Abstract
Purpose:
The mini-tenotomy is a novel minimally invasive surgical technique that weakens rectus muscles to treat small-angle strabismus. The mini-tenotomy is an alternative to the standard rectus muscle recession that requires hooking the muscle, suturing the muscle, removing the muscle from sclera, and reattaching the muscle to sclera.
Methods:
This is a retrospective chart review of outcomes of the mini-tenotomy procedure on 15 consecutive adult patients. A central tenotomy of 3 mm was performed cutting through intact conjunctiva using a blunt Westcott scissors.
Results:
Preoperatively 6 patients were esotropic, measuring between 2 and 16Δ (mean, 8Δ), and 9 patients had vertical deviations that measured between 2 and 6Δ (mean, 3.5Δ).
Final postoperative esodeviations ranged from 1 to 8Δ (mean, 5.8Δ), and hyperdeviations ranged from 0 to 4Δ (mean, 1.3Δ). Final improvement of the deviation was larger for hypertropia, with a mean of 2.3Δ, vs esotropia, with a mean of 1.3Δ.
Conclusion:
The mini-tenotomy is a safe and effective treatment for diplopia caused by a small-angle hypertropia or esotropia. It is a minimally invasive surgery that can be done in office with topical anesthesia. As with any strabismus procedure, more than one surgery may be necessary.
INTRODUCTION
Normal divergence and vertical fusion amplitudes are small, with divergence measuring 4 to 6 prism diopters (Δ) and vertical vergence less than 2 D.1 Because of this, even small esodeviations and vertical deviations can cause significant asthenopic symptoms and diplopia, especially when the deviation is acquired in adulthood. Historically, these small-angle deviations have been treated with prism glasses. Prism spectacles are an excellent option if the patient is wearing spectacles for a refractive error, but for many patients prism spectacles are undesirable. Emmetropic patients, contact lens wearers, or postoperative refractive surgery patients generally do not consider prism spectacles an optimal treatment. Standard strabismus surgery, such as rectus muscle recession and resection, is designed to correct moderate to large-angle strabismus, usually greater than 10Δ. Patients with strabismus less than 6Δ to 8Δ are not good surgical candidates because of the risk for overcorrection. This report introduces an alternative to standard strabismus surgery, a minimally invasive surgical procedure, a mini-tenotomy developed by the author. This procedure can be performed in the office with topical anesthesia and is specifically designed to correct diplopia associated with small-angle strabismus.
METHODS
Charts from 15 consecutive patients who had undergone the mini-tenotomy procedure and had at least 1 month follow-up were reviewed. Mini-tenotomy was considered for the treatment of vertical deviations of 6Δ or less and horizontal deviations of 16Δ or less. The Internal Review Board of Cedars Sinai Medical Center approved the retrospective study, and patient confidentiality was maintained. The author performed the surgery in each case. Patients were examined by the author preoperatively and postoperatively. In two cases (patients 5 and 10), the last postoperative examination was done by the referring ophthalmologist.
The procedure was performed in the office using topical anesthetic with the patient fully awake and no sedation. Proparacaine, phenylephrine 2.5 %, and Vigamox drops were placed on the surgical eye prior to the surgery. Topical phenylephrine 2.5% was used to blanch the conjunctiva to facilitate visualization of the anterior cilliary vessels that come off the rectus muscle insertion. A cotton-tipped applicator soaked in proparacaine was placed on the conjunctiva overlying the surgical muscle for approximately 2 to 3 minutes. A lid speculum opened the eye. To expose the muscle, the patient was directed to look away from the surgical muscle. For example, if an inferior rectus was the surgical muscle, the patient was asked to look up, thus exposing the inferior rectus muscle. The anterior ciliary vessels of the surgical muscle were identified by direct visualization through intact conjunctiva.
With the conjunctiva intact, 3 to 4 mm of central muscle tendon was grasped with a 0.75 Wright tenotomy forceps (Titan Surgical, Los Angeles, California) at approximately 8 to 9 mm posterior to the limbus for the inferior rectus muscle and 7 to 8 mm posterior to the limbus for the medial rectus muscle (Figure 1). Care was taken to avoid grasping the anterior ciliary vessels. Once the rectus tendon was grasped, the forceps were gently moved side to side to see if the eye also moved, thus verifying that the tendon was grasped, rather than just superficial conjunctiva. After the central tendon was secured with the forceps, the tendon was gently pulled up off the globe and blunt Westcott scissors were used to cut the tendon between the forceps and sclera through the intact conjunctiva (Figure 2). After the central tenotomy, the tendon was released to fall back posteriorly (Figure 3). In some cases, if only 1 to 2 mm of tendon was initially cut, the tendon was re-grasped and the mini-tenotomy was repeated to obtain 3 to 4 mm of central tenotomy. The millimeters of central tenotomy were estimated by sight, not measured.
FIGURE 1.
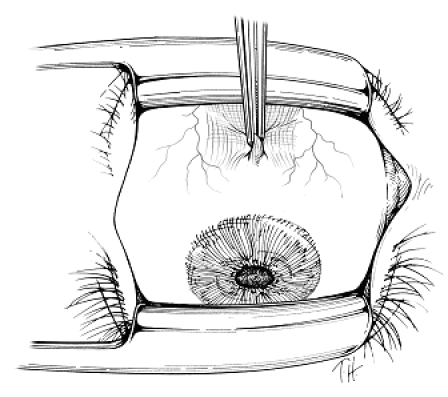
After topical anesthetic is applied, the Wright 0.75-tooth tenotomy forceps grasp the central tendon of the rectus muscle through the intact conjunctiva
FIGURE 2.
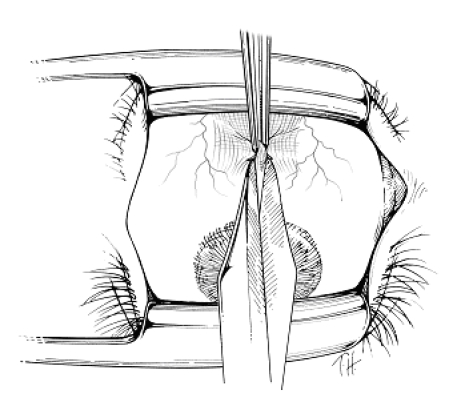
Blunt Westcott scissors is used to cut the central tendon between the forceps and sclera through the intact conjunctiva.
FIGURE 3.
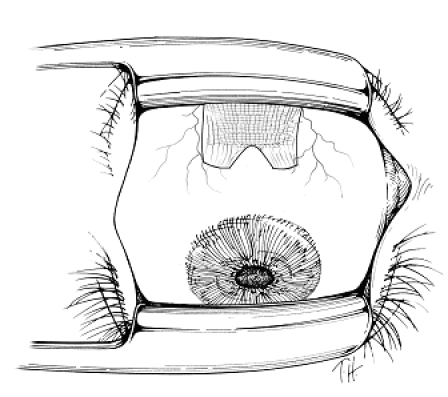
Postoperative drawing of the mini-tenotomy showing the central 3 to 4 mm of the tendon is cut. Note that the two muscle poles at the extremes of the insertion are left intact, maintaining the normally broad insertion.
After the mini-tenotomy the patient was examined by cover test. If a residual deviation was present, the surgeon had the option to perform a mini-tenotomy of the fellow eye (ie, the antagonist of the yoke muscle to the operated muscle). At the end of the procedure, Vigamox drops were placed in the eye and the patient was sent home. A therapeutic regimen of either antibiotic corticosteroid ointment, two times a day for 3 days, or Vigamox drops, two times a day for 3 days, was begun.
RESULTS
A summary of preoperative and postoperative details is shown in the Table. Patient ages ranged from 35 to 86 years, and 11 of 15 patients were 60 years or older. All 15 patients had binocular diplopia, and 5 of 15 were using prism glasses prior to surgery. Preoperatively 6 patients were esotropic, measuring between 2 and 16Δ (mean, 8Δ), and 9 patients had vertical deviations that measured between 2 and 6Δ (mean, 3.5Δ).
TABLE.
DATA FOR 15 PATIENTS WHO UNDERWENT MINI-TENOTOMY
| PATIENT NO. | AGE (yr) | DIAGNOSIS | PREOP DEV (Δ) | MINI-T | POSTOP DEV (Δ) IMMED | CHANGE PER MINI-T (Δ) IMMED | POSTOP FINAL DEV (Δ) | CHANGE PER MINI-T (Δ) FINAL | FOLLOW-UP (mo) | POST MINI-T DIPLOPIA |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 55 | Retinal detachment Hypertropia | Right hypertropia 2 | Left inferior rectus & 2nd mini-T @ 1 yr | 0 | 2 | 0 | 2 | 13 | Resolved |
| 2 | 70 | Divergence paresis Esotropia | Esotropia 16 | Bilateralmedia l rectus | Esophoria 8 | 4 | Esophoria 8 | 4 | 5 | Improvement strabismus surgery |
| 3 | 65 | Divergence paresisEsotropia | Esophoria 4 | Bilateral medial rectus | 0 | 2 | Esotropia 4 | 0 | 3 | No improvement strabismus surgery |
| 4 | 78 | Congenital superior oblique palsyHypertropia | Right hypertropia 5 | L inferior rectus & 2nd mini-T Right superior rectus @ 3 wk | 0 | 2.5 | 0 | 2.5 | 2 | Resolved |
| 5 | 49 | Graves | Right hypertropia 2 | Left inferior rectus | 0 | 2 | Right hypertropia 2 | 0 | 1 | No improvement |
| 6 | 73 | Congenital superior oblique palsyHypertropia | Right hypertropia 4 | Right superior rectus with left inferior rectus | 0 | 4 | Right hypertropia 3 | 1 | 1 | No improvement |
| 7 | 73 | Cataract surgeryHypertropia | Left hypertropia 4 | Right inferior rectus | 0 | 4 | Right hypertropia 1 | 3 | 1 | Resolved |
| 8 | 86 | Divergence paresis Esotropia | Esophoria 6 | Bilateral medial rectus | Esophoria 1 | 3 | Esophoria 6 | 0 | 11 | No improvement prism |
| 9 | 78 | Divergence paresisEsotropia | Esotropia 10 | Bilateral medial rectus | Esophoria 2 | 4 | Esophoria 8 | 1 | 6 | Improvement |
| 10 | 35 | Strabismus surgeryHypertropia | Right hypertropia 3 | Left inferior rectus | 0 | 3 | Right hypertropia 3 | 0 | 1 | No improvement |
| 11 | 71 | Trauma Esotropia | Esotropia 8 | Bilateral medial rectus | Esophoria 2 | 3 | Esophoria 8 | 0 | 4 | No improvement, strabismus surgery |
| 12 | 78 | Cataract surgery | Right hypertropia 2 | Right superior rectus | 0 | 2 | Right hypertropia 1 | 1 | 12 | Improvement |
| 13 | 78 | Cataract surgery | Esophoria 4 | Bilateral medial rectus | 0 | 2 | Esophoria 1 | 1.5 | 4 | Resolved |
| 14 | 68 | Strabismus surgery | Right hypertropia 4 | Left inferior rectus & 2nd mini-T @ 6 wk | 0 | 2 | 0 | 2 | 3 | Resolved |
| 15 | 52 | Diplopia post refractive surgery | Right hypertropia 6 | Right superior rectus | Right hypertropia 2 | 4 | 0 | 6 | 5 | Resolved |
Dev, deviation; Immed, immediately (day of surgery).
Final postoperative esodeviations ranged from 1 to 8Δ (mean, 5.8Δ), and hyperdeviations ranged from 0 to 4Δ (mean, 1.3Δ). Final improvement of the deviation was larger for hypertropia, with a mean of 2.3Δ, vs esotropia, with a mean of 1.3Δ. There seemed to be greater immediate improvement of the deviation (mean, 3.0Δ) as compared to the amount of improvement measured on the last follow-up visit (mean, 1.6Δ). Eight of the 15 patients (53%) were successfully treated with the mini-tenotomy procedure, improving the diplopia so no further treatment with prisms or standard strabismus surgery was necessary. Of 6 esotropic patients, 2 patients (33%) were successfully treated with the mini-tenotomy, whereas 3 required standard strabismus surgery and one was prescribed prism glasses. Hypertropia was successfully treated with the mini-tenotomy procedure in 6 of 9 patients (66%). Patients 1, 4, and 14 had a second mini-tenotomy in order to achieve success. In patients 1 and 14 the second procedure involved the previously tenotomized muscle, and in patient 4 it involved the muscle of the other eye.
Of 3 patients who subsequently had standard strabismus surgery, two had strabismus surgery on a rectus muscle that previously had a mini-tenotomy procedure. At the reoperation, there was minimal scarring and the central tendon was found to be adherent to sclera approximately 2 to 3 mm posterior to the original insertion. The previous mini-tenotomy procedure did not interfere with the standard strabismus surgery. There were no significant complications in any patient; however, 2 patients had a small self-limiting subconjunctival hemorrhage that resolved spontaneously, and one had blurred vision caused by topical anesthetic keratopathy that resolved spontaneously. Conjunctival scarring over the incision site was minimal. Each patient was asked if there had been pain or discomfort during the procedure. No patient experienced significant discomfort; however, 3 patients did not like the feeling of the lid speculum.
DISCUSSION
Rectus muscle tenotomy is one of the first strabismus surgeries, described as early as the late 1800s.2 In 1841 Reute described the tenotomy stating, “The tendon is cut without separating it from its surrounding tissue and the closer to its insertion the smaller the angle of strabismus.”2 Bohm modified the tenotomy in an attempt to avoid overcorrection, leaving the middle of the tendon intact (partial lateral tenotomy).2 Tenotomy of rectus muscles was generally abandoned until Scott3 reported graded rectus muscle tenotomy in 2006. This technique included subconjunctival injection of lidocaine and a conjunctival incision to expose the tendon. Over half the tendon was removed, starting at one pole, leaving one tendon pole attached to sclera, resulting in the cut tendon slanting back at an angle of 45°. Scott noted that a 60% to 70% tenotomy, or removing 6 to 7 mm of tendon, corrected approximately 4Δ of strabismus. It is interesting that the prism diopters of correction per millimeter of tenotomy described by Scott is similar to the correction reported in the present study, where a 3- to 4-mm mini-tenotomy resulted in about 2Δ of correction.
The slanted tenotomy reported by Scott effectively moves the insertion, thus changing the vector of muscle force and potentially inducing incomitance. Scott noted that in most cases this is not a practical issue; however, he did state that a “bothersome” vertical deviation could be induced if an upper tenotomy of one medial rectus muscle was performed along with a lower tenotomy on the contralateral medial rectus muscle. Likewise, an A pattern could theoretically be induced, or a V pattern treated, if the upper poles of both medial rectus muscles were removed, effectively moving the insertions down. This induced incomitance caused by the slanted pole tenotomy was substantiated by van der Muelen-Schot and associates.4 In contrast to the slanted pole tenotomy, the mini-tenotomy described in this report is performed on the central tendon. The central tenotomy keeps the tendon poles intact so the normal wide rectus insertion is maintained, thus avoiding induced incomitance (Figure 3).
A central 3- to 4-mm tenotomy as described in this study releases approximately one-third of the insertion, as the rectus insertions are approximately 9 to 10 mm wide. The partial tenotomy produced a relatively small effect in most cases, correcting no more than 2 to 3 Δ of strabismus. A correction of up to 4 to 5Δ can be obtained if binocular surgery is performed. For example, a right hypertropia of 4Δ could be corrected by a right superior rectus tenotomy and left inferior rectus tenotomy. An esotropia of 4 to 6Δ can be treated with bilateral medial rectus tenotomies. The mini-tenotomy described in this report is somewhat adjustable. One can operate on one muscle, then remeasure the deviation to determine if additional surgery is needed. Additionally, the size of the tenotomy can be enlarged by resnipping additional tendon fibers if a residual deviation is present. In patients in whom the mini-tenotomy fails to alleviate diplopia, standard surgery can be safely done without difficulty.
In some patients the deviation recurred several weeks to months after the mini-tenotomy procedure was done. This may be due to a larger phoria that was not disclosed preoperatively by standard alternate cover test, or it may be due to the scar contracture or muscle reorganization that occurs during the healing process. In this series there were no overcorrections, but several patients were undercorrected. Perhaps a larger tenotomy or posterior stripping of the tenotomized muscle might result in a greater correction.
Technically, the procedure is straightforward but does require facility with the extraocular muscles. The author prefers grasping the rectus tendon with Wright tenotomy forceps (0.75 mm) that have slightly blunt teeth and cutting the tendon with blunt Westcott scissors to avoid the unlikely occurrence of inadvertent scleral perforation. Using this technique, there were no significant complications. Transient blurred vision caused by topical anesthetic–induced keratopathy developed in one patient and resolved over 2 to 3 days, and two patients had a subconjunctival hemorrhage that was treated with direct pressure using a cotton-tipped applicator. The mini-tenotomy performed with topical anesthetic is almost painless. The only complaints were discomfort from insertion of the eyelid speculum. Grasping and cutting the central tendon did not cause pain in this series of patients.
The mini-tenotomy described in this report was found to be useful in treating diplopia in some patients with small-angle strabismus who did not want prism spectacles. It is a minimally invasive surgery that can be done in the office with topical anesthesia, and it provides an option to prism spectacles and standard strabismus surgery.
ACKNOWLEDGMENTS
Funding/Support: This study was supported by the Wright Foundation for Pediatric Ophthalmology and Strabismus.
Financial Disclosures: Dr Wright receives a royalty on a surgical instrument manufactured by Titan Surgical LLC but does not receive royalty from instruments discussed in this article.
Conformity With Author Information: The Internal Review Board from Cedars Sinai Medical Center approved the retrospective study, and patient confidentiality was maintained.
REFERENCES
- 1.Wright KW, Spiegel P. Pediatric Ophthalmology and Strabismus. 2nd ed. New York: Springer-Verlag; 2002. Binocular vision and introduction to strabismus; p. 155. [Google Scholar]
- 2.von Noorden GK, editor. The History of Strabismology. Oostende, Belgium: JP Wayenborgh; 2002. Strabismology from its beginnings to the middle of the 19th century; pp. 41–46. [Google Scholar]
- 3.Scott AB. Graded rectus muscle tenotomy. Arch Chil Oftal. 2006;63:127–128. [Google Scholar]
- 4.van der Muelen-Schot HM, van der Muelen-Schot SB, Simonsz HJ. Caudal or cranial partial tenotomy of the horizontal rectus muscles in A and V pattern strabismus. Br J Ophthalmol. 2008;92:245–251. doi: 10.1136/bjo.2007.121848. [DOI] [PubMed] [Google Scholar]


