Abstract
Arthropod-borne viruses (arboviruses) are important causes of human disease nearly worldwide. All arboviruses circulate among wild animals, and many cause disease after spillover transmission to humans and agriculturally important domestic animals that are incidental or dead-end hosts. Viruses such as dengue (DENV) and chikungunya (CHIKV) viruses that have lost the requirement for enzootic amplification now produce extensive epidemics in tropical urban centers. Many arboviruses recently have increased in importance as human and veterinary pathogens using a variety of mechanisms.
Beginning in 1999, West Nile virus (WNV) underwent a dramatic geographic expansion into the Americas. High amplification associated with avian virulence coupled with adaptation for replication at higher temperatures in mosquito vectors, it has caused the largest epidemic of arboviral encephalitis ever reported in the Americas. Japanese encephalitis virus (JEV), the most frequent arboviral cause of encephalitis worldwide, has spread throughout most of Asia and as far south as Australia from its putative origin in Indonesia and Malaysia. JEV has caused major epidemics as it invaded new areas, often enabled by rice culture and amplification in domesticated swine. Rift Valley fever virus (RVFV), another arbovirus that infects humans after amplification in domesticated animals, undergoes epizootic transmission during wet years following droughts. Warming of the Indian Ocean, linked to the El Niño-Southern Oscillation in the Pacific, leads to heavy rainfall in east Africa inundating surface pools and vertically-infected mosquito eggs laid during previous seasons. Like WNV, JEV and RVFV could become epizootic and epidemic in the Americas if introduced unintentionally via commerce or intentionally for nefarious purposes. Climate warming also could facilitate the expansion of the distributions of many arboviruses, as documented for bluetongue viruses (BTV), major pathogens of ruminants. BTV, especially BTV-8, invaded Europe after climate warming enabled the major midge vector to expand is distribution northward into southern Europe and extended the transmission season and vectorial capacity of local midge species.
Perhaps the greatest health risk of arboviral emergence comes from extensive tropical urbanization and the colonization of this expanding habitat by the highly anthropophilic (attracted to humans) mosquito, Aedes aegypti. These factors led to the emergence of permanent endemic cycles of urban DENV and chikungunya virus (CHIKV), as well as seasonal interhuman transmission of yellow fever and Zika viruses. The recent invasion into the Americas, Europe and Africa of Ae. albopictus, an important CHIKV and secondary DENV vector, could enhance urban transmission of these viruses in tropical as well as temperate regions. The minimal requirements for sustained endemic arbovirus transmission, adequate human viremia and vector competence of Ae. aegypti and/or Ae. albopictus, may be met by two other viruses with the potential to become major human pathogens: Venezuelan equine encephalitis virus, already an important cause of neurological disease in humans and equids throughout the Americas, and Mayaro virus, a close relative of CHIKV that produces a comparably debilitating arthralgic disease in South America. Further research is needed to understand the potential of these and other arboviruses to emerge in the future, invade new geographic areas, and become important public and veterinary health problems.
Keywords: Arbovirus, emergence, epidemic, flavivirus, alphavirus, climate change
I. Introduction to the Arboviruses
Arthropod-borne viruses (arboviruses) are transmitted biologically among vertebrate hosts by hematophagous (blood feeding) arthropod vectors such as mosquitoes and other biting flies, and ticks. Being, by definition, biologically transmitted, arboviruses must replicate in the arthropod vector prior to transmission, as opposed to being mechanically transmitted, without replication in the vector, through contaminated mouthparts (Weaver, 1997). Biological transmission can be vertical, involving the passage of the virus from an infected female vector to both male and female offspring. Horizontal transmission can be venereal, from a vertically infected male directly to a female vector, as well as oral from a vector to a vertebrate host via the saliva during blood feeding. The latter horizontal mode of transmission is most common for the majority of arboviruses and involves infection of the vector alimentary tract following a viremic bloodmeal, dissemination of the virus in the vector, and eventual virus replication in the salivary glands, followed by the injection of infectious saliva during blood feeding.
The arboviruses include a wide variety of RNA virus taxa including the alphaviruses (genus Alphavirus, one of 2 genera in the family Togaviridae); the flaviviruses (genus Flavivirus, one of 3 genera in the family Flaviviridae); the bunyaviruses (Bunyaviridae: Bunyavirus), nairoviruses (Bunyaviridae: Nairovirus) and phleboviruses (Bunyaviridae: Phlebovirus); the orbiviruses (one of 9 genera in the family Reoviridae); the vesiculoviruses (one of 6 genera in the family Rhabdoviridae) and the thogotoviruses (one of 4 genera in the family Orthomyxoviridae). These groups of RNA viruses have a variety of types of RNA genomes and replication strategies, suggesting that the arthropod-borne transmission strategy has arisen many times during the evolution of RNA viruses. The only known DNA arbovirus is African swine fever virus (Asfarviridae: Asfarvirus)(Calisher and Karabatsos, 1988; Karabatsos, 1985; van Regenmortel et al., 2000), and the paucity of DNA arboviruses suggests that the greater genetic plasticity and higher mutation rates exhibited by RNA viruses (Holland and Domingo, 1998) allow them to accommodate a cycle of alternating replication in disparate vertebrate and invertebrate hosts.
Arboviruses circulate among wild animals, and cause disease after spillover transmission to humans and/or domestic animals that are incidental or dead-end hosts. Viruses such as dengue (DENV) and chikungunya (CHIKV) that have lost the requirement for enzootic amplification now produce extensive epidemics. Many arboviruses that have evolved and diversified in the tropics have produced virulent and invasive strains that have caused major outbreaks at temperate latitudes. The ability of these viruses to cause human disease depends on factors ranging from epidemiology to viral genetics. Herein, we review how some of these factors have led to arboviral emergences and resulted in human disease, by using several examples of viruses with a known epidemic history as well as some that have a poorly recognized epidemic potential.
II. Factors associated with Arbovirus Emergence or Invasion
For arboviral amplification to progress rapidly to epidemic levels, competent vector and vertebrate host populations must intersect repeatedly within a permissive environment. This focus or nidus of transmission may be temporally and/or spatially constrained by host or virus ecology, and may vary in complexity depending upon virus epidemiology. Zoonoses exploiting complex rural or suburban ecosystems may have multiple vectors and infect a variety of vertebrate host species, whereas anthroponoses (diseases transmitted from humans to other animals) exploiting urban environments may require only a single anthropophilic vector and human hosts for amplification. Humans are exposed to arboviruses when they invade rural environments or when bridge vectors bring viruses into peridomestic environments. In contrast, for many anthroponoses, human habitations form the nidus of transmission. Frequently arboviruses persist at low or even tenuous maintenance levels until some change in single or multiple factors facilitate rapid and widespread amplification. Although in-depth reviews of these factors have been published (Committee of Emerging Microbial Threats to Health, 2001; Davis and Lederberg, 2001; Fauci, 2005; Gubler, 1998; Mackenzie et al., 2001), recent circumglobal changes in climate and other anthropogenic (derived from human activities) factors, epidemiology, and viral genetics have stimulated the need to update and extend information on the role of these changes in the emergence of arboviruses.
Emerging or invading arboviruses may amplify to epidemic levels because natural systems have been perturbed by changes in viral genetics, host or vector population composition or dynamics, and/or environmental structure that frequently are of anthropogenic origin. Often, outbreaks of emerging arboviruses can be related to relatively small changes in viral genetics or to the introduction of new strains that have increased virulence and viremia levels in vertebrates, thereby expanding host range and increasing amplification potential. Alternatively, genetic changes may enhance vector competence and therefore transmission rates. Changes in vertebrate or vector host species composition may be related to environmental change expanding old or creating new niches, or to invasions related to travel or commerce. Vector range extensions into permissive environments frequently are followed by invasions of the arboviruses they transmit. These invasions typically have been facilitated by travel and commerce, especially over repeatedly traveled routes. Receptivity of an area to viral invasion may be related strongly to environmental conditions conducive to viral replication. Recently, seasonal durations and geographic limits have been expanding as the earth warms. Expanding urbanization has resulted not only in the extreme concentrations of susceptible human hosts, frequently living under socioeconomic conditions conducive to vector population expansion and transmission, but also in the creation of urban heat islands that facilitate transmission.
Emergence of an arbovirus may require change by one or several of the above-mentioned factors. In this review, we analyze the cascade of factors that have facilitated the recent local and circumglobal emergence of selected arboviruses. These arboviruses were chosen because of their public or veterinary health significance, the combinations of factors leading to their emergence, and as examples to help understand the critical features of emerging arboviral risks and how they may be mitigated. Finally, we conclude with a few examples of arboviruses that have been largely ignored, but possess the potential to emerge. Throughout this review, our understanding of the temporal and spatial patterns of invasion and emergence has been complicated by diagnosis, retention and sequencing of available archival strains, and methods of characterization.
III. Examples of Arboviruses with a History of Invasion and Emergence
A. West Nile virus (WNV)
Distribution and Health Significance
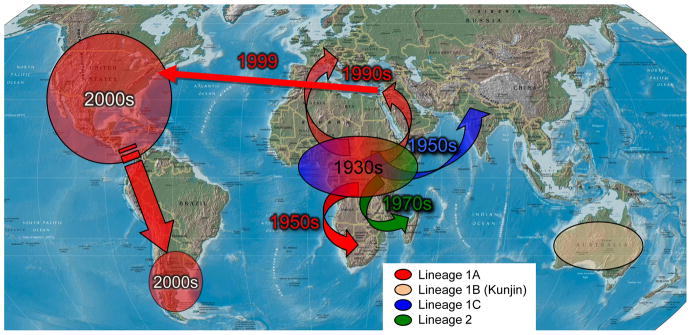
West Nile virus (WNV) is positioned taxonomically within the Japanese encephalitis virus (JEV) serocomplex in the genus Flavivirus. It is maintained and amplified in nature within an enzootic transmission cycle among passeriform birds and Culex mosquitoes, with outbreaks caused by tangential or spillover transmission to equids and humans, dead-end hosts that produce viremias inadequate for mosquito infection. WNV is distributed circumglobally, with two main genetic lineages: Lineage 1 is widely distributed and highly invasive, whereas Lineage 2 appears to have remained enzootic in Africa (Fig. 1). Lineages 3 and 4 have been described from single isolates from Central Europe, but their taxonomic status and medical importance are unclear, whereas Lineage 5 appears to be confined to India (Kramer et al., 2008). Recognized subclades of Lineage 1 include 1a that is widespread throughout Africa and the Mediterranean, Lineage 1b (aka Kunjin virus) that is restricted to Australia, and Lineage 1c that is found in Central Asia through the central highlands of India (Lanciotti et al., 2002). Historically, the northern distribution of Lineage 1a in Europe and Asia and the southern distribution of 1a and 2 in Africa were thought to be constrained by minimum temperature requirements for efficient replication in the mosquito vector, whereas elsewhere WNV is replaced by other members of the JEV serocomplex from central through eastern Asia to the Torres Straight; Kunjin and Murray Valley encephalitis viruses replace JEV south of the Torres Straight (Hall et al., 2002). Previously, the wide distribution of St. Louis encephalitis virus (SLEV) in the New World may have deterred the introduction of WNV, although there has been no evidence presented that WNV was introduced other than once in 1999.
Fig. 1.
Probable temporal sequence and dispersal routes of WNV from its proposed center of origin in sub-Saharan Africa (Powers et al., 2000)(Lanciotti et al. 2002).
Factors Associated with WNV Emergence
Commerce and the international dispersal of mosquitoes in the Cx. pipiens complex (Fonseca et al., 2004; Vinagradova, 2000), the intentional and/or unintentional introduction of the house sparrow [Passer domesticus (Zimmerman, 2002)], climate warming, and perhaps the decline of SLEV may have set the stage for the emergence of WNV in Europe and the New World. Although a wide variety of mosquitoes in the genus Culex have become involved regionally in WNV transmission within North America and may be highly competent vectors, members of the commensal Culex pipiens complex appear to be associated most closely with urban/suburban outbreaks and human infection (Komar, 2003). Similarly, the ubiquitous and aggressively invasive house sparrow is multibrooded and a highly competent host for most WNV strains (Kramer et al., 2008; Langevin et al., 2005; Nemeth et al., 2009), providing the availability of an almost circumglobal maintenance and amplification host. Replication of WNV in the poikilothermic mosquito host is temperature-limited and progresses most effectively under warm midsummer conditions (Kilpatrick et al., 2008; Reisen et al., 2006). Climate change at northern temperate latitudes recently has made these areas more conducive to WNV invasion. In the New World through the mid-1970s, large and fairly widespread SLEV epidemics (Monath, 1980) may have elevated avian herd immunity sufficient to preclude the introduction and establishment of historic Lineage 1a WNV strains.
Recent outbreaks of WNV were recorded throughout the Mediterranean and then Romania, Central Europe and Russia, where Cx. pipiens appeared to be the primary vector (Fyodorova et al., 2006; Savage et al., 1999). Even during years when human outbreaks were not recorded there, epiornitics followed the introduction of WNV into Israel by southbound migrating birds (Malkinson et al., 2002). Some of these viral strains have appeared to become progressively more virulent for birds (Malkinson et al., 2002) and humans.
WNV was introduced into New York during the summer of 1999, and the nucleotide sequence of the invading strain was related closely to a 1998 isolate from Israel that caused widespread illness in geese (Lanciotti et al., 1999) and contained a mutation in the helicase gene that caused high viremia and mortality in American crows (Brault et al., 2007). Interestingly, the resulting NY outbreak seemed to be amplified among house sparrows (Komar, 2000; Komar et al., 2001), was associated with widespread death in American crows (Hochachka et al., 2004), and was transmitted primarily by Cx. pipiens mosquitoes (Nasci et al., 2001b). WNV overwintered successfully in diapausing Cx. pipiens (Nasci et al., 2001a) and perhaps by bird-to-bird transmission at communal American crow roosts (Dawson et al., 2007). By 2002, WNV had spread to the Midwest and was associated with large outbreaks in Illinois, transmitted by Cx. pipiens, and in Louisiana, transmitted by its southern form, Cx. quinquefasciatus. As WNV exploited new geographic areas, different, but highly competent, avian hosts such as blue jays and American robins became recognized as important amplification hosts (Hamer et al., 2009; Kilpatrick et al., 2006). Concurrently, the founding NY99 strain was replaced by WN02 (Davis et al., 2003), a very closely related New World genotype that is transmitted more efficiently by Culex mosquitoes (Moudy et al., 2007), especially at high temperatures (Kilpatrick et al., 2008). North American Culex are moderately competent laboratory vectors (Goddard et al., 2002; Turell et al., 2000; Turell et al., 2001) and therefore require elevated avian viremias for effective infection (Reisen et al., 2005). In 2003, the WNV epicenter moved west into the prairie biomes and the west Coast, where Cx. tarsalis emerged as a significant vector (Reisen et al., 2004). Amplification and the high incidence of human infection in the Canadian and U.S. prairie biomes were associated with Cx. tarsalis, as well as with above-average summer temperatures that exceeded previous 30 year averages (Reisen et al., 2006).
Like SLEV and eastern (EEEV) and western (WEEV) equine encephalitis viruses, WNV seems to “disappear” into the Neotropics with little evidence of human disease. Extensive searches among resident and migratory birds have discovered antibody-positive individuals at a low rate (Bosch et al., 2007; Deardorff et al., 2006; Dupuis et al., 2003; Dupuis et al., 2005; Farfan-Ale et al., 2004; Farfan-Ale et al., 2006; Lorono-Pino et al., 2003) and blood supply examinations have indicated limited human infections (Sanchez-Guerrero et al., 2006). Outbreaks in humans or equids were not recorded until studies were done in the southern temperate latitudes of Argentina (Morales et al., 2006).
In summary, the large-scale epidemic of WNV in North America was enabled by the high amplification phenotype (associated with high avian virulence) of the invading virus, the naïvete of North American birds, the competence of North American Cx. pipiens for vertical and horizontal transmission, successful overwintering within the mosquito host (Anderson et al., 2006; Anderson et al., 2008), and the slight, but significant, evolutionary changes that facilitated rapid transmission during summer temperatures (Kilpatrick et al., 2008) that may have enabled northern expansion into Canada.
Future trends
WNV is now one of the most broadly distributed arboviruses in the world, being found on all continents except Antarctica (Kramer et al., 2008). Invasion typically has been followed by rapid subsidence of disease (Hayes et al., 2005), but then periodic resurgences whenever adequate vector and susceptible avian populations intersect under permissive climatic conditions. Equids are now protected by widespread intentional and natural vaccination; however, the motivation for human vaccine development may be limited by the low attack rate in humans that has been documented following epidemics (Prince and Hogrefe, 2003). In the near term, protection of the public health will continue to rely on mosquito control, public education, and, hopefully, new therapeutics.
B. Japanese encephalitis virus (JEV)
Distribution and significance
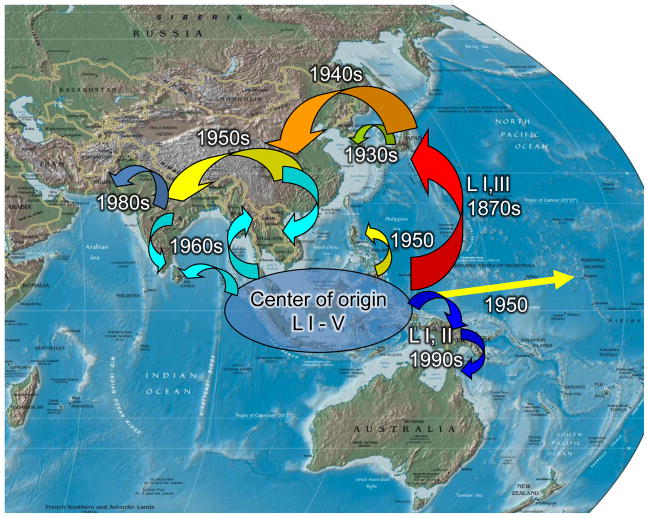
JEV is the most frequent cause of mosquito-borne encephalitis globally and the only encephalitis virus against which large portions of human populations in multiple countries are vaccinated. The public health significance and possibly the global distribution of JEV have been progressively expanding. Since it was first documented as an important cause of encephalitis in Japan in the late 1800s, significant incursions have occurred into Central Asia (Burke and Leake, 1988)(Fig. 2). Currently, more than 3 billion people in Asia reside in areas at risk of JE, with an estimated 30,000–50,000 cases occurring annually (Erlanger et al., 2009).
Fig. 2.
Probable sequence and dispersal routes of JEV from its putative center of origin in the Malay Archipelago (Burke and Leake 1988, Solomon et al. 2003). Pattern of lineage dispersal was difficult to trace.
Taxonomically, Japanese encephalitis virus (JEV) is placed within the genus Flavivirus and is the type virus for the JEV serocomplex that also contains WNV, Murray Valley encephalitis virus and SLEV. JEV is maintained within an ardeid bird – Culex mosquito transmission cycle and is amplified within a domestic swine – Culex cycle. Culex mosquitoes tangentially transmit JEV to equids and humans, which are dead end hosts for the virus (Burke and Leake, 1988). The known distribution of JEV ranges from Korea south to Australia and then northwest into Pakistan (Fig. 2). The distribution of the primary mosquito vector, Culex tritaeniorhynchus, overlaps most of this geographical area, where it is very abundant in association with rice and other irrigated crops. A highly competent laboratory vector (Hammon et al., 1949; Okuno et al., 1975), Cx. tritaeniorhynchus blood feeds predominantly on large mammals (Mitchell et al., 1973; Reisen and Boreham, 1979), including swine, and has been implicated in amplification and tangential transmission (Kono and Kim, 1969). Other Culex in the vishnui, bitaeniorhynchus and pipiens complexes also have also been incriminated as vectors, but have more limited geographic distributions. Expanding irrigated rice cultivation has enabled increases in mosquito vector populations as well as the distribution and abundance of the ardeid maintenance hosts, including the black-crowned night heron (Nycticorax nycticorax) and the Asian cattle egret (Bubulcus ibis coromandus) (Buescher and Scherer, 1959; Buescher et al., 1959; Solomon et al., 2003).
Factors associated with emergence
There is a discrepancy between the proposed JEV evolutionary center of origin (Solomon et al., 2003) and its patterns of expanding distribution as a public health problem as traced by outbreaks (Burke and Leake, 1988). Of the five major genetic lineages, only lineages I, II and III have been found in subtropical or temperate latitudes and are associated with outbreaks of neuroinvasive disease; ancestral lineages IV and V appear restricted to the Indonesian archipelago, where with lineages I – III, they cause limited and sporadic human cases (Fig. 2). Because virgin soil outbreaks typically have been accompanied by extensive neuroinvasive disease in all human age groups as well as disease in pigs, it is unlikely that JEV was a major public health problem in northern Asia until epidemics were recognized in Japan starting in the late 1800s (Burke and Leake, 1988; Erlanger et al., 2009; van den Hurk et al., 2009). Tracing JEV (mostly lineage I) as an emerging health problem from the first epidemics in Japan, sequential outbreaks were documented in northeast (Korea, China and Taiwan), southeast Asia (Vietnam, Thailand) and most recently central (Nepal, India, Pakistan) and south central Asia (Sri Lanka) (Burke and Leake, 1988; Erlanger et al., 2009). This rapid and widespread expansion of JEV was associated closely with increases in human populations, in acreage of irrigated rice, and in pig farming (Erlanger et al., 2009; van den Hurk et al., 2009). In endemic areas of Japan, the avian-Culex maintenance cycle may be bypassed when vertically infected Cx. tritaeniorhynchus (Rosen et al., 1989) directly initiate the amplification cycle in pigs after terminating diapause (Hayashi et al., 1973). The invasion of India, Pakistan (Igarashi et al., 1994) and Nepal (Henderson et al., 1983), where swine farming is limited, may indicate an expanding role for birds in JEV amplification (Boyle et al., 1983; Jamgaonkar et al., 2003; Rodrigues et al., 1981; Soman and Mourya, 1985; Soman et al., 1986; Soman et al., 1977). Although typically associated with lowland rice farming in the outer Terai of Nepal, JEV outbreaks recently have occurred at high elevations in Kathmandu Valley, where the virus now is endemic (Partridge et al., 2007; Zimmerman et al., 1997). JEV lineages I and II also have moved progressively east into New Guinea, with recent incursions across the Torres Straight into northern Australia (Hanna et al., 1999; Mackenzie et al., 2002).
Future trends
Air transport of mosquitoes was the probable cause of JEV outbreaks on isolated Pacific Islands such as Guam (Hammon et al., 1958) and Saipan (Mitchell et al., 1993), demonstrating the potential of this virus to invade new areas such as the west coast of the USA. Here, susceptible mosquitoes and avian hosts could conceivably allow establishment before current surveillance and control programs would detect and eliminate this virus (Nett et al., 2009; van den Hurk et al., 2009). With the spread of JEV into much of the Indian subcontinent, other destinations served by frequent routes of commerce or passenger air travel, such as Africa and Europe, also could be at risk. Tracing the recent, rapid dispersal path of chikungunya virus serves to demonstrate the importance of routes of frequent travel for vector and arbovirus invasions (Powers and Logue, 2007; Simon et al., 2008).
C. Rift valley fever virus
Distribution and significance
Rift Valley fever virus (RVFV) is classified within the genus Phlebovirus in the family Bunyaviridae and causes intermittent epizootics and sporadic epidemics, primarily in east Africa (Bird et al., 2009; Daubney et al., 1931). Infection causes severe and often fatal illness in sheep and cattle, with occasional spill over to include other domestic animals and humans. Camels also frequently become infected, but seem to suffer less illness and lower abortion rates than other livestock. In 1% to 2% of affected humans, RVF progresses to severe disease, including hepatitis, encephalitis, retinitis, blindness, and/or a hemorrhagic fever; the case fatality rate is approximately 10% to 20% (Madani et al., 2003).
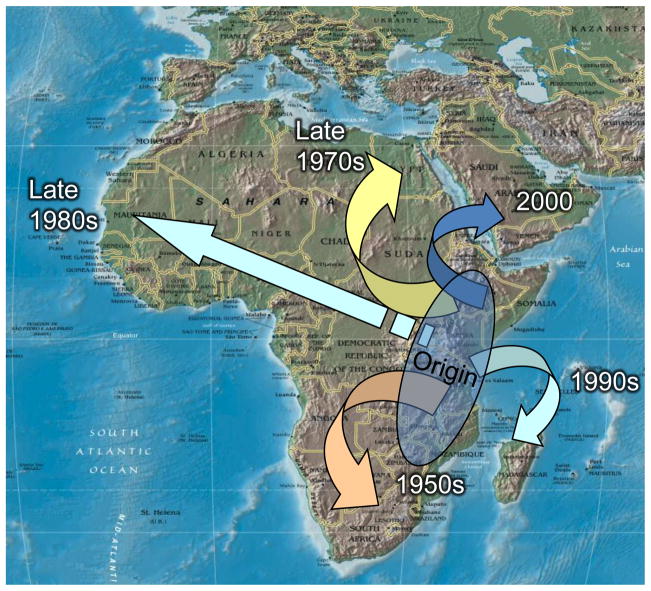
Historically, RVFV was restricted to sub-Saharan eastern Africa, especially Rift Valley of the Kenya and Tanzania (Meegan et al., 1989), where outbreaks are caused by multiple lineages of the virus (Bird et al., 2008). Subsequent outbreaks with human involvement have been documented in South Africa, the Nile Valley from Sudan to the Egyptian delta, and the Saudi Arabian peninsula (Fig. 3). The 1977–79 outbreak in Egypt was especially devastating, with more than 200,000 human infections and 600 deaths and losses in livestock >$100M at that time (Meegan et al., 1978). Ten years later another large outbreak occurred in West Africa centered in Mauritania (Faye et al., 2007; Nabeth et al., 2001). RVFV isolates from both outbreaks were distinct and monophyletic, perhaps indicating dispersal and amplification by a single strain (Bird et al., 2008).
Fig. 3.
Temporal patterns of dispersal by RVFV in Africa (Bird et al. 2003). Dates indicate the earliest detection and possible establishment of virus in each area.
Factors associated with emergence
RVFV is maintained in an enzootic cycle among wildlife, such as African buffaloes, and a wide variety of mosquito species (>30 species, 6 genera). Transmission is enzootic during most years, but epizootic during wet years, especially following droughts. Apparently, virus is maintained between rainy seasons and between high rainfall years by vertical transmission to desiccation resistant eggs of several floodwater Aedes species, especially Aedes macintoshi (Linthicum et al., 1985a). High water years inundate several previous seasons of eggs, giving rise to large numbers of mosquitoes and perhaps multiple viral lineages (Bird et al., 2008). Infection rates among Aedes adults reared from field-collected larvae typically are low (Linthicum et al., 1985a), therefore requiring extensive horizontal amplification for RVFV maintenance. The large variety of wildlife naturally infected with RVFV would seem to support this notion.
Warming in the Indian Ocean is linked closely to the El Niño-Southern Oscillation (ENSO) in the Pacific and is followed by high rainfall events in the Rift Valley that are predictive of RVFV outbreaks (Linthicum et al., 1999). Widespread flooding, apparent from satellite imagery by examining the normalized difference vegetation index data, triggers the simultaneous hatching of large numbers of Aedes eggs, rapidly producing a cohort of blood feeding adults, some of which are infectious with RVFV and able to transmit this infection to ruminants. Both wild and domestic ruminants are drawn or driven by herdsmen to these new sources of water and grass, bringing susceptible hosts into close proximity with infectious mammal-feeding Aedes mosquitoes (Linthicum et al., 1985b). These new mosquito habitats also are colonized by other effective mosquito vectors that take longer to mature and therefore emerge when the first groups of infected ruminants become viremic, further spreading the virus to new hosts. The concordance between the rainy season and the calving of wild and domestic ruminants assures that highly susceptible host populations are available to be fed upon by infectious mosquito vectors during warm humid weather conditions conducive for transmission.
Future trends
Large virgin soil outbreaks in Mauritania, Egypt and Saudi Arabia have demonstrated the ability of RVFV to escape traditional enzootic areas and invade naïve populations. Routes of dispersal have not been fully established, but the movement of viremic camels along trade routes has been suspected (Hoogstraal et al., 1979) as well as vectors carried on storm fronts (Sellers et al., 1982). Before the onset of serious clinical disease, humans develop viremias suitable to infect susceptible mosquitoes. Uncontrolled air travel therefore could introduce RVFV into other continents such as North America or Europe where susceptible wild and domestic hosts and suitable vector mosquitoes reside (Gargan et al., 1988; Turell et al., 2008).
Extensive studies by the USDA and NASA have shown that tracking ENSO in the Pacific Ocean provides an early warning of warming in the Indian Ocean, heavy rainfall in the Rift Valley and outbreaks of RVFV (Anyamba et al., 2009). Several vaccines for RVFV have been developed and appear effective (Bird et al., 2009), however, local agencies have been reticent to preemptively preclude outbreaks by vaccination campaigns. Failure to contain these outbreaks provides a source of virus to seed outbreaks into other areas of Africa and the Middle East as well as the rest of the world. Future containment of RVFV will require pre-emptive vaccination of livestock in Africa and carefully regulated travel restrictions on livestock, wild animals and perhaps humans from affected areas. With a high potential impact on wildlife, domestic animal and human health, failure to contain RVFV could seriously impact veterinary and human health in Asia, Europe and the New World and have economic consequences far exceeding those of the waning WNV outbreak.
D. Bluetongue virus (BTV)
Distribution and significance
BTVs are classified within the genus Orbivirus (family Reoviridae) and currently consist of at least 24 viruses clustered within 10 distinct lineages (Schwartz-Cornil et al., 2008). BTVs cause economically significant disease in ruminants and, because of this veterinary economic impact, was placed on list-A by the Office International des Epizooties (OIE), limiting trade of animal products from affected areas. BTVs are maintained within an enzootic cycle among biting midges in the genus Culicoides (family Ceratopogonidae) and various ruminant species, almost all of which are susceptible to infection. Historically, it was thought that the BTVs evolved and were contained within Africa until the 1940s, when the first Mediterranean outbreak occurred on Cyprus. However, subsequent studies have found BTVs widely distributed in the tropics but not frequently associated with illness and therefore mostly undetected. Clinical disease is most prevalent in domestic sheep, especially those of European ancestry (Purse et al., 2008). Typically, cattle rarely show clinical illness and are considered a reservoir host, whereas goats usually do not develop overt disease (Gibbs and Greiner, 1988); however, during the recent incursion of BTV-8 into western Europe, clinical illness in cattle was common and associated with a low case fatality rate (http://www.oie.int).
Wild ruminants in North America, including deer, pronghorns and desert bighorn sheep, develop severe disease, whereas African wildlife seem mostly unaffected. This disparity in disease susceptibility supports the notion that Africa is the center of origin for BTV and that its enzootic circulation there seemingly has selected for resistance to disease in African wildlife. The distribution of BTV has been divided into three epidemiological zones, based on the occurrence of clinical disease: 1) an enzootic zone in the tropics where infection is common but clinical disease is rare, 2) an epizootic zone at temperate latitudes where disease outbreaks occur frequently, and 3) an incursive zone where infection is infrequent because climate and/or vector species typically are not suitable for transmission (Gibbs and Greiner, 1988).
Factors associated with emergence
The veterinary epidemiology of BTVs in North America and Europe is complex and related strongly to virus and vector genetics and distributions, overwintering mechanisms, and perhaps climate change. Based on a survey of cattle at slaughter, at least 5 viruses (BTV-2, -10, -11, -13, -17) were found in the U.S. (Metcalf et al., 1981), with prevalence greatest in the southwest and least prevalence in the northeast, where the primary vector, Culicoides sonorensis, is replaced by the less competent vector, C. variipennis (Jones and Foster, 1978; Tabachnick et al., 1996). Other species such as C. insignis are suspected as vectors at southern latitudes. Differences in vector competence within the variipennis species complex have been related to a midgut barrier to infection (Tabachnick et al., 1996). Distribution of BTVs in the northern prairie states and Canada seems limited by the temperature requirements for virus replication in the vector (Mullens et al., 1995), with transmission limited to summer periods with temperatures >15°C. Recent warming trends in Canada have facilitated the population dynamics of C. sonorensis (Lysyk, 2007; Lysyk and Danyk, 2007) and may allow more frequent incursions and perhaps the eventual establishment of BTV. Little is known about variation in the temperature requirements of different BTVs.
Until 1996, Europe was considered BTV-free and international trade restrictions by the European Union created huge annual financial losses to enzootic parts of North America from the loss of trade of animals and animal products. Occasional incursions of BTVs into Spain, Portugal and Turkey have been related to prevailing winds originating in North Africa or the Middle East (Sellers, 1980; Sellers et al., 1979; Sellers et al., 1978). BTV apparently became established in Europe after climate warming enabled the major vector, C. imicola, to expand is distribution northward to include parts of southern Europe east into Turkey (Purse et al., 2005). Coincidentally, five strains became established in the Mediterranean during 1998–2005. These strains seem to have invaded following routes from Tunisia and North Africa (BTV-2, -4) and from Turkey from the Middle East (BTV-1, -4, -9, -16) (Purse et al., 2005). In August 2006, BTV-8 invaded central and northern Europe, areas north of the known distribution of C. imicola (Saegerman et al., 2008). This on-going outbreak apparently involves transmission by other Culicoides species, including C. dewulfi and members of the C. obsoletus and C. pulicaris complexes. However, incriminating field infection and vector competence data have been scarce (Carpenter et al., 2008; Carpenter et al., 2009). Climate in this area of Europe has experienced a strong warming trend (Purse et al., 2005) and undoubtedly this change has shortened the extrinsic incubation period of the virus within the Culicoides vector (Mullens et al., 1995), and the gonotrophic (blood feeding and reproductive) cycle of the vector, thereby increasing the frequency of vector-host contact and extending the duration of the transmission season.
For BTV to become established at temperate latitudes, it must be able to overwinter locally. Studies on Culicoides indicate that adults are not active during winter (Takken et al., 2008) and vertical transmission of BTV remains undocumented (White et al., 2005). In contrast, ruminants develop long lasting chronic infections, but recrudescence mechanisms are poorly understood. Possibly, the cellular immune response of the host to Culicoides blood feeding could trigger the release of BTV at the bite area and thereby allow co- or later feeding flies to ingest the virus and renew transmission in the spring (Purse et al., 2008). Although not as yet supported by field evidence, this mechanism is intriguing because it synchronizes fly blood feeding activity and viral recrudescence. Alternatively, virus may overwinter in transplacentally infected calf and lamb fetuses that are viremic at birth (Backx et al., 2009; Gibbs et al., 1979; Worwa et al., 2009).
Future trends
Introductions and subsequent dispersal of BTVs most likely will continue due to intercontinental animal and animal product commerce as well as from windborne flies (Hendrickx et al., 2008; Sellers, 1980). Climate warming most likely will expand the epizootic zone into northern temperate regions and move the zone of incursion further northward. The expanding distribution of various BTVs may eventually result in the removal of trade embargoes, because most areas of the earth will support some level of enzooticity. Three options remain for mitigating the BTV problem: molecular engineering/selective breeding of livestock to increase resistance to disease, vector control and vaccination. Molecular biology may hold the answer if current susceptible breeds of cattle and sheep can be genetically modified to impart resistance. Treating wastewater ponds or other known larval habitats of species such as C. sonorensis in the arid southwestern USA has promise; however, control of other Culicoides that develop in less obvious habitats such as moist pastures will be a much greater challenge, especially in Europe. Chemical dips have been used to control tick infestations and perhaps a similar approach with other compounds could be used to reduce or eliminate adult flies or prevent biting. Complex immune interactions against as many as 24 viruses makes vaccine development challenging, but perhaps vaccines can be developed against specific strains of BTV with a particularly high potential for invasion.
E. Venezuelan equine encephalitis virus (VEEV)
Distribution and significance
VEEV is an alphavirus (Togaviridae: Alphavirus) found only in the New World (Fig. 4). It is the type species within the VEE complex of alphaviruses that includes 7 different species and multiple subtypes and varieties (Weaver et al., 2004). Enzootic subtypes ID and IE occur from Bolivia to Mexico, and the closely related Everglades virus (VEE complex subtype II) occurs only in Florida (Fig. 4). Permanent or semipermanent zoonotic cycles include rodents as reservoir hosts and mosquito vectors in the subgenus Culex (Melanoconion). These enzootic cycles occur in humid tropical forest or swamp habitats and typically go undetected. Direct spillover to humans has been documented in several locations where active case surveillance combined with laboratory diagnostics has uncovered extensive human disease, including fatal cases (Aguilar et al., 2004; Johnson et al., 1968; Quiroz et al.; Watts et al., 1998; Watts et al., 1997). Typically VEE cases overlap considerably in signs and symptoms with many acute, tropical febrile infectious diseases such as dengue fever (DEN), so cases undoubtedly are grossly underreported in locations where clinician awareness and laboratory diagnostics are lacking.
Fig. 4.
Geographic distribution of epidemic/epizootic VEEV strains responsible for major outbreaks, and enzootic VEE complex strains isolated principally in swamp or forest habitats.
Major epidemics occur periodically and somewhat sporadically when VEEV strains emerge with the potential for amplification in equids. These strains within subtypes IAB and IC utilize mosquito vectors such as Aedes and Psorophora spp., which are abundant in agricultural settings and competent to transmit VEEV among susceptible horses, donkeys and mules. Because these amplification hosts generate high titered viremias, extensive VEEV circulation in agricultural settings frequently results in spillover transmission to humans. As with the enzootic VEEV strains, epidemic strains cause a highly incapacitating DEN-like febrile illness that occasionally leads to fatal encephalitis, mainly in children.
Factors associated with emergence
The emergence of epidemic VEE relies on a combination of ecologic and viral genetic factors that must intersect in time and space. The enzootic VEEV strains that circulate continuously generally are not capable of equine amplification because they do not produce sufficient viremia. However, certain amino acid replacements in the E2 envelope glycoprotein that forms the tips of spikes on the VEEV surface mediate enhanced equine amplification (Brault et al., 2002a). Because these replacements can result from a single mutation in the viral genome (Anishchenko et al., 2006), and because alphaviruses, like other RNA viruses, replicate with low genetic fidelity (Weaver et al., 1993), amplification-competent mutations probably occur regularly within sylvatic cycles where enzootic strains are found. Selection of these mutations undoubtedly takes place within equids, though it is also possible that some sort of intermediate host is also involved in the selection of epidemic strains.
Genetic studies have shown that most but not all of the epidemic VEEV strains in subtypes IAB and IC also are more infectious for the epidemic mosquito vector, Aedes (Ochlerotatus) taeniorhynchus, that typically transmits among equids and humans in coastal areas (Brault et al., 2002b). The exception is a IC genotype that failed to spread into coastal areas of Venezuela in 1993, and thus produced only a minor epidemic (Rico-Hesse et al., 1995). Strains isolated from this outbreak inefficiently infected Ae. taeniorhynchus, indicating that the inability of this genotype to adapt to this critical vector limited its spread (Ortiz and Weaver, 2004). Even stronger evidence of the importance of VEEV adaptation to epidemic vectors comes from studies of recent Mexican epizootics. Unlike their closely related enzootic relatives, which presumably represent their ancestors, VEEV strains from the recent outbreaks efficiently infect Ae. taeniorhynchus. The relatively recent adaptation of these Mexican strains to this important vector, coincident with the first epizootic emergence in the region, has been linked to a single amino acid substitution in the E2 protein that increases infection of the mosquito midgut, again underscoring the dramatic effects of small genetic changes on arbovirus phenotypes (Brault et al., 2004).
Phylogenetic studies indicate that only one of 6 different subtype ID VEEV lineages, and none of the IE lineages, have produced the epidemic subtype IAB and IC strains (Powers et al., 1997). This epidemic-progenitor lineage occurs in western Venezuela, Colombia, and the Amazon areas of Ecuador and Peru. The failure of the remaining ID lineages to generate epidemic strains, despite their occurrence in locations where major epidemics have spread, suggests that genetic constraints of the enzootic strains limit the generation of equine-amplification-competent mutants.
In addition to critical mutations, epidemic VEEV emergence also depends on the transport of nascent equine-amplification-competent mutants to locations with susceptible equids and mosquito vectors. Many equids that are pastured near forests where enzootic VEEV circulates become infected and survive with generally benign subtype ID and IE infections, generating a “halo” of immunity around enzootic foci. In addition, several Culex in the subgenus Melanoconion are enzootic vectors and generally not capable of epidemic transmission because they do not disperse far from their forest habitats (Mendez et al., 2001). Therefore, nascent epidemic strains probably must be transported to locations distant from enzootic transmission foci where susceptible equids occur along with epidemic vectors in large numbers. The latter are generally floodwater or saltmarsh Aedes or Psorophora species that undergo population explosions during unusually rainy seasons (Weaver et al., 2004). Another enigma concerning VEEV emergence is why the equine-virulent IAB and IC strains are not maintained following outbreaks, i.e. emergence appears to be unidirectional. The most likely explanation is that the mutations that adapt enzootic strains reduce the fitness of epidemic strains for enzootic hosts or vectors. Experimental infections of rodent reservoir hosts support this hypothesis (SCW, unpublished).
Future Trends
The last major VEE epidemic, which involved ca. 100,000 persons with an estimated 300 deaths, occurred in Venezuela and Colombia in 1995 (Rivas et al., 1997; Weaver et al., 1996). This outbreak may have been initiated by the accidental release from a laboratory of an isolate from the 1962–66 epidemic (Brault et al., 2001). Current understanding of the mechanisms of epidemic VEEV emergence indicate that natural emergence will occur periodically, so long as equine herd immunity is not maintained at adequate levels in Venezuela and Colombia by vaccination or natural acquisition of immunity from enzootic exposure. Epidemics probably have not arisen in the Amazon Basin of Peru and Ecuador, where the progenitor lineage of subtype ID occurs, because equid populations tend to be low in these regions. The risk of epidemic emergence may be increasing by the conversion of large areas of tropical forest to ranching and other forms of agriculture in Colombia and Venezuela. This deforestation increases the ecotonal boundaries around enzootic habitats and may thereby enhance opportunities for infection of bridge vectors or highly mobile hosts such as birds or bats capable of transporting nascent epidemic strains to locations conducive to the generation of an equine amplified cycle.
In addition to the risk of future equine-mediated VEE epidemics, the possibility of human-amplified transmission must be considered (Table). Infected people develop high titered viremia after infection with both enzootic (Aguilar et al., 2004; Quiroz et al.) and epidemic (Bowen and Calisher, 1976; Weaver et al., 1996) VEEV strains. Furthermore, urban, peridomestic mosquito vectors such as Ae. aegypti (Ortiz et al., 2008; Suarez and Bergold, 1968) and Ae. albopictus (Beaman and Turell, 1991; Fernandez et al., 2003; Turell and Beaman, 1992) are capable of transmission after oral doses comparable to human viremia titers. Therefore, the key prerequisites for urban, human-amplified VEEV transmission would appear to be met, because: 1) human viremia is sufficient to infect peridomestic vectors; and 2) these peridomestic mosquitoes have the ability to transmit VEEV. The past epidemic VEEV transmission near major cities such as Maracaibo, Venezuela (Weaver et al., 1996), where Ae. aegypti readily supports DENV transmission, raise the question of why these outbreaks have not sparked urban transmission. Furthermore, enzootic VEEV regularly infects people in neotropical cities like Iquitos, Peru, that are in close proximity to forest habitats and that support epidemic DENV transmission (Rocha et al., 2009). It may just be a matter of time before an Ae. aegypti-borne epidemic VEEV cycle emerges, which would have devastating public health consequences.
Table.
Characteristics of arboviruses with the risk of urbanization
| Virus | History of temporary urbanization* | History of permanent urbanization* | Human viremia suitable for vector transmission** | Experimental competence of urban vectors** | Mutations associated with urban emergence | References |
|---|---|---|---|---|---|---|
| DENV | Yes | yes | yes | yes | No (except Asian strains of DENV-2; see Fig. 5) | (Vasilakis and Weaver, 2008) |
| CHIKV | Yes | Yes | yes | yes | E1 envelope glycoprotein mutation enhances Ae. albopictus infection | (Schuffenecker et al., 2006; Tsetsarkin et al., 2007; Vazeille et al., 2007) |
| YFV | Yes | no | yes | yes | No | (Monath, 2001) |
| ZIKV | yes | no | yes (presumed based on Yap outbreak) | no (but isolation from Ae. aegypti) | No | (Duffy et al., 2009; Marchette et al., 1969) |
| VEEV | No | no | yes | yes | No (although E2 envelope glycoprotein mutations enhance infection of epidemic vectors and equine amplification hosts) | (Anishchenko et al., 2006; Brault et al., 2002a; Brault et al., 2004; Weaver et al., 2004) |
| MAYV | No | no | unknown | yes | No | (Tesh et al., 1999)(Aguilar and Weaver, unpublished) |
urban transmission exceeding 5 years is considered permanent
Aedes aegypti and/or Ae. albopictus
IV. Examples of Arboviral Emergence Associated with Urbanization
A. Dengue viruses (DENV)
Distribution and Health Significance
Dengue viruses comprise four related serotypes that share common transmission cycles (Fig. 5). They are flaviviruses (Flaviviridae: Flavivirus) closely related to JEV and WNV described above; however, unlike all other flaviviruses, DENVs that cause most human disease are not zoonoses, but exclusively utilize humans as reservoir and amplification hosts. Also unlike most arboviruses, they rely on transmission by mosquito vectors that live in close association with people; Ae. (Stegomyia) aegypti is the principal vector in most locations, with Ae. (Stegomyia) albopictus serving as a secondary vector in some locations (Table).
Fig. 5.
Phylogenetic tree of DENV strains derived from complete open reading frames available in the GenBank library. The phylogeny was inferred using Bayesian analysis (one million reiterations) and all horizontal branches are scaled according to the number of substitutions per site. Bayesian probability values are shown for key nodes. Virus strains and branches are colored green for sylvatic (nonhuman primate and arboreal mosquito isolates) and red for endemic (human and peridomestic Aedes isolates) and strains coded by abbreviated country of collection/strain name/year of collection. Dashed green line indicates hypothetical sylvatic DENV-3 lineage suggested by nonhuman primate seroconversions in Malaysia (Rudnick, 1978).
DENV are the most important human arboviral pathogens, with an estimated 50–100 million annual cases of DEN and tens-of-thousands of cases of the more severe and sometimes fatal dengue hemorrhagic fever/shock syndrome (DHF/DSS syndromes) (Endy et al., 2010). The latter disease manifestations were first described after World War II coincident with increased urbanization, particularly in Asia. Today, DEN is hyperendemic in many Asian tropical regions, where 2 or more serotypes circulate endemically and epidemically. Although DENV was probably introduced periodically into the Americas by sailing ships since the 17th century, the emergence of hyperendemic DEN in the Western Hemisphere began later, due to a partially successful campaign to eradicate Ae. aegypti to control yellow fever. This campaign succeeded in most of the Americas from the 1950s to the 1970s, but was then discontinued. Ae. aegypti quickly recolonized nearly all of the Neotropics and subtropics, and the invasion of DENV followed soon thereafter. In 1985, Ae. albopictus was introduced into the U.S. (Hawley et al., 1987) and Brazil from Asia, providing a secondary vector for DENV transmission in the Americas. This species was the primary vector of DENV during a recent outbreak in Hawaii (Effler et al., 2005).
Factors associated with emergence
Although most DENV strains have no vertebrate hosts other than humans, ancestral DENV are represented by primitive nonhuman primate-borne strains that continue to circulate in the forests of West Africa and Southeast Asia (Gubler, 1997; Wang et al., 2000). These DENV use nonhuman primates as reservoir/amplification hosts and canopy mosquitoes as enzootic vectors. Emergence into the evolutionarily and ecologically independent urban cycles occurred independently for each serotype from hundreds to a few thousand years ago (Fig. 5). Experimental studies of vector competence and human models suggest that the emergence of DENV-2 required little or no adaptation to Ae. aegypti or humans (Vasilakis et al., 2007), and epidemiologic and genetic analyses of human isolates indicate that sylvatic DENV-2 can cause typical DEN fever (Vasilakis et al., 2008) and some hemorrhagic manifestations (Cardosa et al., 2009). However, there is evidence that one particular genotype of DENV-2, termed “Asian,” has evolved higher human virulence, in the context of immune enhancement, with limited antigenic cross-reactivity against previous DENV infections (Cologna et al., 2005; Kochel et al., 2002; Vasilakis et al., 2007) and greater infectivity for Ae. aegypti (Armstrong and Rico-Hesse, 2003)(Fig. 5), allowing it to displace the less fit “American” genotype from some parts of the Americas.
Although at least some of the DENVs emerged from sylvatic cycles to infect humans on the order of hundreds of years ago (Fig. 5), highly efficient interhuman transmission probably required the widespread colonization of the tropics by Ae. aegypti. This vector has its origins in West Africa (Mattingly, 1967; Sylla et al., 2009; Tabachnick and Powell, 1979), where its ancestors remain in forested habitats that contain treeholes for larval development. The ancestral form, Ae. aegypti formosus, is not a significant DENV vector, because it is zoophilic and nearly refractory to DENV-2 infection (Bosio et al., 1998; Diallo et al., 2005). Ae. aegypti aegypti probably evolved its domestic behavior in Africa, and was subsequently transported on sailing ships to the Americas (along with YFV) and Asia, setting the stage for highly efficient DENV transmission.
Interhuman DENV transmission is highly efficient due to the relatively high viremia titers found in many infected persons, and the susceptibility, but more importantly, the behavior and ecology of Ae. aegypti. This mosquito prefers artificial water containers as its larval habitat, human habitations as a resting and host-seeking habitat as adults, and human blood as both a protein source for oogenesis (egg development) and energy for flight. In addition, adult females often feed on multiple human hosts during a single gonotrophic cycle (Harrington et al., 2001), increasing both the probability of becoming infected and the number of hosts infected by bite. The tropical urbanization that has accelerated since World War II, combined with the multiple interhemispheric introductions of both Ae. aegypti and Ae. albopictus, has greatly increased the population densities and geographic ranges of these vectors. Ae. aegypti is especially aided by poverty when the lack of municipal water services results in intradomiciliary water storage and the lack of trash collection results in the accumulation of waste receptacles that hold rainwater to support larval development. Community-based vector control through the elimination of these larval development sites or by the use of larvicides has only been effective in Cuba and Singapore, and the lack of sustained success resulted in the reappearance of Ae. aegypti and DEN.
The DHF/DSS syndromes are strongly associated with secondary infections, indicating that the ability of multiple serotypes to circulate sympatrically within Asian urban populations probably explains the relatively recent emergence of these disease syndromes there. The widespread occurrence of the DHF/DSS syndromes was delayed in the Americas, because DENV did not become hyperendemic until the 1980s and later. In addition to urbanization that enhanced conditions for Ae. aegypti and for efficient interhuman transmission, the lack of sustained mosquito control programs, the increase in use of disposable containers and tires, and the increase in human air travel and perhaps commerce have undoubtedly facilitated the spread of DENV strains and enhanced hyperendemicity.
Future Trends
DENV is now hyperendemic in many parts of the tropics and subtropics, and there is no immediate cause for optimism that DEN can be controlled in these locations. Advances in clinical care have decreased case fatality rates for DHF/DSS, but there remains no effective antiviral therapy and no licensed vaccines. The latter are the subject of intensive research and development, with some hope for a commercial vaccine becoming available during the coming decade. However, the association of DHF/DSS with secondary infections, possibly the result of immune enhancement (Halstead and O’Rourke, 1977a; Halstead and O’Rourke, 1977b), indicates that solid and long-lived tetravalent immunity against all 4 DENV serotypes will be required to ensure the safety of a vaccine. If this challenge can be overcome, DENV could in theory be eradicated from urban cycles because humans are the only vertebrate hosts. Reemergence from the sylvatic cycles will remain a risk, but sustained vaccination could prevent this scenario because neutralizing antibodies strongly cross-react between urban strains used for vaccines and sylvatic strains.
The effects of global warming on DENV transmission are not as predictable as those of some other arboviruses. Because warming is expected to be most dramatic in temperate climates, the distributions of the 2 principal DENV vectors could expand. Ae. aegypti cannot tolerate cold winters and currently is limited to subtropical and tropical regions. Its northern and southern expansion could certainly be followed by extended DENV transmission into locations where human behavior and culture permits adequate exposure to this mosquito (e.g. water storage and the presence of artificial containers for larval development, and the lack of barriers to the movement of adult females into homes, such as window screening and air conditioning). However, in some subtropical regions, cultural practices limit exposure to this vector. One example is the southern U.S. where Ae. Aegypti-borne DEN and YF epidemics occurred beginning in the 18th century, but disappeared about a century ago, coincident with improved hygiene and the widespread use of window screening, and later, air-conditioning. In these locations, climate warming might have little or no effect on DENV. Although a less efficient vector, some strains of Ae. albopictus have a diapausing egg state and therefore greater tolerance for temperate winters (Hanson and Craig, 1995; Nawrocki and Hawley, 1987). This species is less endophilic, so human exposure may be less dependent on home construction and probably occurs principally within the peridomestic environment.
B. Chikungunya virus (CHIKV)
Distribution and Health Significance
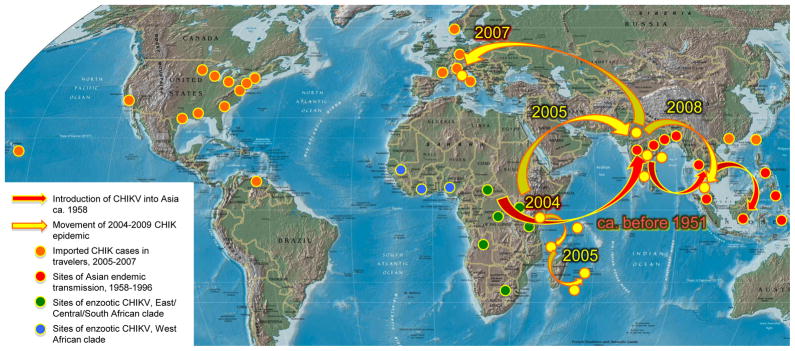
CHIKV is an alphavirus (Togaviridae: Alphavirus) historically found only in the Old World. First isolated in Tanzania in 1953 during an outbreak of human febrile illness accompanied by severe arthralgia and rash, it is now known to circulate in enzootic cycles throughout much of Africa (Fig. 6) (Jupp and McIntosh, 1988). Occasionally, outbreaks of human disease are detected in Africa when adequate laboratory diagnostics are implemented, but cases frequently are confused clinically with DENV. Historical records also indicate that CHIKV, like DENV, was probably transported on sailing ships to Asia and possibly the Americas for centuries, along with Ae. aegypti, where it caused epidemics in port cities but failed to become established.
Fig. 6.
Map showing the locations of the 2 major enzootic genotypes of CHIKV in Africa, and historical introductions into the Indian Ocean islands, Asia and Europe, as well as recent importations via viremic travelers, based on (Lanciotti et al., 2007; Powers et al., 2000; Rezza et al., 2007; Sang et al., 2008).
CHIKV historically has been regarded as a highly debilitating but not a life-threatening pathogen. Patients typically suffer from fever, headache, nausea, vomiting, myalgia, rash, and severe arthralgia. Because these symptoms often mimic those of DEN and because CHIKV circulates in DEN-endemic regions, CHIK has long been underdiagnosed and underappreciated as an important arboviral disease (Carey, 1971). The severe arthralgia that accompanies most CHIKV infections is highly debilitating and typically lasts for several weeks, and sometimes for months or even years, resulting in a high economic cost in addition to human suffering. Disability-adjusted life year (DALY) estimates during the 2006 Indian epidemic exceeded 265 per million in some states, which accounted for up to 69% of the total DALYs there (Krishnamoorthy et al., 2009).
Beginning in the 1950 s, CHIKV was recognized as the etiologic cause of febrile disease epidemics in India and Southeast Asia (Fig. 6). Transmission continued in India until 1973, when the virus apparently disappeared. In Southeast Asia, CHIKV has remained endemic and continues to be an important pathogen hidden, at least to some degree, under the “DEN umbrella.” Unlike Africa, where there is evidence of a sylvatic CHIKV cycle involving arboreal mosquitoes and nonhuman primates, CHIKV appears to be maintained in Asia in a strictly human-peridomestic mosquito cycle.
CHIKV cases have risen meteorically during the last 4 years and CHIKV is now recognized as a dangerous and important, emerging arbovirus due to 2 major epidemics. The first apparently began on the coast of Kenya in 2004 and then spread to the nearby Island of Comoros in 2005 (Fig. 6). Rapid dissemination to other islands in the Indian Ocean then ensued, most notably La Reunion where ca. 300,000 persons were infected, with an attack rate of about 35%. Later in 2006, a closely related CHIKV strain was introduced from the East Africa region into India, where a major epidemic continues. Most estimates from the Indian subcontinent are on the order of 1–2 million cases. Especially troubling in both the Indian Ocean (Robin et al., 2008) and Indian (Mavalankar et al., 2008) epidemics has been the association of CHIKV infection with an excess of human deaths recorded, suggesting that the virus may have become more virulent for humans. Some of these fatal cases having neurological complications do not appear to have been associated with secondary infections or underlying medical problems. Many infected and potentially infective travelers have been detected in Europe, the Americas and Asia, raising concerns about further invasion. This fear was realized in northern Italy, where a traveler from India introduced CHIKV in the summer of 2007, resulting in local transmission via Ae. albopictus giving rise to several hundred infections (Rezza et al., 2007)(Fig. 6). Although CHIKV has not been detected in Italy since 2007, its transmission there suggests that global warming could further extend its potential for transmission into northern latitudes where Ae. albopictus has become established.
Factors associated with emergence
Phylogenetic studies indicate that CHIKV evolved in Africa, where it diverged about 350 years ago into 2 principal lineages: West African, and East/South/Central African. The latter lineage was apparently introduced into Asia ca. 1950 or earlier, where epidemic transmission continued in India until 1973, and endemic/epidemic transmission continues in Southeast Asia (Powers et al., 2000). However, the virus gained little attention due to the health importance of DENV and the lack of differential diagnostics for the 2 viruses in many locations. Although it is clear that DENV caused more human disease since the 1950s, the true disease burden due to CHIKV undoubtedly was underestimated.
CHIKV shares many characteristics with DENV, including some of the factors associated with its emergence such as: 1) the ability to use humans (apparently at least in Asia), as the sole reservoir/amplification hosts; 2) the use of the highly peridomestic and anthropophilic Ae. aegypti, and to a lesser extent, Ae. albopictus, as principal vectors during endemic and epidemic transmission; 3) the use of infected persons for dispersal to new regions suitable for endemic and epidemic transmission, and; 4) genetic changes that enhanced its ability to infect mosquito vectors (Table). The latter involves an amino acid replacement in the E1 envelope glycoprotein that evolved convergently, apparently in response to selection for efficient transmission by Ae. albopictus in locations where Ae. aegypti is absent or less abundant (Tsetsarkin et al., 2007; Vazeille et al., 2007).
Future Trends
Although the epidemics in the Indian Ocean have apparently subsided, epidemic CHIK continues in the Indian subcontinent and endemic transmission continues in Southeast Asia. Historical information suggests that CHIKV will remain endemic in the latter region, but the disappearance of the virus from India in 1973 indicates the possibility that this region cannot sustain transmission for unknown reasons. However, if human and vector populations have increased sufficiently in India, conditions for endemic maintenance may have improved. The ability of Indian strains to use both Ae. aegypti and Ae. albopictus as vectors and nonhuman primates as hosts also may enhance its ability to persist there.
Another major concern regarding CHIKV is the potential for its establishment in Europe or the Americas. The large numbers of travelers who returned infected to these regions during the 2005–2007 epidemics underscore the risks of introduction by frequent air travel by persons leaving epidemic areas (Lanciotti et al., 2007), while the history of autochthonous infections in northern Italy demonstrates the ability of CHIKV to be transmitted from person-to-person, even in temperate regions (Rezza et al., 2007). However, the greatest risk is the establishment of CHIKV in the Neotropics, where the success of DENV indicates that CHIKV could become endemic and cause millions of cases annually.
V. Examples of Other Arboviruses with the Potential for Urban Emergence
There are many known and probably even more unknown arboviruses with the potential for epidemic emergence, especially as climate change and urbanization enhance opportunities for spread and interhuman transmission. We include here a few of many examples of each emergence.
A. Yellow fever virus (YFV)
YFV is a flavivirus (Flaviviridae: Flavivirus) distantly related to WNV and DENV. Strong historical evidence as well as phylogenetic studies indicate that YFV originated in Africa and spread to the New World during the slave trade beginning in the 16th century (Bryant et al., 2007; Monath, 1988; Monath, 2001). Until the early 20th century, many YF epidemics occurred in port cities of North and South America, associated with the importation of both the Ae. aegypti vector and YFV on sailing ships, where onboard transmission cycles occurred among humans. In addition, YFV established permanent enzootic sylvatic transmission cycles in the Neotropics, utilizing nonhuman primates and canopy-dwelling mosquitoes such as Hemagogus janthinomys. These cycles persist today and represent a constant threat of spillover to humans following epizootic or even enzootic transmission (Bryant et al., 2003; Monath, 2001).
Despite YFV being studied extensively since the early 20th century, several enigmas remain regarding the potential for future emergence and urbanization (Table). African strains clearly retain the ability to enter urban cycles and initiate epidemics involving human-mosquito transmission, resulting in tens-of-thousands of human cases annually despite a highly effective human vaccine (17D) developed in 1937 (Monath, 1988). On the other hand, the reasons that the African YFV strains have not invaded Asia, as has CHIKV, remain unknown. Also, major urban YF epidemics have disappeared from the New World since the major campaign to eliminate Ae. aegypti began in the mid 20th century. Although Ae. aegypti has reinfested nearly all of the Neotropics, resulting in hyperendemic DENV, YFV remains largely a zoonotic disease in South America. A possible exception is the recent YF epidemic in Paraguay, apparently involving urban, human-to-human transmission, which was controlled by mass vaccination (2008). This outbreak suggests the continued potential for enzootic YFV strains to initiate urban outbreaks in the Neotropics, and underscores the need to maintain vaccination programs in enzootic regions of South America. Possible explanations for the limited recent urban YF activity include a limited urbanization potential of the extant enzootic, neotropical YFV strains (lower human viremia and/or reduced Ae. aegypti infectivity) compared to African strains, cross-protection provided by DENV, which are hyperendemic in much of Asia, and more limited movement of African strains to Asia after the decline of transportation via sailing ships. Although experimental evidence to test these hypotheses is quite limited, the transmission competence of Ae. aegypti from Bolivia for American YFV strains fails to support a lesser urbanization potential of extant American enzootic strains (Mutebi et al., 2004).
Expansion of epidemic YFV into Asia and the Americas would expose the virus to additional, major tropical urban centers and could increase the chances for the establishment of a permanent endemic transmission cycle. Understanding the reason(s) why this has not occurred is of major public health importance and should be a research priority.
B. Zika virus (ZIKAV)
ZIKAV, also a flavivirus (Flaviviridae: Flavivirus) closely related to YFV, was first isolated from a sentinel monkey in the Zika forest of Uganda in 1947; a year later virus was isolated from Ae. africanus at the same location (Dick et al., 1952). Since that time, ZIKAV has been sporadically isolated, occasionally associated with human disease, and serologic evidence of circulation has been found in Africa (Uganda, Nigeria, Senegal, Egypt) and Asia (India, Malaysia, Thailand, Viet Nam, the Philippines and Indonesia)[reviewed in (Lanciotti et al., 2008)]. However, until recently, ZIKAV has never been associated with large outbreaks of disease. Human seroprevalence can be quite high; for example, 75% of 358 Malaysian residents had neutralizing antibodies in 1954, with an age and seroprevalence correlation suggesting endemicity (Pond, 1963). A Nigerian community exhibited 56% seroprevalence in 1980 (Adekolu-John and Fagbami, 1983).
In Africa, ZIKAV has been isolated from Ae. africanus (Dick et al., 1952; Haddow et al., 1964) and Ae. luteocephalus, (Lee, 1969) and in Malaysia from Ae. aegypti (Marchette et al., 1969); the same vectors involved in enzootic and epidemic YFV and CHIKV transmission, respectively. Like many other sympatric arboviruses, ZIKAV produces a flu-like illness associated with high fever, malaise, dizziness, anorexia, retro-orbital pain, edema, lymphadenopathy, and gastrointestinal manifestations (Olson et al., 1981). A rash is also sometimes reported (Simpson, 1964). Thus, diagnosis requires serology or virus isolation, and most cases probably are assumed to be DEN or malaria.
In 2007, an epidemic including 49 confirmed and 59 probable cases of Zika virus infection was detected on the Pacific Island of Yap (Duffy et al., 2009). Rash, fever, arthralgia, and conjunctivitis were common signs and symptoms, with an estimated 73% attack rate among residents ≥3 years of age, or ca. 5,005 of the 6,892 residents in this age group. Aedes hensilli was the most commonly collected mosquito species, although ZIKAV was not isolated from this species and confirmation its vector status was not achieved. ZIKAV was likely imported into Yap via a viremic traveler, a hypothesis that was supported by the return of an infected health care worker to the U.S. in July, 2007, most probably in a viremic state (Duffy et al., 2009).
C. Mayaro virus (MAYV)
MAYV (Togaviridae: Alphavirus) is related closely to CHIKV and produces a nearly indistinguishable, highly debilitating clinical illness characterized by rash and arthralgia. MAYV was first isolated from febrile forest workers in Trinidad in 1954 and causes sporadic outbreaks in many regions of South America. However, because MAYV produces a DEN-like illness that includes fever, chills, headache, eye pain, generalized myalgia, arthralgia, and gastrointestinal manifestations, many cases are undoubtedly assumed to be DEN in the absence of laboratory diagnosis. However, severe MAYV-induced arthralgia can persist for months, so it is often more incapacitating than DEN (Coimbra et al., 2007; Tesh et al., 1999).
MAYV circulates strictly in South America in a cycle believed to involve nonhuman primates as reservoir/amplification hosts and sylvatic mosquitoes such as H. janthinomys as vectors. Human infections are strongly associated with exposure to forest environments, so they are assumed to represent spillover from the enzootic cycle. However, several factors suggest the possibility of MAYV urbanization, including: 1) the close relationship to CHIKV, another alphavirus in the Semliki Forest Complex with a long and well-established history of urbanization (see above); 2) the regular occurrence of MAY cases near major neotropical cities infested with Ae. aegypti (Tesh et al., 1999), and; 3) the competence of Ae. aegypti to become infected and transmit MAYV to hamsters after ingestion of moderate oral doses (P. V. Aguilar, SCW, University of Texas Medical Branch, unpublished). The critical missing information needed to assess the potential of MAYV to urbanize is the magnitude and duration of human viremia in relation to Ae. aegypti susceptibility (Table). If MAYV does succeed in urbanization, the experience with DENV in the western hemisphere suggests major public health consequences. Although MAYV has not been associated with fatal human disease like DENV, primary infections are often more debilitating, with loss of productivity for weeks or even months due to severe arthralgia. The recent epidemic activity of CHIKV should serve as a warning that seemingly obscure viruses like MAYV should not be underestimated as potentially emerging human pathogens.
VI. Conclusions
Arboviruses have a well-documented history of emergence through several mechanisms, including geographic expansion, often mediated through human transportation, and enhanced amplification in peridomestic commensal and domesticated animals leading to spillover to humans. Both of these mechanisms threaten to increase in the future due to increased human travel and global commerce as well as deforestation and tropical human population growth. Global warming also has the potential to increase the distribution of vectors and to enhance transmission potential in temperate climates by elongating transmission seasons, increasing host-vector contact by shortening vector gonotrophic cycles, and shortening extrinsic incubation times. However, the greatest risk of human disease comes from the ability of some arboviruses to adopt anthroponotic urban or peridomestic transmission cycles involving highly efficient and anthropophilic vectors, Ae. aegypti and Ae. albopictus, or enzootic peridomestic cycles involving urban avian and Culex populations. Combined with the explosions in urban human populations in the tropics, diseases such as DEN and CHIK will continue to increase in incidence until effective vaccines are available or improved control of urban vectors is achieved. Furthermore, there is reason to believe that additional viruses such as VEEV, ZIKAV and MAYV have the potential for urbanization (Table), which could have devastating public health consequences, especially in the Western Hemisphere, where there is no herd immunity. The movement of rural Aedes and Culex vectors and their hosts into urban and peridomestic environments allow effective amplification within simplified transmission cycles in close proximity to humans. Further research is needed to understand the reasons that these urban emergences have not yet occurred and to devise intervention strategies to facilitate their control and prevent future urbanization.
Acknowledgments
The authors research is supported by NIH grants AI069145 and AI071192 (SCW) and AI055607 (WKR).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Outbreak news. Yellow fever, Paraguay. Wkly Epidemiol Rec. 2008;83:105. [PubMed] [Google Scholar]
- Adekolu-John EO, Fagbami AH. Arthropod-borne virus antibodies in sera of residents of Kainji Lake Basin, Nigeria 1980. Trans R Soc Trop Med Hyg. 1983;77:149–51. doi: 10.1016/0035-9203(83)90053-6. [DOI] [PubMed] [Google Scholar]
- Aguilar PV, Greene IP, Coffey LL, Medina G, Moncayo AC, Anishchenko M, Ludwig GV, Turell MJ, O’Guinn ML, Lee J, Tesh RB, Watts DM, Russell KL, Hice C, Yanoviak S, Morrison AC, Klein TA, Dohm DJ, Guzman H, Travassos da Rosa AP, Guevara C, Kochel T, Olson J, Cabezas C, Weaver SC. Endemic Venezuelan equine encephalitis in northern Peru. Emerg Infect Dis. 2004;10:880–8. doi: 10.3201/eid1005.030634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JF, Andreadis TG, Main AJ, Ferrandino FJ, Vossbrinck CR. West Nile virus from female and male mosquitoes (Diptera: Culicidae) in subterranean, ground, and canopy habitats in Connecticut. J Med Entomol. 2006;43:1010–9. doi: 10.1603/0022-2585(2006)43[1010:wnvffa]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Anderson JF, Main AJ, Delroux K, Fikrig E. Extrinsic incubation periods for horizontal and vertical transmission of West Nile virus by Culex pipiens pipiens (Diptera: Culicidae) J Med Entomol. 2008;45:445–51. doi: 10.1603/0022-2585(2008)45[445:eipfha]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Anishchenko M, Bowen RA, Paessler S, Austgen L, Greene IP, Weaver SC. Venezuelan encephalitis emergence mediated by a phylogenetically predicted viral mutation. Proc Natl Acad Sci U S A. 2006;103:4994–9. doi: 10.1073/pnas.0509961103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anyamba A, Chretien JP, Small J, Tucker CJ, Formenty PB, Richardson JH, Britch SC, Schnabel DC, Erickson RL, Linthicum KJ. Prediction of a Rift Valley fever outbreak. Proc Natl Acad Sci U S A. 2009;106:955–9. doi: 10.1073/pnas.0806490106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong PM, Rico-Hesse R. Efficiency of dengue serotype 2 virus strains to infect and disseminate in Aedes aegypti. Am J Trop Med Hyg. 2003;68:539–44. doi: 10.4269/ajtmh.2003.68.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backx A, Heutink R, van Rooij E, van Rijn P. Transplacental and oral transmission of wild-type bluetongue virus serotype 8 in cattle after experimental infection. Vet Microbiol. 2009 doi: 10.1016/j.vetmic.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Beaman JR, Turell MJ. Transmission of Venezuelan equine encephalomyelitis virus by strains of Aedes albopictus (Diptera: Culicidae) collected in North and South America. J Med Entomol. 1991;28:161–4. doi: 10.1093/jmedent/28.1.161. [DOI] [PubMed] [Google Scholar]
- Bird BH, Githinji JW, Macharia JM, Kasiiti JL, Muriithi RM, Gacheru SG, Musaa JO, Towner JS, Reeder SA, Oliver JB, Stevens TL, Erickson BR, Morgan LT, Khristova ML, Hartman AL, Comer JA, Rollin PE, Ksiazek TG, Nichol ST. Multiple virus lineages sharing recent common ancestry were associated with a Large Rift Valley fever outbreak among livestock in Kenya during 2006–2007. J Virol. 2008;82:11152–66. doi: 10.1128/JVI.01519-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J Am Vet Med Assoc. 2009;234:883–93. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- Bosch I, Herrera F, Navarro JC, Lentino M, Dupuis A, Maffei J, Jones M, Fernandez E, Perez N, Perez-Eman J, Guimaraes AE, Barrera R, Valero N, Ruiz J, Velasquez G, Martinez J, Comach G, Komar N, Spielman A, Kramer L. West Nile virus, Venezuela. Emerg Infect Dis. 2007;13:651–3. doi: 10.3201/eid1304.061383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosio CF, Beaty BJ, Black WCt. Quantitative genetics of vector competence for dengue-2 virus in Aedes aegypti. Am J Trop Med Hyg. 1998;59:965–70. doi: 10.4269/ajtmh.1998.59.965. [DOI] [PubMed] [Google Scholar]
- Bowen GS, Calisher CH. Virological and serological studies of Venezuelan equine encephalomyelitis in humans. J Clin Microbiol. 1976;4:22–7. doi: 10.1128/jcm.4.1.22-27.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle DB, Dickerman RW, Marshall ID. Primary viraemia responses of herons to experimental infection with Murray Valley encephalitis, Kunjin and Japanese encephalitis viruses. Aust J Exp Biol Med Sci. 1983;61:655–64. doi: 10.1038/icb.1983.62. [DOI] [PubMed] [Google Scholar]
- Brault AC, Huang CY, Langevin SA, Kinney RM, Bowen RA, Ramey WN, Panella NA, Holmes EC, Powers AM, Miller BR. A single positively selected West Nile viral mutation confers increased virogenesis in American crows. Nat Genet. 2007;39:1162–6. doi: 10.1038/ng2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault AC, Powers AM, Holmes EC, Woelk CH, Weaver SC. Positively charged amino acid substitutions in the E2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J Virol. 2002a;76:1718–30. doi: 10.1128/JVI.76.4.1718-1730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault AC, Powers AM, Medina G, Wang E, Kang W, Salas RA, De Siger J, Weaver SC. Potential sources of the 1995 Venezuelan equine encephalitis subtype IC epidemic. J Virol. 2001;75:5823–32. doi: 10.1128/JVI.75.13.5823-5832.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault AC, Powers AM, Ortiz D, Estrada-Franco JG, Navarro-Lopez R, Weaver SC. Venezuelan equine encephalitis emergence: Enhanced vector infection from a single amino acid substitution in the envelope glycoprotein. Proc Natl Acad Sci USA. 2004;101:11344–9. doi: 10.1073/pnas.0402905101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brault AC, Powers AM, Weaver SC. Vector infection determinants of Venezuelan equine encephalitis virus reside within the E2 envelope glycoprotein. J Virol. 2002b;76:6387–92. doi: 10.1128/JVI.76.12.6387-6392.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant J, Wang H, Cabezas C, Ramirez G, Watts D, Russell K, Barrett A. Enzootic transmission of yellow fever virus in Peru. Emerg Infect Dis. 2003;9:926–33. doi: 10.3201/eid0908.030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant JE, Holmes EC, Barrett AD. Out of Africa: a molecular perspective on the introduction of yellow fever virus into the Americas. PLoS Pathog. 2007;3:e75. doi: 10.1371/journal.ppat.0030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buescher EL, Scherer WF. Ecologic studies of Japanese encephalitis virus in Japan. IX. Epidemiologic correlations and conclusions. Am J Trop Med Hyg. 1959;8:719–22. doi: 10.4269/ajtmh.1959.8.719. [DOI] [PubMed] [Google Scholar]
- Buescher EL, Scherer WF, Mc CH, Moyer JT, Rosenberg MZ, Yoshii M, Okada Y. Ecologic studies of Japanese encephalitis virus in Japan. IV. Avian infection. Am J Trop Med Hyg. 1959;8:678–88. doi: 10.4269/ajtmh.1959.8.678. [DOI] [PubMed] [Google Scholar]
- Burke DS, Leake CJ. Japanese Encephalitis. In: Monath TP, editor. The Arboviruses: Epidemiology and Ecology. III. CRC Press; Boca Raton, Florida: 1988. pp. 63–92. [Google Scholar]
- Calisher CH, Karabatsos N. Arbovirus serogroups: Definition and geographic distribution. In: Monath TP, editor. The Arboviruses: Epidemiology and Ecology. I. CRC Press; Boca Raton, Florida: 1988. pp. 19–57. [Google Scholar]
- Cardosa J, Ooi MH, Tio PH, Perera D, Holmes EC, Bibi K, Abdul Manap Z. Dengue virus serotype 2 from a sylvatic lineage isolated from a patient with dengue hemorrhagic Fever. PLoS Negl Trop Dis. 2009;3:e423. doi: 10.1371/journal.pntd.0000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey DE. Chikungunya and dengue: a case of mistaken identity? J Hist Med Allied Sci. 1971;26:243–62. doi: 10.1093/jhmas/xxvi.3.243. [DOI] [PubMed] [Google Scholar]
- Carpenter S, McArthur C, Selby R, Ward R, Nolan DV, Luntz AJ, Dallas JF, Tripet F, Mellor PS. Experimental infection studies of UK Culicoides species midges with bluetongue virus serotypes 8 and 9. Vet Rec. 2008;163:589–92. doi: 10.1136/vr.163.20.589. [DOI] [PubMed] [Google Scholar]
- Carpenter S, Wilson A, Mellor PS. Culicoides and the emergence of bluetongue virus in northern Europe. Trends Microbiol. 2009;17:172–8. doi: 10.1016/j.tim.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Coimbra TL, Santos CL, Suzuki A, Petrella SM, Bisordi I, Nagamori AH, Marti AT, Santos RN, Fialho DM, Lavigne S, Buzzar MR, Rocco IM. Mayaro virus: imported cases of human infection in Sao Paulo State, Brazil. Rev Inst Med Trop Sao Paulo. 2007;49:221–4. doi: 10.1590/s0036-46652007000400005. [DOI] [PubMed] [Google Scholar]
- Cologna R, Armstrong PM, Rico-Hesse R. Selection for virulent dengue viruses occurs in humans and mosquitoes. J Virol. 2005;79:853–9. doi: 10.1128/JVI.79.2.853-859.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee of Emerging Microbial Threats to Health. Microbial threats to health; emergence, detection and response. National Academies Press; Washington, D.C: 2001. [PubMed] [Google Scholar]
- Daubney R, Hudson JR, Garnham PC. Enzootic hepatitis or Rift Valley fever. An undescribed virus disease of sheep cattle andman from East Africa. J Pathol Bacteriol. 1931:34. [Google Scholar]
- Davis CT, Beasley DW, Guzman H, Raj R, D’Anton M, Novak RJ, Unnasch TR, Tesh RB, Barrett AD. Genetic variation among temporally and geographically distinct West Nile virus isolates, United States, 2001, 2002. Emerg Infect Dis. 2003;9:1423–9. doi: 10.3201/eid0911.030301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JR, Lederberg J. Emerging Infectious Diseases from the Global to the Local Perspective: Workshop Summary. National Academies Press; Washington, D.C: 2001. [PubMed] [Google Scholar]
- Dawson JR, Stone WB, Ebel GD, Young DS, Galinski DS, Pensabene JP, Franke MA, Eidson M, Kramer LD. Crow deaths caused by West Nile virus during winter. Emerg Infect Dis. 2007;13:1912–4. doi: 10.3201/eid1312.070413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deardorff E, Estrada-Franco J, Brault AC, Navarro-Lopez R, Campomanes-Cortes A, Paz-Ramirez P, Solis-Hernandez M, Ramey WN, Davis CT, Beasley DW, Tesh RB, Barrett AD, Weaver SC. Introductions of West Nile virus strains to Mexico. Emerg Infect Dis. 2006;12:314–8. doi: 10.3201/eid1202.050871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diallo M, Sall AA, Moncayo AC, Ba Y, Fernandez Z, Ortiz D, Coffey LL, Mathiot C, Tesh RB, Weaver SC. Potential role of sylvatic and domestic african mosquito species in dengue emergence. Am J Trop Med Hyg. 2005;73:445–9. [PubMed] [Google Scholar]
- Dick GW, Kitchen SF, Haddow AJ. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46:509–20. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, Pretrick M, Marfel M, Holzbauer S, Dubray C, Guillaumot L, Griggs A, Bel M, Lambert AJ, Laven J, Kosoy O, Panella A, Biggerstaff BJ, Fischer M, Hayes EB. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360:2536–43. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- Dupuis AP, 2nd, Marra PP, Kramer LD. Serologic evidence of West Nile virus transmission, Jamaica, West Indies. Emerg Infect Dis. 2003;9:860–3. doi: 10.3201/eid0907.030249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuis AP, 2nd, Marra PP, Reitsma R, Jones MJ, Louie KL, Kramer LD. Serologic evidence for West Nile virus transmission in Puerto Rico and Cuba. Am J Trop Med Hyg. 2005;73:474–6. [PubMed] [Google Scholar]
- Effler PV, Pang L, Kitsutani P, Vorndam V, Nakata M, Ayers T, Elm J, Tom T, Reiter P, Rigau-Perez JG, Hayes JM, Mills K, Napier M, Clark GG, Gubler DJ. Dengue fever, Hawaii, 2001–2002. Emerg Infect Dis. 2005;11:742–9. doi: 10.3201/eid1105.041063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endy TP, Weaver SC, Hanley KA. Dengue Virus - Past, Present and Future. In: Hanley KA, Weaver SC, editors. Frontiers in Dengue Virus Research. Horizon Press; Norwich, U.K: 2010. in press. [Google Scholar]
- Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emerg Infect Dis. 2009;15:1–7. doi: 10.3201/eid1501.080311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farfan-Ale JA, Blitvich BJ, Lorono-Pino MA, Marlenee NL, Rosado-Paredes EP, Garcia-Rejon JE, Flores-Flores LF, Chulim-Perera L, Lopez-Uribe M, Perez-Mendoza G, Sanchez-Herrera I, Santamaria W, Moo-Huchim J, Gubler DJ, Cropp BC, Calisher CH, Beaty BJ. Longitudinal studies of West Nile virus infection in avians, Yucatan State, Mexico. Vector Borne Zoonotic Dis. 2004;4:3–14. doi: 10.1089/153036604773082942. [DOI] [PubMed] [Google Scholar]
- Farfan-Ale JA, Blitvich BJ, Marlenee NL, Lorono-Pino MA, Puerto-Manzano F, Garcia-Rejon JE, Rosado-Paredes EP, Flores-Flores LF, Ortega-Salazar A, Chavez-Medina J, Cremieux-Grimaldi JC, Correa-Morales F, Hernandez-Gaona G, Mendez-Galvan JF, Beaty BJ. Antibodies to West Nile virus in asymptomatic mammals, birds, and reptiles in the Yucatan Peninsula of Mexico. Am J Trop Med Hyg. 2006;74:908–14. [PubMed] [Google Scholar]
- Fauci AS. Emerging and reemerging infectious diseases: the perpetual challenge. Acad Med. 2005;80:1079–85. doi: 10.1097/00001888-200512000-00002. [DOI] [PubMed] [Google Scholar]
- Faye O, Diallo M, Diop D, Bezeid OE, Ba H, Niang M, Dia I, Mohamed SA, Ndiaye K, Diallo D, Ly PO, Diallo B, Nabeth P, Simon F, Lo B, Diop OM. Rift Valley fever outbreak with East-Central African virus lineage in Mauritania, 2003. Emerg Infect Dis. 2007;13:1016–23. doi: 10.3201/eid1307.061487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez Z, Moncayo AC, Carrara AS, Forattini OP, Weaver SC. Vector competence of rural and urban strains of Aedes (Stegomyia) albopictus (Diptera: Culicidae) from Sao Paulo State, Brazil for IC, ID, and IF subtypes of Venezuelan equine encephalitis virus. J Med Entomol. 2003;40:522–7. doi: 10.1603/0022-2585-40.4.522. [DOI] [PubMed] [Google Scholar]
- Fonseca DM, Keyghobadi N, Malcolm CA, Mehmet C, Schaffner F, Mogi M, Fleischer RC, Wilkerson RC. Emerging vectors in the Culex pipiens complex. Science. 2004;303:1535–8. doi: 10.1126/science.1094247. [DOI] [PubMed] [Google Scholar]
- Fyodorova MV, Savage HM, Lopatina JV, Bulgakova TA, Ivanitsky AV, Platonova OV, Platonov AE. Evaluation of potential West Nile virus vectors in Volgograd region, Russia, 2003 (Diptera: Culicidae): species composition, bloodmeal host utilization, and virus infection rates of mosquitoes. J Med Entomol. 2006;43:552–63. doi: 10.1603/0022-2585(2006)43[552:eopwnv]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Gargan TP, 2nd, Clark GG, Dohm DJ, Turell MJ, Bailey CL. Vector potential of selected North American mosquito species for Rift Valley fever virus. Am J Trop Med Hyg. 1988;38:440–6. doi: 10.4269/ajtmh.1988.38.440. [DOI] [PubMed] [Google Scholar]
- Gibbs EP, Lawman MJ, Herniman KA. Preliminary observations on transplacental infection of bluetongue virus in sheep-a possible overwintering mechanism. Res Vet Sci. 1979;27:118–20. [PubMed] [Google Scholar]
- Gibbs EPJ, Greiner EC. Bluetongue and Epizootic Hemorrhagic Disease. In: Monath TP, editor. The Arboviruses: Epidemiology and Ecology. II. CRC Press; Boca Raton, Florida: 1988. pp. 39–70. [Google Scholar]
- Goddard LB, Roth AE, Reisen WK, Scott TW. Vector competence of California mosquitoes for West Nile virus. Emerg Infect Dis. 2002;8:1385–91. doi: 10.3201/eid0812.020536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubler DJ. Dengue and dengue hemorrhagic fever: its history and resurgence as a global public health problem. In: Gubler DJ, Kuno G, editors. Dengue and Dengue Hemorrhagic Fever. CAB International; New York: 1997. pp. 1–22. [Google Scholar]
- Gubler DJ. Resurgent vector-borne diseases as a global health problem. Emerg Infect Dis. 1998;4:442–50. doi: 10.3201/eid0403.980326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddow AJ, Williams MC, Woodall JP, Simpson DI, Goma LK. Twelve Isolations of Zika Virus from Aedes (Stegomyia) Africanus (Theobald) Taken in and above a Uganda Forest. Bull World Health Organ. 1964;31:57–69. [PMC free article] [PubMed] [Google Scholar]
- Hall RA, Broom AK, Smith DW, Mackenzie JS. The ecology and epidemiology of Kunjin virus. Curr Top Microbiol Immunol. 2002;267:253–69. doi: 10.1007/978-3-642-59403-8_13. [DOI] [PubMed] [Google Scholar]
- Halstead SB, O’Rourke EJ. Antibody-enhanced dengue virus infection in primate leukocytes. Nature. 1977a;265:739–41. doi: 10.1038/265739a0. [DOI] [PubMed] [Google Scholar]
- Halstead SB, O’Rourke EJ. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J Exp Med. 1977b;146:201–17. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer GL, Kitron UD, Goldberg TL, Brawn JD, Loss SR, Ruiz MO, Hayes DB, Walker ED. Host selection by Culex pipiens mosquitoes and West Nile virus amplification. Am J Trop Med Hyg. 2009;80:268–78. [PubMed] [Google Scholar]
- Hammon WM, Rees DM, et al. Experimental transmission of Japanese B encephalitis virus by Culex tritaeniorhynchus and Culex pipiens var. pallens, suspected natural vectors. Am J Hyg. 1949;50:46–50. doi: 10.1093/oxfordjournals.aje.a119343. [DOI] [PubMed] [Google Scholar]
- Hammon WM, Tigertt WD, Sather GE, Berge TO, Meiklejohn G. Epidemiologic studies of concurrent virgin epidemics of Japanese B encephalitis and of mumps on Guam, 1947–1948, with subsequent observations including dengue, through 1957. Am J Trop Med Hyg. 1958;7:441–67. doi: 10.4269/ajtmh.1958.7.441. [DOI] [PubMed] [Google Scholar]
- Hanna JN, Ritchie SA, Phillips DA, Lee JM, Hills SL, van den Hurk AF, Pyke AT, Johansen CA, Mackenzie JS. Japanese encephalitis in north Queensland, Australia, 1998. Med J Aust. 1999;170:533–6. doi: 10.5694/j.1326-5377.1999.tb127878.x. [DOI] [PubMed] [Google Scholar]
- Hanson SM, Craig GB., Jr Aedes albopictus (Diptera: Culicidae) eggs: field survivorship during northern Indiana winters. J Med Entomol. 1995;32:599–604. doi: 10.1093/jmedent/32.5.599. [DOI] [PubMed] [Google Scholar]
- Harrington LC, Edman JD, Scott TW. Why do female Aedes aegypti (Diptera: Culicidae) feed preferentially and frequently on human blood? J Med Entomol. 2001;38:411–22. doi: 10.1603/0022-2585-38.3.411. [DOI] [PubMed] [Google Scholar]
- Hawley WA, Reiter P, Copeland RS, Pumpuni CB, Craig GB., Jr Aedes albopictus in North America: probable introduction in used tires from northern Asia. Science. 1987;236:1114–6. doi: 10.1126/science.3576225. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Shichijo A, Mifune K, Matsuo S, Wada Y, Mogi M, Itoh T. Ecological studies of Japanese encephalitis virus: Results of investigations in Nagasaki area, Japan, in 1969, 1970 and 1971. Trop Med. 1973;15:214–222. [Google Scholar]
- Hayes EB, Komar N, Nasci RS, Montgomery SP, O’Leary DR, Campbell GL. Epidemiology and transmission dynamics of West Nile virus disease. Emerg Infect Dis. 2005;11:1167–73. doi: 10.3201/eid1108.050289a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson A, Leake CJ, Burke DS. Japanese encephalitis in Nepal. Lancet. 1983;2:1359–60. doi: 10.1016/s0140-6736(83)91110-8. [DOI] [PubMed] [Google Scholar]
- Hendrickx G, Gilbert M, Staubach C, Elbers A, Mintiens K, Gerbier G, Ducheyne E. A wind density model to quantify the airborne spread of Culicoides species during north-western Europe bluetongue epidemic, 2006. Prev Vet Med. 2008;87:162–81. doi: 10.1016/j.prevetmed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Hochachka WM, Dhondt AA, McGowan KJ, Kramer LD Impact of West Nile virus on American Crows in the Northeastern United States, a.i.r.t.e.m.p. Ecohealth. 2004;1:60–68. [Google Scholar]
- Holland J, Domingo E. Origin and evolution of viruses. Virus Genes. 1998;16:13–21. doi: 10.1023/a:1007989407305. [DOI] [PubMed] [Google Scholar]
- Hoogstraal H, Meegan JM, Khalil GM, Adham FK. The Rift Valley fever epizootic in Egypt 1977–78. 2. Ecological and entomological studies. Trans R Soc Trop Med Hyg. 1979;73:624–9. doi: 10.1016/0035-9203(79)90005-1. [DOI] [PubMed] [Google Scholar]
- Igarashi A, Tanaka M, Morita K, Takasu T, Ahmed A, Akram DS, Waqar MA. Detection of west Nile and Japanese encephalitis viral genome sequences in cerebrospinal fluid from acute encephalitis cases in Karachi, Pakistan. Microbiol Immunol. 1994;38:827–30. doi: 10.1111/j.1348-0421.1994.tb01866.x. [DOI] [PubMed] [Google Scholar]
- Jamgaonkar AV, Yergolkar PN, Geevarghese G, Joshi GD, Joshi MV, Mishra AC. Serological evidence for Japanese encephalitis virus and West Nile virus infections in water frequenting and terrestrial wild birds in Kolar District, Karnataka State, India. A retrospective study. Acta Virol. 2003;47:185–8. [PubMed] [Google Scholar]
- Johnson KM, Shelokov A, Peralta PH, Dammin GJ, Young NA. Recovery of Venezuelan equine encephalomyelitis virus in Panama. A fatal case in man. Am J Trop Med Hyg. 1968;17:432–40. doi: 10.4269/ajtmh.1968.17.432. [DOI] [PubMed] [Google Scholar]
- Jones RH, Foster NM. Heterogeneity of Culicoides variipennis field populations to oral infection with bluetongue virus. Am J Trop Med Hyg. 1978;27:178–183. doi: 10.4269/ajtmh.1978.27.178. [DOI] [PubMed] [Google Scholar]
- Jupp PG, McIntosh BM. Chikungunya virus disease. In: Monath TP, editor. The Arbovirus: Epidemiology and Ecology. II. CRC Press; Boca Raton, Florida: 1988. pp. 137–157. [Google Scholar]
- Karabatsos N. Am Soc Trop Med Hyg. San Antonio: 1985. International Catalogue of Arboviruses. [DOI] [PubMed] [Google Scholar]
- Kilpatrick AM, Kramer LD, Jones MJ, Marra PP, Daszak P. West Nile virus epidemics in North America are driven by shifts in mosquito feeding behavior. PLoS Biol. 2006;4:e82. doi: 10.1371/journal.pbio.0040082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick AM, Meola MA, Moudy RM, Kramer LD. Temperature, viral genetics, and the transmission of West Nile virus by Culex pipiens mosquitoes. PLoS Pathog. 2008;4:e1000092. doi: 10.1371/journal.ppat.1000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochel TJ, Watts DM, Halstead SB, Hayes CG, Espinoza A, Felices V, Caceda R, Bautista CT, Montoya Y, Douglas S, Russell KL. Effect of dengue-1 antibodies on American dengue-2 viral infection and dengue haemorrhagic fever. Lancet. 2002;360:310–2. doi: 10.1016/S0140-6736(02)09522-3. [DOI] [PubMed] [Google Scholar]
- Komar N. West Nile viral encephalitis. Rev Sci Tech. 2000;19:166–76. doi: 10.20506/rst.19.1.1201. [DOI] [PubMed] [Google Scholar]
- Komar N. West Nile virus: epidemiology and ecology in North America. Adv Virus Res. 2003;61:185–234. doi: 10.1016/s0065-3527(03)61005-5. [DOI] [PubMed] [Google Scholar]
- Komar N, Panella NA, Burns JE, Dusza SW, Mascarenhas TM, Talbot TO. Serologic evidence for West Nile virus infection in birds in the New York City vicinity during an outbreak in 1999. Emerg Infect Dis. 2001;7:621–5. doi: 10.3201/eid0704.010403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono R, Kim KH. Comparative epidemiological features of Japanese encephalitis in the Republic of Korea, China (Taiwan) and Japan. Bull World Health Organ. 1969;40:263–77. [PMC free article] [PubMed] [Google Scholar]
- Kramer LD, Styer LM, Ebel GD. A global perspective on the epidemiology of West Nile virus. Annu Rev Entomol. 2008;53:61–81. doi: 10.1146/annurev.ento.53.103106.093258. [DOI] [PubMed] [Google Scholar]
- Krishnamoorthy K, Harichandrakumar KT, Krishna Kumari A, Das LK. Burden of chikungunya in India: estimates of disability adjusted life years (DALY) lost in 2006 epidemic. J Vector Borne Dis. 2009;46:26–35. [PubMed] [Google Scholar]
- Lanciotti RS, Ebel GD, Deubel V, Kerst AJ, Murri S, Meyer R, Bowen M, McKinney N, Morrill WE, Crabtree MB, Kramer LD, Roehrig JT. Complete genome sequences and phylogenetic analysis of West Nile virus strains isolated from the United States, Europe, and the Middle East. Virology. 2002;298:96–105. doi: 10.1006/viro.2002.1449. [DOI] [PubMed] [Google Scholar]
- Lanciotti RS, Kosoy OL, Laven JJ, Panella AJ, Velez JO, Lambert AJ, Campbell GL. Chikungunya virus in US travelers returning from India, 2006. Emerg Infect Dis. 2007;13:764–7. doi: 10.3201/eid1305.070015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, Stanfield SM, Duffy MR. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–9. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanciotti RS, Roehrig JT, Deubel V, Smith J, Parker M, Steele K, Crise B, Volpe KE, Crabtree MB, Scherret JH, Hall RA, MacKenzie JS, Cropp CB, Panigrahy B, Ostlund E, Schmitt B, Malkinson M, Banet C, Weissman J, Komar N, Savage HM, Stone W, McNamara T, Gubler DJ. Origin of the West Nile virus responsible for an outbreak of encephalitis in the northeastern United States. Science. 1999;286:2333–7. doi: 10.1126/science.286.5448.2333. [DOI] [PubMed] [Google Scholar]
- Langevin SA, Brault AC, Panella NA, Bowen RA, Komar N. Variation in virulence of West Nile virus strains for house sparrows (Passer domesticus) Am J Trop Med Hyg. 2005;72:99–102. [PubMed] [Google Scholar]
- Lee VH. Report of virus Research Laboratory. University of Ibadan; Ibadan, Nigeria: 1969. Studies of arthropod hosts: Virus isolations; p. 100. [Google Scholar]
- Linthicum KJ, Anyamba A, Tucker CJ, Kelley PW, Myers MF, Peters CJ. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science. 1999;285:397–400. doi: 10.1126/science.285.5426.397. [DOI] [PubMed] [Google Scholar]
- Linthicum KJ, Davies FG, Kairo A, Bailey CL. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J Hyg (Lond) 1985a;95:197–209. doi: 10.1017/s0022172400062434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linthicum KJ, Kaburia HF, Davies FG, Lindqvist KJ. A blood meal analysis of engorged mosquitoes found in Rift Valley fever epizootics area in Kenya. J Am Mosq Control Assoc. 1985b;1:93–5. [PubMed] [Google Scholar]
- Lorono-Pino MA, Blitvich BJ, Farfan-Ale JA, Puerto FI, Blanco JM, Marlenee NL, Rosado-Paredes EP, Garcia-Rejon JE, Gubler DJ, Calisher CH, Beaty BJ. Serologic evidence of West Nile virus infection in horses, Yucatan State, Mexico. Emerg Infect Dis. 2003;9:857–9. doi: 10.3201/eid0907.030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysyk TJ. Seasonal abundance, parity, and survival of adult Culicoides sonorensis (Diptera: Ceratopogonidae) in southern Alberta, Canada. J Med Entomol. 2007;44:959–69. doi: 10.1603/0022-2585(2007)44[959:sapaso]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Lysyk TJ, Danyk T. Effect of temperature on life history parameters of adult Culicoides sonorensis (Diptera: Ceratopogonidae) in relation to geographic origin and vectorial capacity for bluetongue virus. J Med Entomol. 2007;44:741–51. doi: 10.1603/0022-2585(2007)44[741:eotolh]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Mackenzie JS, Chua KB, Daniels PW, Eaton BT, Field HE, Hall RA, Halpin K, Johansen CA, Kirkland PD, Lam SK, McMinn P, Nisbet DJ, Paru R, Pyke AT, Ritchie SA, Siba P, Smith DW, Smith GA, van den Hurk AF, Wang LF, Williams DT. Emerging viral diseases of Southeast Asia and the Western Pacific. Emerg Infect Dis. 2001;7:497–504. doi: 10.3201/eid0707.017703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie JS, Johansen CA, Ritchie SA, van den Hurk AF, Hall RA. Japanese encephalitis as an emerging virus: the emergence and spread of Japanese encephalitis virus in Australasia. Curr Top Microbiol Immunol. 2002;267:49–73. doi: 10.1007/978-3-642-59403-8_3. [DOI] [PubMed] [Google Scholar]
- Madani TA, Al-Mazrou YY, Al-Jeffri MH, Mishkhas AA, Al-Rabeah AM, Turkistani AM, Al-Sayed MO, Abodahish AA, Khan AS, Ksiazek TG, Shobokshi O. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin Infect Dis. 2003;37:1084–92. doi: 10.1086/378747. [DOI] [PubMed] [Google Scholar]
- Malkinson M, Banet C, Weisman Y, Pokamunski S, King R, Drouet MT, Deubel V. Introduction of West Nile virus in the Middle East by migrating white storks. Emerg Infect Dis. 2002;8:392–7. doi: 10.3201/eid0804.010217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchette NJ, Garcia R, Rudnick A. Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. Am J Trop Med Hyg. 1969;18:411–5. doi: 10.4269/ajtmh.1969.18.411. [DOI] [PubMed] [Google Scholar]
- Mattingly PF. Taxonomy of Aedes aegypti and related species. Bull World Health Organ. 1967;36:552–4. [PMC free article] [PubMed] [Google Scholar]
- Mavalankar D, Shastri P, Bandyopadhyay T, Parmar J, Ramani KV. Increased mortality rate associated with chikungunya epidemic, ahmedabad, India. Emerg Infect Dis. 2008;14:412–5. doi: 10.3201/eid1403.070720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meegan J, Le Guenno B, Ksiazek T, Jouan A, Knauert F, Digoutte JP, Peters CJ. Rapid diagnosis of Rift Valley fever: a comparison of methods for the direct detection of viral antigen in human sera. Res Virol. 1989;140:59–65. doi: 10.1016/s0923-2516(89)80085-8. [DOI] [PubMed] [Google Scholar]
- Meegan JM, Moussa MI, el-Mour AF, Toppouzzada RH, Wyess RN. Ecological and epidemiological studies of Rift Valley fever in Egypt. J Egypt Public Health Assoc. 1978;53:173–5. [PubMed] [Google Scholar]
- Mendez W, Liria J, Navarro JC, Garcia CZ, Freier JE, Salas R, Weaver SC, Barrera R. Spatial dispersion of adult mosquitoes (Diptera: Culicidae) in a sylvatic focus of Venezuelan equine encephalitis virus. J Med Entomol. 2001;38:813–21. doi: 10.1603/0022-2585-38.6.813. [DOI] [PubMed] [Google Scholar]
- Metcalf HE, Pearson JE, Klingsporn AL. Bluetongue in cattle: a serologic survey of slaughter cattle in the United States. Am J Vet Res. 1981;42:1057–61. [PubMed] [Google Scholar]
- Mitchell CJ, Chen PS, Boreham PF. Host-feeding patterns and behaviour of 4 Culex species in an endemic area of Japanese encephalitis. Bull World Health Organ. 1973;49:293–9. [PMC free article] [PubMed] [Google Scholar]
- Mitchell CJ, Savage HM, Smith GC, Flood SP, Castro LT, Roppul M. Japanese encephalitis on Saipan: a survey of suspected mosquito vectors. Am J Trop Med Hyg. 1993;48:585–90. doi: 10.4269/ajtmh.1993.48.585. [DOI] [PubMed] [Google Scholar]
- Monath TP. epidemiology. In: Monath TP, editor. St Louis Encephalitis. Am. Public Health Assoc; Washington, D. C: 1980. pp. 239–312. [Google Scholar]
- Monath TP. Yellow fever. In: Monath TP, editor. The Arboviruses: Epidemiology and Ecology. V. CRC Press; Boca Raton, Florida: 1988. pp. 139–241. [Google Scholar]
- Monath TP. Yellow Fever. In: Service MW, editor. The Encyclopedia of Arthropod-transmitted Infections. CAB International; Wallingford, UK: 2001. pp. 571–577. [Google Scholar]
- Morales MA, Barrandeguy M, Fabbri C, Garcia JB, Vissani A, Trono K, Gutierrez G, Pigretti S, Menchaca H, Garrido N, Taylor N, Fernandez F, Levis S, Enria D. West Nile virus isolation from equines in Argentina, 2006. Emerg Infect Dis. 2006;12:1559–61. doi: 10.3201/eid1210.060852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudy RM, Meola MA, Morin LL, Ebel GD, Kramer LD. A newly emergent genotype of West Nile virus is transmitted earlier and more efficiently by Culex mosquitoes. Am J Trop Med Hyg. 2007;77:365–70. [PubMed] [Google Scholar]
- Mullens BA, Tabachnick WJ, Holbrook FR, Thompson LH. Effects of temperature on virogenesis of bluetongue virus serotype 11 in Culicoides variipennis sonorensis. Med Vet Entomol. 1995;9:71–6. doi: 10.1111/j.1365-2915.1995.tb00119.x. [DOI] [PubMed] [Google Scholar]
- Mutebi JP, Gianella A, Travassos da Rosa A, Tesh RB, Barrett AD, Higgs S. Yellow fever virus infectivity for Bolivian Aedes aegypti mosquitoes. Emerg Infect Dis. 2004;10:1657–60. doi: 10.3201/eid1009.031124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabeth P, Kane Y, Abdalahi MO, Diallo M, Ndiaye K, Ba K, Schneegans F, Sall AA, Mathiot C. Rift Valley fever outbreak, Mauritania, 1998: seroepidemiologic, virologic, entomologic, and zoologic investigations. Emerg Infect Dis. 2001;7:1052–4. doi: 10.3201/eid0706.010627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasci RS, Savage HM, White DJ, Miller JR, Cropp BC, Godsey MS, Kerst AJ, Bennett P, Gottfried K, Lanciotti RS. West Nile virus in overwintering Culex mosquitoes, New York City, 2000. Emerg Infect Dis. 2001a;7:742–4. doi: 10.3201/eid0704.010426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasci RS, White DJ, Stirling H, Oliver JA, Daniels TJ, Falco RC, Campbell S, Crans WJ, Savage HM, Lanciotti RS, Moore CG, Godsey MS, Gottfried KL, Mitchell CJ. West Nile virus isolates from mosquitoes in New York and New Jersey, 1999. Emerg Infect Dis. 2001b;7:626–30. doi: 10.3201/eid0704.010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawrocki SJ, Hawley WA. Estimation of the northern limits of distribution of Aedes albopictus in North America. J Am Mosq Control Assoc. 1987;3:314–7. [PubMed] [Google Scholar]
- Nemeth N, Young G, Ndaluka C, Bielefeldt-Ohmann H, Komar N, Bowen R. Persistent West Nile virus infection in the house sparrow (Passer domesticus) Arch Virol. 2009;154:783–9. doi: 10.1007/s00705-009-0369-x. [DOI] [PubMed] [Google Scholar]
- Nett RJ, Campbell GL, Reisen WK. Potential for the Emergence of Japanese Encephalitis Virus in California. Vector-Borne and Zoonotic Diseases. 2009 doi: 10.1089/vbz.2008.0052. in press. [DOI] [PubMed] [Google Scholar]
- Okuno T, Mitchell CJ, Chen PS, Hsu S, Ryu E. Experimental transmission of Japanese encephalitis virus by Culex tritaeniorhynchus and C. fuscocephalus. Ann Trop Med Parasitol. 1975;69:203–6. doi: 10.1080/00034983.1975.11687002. [DOI] [PubMed] [Google Scholar]
- Olson JG, Ksiazek TG, Suhandiman, Triwibowo Zika virus, a cause of fever in Central Java, Indonesia. Trans R Soc Trop Med Hyg. 1981;75:389–93. doi: 10.1016/0035-9203(81)90100-0. [DOI] [PubMed] [Google Scholar]
- Ortiz DI, Kang W, Weaver SC. Susceptibility of Ae. aegypti (Diptera: Culicidae) to infection with epidemic (subtype IC) and enzootic (subtypes ID, IIIC, IIID) Venezuelan equine encephalitis complex alphaviruses. J Med Entomol. 2008;45:1117–25. doi: 10.1603/0022-2585(2008)45[1117:soaadc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Ortiz DI, Weaver SC. Susceptibility of Ochlerotatus taeniorhynchus (Diptera: Culicidae) to infection with epizootic (subtype IC) and enzootic (subtype ID) Venezuelan equine encephalitis viruses: evidence for epizootic strain adaptation. J Med Entomol. 2004;41:987–93. doi: 10.1603/0022-2585-41.5.987. [DOI] [PubMed] [Google Scholar]
- Partridge J, Ghimire P, Sedai T, Bista MB, Banerjee M. Endemic Japanese encephalitis in the Kathmandu valley, Nepal. Am J Trop Med Hyg. 2007;77:1146–9. [PubMed] [Google Scholar]
- Pond WL. Arthropod-Borne Virus Antibodies in Sera from Residents of South-East Asia. Trans R Soc Trop Med Hyg. 1963;57:364–71. doi: 10.1016/0035-9203(63)90100-7. [DOI] [PubMed] [Google Scholar]
- Powers AM, Brault AC, Tesh RB, Weaver SC. Re-emergence of chikungunya and o’nyong-nyong viruses: evidence for distinct geographical lineages and distant evolutionary relationships. J Gen Virol. 2000;81:471–479. doi: 10.1099/0022-1317-81-2-471. [DOI] [PubMed] [Google Scholar]
- Powers AM, Logue CH. Changing patterns of chikungunya virus: re-emergence of a zoonotic arbovirus. J Gen Virol. 2007;88:2363–77. doi: 10.1099/vir.0.82858-0. [DOI] [PubMed] [Google Scholar]
- Powers AM, Oberste MS, Brault AC, Rico-Hesse R, Schmura SM, Smith JF, Kang W, Sweeney WP, Weaver SC. Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis from a single genotype of enzootic subtype ID virus. J Virol. 1997;71:6697–705. doi: 10.1128/jvi.71.9.6697-6705.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince HE, Hogrefe WR. Detection of West Nile virus (WNV)-specific immunoglobulin M in a reference laboratory setting during the 2002 WNV season in the United States. Clin Diagn Lab Immunol. 2003;10:764–8. doi: 10.1128/CDLI.10.5.764-768.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purse BV, Brown HE, Harrup L, Mertens PP, Rogers DJ. Invasion of bluetongue and other orbivirus infections into Europe: the role of biological and climatic processes. Rev Sci Tech. 2008;27:427–42. [PubMed] [Google Scholar]
- Purse BV, Mellor PS, Rogers DJ, Samuel AR, Mertens PP, Baylis M. Climate change and the recent emergence of bluetongue in Europe. Nat Rev Microbiol. 2005;3:171–81. doi: 10.1038/nrmicro1090. [DOI] [PubMed] [Google Scholar]
- Quiroz E, Aguilar PV, Cisneros J, Tesh RB, Weaver SC. Venezuelan equine encephalitis in panama: fatal endemic disease and genetic diversity of etiologic viral strains. PLoS Negl Trop Dis. 2009;3:e472. doi: 10.1371/journal.pntd.0000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisen W, Lothrop H, Chiles R, Madon M, Cossen C, Woods L, Husted S, Kramer V, Edman J. West Nile virus in California. Emerg Infect Dis. 2004;10:1369–78. doi: 10.3201/eid1008.040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisen WK, Boreham PF. Host selection patterns of some Pakistan mosquitoes. Am J Trop Med Hyg. 1979;28:408–21. doi: 10.4269/ajtmh.1979.28.408. [DOI] [PubMed] [Google Scholar]
- Reisen WK, Fang Y, Martinez VM. Avian host and mosquito (Diptera: Culicidae) vector competence determine the efficiency of West Nile and St. Louis encephalitis virus transmission. J Med Entomol. 2005;42:367–75. doi: 10.1093/jmedent/42.3.367. [DOI] [PubMed] [Google Scholar]
- Reisen WK, Fang Y, Martinez VM. Effects of temperature on the transmission of west nile virus by Culex tarsalis (Diptera: Culicidae) J Med Entomol. 2006;43:309–17. doi: 10.1603/0022-2585(2006)043[0309:EOTOTT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Rezza G, Nicoletti L, Angelini R, Romi R, Finarelli AC, Panning M, Cordioli P, Fortuna C, Boros S, Magurano F, Silvi G, Angelini P, Dottori M, Ciufolini MG, Majori GC, Cassone A. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370:1840–6. doi: 10.1016/S0140-6736(07)61779-6. [DOI] [PubMed] [Google Scholar]
- Rico-Hesse R, Weaver SC, de Siger J, Medina G, Salas RA. Emergence of a new epidemic/epizootic Venezuelan equine encephalitis virus in South America. Proc Natl Acad Sci U S A. 1995;92:5278–81. doi: 10.1073/pnas.92.12.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivas F, Diaz LA, Cardenas VM, Daza E, Bruzon L, Alcala A, De la Hoz O, Caceres FM, Aristizabal G, Martinez JW, Revelo D, De la Hoz F, Boshell J, Camacho T, Calderon L, Olano VA, Villarreal LI, Roselli D, Alvarez G, Ludwig G, Tsai T. Epidemic Venezuelan equine encephalitis in La Guajira, Colombia, 1995. J Infect Dis. 1997;175:828–32. doi: 10.1086/513978. [DOI] [PubMed] [Google Scholar]
- Robin S, Ramful D, Le Seach F, Jaffar-Bandjee MC, Rigou G, Alessandri JL. Neurologic Manifestations of Pediatric Chikungunya Infection. J Child Neurol. 2008 doi: 10.1177/0883073808314151. [DOI] [PubMed] [Google Scholar]
- Rocha C, Morrison AC, Forshey BM, Blair PJ, Olson JG, Stancil JD, Sihuincha M, Scott TW, Kochel TJ. Comparison of two active surveillance programs for the detection of clinical dengue cases in Iquitos, Peru. Am J Trop Med Hyg. 2009;80:656–60. [PubMed] [Google Scholar]
- Rodrigues FM, Guttikar SN, Pinto BD. Prevalence of antibodies to Japanese encephalitis and West Nile viruses among wild birds in the Krishna-Godavari Delta, Andhra Pradesh, India. Trans R Soc Trop Med Hyg. 1981;75:258–62. doi: 10.1016/0035-9203(81)90330-8. [DOI] [PubMed] [Google Scholar]
- Rosen L, Lien JC, Shroyer DA, Baker RH, Lu LC. Experimental vertical transmission of Japanese encephalitis virus by Culex tritaeniorhynchus and other mosquitoes. Am J Trop Med Hyg. 1989;40:548–556. doi: 10.4269/ajtmh.1989.40.548. [DOI] [PubMed] [Google Scholar]
- Rudnick A. Ecology of Dengue virus. Asian J Infect Dis. 1978;2:156–160. [Google Scholar]
- Saegerman C, Berkvens D, Mellor PS. Bluetongue epidemiology in the European Union. Emerg Infect Dis. 2008;14:539–44. doi: 10.3201/eid1404.071441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Guerrero SA, Romero-Estrella S, Rodriguez-Ruiz A, Infante-Ramirez L, Gomez A, Villanueva-Vidales E, Garcia-Torres M, Dominguez AM, Vazquez JA, Calderon ED, Valiente-Banuet L, Linnen JM, Broulik A, Harel W, Marin YLRA. Detection of West Nile virus in the Mexican blood supply. Transfusion. 2006;46:111–7. doi: 10.1111/j.1537-2995.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- Sang RC, Ahmed O, Faye O, Kelly CL, Yahaya AA, Mmadi I, Toilibou A, Sergon K, Brown J, Agata N, Yakouide A, Ball MD, Breiman RF, Miller BR, Powers AM. Entomologic investigations of a chikungunya virus epidemic in the Union of the Comoros, 2005. Am J Trop Med Hyg. 2008;78:77–82. [PubMed] [Google Scholar]
- Savage HM, Ceianu C, Nicolescu G, Karabatsos N, Lanciotti R, Vladimirescu A, Laiv L, Ungureanu A, Romanca C, Tsai TF. Entomologic and avian investigations of an epidemic of West Nile fever in Romania in 1996, with serologic and molecular characterization of a virus isolate from mosquitoes. Am J Trop Med Hyg. 1999;61:600–11. doi: 10.4269/ajtmh.1999.61.600. [DOI] [PubMed] [Google Scholar]
- Schuffenecker I, Iteman I, Michault A, Murri S, Frangeul L, Vaney MC, Lavenir R, Pardigon N, Reynes JM, Pettinelli F, Biscornet L, Diancourt L, Michel S, Duquerroy S, Guigon G, Frenkiel MP, Brehin AC, Cubito N, Despres P, Kunst F, Rey FA, Zeller H, Brisse S. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 2006;3:e263. doi: 10.1371/journal.pmed.0030263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz-Cornil I, Mertens PP, Contreras V, Hemati B, Pascale F, Breard E, Mellor PS, MacLachlan NJ, Zientara S. Bluetongue virus: virology, pathogenesis and immunity. Vet Res. 2008;39:46. doi: 10.1051/vetres:2008023. [DOI] [PubMed] [Google Scholar]
- Sellers RF. Weather, host and vector--their interplay in the spread of insect-borne animal virus diseases. J Hyg (Lond) 1980;85:65–102. doi: 10.1017/s0022172400027108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers RF, Gibbs EP, Herniman KA, Pedgley DE, Tucker MR. Possible origin of the bluetongue epidemic in Cyprus, August 1977. J Hyg (Lond) 1979;83:547–55. doi: 10.1017/s0022172400026401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers RF, Pedgley DE, Tucker MR. Possible windborne spread of bluetongue to Portugal, June–July 1956. J Hyg (Lond) 1978;81:189–96. doi: 10.1017/s0022172400025018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers RF, Pedgley DE, Tucker MR. Rift Valley fever, Egypt 1977: disease spread by windborne insect vectors? Vet Rec. 1982;110:73–7. doi: 10.1136/vr.110.4.73. [DOI] [PubMed] [Google Scholar]
- Simon F, Savini H, Parola P. Chikungunya: a paradigm of emergence and globalization of vector-borne diseases. Med Clin North Am. 2008;92:1323–43. ix. doi: 10.1016/j.mcna.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Simpson DI. Zika Virus Infection in Man. Trans R Soc Trop Med Hyg. 1964;58:335–8. [PubMed] [Google Scholar]
- Solomon T, Ni H, Beasley DW, Ekkelenkamp M, Cardosa MJ, Barrett AD. Origin and evolution of Japanese encephalitis virus in southeast Asia. J Virol. 2003;77:3091–8. doi: 10.1128/JVI.77.5.3091-3098.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soman RS, Mourya DT. Transovarial transmission of Japanese encephalitis virus in Culex bitaeniorhynchus mosquitoes. Indian J Med Res. 1985;81:257–9. [PubMed] [Google Scholar]
- Soman RS, Mourya DT, Mishra AC. Transovarial transmission of Japanese encephalitis virus in Culex vishnui mosquitoes. Indian J Med Res. 1986;84:283–5. [PubMed] [Google Scholar]
- Soman RS, Rodrigues FM, Guttikar SN, Guru PY. Experimental viraemia and transmission of Japanese encephalitis virus by mosquitoes in ardeid birds. Indian J Med Res. 1977;66:709–18. [PubMed] [Google Scholar]
- Suarez OM, Bergold GH. Investigations of an outbreak of Venezuelan equine encephalitis in towns of eastern Venezuela. Am J Trop Med Hyg. 1968;17:875–80. doi: 10.4269/ajtmh.1968.17.875. [DOI] [PubMed] [Google Scholar]
- Sylla M, Bosio C, Urdaneta-Marquez L, Ndiaye M, Black WC. Gene Flow, Subspecies Composition, and Dengue Virus-2 Susceptibility among Aedes aegypti Collections in Senegal. PLoS Negl Trop Dis. 2009;3:e408. doi: 10.1371/journal.pntd.0000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick WJ, MacLachlan NJ, Thompson LH, Hunt GJ, Patton JF. Susceptibility of Culicoides variipennis sonorensis to infection by polymerase chain reaction-detectable bluetongue virus in cattle blood. Am J Trop Med Hyg. 1996;54:481–5. doi: 10.4269/ajtmh.1996.54.481. [DOI] [PubMed] [Google Scholar]
- Tabachnick WJ, Powell JR. A world-wide survey of genetic variation in the yellow fever mosquito, Aedes aegypti. Genet Res. 1979;34:215–29. doi: 10.1017/s0016672300019467. [DOI] [PubMed] [Google Scholar]
- Takken W, Verhulst N, Scholte EJ, Jacobs F, Jongema Y, van Lammeren R. The phenology and population dynamics of Culicoides spp. in different ecosystems in The Netherlands. Prev Vet Med. 2008;87:41–54. doi: 10.1016/j.prevetmed.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Tesh RB, Watts DM, Russell KL, Damodaran C, Calampa C, Cabezas C, Ramirez G, Vasquez B, Hayes CG, Rossi CA, Powers AM, Hice CL, Chandler LJ, Cropp BC, Karabatsos N, Roehrig JT, Gubler DJ. Mayaro virus disease: an emerging mosquito-borne zoonosis in tropical South America. Clin Infect Dis. 1999;28:67–73. doi: 10.1086/515070. [DOI] [PubMed] [Google Scholar]
- Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;3:e201. doi: 10.1371/journal.ppat.0030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turell MJ, Beaman JR. Experimental transmission of Venezuelan equine encephalomyelitis virus by a strain of Aedes albopictus (Diptera: Culicidae) from New Orleans, Louisiana. J Med Entomol. 1992;29:802–5. doi: 10.1093/jmedent/29.5.802. [DOI] [PubMed] [Google Scholar]
- Turell MJ, Dohm DJ, Mores CN, Terracina L, Wallette DL, Jr, Hribar LJ, Pecor JE, Blow JA. Potential for North American mosquitoes to transmit Rift Valley fever virus. J Am Mosq Control Assoc. 2008;24:502–7. doi: 10.2987/08-5791.1. [DOI] [PubMed] [Google Scholar]
- Turell MJ, O’Guinn M, Oliver J. Potential for New York mosquitoes to transmit West Nile virus. Am J Trop Med Hyg. 2000;62:413–4. doi: 10.4269/ajtmh.2000.62.413. [DOI] [PubMed] [Google Scholar]
- Turell MJ, O’Guinn ML, Dohm DJ, Jones JW. Vector competence of North American mosquitoes (Diptera: Culicidae) for West Nile virus. J Med Entomol. 2001;38:130–4. doi: 10.1603/0022-2585-38.2.130. [DOI] [PubMed] [Google Scholar]
- van den Hurk AF, Ritchie SA, Mackenzie JS. Ecology and geographical expansion of Japanese encephalitis virus. Annu Rev Entomol. 2009;54:17–35. doi: 10.1146/annurev.ento.54.110807.090510. [DOI] [PubMed] [Google Scholar]
- van Regenmortel MHV, Fauquet CM, Bishop DHL, Carstens EB, Estes MK, Lemon SM, Maniloff J, Mayo MA, McGeogh DJ, Pringle CR, Wickner RB. Seventh Report of the International Committee on Taxonomy of Viruses. Academic Press; San Diego: 2000. Virus Taxonomy. Classification and Nomenclature of Viruses. [Google Scholar]
- Vasilakis N, Shell EJ, Fokam EB, Mason PW, Hanley KA, Estes DM, Weaver SC. Potential of ancestral sylvatic dengue-2 viruses to re-emerge. Virology. 2007;358:402–12. doi: 10.1016/j.virol.2006.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilakis N, Tesh RB, Weaver SC. Sylvatic dengue virus type 2 activity in humans, Nigeria, 1966. Emerg Infect Dis. 2008;14:502–4. doi: 10.3201/eid1403.070843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilakis N, Weaver SC. The history and evolution of human dengue emergence. Adv Virus Res. 2008;72:1–76. doi: 10.1016/S0065-3527(08)00401-6. [DOI] [PubMed] [Google Scholar]
- Vazeille M, Moutailler S, Coudrier D, Rousseaux C, Khun H, Huerre M, Thiria J, Dehecq JS, Fontenille D, Schuffenecker I, Despres P, Failloux AB. Two Chikungunya isolates from the outbreak of La Reunion (Indian Ocean) exhibit different patterns of infection in the mosquito, Aedes albopictus. PLoS ONE. 2007;2:e1168. doi: 10.1371/journal.pone.0001168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinagradova EB. Culex pipiens pipiens mosquitoes: taxonomy, distribution, physiology, genetics, applied importance and control. Pensoft; Moscow, Russia: 2000. [Google Scholar]
- Wang E, Ni H, Xu R, Barrett AD, Watowich SJ, Gubler DJ, Weaver SC. Evolutionary Relationships of Endemic/Epidemic and Sylvatic Dengue Viruses. J Virol. 2000;74:3227–3234. doi: 10.1128/jvi.74.7.3227-3234.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts DM, Callahan J, Rossi C, Oberste MS, Roehrig JT, Wooster MT, Smith JF, Cropp CB, Gentrau EM, Karabatsos N, Gubler D, Hayes CG. Venezuelan equine encephalitis febrile cases among humans in the Peruvian Amazon River region. Am J Trop Med Hyg. 1998;58:35–40. doi: 10.4269/ajtmh.1998.58.35. [DOI] [PubMed] [Google Scholar]
- Watts DM, Lavera V, Callahan J, Rossi C, Oberste MS, Roehrig JT, Cropp CB, Karabatsos N, Smith JF, Gubler DJ, Wooster MT, Nelson WM, Hayes CG. Venezuelan equine encephalitis and Oropouche virus infections among Peruvian army troops in the Amazon region of Peru. Am J Trop Med Hyg. 1997;56:661–7. doi: 10.4269/ajtmh.1997.56.661. [DOI] [PubMed] [Google Scholar]
- Weaver SC. Vector Biology in Viral Pathogenesis. In: Nathanson N, editor. Viral Pathogenesis. Lippincott-Raven; New York: 1997. pp. 329–352. [Google Scholar]
- Weaver SC, Bellew LA, Gousset L, Repik PM, Scott TW, Holland JJ. Diversity within natural populations of eastern equine encephalomyelitis virus. Virology. 1993;195:700–9. doi: 10.1006/viro.1993.1421. [DOI] [PubMed] [Google Scholar]
- Weaver SC, Ferro C, Barrera R, Boshell J, Navarro JC. Venezuelan equine encephalitis. Annu Rev Entomol. 2004;49:141–74. doi: 10.1146/annurev.ento.49.061802.123422. [DOI] [PubMed] [Google Scholar]
- Weaver SC, Salas R, Rico-Hesse R, Ludwig GV, Oberste MS, Boshell J, Tesh RB. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. VEE Study Group. Lancet. 1996;348:436–40. doi: 10.1016/s0140-6736(96)02275-1. [DOI] [PubMed] [Google Scholar]
- White DM, Wilson WC, Blair CD, Beaty BJ. Studies on overwintering of bluetongue viruses in insects. J Gen Virol. 2005;86:453–62. doi: 10.1099/vir.0.80290-0. [DOI] [PubMed] [Google Scholar]
- Worwa G, Hilbe M, Ehrensperger F, Chaignat V, Hofmann MA, Griot C, Maclachlan NJ, Thuer B. Experimental transplacental infection of sheep with bluetongue virus serotype 8. Vet Rec. 2009;164:499–500. doi: 10.1136/vr.164.16.499. [DOI] [PubMed] [Google Scholar]
- Zimmerman EA. House sparrow history 2002 [Google Scholar]
- Zimmerman MD, Scott RM, Vaughn DW, Rajbhandari S, Nisalak A, Shrestha MP. Short report: an outbreak of Japanese encephalitis in Kathmandu, Nepal. Am J Trop Med Hyg. 1997;57:283–4. doi: 10.4269/ajtmh.1997.57.283. [DOI] [PubMed] [Google Scholar]