Abstract
OBJECTIVES
1. To measure the proportion of patients with chronic rhinosinusitis (CRS) who experience clinically significant improvement after endoscopic sinus surgery (ESS) in a prospective, multi-institutional fashion. 2. To identify preoperative characteristics which predict clinically significant improvement in quality of life (QOL) after ESS.
STUDY DESIGN
Prospective, multi-institutional cohort study
SETTING
Academic tertiary care centers
SUBJECTS & METHODS
302 patients with CRS from three centers were enrolled between July 2004 and December 2008 and followed for an average of 17.4 months postoperatively. Preoperative patient characteristics, computed tomography (CT) scan, endoscopy score and pre- and postoperative quality of life (QOL) were collected. Univariate and multivariate analyses were performed.
RESULTS
Patients improved an average of 15.8% (18.9 points) on the Rhinosinusitis Disability Index and 21.2% (21.2 points) on the Chronic Sinusitis Survey (both p<0.001). Patients significantly improved on all eight Medical Short Form-36 subscales (all p<0.001). Among patients with poor baseline QOL, 71.7% of patients experienced clinically significant improvement on the RSDI and 76.1% on the CSS. Patients undergoing primary surgery were 2.1 times more likely to improve on the RSDI (95% CI: 1.2, 3.4; p=0.006) and 1.8 times more likely to improve on the CSS (95% CI: 1.1, 3.1; p=0.020) as compared to patients undergoing revision surgery.
CONCLUSION
In this prospective, multi-institutional study, most patients experienced clinically significantly improvement across multiple QOL outcomes after ESS. Specific patient characteristics provided prognostic value with regard to outcomes.
Keywords: sinusitis, quality of life, outcomes, endoscopic sinus surgery, health-services research
INTRODUCTION
According to The National Health Interview Survey, chronic rhinosinusitis (CRS) affects 14–16% of the U.S. population and has significant socioeconomic implications with annual direct costs of $4.3 billion.1,2 In addition, the Medical Short Form-36 (SF-36) general quality of life (QOL) instrument has shown that patients with CRS exhibit statistically significant deviations from the general population in several domains.3 Using this instrument, patients with sinusitis scored lower in measures of bodily pain and social functioning than patients with congestive heart failure, angina, chronic obstructive pulmonary disease, or back pain.4 Due to the chronicity of the disease, and the relatively poor response of some patients to initial medical therapies, patients with CRS undergo 500,000 surgical procedures annually, with the primary goal of improving QOL. A major goal of our research has been to study patient factors such as standard diagnostic tests or comorbidities that best predict surgical outcomes to aid in preoperative patient counseling and surgical case selection.
Several studies have reported improvement in the large majority of patients undergoing endoscopic sinus surgery (ESS) but have been limited by retrospective data collection or unvalidated outcomes.5,6 Some prospective studies have reported improvement in mean QOL and symptom scores following ESS but they did not define the proportion of patients that improved, they were largely single institution results, or they had limited sample sizes for analysis.3,7–11 The goal of this study was to report outcomes of ESS using prospective, multi-institutional data from a large cohort and validated disease-specific and general health-related QOL instruments. In addition, preoperative patient factors were evaluated for their ability to predict clinically significant outcomes so that surgeons can appropriately counsel patients and optimize surgical case selection.
MATERIALS & METHODS
Study Participants and Data Collection
Adult (≥ 18 years) study subjects were enrolled from three performance sites, Oregon Health & Science University (OHSU), the Medical College of Wisconsin (MCW), and Stanford University as part of a multi-institutional prospective cohort study. All patients had a diagnosis of CRS based on the Rhinosinusitis Task Force criteria.12 Patients were enrolled at the time they elected to undergo endoscopic sinus surgery after failing broad-spectrum or culture directed antibiotics in addition to a trial of oral and topical steroid therapy. All study protocols and informed consent were collected and approved by the Institutional Review Boards at each study site.
Demographic data and social history were self-reported by the patient and included age, gender, race and/or ethnicity, annual household income, education level, cigarette use and alcohol consumption. For the analysis, annual household income was dichotomized in order to approximate the median US household income (< $50,000 or ≥ $50,000). Heavy alcohol consumption was defined as 14 drinks/week for men and 7 drinks/week for women.13 Presence or absence of clinical characteristics were documented by the physician and included asthma, nasal polyposis, allergies confirmed by testing, acetylsalicylic acid (ASA) intolerance, depression, and history of prior sinus surgery. Preoperative computed tomography (CT) scan and preoperative endoscopy exam were scored by the physician using the Lund-MacKay and Lund-Kennedy scoring systems. Two validated disease-specific instruments, the Rhinosinusitis Disability Index (RSDI, quality of life) and the Chronic Sinusitis Survey (CSS, symptom and medication use), and one validated general health-related QOL instrument, the Medical Outcomes Study Short Form-36 (SF-36) were administered by an experienced research coordinator pre- and post-operatively.7,14 In this observational study, the extent of surgery was tailored to the patient’s disease process as defined by signs, symptoms, CT scan and clinical judgment. Sinus mucosal tissue was collected from the ethmoid cavity at the time of surgery.
Statistical Analyses
The objectives of this study were: (1) to measure the proportion of patients who experienced clinically significant improvement after ESS in a prospective, multi-institutional fashion, and (2) identify baseline characteristics that were predictive of clinically significant improvement in QOL after ESS.
Clinically significant improvement was defined for each outcome as a change of ≥ 1/2 standard deviation (SD) of the baseline QOL score.15 Using this construct, improvement was defined as a decrease of ≥10.35 points on the RSDI and an increase of≥ 9.75 points on the CSS. Improvement was defined for each SF-36 subscale in a similar fashion (Table 1). To address ceiling effects, patients in the top (best) quintile of QOL scores were removed as a reasonable proxy for patients with baseline scores considered too high to achieve clinically significant improvement; the remaining patients were defined as having poor baseline QOL.
TABLE 1.
Mean change in disease-specific and general health-related QOL after endoscopic sinus surgery
| Preoperative | Postoperative | Absolute Δ* | |
|---|---|---|---|
| Disease specific QOL: | (mean ± SD) | (mean ± SD) | (mean ± SD) |
| RSDI total | 46.9 ± 20.7 | 28.1 ± 22.4 | 18.9 ± 19.6 |
| Physical | 18.7 ± 7.6 | 11.5 ± 8.2 | 7.2 ± 7.5 |
| Functional | 15.3 ± 7.3 | 8.7 ± 7.7 | 6.6 ± 7.3 |
| Emotional | 13.0 ± 8.4 | 7.9 ± 7.9 | 5.1 ± 7.6 |
| CSS total | 37.8 ± 19.5 | 59.0 ± 21.4 | 21.2 ± 22.6 |
| Symptom | 29.1 ± 26.5 | 59.6 ± 29.3 | 30.6 ± 32.0 |
| Medication | 46.3 ± 25.2 | 58.2 ± 24.5 | 11.9 ± 26.2 |
| General health QOL: | |||
| SF-36 subscale | |||
| GH | 53.2 ± 23.9 | 58.6 ± 24.5 | 5.5 ± 19.8 |
| PF | 74.9 ± 24.5 | 81.6 ± 23.1 | 6.7 ± 18.5 |
| RP | 44.3 ± 42.3 | 65.6 ± 41.7 | 21.3 ± 43.2 |
| RE | 67.3 ± 40.0 | 79.9 ± 34.3 | 12.6 ± 39.6 |
| SF | 65.1 ± 26.1 | 72.9 ± 27.3 | 7.8 ± 28.7 |
| BP | 56.9 ± 24.2 | 63.9 ± 25.7 | 7.0 ± 22.6 |
| VT | 36.8 ± 23.3 | 51.9 ± 24.8 | 15.1 ± 22.7 |
| MH | 66.9 ± 20.3 | 74.7 ± 18.5 | 7.8 ± 16.3 |
denotes absolute change values of quality of life measures.
designates that all changes are statistically significant with p-values < 0.001. QOL = quality of life. RSDI = Rhinosinusitis Disability Index. CSS = Chronic Sinusitis Survey. SF-36 = Medical Outcomes Short Form-36. GH = general health subscale. PF = physical functioning subscale. RP = role-physical subscale. RE = role-emotional subscale. SF = social functioning subscale. BP = bodily pain subscale. VT = vitality subscale. MH = mental health subscale.
Multivariate logistic regression models were created to identify preoperative characteristics that predicted clinically significant improvement after surgery. Baseline variables were first screened to determine potential predictors of QOL improvement. Variables that were predictive on univariate analysis at the p ≤ 0.25 level were considered candidate variables for logistic regression modeling. Final models were chosen using forward selection and backwards elimination stepwise procedures based on p = 0.05 (entry) and p = 0.10 (removal) levels of significance after controlling for age and gender.
Post Hoc Analysis of Sinus Mucosa Specimens
A post hoc analysis was performed on a subset of patients with ethmoid sinus mucosal biopsies performed at the time of surgery at a single-institution (OHSU; n=92). Three histological parameters (eosinophil density, basement membrane thickening, subepithelial edema) and their ability to predict QOL outcomes were examined based on preliminary data and previously published methodology.16
RESULTS
Baseline Characteristics of the Cohort
Four hundred and thirty-eight patients were enrolled at three sites between July 2004 and December 2008. One hundred and thirty-six patients were lost to follow up because of changes in insurance status, unwillingness to participate, administrative changes, and long-distance travel. Only participants with a minimum of 6 months postoperative follow up were included in this analysis. A total of 302 participants (68.9%) from three sites (OHSU, n=133; MCW, n=101; and Stanford University, n=68) were followed for a mean of 17.4 months (SD 6.9) post-operatively. Baseline characteristics of patients in the cohort are described in Table 2 and were compared to those lost to follow up. Asthma was more prevalent in patients with follow up (43.4% vs 30.4%; p=0.010); there were no other differences detected between those with follow up and those lost to follow up. The frequencies of surgical procedures performed are reported in Table 3.
TABLE 2.
Characteristics of cohort of patients with CRS (n=302)
| mean ± SD | n (%) | |
|---|---|---|
| Age (years) | 48.6 ± 13.8 | |
| Education (years) | 14.9 ± 2.7 | |
| Gender: | ||
| Male | 155 (51.3) | |
| Female | 147 (48.7) | |
| Race/ethnicity: | ||
| White | 267 (88.4) | |
| Asian | 13 (4.3) | |
| Black or African American | 9 (3.0) | |
| Hispanic/Latino | 6 (2.0) | |
| American Indian/Alaskan Native | 4 (1.3) | |
| Native Hawaiian/Pacific Islander | 2 (0.7) | |
| Other | 1 (0.3) | |
| Annual household income: | ||
| $0–25,000 | 39 (12.9) | |
| $26–50,000 | 63 (20.9) | |
| $51–75,000 | 55 (18.2) | |
| $76–100,000 | 54 (17.9) | |
| $100,000+ | 90 (29.8) | |
| Clinical characteristics: | ||
| Asthma | 131 (43.4) | |
| Nasal polyposis | 125 (41.4) | |
| Allergy | 93 (30.8) | |
| Aspirin intolerance | 39 (12.9) | |
| Depression | 48 (15.9) | |
| Prior sinus surgery | 185 (61.3) | |
| Social history: | ||
| Tobacco use (packs/day) | 0.3 ± 0.1 | 16 (5.3) |
| Alcohol consumption (grams/week) | 22.8 ± 52.8 | 126 (41.7) |
| Preoperative diagnostic testing: | ||
| Lund-Kennedy endoscopy score | 6.9 ± 4.8 | |
| Lund-MacKay CT score | 13.0 ± 6.4 | |
CRS = chronic rhinosinusitis. SD = standard deviation. CT = computed tomography.
TABLE 3.
Frequency of surgical procedures performed (n=302)
| Left side n(%) | Right side n(%) | |
|---|---|---|
| Maxillary antrostomy | 240 (79.5) | 252 (83.4) |
| Ethmoidectomy: | ||
| Partial | 43 (14.2) | 49 (16.2) |
| Total | 220 (72.8) | 222 (73.5) |
| Sphenoidotomy | 162 (53.6) | 171 (56.6) |
| Frontal sinusotomy | 172 (56.9) | 150 (49.7) |
| Septoplasty | 92 (30.5) | |
| Image guidance | 193 (63.9) | |
Disease-Specific and General Health-Related QOL Improvement after ESS
Mean scores significantly improved on the RSDI (18.9 points or 15.8%; p<0.001) and on the CSS (21.2 points or 21.2%; p<0.001; Table 1) following surgery. SF-36 scores significantly improved across all 8 subscales (all p<0.001; Table 1).
Among patients with poor baseline QOL, 71.7% of patients experienced clinically significant improvement on the RSDI and 76.1% of patients experienced clinically significant improvement on the CSS (Figure 1). Among patients with poor baseline QOL, 32.9% to 66.4% of patients improved on each of the SF-36 subscales (Figure 2).
Figure 1.
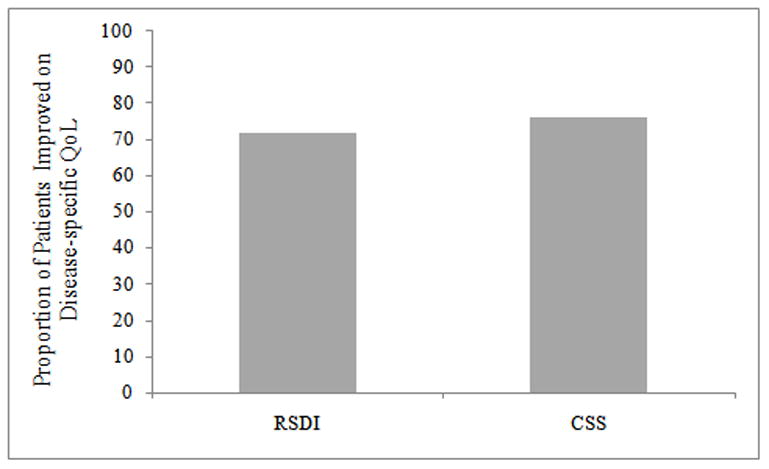
Proportion of patients with poor baseline quality of life (QOL) who experience clinically significant improvement in disease-specific quality of life after endoscopic sinus surgery. RSDI = Rhinosinusitis Disability Index. CSS = Chronic Sinusitis Survey.
Figure 2.
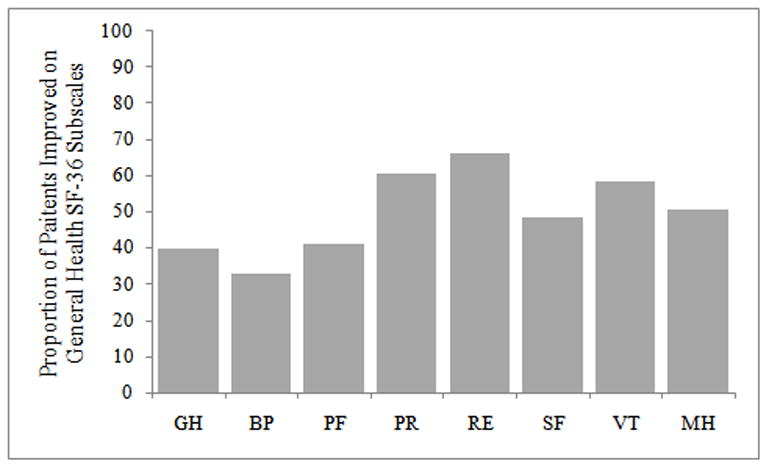
Proportion of patients with poor baseline quality of life who experience clinically significant improvement in general health-related quality of life after endoscopic sinus surgery. SF-36 = Medical Outcomes Short Form-36. GH = general health subscale. PF = physical functioning subscale. RP = role-physical subscale. RE = role-emotional subscale. SF = social functioning subscale. BP = bodily pain subscale. VT = vitality subscale. MH = mental health subscale.
Patient Characteristic Screening for Prediction of QOL Improvement
RSDI
On univariate screening, gender, education level, and the proportion of patients with asthma, ASA intolerance, and a history of prior sinus surgery were significantly different between those who improved and those who did not improve on the RSDI at the p ≤ 0.25 level (Table 4).
TABLE 4.
Univariate screening for predictive variables on the RSDI
| Total Cohort (n=302) | Poor Baseline QoL (n=240) | |||||
|---|---|---|---|---|---|---|
| Variables: | Improved | Did not improve | p-value | Improved | Did not improve | p-value |
| Age (mean ± SD) | 48.3 ± 13.6 | 49.2 ± 14.3 | 0.561 | 47.9 ± 13.6 | 48.2 ± 12.7 | 0.890 |
| Education ( mean yrs.) | 15.2 ± 2.6 | 14.6 ± 2.9 | 0.113* | 15.2 ± 2.5 | 14.5 ± 3.0 | 0.094* |
| Gender (%) | ||||||
| Male | 60.6 | 39.4 | 68.5 | 31.5 | ||
| Female | 68.0 | 32.0 | 0.181* | 75.0 | 25.0 | 0.268 |
| Race | ||||||
| White | 65.2 | 34.8 | 72.0 | 28.0 | ||
| Non-white | 57.1 | 42.9 | 0.352 | 69.0 | 31.0 | 0.731 |
| Annual household income | ||||||
| < $50,000/year | 62.7 | 37.3 | 67.1 | 32.9 | ||
| ≥ $50,000/year | 65.3 | 34.7 | 0.658 | 74.2 | 25.8 | 0.241* |
| Nasal polyposis | ||||||
| Present | 64.0 | 36.0 | 72.7 | 27.3 | ||
| Absent | 64.4 | 35.6 | 0.942 | 70.9 | 29.1 | 0.760 |
| Asthma | ||||||
| Present | 59.5 | 40.5 | 66.7 | 33.3 | ||
| Absent | 67.8 | 32.2 | 0.136* | 75.4 | 24.6 | 0.139* |
| ASA Intolerance | ||||||
| Present | 51.3 | 48.7 | 62.1 | 37.9 | ||
| Absent | 66.2 | 33.8 | 0.070* | 73.0 | 27.0 | 0.221 |
| Allergies by testing | ||||||
| Present | 61.3 | 38.7 | 73.5 | 26.5 | ||
| Absent | 65.5 | 34.5 | 0.476 | 70.9 | 29.1 | 0.687 |
| Depression | ||||||
| Present | 70.8 | 29.2 | 78.6 | 21.4 | ||
| Absent | 63.0 | 37.0 | 0.299 | 70.2 | 29.8 | 0.274 |
| History of sinus surgery | ||||||
| Primary | 74.4 | 25.6 | 83.5 | 16.5 | ||
| Revision | 57.8 | 42.2 | 0.004* | 64.4 | 35.6 | 0.001* |
| Current smoker | ||||||
| Smokers | 75.0 | 25.0 | 71.4 | 28.6 | ||
| Non-smokers | 63.6 | 36.4 | 0.356 | 71.7 | 28.3 | 0.984 |
| Alcohol consumption | ||||||
| Not heavy | 64.0 | 36.0 | 72.2 | 27.8 | ||
| Heavy | 68.4 | 31.6 | 0.694 | 61.5 | 38.5 | 0.405 |
| Preoperative diagnostic testing: (mean ± SD) | ||||||
| Lund-Kennedy endoscopy | 6.8 ± 4.8 | 7.2 ± 4.8 | 0.547 | 6.8 ± 4.7 | 7.2 ± 4.4 | 0.462 |
| Lund-MacKay CT | 13.2 ± 6.3 | 12.7 ± 6.7 | 0.558 | 13.4 ± 6.2 | 12.5 ± 6.3 | 0.325 |
RSDI = Rhinosinusitis Disability Index. QOL = quality of life. SD = standard deviation. CT = computed tomography.
denotes statistically significant candidate variables for final outcome models at the p ≤ 0.25 level for both total cohort and candidates with poor baseline QOL.
CSS
On univariate screening, age, education level, annual household income, history of prior sinus surgery, and mean preoperative endoscopy score were significantly different between those who improved and those who did not improve on the CSS at the p≤0.25 level (Table 5).
TABLE 5.
Univariate screening for predictive variables on the CSS
| Total Cohort (n=302) | Poor Baseline QoL (n=236) | |||||
|---|---|---|---|---|---|---|
| Variables: | Improved | Did not improve | p-value | Improved | Did not improve | p-value |
| Age (mean ± SD) | 47.9 ± 13.7 | 50.2 ± 13.8 | 0.163* | 48.0 ± 13.5 | 47.6 ± 12.0 | 0.858 |
| Education ( mean yrs.) | 15.1 ± 2.7 | 14.7 ± 2.6 | 0.208* | 15.2 ± 2.7 | 14.4 ± 2.6 | 0.054* |
| Gender (%) | ||||||
| Male | 65.8 | 34.2 | 72.0 | 28.0 | ||
| Female | 65.5 | 34.5 | 0.958 | 80.2 | 19.8 | 0.145* |
| Race | ||||||
| White | 66.4 | 33.6 | 76.8 | 23.2 | ||
| Non-white | 60.0 | 40.0 | 0.453 | 70.4 | 29.6 | 0.461 |
| Annual household income | ||||||
| < $50,000/year | 61.0 | 39.0 | 70.7 | 29.3 | ||
| ≥ $50,000/year | 67.8 | 32.2 | 0.240* | 78.5 | 21.5 | 0.192* |
| Nasal polyposis | ||||||
| Present | 63.2 | 36.8 | 73.5 | 26.5 | ||
| Absent | 67.4 | 32.6 | 0.447 | 77.9 | 22.1 | 0.429 |
| Asthma | ||||||
| Present | 64.9 | 35.1 | 73.1 | 26.9 | ||
| Absent | 66.3 | 33.7 | 0.802 | 78.6 | 21.4 | 0.332 |
| ASA Intolerance | ||||||
| Present | 66.7 | 33.3 | 77.4 | 22.6 | ||
| Absent | 65.5 | 34.5 | 0.888 | 75.9 | 24.1 | 0.850 |
| Allergies by testing | ||||||
| Present | 63.0 | 37.0 | 73.3 | 26.7 | ||
| Absent | 66.8 | 33.2 | 0.525 | 77.4 | 22.6 | 0.501 |
| Depression | ||||||
| Present | 66.0 | 34.0 | 76.3 | 23.7 | ||
| Absent | 65.6 | 34.4 | 0.964 | 76.0 | 24.0 | 0.969 |
| History of sinus surgery | ||||||
| Primary | 74.1 | 25.9 | 85.7 | 14.3 | ||
| Revision | 60.3 | 39.7 | 0.014* | 69.9 | 30.1 | 0.006* |
| Current smoker | ||||||
| Smokers | 62.5 | 37.5 | 64.3 | 35.7 | ||
| Non-smokers | 65.8 | 34.2 | 0.784 | 76.8 | 23.2 | 0.287 |
| Alcohol consumption | ||||||
| Not heavy | 65.5 | 34.5 | 81.2 | 18.8 | ||
| Heavy | 68.4 | 31.6 | 0.794 | 75.7 | 24.3 | 0.615 |
| Preoperative diagnostic testing: (mean ± SD) | ||||||
| Lund-Kennedy endoscopy | 6.5 ± 4.8 | 7.8 ± 4.5 | 0.018* | 6.6 ± 4.9 | 8.6 ± 4.1 | 0.006* |
| Lund-MacKay CT | 12.9 ± 6.4 | 13.4 ± 6.5 | 0.449 | 13.1 ± 6.3 | 15.0 ± 5.8 | 0.054* |
CSS = Chronic Sinusitis Survey. QOL = quality of life. SD = standard deviation. CT = computed tomography.
denotes statistically significant candidate variables for final outcome models at the p ≤ 0.25 level for both total cohort and candidates with poor baseline QOL.
Sample Size for Construction of the Logistic Regression Models
As part of the initial study design, sample size and power calculations were performed. Logistic regression models of the form:
were used to predict the occurrence of clinically significant improvement where x represented the independent predictor variable and p was the probability of the event. Approximately 10 events were required for each independent variable to assure adequate support for logistic regression modeling. The total sample size, n, was based on the formula n = 10q/min(p(^),1−p(^)), where p(^) was an estimate of the probability (p) of the event, and (1−p) was the converse of the probability of the event. Prior to the study, it was estimated that at least 80% of patients would improve on the RSDI and CSS; 300 patients supported the modeling of six predictor variables after univariate screening.
Predictors of Disease-Specific Quality of Life Improvement after ESS
The first multivariate logistic regression model examined predictors of clinically significant improvement on the RSDI. After adjustment for age and gender, only a history of prior sinus surgery predicted outcomes: patients undergoing primary sinus surgery were 2.1 times as likely to improve as patients undergoing revision sinus surgery (95% CI: 1.2, 3.4; p=0.006; Table 6). For the variables initially identified on univariate screening, gender, education level, as well as asthma and ASA intolerance, were not significant predictors.
TABLE 6.
Predictors of disease-specific QOL improvement after ESS (n=302).
| Models: | Independent predictors: | OR | (95% CI) | p-value |
|---|---|---|---|---|
| RSDI | Age (years) | 1.0 | (0.9, 1.1) | 0.815 |
| Gender | 1.4 | (0.8, 2.2) | 0.196 | |
| Primary surgery | 2.1 | (1.2, 3.4) | 0.006 | |
| CSS | Age (years) | 1.0 | (0.9, 1.1) | 0.221 |
| Gender | 1.0 | (0.6, 1.6) | 0.936 | |
| Primary surgery | 1.8 | (1.1, 3.1) | 0.020 |
ESS = endoscopic sinus surgery. QOL = quality of life. OR = odds ratio. CI = confidence intervals. RSDI = Rhinosinusitis Disability Index. CSS = Chronic Sinusitis Survey. Gender was controlled using males as the reference group. Odds ratios for primary surgery are compared to patients undergoing revision sinus surgery.
The second multivariate logistic regression model examined predictors of clinically significant improvement on the CSS. After adjustment for age and gender, a history of prior sinus surgery predicted less improvement in QOL after ESS. Patients undergoing primary sinus surgery were 1.8 times as likely to improve as patients undergoing revision sinus surgery (95% CI: 1.1, 3.1; p=0.020; Table 6). For the variables initially identified on univariate screening, age, education level, annual household income, and endoscopy score were not significant predictors.
Preliminary Findings Regarding Histopathologic Predictors of QOL Outcomes
Since our evaluation of various preoperative patient characteristics revealed limited predictive information, we elected to perform a sub-analysis on a portion of our cohort from the OHSU enrollment site (with ethmoid mucosa available for review) to evaluate the predictive value of certain histopathologic features (n=92).9,16,17 On post-hoc analysis, three histopathologic features were examined as potential predictors of QOL outcomes (Table 7) based on prior findings.9,16 On univariate screening, 78.7% of patients with <10 eosinophils per high powered field (HPF) improved on the RSDI as compared to 64.4% of patients with ≥10 eosinophils/HPF (p=0.128). 71.7% of patients with <10 eosinophils/HPF improved on the CSS as compared to 55.6% of patients with ≥ 10 eosinophils/HPF (p=0.108). On the CSS, only 58.9% of patients with subepithelial edema improved, whereas 84.2% of patients without subepithelial edema improved (p=0.040).
Table 7.
Proportion of patients who experience clinically significant improvement in QOL after ESS related to eosinophil density, basement membrane thickening, and subepithelial edema (n=92).
| RSDI | p-value | CSS | p-value | |
|---|---|---|---|---|
| Eosinophilia | (%) | (%) | ||
| 0–10 count/HPF | (78.7) | (71.7) | ||
| ≥10 count/HPF | (64.4) | 0.128 | (55.6) | 0.108 |
| BM thickening | ||||
| < 5 microns | (77.5) | (64.1) | ||
| 5–10 microns | (65.8) | (57.9) | ||
| 10–15 microns | (76.9) | (76.9) | ||
| 15+ microns | (0.0) | 0.204 | (100.0) | 0.550 |
| Subepithelial edema | ||||
| Absent | (68.4) | (84.2) | ||
| Present | (73.6) | 0.507 | (58.9) | 0.040 |
QOL = quality of life. RSDI = Rhinosinusitis Disability Index. CSS = Chronic Sinusitis Survey. HPF = high power field (400×). BM = basement membrane.
After adjustment for surgery status (revision vs. primary), patients with <10 eosinophils/HPF were 2.16 times (95% CI: 0.85, 5.45; p=0.105) as likely to improve on the RSDI after surgery and 1.95 times (95% CI: 0.82, 4.64; p=0.133) as likely to improve on the CSS as patients with ≥ 10 eosinophils/HPF. Patients without subepithelial edema were 3.76 (95% CI: 1.00, 14.09; p=0.050) times as likely to improve on the CSS after surgery as patients with subepithelial edema.
DISCUSSION
In this large, multi-institutional, prospective cohort study, 72–76% of patients with CRS and poor baseline QOL experienced clinically significant improvement in disease-specific QOL outcomes after ESS. To help place this within the context of the general medical literature and diverse disease processes, general health-related QOL was also found to significantly improve after sinus surgery. Clinical factors including asthma, ASA intolerance, and prior sinus surgery as well as preoperative diagnostic testing were found to be important potential predictors of outcomes. However, few of these variables were significant predictors of improvement when multiple risk factors were accounted for in the predictive model. Ultimately, primary ESS patients were twice as likely to improve after surgery as patients undergoing revision ESS though a baseline measure of disease severity (endoscopy score) was worse in the revision ESS group. Furthermore, preliminary data suggested that mucosal eosinophilia and subepithelial edema, present at the time of surgery, may be important factors in predicting QOL outcomes.
Prior studies have reported higher proportions of patients improving following ESS as compared to the current study. In 1994, Terris and Davidson combined 10 primarily retrospective case series from single institutions published between 1989–1993.5 Based on this review of articles, the authors reported a 91% “improvement rate” following ESS in 1713 patients. The primary outcomes were retrospective chart review with abstraction of patient results or unvalidated patient survey responses. Resolution of symptoms or decreased episodes of sinusitis were used as indicators of improvement. There was no standard for categorizing preoperative status, extent of disease, or surgical outcomes. With the introduction of both validated disease-specific QOL and general health-related QOL outcomes instruments, several centers have reported prospective, single institution outcomes primarily utilizing mean pre- and postoperative QOL scores to demonstrate the improvements patients experienced with ESS.9,10 These studies generally reported improvement in mean QOL scores following ESS but were unable to interpret the clinical relevance of that change or further delineate subgroups of patients who did not experience improvement. Both issues are of critical importance with regard to patient counseling and surgical case selection. In addition, single institution studies have been criticized for the potential lack of generalizability to the population of patients undergoing sinus surgery, an issue at least partially addressed by incorporating a multi-institutional study design. In this study, we attempted to address all of these issues to provide a framework for the clinical relevance of QOL change following ESS, identify subgroups more likely to improve, and include multi-institutional data in our analyses.
Defining “clinically significant improvement” with validated QOL instruments is an important means for translating research into meaningful terms that patients can understand and clinicians can factor into shared decision-making. It is also necessary for building models to predict treatment outcomes. The challenge becomes how to discriminate clinically significant improvement. This investigation utilized improvement by at least 1/2 of the standard deviation of the baseline QOL score to indicate clinically significant change. Interestingly, this approximates a patient’s ability to detect relevant change in other areas utilizing QOL outcomes and has been described as a “universal” phenomenon in the QOL literature.15 For comparison with other published literature, we noted that 80.8% of patients experienced at least a 50% reduction in the duration of symptoms and/or medication use on the CSS; this was nearly identical to the 82% reported in a study by Gliklich.7 In addition, when considering potential changes in QOL score, one must consider that some patients’ preoperative QOL scores were high enough that they were unable to experience clinically significant improvement in QOL. Therefore inclusion of those patients in the analyses resulted in a potentially lower proportion of patients with clinically significant improvement following intervention. We addressed this potential ceiling effect by performing one analysis that included all patients and a secondary analysis that excluded patients in the top quintile of preoperative QOL scores. The results from the predictive models were similar. Ultimately, translating data into clinically meaningful terms will assist clinicians in providing realistic expectations to patients, but determining the best definition for reporting clinically significant change continues to be an area of investigation.
Several clinical factors including comorbidities such as asthma or ASA intolerance, prior sinus surgery, and diagnostic testing including endoscopy score were significant in the univariate screening of potential predictors of QOL outcomes. These clinical factors have been studied elsewhere in the literature and have been shown to impact outcomes.18,19 Demographic characteristics including gender, annual household income, and education level were also important in univariate screening and have been studied by us and others in the general QOL literature.20 Surprisingly, when we accounted for all of these patient factors (comorbidities, diagnostic tests, and demographic characteristics) in our predictive model, very few patient factors were found to be predictive of outcomes of ESS. Whether patients were undergoing primary or revision surgery was clearly predictive such that the chances of QOL improvement were twice as high for primary surgery as compared to revision surgery. Therefore, patient characteristics discernable on presentation for sinus surgery or “clinical phenotype” did not provide the predictive information we sought. This led us to investigate other factors that may have predictive importance.
Based on several studies, it appears that inflammation is an important factor in determining treatment outcomes.9,10,18,19 In following this concept of inflammatory status predicting outcomes, we began to examine our cohort for other indicators of inflammation that have been suggested to predict outcomes.9,16,17 Specifically, markers of inflammation present in the sinus mucosa may provide predictive information regarding outcomes based upon their ability to discriminate the severity of the inflammatory process. In a post hoc analysis, our preliminary focus on histological markers of inflammation in the sinonasal mucosa revealed the finding of heterogeneity within clinical phenotypes (e.g. CRS with polyps) with regard to the presence of inflammatory markers and outcomes of treatment.16 When evaluated using predictive models, mucosal eosinophil density and sub-epithelial edema appeared to provide predictive information such that patients with lower eosinophil density or less subepitheilial edema were 2 to 4 times more likely to improve with ESS. The observational nature of this study and the routine use of perioperative co-interventions, including systemic steroids that are thought to impact the expression of these markers, should be considered in the context of these results. Future investigations should continue to evaluate histological and molecular inflammatory markers in a more controlled fashion for their utility in defining disease and predicting treatment outcomes. If found to be an important determinant of outcome, inflammatory marker evaluation through preoperative mucosal sampling might play a role in future patient counseling regarding outcomes of sinus surgery.
CONCLUSION
In this prospective, multi-institutional cohort study, the majority of patients experienced clinically significant improvement in QOL outcomes with ESS. Certain clinical phenotypes, such as CRS associated with asthma, CRS associated with ASA intolerance, and CRS associated with prior sinus surgery, were significant in the univariate screening of predictors of QOL outcomes but among these, history of prior sinus surgery appears to be most predictive. In addition, standard diagnostic tests such as endoscopy were significant in the univariate screening of potential predictors of QOL outcomes, but not significant in the final predictive models. Finally, preliminary analyses suggested that mucosal inflammatory markers provide important predictive information and deserve further investigation.
Acknowledgments
Supported by a grant from the NIH/NIDCD, R01 DC005805 (PI:TL Smith) Public clinical trial registration (http://www.clinicaltrials.gov), ID: NCT00799097
This study was made possible by a grant from the National Institute on Deafness and Other Communication Disorders (R01 DC005805 PI: TL Smith), one of the National Institutes of Health, Besthesda, MD.
Footnotes
Accepted for oral presentation at the annual meeting of the American Academy of Otolaryngology - Head and Neck Surgery, San Diego, CA., October 4-7, 2009.
References
- 1.Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2000 Summary, National Center for Health Statistics, Hyattsville, MD. Vital Health Stat. 2000;328:1–32. [Google Scholar]
- 2.Anand VK. Epidemiology and economic impact of rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2004;193:3–5. doi: 10.1177/00034894041130s502. [DOI] [PubMed] [Google Scholar]
- 3.Durr DG, Desrosiers MY, Dassa C. Impact of rhinosinusitis in health care delivery: the Quebec experience. J Otolaryngol. 2001;30(2):93–97. doi: 10.2310/7070.2001.20813. [DOI] [PubMed] [Google Scholar]
- 4.Khalid AN, Quraishi SA, Kennedy DW. Long-term quality of life measures after functional endoscopic sinus surgery. Am J Rhinol. 2004;18(3):131–136. [PubMed] [Google Scholar]
- 5.Terris MH, Davidson TM. Review of published results for endoscopic sinus surgery. ENT Journal. 1994;73:574–580. [PubMed] [Google Scholar]
- 6.Senior BA, Kennedy DW, Tanabodee J, et al. Long-term results of functional endoscopic sinus surgery. Laryngoscope. 1998;108(2):151–157. doi: 10.1097/00005537-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Gliklich RE, Metson R. Effect of sinus surgery on quality of life. Otolaryngol Head Neck Surg. 1997;117:12–17. doi: 10.1016/S0194-59989770199-2. [DOI] [PubMed] [Google Scholar]
- 8.Bhattacharyya N. Symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2004;130(3):329–333. doi: 10.1001/archotol.130.3.329. [DOI] [PubMed] [Google Scholar]
- 9.Kountakis SE, Arango P, Bradley D, et al. Molecular and cellular staging for the severity of chronic rhinosinusitis. Laryngoscope. 2004;114(11):1895–1905. doi: 10.1097/01.mlg.0000147917.43615.c0. [DOI] [PubMed] [Google Scholar]
- 10.Smith TL, Mendolia-Loffredo S, Loehrl T, et al. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005;115(12):2199–1205. doi: 10.1097/01.mlg.0000182825.82910.80. [DOI] [PubMed] [Google Scholar]
- 11.Witsell DL, Stewart MG, Monsell EM, et al. The cooperative outcomes group for ENT: A multicenter prospective cohort study on the effectiveness of medical and surgical treatment for patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;132:171–179. doi: 10.1016/j.otohns.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129(3 Suppl):S1–32. doi: 10.1016/s0194-5998(03)01397-4. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention, Alcohol and Public Health. Department of Health and Human Services; Sep, 2008. [Accessed June 6th, 2009]. http://www.cdc.gov/alcohol/ [Google Scholar]
- 14.Benninger MS, Senior BA. The development of the rhinosinusitis disability index. Otolaryngol Head Neck Surg. 1997;123(11):1175–1179. doi: 10.1001/archotol.1997.01900110025004. [DOI] [PubMed] [Google Scholar]
- 15.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 16.Soler ZM, Sauer D, Mace J, et al. Relationship between clinical measures and histopathologic findings in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2009 doi: 10.1016/j.otohns.2009.06.085. Accepted for publication June 16th, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferguson BJ. Eosinophilic mucin rhinosinusitis: a distinct clinicopathological entity. Laryngoscope. 2000;110(5):799–813. doi: 10.1097/00005537-200005000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy DW. Prognostic factors, outcomes and staging in ethmoid sinus surgery. Laryngoscope. 1992;102:1–18. [PubMed] [Google Scholar]
- 19.Batra PS, Kern PC, Tripathi A, et al. Outcome analysis of endoscopic sinus surgery in patients with nasal polyps and asthma. Laryngoscope. 2003;113(10):1703–1706. doi: 10.1097/00005537-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Ford ES, Mannino DM, Redd SC, et al. Determinants of quality of life among people with asthma: findings from the Behavioral Risk Factor Surveillance System. J Asthma. 2004;41(3):327–336. doi: 10.1081/jas-120026090. [DOI] [PubMed] [Google Scholar]


