Abstract
Excessive gestational weight gain has been shown to relate to high postpartum weight retention and the development of overweight and obesity later in life. Since many women are concerned about the health of their baby during pregnancy and are in frequent contact with their health care providers, pregnancy may be an especially powerful “teachable moment” for promoting healthy eating and physical activity behaviors among women. Initial research suggests that helping women gain the recommended amount during pregnancy through healthy eating and physical activity could make a major contribution to preventing postpartum weight retention. However, more randomized controlled trials with larger samples sizes are needed to identify the most effective and disemminable intervention. Providers have the potential to prevent high postpartum weight retention and future obesity by monitoring weight gain during pregnancy and giving appropriate advice about recommended amounts of gestational weight gain.
Obesity is major health problem in the United States. National data indicate that 65.1% of Americans are considered overweight or obese (BMI ≥25).1 The prevalence of obesity (body mass index [BMI] >30 kg/m2) has increased more than 50% (from 14.5% to 33.6%) over the past two decades.2,3 The known risks of morbidity associated with overweight include hypertension, cardiovascular disease, diabetes, and cancer. Weight gain during adult life is also associated with increased risk of heart disease and death.4,5 Even modest amounts of weight gain dramatically increase the risk for the development of diabetes after 18 years of age.5–7
The link between pregnancy and obesity
An important contributing factor to weight gain among young adult women is sustained weight retention after pregnancy. Although studies of the general population have reported average weight gains of only 0.4 to 3.8 kg more than aging,8–18 there is marked variability in weight changes associated with pregnancy. Approximately 25% of women experience weight retention of 4.5 kg or more in association with pregnancy.15,19–21 Moreover, weight changes at the time of pregnancy are strongly related to subsequent weight change. In two large prospective studies22,23 weight gains during the pregnancy and weight changes during the year postpartum were both independently related to weight gain23 or the development of overweight22 at 10 and 15 years follow-ups, respectively. Linne24 reported that 45.6% of normal weight individuals who gained excessive amounts of weight during pregnancy (average = 18.8 kg) shifted from normal weight to overweight at 15 years follow-up (Figure 1). Moreover, 43.8% of normal weight women who had retained significant amounts of weight at 12 months postpartum (M= 4.8 kg) became overweight at 15 years follow-up. Rooney et al. 23 reported that women who were back to their pre-pregnancy weight by 6 months postpartum gained only 2.4 kg over the next 10 years, whereas those who retained weight at postpartum gained 8.3 kg over the 10 year follow-up. Thus, high gestational weight gain and postpartum weight retention appear to set the stage for future weight gain and the development of obesity.
Figure 1.
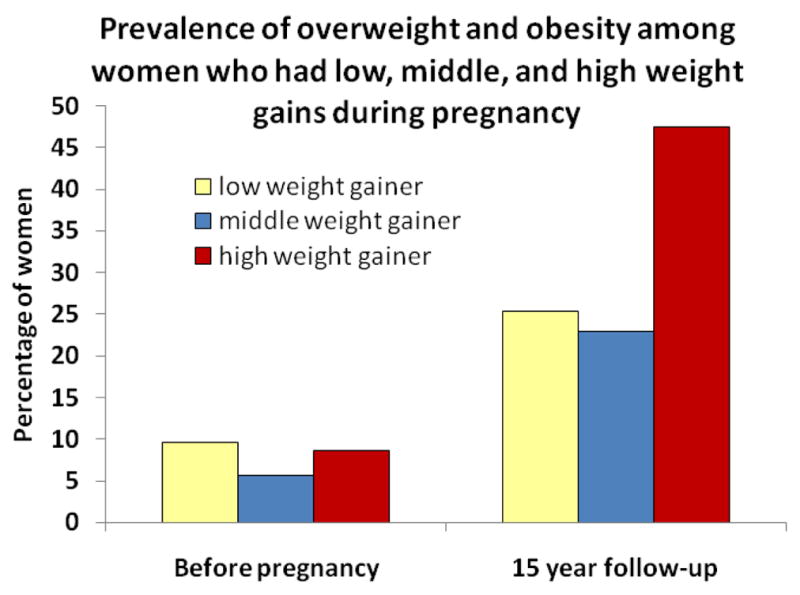
Prevalence of overweight and obesity among women who had low, middle, and high weight gains during pregnancy. NOTE: Adapted from Linne et al, 2004 22 Low weight gainers gained an average of 9.8 ± 1.9 kg; middle weight gainers gained 14.0 ±0.9 kg; and, high weight gainers gained 18.8 ± 2.3 kg during pregnancy.
Variables associated with high postpartum weight retention provide targets for intervention
The strongest predictor of 1-year postpartum weight retention is the amount of weight gained during pregnancy.21–23,25,26 The IOM guidelines, published in 1990, recommend ranges of weight gain by pre-pregnancy BMI 27 (Table 1). These ranges were selected to optimize fetal growth and maternal/infant outcomes 27 and are currently under consideration for revision by the IOM in the context of today’s obesity epidemic. Despite the wide adoption of the 1990 IOM guidelines, however, many women continue to gain more than the recommended amount. Recent data suggest that 37% of normal weight women and 64% of overweight women gain more that IOM recommendations.19,28 Although there is a broad range of weight changes that are associated with healthy pregnancy outcomes,29 weight gains that exceed the IOM recommended levels have been connected to gestational complications (hypertension, diabetes, and pre-eclampsia), complications in delivery (cesarean sections), babies that are large for gestational age (macrosomia),30–34 and obesity in offspring by age 3.35,36 Weight gains outside IOM recommendations are also associated with greater postpartum weight retention and an increased risk of future overweight.37–40 Thus, in order to prevent postpartum weight retention, it is critical to try to prevent excessive weight gain during pregnancy. 41
Table 1.
The 1990 IOM recommendations for total weight gain ranges for pregnant women
| Recommended total gestational weight gain | ||
|---|---|---|
| BMI category | kg | lb |
| < 19.8 | 12.5–18 | 28–40 |
| 19.8–26 | 11.5–16 | 25–35 |
| 26.0–29.0 | 7–11.5 | 15–25 |
| > 29.0 | ≥ 6.8 | ≥ 15 |
Adapted from the 1990 Institute of Medicine report 27
Behaviors during pregnancy have also been found to relate to the risk of excessive gestational weight gain 42–46 (Figure 2). Olson et al44 evaluated multivariable biopsychosocial models of gestational weight gain in 622 healthy women. In the final adjusted model, women who reported eating “much more” food during mid-pregnancy were 2.35 times more likely than women who ate “a little more” food to gain too much weight in pregnancy. Moreover, women who were less physically active during pregnancy than before pregnancy were 1.7 times more likely to gain more than recommended than those who maintained or increased their physical activity. Other studies have reported similar findings and also shown additional relationships with excessive gestational weight gain and high fat intake,42 low fiber intake,42 and high intake of sweets.42 These findings suggest that targeting healthy eating and modest physical activity during pregnancy may help improve maternal weight gain outcomes.
Figure 2.

Variables related to excessive gestational weight gain
At risk populations
Certain subgroups of women appear to be at greater risk of high gestational weight gain than others and may benefit from interventions to promote healthy weight gain during pregnancy. Many studies have found that pre-pregnancy weight is a significant predictor of weight changes during pregnancy. Although obese women gain less weight than normal weight women during pregnancy, women who are obese (BMI≥30) prior to pregnancy appear more likely to exceed IOM weight gain guidelines (using the IOM overweight criterion of BMI > 26) compared with normal weight women.29,47,48 The multiple risks associated with excess gestational weight gain may be compounded by risks associated with high pre-pregnancy BMI.49–52 Compared with normal-weight females, obese pregnant women have an increased risk of early-trimester loss and recurrent miscarriage 53 as well as congenital anomalies, including neural tube defects, heart defects, and omphalocele.54–56 Other complications include chronic hypertension, pregnancy-induced hypertension, pregestational diabetes, gestational diabetes, post-date delivery,57–61 urinary tract infection,62 asthma, obstructive sleep apnea, and gallbladder disease59,63–65 Numerous delivery, 59 operative, 66 and post-partum67–70 complications are also associated with pre-pregnancy obesity. Moreover, maternal obesity has a significant impact on offspring risks, including higher rates of fetal macrosomia, still birth 71,72 and childhood obesity73.
Weight loss prior to conception is likely an effective way to decrease complications associated with pregnancy in obese women; however, limited research has been conducted in this area. Bariatric procedures prior to conception have been found to significantly reduce rates of pregnancy-induced hypertension and gestational diabetes,74 chronic hypertension, pregestational diabetes, and large for gestational age infants.75 However, bariatric surgery is a potential option for only a small subset of women who have a BMI > 35, comorbid conditions, history of failed nonsurgical interventions, acceptable operative risks, and motivation to adhere to long-term post-surgical dietary regimen 76. Practitioners may consider advising effective non-surgical weight loss strategies prior to conception, including daily self-monitoring food intake, 77–80 daily self-weighing, 78,81 and consuming meal replacement products, typically for 2 meals a day initially, and then one meal a day long-term.82,83 However, since physicians often cannot devote the time needed to help a patient with their weight loss efforts, it may be useful to refer patients to other programs that can provide more intensive assistance with weight loss prior to conception.84 Ideally, efforts to promote pre-pregnancy weight control should be carried over during pregnancy to prevent excessive gestational weight gain.
Race may also affect pregnancy weight changes. African-American women consistently gain less weight than white women during pregnancy. 19,26,40 However, they are no different from white women in terms of falling above, at, or below IOM guidelines.40,47 Age also affects weight gain during pregnancy; younger women gain more weight than older women, but this effect may be due to high weight gain during growth in adolescent women.85 Primiparity is also associated with larger weight gains during pregnancy. Abrams and Parker85 found that weight gains of women with parity of 0,1, or 2+ were 34.0, 33.2, and 31.5 lbs; and, in another study, 34% of primiparous women exceeded the IOM guidelines, while only 16% of multiparous women exceeded the guidelines.26
Smoking cessation is strongly recommended during pregnancy because, in part, of its association with low infant birth weight.86 Studies comparing women who do not smoke with those who continue to smoke find that non-smokers tend to gain more weight than smokers.26 Smoking during pregnancy has also been associated with increased risk of obesity in the offspring. 87,88 Low income has also been related to greater risk of exceeding weight gain guidelines.89,90 Finally, genetic factors may contribute to the rate of gestational weight gain.91
Pregnancy as a “teachable moment”
The label “teachable moment” has been used to describe naturally occurring life transitions or health events thought to motivate individuals to spontaneously adopt risk-reducing health behaviors; the concept of “teachable moments” has a strong foundation in widely accepted conceptual models of behavior.92,93
McBride et al.94 recently proposed a model to describe characteristics of effective teachable moments using smoking cessation as an example. Teachable moments were characterized as times that (1) increase perceptions of personal risk and outcome expectancies, (2) prompt strong affective or emotional responses, and (3) redefine self-concept or social roles. McBride et al.94 posited that the greater the degree to which a health event alone or in combination with a proximally timed intervention influences all three domains, the greater the likelihood the event will prompt behavioral change.
Using this model, pregnancy may be conceptualized as a powerful “teachable moment.” Pregnancy provides an immediate and personal experience with risk related to the mother’s and baby’s health and enhances the perceived value of healthy eating and exercise.95,96 Moreover, the emotional responses surrounding pregnancy may also make it an opportune time to initiate change. Emotional responses are thought to influence an individual’s judgments about the significance and meaning of an event.93 Pregnancy may prompt feelings of elation and fear about the well-being of the fetus, which may motivate women to change their eating and exercise habits.
Finally, consideration of the pregnancy’s impact on social role and self-concept is important in viewing it as a “teachable moment.” Clearly, pregnancy is a time when personal and social roles change as women become mothers in addition to their other roles. Primiparous women are adopting the maternal role for the first time, which carries expectations for major changes in lifestyle and self-image.97,98 Women are also becoming a role model for their new child, which, again, may have implications for adopting healthy eating and exercise habits. Thus, intervening during pregnancy may capitalize on this natural period of redefinition that occurs among women (Figure 3).
Figure 3.
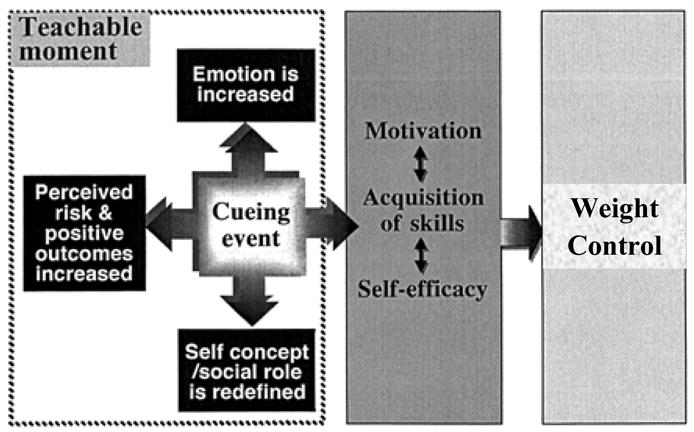
Pregnancy as a “teachable moment” for weight control. Reprinted and adapted with permission from McBride et al. 122
Weight gain prevention interventions during pregnancy
A handful of studies have evaluated interventions during pregnancy to promote weight gain within recommendations and prevent postpartum weight retention. Gray-Donald et al99 examined the effects of periodic dietary counseling on weight gain in a non-randomized study of the Cree population. The intervention was found to have only a minor impact; the authors noted that cultural factors, however, likely limited the intervention’s efficacy in the Cree population.99 In another non-randomized study, Kinnunen et al.100 examined the effects of an intervention that included four dietary counseling sessions with a public health nurse. Results indicated that more women in intervention clinics than control clinics made the dietary changes targeted by the intervention (higher intakes of vegetables, fruits, berries, and high fiber bread), but no significant group differences in magnitude of gestational weight gain were observed.
Studies that have included a focus on weight monitoring and more intensive counseling sessions have found significant effects on gestational gain. Olson et al.101 conducted a study evaluating the effects of periodic weight monitoring, graphing, and education to prevent excessive weight gain during pregnancy in a sample of women from upstate New York. Results indicated that, in the low income women, 33% exceeded weight gain recommendations in the intervention groups compared with 52% in the historical control group. However, no effect was found among the higher income women. Claesson et al.102 conducted a non-randomized evaluation of an intervention program in Sweden for obese women that included weekly 30 minute counseling sessions (focused on weight control and motivation and conducted by midwives) and weekly (1–2 times/week) aqua aerobic classes. Results indicated that the intervention succeeded in reducing magnitude of weight gain during pregnancy (7.5 vs. 9.8 kg, respectively) and 12-week postpartum weight retention (−3.3 vs −.52 kg, respectively), independent of socioeconomic status.
Only two randomized-controlled trials have been conducted evaluating intervention effects on weight gain during pregnancy; both studies had sample sizes less than 120. Polley et al.103 examined whether a behavioral intervention delivered during pregnancy could decrease the percentage of women who gained more than the IOM recommendations. Results indicated that the intervention was successful in decreasing the percentage of normal weight women who exceeded the IOM recommendations relative to no-treatment controls (33% vs. 58%, respectively); no effect was found in overweight but a trend in the opposite direction was observed. In another randomized trial of 50 obese women from Denmark, Wolff et al 104 examined the effects of 10, 1-hour dietary counseling sessions in reducing gestational weight gain. The intervention was found to significantly restrict gestational weight gain relative to controls (6.6 vs 13.3 kg).
These preliminary studies suggest that monitoring weight gain, quantity of food intake, and physical activity are appropriate behavioral targets and, combined with behavioral counseling, appear to curb excessive gestational weight gain and postpartum weight retention. However, larger randomized controlled trials are needed to adequately test the effects of behavioral intervention during pregnancy on the long-term weight retention and obesity.
Are there adverse effects of intervening during pregnancy?
Available data suggest that prevention of excessive weight gain during pregnancy does not have adverse consequence on the developing fetus or mother. In Wolff et al.’s randomized trial,104 the intervention did not have any detectable adverse effects on fetal growth, and fewer incidences of pregnancy and birth complications were observed in the intervention than in the control group. Similarly, Claesson et al.102 found no significant differences between intervention and control groups regarding mode of delivery and neonatal outcomes. Neither Gray-Donald et al.,99 Polley et al.,103 nor Olson et al.105 found any differences in birth weight between intervention and control groups. However, results of these studies require further investigation in larger randomized controlled trials.
Although there are certain contraindications to exercise during pregnancy (e.g., pregnancy-induced hypertension, incompetent cervix), research on moderate aerobic exercise does not appear to have a negative effect on the developing fetus.106,107 Kulpa et al.106 randomly assigned pregnant women to usual care or an exercise condition and found that the exercise intervention significantly reduced the amount of pregnancy weight gain (27 vs. 34 lb) with no adverse effects on gestational age, birth weight, Apgar scores, or obstetric complications. Based, in part, on these data, current recommendations by the American College of Obstetricians and Gynecologists are in line with the Centers for Disease Control and Prevention and American College of Sports Medicine recommendation for exercise: To accumulate 30 minutes or more of moderate exercise on most, if not all days of the week- in the absence of either medical or obstetric complications.108,109
Talking to patients about appropriate weight gain
In light of the increasing rates of high postpartum weight retention and obesity, the IOM is currently re-examining its 1990 gestational weight gain recommendations. 110 Nonetheless, there is strong evidence that prenatal care providers are either not providing weight gain advice or not following existing IOM guidelines when they advise their patients. Approximately one third of women report receiving no weight gain advice from their prenatal care provider,111,112 and, among those patients receiving advice, approximately one third report receiving advice inconsistent with the current IOM guidelines.111 Stotland and colleagues111 evaluated 1198 women and found that 50% of high BMI participants (BMI > 26) reported receiving advice to over-gain; by contrast, 35% of low-BMI participants (BMI < 19.8) report receiving advice to under-gain.111 Similar findings have been reported elsewhere. 33 Reasons for lack of provider adherence to IOM guidelines include lack of awareness, familiarity, and agreement with guidelines.113,114 Some providers may not be aware of the BMI specific weight gain guidelines and advise all women to gain within the same range.111 Also, providers may reduce their weight gain goals for obese patients but overlook more moderate degrees of overweight. 111 In addition, weight gain during pregnancy is a sensitive topic for many patients, and providers may be reluctant to broach the issue.115
Nonetheless, in the absence of definitive empirical findings to guide practice, providing weight gain goals and graphing weight gain during pregnancy in relation to IOM recommendations would appear to be a step to at least reduce the likelihood of excess pregnancy weight gain. Providers’ advice about gestational weight gain is strongly associated with actual weight gain outcomes.33,111,116 Although there is a wide range of weight gain associated with healthy pregnancy outcomes,117 patients who are exceeding recommendations may be advised to “check-in” with their health behaviors and modify any unhealthy eating and exercise habits.103 Promoting physical activity and discouraging sugar-sweetened beverage intake and fast food consumption may also contribute to prevention of excessive gestational weight gain and promote healthy postpartum habits.37 Weight gain graphs and educational materials to promote healthy gestational weight gain are available online from the study from the study by Olson and colleagues105 (http://www.nutritionworks.cornell.edu/features/index.cfm?Action=Course&CourseID=76).
Advantages of intervening during pregnancy include capitalizing on pregnancy’s potential as a “teachable moment” and implementing interventions in the context of usual prenatal care. However, translating research findings into clinical practice remains a challenge. 98,101,118 In practice, financial barriers may prohibit patients from being able to afford, for example, the cost of a scale or transportation to attend clinic visits. Patient adherence to recommended strategies (e.g., weight graphing, physical activity), particularly among diverse patient populations during pregnancy, remains understudied. In clinical practice, a pregnant patient may be seen by multiple practitioners and at varying time intervals, making consistent goal-setting and follow-up with behavioral goals a challenge. Providing educational materials and behavioral counseling may also prove difficult within the time constraints of clinical practice. More research is needed to identify the most effective and disseminable intervention for promoting appropriate gestational weight gain within the context of our current healthcare system. Barriers to providing advice about appropriate weight gain also need to be addressed, including the role of patient adherence, financial barriers, limited physician time and lack of payment by health-insurance and managed-care plans.119,120 To combat the rising obesity epidemic, multi-level interventions across the lifespan will need to be implemented.121 By monitoring and giving appropriate advice about gestational weight gain, health care providers can influence weight gain during pregnancy and potentially reduce the incidence of overweight and obesity in women and children.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847– 2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 2.Flegal K, Carroll MD, Ogden CL, Johnson CL. Prevalence of trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006 Apr 5;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.NHLBI. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res. 1998;6:51S–210S. [PubMed] [Google Scholar]
- 5.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160(7):898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 6.Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17(9):961–969. doi: 10.2337/diacare.17.9.961. [DOI] [PubMed] [Google Scholar]
- 7.Sower J. Modest weight gain and the development of diabetes: another perspective. Ann Intern Med. 1995;122:548–549. doi: 10.7326/0003-4819-122-7-199504010-00012. [DOI] [PubMed] [Google Scholar]
- 8.Harris HE, Ellison GTH, Hollliday M, Lucassen E. The impact of pregnancy on the long term weight gain of primiparous women in England. Int J Obes Relat Metab Disord. 1997;21:747–755. doi: 10.1038/sj.ijo.0800466. [DOI] [PubMed] [Google Scholar]
- 9.Rossner S. Pregnancy, weight cycling and weight gain in obesity. Int J Obes Relat Metab Disord. 1992;16:145–147. [PubMed] [Google Scholar]
- 10.Newcombe RG. Development of obesity in parous women. J Epidemiol Community Health. 1982;36:306–309. doi: 10.1136/jech.36.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown JE, Kaye SA, Folsom AR. Parity-related weight change in women. Int J Obesity. 1992;16:627–631. [PubMed] [Google Scholar]
- 12.Williamson DF, Madans J, Pamak E, Flegal KM, Kendrick JS, Serdula MK. A propsective study of childbearing and 10-year weight gain in U.S. white women 25 to 45 years of age. Int J Obes. 1994;18:561–569. [PubMed] [Google Scholar]
- 13.Cederlof R, Kaij L. The effect of childbearing on body weight: a twin control study. Acta Psychiatrica Scandinavica. 1970;219:47–49. [Google Scholar]
- 14.Prentice AM, Whitehead RG, Roberts SB, Paul AA. Long-term energy balance in child-bearing Gambian women. Am J Clin Nutr. 1981;34:2790–2799. doi: 10.1093/ajcn/34.12.2790. [DOI] [PubMed] [Google Scholar]
- 15.Ohlin A, Rossner J. Maternal body weight development after pregnancy. Int J Obes Relat Metab Disord. 1990;14:159–173. [PubMed] [Google Scholar]
- 16.Hunt SC, Daines MM, Adams TD, Heath EM, Williams RR. Pregnancy weight retention in morbid obesity. Obes Res. 1995;3:121–130. doi: 10.1002/j.1550-8528.1995.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 17.Smith DE, Lewis CE, Caveny JL, Perkins LL, Burke GL, Bild DE. Longitudinal changes in adiposity associated with pregnancy: The CARDIA Study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 18.Gunderson EP, Murtaugh MA, Lewis CE, Quesenberry CP, West DS, Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J Obes. 2004;28:525–535. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keppel K, Taffel S. Pregnancy-related weight gain and retention: implications of the 1990 Institute of Medicine guidelines. Am J Pub Health. 1993;83:1100–1103. doi: 10.2105/ajph.83.8.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kac G, Benicio MH, Velasquez-Melendez G, Valente JG, Struchiner CJ. Gestational weight gain and prepregnancy weight influence postpartum weight retention in a cohort of Brazilian women. J Nutr. 2004;134(3):661–666. doi: 10.1093/jn/134.3.661. [DOI] [PubMed] [Google Scholar]
- 21.Greene GW, Smiciklas-Wright H, Scholl TO, Karp RJ. Postpartum weight change: how much of the weight gained in pregnancy will be lost after delivery? Obstet Gynecol. 1988;71:701–707. [PubMed] [Google Scholar]
- 22.Linne Y, Dye L, Barkeling B, Rossner S. Long-term weight development in women: a 15-year follow-up of the effects of pregnancy. Obes Res. 2004 Jul;12(7):1166–1178. doi: 10.1038/oby.2004.146. [DOI] [PubMed] [Google Scholar]
- 23.Rooney BL, Schauberger CW. Excess pregnancy weight gain and long-term obesity:One decade later. Obstet Gynecol. 2002;100(2):245–252. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- 24.Linne Y, Dye L, Rossner S. Long-term weight development in women: a 15-year follow-up of the effects of pregnancy. Obes Res. 2004;12(7):1116–1178. doi: 10.1038/oby.2004.146. [DOI] [PubMed] [Google Scholar]
- 25.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 1999;21(2):261–275. doi: 10.1093/oxfordjournals.epirev.a018001. [DOI] [PubMed] [Google Scholar]
- 26.Scholl TO, Hediger ML, Schall JI, Ances IG, Smith WK. Gestational weight gain, pregnancy outcome, and postpartum weight retention. Obstet Gynecol. 1995;86:423–427. doi: 10.1016/0029-7844(95)00190-3. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine (U.S.). Subcommittee on Nutritional Status and Weight Gain during Pregnancy., Institute of Medicine (U.S.) Nutrition during pregnancy : part I, weight gain : part II, nutrient supplements. Washington, D.C.: National Academy Press; 1990. Subcommittee on Dietary Intake and Nutrient Supplements during Pregnancy. [Google Scholar]
- 28.Olson CM, Strawderman MS, Hinton PS, Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes. 2003;27:117–127. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 29.Carmichael SL, Abrams B, Selvin S. The pattern of maternal weight gain in women with good pregnancy outcomes. Am J Pub Health. 1997;87(12):1984–1988. doi: 10.2105/ajph.87.12.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hellerstedt W, Himes J, Story M, Alton IR, Edwards L. The effects of cigarette smoking and gestational weight change on birth outcomes in obese and normal-weight women. Am J Pub Health. 1997;87:591–596. doi: 10.2105/ajph.87.4.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abrams B, Altman SL, Pickett KE. Pregnancy weight gain: still controversial. Am J Clin Nutr. 2000;71 (suppl):1233s–1241s. doi: 10.1093/ajcn/71.5.1233s. [DOI] [PubMed] [Google Scholar]
- 32.Shepard MJ, Saftlas AF, Leo-Summers L, Bracken MB. Maternal anthropometric factors and risk of primary cesarean delivery. Am J Pub Health. 1998;88:1334–1538. doi: 10.2105/ajph.88.10.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cogswell ME, Serdula MK, Hungerford DW, Yip R. Gestational weight gain among averageweight and overweight women-what is excessive? Am J Obstet Gynecol. 1995;172:705–712. doi: 10.1016/0002-9378(95)90598-7. [DOI] [PubMed] [Google Scholar]
- 34.Witter F, Caufield L, Stolzfus R. Influence of maternal anthropometric status and birth weight on the risk of cesarean delivery. Obstet Gynecol. 1995;85:947–951. doi: 10.1016/0029-7844(95)00082-3. [DOI] [PubMed] [Google Scholar]
- 35.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007 Apr;196(4):322 e321–328. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olson CM, Strawderman MS, Dennison BA. Maternal weight gain during pregnancy and child weight at age 3 years. Matern Child Health J. 2008 Sep 26; doi: 10.1007/s10995-008-0413-6. [DOI] [PubMed] [Google Scholar]
- 37.Gore S, Brown DM, Smith-West D. The role of postpartum weight retention in obesity among women: a review of evidence. Ann Behav Med. 2003;26(2):149–159. doi: 10.1207/S15324796ABM2602_07. [DOI] [PubMed] [Google Scholar]
- 38.Gunderson EP, Abrams B, Selvin S. The relative importance of gestational gain and maternal characteristics associated with the risk of becoming overweight after pregnancy. Int J Obes Relat Metab Disord. 2000;24(12):1660–1668. doi: 10.1038/sj.ijo.0801456. [DOI] [PubMed] [Google Scholar]
- 39.Linne Y, Dye L, Rossner S. Weight development over time in parous women: the SPAWN study15 years follow-up. Int J Obes. 2003;12:1516–1522. doi: 10.1038/sj.ijo.0802441. [DOI] [PubMed] [Google Scholar]
- 40.Parker JD, Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81:768–774. [PubMed] [Google Scholar]
- 41.Olson CM. A call for intervention in pregnancy to prevent maternal and child obesity. Am J Prev Med. 2007 Nov;33(5):435–436. doi: 10.1016/j.amepre.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 42.Olafsdottir AS, Skuladottir GV, Thorsdottir I, Hauksson A, Steingrimsdottir L. Maternal diet in early and late pregnancy in relation to weight gain. Int J Obes (Lond) 2006 Mar;30(3):492–499. doi: 10.1038/sj.ijo.0803184. [DOI] [PubMed] [Google Scholar]
- 43.Olson CM, Strawderman MS, Hinton PS, Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes Relat Metab Disord. 2003 Jan;27(1):117–127. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 44.Olson CM, Strawderman MS. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. J Am Diet Assoc. 2003 Jan;103(1):48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 45.Lagiou P, Tamimi RM, Mucci LA, Adami HO, Hsieh CC, Trichopoulos D. Diet during pregnancy in relation to maternal weight gain and birth size. Eur J Clin Nutr. 2004 Feb;58(2):231–237. doi: 10.1038/sj.ejcn.1601771. [DOI] [PubMed] [Google Scholar]
- 46.Sternfeld B, Quesenberry CP, Jr, Eskenazi B, Newman LA. Exercise during pregnancy and pregnancy outcome. Med Sci Sports Exerc. 1995 May;27(5):634–640. [PubMed] [Google Scholar]
- 47.Schieve LA, Cogswell ME, Scanlon KS. An empiric evaluation of the Institute of Medicine’s pregnancy guidelines by race. Obstet Gynecol. 1998;91:878–884. doi: 10.1016/s0029-7844(98)00106-9. [DOI] [PubMed] [Google Scholar]
- 48.Olson CM, Strawderman MS. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. JADA. 2003;103:48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 49.Little RE, Weinberg CR. Risk factors for antepartum and intrapartum stillbirth. Am J Epidemiol. 1993;137:1177–1189. doi: 10.1093/oxfordjournals.aje.a116620. [DOI] [PubMed] [Google Scholar]
- 50.Cnattingius S, Bergsrom R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. New Eng J Med. 1998;338:147–152. doi: 10.1056/NEJM199801153380302. [DOI] [PubMed] [Google Scholar]
- 51.Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287, 213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175–1182. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 52.Stephansson O, Dickman PW, Johansson A, Cnattingius S. Maternal weight, pregnancy weight gain, and the risk of antepartum stillbirth. Am J Obstet Gynecol. 2001;184:463–469. doi: 10.1067/mob.2001.109591. [DOI] [PubMed] [Google Scholar]
- 53.Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod. 2004 Jul;19(7):1644–1646. doi: 10.1093/humrep/deh277. [DOI] [PubMed] [Google Scholar]
- 54.Waller DK, Mills JL, Simpson JL, Cunningham GC, Conley MR, Lassman MR, et al. Are obese women at higher risk for producing malformed offspring? Am J Obstet Gynecol. 1994 Feb;170(2):541–548. doi: 10.1016/s0002-9378(94)70224-1. [DOI] [PubMed] [Google Scholar]
- 55.Cedergren MI, Kallen BA. Maternal obesity and infant heart defects. Obes Res. 2003 Sep;11(9):1065–1071. doi: 10.1038/oby.2003.146. [DOI] [PubMed] [Google Scholar]
- 56.Watkins ML, Rasmussen SA, Honein MA, Botto LD, Moore CA. Maternal obesity and risk for birth defects. Pediatrics. 2003 May;111(5 Part 2):1152–1158. [PubMed] [Google Scholar]
- 57.Ehrenberg HM, Dierker L, Milluzzi C, Mercer BM. Prevalence of maternal obesity in an urban center. Am J Obstet Gynecol. 2002 Nov;187(5):1189–1193. doi: 10.1067/mob.2002.127125. [DOI] [PubMed] [Google Scholar]
- 58.Usha Kiran TS, Hemmadi S, Bethel J, Evans J. Outcome of pregnancy in a woman with an increased body mass index. BJOG. 2005 Jun;112(6):768–772. doi: 10.1111/j.1471-0528.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 59.Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001 Aug;25(8):1175–1182. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 60.Johnson JW, Longmate JA, Frentzen B. Excessive maternal weight and pregnancy outcome. Am J Obstet Gynecol. 1992 Aug;167(2):353–370. doi: 10.1016/s0002-9378(11)91414-8. discussion 370–352. [DOI] [PubMed] [Google Scholar]
- 61.Stotland NE, Washington AE, Caughey AB. Prepregnancy body mass index and the length of gestation at term. Am J Obstet Gynecol. 2007 Oct;197(4):378 e371–375. doi: 10.1016/j.ajog.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 62.Abrams BF, Laros RK., Jr Prepregnancy weight, weight gain, and birth weight. Am J Obstet Gynecol. 1986 Mar;154(3):503–509. doi: 10.1016/0002-9378(86)90591-0. [DOI] [PubMed] [Google Scholar]
- 63.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002 Aug 10;360(9331):473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 64.Kowall J, Clark G, Nino-Murcia G, Powell N. Precipitation of obstructive sleep apnea during pregnancy. Obstet Gynecol. 1989 Sep;74(3 Pt 2):453–455. [PubMed] [Google Scholar]
- 65.Lewis DF, Chesson AL, Edwards MS, Weeks JW, Adair CD. Obstructive sleep apnea during pregnancy resulting in pulmonary hypertension. South Med J. 1998 Aug;91(8):761–762. doi: 10.1097/00007611-199808000-00013. [DOI] [PubMed] [Google Scholar]
- 66.Saravanakumar K, Rao SG, Cooper GM. Obesity and obstetric anaesthesia. Anaesthesia. 2006 Jan;61(1):36–48. doi: 10.1111/j.1365-2044.2005.04433.x. [DOI] [PubMed] [Google Scholar]
- 67.Perlow JH, Morgan MA. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994 Feb;170(2):560–565. doi: 10.1016/s0002-9378(94)70227-6. [DOI] [PubMed] [Google Scholar]
- 68.Hood DD, Dewan DM. Anesthetic and obstetric outcome in morbidly obese parturients. Anesthesiology. 1993 Dec;79(6):1210–1218. doi: 10.1097/00000542-199312000-00011. [DOI] [PubMed] [Google Scholar]
- 69.Galtier-Dereure F, Montpeyroux F, Boulot P, Bringer J, Jaffiol C. Weight excess before pregnancy: complications and cost. Int J Obes Relat Metab Disord. 1995 Jul;19(7):443–448. [PubMed] [Google Scholar]
- 70.Rasmussen KM, Kjolhede CL. Prepregnant overweight and obesity diminish the prolactin response to suckling in the first week postpartum. Pediatrics. 2004 May;113(5):e465–471. doi: 10.1542/peds.113.5.e465. [DOI] [PubMed] [Google Scholar]
- 71.Weiss JL, Malone FD, Emig D, Ball RH, Nyberg DA, Comstock CH, et al. Obesity, obstetric complications and cesarean delivery rate--a population-based screening study. Am J Obstet Gynecol. 2004 Apr;190(4):1091–1097. doi: 10.1016/j.ajog.2003.09.058. [DOI] [PubMed] [Google Scholar]
- 72.Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004 Feb;103(2):219–224. doi: 10.1097/01.AOG.0000107291.46159.00. [DOI] [PubMed] [Google Scholar]
- 73.Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003 Apr;11(4):496–506. doi: 10.1038/oby.2003.69. [DOI] [PubMed] [Google Scholar]
- 74.Dixon JB, Dixon ME, O’Brien PE. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstet Gynecol. 2005 Nov;106(5 Pt 1):965–972. doi: 10.1097/01.AOG.0000181821.82022.82. [DOI] [PubMed] [Google Scholar]
- 75.Wittgrove AC, Jester L, Wittgrove P, Clark GW. Pregnancy following gastric bypass for morbid obesity. Obes Surg. 1998 Aug;8(4):461–464. doi: 10.1381/096089298765554368. discussion 465–466. [DOI] [PubMed] [Google Scholar]
- 76.American Gastroenterological Association medical position statement on Obesity. Gastroenterology. 2002 Sep;123(3):879–881. doi: 10.1053/gast.2002.35513. [DOI] [PubMed] [Google Scholar]
- 77.Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;6(3):219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- 78.Wing RR, Tate DF, Gorin A, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. New Engl J Med. 2006;346:393–403. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 79.Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther. 1993;24(3):377–394. [Google Scholar]
- 80.Wadden TA, Foster GD. Behavioral treatment of obesity. Med Clin N Amer. 2000;84(2):441– 462. doi: 10.1016/s0025-7125(05)70230-3. [DOI] [PubMed] [Google Scholar]
- 81.Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring) 2007 Dec;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- 82.Ditschuneit HH, Flechtner-Mors M, Adler G. Metabolic and weight loss effects of long-term dietary intervention in obese subjects. Am J Clin Nutr. 1999 doi: 10.1093/ajcn/69.2.198. [DOI] [PubMed] [Google Scholar]
- 83.Heymsfield SB, van Mierlo CA, van der Knaap HC, Heo M, Frier HI. Weight management using a meal replacement strategy: meta and pooling analysis from six studies. Int J Obes Relat Metab Disord. 2003 May;27(5):537–549. doi: 10.1038/sj.ijo.0802258. [DOI] [PubMed] [Google Scholar]
- 84.McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139(11):933–949. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 85.Abrams B, Parker JD. Maternal weight gain in women with good pregnancy outcome. Obstet Gynecol. 1990;76(1):1–7. [PubMed] [Google Scholar]
- 86.Winzer-Serhan UH. Long-term consequences of maternal smoking and developmental chronic nicotine exposure. Front Biosci. 2008;13:636–649. doi: 10.2741/2708. [DOI] [PubMed] [Google Scholar]
- 87.Mendez MA, Torrent M, Ferrer C, Ribas-Fito N, Sunyer J. Maternal smoking very early in pregnancy is related to child overweight at age 5–7 y. Am J Clin Nutr. 2008 Jun;87(6):1906–1913. doi: 10.1093/ajcn/87.6.1906. [DOI] [PubMed] [Google Scholar]
- 88.Dubois L, Girard M. Early determinants of overweight at 4.5 years in a population-based longitudinal study. Int J Obes (Lond) 2006 Apr;30(4):610–617. doi: 10.1038/sj.ijo.0803141. [DOI] [PubMed] [Google Scholar]
- 89.Walker LO. Predictors of weight gain at 6 and 18 months after childbirth: a pilot study. J Obest Gynecol Neonat Nurs. 1996;25:39–48. doi: 10.1111/j.1552-6909.1996.tb02511.x. [DOI] [PubMed] [Google Scholar]
- 90.Walker LO. Weight and weight related distress after childbirth: relationships of stress, social support, and depressive symptoms. J Hol Nurs. 1997;15:389–405. doi: 10.1177/089801019701500406. [DOI] [PubMed] [Google Scholar]
- 91.Dishy V, Gupta S, Landau R, Xie H, Kim RB, Smiley RM, et al. G-protein [beta]3 subunit 825 C/T polymorphism is associated with weight gain during pregnancy. Pharmacogenetics. 2003;13(4):241–242. doi: 10.1097/00008571-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 92.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 93.Lazarus RS. Coping Theory and Research : Past, Present, and Future. Psychosom Med. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 94.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;8(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 95.McBride CM, Puleo E, Pollak KI, Clipp EC, Woolford S, Emmons KM. Understanding the role of cancer worry in creating a “teachable moment” for multiple risk factor reduction. Soc Sci Med. 2008 Feb;66(3):790–800. doi: 10.1016/j.socscimed.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Clissold TL, Hopkins WG, Seddon RJ. Lifestyle behaviours during pregnancy. N Z Med J. 1991 Mar 27;104(908):111–112. [PubMed] [Google Scholar]
- 97.Sabir M, Breckman R, Meador R, Wethington E, Reid MC, Pillemer K. The CITRA researchpractice consensus-workshop model: exploring a new method of research translation in aging. Gerontologist. 2006 Dec;46(6):833–839. doi: 10.1093/geront/46.6.833. [DOI] [PubMed] [Google Scholar]
- 98.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 99.Gray-Donald K, Robinson E, Collier A, David K, Renaud L, Rodrigues S. Intervening to reduce weight gain in pregnancy and gestational diabetes mellitus in Cree communities: An evaluation. Canad Med Assoc J. 2000;163(10):1247–1251. [PMC free article] [PubMed] [Google Scholar]
- 100.Kinnunen TI, Pasanen M, Aittasalo M, Fogelholm M, Hilakivi-Clarke L, Weiderpass E, et al. Preventing excessive weight gain during pregnancy - a controlled trial in primary health care. Eur J Clin Nutr. 2007 Jul;61(7):884–891. doi: 10.1038/sj.ejcn.1602602. [DOI] [PubMed] [Google Scholar]
- 101.Ornstein S, Nietert PJ, Jenkins RG, Wessell AM, Nemeth LS, Rose HL. Improving the translation of research into primary care practice: results of a national quality improvement demonstration project. Jt Comm J Qual Patient Saf. 2008 Jul;34(7):379–390. doi: 10.1016/s1553-7250(08)34048-3. [DOI] [PubMed] [Google Scholar]
- 102.Claesson IM, Sydsjo G, Brynhildsen J, Cedergren M, Jeppsson A, Nystrom F, et al. Weight gain restriction for obese pregnant women: a case-control intervention study. BJOG. 2008 Jan;115(1):44–50. doi: 10.1111/j.1471-0528.2007.01531.x. [DOI] [PubMed] [Google Scholar]
- 103.Polley BA, Wing RR, Meier A, Sims C, DeBranski C. Preventing excessive weight gain during pregnancy in overweight and normal weight women. Ann Behav Med. 1997;19 (Suppl):S071. [Google Scholar]
- 104.Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes (Lond) 2008 Mar;32(3):495–501. doi: 10.1038/sj.ijo.0803710. [DOI] [PubMed] [Google Scholar]
- 105.Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gynecol. 2004 Aug;191(2):530–536. doi: 10.1016/j.ajog.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 106.Kulpa PJ, White BM, Visscher R. Aerobic exercise in pregnancy. Am J Obstet Gynecol. 1987;156:1395–1403. doi: 10.1016/0002-9378(87)90006-8. [DOI] [PubMed] [Google Scholar]
- 107.Jovanovic-Peterson L, Durak EP, Peterson CM. Randomized trial of diet versus diet plus cardiovascular conditioning on glucose levels in gestational diabetes. Am J Obstet Gynecol. 1989;161:415–419. doi: 10.1016/0002-9378(89)90534-6. [DOI] [PubMed] [Google Scholar]
- 108.Gynecologists ACoOa. Exercise during pregnancy and the postpartum period. Washington, D. C.: Technical Bulletin #189; 1994. [Google Scholar]
- 109.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 110.Committee on the Impact of Pregnancy Weight on Maternal and Child Health, National Research Council (U.S.). Board on Children Youth and Families., Institute of Medicine (U.S.). Food and Nutrition Board. Influence of pregnancy weight on maternal and child health : workshop report. Washington, D.C.: National Academies Press; 2007. [Google Scholar]
- 111.Stotland NE, Haas JS, Brawarsky P, Jackson RA, Fuentes-Afflick E, Escobar GJ. Body mass index, provider advice, and target gestational weight gain. Obstet Gynecol. 2005 Mar;105(3):633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- 112.Cogswell ME, Scanlon KS, Fein SB, Schieve LA. Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstet Gynecol. 1999 Oct;94(4):616–622. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 113.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999 Oct 20;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 114.Feig DS, Naylor CD. Eating for two: are guidelines for weight gain during pregnancy too liberal? Lancet. 1998 Apr 4;351(9108):1054–1055. doi: 10.1016/S0140-6736(97)06261-2. [DOI] [PubMed] [Google Scholar]
- 115.Wadden TA, Didie E. What’s in a name? Patients’ preferred terms for describing obesity. Obes Res. 2003 Sep;11(9):1140–1146. doi: 10.1038/oby.2003.155. [DOI] [PubMed] [Google Scholar]
- 116.Taffel SM, Keppel KG. Advice about weight gain during pregnancy and actual weight gain. Am J Public Health. 1986;76:1396–1399. doi: 10.2105/ajph.76.12.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Abrams B, Altman SL, Pickett KE. Pregnancy weight gain: still controversial. Am J Clin Nutr. 2000 May;71(5 Suppl):1233S–1241S. doi: 10.1093/ajcn/71.5.1233s. [DOI] [PubMed] [Google Scholar]
- 118.Baumbusch JL, Kirkham SR, Khan KB, McDonald H, Semeniuk P, Tan E, et al. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health. 2008 Apr;31(2):130–140. doi: 10.1002/nur.20242. [DOI] [PubMed] [Google Scholar]
- 119.Lyznicki JM, Young DC, Riggs JA, Davis RM. Obesity: assessment and management in primary care. Am Fam Physician. 2001 Jun 1;63(11):2185–2196. [PubMed] [Google Scholar]
- 120.Abramson S, Stein J, Schaufele M, Frates E, Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000;10(1):40–48. doi: 10.1097/00042752-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 121.Phelan S, Foster GD. Environmental challenges and assessment. In: Berdanier CJDEF, editor. CRC Handbook of Nutrition and Food. Atlanta: CRC Press; 2007. pp. 649–656. [Google Scholar]
- 122.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003 Apr;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]


