Abstract
OBJECTIVES:
The aim of this study was to examine the frequency of Cushing’s syndrome (CS) in obese patients devoid of specific clinical symptoms of Cushing’s syndrome.
METHODS:
A total of 150 obese patients (129 female, 21 male; mean age 44.41 ± 13.34 yr; mean BMI 35.76 ± 7.13) were included in the study. As a first screening step, we measured 24-h urinary free cortisol (UFC). An overnight 1-mg dexamethasone suppression test was also performed on all patients. Urinary free cortisol levels above 100 μg/24 h were considered to be abnormal. Suppression of serum cortisol <1.8 μg/dL after administration of 1 mg dexamethasone was the cut-off point for normal suppression. The suppression of the serum cortisol levels failed in all of the patients.
RESULTS:
Measured laboratory values were as follows: ACTH, median level 28 pg/ml, interquartile range (IQR) 14–59 pg/ml; fasting glucose, 100 (91–113) mg/dL; insulin, 15.7 (7.57–24.45) mU/ml; fT4, 1.17 (1.05–1.4) ng/dL; TSH, 1.70 (0.91–2.90) mIU/L; total cholesterol, 209 (170.5–250) mg/dL; LDL-c, 136 (97.7–163) mg/dL; HDL-c, 44 (37.25–50.75) mg/dL; VLDL-c, 24 (17–36) mg/dL; triglycerides, 120.5 (86–165) mg/dL. The median UFC level of the patients was 30 μg/24 h (IQR 16–103). High levels of UFC (>100 μg/24 h) were recorded in 37 patients (24%). Cushing’s syndrome was diagnosed in 14 of the 150 patients (9.33%). Etiologic reasons for Cushing’s syndrome were pituitary microadenoma (9 patients), adrenocortical adenoma (3 patients), and adrenocortical carcinoma (1 patient).
CONCLUSION:
A significant proportion (9.33%) of patients with simple obesity were found to have Cushing’s syndrome. These findings argue that obese patients should be routinely screened for Cushing’s syndrome.
Keywords: Cushing’s syndrome, Obesity, Screening, Cortisol, Adrenocorticorticotropic hormone
INTRODUCTION
Obesity is the most common metabolic problem in industrialized countries. In the USA, 32% of adults are classified as overweight, and 22.5% of these individuals are obese.1 Both overweight and obese subjects are at an increased risk for cardiovascular diseases,2 some types of cancer,3 diabetes4, and even premature death.5 Obesity is often accompanied by other chronic disorders including hypertension, osteoarthritis, bile stones, and dyslipidemia.6–12 In addition to these physical disorders, obesity is commonly associated with psychological and psycho-social problems.10
Obesity can coexist with diverse physical disorders, and physicians should first focus on the differential diagnosis of possible underlying disorders before initiating any management procedure. Obesity is a prominent feature of endocrine diseases including hypothyroidism, insulin-excess syndromes, polycystic ovary syndrome (PCOS), hypogonadism, hypothalamic disease/injury, growth hormone deficiency, leptin deficiency or leptin receptor defects, pseudohypoparathyroidism, and Cushing’s syndrome (CS).11,12
Diagnosis of CS is primarily based on the signs and symptoms of the disorder. Nevertheless, a significant number of CS patients present only with simple obesity13–14 or with type 2 diabetes mellitus and poor glycemic control.15–17 Metabolic syndrome may also indicate the presence of CS. Patients without specific clinical features of CS have been referred to as sub-clinical Cushing’s syndrome (SCS)15 patients, and the diagnosis of SCS affords a considerable challenge to the physician.
We accordingly set out to determine the frequency of CS in patients presenting with simple obesity in the absence of other specific signs or symptoms indicative of CS.
PATIENTS AND METHODS
This study included 150 consecutive simple obese patients (129 female, 21 male, mean age: 44.41 ± 13.34 yr, body mass index (BMI) > 25 kg/m2) who were followed and treated at the Endocrinology Metabolism outpatient clinic at Cerrahpasa Medical Faculty between June 2003 and June 2004. Written informed consent was obtained from all patients before commencement of the study. Review of patient medical history was used to exclude subjects in which the dexamethasone suppression test could be biased either by medication (including exogenous glucocorticoid intake) or by other factors known to influence the test (including drug use, alcoholism, obvious depression, or pregnancy). None of the patients had nephropathy (creatinine clearance <30 ml/min), acute illness, or sleep disorders.
All patients in our study had simple obesity; none of them had diabetes mellitus. Since the patients had simple obesity, careful examinations did not reveal hirsutism, buffalo hump, easy bruising, or any other manifestations suggestive of CS suggestive manifestations.
Clinical characteristics recorded included BMI and anthropometric measurements. Morning blood samples following fasting (12 h) were drawn from an antecubital vein for determination of the concentrations of adrenocorticorticotropic hormone (ACTH) (N: 0–46 pg/ml), cortisol (N: 5–28 μg/dL), glucose, insulin (N: 0–20 μIU/L), serum lipids (total cholesterol, LDL, HDL, VLDL-cholesterol, and triglyceride), free thyroxin (fT4) (N: 0.93–1.77 ng/dL), and thyrotropin (TSH) (N: 0.15–3.7 IU/ml). Urine (24 h) was collected from each subject in order to perform urinary free cortisol (UFC) measurements. Patients whose 24-h UFC excretion exceeded 100μg/dL were defined as abnormal. All patients subsequently underwent a 1-mg overnight dexamethasone suppression test (DMS). Suppression of serum cortisol to <1.8 μg/dL after dexamethasone administration was the cut-off point for normal suppression without consideration of 24-h UFC. Measurement of serum ACTH levels and an 8-mg DMS were performed as second-step investigations in all patients who failed to achieve serum cortisol suppression <1.8 μg/dL after administration of 1 mg DMS. Complementary imaging studies, magnetic resonance imaging (MRI) of the sella, cavernous sinus sampling, and abdominal computed tomography (CT) were performed when the results of the second-step evaluations were consistent with ACTH-dependent or ACT-independent CS.
Insulin, cortisol, fT4, TSH, and ACTH were assessed by radioimmunoassay (RIA) using a Packard Riastar gamma counter (Perkin-Elmer, Waltham, MA, USA) and commercial assay kits. Other biochemical laboratory tests were measured with an Olympus AU 600 autoanalyser (Olympus, Tokyo, Japan). Insulin resistance was assessed using the homeostasis model assessment ratio (HOMA-R) formula (18).
Calculations were done with SPSS software (version 10; SPSS Inc, Chicago, IL, USA), and differences in the values of the variables between the groups were evaluated by the Mann-Whitney U test. The degree of the correlation between parameters was evaluated by regression analysis. A value of p<0.05 was considered to be statistically significant.
RESULTS
We analyzed a series of patients presenting with simple obesity for the presence of sub-clinical CS. The clinical characteristics and laboratory findings for these patients are summarized in Tables 1 and 2.
Table 1.
Summary of physical examination findings in the patient group
| (Mean ± SD) (n=150) | |
|---|---|
| BMI (kg/m2) | 35.76 ± 7.13 |
| Waist (cm) | 104.07 ± 15.77 |
| Waist-to-hip ratio | 0.98 ± 0.92 |
| Systolic blood pressure (mm/Hg) | 135.13 ± 20.49 |
| Diastolic blood pressure (mm/Hg) | 87.23 ± 13.03 |
Table 2.
Laboratory findings in the study patients
| Simple obesity | Cushing’s syndrome | p | |
|---|---|---|---|
| ACTH (pg/ml) | 25.7 [15–51] | 35 [13.5–94.5] | 0.43 |
| Cortisol (μg/dL) | 10.2 [7.8–14.8] | 9.4 [8.1–13.5] | 0.88 |
| Glucose (mg/dL) | 99 [91–113] | 100 [93.5–114] | 0.91 |
| Insulin (mU/ml) | 14.7 [7.4–24.2] | 18.9 [14.9–28.5] | 0.07 |
| f T4 (ng/dL) | 1.2 [1.07–1.4] | 1.1 [1.04–1.63] | 0.56 |
| TSH (mIU/L) | 1.64 [0.9–2.8] | 1.78 [1.6–4.2] | 0.25 |
| Cholesterol (mg/dL) | 203 [172–249] | 238.5 [178–264] | 0.24 |
| LDL-c (mg/dL) | 129 [97–159] | 168 [122–168] | 0.15 |
| HDL-c (mg/dL) | 44 [37.5–50.5] | 46 [29–66] | 0.72 |
| VLDL-c (mg/dL) | 24 [17–33] | 38 [16.2–50] | 0.2 |
| Triglyceride (mg/dL) | 120 [86–161] | 208 [89.8–251] | 0.15 |
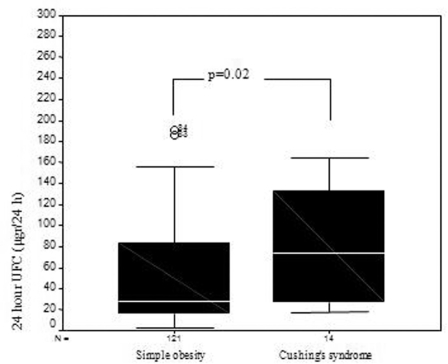
| Urine cortisol (μg/24 h) | 28 [15–92.5] | 74 [27–133] | 0.02 |
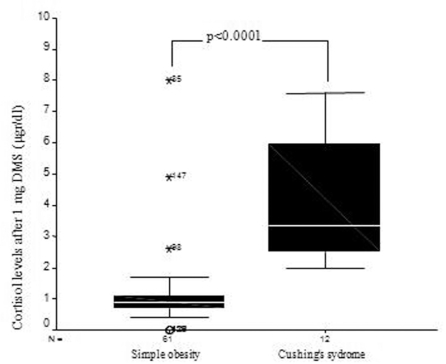
| DMST cortisol (μg/dL) | 0.88 [0.7–1.15] | 3.35 [2.5–6.5] | < 0.0001 |
| HOMA-R (mg/dl × mU/ml) | 4.02 [1.91–6.59] | 4.66 [4.38–9.08] | 0.06 |
Values are medians and interquartile ranges.
DMST: 1-mg dexamethasone suppression test
In 37 patients (24%), 24-h UFC excretion exceeded the cut-off point (median, 30; interquartile range (IQR), 16–103 μg/24 h). Fourteen patients had unsuppressed cortisol levels as indicated by the 1-mg dexamethasone suppression test. Complementary imaging studies were performed on these 14 CS patients, which revealed pituitary microadenoma in 9 patients, adrenal adenoma in 3 patients, and adrenal carcinoma in 1 patient. Histological diagnosis was obtained in 13 patients; one patient declined to undergo surgical intervention for definitive diagnosis (Table 3).
Table 3.
Etiologies of the 14 patients diagnosed with Cushing’s syndrome
| N | % | |
|---|---|---|
| Pituitary adenoma | 9 | 64.28 |
| Surrenal cortex adenoma | 3 | 21.42 |
| Surrenal cortex carcinoma | 1 | 7.15 |
| Declined further evaluation | 1 | 7.15 |
We compared the group of 14 obese patients with CS to the remaining group of 136 patients with simple obesity. There was no significant difference in levels of ACTH (p=0.43) or basal cortisol (p=0.88) between the CS group and the group of simple obese patients without CS. However, 24-h UFC excretion (Figure 1) and morning cortisol levels following administration of 1 mg DMS (Figure 2) were significantly more elevated in obese patients with CS than in simple obese patients without CS.
Figure 1.
Twenty-four-hour free cortisol levels in patients with Cushing’s syndrome and simple obesity
Figure 2.
The comparison of the 1-mg dexamethasone suppression test results for both groups
There were no significant differences between the groups in mean values for serum lipids, glucose, BMI, systolic blood pressure, or waist-to-hip ratio. Diastolic pressure was higher in patients with CS (p=0.02). Although higher HOMA-R values were recorded in patients with CS (median, 4.66 mg/dL × mU/ml; IQR, 1.38–9.08) compared to simple obese patients (median, 4.02 mg/dL × mU/ml; IQR, 1.91–6.59), the difference between the two groups narrowly failed to achieve statistical significance (p=0.06).
DISCUSSION
Here, we report on 150 obese patients screened for CS. A diagnosis of CS was established in 14 patients (9.33%). This finding confirms the need to evaluate patients with simple obesity for CS despite the absence of other signs or symptoms of the disorder.
This conclusion is supported by several previous studies. Obesity is a frequent clinical sign of CS, and adipose tissues in CS patients typically have a central distribution. Obese patients with CS may live without any evident metabolic disorder associated with CS. However, CS screening in simple obesity is usually not performed unless the patient has other clinical features of CS, such as poorly controlled hypertension, diabetes, osteoporosis with rapid progression, or hypokalemia that is unresponsive to the therapy. Delayed identification of SCS in obese patients results in the progression of CS, with the risk of irreversible complications. We therefore initiated a screening program for CS in our simple obese outpatients. The use of sensitive assays resulted in a significant improvement in the identification of CS. We documented 14 cases of CS in a sample of 150 simple obese patients. The high proportion of patients with Cushing’s syndrome that we identified despite the rareness of CS could be because we screened for CS in an obese population. These findings argue that every patient with simple obesity should be investigated for CS.
Some patients with type 2 diabetes and poor glycemic control may also have subclinical CS (SCS), and these patients should be screened for CS. Recent studies have provided a rationale for the systemic screening of CS in patients with type 2 diabetes.16,17 Hypercortisolism can result in insulin resistance; glucose intolerance (or type 2 diabetes) secondary to insulin resistance occurs in approximately 75% of patients with CS. In this subgroup, 50% of the subjects had overt type 2 diabetes (20–25% of all CS patients). It has been well documented since the 1960s that patients with CS typically suffer from hyperinsulinemia, insulin resistance, and type 2 diabetes.19,20
Catargi et al. screened 200 overweight inpatients with type 2 diabetes and poor glycemic control (HbA1c >8%).15 None displayed the specific clinical features of CS in addition to their poorly-controlled type 2 diabetes. A total of 52 (26%) patients had impaired 1-mg DMS (failure to suppress cortisol <2.1 μg/dL). Of these, 17 (8.5%) displayed at least one additional biological abnormality of the hypothalamic-pituitary-adrenal axis. Imaging studies showed abnormalities in 11 of these 17 patients (5.5% of the whole series). Definitive occult CS was identified in 4 patients (2%), with 3 (1.5%) having Cushing’s disease and 1 (0.5%) with surgically proven adrenal adenoma. However, definitive diagnosis of CS in the remaining seven patients (3.5%) required further investigation. A unilateral adrenal tumor of 10–29 mm was subsequently revealed by abdominal CT and iodocholesterol scintigraphy. These seven patients, therefore, had probable adrenal-dependent CS but did not undergo surgery. Six months after treatment for CS, a mean 5.5% reduction in body weight and a mean 2.5% reduction in HbA1c were reported in four patients. Oral antidiabetic medications were resumed in one patient, and the daily insulin dose was dramatically reduced in another. This study highlights the need to perform prospective CS screening on overweight, poorly controlled type 2 diabetic patients. 15
Assessment of 24-h UFC is a convenient screening test for CS in outpatient clinics. The false-negative rate for UFC is extremely low, though false-positive rates tend to be high. CS can, therefore, be excluded if 24-h UFC is normal. In patients with elevated 24-h UFC levels, a diagnosis of CS should be confirmed by a 1-mg overnight dexamethasone suppression test. In our study group, only 14 of 30 patients having elevated UFC were confirmed as having CS by the 1-mg DMS test. The remaining 16 obese patients were considered to be false-positives. Wood et al. established that suppression of plasma cortisol to less than 1.8 μg/dL excluded CS without an increase in the false-positive rate. 21 A study by Baid SK et al. demonstrated that the results of screening tests specific to CS may be falsely abnormal in overweight and obese populations.22
In our study, definitive CS was identified in 13 of 14 patients with unsuppressed serum cortisol after the results of the 1-mg DMS test were considered. One patient declined further investigation. The remaining 13 patients underwent further biochemical and imaging studies. Definitive diagnoses of CS were proven by histological analysis of surgically-removed material. Among 30 patients with elevated 24-h UFC, levels were significantly more elevated in the group of patients with unsuppressed cortisol after administration of 1 mg DMS (p=0.002) than in simple obese patients with suppressed cortisol levels.
Distinguishing simple obese patients from CS presents a challenge for the physician. Future studies on larger patient populations will be required to address the true prevalence of CS. Appropriate study groups will include patients with relevant clinical features, including simple obesity, poorly controlled diabetes, osteoporosis, and PCOS.
REFERENCES
- 1.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalance of overweight among US adults: The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–11. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 2.Manson JE, Colditz GA, Stampfer MJ, Willet WJ, Rosner B, Manson RR, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 1990;322:882–9. doi: 10.1056/NEJM199003293221303. [DOI] [PubMed] [Google Scholar]
- 3.Huang Z, Hankinson SE, Colditz GA, Stampfer MJ, Hunter DJ, Manson JE, et al. Dual effects of weight and weight gain on breast cancer risk. JAMA. 1997;278:1407–11. [PubMed] [Google Scholar]
- 4.Colditz GA, Willet WC, Stampfer MJ, Manson JE, Hennekenz CE, Arky RA, et al. Weight as a risk factor for clinical diabetes in women. Am J Epidemiol. 1990;132:501–13. doi: 10.1093/oxfordjournals.aje.a115686. [DOI] [PubMed] [Google Scholar]
- 5.Manson JE, Willet WC, Stampfer MJ, Golditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–85. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 6.Witteman JCM, Willet WC, Stampfer MJ, Colditz GA, Kok FJ, Sacks FM, et al. Moderate alcohol consumption and increased risk of systemic hypertension. Am J Cardiol. 1990;65:633–7. doi: 10.1016/0002-9149(90)91043-6. [DOI] [PubMed] [Google Scholar]
- 7.Carman WC, Sowers M, Havthorne VM, Weissfeld LA. Obesity is a risk factor for osteoarthritis of the hand and the wrist: a prospective study. Am J Epidemiol. 1994;139:119–29. doi: 10.1093/oxfordjournals.aje.a116974. [DOI] [PubMed] [Google Scholar]
- 8.Maclure KM, Hayes KC, Colditz GA, Stampfer MJ, Speizer FE, Willet WC. Weight, diet and risk of symptomatic gallstones in middle-aged women. N Engl J Med. 1989;321:563–69. doi: 10.1056/NEJM198908313210902. [DOI] [PubMed] [Google Scholar]
- 9.Beirman EL, Hirsch J. Obesity. In: Williams RH, editor. Textbook of Endocrinology. 9th edition. Philadelphia: W.B. Saunders; 1998. pp. 906–21. [Google Scholar]
- 10.Fine JT, Colditz GA, Coakley EH, Moseley G, Manson JE, Willet WC, et al. A prospective study of eight change and health-related quality of life in women. JAMA. 1999;282:2136–42. doi: 10.1001/jama.282.22.2136. [DOI] [PubMed] [Google Scholar]
- 11.Maddox GL, Leiderman V. Overweight as a social disability with medical implications. J Med Educ. 1969;44:214–20. doi: 10.1097/00001888-196903000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Price JH, Desmond SM, Krol RA, Synder FF, O’Connel JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45. [PubMed] [Google Scholar]
- 13.Garrapa GG, Pantanetti P, Arnaldi G, Mantero F, Faloia E. Body composition and metabolic features in women with adrenal incidentaloma or Cushing’s syndrome. J Clin Endocrinol Metab. 2001;86:5301–6. doi: 10.1210/jcem.86.11.8059. [DOI] [PubMed] [Google Scholar]
- 14.Douyon L, Schteingart DE. Effect of obesity and starvation on thyroid hormone, growth hormone, and cortisol secretion. Endocrinol Metab Clin North Am. 2002;31:173–89. doi: 10.1016/s0889-8529(01)00023-8. [DOI] [PubMed] [Google Scholar]
- 15.Catargi B, Rigalleau V, Poussin A, Ronci-Chaix N, Bex V, Vergot N, et al. Occult Cushing’s syndrome in type-2 ciabetes. J Clin Endocrinol Metab. 2003;12:5808–13. doi: 10.1210/jc.2003-030254. [DOI] [PubMed] [Google Scholar]
- 16.Caetano MS, Silva Rdo C, Kater CE. Increased diagnostic probability of subclinical Cushing’s syndrome in a population sample of overweight adult patients with type 2 diabetes mellitus. Arq Bras Endocrinol Metabol. 2007;51:1118–27. doi: 10.1590/s0004-27302007000700015. [DOI] [PubMed] [Google Scholar]
- 17.Reimondo G, Pia A, Allasino B, Tassone F, Bovio S, Borretta G, et al. Screening of Cushing’s syndrome in adult patients with newly diagnosed diabetes mellitus. Clin Endocrinol. 2007;67:225–9. doi: 10.1111/j.1365-2265.2007.02865.x. [DOI] [PubMed] [Google Scholar]
- 18.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 19.Christy NP. Harvey Cushing as clinical investigator and laboratory worker. Am J Med Sci. 1981;281:79–96. doi: 10.1097/00000441-198103000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Yanovski JA, Cutler GB., Jr Glucocorticoid action and the clinical features of Cushing’s syndrome. Endocrinol Metab Clin North Am. 1994;23:487–509. [PubMed] [Google Scholar]
- 21.Wood PJ, Barth JH, Feedman DB. Evidence for the low dose dexamethasone suppression test to screen for Cushing’s syndrome – recommendations for a protocol for biochemistry laboratories. Ann Clin Biochem. 1997;34:222–9. doi: 10.1177/000456329703400302. [DOI] [PubMed] [Google Scholar]
- 22.Baid SK, Rubino D, Sinaii N, Ramsey S, Frank A, Nieman LK. Specificity of screening tests for Cushing’s syndrome in an overweight and obese population. J Clin Endocrinol Metab. 2009;94:3857–64. doi: 10.1210/jc.2008-2766. [DOI] [PMC free article] [PubMed] [Google Scholar]