Abstract
The use of illegal drugs is common in alcohol dependence and significant psychological and social consequences are associated with the concurrent use of alcohol and illegal drugs. However, little literature has examined the patterns of concurrent drug use in alcohol dependent individuals. A latent class analysis (LCA) was used to determine whether patterns of past year illegal drug use existed in a national sample of 6,059 alcohol dependent respondents of the combined 2005, 2006 and 2007 National Survey on Drug Use and Health. Multinomial logistic regression was then used to determine whether demographic variables, mental health disturbance and social consequences were predictive of drug use classes. Results of the LCA demonstrated a five class solution with optimal fit deduced by Bayesian Information Criterion minima. The five classes included: a close to zero probability of illegal drug use (class 1: 65%), medium marijuana, medium sedatives/tranquilizers and high analgesics (class 2: 7%), high marijuana, medium cocaine use (class 3: 21%), high probabilities of marijuana, cocaine, sedatives and analgesic use (class 4: 6%) and a high concurrent drug use except other hallucinogens (class 5: 1%). Regression results suggest that younger age, comorbidity, engaging in deviant behaviors, sexually transmitted infection and incarceration are associated with concurrent illegal drug use in alcohol dependent individuals. Findings advocate that more intense psychiatric and drug dependence treatment resources may be needed for concurrent drug using alcohol dependent populations and provide evidence for targeted prevention and treatment interventions.
Keywords: comorbidity, latent class analysis, epidemiology, sexually transmitted disease, risk factors
1. Introduction
The majority of alcohol dependent individuals use more substances than alcohol. In the alcohol dependence literature, concurrent lifetime diagnosis of another substance dependency is 64% and reports of past 90 day use of illegal drugs are 68% (Staines et al., 2001). Among alcohol dependent individuals, concurrent cocaine, benzodiazepine, marijuana and heroin use are common ranging from 30 to 60%, 12 to 20%, 20 to 50% and 7 to 10%, respectively (Midanik et al., 2007; Petry, 2001). Many adults with alcohol dependence have multiple drug use disorders (Hasin et al., 2007; Staines et al., 2001).
Co-occurring alcohol disorder and drug use have been associated with greater frequency of alcohol use and alcohol disorder (Midanik et al., 2007), problems associated with the treatment and remission of alcohol disorder (Karno, 2008; Ives and Ghelani, 2006) as well as greater prevalence of psychological and social harms (Hedden et al., 2009). Although the use of illegal drugs is common in alcohol dependence and significant psychological and social consequences are associated with the concurrent use of alcohol and illegal drugs, very little systemic research on the heterogeneity of concurrent-drug use in alcohol dependent individuals exists (Ives and Ghelani, 2006; Staines et al., 2001).
Whereas, extant research has classified subtypes of drug use in various populations (Agrawal et al., 2007; Lynskey et al., 2006; Cuffel et al., 1993; Hasin et al., 2007; Regier et al., 1990; Whitesell et al., 2006; Stinson et al., 2005) few studies have focused on subtypes of concurrent-drug users in the adult alcohol dependent population. Existing studies of concurrent drug use in alcohol dependent individuals often categorize individuals as concurrent drug users without differentiating between drug type (Curran et al., 2008; Karno et al., 2008). Studies on concurrent drug use in alcohol dependence which do differentiate between drug type often focus on a particular illegal drug of interest such as alcohol and the concurrent use of marijuana (Norton and Colliver, 1988) or cocaine (Brady et al., 1995; Grant and Harford, 1990; Hedden et al., 2009).
Studies of concurrent drug use have demonstrated that the use of alcohol in combination with other drugs has been associated with more severe psychological and social consequences than alcohol abuse or dependence alone (Hedden et al., 2009; Brady et al., 1995). For example, Brady and colleagues found that cocaine dependent individuals in treatment who abuse alcohol were more likely to exhibit cocaine related psychosis and had higher Hamilton Depression scores compared to cocaine dependent patients that did not abuse alcohol (Brady et al., 1995). Also, among persons reporting alcohol or drug abuse/dependence, comorbid mental disorders including anxiety and mood/affective disorders are common (Grant et al., 2004; Hasin et al., 2007; Merikangas et al., 1998; Regier et al., 1990). Kandel and colleagues demonstrate that the odds of mental health co-morbidities such as anxiety and depression are double for individuals who report dependency on both alcohol and illegal drug use compared to individuals with single dependency (Kandel et al., 2001). In individuals receiving treatment for heroin, cocaine and/or alcohol, affective and antisocial personality disorders were more likely in individuals with 2 or more dependencies compared to individuals with single dependency (Conway et al., 2003).
Also, adverse social consequences such a sexually transmitted infection and incarceration are more likely in individuals with co-occurring substance use disorders (Hedden et al., 2009; Midanik et al., 2007; Heil et al., 2001). For example, Heil and colleagues demonstrated that cocaine dependent alcoholics were more likely to report adverse consequences from use, including violent impulses and unwanted sexual relations (Heil et al., 2001). Using 7,612 individuals from the 2000 National Alcohol Survey, simultaneous use of alcohol with other drugs was associated with social consequences including legal problems, accidents and health problems (Midanik et al., 2007). Using the 2005 NSDUH, Hedden and colleagues demonstrated that concurrent alcohol and cocaine users were more likely to report lifetime sexually transmitted infections (STIs) and incarceration compared to single users (Hedden et al., 2009).
Literature suggests that individuals with concurrent abuse or dependence of alcohol and illegal drug use may differ from those with alcohol abuse or dependence alone. Particularly, differences in psychiatric disorders and social consequences have been described. However, no study to our knowledge has looked at psychological and social consequence as related to patterns of drug use in alcohol dependent individuals. Therefore, this study assessed the patterns of multiple illegal drugs of use in a nationally representative sample of an alcohol dependent adult population aged 18 years and older using the combined datasets from the 2005, 2006 and 2007 National Survey on Drug Use and Health (NSDUH). Illegal drug use included: marijuana, cocaine, non-prescription use of stimulants, ecstasy, other hallucinogens, non-prescription use of sedatives or tranquilizers and non-prescription use of opioid analgesics. Furthermore, correlates of concurrent drug use including demographic variables, psychiatric disorders and social consequences were assessed. It was hypothesized that classes of alcohol dependent individuals with greater concurrent drug use (i.e. high probabilities of multiple types of drug use) would have more extreme psychological and social consequences.
2. Methods
2.1 Sample
Data were from the combined 2005–2007 datasets of the NSDUH (Substance Abuse and Mental Health Services Administration, 2006; Substance Abuse and Mental Health Services Administration, 2007; Substance Abuse and Mental Health Services Administration, 2008). The NSDUH is a series of cross-sectional surveys sponsored by the Substance Abuse and Mental Health Administration whose primary purpose is to measure the prevalence and correlates of drug use among the general population in the United States. The target population was non-institutionalized participants who were 12 years and older. The sampling design used an independent multistage area probability sample for each of the 50 states and the District of Columbia. The survey used computer assisted self-interviewing (CAI) techniques: a combination of computer assisted personal interviewing conducted by interviewers and audio assisted self-interviewing. Final samples of 68,308, 67,802 and 67,870 CAI interviews were obtained with a weighted CAI response rate of 76%, 74% and 74% for 2005, 2006 and 2007, respectively. An incentive of $30 was given for participation. Further description of the sampling methods for the 2005–2007 NSDUH are found elsewhere (Substance Abuse and Mental Health Services Administration, 2006; Substance Abuse and Mental Health Services Administration, 2007; Substance Abuse and Mental Health Services Administration, 2008).
The domain of interest was past year alcohol dependent adult (18 years or older) individuals (n=6,059). Participants meeting past year alcohol dependence for the 2005, 2006 or 2007 NSDUH datasets included 2,023, 1,990, and 2,046 of the sample, respectively. Alcohol dependence was defined based upon meeting 3 of the 7 criteria listed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 1994).
2.2 Measures
Past year drug use was assessed via self-report for each cross-sectional survey, 2005–2007. Participants who reported using the listed drugs in either the 2005, 2006 or 2007 NSDUH were considered positive for “Illegal Drug Use”. Specifically, participants were asked whether they had engaged in any of the following forms of illegal drug use during the past year: 1) marijuana, 2) cocaine, 3) ecstasy, 4) other hallucinogens, and non-prescription use of 5) stimulants, 6) sedatives or tranquilizers, and 7) opioid analgesics. Seven binary (past year use=1, no past year use=0) indicators of illegal drug use were created. Past year use of heroin was not included in the analyses given its infrequency of use for this sample (raw n=88, weighted percent=1.5%).
Demographic variables included: gender, race/ethnicity, age, education status and income. Due to sample size consideration, race/ethnicity was aggregated into the following levels: Caucasian, African American, Hispanic or other. Age was aggregated into the categories of 18–25 years, 26–34 years, and greater than 35 years of age. Education status was grouped into the following categories: less than high school, high school, some undergraduate school, and undergraduate/graduate school. Annual income levels consisted of less than $20,000, $20,000–$49,000, $50,000–$74,999 and greater than $75,000.
Psychological disorders included lifetime generalized anxiety disorder (GAD) and major depressive disorder (MDD) and were assessed by participant self-reports of previous diagnosis by a medical doctor or health care professional. ‘Deviant behaviors’ were assessed and used as a proxy for conduct disorder. Specifically, a measure of deviant behavior was assessed using the survey questions: “During the past 12 months, how many times have you attacked someone with the intent to seriously hurt them?”, “During the past 12 months, how many times have you sold illegal drugs”, and “During the past 12 months, how many times have you stolen or tried to steal anything worth more than US $50?”. Participants who self-reported any of the three behaviors were categorized as having ‘deviant behavior’ (Martins et al., 2006). Other variables included self-reports of lifetime sexually transmitted infection (STI), incarceration and treatment for alcohol/drug use.
2.3 Statistical Analysis
All analyses were performed via SAS version 9.1 and MPLUS version 5 using the sampling weights and complex survey design measures. Descriptive statistics were used to describe the sample. Specifically, counts and percentages were used to describe categorical variables.
Hierarchical latent class analysis (LCA) accounting for the complex sampling design was used to explain heterogeneity of concurrent drug use in the adult alcohol dependent sample (Hagenaars and McCutcheon, 2002). LCA, a method of data reduction that allows for non-additive associations among illegal drug use, was used to identify latent class patterns of adult alcohol dependent individuals with similar concurrent drug use profiles. In order to determine the model with the optimal number of classes, models were run with between 1 and 6 classes and evaluated. The model with the number of classes associated with minimum values of fit statistics including, Akaikes Information Criterion (AIC), Bayesian Information Criterion (BIC) and Sample Size Adjusted BIC (ABIC) was chosen (Nylund et al., 2007). The BIC was given priority over other fit statistics given its optimal performance in simulation studies (Nylund et al., 2007). The optimal latent class model was checked for model fit and model assumptions including conditional independence (Garrett and Zeger, 2000). Specifically, conditional independence was tested by estimating class conditional odds ratios and 95% confidence intervals for each of the bi-variable combinations. Model identifiability was checked intrinsically and then empirically by including multiple random starting values in order to avoid local solutions that may not reflect global maximum likelihood (Muthen and Muthen, 2007). Once the number of classes was determined, correlates including demographics, psychological and social consequences were added to multinomial regression models singly and then multiply.
To account for classification error, the latent class probabilities were exported into SAS 9.1 and then used to output class indices for 20 independent datasets using a random uniform number generator to simulate a multinomial distribution. Each of the 20 outputted data sets were analyzed and estimates were combined using Rubin’s rules for combining estimates (Rubin, 1987).
3. Results
Demographic characteristics of the adult alcohol dependent sample are listed in Table 1. Most of the alcohol dependent sample was male (66%) and white (68%), older than 35 years of age, and had undergraduate school and graduate school (48%) as highest education level. The most prevalent illegal drug of use was marijuana (41%), followed by non-prescription use of opioid analgesics (23%), cocaine (19%), non-prescription use of sedatives and tranquilizers (12%), non-prescription use of stimulants (7%), ecstasy (5%) and other hallucinogens (5%).
Table 1.
Characteristics of Adult Alcohol Dependent Individuals (n=6,059), NSDUH 2005–2007
| Characteristic | N (%) |
|---|---|
| Gender | |
| Female | 2450 (33.9) |
| Male | 3609 (66.2) |
| Age | |
| 18–25 | 4040 (31.6) |
| 26–34 | 818 (21.6) |
| >34 | 1201 (46.8) |
| Race | |
| White | 4021 (68.0) |
| African American | 590 (12.4) |
| Hispanic | 550 (4.7) |
| Other | 898 (14.8) |
| Education | |
| < High School | 1216 (18.7) |
| High School | 2048 (33.1) |
| College | 2795 (48.2) |
| Income | |
| <$20K | 2108 (28.6) |
| $20K–$49K | 2175 (35.4) |
| $50K–$75K | 731 (13.3) |
| >75K | 1045 (22.7) |
| Lifetime Anxiety | |
| No | 5015 (84.3) |
| Yes | 916 (15.8) |
| Lifetime Depression | |
| No | 4593 (76.8) |
| Yes | 1338 (23.2) |
| Past-year Deviant Behavior | |
| No | 4595 (83.7) |
| Yes | 1425 (16.3) |
| Lifetime STD | |
| No | 5468 (92.6) |
| Yes | 463 (7.4) |
| Lifetime Incarceration | |
| No | 3410 (53.9) |
| Yes | 2639 (46.1) |
| Alcohol Dependence Criteria | |
| three | 3006 (46.0) |
| four | 1587 (27.4) |
| five to seven | 1466 (26.6) |
| Ever in Tx for ETOH or Drugs | |
| No | 4464 (70.1) |
| Yes | 1579 (30.0) |
N represent raw numbers and % represent weighted percentages
An identified latent class model indicated that a five class model was optimal. Fit statistics were computed for the 1 to 6 class models. The number of classes was chosen using theoretical reasoning, fit statistics and practical consideration. The fit statistics of AIC (28,405.2), BIC (28,666.8) and ABIC (28,542.9) were lower for the 5-class compared to the 4-class model (AIC=28,490.5; BIC=28,698.5; ABIC=28,600.0) and similar to the 6-class model (AIC=28,376.2; BIC=28,691.6; ABIC=28,542.2). The BIC was lowest for the 5 class model as opposed to the 6 class model suggesting that the minimum fit index value occurred for the 5 class solution (Nylund, 2007). Furthermore, the ABIC value was not differentiated in the 5 and 6 class model. The parsimonious 5 class solution was chosen over the 6 class solution due to production of the minimum BIC fit statistic. In addition to picking the model with good fit statistics, the five class model was chosen over the four class model because the five class model differentiated between high concurrent drug users who had high probabilities of all illegal drug use except other hallucinogens and high concurrent drug users who had high probabilities of all illegal drugs except ecstasy and stimulants. The entropy value for the 5 class model was approximately, 0.7.
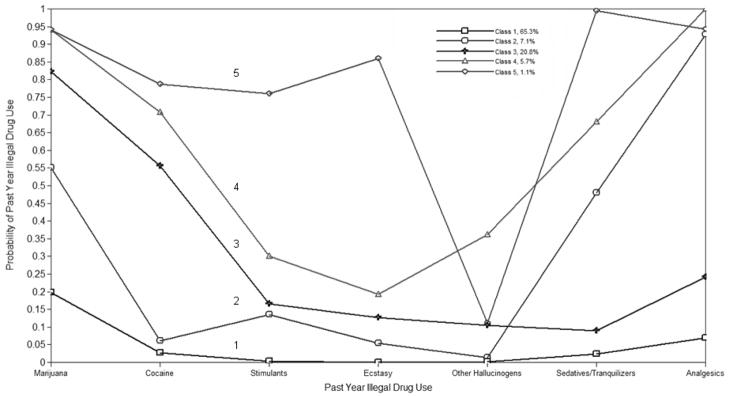
Figure 1 plots the past year illegal drug use on the x-axis and the probability of past year use of each drug for the five classes as indicated on the y-axis. The probabilities of endorsing past year illegal drug use are plotted for the seven illegal drugs for each of the five classes. The five class solution included a ‘no illegal drug use’ class (class 1) consisting of 65% of the adult alcohol dependent sample and included participants with near zero probabilities of past year illegal drug use. Class 2, consisting of 7% of the sample of adults with alcohol dependence, had medium probabilities of marijuana use, medium probabilities of non-prescription sedative/tranquilizer use and high probabilities of non-prescription analgesic use. Class 3, consisting of 21% of the sample, included individuals with high probabilities of marijuana use and medium probabilities of cocaine use. Two high concurrent-drug use classes emerged: Class 4 and Class 5. Class 4 included adults with alcohol dependence (6%) with high probabilities of marijuana, cocaine, non-prescription tranquilizers/sedatives and non-prescription analgesic use. Class 5 was the smallest class consisting of 1% of the sample and was characterized as adults with alcohol dependence with high probabilities of each illegal drug except other hallucinogens.
Figure 1.
Conditional Probabilities of Adult Alcohol Dependent Participants Based on a 5-Class Latent Class Analysis (n=6,059)
Table 2 demonstrates the sample characteristics of the adults with alcohol dependence by latent class, given the five class solution. Participants in Class 1 are less likely to report lifetime MDD, GAD, deviant behavior, having an STI and been incarcerated compared to the concurrent drug using classes. Also, participants in Classes 2, 4 and 5 were most likely to report having had lifetime MDD and GAD compared to participants in Class 1. Participants in Class 5 were most likely to report GAD (26%), MDD (40%) and deviant behavior (68%). Compared to the other concurrent-drug using classes participants in class one are less likely to have been in treatment for alcohol or drug use (27%). Although all individuals in the study met alcohol dependence criteria, individuals in class 1 were more likely to report meeting 3 criteria and were less likely to report meeting 5+ criteria compared to all other classes. Furthermore, the heaviest concurrent-drug use class, Class 5, was more likely to have been in treatment for alcohol or drug use compared to all other classes.
Table 2.
Characteristics of Adult Alcohol Dependent Individuals by Concurrent Drug Use Class, NSDUH 2005 to 2007
| Characteristic, N (%) | Class 1 | Class 2 | Class 3 | Class 4 | Class 5 |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 1397 (33.4) | 222 (40.4) | 590 (32.1) | 198 (36.5) | 44 (39.1) |
| Male | 2122 (66.6) | 256 (59.7) | 888 (67.9) | 288 (63.5) | 55 (60.9) |
| Age | |||||
| 18–25 | 2063 (24.5) | 361 (42.2) | 1115 (40.7) | 417 (61.1) | 85 (65.6) |
| 26–34 | 539 (21.2) | 56 (22.5) | 172 (22.8) | 43 (19.4) | 9 (26.5) |
| >34 | 917 (54.3) | 62 (35.3) | 191 (36.5) | 27 (19.5) | 4 (7.8) |
| Race | |||||
| White | 2230 (67.0) | 355 (73.8) | 973 (66.6) | 385 (75.4) | 77 (87.1) |
| African American | 387 (13.1) | 29 (6.7) | 148 (14.0) | 23.4 (7.8) | 3 (2.9) |
| Hispanic | 332 (5.3) | 36 (4.0) | 144 (4.0) | 29 (2.5) | 8 (3.6) |
| Other | 569 (14.7) | 58 (15.5) | 213 (15.5) | 49 (14.2) | 10 (6.3) |
| Education | |||||
| < High School | 673 (18.3) | 101 (20.0) | 304 (18.9) | 112 (21.1) | 25 (18.9) |
| High School | 1186 (32.6) | 161 (31.6) | 492 (34.0) | 170 (35.5) | 39 (40.7) |
| College | 1660 (49.1) | 216 (48.5) | 681 (47.1) | 204 (43.3) | 34 (40.5) |
| Income | |||||
| <$20K | 1155 (26.0) | 167 (30.4) | 563 (32.9) | 190 (37.8) | 33 (38.4) |
| $20K–$49K | 1297 (36.4) | 167 (33.3) | 518 (34.1) | 158 (32.1) | 36 (34.3) |
| $50K–$75K | 442 (13.9) | 58 (11.5) | 162 (12.7) | 58 (11.7) | 11 (8.6) |
| >75K | 624 (23.7) | 87 (24.8) | 235 (20.2) | 80 (18.4) | 19 (18.6) |
| Lifetime Anxiety | |||||
| No | 2995 (85.9) | 365 (77.4) | 1228 (83.9) | 356 (76.6) | 72 (74.0) |
| Yes | 454 (14.1) | 103 (22.6) | 217 (16.1) | 118 (23.4) | 24 (26.0) |
| Lifetime Depression | |||||
| No | 2740 (77.7) | 329 (70.2) | 1134 (79.2) | 327 (68.6) | 63 (60.0) |
| Yes | 709 (22.3) | 139 (29.8) | 311 (20.8) | 147 (31.4) | 33 (40.1) |
| Past-Year Deviant Behavior | |||||
| No | 2999 (90.5) | 329 (75.5) | 1006 (75.3) | 231 (53.9) | 31 (32.0) |
| Yes | 504 (9.5) | 147 (24.5) | 458 (24.7) | 250 (46.1) | 66 (68.0) |
| Lifetime STD | |||||
| No | 3224 (93.6) | 428 (92.2) | 1301 (90.1) | 430 (92.0) | 86 (84.8) |
| Yes | 225 (6.4) | 40 (7.8) | 143 (9.9) | 44 (8.0) | 10 (15.2) |
| Lifetime Incarceration | |||||
| No | 2127 (57.7) | 261 (49.4) | 762 (47.9) | 214 (40.3) | 47 (45.8) |
| Yes | 1384 (42.3) | 217 (50.6) | 715 (52.1) | 272 (59.7) | 51 (54.2) |
| Alcohol Dependence Criteria | |||||
| three | 1878 (49.9) | 215 (36.5) | 672 (39.0) | 201 (39.6) | 40 (38.0) |
| four | 891 (27.0) | 130 (29.5) | 401 (27.8) | 140 (28.2) | 26 (25.7) |
| five to seven | 749 (23.1) | 134 (34.0) | 405 (33.2) | 145 (32.3) | 33 (36.3) |
| Ever in Tx for ETOH or Drugs | |||||
| No | 2728 (73.3) | 347 (67.8) | 1021 (63.2) | 310 (62.2) | 58 (59.9) |
| Yes | 786 (26.7) | 130 (32.2) | 451 (36.8) | 172 (37.8) | 40 (40.1) |
Numbers and percentages represent combined estimates over 20 simulations to account for classification error N represent raw numbers and % represent weighted percentages
Results from the simple and multiple multinomial regression models are presented in Table 3 which lists the OR and AOR given that class 1 or the ‘no past year illegal drug use’ class is the referent group. Simple multinomial regression models indicate that individuals with alcohol dependence reporting GAD during their lifetime had 1.9 (95% CI: 1.3, 2.7) the odds of being in class 4 compared to class 1. Although not always statistically significant, the odds of being in any of the concurrent drug using classes compared to class 1 ranged from 1.2 to 2.1 for participants reporting lifetime GAD. In alcohol dependent participants reporting a history of MDD the odds of being in class 4 were 1.6 (95% CI: 1.1, 2.4) and being in class 5 were 2.3 (95% CI: 1.2, 4.7) compared to class 1. Concurrent drug users (Classes 2 to 5) were also more likely to report deviant behavior, having ever had an STI, having been booked or incarcerated, meeting more (5+) alcohol dependence criteria and having been in treatment for an alcohol or drug problem compared to participants with practically no concurrent drug use in the past year (Class 1).
Table 3.
Crude Odds Ratios (OR), Adjusted Odds Ratio (AOR) and 95% Confidence Intervals (CI) of Adult Alcohol Dependent Individuals, NSDUH 2005, 2006, and 2007
| Class 2 |
Class 3 |
Class 4 |
Class 5 |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) |
| Gender | ||||||||
| Female | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Male | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.0)* | 1.1 (0.8, 1.4) | 1.0 (0.7, 1.3) | 0.9 (0.6, 1.3) | 0.8 (0.5, 1.2) | 0.8 (0.4, 1.5) | 0.7 (0.3, 1.6) |
| Age | ||||||||
| 18–25 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 26–34 | 0.6 (0.4, 0.9)** | 0.7 (0.4, 1.0)* | 0.7 (0.5, 0.9)** | 0.6 (0.4, 0.9)** | 0.4 (0.2, 0.6)** | 0.4 (0.2, 0.7)** | 0.5 (0.2, 1.2) | 0.5 (0.2, 1.7) |
| >34 | 0.4 (0.3, 0.6)** | 0.4 (0.2, 0.6)** | 0.4 (0.3, 0.6)** | 0.4 (0.3, 0.5)** | 0.1 (0.1, 0.3)** | 0.2 (0.1, 0.3)** | 0.1 (0.0, 0.3)** | 0.1 (0.0, 0.4)** |
| Race | ||||||||
| White | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| African American | 0.5 (0.2, 0.9)** | 0.5 (0.2, 1.0)* | 1.1 (0.7, 1.6) | 1.0 (0.7, 1.6) | 0.5 (0.3, 1.1) | 0.4 (0.2, 0.9)** | 0.1 (0.0, 1.0) | 0.1 (0.0, 0.9)** |
| Hispanic | 0.7 (0.3, 1.7) | 0.6 (0.2, 1.7) | 0.8 (0.5, 1.2) | 0.7 (0.4, 1.2) | 0.4 (0.2, 0.9)** | 0.3 (0.2, 0.8)** | 0.5 (0.1, 1.9) | 0.4 (0.1, 1.6) |
| Other | 1.0 (0.5, 1.8) | 0.9 (0.5, 1.7) | 1.1 (0.7, 1.5) | 0.9 (0.6, 1.4) | 0.8 (0.4 1.9) | 0.7 (0.3, 1.5) | 0.3 (0.1, 0.9)** | 0.3 (0.1, 0.9)** |
| Education | ||||||||
| < High School | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| High School | 0.9 (0.5, 1.5) | 1.0 (0.5, 1.8) | 1.0 (0.7, 1.5) | 1.2 (0.8, 1.8) | 1.0 (0.6, 1.5) | 1.2 (0.7, 2.1) | 1.2 (0.6, 2.7) | 1.5 (0.6, 3.5) |
| College | 0.9 (0.5, 1.6) | 1.0 (0.5, 1.9) | 0.9 (0.7, 1.3) | 1.2 (0.8, 1.8) | 0.8 (0.5, 1.2) | 1.2 (0.7, 1.9) | 0.8 (0.3, 2.0) | 1.1 (0.4, 3.0) |
| Income | ||||||||
| <$20K | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| $20K–$49K | 0.8 (0.5, 1.3) | 0.9 (0.5, 1.5) | 0.7 (0.6, 1.0) | 0.8 (0.6, 1.1) | 0.6 (0.4, 1.0) | 0.7 (0.4, 1.1) | 0.6 (0.3, 1.4) | 0.7 (0.3, 1.7) |
| $50K–$75K | 0.7 (0.4, 1.4) | 0.8 (0.4, 1.6) | 0.7 (0.5, 1.1) | 0.9 (0.6, 1.4) | 0.6 (0.3, 1.0) | 0.7 (0.4, 1.2) | 0.4 (0.1, 1.3) | 0.5 (0.1, 1.8) |
| >75K | 0.9 (0.5, 1.5) | 1.1 (0.6, 2.0) | 0.7 (0.5, 1.0)** | 0.9 (0.6, 1.3) | 0.5 (0.3, 0.9)** | 0.7 (0.4, 1.2) | 0.5 (0.2, 1.3) | 0.7 (0.3, 1.8) |
| Lifetime Anxiety | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.8 (1.0, 3.0) | 1.4 (0.8, 2.6) | 1.2 (0.9, 1.6) | 1.2 (0.8, 1.7) | 1.9 (1.3, 2.7)** | 1.6 (1.0, 2.5)* | 2.1 (0.9, 4.9) | 1.3 (0.5, 3.7) |
| Lifetime Depression | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.5 (0.9, 2.4) | 1.1 (0.7, 1.9) | 0.9 (0.7, 1.2) | 0.8 (0.5, 1.1) | 1.6 (1.1, 2.4)** | 1.2 (0.7, 1.9) | 2.3 (1.2, 4.7)** | 1.4 (0.6, 3.7) |
| Past-year Deviant Behavior | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 3.1 (2.1,4.7)** | 2.5 (1.6, 4.0)** | 3.1 (2.3, 4.2)** | 2.3 (1.7, 3.2)** | 8.2 (5.7, 11.7)** | 5.4 (3.5, 8.5)** | 20.5 (10.3, 41.0)** | 13.6 (5.8, 32.0)** |
| Lifetime STD | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.2 (0.5, 2.7) | 1.1 (0.5, 2.4) | 1.6 (1.0, 2.5)** | 1.6 (1.0, 2.5)* | 1.3 (0.7, 2.3) | 1.1 (0.5, 2.1) | 2.6 (0.8, 7.9) | 1.9 (0.6, 6.2) |
| Lifetime Incarceration | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.4 (0.9, 2.1) | 1.4 (0.8, 2.3) | 1.5 (1.2, 1.9)** | 1.2 (0.9, 1.6) | 2.0 (1.4, 2.9)** | 1.7 (1.2, 2.5)** | 1.6 (0.8, 3.4) | 1.3 (0.5, 3.0) |
| Alcohol Dependence Criteria | ||||||||
| three | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| four | 1.5 (0.9, 2.4) | 1.5 (0.9, 2.3) | 1.3 (1.0, 1.8) | 1.3 (0.9, 1.8) | 1.3 (0.8, 2.1) | 1.2 (0.7, 2.0) | 1.2 (0.5, 3.1) | 1.3 (0.6, 3.2) |
| five to seven | 2.0 (1.3, 3.2)** | 2.0 (1.2, 3.3)** | 1.8 (1.3, 2.5)** | 1.8 (1.3, 2.6)** | 1.8 (1.1, 2.8)** | 1.7 (1.0, 2.8)** | 2.1 (0.9, 4.8)** | 2.2 (0.9, 5.4)* |
| Ever in Tx for ETOH or Drugs | ||||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.3 (0.8, 2.0) | 1.2 (0.7, 1.9) | 1.6 (1.2, 2.1)** | 1.7 (1.2, 2.3)** | 1.7 (1.1, 2.5)** | 1.7 (1.0, 2.7)** | 1.8 (0.9, 3.6) | 1.9 (0.9, 4.0)* |
Odds ration and confidence intervals represent combined estimates over 20 simulations to account for classification error Multivariable analysis controls for year of data collection
p<0.1
p<0.5
Results of the multiple multinomial regression model demonstrated that adults with alcohol dependence who reported deviant behavior were more likely to be in the concurrent drug using classes (Classes 2, 3, 4 and 5) compared to class1. Alcohol dependent participants reporting a history of incarceration had 1.7 (95% CI: 1.2, 2.5) the odds being in class 4 compared to class 1. Alcohol dependent participants meeting 5 or more of the alcohol dependence criteria compared to 3 dependence criteria had odds ranging from 1.7 to 2.2 for being in the concurrent drug using classes compared to class 1. Reporting ever having been in treatment for an alcohol or drug problem was more likely for class 3 (AOR=1.7, 95% CI: 1.2, 2.3) and class 4 (AOR=1.7, 95% CI: 1.1, 2.7) compared to class1.
4. Discussion
To our knowledge, this is the first study to examine patterns of past year illegal drug use among adults meeting criteria for alcohol dependence in a nationally representative sample. Findings indicate that illegal drug use is common in this population; the most common illegal drug used was marijuana (41%) followed by non-prescription opioid analgesics (23%) and cocaine (19%). Furthermore, study findings revealed that illegal drug use in adult alcohol dependent individuals is linked to a number of psychosocial problems; however, only 30% of the adults with alcohol dependence in this sample reported ever receiving treatment for alcohol or drugs.
LCA findings suggested five patterns of past year illegal drug use and different psychosocial correlates of the illegal drug use patterns in adults with alcohol dependence. Similar to existing literature, adults with alcohol dependence who use illegal drugs (i.e. those characterized by classes 2–5) were more likely than adult with alcohol dependence with nearly no illegal drug use (i.e. class 1) to have had the following: GAD, MDD, Deviant Behaviors, STIs, or incarceration (Stinson et al., 2005; Conway et al., 2003; Hedden et al., 2009). Specifically, participants with GAD were more likely to be in class 4 (characterized with multiple illegal drug use: marijuana, cocaine, non-prescription tranquilizers/sedatives, and non-prescription analgesic use) compared to class 1. Also, participants with MDD were more likely have been in either class 4 and 5 (both characterized by multiple illegal drug use with Class 4 less likely to use stimulants or ecstasy) compared to class 1. Comparable to existing literature on the association between STI and the concurrent use of alcohol and cocaine, alcohol dependent individuals with STI history were more likely to be in class 3 (characterized by marijuana and cocaine use) compared to class1 (Hedden et al., 2009; Heil et al., 2001). Adults with alcohol dependence and incarceration history were also more likely to be in classes 3 and 4 compared to class 1 (Hedden et al., 2009; Mumola and Karberg, 2006). Further, participants reporting Deviant Behaviors and meeting 5 to 7 of the Alcohol Dependence Criteria were more likely to be in the illegal drug using Classes (Classes 2–5) (Conway et al., 2003; Staines et al., 2001). Generally, findings suggest that adults with alcohol dependence with histories of past year illegal drug use (53% of our sample) have broader psychosocial treatment needs than adults with alcohol dependence with nearly no illegal drug use.
4.1 Strengths and Limitations
This study included a nationally representative population, which allowed us to generalize study findings to the U.S. population of adult individuals with alcohol dependence. Furthermore, it included assessment of participant use of a range of illegal drugs of use and assessment of mental health disorders consistent with the DSM-IV. However, limitations of this study should be noted; the NSDUH had a cross sectional design. This prevented us from being able to make causal inferences regarding the temporal order of illegal drug use and psychosocial problems as well as measuring the persistence of Alcohol Dependence over time. Also, the NSDUH did not take into account economic cost and availability of illegal drug use. That is, as prices of certain drugs rise or fall so does selection of illegal drugs of use (Petry, 2001). The choice of certain illegal drugs of use in this study may have been confounded by their availability and or cost. Although nicotine dependence often associated with alcohol dependence and illegal drug would have been pertinent to the regression analyses, nicotine dependence was only measured for the time frame of ‘past month’ rather than ‘past year’ in the NSDUH survey and was therefore not added to the analyses. Furthermore, since the data was obtained by self-report, participants may have under or over-reported their drug use compared to treatment seeking individuals or due to stigmas associated with mental or physical health and drug use (Harrison, 1997).
4.2 Implications for Prevention and Treatment
The study provides evidence for 1) the existence of distinct subgroups of illegal drug use among adult alcoholics and 2) different relationships between patterns of illegal drug use and psychosocial problems. Findings suggest the need for public health officials to boost efforts to prevent and screen for alcohol and illegal drug use. For many young persons, alcohol is the first drug they abuse. Increasing efforts to prevent young persons from initiating alcohol use may reduce the number of individuals who become involved with other illegal drug use (Ives and Ghelani, 2006). Treating alcohol disorders and preventing the onset of alcohol use will likely serve to reduce adverse psychological and social consequences associated with alcohol and other drug use.
Class 3, characterized by a high probability of marijuana and cocaine use, was associated with history of STI suggesting that STI screening should be a comprehensive component of substance disorder treatment. All concurrent drug using classes were associated with deviant behaviors and Class 3 and 4 were further associated with history of incarceration. This is especially concerning given that drug-related offenses account for an overwhelming portion of offenders in federal and state prisons (Mumola, 2006) and suggests that drug treatment programs in prisons are needed.
Given that different classes of concurrent drug use exist, multiple and targeted treatment strategies are needed. For example, Classes 4 and 5, characterized by multiple drug use as well as anxiety and/or depression, may benefit from combinations of cognitive behavior therapy (CBT) and pharmacotherapy which are known to dually treat such comorbidities and substance disorders (Hesse, 2009). CBT for the addiction plus Selective Serotonin Reuptake Inhibitors could be effective to reduce anxiety and/or depressive symptoms without addiction liability. For individuals with concurrent alcohol and cocaine dependence without anxiety/depression, they may benefit from CBT plus topiramate (Johnson et al., 2005).
Furthermore, determining differing characteristics of concurrent drug users is necessary such that treatment resources may be efficiently allocated. Study findings reveal that greater efforts are needed to bring adults with alcohol dependence into treatment as only 30% appear to ever have attended treatment for alcohol or drug use. Given that concurrent drug use is associated with greater severity of psychological and social consequences more resources may need to be allocated to the treatment of individuals with alcohol dependence and concurrent illegal drug use.
Acknowledgments
Role of Funding Source
Funding for this study was primarily provided by NIDA Dependence Epidemiology Training Grant, T32DA00729. Additional funding was provided by NIDA grant DA020667 (P.I.: Dr. Martins), NIDA grant DA023434 (P.I.: Dr. Martins), NIDA grant DA016368 (P.I.: Dr. Malcolm), and NIDA grant DA019903 (P.I.: Dr. Malcolm). Funding for Dr. Leah Floyd was provided by NIDA grant DA020630 (P.I. Dr. Pierre Alexandre). NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors
Sarra L Hedden conceptualized the manuscript, did the literature search, wrote the first draft of the manuscript and undertook the statistical analysis. Silvia Martins helped with the conceptualization of the paper, aided in the literature search, contributed to the statistical methods, contributed to the clinical interpretation of the statistical results and edited the manuscript. Robert Malcolm aided in the conceptualization and interpretation of the analysis of the paper as well as aided in the conceptualization/writing of the introduction and conclusions. Leah Floyd edited the manuscript and added to the literature search and helped write the conclusions. Courtenay Cavanaugh edited the manuscript and aided in writing the results and conclusions. William Latimer revised the manuscript, aided in the interpretation of the results and the conceptualization/writing of the conclusions. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sarra L. Hedden, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, 2213 McElderry Street, Suite 400, Baltimore, MD 21205 U.S.A. Tel: (410) 502-9515; Fax (410) 955-0237; E-mail: shedden@jhsph.edu.
Silvia S. Martins, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, 624 N. Broadway, 8th floor, Suite 896, Baltimore, MD 21205, U.S.A. Tel: (410) 614-2852; Fax (410) 955-9088; E-mail: smartins@jhsph.edu
Robert J. Malcolm, Medical University of South Carolina, Department of Psychiatry and Behavioral Sciences, Center for Drug and Alcohol Programs, 67 President Street, Charleston, SC 29425, U.S.A. Tel: (843) 792-5214; Fax: (843) 792-7353; E-mail: malcolmr@musc.edu
Leah Floyd, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, 2213 McElderry St., Suite 400, Baltimore, MD 21205 U.S.A. Tel: (410) 502-9511; Fax (410) 955-0237; E-mail: lfloyd@jhsph.edu.
Courtenay E. Cavanaugh, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, 2213 McElderry St., Suite 400, Baltimore, MD 21205 U.S.A. Tel: (410) 502-9515; Fax (410) 955-0237; E-mail: cocavana@jhsph.edu.
William W. Latimer, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, 2213 McElderry St., Suite 400, Baltimore, MD 21205 U.S.A. Tel: (410) 502-9500; Fax (410) 955-0237; E-mail: wlatimer@jhsph.edu.
References
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- Brady KT, Sonne S, Randall CL, Adinoff B, Malcolm R. Features of cocaine dependence with concurrent alcohol abuse. Drug and Alcohol Dependence. 1995;39(1):69–71. doi: 10.1016/0376-8716(95)01128-l. [DOI] [PubMed] [Google Scholar]
- Conway KP, Kane RJ, Ball SA, Poling JC, Rounsaville BJ. Personality, substance of choice, and polysubstance involvement among substance dependent patients. Drug Alcohol Depend. 2003;71(1):65–75. doi: 10.1016/s0376-8716(03)00068-1. [DOI] [PubMed] [Google Scholar]
- Cuffel BJ, Heithoff KA, Lawson W. Correlates of patterns of substance abuse among patients with schizophrenia. Hosp Community Psychiatry. 1993;44(3):247–251. doi: 10.1176/ps.44.3.247. [DOI] [PubMed] [Google Scholar]
- Curran GM, Sullivan G, Williams K, Han X, Allee E, Kotrla KJ. The association of psychiatric comorbidity and use of the emergency department among persons with substance use disorders: an observational cohort study. BMC Emerg Med. 2008;8(1):17. doi: 10.1186/1471-227X-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett ES, Zeger SL. Latent class model diagnosis. Biometrics. 2000;56:1055–1067. doi: 10.1111/j.0006-341x.2000.01055.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Concurrent and simultaneous use of alcohol with cocaine: results of a national survey. Drug Alcohol Depend. 1990;25(1):97–104. doi: 10.1016/0376-8716(90)90147-7. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hagenaars JA, McCutcheon AL. Applied Latent Class Analysis. New York: Cambridge University Press; 2002. [Google Scholar]
- Harrison L. The validity of self-reported drug use in survey research: An overview and critique of research methods. NIDA Research Monograph. 1997;167:17–36. [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hedden SL, Malcolm RJ, Latimer WW. Differences between adult non-drug users versus alcohol, cocaine and concurrent alcohol and cocaine problem users. Addict Behav. 2008;34(3):323–326. doi: 10.1016/j.addbeh.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heil SH, Badger GJ, Higgins ST. Alcohol dependence among cocaine-dependent outpatients: Demographics, drug use, treatment outcome and other characteristics. J Stud Alcohol. 2001;62(1):14–22. doi: 10.15288/jsa.2001.62.14. [DOI] [PubMed] [Google Scholar]
- Hesse M. Integrated psychological treatment for substance use and co-morbid anxiety or depression vs. Treatment for substance use alone. A systematic review of the published literature. BMC Psychiatry. 2009;9(6) doi: 10.1186/1471-244X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ives R, Ghelani P. Polydrug use (the use of drugs in combination); A brief review. Drugs: Education, Prevention and Policy. 2006;13(3):225–232. [Google Scholar]
- Johnson BA. Recent advances in the development of treatments for alcohol and cocaine dependence: Focus on topiramate and other modulators of GABA or glutamate function. CNS Drugs. 2005;19:873–896. doi: 10.2165/00023210-200519100-00005. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Huang FY, Davies M. Comorbidity between patterns of substance use dependence and psychiatric syndromes. Drug Alcohol Depend. 2001;64(2):233–241. doi: 10.1016/s0376-8716(01)00126-0. [DOI] [PubMed] [Google Scholar]
- Karno MP, Grella CE, Niv N, Warda U, Moore AA. Do substance type and diagnosis make a difference? A study of remission from alcohol- versus drug-use disorders using the National Epidemiologic Survey on Alcohol and Related Conditions. J Stud Alcohol and Drugs. 2008;69(4):491–495. doi: 10.15288/jsad.2008.69.491. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Agrawal A, Bucholz KK, Nelson EC, Madden PA, Todorov AA, Grant JD, Martin NG, Heath AC. Subtypes of illicit drug users: A latent class analysis of data from an Australian twin sample. Twin Res Hum Genet. 2006;9(4):523–530. doi: 10.1375/183242706778024964. [DOI] [PubMed] [Google Scholar]
- Martins SS, Mazzotti G, Chilcoat HD. Recent-onset ecstasy use: Association with deviant behaviors and psychiatric comorbidity. Exp Clin Psychopharmacol. 2006;14(3):275–286. doi: 10.1037/1064-1297.14.3.275. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 national alcohol survey. Drug Alcohol Depend. 2007;90(1):72–80. doi: 10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumola CJ, Karberg JC. Drug use and dependence, state, and federal prisoners 2004. US Department of Justice; 2006. Oct, [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide: Statistical analysis with latent variables. 5. Los Angeles: Muthen & Muthen; 2007. [Google Scholar]
- Norton R, Colliver J. Prevalence and patterns of combined alcohol and marijuana use. J Stud Alcohol. 1988;49(4):378–380. doi: 10.15288/jsa.1988.49.378. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–569. [Google Scholar]
- Petry NM. A behavioral economic analysis of polydrug abuse in alcoholics: asymmetrical substitution of alcohol and cocaine. Drug Alcohol Depend. 2001;62(1):31–39. doi: 10.1016/s0376-8716(00)00157-5. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Rubin D. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 1987. [Google Scholar]
- Staines GL, Magura S, Foote J, Deluca A, Kosanke N. Polysubstance use among alcoholics. J Addict Dis. 2001;20(4):53–69. doi: 10.1300/j069v20n04_06. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2005;80(1):105–116. doi: 10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2006. NSDUH Series H-30, DHHS Publication No. SMA 06-4194. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2007. NSDUH Series H-32, DHHS Publication No. SMA 07-4293. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD.: 2008. NSDUH Series H-32, DHHS Publication No. SMA 07-4293. [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, Manson SM. Latent class analysis of substance use: Comparison of two American Indian reservation populations and a national sample. J Stud Alcohol. 2006;67(1):32–43. doi: 10.15288/jsa.2006.67.32. [DOI] [PubMed] [Google Scholar]