Abstract
West Virginia is a state at the forefront of the obesity epidemic and one that is experiencing immense health and economic costs as a result. The childhood obesity research discussed in this article was conducted over the past 10 years through 4 projects that range from a school-based cardiovascular risk screening program to an evaluation of state legislation targeting childhood obesity via modifications in the school environment. In the course of these projects, we have collected BMI and other health indices on students, provided feedback to students and their parents, and assessed the obesity and health-related beliefs of West Virginians through individual and focus-group interviews and questionnaires. Our work has been accomplished by using an active-consent process, and BMI has typically been only 1 component of the comprehensive health data we collect and feedback we provide. Collaboration with state and local partners and regular dissemination of our findings have been key elements of the approach taken. The research and policy implications of our findings and approach are discussed.
Keywords: childhood obesity, body mass index, school-based screenings, perceptions
West Virginia is a state at the forefront of the obesity epidemic. It has the second highest rates of adult obesity and youth overweight* in the nation.1 Moreover, West Virginia has evidenced an increasing trend in obesity that exceeds the trend seen nationwide.2 Consistent with these findings, the state has the highest rate of adult diabetes and the highest death rate from heart disease in the nation.3,4 Health care costs associated with obesity in the state have been estimated to be $588 million per year.5
The environment in West Virginia poses a number of challenges for obesity-prevention and treatment initiatives. As the second most rural state in the nation and the only state to reside wholly within Appalachia, two thirds of West Virginia’s 1.8 million people live in communities of <2500 people. Eighty percent of the state’s counties have full or partial designation as health professions shortage areas, and 85% have full or partial designation as medically underserved.6,7 Economically, West Virginia ranks near the bottom, with the second lowest personal per-capita income8 and the fourth highest percentage of children living in poverty.9
The findings discussed in this article were derived from our work addressing the childhood obesity epidemic in West Virginia over the past 10 years through 4 projects that range from a school-based cardiovascular risk screening program to an evaluation of state legislation to reduce childhood obesity through modifications in the school environment.† In the course of these projects we have collected BMI and other health indices from students, provided feedback on weight and cardiovascular risk factors to families, and assessed the health-related beliefs of children and parents through interviews and questionnaires. It is important to note that unlike the surveillance and screening programs conducted in other states,10,11 our screenings have been conducted through an active-consent process, and BMI has typically been only 1 component of the data we collect and feedback we provide. In this article we will provide an overview of these projects and findings as they relate to the collection and reporting of BMI.
CORONARY ARTERY RISK DETECTION IN APPALACHIAN COMMUNITIES
Background and Specific Aims
The Coronary Artery Risk Detection in Appalachian Communities (CARDIAC) project began in 1998 as a surveillance, intervention, and research initiative designed to combat the unacceptably high prevalence of heart disease and diabetes in West Virginia. A component of higher education involving many of the state’s colleges and universities, its specific aims include:
reduce heart disease mortality to no more than 200 deaths per 100 000 population (baseline age adjusted rate of 323.5 in 1998), West Virginia’s Healthy People 2010 flag-ship objective;
provide the opportunity for West Virginia’s health science students to learn concepts of health promotion/disease prevention at the community level; and
partner with state government, secondary and higher education, and the private sector to reverse the obesity epidemic in West Virginia.
The CARDIAC project uses the robust West Virginia Rural Health Education Partnership, a statewide coalition of rural communities and higher education, as the platform on which to identify children and their families at risk of heart disease and diabetes. As part of their required rural-based clinical experiences, health science students are trained by CARDIAC staff and local school nurses to measure BMI and blood pressure and screen for the rash of acanthosis nigricans (AN) as an indicator of possible insulin resistance. During the CARDIAC screenings, fasting lipid profiles, and glucose and insulin levels when AN is present, are obtained by venipuncture performed by experienced phlebotomists. This comprehensive screening program is available to 5th-grade public school students in each of the state’s 55 counties. Active consent of a parent or guardian and child assent are required for participation. Historically, approximately half of the eligible 5th-graders participate (nearly 8000 subjects per year).
Additional CARDIAC initiatives have included developing a longitudinal cohort of students who have been screened across multiple years, and BMI screenings for kindergarten and 2nd-graders throughout the state, also by an active-consent process.
Detailed descriptions of the demographics of the CARDIAC study population, anthropometric measurement protocol, and statistical analysis were published previously.12
Active Versus Passive Consent
The West Virginia University Institutional Review Board for the Protection of Human Subjects requires the active consent of parents and the child’s assent when comprehensive screening, including venipuncture, is performed.
One potential advantage of active consent is that there has been virtually no complaint from parents, their children, or school authorities about the screening process. A notable disadvantage is that our sample is not without selection bias, the extent of which is currently being evaluated.
We added a program offering BMI-only screenings for younger children in selected counties 3 years ago and continued to use active parental consent. The acceptability of this program is presently undergoing evaluation, and strong consideration is being given to adopting a passive-consent process in the next school year, in keeping with current recommendations for universal school-based screenings.13
Screening Results
We recently examined the past 4 years of CARDIAC screening (2002–2006), which included 29 436 5th-graders (mean age: 10.86 years; 53.1% girls). BMI percentiles were calculated according to Centers for Disease Control and Prevention recommendations, and students were placed into 1 of the following weight-status categories: normal or underweight (51.8%) (BMI at <85th percentile), overweight (17.8%) (BMI at ≥85th and <95th percentile), obese (18.6%) (BMI at ≥95th and <99th percentile), or morbidly obese14 (11.7%) (BMI at >99th percentile). The percentage of students within each weight category that had abnormal risk factors are presented in Table 1. Omnibus significance was determined with Kruskal-Wallis nonparametric tests calculated according to BMI category for the other risk factors measured. Significant differences were found for all groups (all P < .05). Mann-Whitney nonparametric tests were then conducted to determine pairwise comparisons (Table 1).
TABLE 1.
Description of Percentage in Each Weight Category According to Percent of Participants in Each Risk-Factor Group
| Risk Factor (% of Students Tested in Each Group) |
Normal or Underweight, % |
Overweight, % | Obese, % | Morbidly Obese, % |
|---|---|---|---|---|
| Elevated blood pressure (19.1%) | 12.9 | 18.3 | 24.7 | 38.9 |
| Elevated TC (11.9%) | 8.4 | 12.6 | 17.6a | 17.8a |
| Low HDL (18.5%) | 10.1 | 19.1 | 28.8 | 40.2 |
| Elevated LDL (8.8%) | 6.2 | 10.1 | 12.9b | 12.5b |
| Elevated TRIG (8.7%) | 2.9 | 8.4 | 16.8 | 22.7 |
| Positive for AN (5.7%) | 1.7 | 3.7 | 8.3 | 22.8 |
| Elevated insulin level (4.9%)c | 0.5 | 1.2 | 6.3 | 22.8 |
Weight categories were defined as: normal or underweight, BMI at <85th percentile; overweight, BMI at ≥85th and <95th percentile; obese, BMI at ≥95th and <99th percentile; and morbidly obese, BMI at >99th percentile.
Numbers with the same superscript letter do not significantly differ from one another; all other comparisons according to weight category were significant (P < .05).
Only tested positive for AN.
Examination of the BMI results across grades revealed that as students matriculated through elementary school, the percentage of those who were overweight progressively increased from 35.0% in kindergarten to 37.8% in 2nd grade and to 48.1% in 5th grade.
WEIGHT-RELATED HEALTH BELIEFS AND PERCEPTIONS
West Virginia’s social and physical environment is unique, with its Appalachian heritage, mountainous and rural geography, poverty, and onerous health indicators. Because of these characteristics, we have considered formative research into the health beliefs of the population a key aspect of intervention development; where feasible, we have also assessed health beliefs after our interventions. We have examined child and adult health beliefs in 3 separate studies, and although these studies have varied according to age group and target behavior, a focus on weight and obesity has been central to each. Across these studies, we have sought to develop an understanding of the ways in which West Virginians perceive their children’s weight, the delivery of health programs in the school setting, and interventions designed to prevent future illness and improve child health. This research has been guided by the theory of planned behavior15 and has used both qualitative (eg, focus-group interviews) and quantitative (ie, questionnaires) methods. A brief description of the studies and methods follows. Each of these studies was approved by the West Virginia University Institutional Review Board.
Overview of Research Studies
In the preschool health-promotion (preschool) project, we developed and evaluated an obesity-prevention program for families in 12 preschools distributed across 4 West Virginia counties by using a randomized, controlled trial at the level of the school. Formative focus-group and individual interviews with parents and teachers (n = 22) and formative health-beliefs questionnaires (HBQs) from parents (n = 112) were used for intervention design. Postintervention evaluative questionnaires were also completed by parents (n = 92).
Our aim for the dyslipidemia-detection (dyslipidemia) project, so named because of its link to the CARDIAC cholesterol-screening initiative, was to continue the investigation of West Virginia health beliefs and develop a beliefs-based intervention to improve participation in the CARDIAC project. The intervention program, which was delivered in 72 schools across 12 West Virginia counties, was also examined via a randomized, controlled trial. Formative focus-group and individual interviews were conducted with 167 5th-grade children, 70 parents, and 14 community leaders. HBQs were obtained by mail from 342 parents of 5th-grade students (38% response rate) by using a systematic random-sampling procedure. Evaluative (ie, postintervention) questionnaires were solicited from a subsample of 102 parents, and 89 (87%) were completed. In addition, telephone interviews were conducted with 200 parents of children who completed the CARDIAC screening.
The Evaluation of the West Virginia Healthy Lifestyles Act (lifestyles) is an ongoing examination of the outcomes associated with recently enacted legislation to address childhood obesity. The legislation includes numerous components to improve the nutrition and physical activity environment within West Virginia schools, and the evaluation includes focus-group and key informant interviews and surveys with children, parents, school personnel and health care providers. We conducted additional focus-group and individual interviews to supplement our existing knowledgebase in designing survey instruments with 10 children, 11 parents, 19 teachers and school personnel, and 4 community leaders.
Methods and Measures
Interviews
Across the studies outlined above, we conducted interviews with ~175 students, 300 parents, and 40 school employees and community leaders. Participants were recruited by fliers distributed through the schools and after-school programs and paid a nominal amount ($10 –$20) for their time. Interviews were conducted by trained research staff following semi-structured interview guides and were tape-recorded and transcribed for analysis. Transcripts were entered into N6 qualitative software16 and were reviewed and coded for content by a minimum of 2 interdisciplinary research staff. See the work by Deskins et al17 for a detailed, representative description of the methods used. The specific questions posed in the interviews varied according to project on the basis of the research topics being addressed, but all projects included questions related to perceptions of weight, obesity, health screenings, and general health.
Questionnaires
HBQs, designed initially for the preschool project, were expanded for use in the dyslipidemia project. These theory of planned behavior– based instruments assess adult beliefs related to their own (HBQ-adult form) or their child’s (HBQ-parent form) health in the following domains: weight, exercise, nutrition, general health, cardiovascular health, and health screenings. Participants were paid $20 for questionnaire completion.
Items within the HBQs can be summed to yield 7 concepts (belief outcomes, evaluation of outcomes, normative beliefs, motivation to comply, perceived likelihood, perceived facilitators, and perceived inhibitors) and 3 composite constructs (attitude toward behavior, subjective norm, and perceived behavioral control) identified by the theory.18 Reliability, assessed by Cronbach’s α, ranged from .72 to .90 for the 10 HBQ-adult scales and from .78 to .93 for the 10 HBQ-parent scales.19 Eight of the 10 values for each scale exceeded .80, and all values exceeded the .70 cutoff recommended for reliability by Nunnally.20 Test-retest correlations, assessed for the HBQ-adult scales across a 4-week interval, ranged from .60 to .80 (all P < .01).
For purposes of this article, we reviewed the data from our focus groups and questionnaires across the preschool, dyslipidemia, and lifestyles projects to identify findings relevant to BMI assessment and reporting in the school setting. Specifically, we extracted the quotations with the content codes of school, weight/obesity, and health screenings for review and identification of prevailing themes, and we selected questionnaire items related to perception of child weight and participation in health-screening programs for analysis.
Parent Perception of Child Weight
Perception of Weight Status
Parent perceptions of child weight status were assessed in both the preschool and dyslipidemia projects. These projects also included direct measurement of child height and weight with feedback to parents about the child’s weight status as determined by BMI. Before measuring the child, parents completed the HBQ, which included the item, “I would describe my child’s weight as ___ ”; response options included moderately underweight, somewhat underweight, about right, somewhat overweight, moderately overweight, and obese. For analysis, somewhat and moderately underweight were combined into a single category of underweight, and somewhat and moderately overweight were similarly combined into a single category of overweight.
Parent responses are provided in Table 2. As indicated, only 5% of the parents of overweight preschool-aged children correctly characterized their child’s weight, and this increased to only 26% for the 5th-grade sample. For children whose BMI was in the obese range, 19% of the preschool parents but a majority (67%) of the 5th-grade parents recognized overweight. No parents labeled their children as obese, although 22 children had BMIs at ≥99th percentile. Although parental accuracy improved with increasing child age, >50% of the overweight and obese children in the 5th grade were labeled as “about right” by their parents. A small proportion of parents of underweight and healthy-weight children overestimated their child’s weight class, but this occurred far less frequently than errors of underestimation.
TABLE 2.
Comparison of Parent Perception and Measured Weight Status in 2 Ages of Children
| Measured BMI and Child Participants |
Parent Perception | |||
|---|---|---|---|---|
| Underweight, %a | About Right, % | Overweight, %b | Obese, % | |
| Underweight | ||||
| Preschool (n = 1) | — | 100 | — | — |
| 5th grade (n = 1) | — | 100 | — | — |
| Healthy weight | ||||
| Preschool (n = 51) | 11.8 | 88.2 | — | — |
| 5th grade (n = 113) | 8.0 | 89.4 | 2.7 | — |
| Overweight | ||||
| Preschool (n = 19) | — | 94.74 | 5.3 | — |
| 5th grade (n = 31) | — | 74.2 | 25.8 | — |
| Obese | ||||
| Preschool (n = 16) | 6.2 | 75.0 | 18.7 | — |
| 5th grade (n = 51) | — | 31.4 | 66.6 | — |
—indicates that no BMI values and parent perceptions fell in these categories.
Somewhat and moderately underweight were combined as underweight.
Somewhat and moderately overweight were combined as overweight.
Determination of Weight Status
Parental misperception of child weight has been reported by other authors, with the magnitude of the misclassification in our samples seeming generally comparable with that reported for other populations.21–23 Among the potential reasons for these misperceptions are the absence of weight-based feedback from physicians,24,25 beliefs that children will “grow into” their weight as they mature,26 and the fact that parents may use social or role-based indicators to determine weight status rather than growth charts or BMI.27 It has also been suggested that as children (and adults) have grown increasingly overweight and obese, our social norms regarding “normal” body size have changed to accommodate the increased sizes.28
Within West Virginia, our focus-group and HBQ data provide support for these explanations. Parents within the dyslipidemia and lifestyles projects indicated that they were skeptical about measurements taken at any particular point in time because children grow at different rates. Some parents voiced mistrust of growth charts and school-based measurements, indicating that they would rely on their family physicians to provide feedback on child weight.
“Well, when they get older, they’ll slim down … it’s a growing thing.”
“They could be overweight now but then sprout up suddenly and be okay the next month.”
“I think people are just used to seeing kids overweight and things like that. … All you have to do is just walk through town and look at the people.”
“I don’t trust the percentile charts.”
In addition, parent responses on the HBQ indicated an overwhelming absence of weight or BMI-based feedback from physicians. In our 5th-grade sample (dyslipidemia), only 23% of the parents of children with BMIs in the overweight or obese range reported that their physician had expressed concern about the child’s weight. Moreover, only 35% of spouses or other family members expressed concern, indicating that there is little weight-related medical or social feedback to assist parents in determining when a child is overweight.
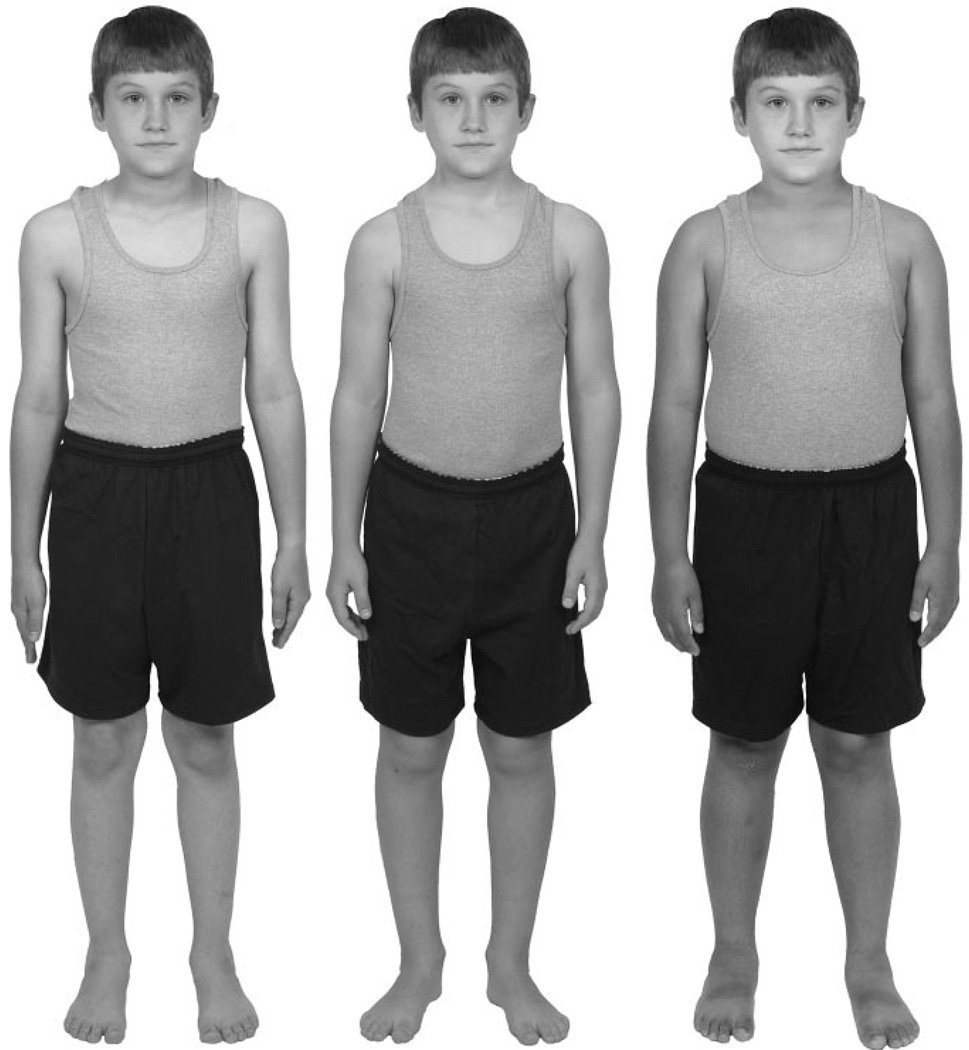
How, then, do parents determine their child’s weight status? The dyslipidemia and lifestyles focus groups revealed that parents primarily determine their child’s weight status “just by looking at them.” To better understand the factors that influence this, we have been developing body-size guides for children that mirror our measures for adults.29 Unfortunately, children’s bodies do not lend themselves to reliable visual determination of weight status. Although men and women can readily discriminate between adult bodies that differ by 3 points in BMI,29 pilot testing with images from our children’s measures revealed that adults cannot differentiate between child bodies with vastly differing BMI percentiles. As indicated in Fig 1, children with BMI percentiles of 55, 75, and 95 look surprisingly similar despite the fact that these children range from normal weight to obese.
FIGURE 1.
Images of 3 prepubescent boys with BMI values ranging from normal weight to obese. BMI percentiles for the boys are, from left to right, 55, 75, and 95.
School-Based Health-Screening Programs
Acceptability of Standard Health-Screening Versus BMI-Screening Programs
West Virginia schools have a long history of conducting health-screening programs with children, particularly in the areas of vision, hearing, and scoliosis. Across the nation, schools have recently become the focus of many BMI-screening and education efforts, due in equal measure to the public health need to address the obesity epidemic and data indicating that primary care providers often fail to use the BMI charts or provide weight guidance to their patients. The reduced frequency of well-child appointments as children age compounds the difficulty of relying on physicians to provide weight-related guidance and feedback.
In West Virginia, parents’ views about school-based health services were mixed and depended largely on the type of screening conducted. Focus groups in the dyslipidemia and lifestyles projects assessed the acceptability of school-based screenings, with an emphasis on comprehensive cardiovascular screenings and BMI-only screenings, respectively. Most parents appreciated the convenience of the standard and comprehensive health screenings that occur in schools and expressed confidence in school nurses. A few parents viewed the screenings as serving only those families without access to private physicians.
“I think they should do more of them [health screenings] through the schools.”
“It [health information] would be good to know. I do know that they’ve had screenings for their teeth, vision, hearing, and they have actually come home from school with notes that say this one needs his eyes examined or this one may need braces.”
“I think they [parents] rely on school screenings a lot for their children.”
Parent perceptions of weight/BMI screenings in schools were generally less positive. Childhood obesity was described as an issue for parents, not the schools, to address, although some parents recognized the value of schools identifying children with weight-related health problems. Parents felt strongly that screenings should be performed in private, and consistent with the report by Kubik et al,26 parents believed that their permission should be required before a child’s weight or BMI is assessed. Concerns about measuring BMI in the schools were focused on 4 areas: (1) fear that the child would be embarrassed or stigmatized by the weight measurement; (2) concern that measurement and reporting had the potential to increase eating disorders, particularly among girls; (3) discomfort with the school’s involvement in matters related to family lifestyle; and (4) a preference to receive health care information from the family physician.
“[Attention-deficit/hyperactivity disorder] is a teacher’s job; childhood obesity is a parent’s responsibility.”
“I think schools are sticking their noses where they don’t belong.”
“My daughter already has issues with her weight … singling her out would be harmful.”
“People will discredit the information [BMI reports] because they think it’s none of the school’s business.”
“I want to know what is being collected even if it’s just going into a database. I feel like anything involving my child, I should know about.”
“Something from the school came home mentioning BMI measurement, but I figured I’d take ’em to the doctor. I opted out because I know our family history.”
“Well if he needs it done, we’ll do it at the doctor’s office. All people don’t have that accessibility so they may consent for it to be done at the school.”
“The only reason it might be okay [screening child without parent permission] is because there are parents who don’t sign up or pay attention, and that’s the child who’s likely to need it most and fall through the cracks.”
Factors That Influence Participation in Health Screenings
The very factors that lead some parents to decline school-based screenings have motivated others to consent to their child’s participation. Parents cited concern about the child’s weight, lack of cholesterol testing by the child’s physician, interest in learning more about how to keep their child healthy, and a family history of weight problems, heart disease, and diabetes as reasons for consenting to their child’s participation in the CARDIAC project. The extent to which various parent concerns about child weight and school involvement might have affected the representativeness of the CARDIAC sample is unknown, but these factors should be considered by school systems deciding between active- and passive-consenting processes for BMI assessment.
In an effort to understand more about the population of parents and children who consented to participation in the CARDIAC project, we split the dyslipidemia sample of 342 parents who completed the HBQs into 2 groups: those who did (n = 198 [58%]) and did not (n = 144 [42%]) consent to their child’s participation in the CARDIAC project. The HBQ sample was recruited independently by mail and was paid for participation, thereby eliminating some of the potential biases inherent in the CARDIAC sample (eg, concerns about weighing child, fear of blood draw), although arguably reflecting others.
Examination of the demographic characteristics of CARDIAC participants and nonparticipants revealed only 2 significant differences: parents of participating children were more likely to have health insurance, and participating children were more likely to have a regular health care provider than their nonparticipating counterparts (P < .05). No significant differences in parent age, gender, education, employment status, or parent and child BMI (based on parent-reported height and weight) were observed.
Parent Preferences Regarding Health Reports
During the dyslipidemia project, we used formative focus groups to ascertain parent preferences regarding the content of, and delivery process for, health-screening reports. We later used additional parent focus groups to review the materials that were developed. The findings from these groups have been used by the CARDIAC project in the design of their health reports.
In general, parents expressed a strong preference for reports that were mailed to the home. Parents were concerned about the loss of reports given to children in school and about the likelihood that children would open the reports to compare the results with their friends. In addition, regarding BMI values and labels in particular, parents did not want the results shared directly with the children. The paramount concern was, again, protecting children from embarrassment and distress.
“You know kids, if it’s given to them in a sealed envelope the first thing they’re going to do is open it up, and they’re going to show each other.”
“They [the results] should be in a sealed envelope mailed home to the family.”
“Children should not get these results; it should be up to the parents to decide to share it with them.”
Although parent preferences should be considered, the cost of mailing reports on a large scale may be prohibitive over time. Moreover, an important teaching opportunity will be lost if the results are not discussed with children at the time of the screening. Decisions about what information to impart and to whom are key for all BMI-surveillance programs and require careful examination of the program goals and environmental context.
In addition to requests for a very clear statement of the findings, many parents wanted information about what steps to take to improve their child’s health. Parents indicated that standard, media-based information on nutrition, in particular, was often confusing and felt that they would benefit by health reports that included information on appropriate nutrition for children of all ages and weights. School personnel also requested inclusion of this information in the reports.
The Impact of CARDIAC Screenings on Parent Perceptions, Intentions, and Behaviors
BMI-surveillance programs can be used both to document the health status of a population and to provide health feedback and education to participants. Within this latter context, the impact of providing BMI feedback is largely unknown. Will parents take steps to modify a child’s diet or exercise habits if they are told that the child is overweight? Will providing feedback on the child’s weight status improve the parents’ understanding of that status? Are individuals who actively choose to participate in screenings more likely to demonstrate changes in knowledge and behaviors than those who are assessed in universal screening programs?
Data obtained during the dyslipidemia project provided partial answers to some of these questions as they relate to the more comprehensive CARDIAC screenings. Telephone interviews conducted 4 to 6 weeks after screening with the parents of children who were determined to be “at risk” (as a result of cholesterol levels or the presence of AN), revealed that 40% made changes in the child’s diet, 34% made changes in the child’s physical activity, and 12% made changes in the child’s health care after receiving the CARDIAC reports. Although these data were obtained in the context of a comprehensive cardiovascular screening program rather than a program that measured only BMI, they are encouraging nonetheless. Conversely, results for the question of improved parental understanding of the child’s weight status are less positive. Parents who completed HBQs before and after the CARDIAC screening demonstrated no significant increase in the accuracy of their perceptions regarding child weight. Parent accuracy was 64% before the CARDIAC project and 67% afterward (P > .05); the primary improvement in accuracy occurred in parents who misidentified their child as underweight before the CARDIAC assessment and corrected their assessment after the screening. The lack of improvement may reflect a lack of salience for the BMI results, because these results were accompanied by cholesterol and blood pressure findings, or they may reflect parents’ dismissal of the BMI labels.
DISCUSSION AND FUTURE DIRECTIONS
In our research in West Virginia, we have documented high rates of overweight and obesity in our youth, the presence of escalating health risks as youth BMI increases, a significant underrecognition of children’s weight status by parents, and a concerning absence of weight-related guidance by primary care providers. These findings parallel the work by numerous others across the United States. Fortunately, we have also demonstrated that health assessments in the West Virginia school setting are generally accepted, even appreciated, by the majority of parents, at least in the context of comprehensive screenings and an active-consent process. We have also found encouraging evidence that parents positively modified lifestyle (diet and physical activity) within the home in response to learning of their child’s risk status. We feel that a careful examination of the health beliefs in our population has enabled us to provide culturally sensitive materials to promote health screenings and has facilitated acceptance of the screening reports. However, many questions about how best to address the West Virginia obesity epidemic remain.
In the ongoing lifestyles project, we will be expanding the knowledge base for addressing obesity in West Virginia by determining the acceptability of BMI-only assessment in schools, the impact of BMI health reports on children and families, the perceptions and practices of health care providers related to childhood obesity and the Healthy Lifestyles legislation, and the impact of the legislated changes on nutrition, physical activity, and health education in the schools. If the CARDIAC project adopts a passive-consent process for BMI screenings in the next year, we will also be in a position to compare the impact of BMI-only screenings conducted under both active-and passive-consent conditions. If the CARDIAC project continues with active consent, we will have additional information on the acceptability and impact of this process.
A decade of comprehensive risk-factor screening in West Virginia seems to have affected public policy at the state and local levels. The legislature has provided line-item support for CARDIAC screening and intervention programs since 2001. Documentation of the severity of the obesity problem, considerably exceeding that obtained through the Youth Risk Behavior Surveillance System, contributed to the adoption of the Healthy Lifestyle Act. In addition, in 2007 the West Virginia Board of Education became the first in the nation to adopt many of the Institute of Medicine’s most recent recommendations for healthier school nutrition.
Passage of the Healthy Lifestyles Act, strong state support for the lifestyles project evaluating the legislation, and the recent adoption of new Institute of Medicine– based child nutrition policies by the Board of Education30 are solid indicators of a serious effort to address childhood obesity in West Virginia. Also underway are a redesign of the state Medicaid program as a patient-centered system that emphasizes prevention, personal responsibility, and coordinated health care. This will support the movement toward a “chronic-care” model for obesity recently suggested by an expert panel.31 We believe that both comprehensive health screenings and BMI-only screenings have a significant role to play in evaluating the success of these strategies and helping to sustain the larger movement to improve health in West Virginia. The key issue is how best to use the screening data to support these initiatives.
During the 2007–2008 academic year, we began integrating screening data with local school wellness policies (required by the Child Nutrition and WIC [Supplemental Nutrition Program for Women, Infants, and Children] Reauthorization Act of 2004). Providing data directly to the wellness councils informs those most responsible at the local level for addressing childhood obesity and sets the stage for increased dialogue about best practices and strategies that have been implemented in other school districts. Importantly, the West Virginia Department of Education has been a key partner in our work. Before the collaboration with local wellness councils and continuing this year, aggregate data were distributed to school administrators and relevant state agencies in the form of an annual governor and legislative report, “Findings From the CARDIAC Project.” Our current lifestyles project is also designed for dissemination, including scheduled presentation of findings to the governor and state legislature.
The personal, health, and economic costs of obesity in West Virginia and the nation will inexorably rise as the alarming number of overweight and obese youth become adults. The increase in the prevalence of obesity among children and adults, accepted by many as an inevitable “social norm,” clearly calls for a different kind of individualized and public health response. We are hopeful that the data being collected through our projects, and the model of providing regular, quantitative feedback on health indices and policy impact to both families and policy makers, will continue to build the evidence base and stimulate progress in reversing the obesity epidemic in West Virginia.
CONCLUSIONS
In West Virginia, providing comprehensive health reports that include BMI seems to have affected parents’ management of their children’s dietary intake, physical activity, and health care. Moreover, a decade of comprehensive risk-factor screening has influenced public policy at the state level. Our collective work has provided a solid foundation for the development of additional initiatives to address childhood obesity, initiatives that are needed to affect clinical and educational practices and policies at the state and local levels. Continued dissemination of the findings from screening and research programs, and collaboration at all levels, are essential for reducing the health and economic burden of obesity in West Virginia.
ACKNOWLEDGMENTS
This research has been supported by National Heart, Lung, and Blood Institute grant RO1-HL070120, Centers for Disease Control and Prevention grant H75-CCH322130, and funding from the Robert Wood Johnson and Claude Worthington Benedum Foundations.
We gratefully acknowledge the assistance of the faculty and staff of the Health Research Center and the CARDIAC project, who provided immeasurable contributions to the completion of these projects.
ABBREVIATIONS
- CARDIAC
Coronary Artery Risk Detection in Appalachian Communities
- AN
acanthosis nigricans
- HBQ
health-beliefs questionnaire
Footnotes
Overweight was the descriptor used to identify children with a BMI at ≥95th percentile in this study; throughout the remainder of the article we use the updated terminology and reference values for overweight (BMI values at ≥85th and <95th percentiles) and obesity (BMI values at ≥95th percentile) in children.
In 2005, the West Virginia legislature passed the Healthy Lifestyles Act, which set new physical education, nutrition, and health education standards for schools and required assessment of student BMI to measure progress in addressing the obesity epidemic.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
References
- 1.Centers for Disease Control and Prevention. BRFSS prevalence and trends data. [Accessed January 18, 2008]; Available at: http://apps.nccd.cdc.gov/brfss.
- 2.Centers for Disease Control and Prevention. Prevalence and trends data: Overweight and obesity 1995–2008 (all states) [Accessed July 21, 2009]; Available at: http://apps.nccd.cdc.gov/brfss.
- 3.Centers for Disease Control and Prevention. Prevalence and trends data: diabetes—2006. [Accessed January 8, 2008]; Available at: http://apps.nccd.cdc.gov/brfss/list.asp?cat=DB&yr=2006&qkey=1363&state=All.
- 4.Centers for Disease Control and Prevention. Miniño AM, Heron MP, Murphy SL, Kochanek KD. National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep. 2007;55(19):1–119. [PubMed] [Google Scholar]
- 5.Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obes Res. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- 6.Medically underserved areas/medically underserved populations (MUA/Ps): West Virginia—all counties. [Accessed July 21, 2009]; Available at: http://muafind.hrsa.gov/index.aspx.
- 7.Health professional shortage areas (HPSAs): West Virginia. [Accessed July 21, 2009]; Available at: http://hpsafind.hrsa.gov/HPSASearch.aspx.
- 8.Personal income per capita in current dollars. [Accessed July 21, 2009];2007 Available at: www.census.gov/statab/ranks/rank29.html.
- 9.US Census Bureau. Current population survey (CPS): annual social and economic (ASEC) supplement. [Accessed January 18, 2008]; Available at: http://pubdb3.census.gov/macro/032007/pov/new46_100125_03.htm.
- 10.Arkansas Center for Health Improvement; University of Arkansas for Medical Sciences. [Accessed July 21, 2009];Year Four Assessment of Childhood and Adolescent Obesity in Arkansas. Available at: www.achi.net/ChildObDocs/ACHI_2007_BMI_ONLINE_State_Report.pdf.
- 11.Commonwealth of Pennsylvania. Health department announces revised growth-screening program for schools [press release] [Accessed February 15, 2008]; Available at: www.state.pa.us/papower/cwp/view.asp?A=11&Q=438070&tx=1.
- 12.Demerath E, Muratova V, Spangler E, Li J, Minor VE, Neal WA. School-based obesity screening in rural Appalachia. Prev Med. 2003;37(6 pt 1):553–560. doi: 10.1016/j.ypmed.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Koplan JP, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 14.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12.e2–17.e2. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 15.Ajzen I. Attitudes, Personality, and Behavior. Buckingham United Kingdom : Open University Press; 1988. [Google Scholar]
- 16.Richards L. Using N6 in Qualitative Research. Melbourne, Australia: QSR International Pty Ltd; 2002. [Google Scholar]
- 17.Deskins S, Harris CV, Bradlyn AS, et al. Preventive care in Appalachia: use of the theory of planned behavior to identify barriers to participation in cholesterol screenings among West Virginians. J Rural Health. 2006;22(4):367–374. doi: 10.1111/j.1748-0361.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I. Nature and operation of attitudes. Annu Rev Psychol. 2001;52:27–58. doi: 10.1146/annurev.psych.52.1.27. [DOI] [PubMed] [Google Scholar]
- 19.Harris CV, Coffman JW, Olexa J, et al. Evaluation of a tailored obesity prevention program for rural families. Centers for Disease Control and Prevention Diabetes and Obesity Conference; May 16 –19, 2006; Denver, CO. Presented at: [Google Scholar]
- 20.Nunnally J. Psychometric Theory. New York, NY: McGraw-Hill; 1978. [Google Scholar]
- 21.Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of over-weight preschool children. Pediatrics. 2000;106(6):1380–1386. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 22.Carnell S, Edwards C, Croker H, Boniface D, Wardle J. Parental perceptions of overweight in 3–5 y olds. Int J Obes (Lond) 2005;29(4):353–355. doi: 10.1038/sj.ijo.0802889. [DOI] [PubMed] [Google Scholar]
- 23.Boutelle K, Fulkerson JA, Neumark-Sztainer D, Story M. Mothers’ perceptions of their adolescents’ weight status: are they accurate? Obes Res. 2004;12(11):1754–1757. doi: 10.1038/oby.2004.217. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton JL, James FW, Bazargan M. Provider practice, overweight and associated risk variables among children from a multi-ethnic underserved community. J Natl Med Assoc. 2003;95(6):441–448. [PMC free article] [PubMed] [Google Scholar]
- 25.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114(2) doi: 10.1542/peds.114.2.e154. Available at: www.pediatrics.org/cgi/content/full/114/2/e154. [DOI] [PubMed] [Google Scholar]
- 26.Kubik MY, Story M, Rieland G. Developing school-based BMI screening and parent notification programs: findings from focus groups with parents of elementary school students. Health Educ Behav. 2007;34(4):622–633. doi: 10.1177/1090198105285373. [DOI] [PubMed] [Google Scholar]
- 27.Jain A, Sherman SN, Chamberlin DL, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 28.Maximova K, McGrath JJ, Barnett T, O’Loughlin J, Paradis G, Lambert M. Do you see what I see? Weight status misperception and exposure to obesity among children and adolescents. Int J Obes (Lond) 2008;32(6):1008–1015. doi: 10.1038/ijo.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris CV, Bradlyn AS, Coffman J, Gunel E, Cottrell L. BMI-based body size guides for women and men: development and validation of a novel pictorial method to assess weight-related concepts. Int J Obes (Lond) 2008;32(2):336–342. doi: 10.1038/sj.ijo.0803704. [DOI] [PubMed] [Google Scholar]
- 30.West Virginia Department of Education. The West Virginia Board of Education strengthens nutrition policy [press release] [Accessed March 5, 2008]; Available at: http://wvde.state.wv.us/news/1595.
- 31.Expert Committee. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]