Abstract
Purpose
To evaluate the validity and repeatability of crystalline lens thickness measurements obtained by anterior segment optical coherence tomography.
Methods
Forty-seven normal children (mean age, 11.06 ± 2.30 years) had their crystalline lens thickness measured with the Visante anterior segment optical coherence tomography (OCT) (Carl Zeiss Meditec, Dublin, CA) and with conventional corneal touch A-scan ultransonography (ultrasound) (Humphrey 820). The subjects’ right corneas were anesthetized, and their right eyes were cyclopleged. Five ultrasound measurements were recorded per eye, and three Visante OCT measurements were recorded per eye. Thirty-eight subjects had measurements at a second visit where three additional Visante OCT measurements were recorded.
Results
The mean of the differences between the Visante OCT and ultrasound was −0.045 mm (p = 0.017) with 95% limits of agreement from −0.29 to 0.20 mm indicating that the measurement of crystalline lens thickness was slightly thinner with the Visante OCT. When validity was assessed using only Visante OCT images that contained the corneal reflex, the mean of the differences was 0.019 mm (p = 0.11) with 95% limits of agreement from −0.091 to 0.13 mm. For the repeatability of the Visante OCT, the mean of the differences between visit one and visit two was −0.008 mm (p = 0.25) with 95% limits of agreement from −0.088 to 0.072 mm. Repeatability improved when reassessed using only images that contain the corneal reflex; the mean of the differences was −0.0001 mm (p = 0.97) with 95% limits of agreement from −0.030 to 0.030 mm.
Conclusion
The Visante OCT is a non-contact instrument that is simple to use, and it provides valid crystalline lens thickness measurements with excellent repeatability. Validity and repeatability are optimized when the Visante OCT images contain the corneal reflex and a consistent corneal index refraction is applied to the entire image.
Keywords: Anterior segment optical coherence tomography, crystalline lens, validity, repeatability, Visante OCT
Accurate measurements of crystalline lens thickness are important to studies of myopia progression,1, 2 refractive error,3 and ocular accommodation. A variety of methods are available to measure the axial components of the eye. A-scan ultrasonography is the gold standard for both clinical practice and research to measure the thickness of the crystalline lens. The drawback of this method is that the ultrasound probe physically contacts the cornea and requires corneal anesthesia prior to measurement, making this method more challenging when performed on children. In addition, precise positioning of the A-scan probe is difficult because there is no distinct landmark that can be used to align the instrument with the cornea. It is not surprising that A-scan ultrasonography has been shown to be insensitive to lens thickness changes less than or equal to 0.75 D.4 Therefore, minimal changes in lens thickness due to accommodation, lens growth, or index of refraction changes may go undetected when measured using A-scan ultrasonography.
The Visante anterior segment optical coherence tomographer (OCT) (Carl Zeiss Meditec, Dublin, CA) is a new instrument designed to image the anterior segment of the eye. It utilizes low-coherence interferometry to create a detailed image of human tissue. Crystalline lens thickness measurements can be made using the images captured by this instrument. The Visante OCT is easy to use and does not require corneal contact, making it a more advantageous option for studying children. The Visante OCT has previously been shown to be a reliable tool to measure the anterior chamber angle,5,6 anterior chamber volume,7 and central corneal thickness.8, 9 A recent study also used a model eye to assess the accuracy and validity of Visante OCT anterior segment measurements and reported formulas that reduced errors when measuring the model eye.10 To the best of our knowledge, no human studies have been conducted to assess the validity and repeatability of the Visante OCT in the measurement of crystalline lens thickness.
The current study assessed the inter-instrument agreement between the Visante OCT and conventional A-scan ultrasonography (ultrasound) for the measurement of crystalline lens thickness. The between-visit repeatability of measurements made with the Visante OCT was also assessed.
METHODS
Subjects
Subjects were 47 children ages eight to 15 years who participated in a study of myopia development and crystalline lens oscillations after saccadic eye movements. The Ohio State University’s Biomedical Sciences Institutional Review Board, in accordance with the tenets of the Declaration of Helsinki, approved the study protocol. Subjects were educated on the purpose and the procedures of the study, and parental consent and child assent were obtained before enrollment into the study. Data for this study were obtained from two visits. At the first visit, the crystalline lens thickness was measured with A-scan ultrasonography and the Visante OCT. A subset of 38 children had Visante crystalline lens measurements made at a second study visit that was approximately two weeks after the initial study visit. No visits were separated by more than three months.
A-Scan Ultrasound Measurement
Crystalline lens thickness was measured by corneal touch A-scan ultrasonography (Model 820, Allergan-Humphrey, San Leandro, CA) using a focused transducer with a frequency of 10 MHz in semi-automatic mode. Cycloplegia was performed on the right eye of each subject with two drops of 1% tropicamide separated by five minutesafter one drop of 0.5% proparacaine. After 30 minutes, each subject’s right cornea was anesthetized with one drop of 0.5% proparacaine. Five consecutive measures were obtained by one examiner (MDB). Ultrasound traces with small corneal or retinal peaks were deleted, and an effort was made to select traces with good component definition. The mean of the five recordings of lens thickness was used to compare to the measurements made by the Visante OCT.
Visante OCT Anterior Segment Optical Coherence Tomography Measurement
The right eye was imaged with anterior segment optical coherence tomography (Zeiss Visante OCT Model 1000, Carl Zeiss Meditec, Dublin, CA). Version 1.0 of the Visante OCT software was used in this study. The Visante OCT is a non-contact, non-invasive, high-resolution device that uses infrared light to image the anterior segment of the eye and measure intra-ocular distances. The system uses a Michelson interferometer illuminated by partial or low-coherence light from a 1310 nm superluminescent diode. A beam splitter creates two separate light rays, one targeting the sample and the other targeting the reference mirror. A signal is detected only when the reflections are nearly matched in time-of-flight. Similar to the scanning technology of the ultrasound B-scan, the Visante OCT acquires multiple scans to create a two-dimensional image. Low resolution images are produced from 256 A-scans in 125 milliseconds and a high resolution image from 512 A-scans in 250 milliseconds.11
The scanning of the crystalline lens is a non-contact procedure in which the subject fixates on an internal fixation target. Subjects were cyclopleged, as explained above, and images were captured 30 minutes after instillation of the first drop. The crystalline lens was imaged on the “anterior segment single” scanning mode for low-resolution images. Images gathered early in the study did not always contain the “corneal reflex,” which the Visante OCT manual states is an indication that the image is optimally aligned and appears as a central white line in the image.11 Therefore, statistical analyses were performed for the entire dataset as well as for the subset of only the images that contained the corneal reflex. Figure 1 is an image of the crystalline lens with the corneal reflex captured by the Visante OCT. Three images of the right eye were captured and stored for later analysis. Crystalline lens thickness was measured by a single observer using the Visante OCT internal caliper system. In all cases, the thickest portion of the crystalline lens was measured. The same protocol was followed at the second visit to capture three additional images of the crystalline lens.
Figure 1.
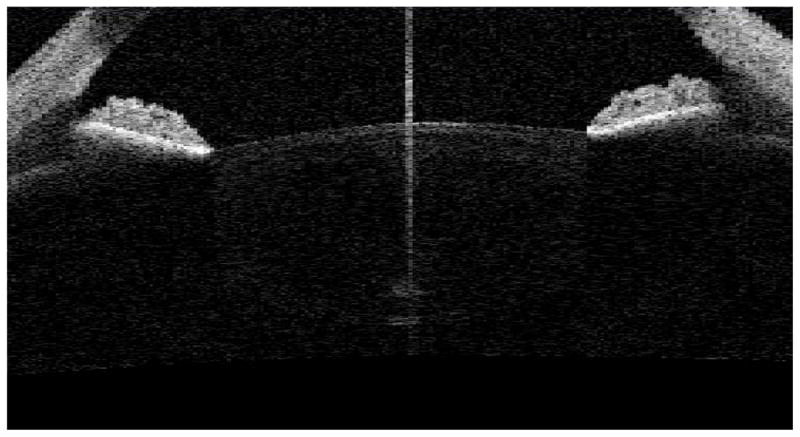
An image of the crystalline lens captured by the Visante OCT in anterior segment single scanning mode Version 1.0. The central, vertical white line is the “corneal reflex” according to the manufacturer.
The Visante OCT software available for this study was designed to measure the ocular components in the anterior chamber and the cornea. In order to obtain an image of the entire crystalline lens, the focus of the instrument must be moved posterior to the cornea. If no adjustments are made, Version 1.0 of the software attempts to locate the cornea by designating both anterior and posterior corneal surfaces arbitrarily on the anterior portion of the crystalline lens. The software assigns a refractive index of 1.000 (air) for all structures anterior to the anterior corneal boundary, 1.388 (cornea) for all structures within the corneal boundaries, and 1.343 (aqueous) for all structures posterior to the posterior corneal boundary. To eliminate this problem, the refractive index of the entire image was set at 1.388 (cornea) because this is the refractive index available in the Visante software that is the closest to the indices of the crystalline lens. This was accomplished by clicking “surfaces” under the “edit tab.” The entire anterior corneal boundary was placed at the top of the screen, and the entire posterior corneal boundary was placed at the bottom of the screen. Lens thickness measurements were made only after these changes were completed.
Statistical Analysis
Statistical analyses were performed using SPSS, version 15.0 (SPSS Inc, Chicago, Illinois). Validity was determined by comparing the average of the five A-scan measurements of each subject to the average of the three Visante OCT measurements of the same subject at visit one. The means were compared using a two-tailed paired t-test and the difference between the means was compared to zero. Intersession repeatability of the Visante OCT was assessed by comparing the average of three measurements of crystalline lens thickness at the first visit to three measurements of crystalline lens thickness at the second visit. Repeatability was assessed using difference versus mean plots as described by Bland and Altman.12 Bias of the method can be characterized by comparing the mean difference between the instruments to zero. The degree of repeatability is expressed by the 95% limits of agreement (mean ± [1.96 × standard deviation]).
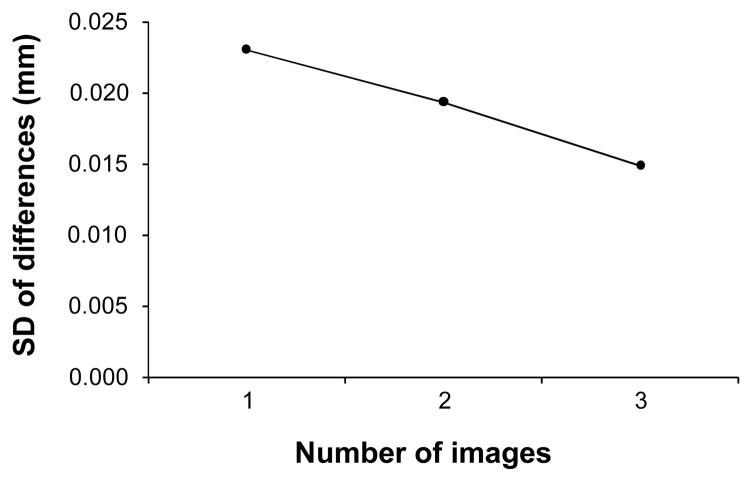
To determine whether all three Visante OCT lens images were necessary to obtain the level of repeatability that we report, we examined the improvement in intersession repeatability as the number of images with the corneal reflex beam present increased. This was done by plotting the standard deviation of the differences between visits as a function of the number of Visante OCT images taken.
RESULTS
Forty-seven subjects completed the first visit, and thirty-eight subjects returned for a second visit. The mean age (± standard deviation [SD]) of the subjects was 11.1 ± 2.3 years (range 8 to 15 years). The mean spherical equivalent refraction, as measured by cycloplegic autorefraction, was −1.21 ± 2.33 D (mean ± SD). Of the 47 subjects, 22 were myopes and 25 were non-myopes. Myopia is defined as greater than −0.75D of myopia in both meridians.
Validity of Visante OCT Measurements
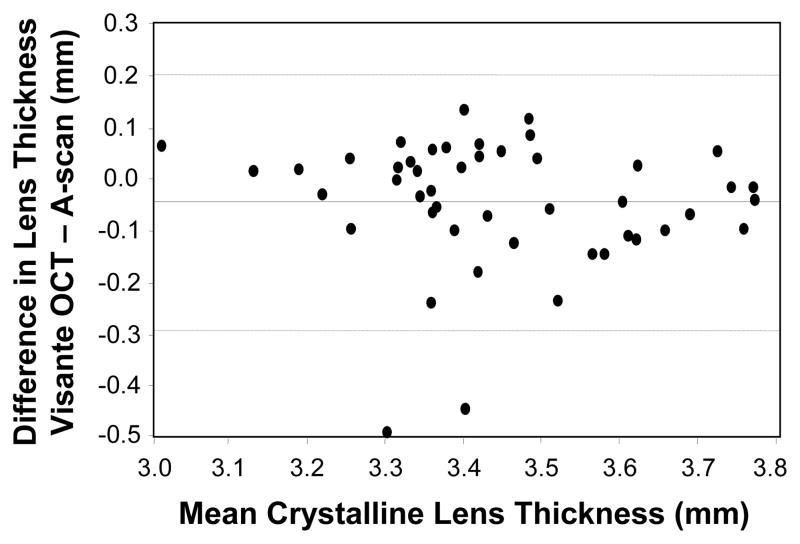
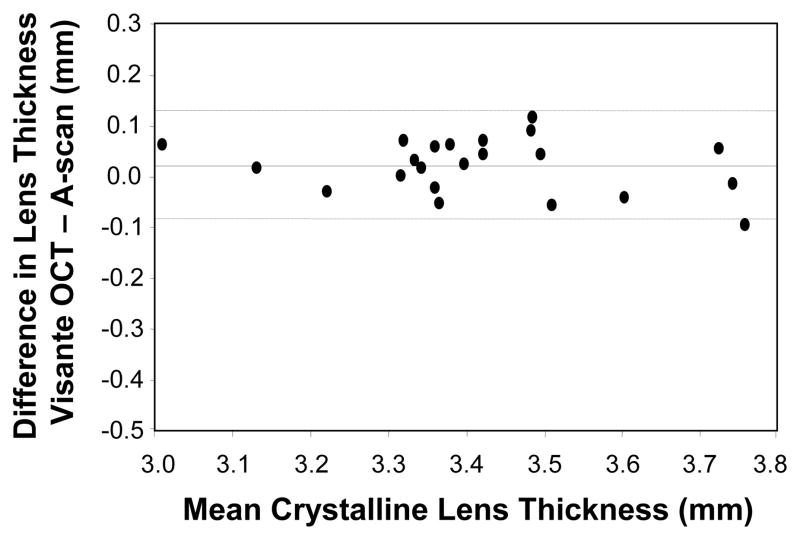
The mean crystalline lens measurement by A-scan ultrasonography was significantly thicker than that measured with the Visante OCT (t46 = 2.49, p = 0.017). Figure 2 is a difference versus mean plot for the two crystalline lens thickness measurements as suggested by Bland and Altman (1986).12 The mean of the difference in crystalline lens thickness between the Visante OCT and A-scan ultrasonography was −0.045 mm with 95% limits of agreement from −0.29 to 0.20 mm. When validity was reassessed using only the Visante images that contained the corneal reflex, the mean of the differences was 0.019 mm with 95% limits of agreement from −0.09 to 0.13 mm, and this was not a statistically significant difference (t21 = −1.66, p = 0.11). Figure 3 is a plot of the validity of the Visante OCT using only the images that contain the corneal reflex. Descriptive statistics are shown in Table 1.
Figure 2.
Bland-Altman difference versus mean plot (Visante OCT – A-scan; n = 47). The mean difference (solid line) was significantly different from zero (p = 0.017). The dashed lines outline the 95% limits of agreement.
Figure 3.
Bland-Altman difference versus mean plot (Visante OCT – A-scan) for only the images where a corneal reflex was visible (n = 22). The mean difference (solid line) was not significantly different from zero (p = 0.11). The dashed lines outline the 95% limits of agreement.
Table 1.
Means and standard deviations for the A-scan ultrasound and the Visante OCT.
| A-scan | Visante OCT | |||||
|---|---|---|---|---|---|---|
| Mean (mm) | ±SD | Mean (mm) | ±SD | Mean (mm) | ±SD | |
| Validity | ||||||
| All images (n=47) | 3.47 | 0.19 | 3.42 | 0.18 | ||
| Images with corneal reflex (n=22) | 3.40 | 0.20 | 3.42 | 0.19 | ||
| Repeatability | visit one | visit two | ||||
| All images (n=38) | 3.47 | 0.18 | 3.47 | 0.18 | ||
| Images with corneal reflex (n=25) | 3.44 | 0.18 | 3.44 | 0.18 | ||
Repeatability of Visante OCT Measurements
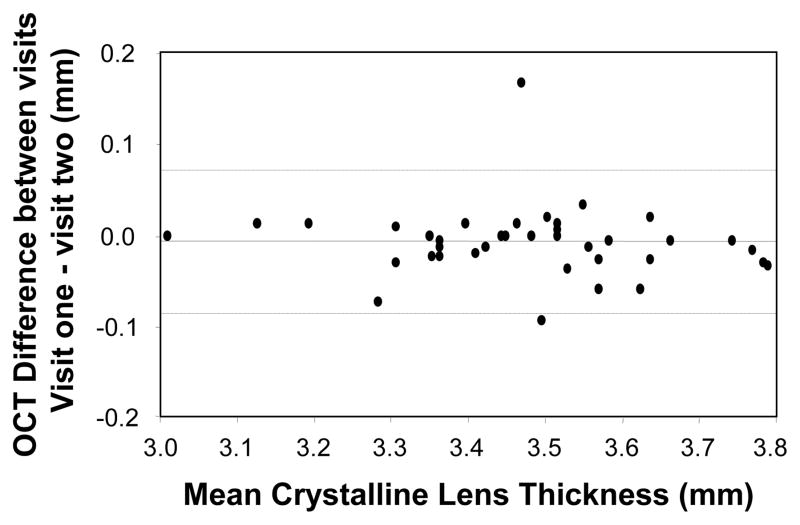
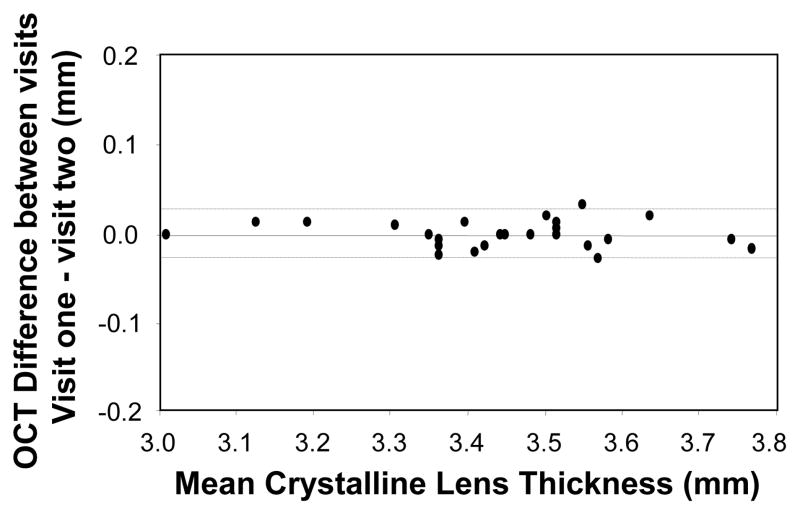
The mean crystalline lens thickness measured at visit one was not significantly different from that measured at the second visit (t37 = −1.16, p = 0.25). The mean of the differences in crystalline lens thickness between visits was −0.008 mm with 95% limits of agreement from −0.088 to 0.072 mm. Figure 4 is a plot of the repeatability of all crystalline lens thickness measurements made with the Visante OCT. When repeatability was reassessed using only the images that contained the corneal reflex, the mean of the differences between visits decreased to −0.0001 mm with 95% limits of agreement from −0.03 to 0.03, which was not statistically significant (t24 = −0.040, p = 0.97). Figure 5 is a plot of the between-visit repeatability of crystalline lens thickness measurements made with the Visante OCT when only images with a corneal reflex were considered.
Figure 4.
Bland-Altman difference vs. mean plot of the between-visits repeatability of the Visante OCT (visit one – visit two) for subjects with measurements at two visits (n = 38). The dashed lines outline the 95% limits of agreement.
Figure 5.
Bland-Altman difference vs. mean plot of the between-visits repeatability of the Visante OCT (visit one – visit two) for only the images where a corneal reflex was visible (n =25). The mean difference (solid line) was not significantly different from zero (p = 0.97). The dashed lines outline the 95% limits of agreement.
Figure 6 is a plot of the repeatability of Visante OCT lens measurements (the standard deviation of the differences between visits) as a function of the number of images. The best repeatability was obtained when all three images per session were included; therefore, to obtain the repeatability that we report, at least three lens images with the corneal reflex present must be obtained. Additional improvement in repeatability may be possible with additional images; however, the limits of agreement with three images (± 0.03 mm) are already superior to those found with ultrasonography.
Figure 6.
Plot of repeatability (standard deviation of the differences between visits) as a function of the number of Visante OCT lens images obtained that contained the corneal reflex beam.
DISCUSSION
Accurate measurements of optical dimensions of the eye are important to studies in the development of refractive error, crystalline lens growth, presbyopia, and cataract surgery. The repeatability of partial coherence interferometry measurement techniques has been shown to be better than A-scan ultrasound for axial length measurements.13 In our study, we demonstrated validity and excellent repeatability through a novel use of the Visante OCT to measure the thickness of the crystalline lens.
A-scan ultrasonography is currently used widely in pediatric research14–16 and the instrumentation is typically more readily available than other systems that can measure crystalline lens thickness, such as a Scheimpflug camera. Still, one might consider it to be disadvantageous in a study of children due to the use of local anesthetics and direct physical contact with the eye. In addition, the applanation technique may cause corneal indention and distort ocular component measurements.17 Moreover, there is no landmark to provide precise measurement of the same axial dimension. It is imperative to make precise axial measurements, based on geometric optics and the Gullstrand #1 model eye, where a change of approximately ± 0.4 mm in axial length around emmetropia is equivalent to approximately a 1.00-D refractive change. It has previously been reported that repeatability for ocular components should be within ± 0.1 mm.18, 19 The repeatability of the A-scan ultrasound for the measurement of crystalline lens thickness has been previously reported, and a summary is displayed in Table 2. Although the statistical analyses used across the studies in Table 2 are not consistent, all studies show repeatability greater than ± 0.1 mm. In addition, Kurtz et al. showed that the A-scan is sensitive to lens thickness changes only if they exceed 1.00 D using the conventional hand-held technique.4 For the reasons stated above, a more accurate measurement technique may be advantageous and necessary to effectively study lens thickness changes.
Table 2.
Repeatability of A-scan ultrasonography.
| Research Group | Year | Repeatability* |
|---|---|---|
| Rudnicka23 | 1992 | ± 0.120 |
| Optimum Accuracy per manufacturer 23 | 1991 | ± 0.134 |
| Jansson25 | 1963 | ± 0.135 |
| Storey & Rabie26 | 1983 | ± 0.160 |
| Zadnik27 | 1992 | ± 0.200 |
1.96 × standard deviation of mean differences
Index of Refraction
The Gullstrand #2 Simplified Schematic Eye establishes a refractive index for the crystalline lens at 1.413. The Gullstrand #1 Exact Eye creates a heterogeneous lens with an index of 1.386 for the cortex and 1.406 for the nucleus.20 In vivo, the crystalline lens has a gradient refractive index that increases from the cortex to the nucleus. Assigning one or even two refractive indices to the crystalline lens is not physiologically accurate. We are aware that the index assigned by the Visante OCT is neither equivalent to the lens refractive indices in the schematic eyes nor to the refractive indices of our subjects’ crystalline lenses. However, the index of refraction assigned to the cornea by the Visante software is 1.388, which is the closest option available to the estimated Gullstrand values. By extending the boundary limits of the cornea in the Visante OCT software, an index of refraction of 1.388 could be applied to the entire crystalline lens.
Variability of the Visante OCT in Crystalline Lens Thickness
Ocular accommodation has been shown to increase the variability of lens thickness measured by A-scan ultrasound.21 Therefore, adequate cycloplegia is necessary for repeatable crystalline lens thickness measurement. Cycloplegia was achieved with the instillation of 1% tropicamide as described in the literature.22 In comparison to A-scan ultrasound, the Visante OCT produced significantly thinner measurements of crystalline lens thickness when the corneal reflex was not present in the Visante OCT image, although the difference of 0.045 mm was less than the best-reported repeatability of A-scan ultrasonography.23 One hypothesis that might explain this result is that the refractive index assigned to the crystalline lens (1.388) using the Visante OCT software was slightly greater than the refractive index underlying the assumptions made in A-scan ultrasonography, causing the Visante OCT lens thickness measurements to be slightly thinner. This is inferred from the following formula: Thickness = Optical Path Length ÷ index of refraction.
Another possible reason for the small difference found could be that an off-axis portion of the crystalline lens was measured with either of the devices, resulting in a slight error in the thickness measurement. An off-center measurement produces a smaller measurement, and an oblique measurement produces a thicker or thinner result. This error can be minimized with the Visante OCT by capturing images with the corneal reflex and measuring the axial dimension of the thickest part of the lens closest to the reflex. In contrast, an off-center measurement is difficult to minimize with A-scan ultransonography because there is no way to ensure that the thickest portion of the lens is consistently measured. In addition, the A-scan assumes a specific velocity of sound as the sound waves pass through the ocular media. If the assumed velocity of sound in the crystalline lens is the same as the actual velocity, the measurement made by the A-scan will be physiologically accurate. This is of particular interest when studying children because the velocity of sound through a child’s crystalline lens may differ slightly from the velocity of sound through an adult’s crystalline lens.
Finally, the known repeatability of the A-scan biometry for the measurement of crystalline lens thickness ranges from ±0.120 to ±0.200 mm,23 demonstrating that A-scan measurements are less precise than the Visante OCT in this study. This means that if this experiment was repeated, a different average thickness of the crystalline lens would possibly be found with A-scan measurements. The largest difference between the Visante OCT and the A-scan reported here (0.045 mm) may not be clinically meaningful because the difference is less than the reported repeatability of A-scan.
The A-scan ultrasound and the Visante OCT did not produce significantly different measurements of crystalline lens thickness when the results were analyzed using only Visante OCT images in which the corneal reflex was visible. The mean of the differences in crystalline lens thickness measurements between the instruments including all subjects was −0.045 mm as compared to 0.019 mm when only the images with a corneal reflex were analyzed. The non-significant difference between the instruments indicates that thetwo devices’ measurements were more similar when the corneal reflex is captured in the Visante OCT images. Because the mean value of the Visante OCT measurements did not change with or without the corneal reflex present, this may indicate that the small difference found using the larger sample was the result of the higher variability of A-scan measurements.
Repeatability of the Visante OCT in Crystalline Lens Thickness
The Visante OCT has excellent repeatability when measuring the cornea.24 The mean of the differences in Visante OCT crystalline lens thickness measurements between visits was not significant. The agreement between visits was much better in the subset of subjects that had a visible corneal reflex in all images (95% Limits of Agreement: ±0.030 mm compared to ±0.08mm.) To maximize repeatability, it is necessary to include the corneal reflex in crystalline lens images captured by the Visante OCT; however, even if the corneal reflex is not present in the image, the repeatability of the Visante OCT is better than that of A-scan ultrasonography.
Visante OCT Software Version 2.0
The Visante software has been updated since the data for this study were collected. In the current Visante software version, Version 2.0, the “anterior segment single” mode and built-in software caliper system cannot be used to measure the thickness of the crystalline lens. In Version 2.0, an image of the crystalline lens, i.e., an image in which the cornea is not visible, can only be obtained using a new “raw image mode” that applies a refractive index of 1.0 (air) to the entire image. The software calipers cannot be used when an image is made using the raw image mode. To verify that accurate measurements can still be made in Version 2.0, 20 images in air (n=1.00) of the crystalline lens containing the corneal reflex were exported as JPEG image files, and the images were opened in image processing software (Matrox Inspector 4.0; Matrox Electronic Systems Ltd.; Quebec, Canada). The thickness of the crystalline lens was measured in pixels and converted to millimeters using the conversion 1 mm = 51 pixels. This conversion was determined by exporting an image with refractive index set to air (1.0) with a 1-mm line drawn by the Visante software. The number of pixels in a millimeter was measured in the image processing software.
The result of applying a uniform refractive index to the entire image is a non-physiologic appearance within the aqueous and vitreous; however, with the method described above, no measurements are made outside of the lens. All measurements that we report are between two points along the longest axial dimension of the lens. Because OCT technology relies on optical path length when determining thicknesses, other structures in the image do not influence the optical path length through the crystalline lens, which is supported by our results.
In order to compare the measurement made with the Visante OCT software version 2.0 to version 1.0, the lens thickness measurement in millimeters, with an applied refractive index of 1.0, was converted to a refractive index of 1.388 (the index applied in version 1.0 of the Visante software). The two values were compared using a paired t-test. No significant difference was observed (p=0.12). Therefore, although external image processing is required to obtain lens thickness measurements with version 2.0 of the Visante software, the newer software still provides a viable method of obtaining the thickness of the crystalline lens.
CONCLUSIONS
Crystalline lens measurements made with the Visante anterior segment OCT were valid compared to those made with A-scan ultrasonography. Measurements made with the Visante OCT were also repeatable. The device is non-contact, easy to operate, and able to produce a detailed, 2-dimensional, high-resolution image of the crystalline lens. The best repeatability was achieved with the device when the corneal reflex was visible in the crystalline lens image (±0.030 mm). The best reported repeatability of A-scan ultrasonography is ±0.12 mm,23 four times larger than what was found for the Visante OCT in this study. The Visante OCT should be considered as an alternative to conventional A-scan ultrasound in ocular biometry studies involving the crystalline lens.
Acknowledgments
Supported by National Eye Institute, National Institutes of Health grants EY007151 and EY015447. We acknowledge the support of Vistakon and the American Optometric Foundation.
Footnotes
Presented, in part, as a paper at the American Academy of Optometry Annual Meeting, October 2007, Tampa Florida.
References
- 1.Mutti DO, Zadnik K, Fusaro RE, Friedman NE, Sholtz RI, Adams AJ. Optical and structural development of the crystalline lens in childhood. Invest Ophthalmol Vis Sci. 1998;39:120–33. [PubMed] [Google Scholar]
- 2.Zadnik K, Mutti DO, Fusaro RE, Adams AJ. Longitudinal evidence of crystalline lens thinning in children. Invest Ophthalmol Vis Sci. 1995;36:1581–7. [PubMed] [Google Scholar]
- 3.Garner LF, Yap MK, Kinnear RF, Frith MJ. Ocular dimensions and refraction in Tibetan children. Optom Vis Sci. 1995;72:266–71. doi: 10.1097/00006324-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz D, Manny R, Hussein M. Variability of the ocular component measurements in children using A-scan ultrasonography. Optom Vis Sci. 2004;81:35–43. doi: 10.1097/00006324-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Li H, Leung CK, Cheung CY, Wong L, Pang CP, Weinreb RN, Lam DS. Repeatability and reproducibility of anterior chamber angle measurement with anterior segment optical coherence tomography. Br J Ophthalmol. 2007;91:1490–2. doi: 10.1136/bjo.2007.118901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dada T, Sihota R, Gadia R, Aggarwal A, Mandal S, Gupta V. Comparison of anterior segment optical coherence tomography and ultrasound biomicroscopy for assessment of the anterior segment. J Cataract Refract Surg. 2007;33:837–40. doi: 10.1016/j.jcrs.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Wang N, Wang B, Zhai G, Lei K, Wang L, Congdon N. A method of measuring anterior chamber volume using the anterior segment optical coherence tomographer and specialized software. Am J Ophthalmol. 2007;143:879–81. doi: 10.1016/j.ajo.2006.11.051. [DOI] [PubMed] [Google Scholar]
- 8.Pinero DP, Plaza AB, Alio JL. Anterior segment biometry with 2 imaging technologies: very-high-frequency ultrasound scanning versus optical coherence tomography. J Cataract Refract Surg. 2008;34:95–102. doi: 10.1016/j.jcrs.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Li H, Leung CK, Wong L, Cheung CY, Pang CP, Weinreb RN, Lam DS. Comparative study of central corneal thickness measurement with slit-lamp optical coherence tomography and visante optical coherence tomography. Ophthalmology. 2008;115:796–801. e2. doi: 10.1016/j.ophtha.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Dunne MC, Davies LN, Wolffsohn JS. Accuracy of cornea and lens biometry using anterior segment optical coherence tomography. J Biomed Opt. 2007;12:064023. doi: 10.1117/1.2821844. [DOI] [PubMed] [Google Scholar]
- 11.Visante OCT User Manual: Model 1000: Carl Zeiss Meditec; 2006.
- 12.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 13.Carkeet A, Saw SM, Gazzard G, Tang W, Tan DT. Repeatability of IOLMaster biometry in children. Optom Vis Sci. 2004;81:829–34. doi: 10.1097/01.opx.0000145020.33250.c0. [DOI] [PubMed] [Google Scholar]
- 14.Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci. 2002;43:2852–8. [PubMed] [Google Scholar]
- 15.Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, Leske MC, Manny R, Marsh-Tootle W, Scheiman M. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 16.Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510–9. doi: 10.1167/iovs.06-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 2001;21:477–83. doi: 10.1046/j.1475-1313.2001.00611.x. [DOI] [PubMed] [Google Scholar]
- 18.Storey JK. The Marton Lecture: ultrasound in ophthalmic optics. Ophthalmic Physiol Opt. 1981;1:133–57. [PubMed] [Google Scholar]
- 19.Michaels DD. Optics, refraction, and visual function. Curr Opin Ophthalmol. 1992;3:69–70. doi: 10.1097/00055735-199202000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Rabbetts RB. Bennett & Rabbetts’ Clinical Visual Optics. 3. Butterworth-Heinemann; 1998. [Google Scholar]
- 21.Steele CF, Crabb DP, Edgar DF. Effects of different ocular fixation conditions on A-scan ultrasound biometry measurements. Ophthalmic Physiol Opt. 1992;12:491–5. [PubMed] [Google Scholar]
- 22.Egashira SM, Kish LL, Twelker JD, Mutti DO, Zadnik K, Adams AJ. Comparison of cyclopentolate versus tropicamide cycloplegia in children. Optom Vis Sci. 1993;70:1019–26. doi: 10.1097/00006324-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Rudnicka AR, Steele CF, Crabb DP, Edgar DF. Repeatability, reproducibility and intersession variability of the Allergan Humphrey ultrasonic biometer. Acta Ophthalmol (Copenh) 1992;70:327–34. doi: 10.1111/j.1755-3768.1992.tb08573.x. [DOI] [PubMed] [Google Scholar]
- 24.Mohamed S, Lee GK, Rao SK, Wong AL, Cheng AC, Li EY, Chi SC, Lam DS. Repeatability and reproducibility of pachymetric mapping with Visante anterior segment-optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48:5499–504. doi: 10.1167/iovs.07-0591. [DOI] [PubMed] [Google Scholar]
- 25.Jansson F. Measurement of intraocular distances by ultrasound and comparison between optical and ultrasonic determinations of the depth of the anterior chamber. Acta Ophthalmol (Copenh) 1963;41:25–61. doi: 10.1111/j.1755-3768.1963.tb02420.x. [DOI] [PubMed] [Google Scholar]
- 26.Storey JK, Rabie EP. Ultrasound a research tool in the study of accommodation. Ophthalmic Physiol Opt. 1983;3:315–20. [PubMed] [Google Scholar]
- 27.Zadnik K, Mutti DO, Adams AJ. The repeatability of measurement of the ocular components. Invest Ophthalmol Vis Sci. 1992;33:2325–33. [PubMed] [Google Scholar]