Abstract
Purpose:
Determine anisometropia prevalence and associated risk factors in Hispanic and African-American preschoolers.
Design
Population-based cross-sectional study.
Participants
3030 Hispanic and 2994 African-American children aged 6 to 72 months from Inglewood, CA.
Methods
Retinomax autorefraction was performed on all participants after cycloplegia. Anisometropia was defined by difference in spherical equivalent (SE), by difference in plus cylinder in any axis (cylindrical), and by difference in cylinder axis vectors (J0 and J45) between the eyes. Strabismus was determined by prism-cover testing. A parental questionnaire explored potential risk factors including developmental delay, prematurity, prenatal exposure and family history.
Main Outcome Measures
Anisometropia prevalence was determined for age, gender and ethnicity. The association of anisometropia with strabismus and reported risk factors was assessed.
Results
The prevalence of SE anisometropia ≥1.0 diopter (D) was 4.3% for Hispanics and 4.2% for African Americans. Prevalence of cylindrical anisometropia ≥1.0D was 5.6% and 4.5%, respectively. Prevalence of cylindrical or SE anisometropia ≥3.0D was ≤ 0.4% for both ethnic groups. Cylinder vector anisometropia ≥ 0.5 was twice as common as cylindrical anisometropia ≥1.0D. SE anisometropia decreased at age one year in Hispanics (p=0.0016) but not African Americans. Cylindrical anisometropia decreased in the first year of life in both ethnic groups (p ≤ 0.001). There was no trend in SE or cylindrical anisometropia beyond one year of age, but cylinder vector anisometropia steadily decreased beyond one year of age in both ethnic groups. Cylinder vector anisometropia was more prevalent in African-Americans, but there was no difference in other measurements of anisometropia between ethnic groups. Anisometropia did not vary by gender. Strabismus was associated with all types of anisometropia. No association of anisometropia with gestational age, birth weight, cerebral palsy, family history, or prenatal exposure could be found.
Conclusions
Spherical and cylindrical anisometropia (≥ 1.0D) each affects 4% to 6% of Hispanic and African-American preschoolers. Anisometropia ≥3.0D is rare. Except for cylinder axis vector, the prevalence of anisometropia does not diminish beyond one year of age. Strabismus is associated with all forms of anisometropia. The association of other purported biological and environmental risk factors with anisometropia is notably lacking in this population.
Amblyopia is estimated to affect 0.75–4.0% of the population and 25–79% of cases of unilateral amblyopia are attributed, at least in part, to anisometropia.1,2 Anisometropia sufficient to cause amblyopia must be present in early life, but no population-based study has been performed to determine the prevalence of anisometropia in children of pre-school age in the United States. Prevalence estimates of anisometropia vary in different studies and may be dependent on age inclusion criteria and definition of anisometropia. Ethnic or racial differences in anisometropia prevalence have not been studied directly.
Few biological or environmental risk factors for anisometropia have been reported. Spherical equivalent anisometropia (≥ 1.0 diopter [D]), affecting 1.6% of 6-year-olds, has been significantly associated with exotropia and neonatal intensive care unit (NICU) admission in a population-based study, while anisoastigmatism (≥ 1.0D), affecting 1.0% of 6-year-olds, has been associated with maternal age >35 years and NICU admission.3 Both forms of anisometropia were associated with amblyopia, but not with esotropia or low birth weight (<2500 gm.). Other studies have purported associations with family history of myopia, prematurity, and developmental delay.4–7
The Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) is a population-based study designed to: 1) estimate and compare the prevalence of strabismus, amblyopia, and refractive error in a sample of African-American, Asian-American, Hispanic, and non-Hispanic White children 6 to 72 months of age, and 2) evaluate the association of selected demographic, behavioral, biological, and ocular risk factors with these ocular disorders. To date, examination of the African-American and Hispanic/Latino populations has been completed. Assessment of the other ethnic groups is ongoing. The purpose of this report is to describe the prevalence of various degrees of anisometropia in Hispanic and African-American preschoolers and identify any ethnic, gender, or age-related differences in prevalence of anisometropia. Such information may impact the cost-benefit analysis of any preschool screening programs to detect anisometropia with the goal of preventing amblyopia. The second purpose of this report is to identify biological or environmental risks associated with anisometropia in this population.
Methods
Subjects were identified by door-to-door screening of families within 44 census tracts in and around the city of Inglewood in Los Angeles County, CA. The details of the screening process have been reported elsewhere.8 Institutional Review Board (IRB) approval was obtained and informed consent was obtained for every participant. The study was performed in compliance with the Health Insurance Portability and Accountability Act (HIPAA) regulations.
Comprehensive eye examinations on all participants were performed by MEPEDS optometrists or ophthalmologists who specialized in pediatric eye care and who were trained and certified using standardized protocols. The examination included visual acuity, stereoacuity, assessment of ocular motility and alignment, refraction, and ophthalmoscopic examination. Children underwent Retinomax autorefraction 30 to 60 minutes after cycloplegia with 2 drops of 1% cyclopentolate 5 minutes apart (0.5% for children ≤ 12 months of age). If drops were refused, noncycloplegic retinoscopy was performed. Also, if Retinomax readings had a confidence value <8 after three attempts, cycloplegic retinoscopy was performed.
Spherical equivalent (SE) anisometropia was defined as the difference in spherical equivalent between the two eyes. Cylindrical anisometropia was defined as the difference in absolute cylinder between the eyes regardless of axis. Prevalence of SE anisometropia and cylindrical anisometropia ≥1.0 D and ≥3.0 diopters (D) were calculated. In order to account for interocular differences in cylinder axis, the vertical Jackson cross cylinder vector (J0) and oblique Jackson cross cylinder vector (J45) were calculated for each eye according to the formula of Thibos9, wherein J0 = −cylinder power × cos (2π × cyl axis/180), and J45 = −cylinder power × sin (2π × cyl axis/180). Anisometropia by vector analysis was defined as a difference of ≥ 0.5 in J0 or J45 between the two eyes. This is equivalent to a cylinder power difference of ≥1.0D at 0° and 45°, respectively.
A parental questionnaire was administered on the day of the clinical examination probing for family history of eye diseases and subjects’ medical histories. Specific risk factors identified from the questionnaire or the examination that were assessed were: age group; ethnicity; parental history of strabismus or amblyopia; maternal age (at the birth of the child) ≥ 35 years; history of breast feeding; prenatal tobacco or ethanol exposure; gestational age (weeks); birth weight (kg); parental report of a diagnosis of Down Syndrome or cerebral palsy; and strabismus in the subject on examination.
For univariate analyses, comparisons of proportions between groups were performed using the chi-square test. The univariate associations of gestational age and birth weight with anisometropia were tested using logistic regression. Risk factor associations with p-value <0.1 were entered into a stepwise multivariate model to determine independent associations and odds ratios. Odds ratios (OR) for independent risk factors are reported if confidence intervals excluded 1.0. The Cochrane-Armitage trend test was used to look at the linear association between age and anisometropia.
Results
7,974 eligible children were identified for MEPEDS; 6151 (77%) completed an ophthalmic examination. Of these, 6024 (2994 African-American and 3030 Hispanic children) underwent refraction. 1% of Hispanic children and 4% of African-American children refused cycloplegic eyedrops; these children underwent noncycloplegic retinoscopy. Among children receiving cycloplegic eyedrops, 90% overall underwent successful Retinomax autorefraction in both eyes. The remaining 10% underwent cycloplegic retinoscopy. 45 Hispanic children and 38 African-American children were up to 4 weeks shy of age 6 months. These children were considered to be 6 months old for purposes of analysis.
Overall the prevalence of SE anisometropia ≥1.0D was 4.3% for Hispanics and 4.2% for African Americans. Prevalence of SE anisometropia ≥ 3.0D was 0.4% for both Hispanics and African Americans (Table 1).
Table 1.
Frequency distribution of the type and magnitude of anisometropia stratified by age group and race/ethnicity in the Multi-Ethnic Pediatric Eye Disease Study╫
| Spherical Equivalent Anisometropia n (%) | Cylindrical Anisometropia n (%) | Vector Axis Anisometropia n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age group in months | Hispanic | African-American | Hispanic | African-American | Hispanic | African-American | ||||
| ≥1.0D | ≥3.0D | ≥1.0D | ≥3.0D | ≥1.0D | ≥3.0D | ≥1.0D | ≥3.0D | ≥0.5 | ≥0.5 | |
| 6–11 | 23 (7.76) | 1 (0.34) | 13 (4.69) | 0 (0.00) | 29 (9.80) | 1 (0.34) | 26 (9.39) | 0 (0.00) | 61 (20.61) | 62 (22.38) |
| 12–23 | 27 (4.97) | 1 (0.18) | 30 (5.46) | 2 (0.36) | 34 (6.26) | 2 (0.37) | 30 (5.46) | 0 (0%) | 66 (12.15) | 75 (13.66) |
| 24–35 | 24 (4.20) | 2 (0.35) | 19 (3.49) | 2 (0.37) | 26 (4.55) | 2 (0.35) | 26 (4.77) | 2 (0.37) | 56 (9.79) | 68 (12.48) |
| 36–47 | 17 (3.20) | 3 (0.56) | 20 (3.76) | 3 (0.56) | 35 (6.58) | 3 (0.56) | 17 (3.20) | 0 (0%) | 51 (9.59) | 54 (10.15) |
| 48–59 | 17 (3.13) | 2 (0.37) | 22 (4.01) | 3 (0.55) | 26 (4.79) | 1 (0.18) | 15 (2.74) | 0 (0%) | 42 (7.73) | 50 (9.12) |
| 60–72 | 21 (3.84) | 2 (0.37) | 23 (4.24) | 1 (0.18) | 20 (3.68) | 1 (0.18) | 22 (4.05) | 0 (0%) | 39 (7.17) | 46 (8.47) |
| Total | 129 (4.26) | 11 (0.36) | 127 (4.24) | 11 (0.37) | 170 (5.61) | 10 (0.33) | 136 (4.54) | 2 (0.07) | 315 (10.40) | 355 (11.86) |
| Trend Test p-values: All age groups | ||||||||||
| Two-sided | 0.0061 | 0.6631 | 0.4171 | 0.6947 | 0.0018 | 0.5576 | 0.0003 | 0.5261 | <0.0001 | <0.0001 |
| Trend Test p-values: 12 – 72 months | ||||||||||
| p-values | 0.2083 | 0.6381 | 0.4734 | 0.8373 | 0.1036 | 0.4917 | 0.0674 | 0.3199 | 0.0023 | 0.0011 |
| Chi-square test p-values: 6–11 months vs 12 – 72 months | ||||||||||
| p-values | 0.0016 | 1.0000* | 0.6956 | 0.6138* | 0.0010 | 1.0000* | <0.0001 | 1.0000* | <0.0001 | < 0.0001 |
Fisher’s Exact Test P-values.
Total number of African American and Hispanic children examined was 2994 and 3030 respectively.
D = diopters
The prevalence of cylindrical anisometropia ≥1.0D was 5.6% for Hispanics and 4.5% for African Americans. Anisometropia defined by cylinder vector difference of ≥0.5 at J0 or J45 had around twice the prevalence (10.4% for Hispanics; 11.9% for African Americans) of absolute cylindrical anisometropia. Prevalence of cylindrical anisometropia ≥3.0D was 0.3% for Hispanics; 0.1% for African Americans (Table 1).
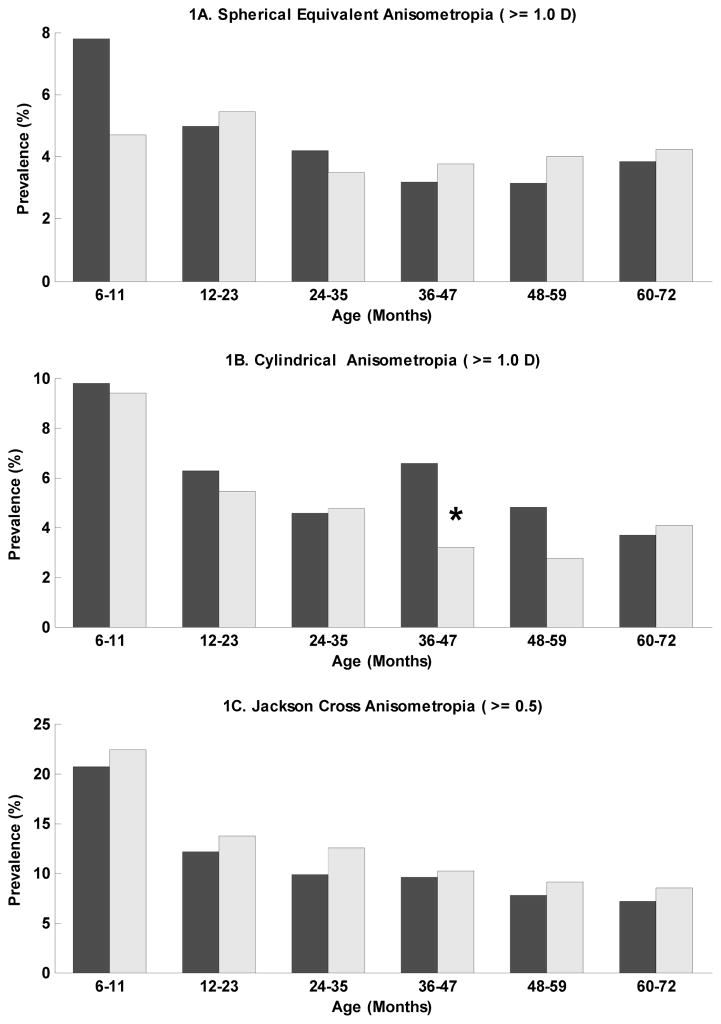
The prevalence of SE anisometropia ≥1.0D decreased from age <12 months to ≥12 months in Hispanics (p=0.0016, chi-square) but not African Americans (p=0.69) (Figure 1a), while the prevalence of cylindrical anisometropia ≥1.0D decreased from age <12 months to ≥ 12 months in both ethnic groups (p= 0.001 and p<0.001, respectively) (Figure 1b). There was no age-related trend in SE or cylindrical anisometropia in either ethnic group beyond one year of age. On the other hand, the trend test over six age groups showed a significant decreasing trend in cylinder vector (J0 or J45) anisometropia with age group for both Hispanic and African American children, even beyond 12 months of age (p<0.0001) (Figure 1c). In multivariate regression, young age (<24 months for cylindrical; <36 months for cylinder vector) was an independent risk factor for astigmatic anisometropia, but not SE anisometropia (Table 2).
Figure 1.
The prevalence of different forms of anisometropia is shown by age and ethnicity (dark bars = Hispanics; light bars = African-Americans). The prevalence of spherical equivalent (SE) anisometropia ≥1.0 diopters (D) is stable beyond 12 months of age for both ethnic groups (Fig 1a). The prevalence of cylindrical anisometropia ≥1.0 D is stable beyond 12 months of age except in the 36–47 month age group, in which it is significantly more prevalent (*) in Hispanics compared to African-Americans (Fig 1b). The prevalence of Jackson Cross anisometropia ≥0.5 steadily decreases with age (Fig 1c). The total number of African American and Hispanic children examined was 2994 and 3030 respectively.
Table 2.
Independent risk factors associated with different types of anisometropia in the Multi-Ethnic Pediatric Eye Disease Study based on stepwise multivariate regression analyses.
| Risk factor* | OR | CI |
|---|---|---|
| SE Anisometropia | ||
| Esotropia vs No Strabismus | 6.20 | (3.24, 11.89) |
| Exotropia vs No Strabismus | 3.52 | (1.79, 6.95) |
| Hypermetropic SE Anisometropia | ||
| Esotropia vs No Strabismus | 7.53 | (3.81, 14.91) |
| Family_amblyopia | 3.50 | (1.22, 10.03) |
| Cylinder Anisometropia | ||
| Age group | ||
| 06–11 Months vs 60–72 Months | 2.74 | (1.81, 4.16) |
| 12–23 Months vs 60–72 Months | 1.60 | (1.07, 2.39) |
| Esotropia vs No Strabismus | 3.02 | (1.35, 6.73) |
| Exotropia vs No Strabismus | 3.99 | (2.21, 7.19) |
| Cylinder vector anisometropia | ||
| Age group | ||
| 06–11 Months vs 60–72 Months | 2.91 | (2.11, 4.00) |
| 12–23 Months vs 60–72 Months | 1.61 | (1.20, 2.16) |
| 24–35 Months vs 60–72 Months | 1.39 | |
| Esotropia vs No Strabismus | 2.04 | (1.01, 4.10) |
| Exotropia vs No Strabismus | 3.75 | (2.25, 6.26) |
| Down syndrome | 6.21 | (1.27, 30.25) |
OR = odds ratio; CI = confidence interval; SE = spherical equivalent
variables listed in order of entry into the model
Only the 36–47 month-old age group of Hispanic children had significantly more cylindrical anisometropia than African-Americans (p=0.01). There was no significant overall difference in anisometropia between ethnic groups after adjusting for age (p=0.98 for SE; 0.10 for cylindrical). There was no gender-related difference in anisometropia for either ethnic group (p>0.3).
All forms of anisometropia were significantly associated with both esotropia and exotropia (Table 2). 70% of those with SE anisometropia had pure hypermetropic anisometropia. For such cases, esotropia, but not exotropia, was a significant association and family history of amblyopia became a risk factor.
Down syndrome, affecting 14 children, was a risk factor only for cylinder vector anisometropia. Maternal age, gestational age, prematurity, birth weight, prenatal exposure to alcohol or tobacco, and family history of strabismus or spectacle use were not significant risk factors for any type of anisometropia.
Discussion
No previous population-based studies have investigated the prevalence of anisometropia in children less than four years of age. This study demonstrates that anisometropia ≥1.0D is common throughout preschool years especially in the first year of life, but anisometropia ≥3.0D is rare. Hispanic and African-American boys and girls of preschool age are approximately equally affected by both cylindrical and SE anisometropia, with a prevalence of 4% for each type of anisometropia (≥ 1 D) at age five years. This prevalence does not vary significantly with age beyond one year of age. This is considerably higher than prevalences of 1.0% cylindrical and 1.5% SE anisometropia found in predominantly six-year-old Australians using the same anisometropia definitions.3 In contrast, using similar definitions, Dobson et. al. found a prevalence of 15.0% cylindrical and 6.7% SE anisometropia in a population of 4–13 year-old Native Americans with a high prevalence of astigmatism.10 These differences in prevalence suggest that anisometropia is related to environmental or ethnic differences, rather than to a change in prevalence beyond five years of age.
The prevalence of astigmatic anisometropia defined by cylinder vector analysis declined steadily from age six months to six years. Inter-ocular differences ≥0.5 in J0 or J45 cylinder vector components were seen in 7% of Hispanics and 8% of African-American 5-year-olds. This amount of J0 or J45 anisometropia was three times as common (23%) in 4–13 year-old Native Americans.10 This is not surprising given the high prevalence of astigmatism in that population.
There is a striking difference in the prevalence of the two different measures of astigmatic anisometropia. Cylinder vector anisometropia is twice as common as cylindrical anisometropia and decreases steadily with age, while cylindrical anisometropia prevalence remains stable beyond one year of age. This suggests that inter-ocular differences in astigmatism axis are more common than absolute cylindrical anisometropia, but diminish with age.
It is unlikely that improvement in Retinomax testability with age affected the outcomes of this study. More than 60% of subjects less than one year of age, 70% of subjects less than 2 years of age and 90% of subjects more than two years of age were testable in both eyes.11 Nearly all of those that were not testable with Retinomax were testable with retinoscopy. Retinomax testability was the same for both ethnic groups even though the change in prevalence of SE anisometropia was not. It is thus unlikely that the anisometropia prevalence was impacted by the decreased Retinomax testability in very young subjects.
Surprisingly few biological or environmental risk factors stand out in association with anisometropia. Strabismus is associated with all forms of anisometropia and family history of amblyopia is associated with hypermetropic SE anisometropia. The association with Down syndrome only applies to the cylinder vector and is based on only 14 subjects, four of whom had anisometropia. Previously reported risk factors from retrospective studies, such as prematurity, were not found in this population-based study.4–7 It is possible these and other previously reported risk factors only apply to ethnically distinct populations not yet included in the MEPEDS cohort completed so far.
Preschool refractive error screening could detect many children with amblyogenic levels of anisometropia, but no unselected, population-based data have been published relating levels of anisometropia with amblyopia risk. One study of a non-strabismic pediatric ophthalmology clinic population showed a significantly increased prevalence of amblyopia associated with myopic anisometropia >2.0 D, hyperopic anisometropia > 1.0 D, or cylinder anisometropia >1.5 D.12 A population-based study of 4–13 year-old Native Americans also showed a significant association of hyperopic anisometropia (≥ 1.0 D) and cylindrical anisometropia (≥ 3.0 D), but not myopic anisometropia, with amblyopia.13 Although there was a significant trend of increasing inter-ocular acuity difference with increasing cylinder vector anisometropia, even anisometropia ≥ 1.0 (equivalent to ≥2.0 D cylindrical anisometropia in the absence of a difference of axis) was not associated with increased risk of amblyopia compared to isometropic subjects in that population. Failure to detect an increased risk for amblyopia in that group may be related to the inclusion of children with similar amounts of astigmatism in the two eyes, but mirror image axes of oblique astigmatism. The risk for unilateral amblyopia due to symmetrical inter-ocular differences in cylinder axis remains unknown.
The American Academy of Ophthalmology and the American Association of Pediatric Ophthalmology and Strabismus (AAPOS) have established practice guidelines for prescribing eyeglasses for anisometropia for ages 0–1 year, 1–2 years and 2–3 years14 (http://one.aao.org/CE/PracticeGuidelines/Snippet.aspx?cid=73f2ae51-0f10-4be4-97f7-a744e04d6a30 accessed on April 24, 2009). These guidelines are for the purpose of minimizing amblyopia risk, and are based on consensus opinion only. These guidelines tolerate more anisometropia earlier in life, consistent with the trend of decreasing anisometropia in the first two years of life described herein. Less than 1% of our cases qualified for eyeglasses based on the AAPOS guidelines for treating anisometropia. (Table 3) There were no significant differences between Hispanics and African-Americans in the numbers who qualified for spectacles based on these criteria.
Table 3.
Prevalence of anisometropia requiring treatment based on American Association of Pediatric Ophthalmology and Strabismus (AAPOS) treatment thresholds stratified by age group in the Multi-Ethnic Pediatric Eye Disease Study.
| Age group in months | Number of Children | Spherical Equivalent Anisometropia | Cylindrical Anisometropia | ||
|---|---|---|---|---|---|
| Threshold (diopters) | Number of cases (%) | Threshold (diopters) | Number of cases (%) | ||
| 6 – 11 | 573 | ≥2.5D | 1 (0.17) | ≥2.5D | 1 (0.17) |
| 12 – 23 | 1092 | ≥2.0D | 6 (0.55) | ≥2.0D | 3 (0.27) |
| 24 – 35 | 1117 | ≥1.5D | 18 (1.61) | ≥2.0D | 7 (0.63) |
The AAPOS treatment guidelines also recommend that anisometropia with oblique astigmatism (defined as ≥ 15° from the 90° or 180° axis) >1 diopter should be treated at any age.15 Only 0.8% of our study participants met this criterion of anisometropia with oblique astigmatism in either eye.
Except for the steady decline in cylinder vector anisometropia (for which there are no treatment guidelines, and the risk of amblyopia is unknown), the age-related trend shows that the prevalence of anisometropia is relatively stable between one and six years of age. This suggests that screening programs for anisometropia in preschoolers would detect similar numbers of affected children when applied any time in this age group.
The validity of the MEPEDS findings are supported by population-based data, rigorous protocols and quality control, high participation rates, and a large sample size. However, cross-sectional studies as this cannot assess likely stability of anisometropia in individuals. Thus, individuals may develop or resolve anisometropia over the period of time that the population prevalence of anisometropia is stable. Further studies need to assess longitudinal changes in anisometropia and the levels of anisometropia that confer significant amblyopia risk before cost effective screening regimens can be developed.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Robaei D, Rose KA, Ojaimi E, et al. Causes and associations of amblyopia in a population-based sample of 6-year-old Australian children. Arch Ophthalmol. 2006;124:878–84. doi: 10.1001/archopht.124.6.878. [DOI] [PubMed] [Google Scholar]
- 2.Multi-ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2008;115:1229–36. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huynh SC, Wang XY, Ip J, et al. Prevalence and associations of anisometropia and aniso-astigmatism in a population based sample of 6 year old children. Br J Ophthalmol. 2006;90:597–601. doi: 10.1136/bjo.2005.083154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindqvist S, Vik T, Indredavik MS, Brubakk AM. Visual acuity, contrast sensitivity, peripheral vision and refraction in low birthweight teenagers. Acta Ophthalmol Scand. 2007;85:157–64. doi: 10.1111/j.1600-0420.2006.00808.x. [DOI] [PubMed] [Google Scholar]
- 5.Robaei D, Kifley A, Gole GA, Mitchell P. The impact of modest prematurity on visual function at age 6 years: findings from a population-based study. Arch Ophthalmol. 2006;124:871–7. doi: 10.1001/archopht.124.6.871. [DOI] [PubMed] [Google Scholar]
- 6.Saunders KJ, McCulloch DL, Shepherd AJ, Wilkinson AG. Emmetropisation following preterm birth. Br J Ophthalmol. 2002;86:1035–40. doi: 10.1136/bjo.86.9.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandfeld Nielsen L, Skov L, Jensen H. Visual dysfuntions and ocular disorders in children with developmental delay. II. Aspects of refractive errors, strabismus and contrast sensitivity. Acta Ophthalmol Scand. 2007;85:419–26. doi: 10.1111/j.1600-0420.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 8.Varma R, Deneen J, Cotter S, et al. Multi-Ethnic Pediatric Eye Disease Study Group. The Multi-Ethnic Pediatric Eye Disease Study: design and methods. Ophthalmic Epidemiol. 2006;13:253–62. doi: 10.1080/09286580600719055. [DOI] [PubMed] [Google Scholar]
- 9.Thibos LN, Wheeler W, Horner DG. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–75. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Dobson V, Harvey EM, Miller JM, Clifford-Donaldson CE. Anisometropia prevalence in a highly astigmatic school-aged population. Optom Vis Sci. 2008;85:512–9. doi: 10.1097/OPX.0b013e31817c930b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borchert M, Wang Y, Tarczy-Hornoch K, et al. MEPEDS Study Gruop. Testability of the Retinomax Autorefractor and IOLMaster in preschool children: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2008;115:1422–5. doi: 10.1016/j.ophtha.2007.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weakley DR., Jr The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108:163–71. doi: 10.1016/s0161-6420(00)00425-5. [DOI] [PubMed] [Google Scholar]
- 13.Dobson V, Miller JM, Clifford-Donaldson CE, Harvey EM. Associations between anisometropia, amblyopia, and reduced stereoacuity in a school-aged population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 2008;49:4427–36. doi: 10.1167/iovs.08-1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel. Amblyopia. San Francisco, CA: American Academy of Ophthalmology; 2007. [Accessed May 25, 2009]. Preferred Practice Pattern; pp. xx–xx. Available at: http://one.aao.org/CE/PracticeGuidelines/PPP.aspx?sid=d9939a8b-1675-4bf8-85fb-154652305795. AQ: provide specific, inclusive pagination for material being cited. [Google Scholar]
- 15.Donahue SP, Arnold RW, Ruben JB AAPOS Vision Screening Committee. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003;7:314–6. doi: 10.1016/s1091-8531(03)00182-4. [DOI] [PubMed] [Google Scholar]