Cost-effectiveness of treating ocular hypertension. Ophthalmology. 2008;115:94–98. doi: 10.1016/j.ophtha.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 36.Collaborative Normal-Tension Glaucoma Study Group Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–497. doi: 10.1016/s0002-9394(98)00223-2. [DOI] [PubMed] [Google Scholar]