Abstract
Background
Voriconazole is a broad spectrum antifungal agent associated with photosensitivity and accelerated photoaging. A possible link with aggressive squamous cell carcinoma (SCC) has also been reported.
Objective
To determine the incidence and frequency of cutaneous SCC amongst patients undergoing long-term treatment with voriconazole who also manifest features of chronic phototoxicity.
Methods
A retrospective review of patients who developed one or more squamous cell neoplasms during long-term treatment with voriconazole at three academic dermatology centers.
Results
51 cutaneous SCC were identified in 8 patients (median age 34.5 years, range 9–54) treated with chronic voriconazole (median duration 46.5 months, range 13–60). Underlying diagnoses included graft-versus-host disease, HIV, and Wegener’s granulomatosis. Signs of chronic phototoxicity and accelerated photoaging included erythema, actinic keratoses, and lentigo formation.
Limitations
The retrospective nature of the study cannot determine the true population risk of SCC associated with voriconazole therapy. A prospective cohort study is needed.
Conclusion
A high index of suspicion for photosensitivity and SCC may be warranted with chronic voriconazole use when utilized in the setting of concurrent immunosuppression.
Keywords: Fungal infection, Immunosuppression, Photoaging, Photosensitivity, Phototoxicity, Squamous cell carcinoma, Voriconazole
INTRODUCTION
Voriconazole (Vfend®, Pfizer, New York) is a second-generation triazole antifungal approved by the FDA in 2002 for the treatment of invasive aspergillosis, candidemia in non-neutropenic patients, esophageal candidiasis and disseminated candidal infections, and infections due to Scedosporium apiospermum and Fusarium spp. It’s antifungal spectrum, oral bioavailability, and generally well-tolerated side effect profile has led to the drug’s widespread use in the treatment of invasive aspergillosis1 as well as “off-label” use as long-term prophylactic therapy following allogeneic hematopoeitic cell transplantation (HCT).2,3
Frequently reported adverse reactions during voriconazole therapy are vision abnormalities (21%), hepatic transaminase elevation (15.6%), and skin rash (7%), including photosensitivity.4 Phototoxicity from the drug results in prominent sunburn-like erythema that is limited to the exposed surfaces of the skin, particularly the head and neck, dorsal hands, and forearms.2,5 Vesicle and bullae formation on sun exposed areas resembling porphyria cutanea tarda (drug-induced pseudoporphyria) may occur.6–8 Although the long-term effects of drug-induced phototoxicity are not well-described, three reports of single patients from Australia, France, and Belgium depict aggressive and multifocal squamous cell carcinoma (SCC) of the skin in immunocompromised patients undergoing chronic treatment with voriconazole.9–11 In this report, we describe the first series of eight US patients, including two children and two young adults, who developed SCC during chronic treatment with voriconazole. One patient expired from metastasis of his SCC. All patients had concurrent signs of chronic photodamage, suggesting that in the setting of immune compromise, chronic voriconazole-associated photosensitivity may accelerate ultraviolet radiation-induced skin damage and promote the development of skin cancer.
METHODS
In this analysis, eight patients with a history of voriconazole-associated phototoxicity who developed cutaneous SCC were identified at the National Institutes of Health (NIH), University of California-San Francisco Medical Center, and the Duke University Dermatology Units between 4/2005 and 1/2009. Medical records, clinical photography, and histologic specimens were reviewed. Solid organ allograft recipients and patients with a history of azathioprine exposure were excluded due to the expected high rate of SCC in these settings. Patients with a history of SCC prior to voriconazole exposure were also excluded.
RESULTS AND REPRESENTATIVE CASES
Eight patients, including 2 children and two young adults, with features of voriconazole-related phototoxicity who developed one or more cutaneous SCC were identified (Table I; Figure 1). Manifestations of phototoxicity and chronic photodamage included erythema of photoexposed surfaces, actinic keratoses (Figure 1A,B), and numerous lentigines, including dark brown lentigines resembling xeroderma pigmentosum in one patient (Figure 1E,F). The median age at time of first SCC diagnosis was 34.5 years (range 9–54). A total of 51 SCC were diagnosed. Patients were treated with voriconazole 50mg QD-350mg BID (median 200mg BID) for a median duration of 46.5 months (range 13–60) at the time of diagnosis of the first SCC. Six patients had a history of hematopoietic stem cell transplantation, one was infected with HIV, and one had long-standing Wegener’s granulomatosis. The median duration of immunosuppression (excluding the HIV patient) was 51 months (range 13–122 months).
TABLE I.
Characteristics of patients with squamous cell carcinoma following chronic treatment with voriconazole.
| Patient | Age/sex | Ethnicity | Past medical history/duration of immunosuppression |
Voriconazole dose/duration |
History of immunosuppressant Use |
Other photosensitizing drugs |
Phototoxicity/ photodamage |
Neoplasia |
|---|---|---|---|---|---|---|---|---|
| 1 | 9/M | Caucasian | ALL/46 months s/p CBHCT |
150mg BID/39 mo.† | cyclosporine, daclizumab, prednisone,* thalidomide,* topical tacrolimus |
TMP/SMX | Erythema, cheilitis, lentigo formation on face, neck, dorsal forearms, hands |
AK/superficially invasive SCC SCC (2) |
| 2 | 11/M | Caucasian | ALL, ITP, 54 months s/p CBHCT |
50mg qd/54 mo. | azathioprine*, cyclosporine, daclizumab, sirolimus, prednisone*, thalidomide* |
none | Faint erythema, mild lentigo formation lateral neck, dorsal hands |
AK (2) SCCis (2) SCC (2) |
| 3 | 22/M | Caucasian | HIV (age 2) | 250mg bid/15 mo. | none | TMP/SMX | Extensive erythema and lentigo formation dorsal hands, head/neck, forearms, upper back |
SCC |
| 4 | 41/M | Caucasian | Non-Hodgkin's lymphoma/48 months s/p PBHCT |
250 mg bid/48 mo. | etanercept, methylprednisolone*, rituximab, tacrolimus* |
none | Faint erythema/extensive lentigo formation lateral, posterior neck |
SCC (4) |
| 5 | 46/M | Caucasian | Wegener's granulomatosis/122 months |
200mg bid/45 mo | prednisone, methotrexate |
none | Telangiectasias | SCC (10) |
| 6 | 43/M | Caucasian | ALL, 51 months s/p allo SCT |
200mg bid/51 mo | cyclosporine, prednisone, mycophenolate mofetil*, sirolimus* |
TMP/SMX | Erythema, telangiectasias, advanced photodamage |
SCC (25) |
| 7 | 28/M | Caucasian | CML, 84 months s/p allo SCT |
200mg bid/60 mo | tacrolimus*, mycophenolate mofetil, prednisone*, sirolimus* |
dapsone | Erythema, dermatoheliosis |
SCC (2), inflamed AKs |
| 8 | 54/M | Caucasian | CLL/SLL (small lymphocytic leukemia) 13 months s/p allo SCT |
350mg bid/13 mo | prednisone, tacrolimus |
None | Erythema, actinic keratoses |
SCC (2), AK (5) |
AK: actinic keratosis
ALL: acute lymphoblastic leukemia
CLL: chronic lymphocytic leukemia
CBSCT: cord blood stem cell transplant
ITP: idiopathic thrombocytopenic purpura
PBSCT: peripheral blood stem cell transplant
SCC: squamous cell carcinoma
SCCis: squamous cell carcinoma in situ
Drug discontinued 6 months prior to evaluation
Current immunosuppressant therapy at time of evaluation
FIGURE 1. Cutaneous manifestations of long-term treatment with voriconazole.



A. Nine year-old boy with extensive lentigo formation and multiple actinic keratoses on the head and neck following three years of treatment with voriconazole (Pt 1).
B. Hyperkeratotic lesion with erythema on the left neck of Pt 1. Histology demonstrated acanthotic solar keratosis with acantholysis, bordering on superficially invasive SCC.
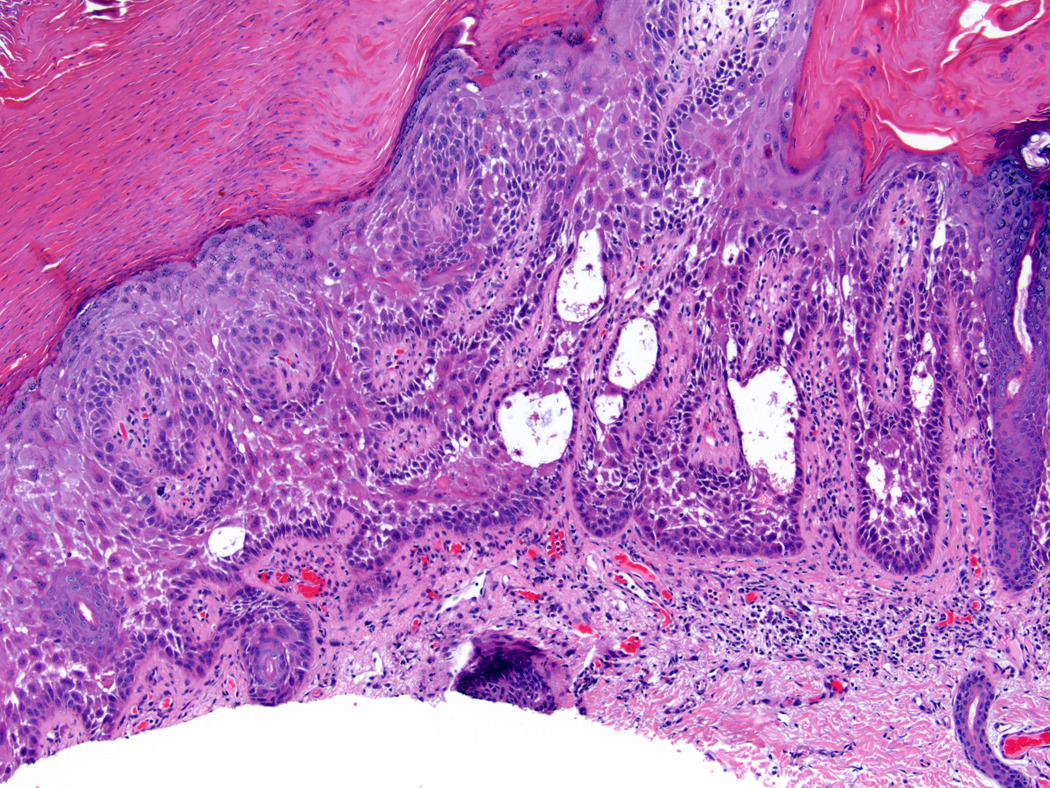
C. Histology of lesion on left neck (Figure 1B) identified acanthotic solar keratosis with acantholysis. This lesion bordered on superficially invasive squamous cell carcinoma (hematoxylin and eosin, original magnification 100×).
D. 22 year-old male with long-standing HIV infection with SCC on left lateral neck following 15 months of voriconazole therapy (Pt. 3). Chronic phototoxicity with erythema and dark brown lentiginous pigmentation is present on the head and lateral neck.
E. Similar erythema and pigmentation resembling xeroderma pigmentosum is present on the photo-exposed surfaces of the posterior neck and upper extremities (Pt. 3).
F. 46-year old male (Pt. 5) following four years of treatment with voriconazole with recurrent SCC on the left preauricular cheek. The patient subsequently died of metastatic disease.
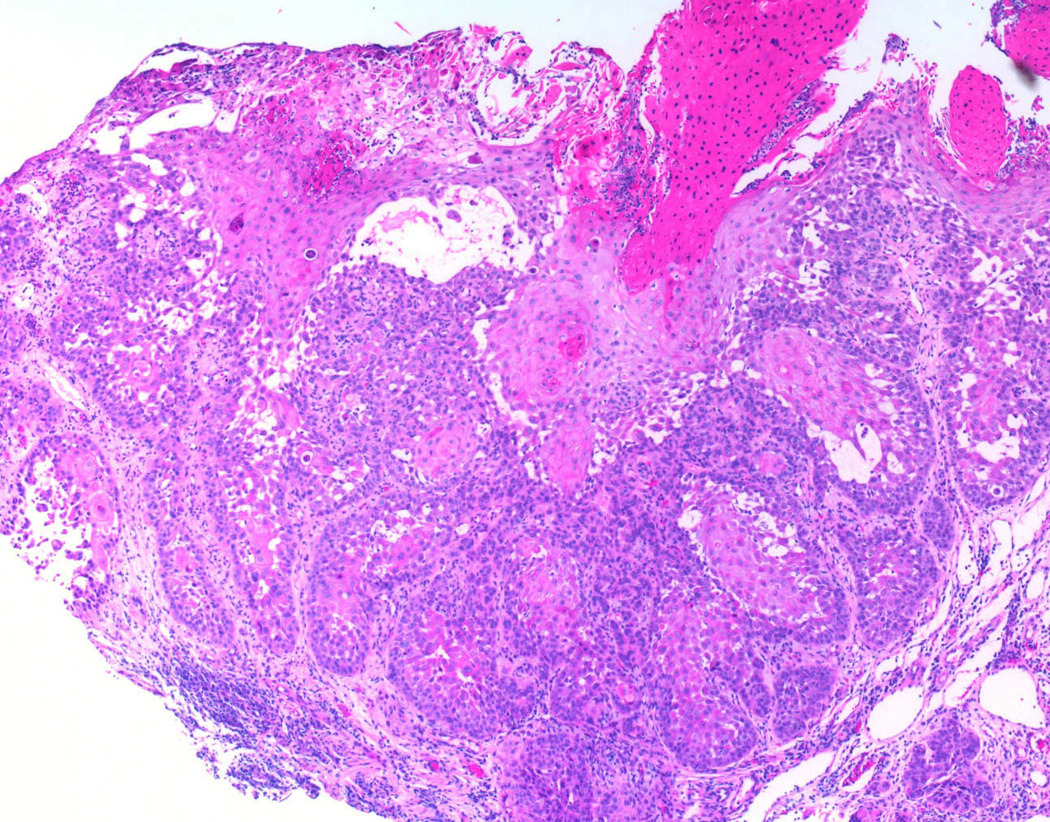
G. Histology of SCC from right cheek (Pt. 5) reveals deeply invasive SCC with keratinocyte pleomorphism, representative of the multiple SCCs that developed in this patient (hematoxylin and eosin, original magnification 40×).
Accelerated photodamage and actinic keratosis/SCC in a pediatric patient following long-term voriconazole therapy
A nine year old Caucasian boy (Table I, Pt. 1) was evaluated for a three-year history of skin eruption on the face, dorsal hands, and anterior neck. Three years, ten months prior to evaluation the patient received an unrelated cord blood HCT for Philadelphia chromosome positive acute lymphocytic leukemia. At the time of transplantation, he began voriconazole (150 mg BID) which had been discontinued 6 months prior to his current evaluation. The patient had a history of acute skin graft-versus-host disease (GVHD) which responded to cyclosporine and methlyprednisone. Approximately four months following transplantation, erythema of his forearms, cheeks, and lower extremities was noted, and was attributed to mild GVHD. The eruption did not respond to topical tacrolimus, oral corticosteroids, daclizumab, cyclosporine, thalidomide, and tacrolimus. His medications at the time of evaluation were acyclovir, amlodipine, trimethoprim/sulfamethoxazole (TMP/SMX), prednisone 2.5 mg QOD, and thalidomide 100mg QD.
Upon examination, multiple erythematous papules were present on the anterior chest with erosions on the face, distal arms and posterior neck. Ephelides, lentigines and erythema were limited to the photoexposed surfaces of the body (Figure 1A, B). Hyperkeratotic papules were noted on the hands and posterior neck. A skin biopsy from the posterior neck demonstrated actinic keratosis, but superficially invasive SCC could not be ruled out (Figure 1C). Oral acitretin, topical 5-flourouracil, and aggressive photodynamic therapy was instituted; however, the child subsequently developed two additional high-risk invasive SCCs of the right conchal bowl and the lower lip.
Adult patient with multiple aggressive SCC following long-term voriconazole treatment
A 46-year-old male (Table I, Pt. 5) with a 10 year history of Wegener’s granulomatosis on chronic therapy with prednisone and methotrexate developed pulmonary aspergillosis. Treatment with amphotericin was complicated by renal toxicity, and voriconazole (200 milligrams twice daily) was initiated and maintained for long-term prophylaxis. Following three years of treatment, he developed photosensitivity, photodamage, and multiple actinic keratoses on the face, arms and dorsal hands. During the next two years he developed 10 SCCs, predominantly on the scalp and cheeks. These included acantholytic and desmoplastic subtypes, with recurrent tumor foci on the left preauricular area (Figure 1F). Multiple tumors recurred following Mohs micrographic surgery, and cetuximab was initiated for multiple inoperable SCC, followed by the addition of carboplatin when cetuximab failed to halt the progressive enlargement of tumors on the forehead and left preauricular area (Figure 1G). Radiation therapy was initiated for involvement of the left parotid, followed by total parotidectomy. Four months later a focal mass lesion was demonstrated by MRI in the right parietal lobe and was confirmed to be metastatic disease by biopsy. The patient expired from complications of metastatic disease.
DISCUSSION
Voriconazole-induced photosensitivity most commonly presents as a “sunburn” response on sun-exposed surfaces of the body; it may also present as cheilitis, exfoliative dermatitis, pseudoporphyria cutanea tarda, or lesions resembling discoid lupus erythematosus.5,6,8,12 In general, these reactions are reversible upon discontinuation of the drug. Recent reports have also described pigmentary changes limited to the photo-exposed surfaces of the skin in voriconazole-treated pediatric patients, suggestive of accelerated photoaging and chronic photodamage.2,13 Of greatest concern are three single international case reports of aggressive and multifocal cutaneous squamous cell carcinoma with voriconazole use in the immunocompromised setting (renal allograft recipient, HIV infection, and chronic granulomatous disease.)9–11 In addition, preliminary abstract data suggests that lung transplant patients taking voriconazole antifungal prophylaxis may be at increased risk of non-melanoma skin cancer.14
Chronic immunosuppression is a well-recognized risk factor for the development of non-melanoma skin cancer. SCC in particular is a significant long-term complication for many renal allograft recipients.15 However, the short duration of immunosuppression preceding the development of SCC, the unusually high number of SCC tumors following SCT, and the young age at onset of SCC observed in this series suggest that voriconazole-associated phototoxicity accelerates the risk of SCC formation in the immunocompromised setting.
The mechanism of voriconazole-induced photosensitivity is not clearly understood, but may result from a metabolite of the drug, rather than the drug itself. Although voriconazole does not absorb in the UVA or UVB spectrum, its major metabolite, voriconazole N-oxide, absorbs in the UVB and UVA ranges,16 and may therefore act as the requisite chromophore for phototoxicity. Voriconazole is extensively metabolized by the cytochrome P450 enzymes CYP2C19, CYP2C9, and CYP3A4, and less than 2% of the drug is excreted unchanged.17 Polymorphisms in CYP2C19 significantly influence voriconazole metabolism.17 Homozygous poor metabolism polymorphisms in CYP2C19 result in plasma voriconazole concentrations 3–5 times that found in extensive metabolizers. The prevalence of homozygous poor metabolizer CYP2C19 polymorphisms in the population is 20–30% in Asians and 2–3% in Caucasians.17 To our knowledge, a relationship between voriconazole metabolism and phototoxicity has not been reported, and further investigation is needed to determine the variability in photosensitivity observed between individual patients.
All of the patients in this series demonstrated one or more cutaneous signs of phototoxicity, implicating ultraviolet radiation-induced DNA damage in promoting cutaneous malignancy. In addition to direct UVA-induced DNA damage, there is evidence that UV-induced alteration of the microenvironment (cell-cell interactions, cytokine release, cell-extracellular matrix interactions, inflammation, and loss of T regulatory cells) may also promote the development of cutaneous malignancy.18 The extensive lentigo formation seen in this series is reminiscent of a similar phenomenon noted in patients undergoing phototherapy with psoralen (a photosensitizer) and ultraviolet A (PUVA). Patients receiving high cumulative doses of PUVA are at greatly increased risk of SCC formation, an effect that persists even after discontinuation of the treatment.19
There is also experimental evidence that phototoxic drug exposure is associated with an elevated risk of cutaneous malignancy. Photocarcinogenesis studies utilizing fluoroquinolones have demonstrated accelerated skin tumor formation in mice, even when sub-phototoxic doses of UVA radiation were administered chronically.20 A correlation between photosensitizing drug exposure and non-melanoma skin cancer was also identified in two recent population-based case-control studies.21,22 Although we cannot completely discount the potential contribution of other potential photosensitizing agents (TMP/SMX, dapsone) administered concurrently with voriconazole in four patients in this series, it should be noted that other signs of premature photoaging (lentiginoses, actinic keratoses) and SCC are not typically encountered with the use of these agents.
Although prolonged immunosuppressive therapy and severity of GVHD are known risk factors for the development of SCC in the HCT setting,23 in our 5-year experience systematically evaluating approximately 150 treatment-refractory patients with chronic GVHD at the NIH, cutaneous SCC is uncommon, despite chronic immunosuppression employed in nearly all patients. In contrast to the organ transplant setting, the cumulative incidence of oral and cutaneous SCC in a cohort of 24,011 HCT recipients was only 1.1% at 20 years (95% CI: 0.7–1.7).23 Similarly, a 20-year follow-up of 4,810 allogeneic HCT recipients at the Fred Hutchinson Cancer Research Center yielded a cumulative SCC incidence estimate of only 3.4%.24
Both the early age of onset (median 34.5 years; range 9–54) and short duration of immunosuppression (median 51 months; range 13–122) prior to the development of skin cancer in our series are also highly unusual in comparison to established data on SCC incidence following immunosuppression in the renal allograft and HCT settings. The latency between renal transplantation and first skin cancer formation is approximately three years in allograft recipients over age 60, but increases to 8 years in patients younger than 40 years.15 In the Curtis23 bone marrow registry review of 24,011 HCT patients, the median interval between HCT and SCC diagnosis was 7 years. Similarly, at Fred Hutchinson Cancer Research Center, SCC developed a median 6.3 years after HCT in a somewhat older population (median age 48.9 years).24 In comparison, the median duration to first SCC amongst the 6 HCT recipients in this series was only 4.1 years, despite a younger age (median 34.5 years, range 9–54) at time of transplantation.
Even with the apparent link between photosensitizing drugs and cancer risk suggested by both this study and preliminary population based-data, a complete understanding of the role of phototoxic drugs in SCC development in individual patients, particularly those who are immunosuppressed, is unclear. Most phototoxic drugs, including TMP/SMX and flouroquinolones, are typically prescribed for a limited time period, and alternative regimens are readily available if severe photosensitivity is detected. By contrast, voriconazole is often employed as chronic therapy for ambulatory, immunocompromised patients for whom oral alternatives with similar broad-spectrum anti-fungal activity were not available until recently. Thus, SCC development may require chronic phototoxicity as well as a “high-risk” immunocompromised population in a manner analogous to the increased risk of SCC following long-term PUVA phototherapy in patients who also receive cyclosporine.25
We believe a high index of suspicion for photosensitivity is warranted when using voriconazole, particularly in light of the potential for misdiagnosis of this reaction as GVHD in the post-HCT setting.2 Until the role of voriconazole in the development of SCC in the immunocompromised setting is more clearly understood, we recommend strict photoprotective measures be employed. Careful reappraisal of the need for long-term voriconazole prophylaxis may be of value, particularly in patients who manifest signs of chronic photodamage or have a history of skin cancer.
Acknowledgments
Funding Source: This research was supported in part by the Intramural Program of the NIH, Center for Cancer Research, National Cancer Institute.
Glossary
Abbreviations used
- AK
actinic keratosis
- GVHD
graft-versus-host disease
- HCT
hematopoeitic cell transplantation
- SCC
squamous cell carcinoma
- TMP/SMX
trimethoprim/sulfamethoxazole
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None declared
Capsule Summary
Voriconazole is an oral broad-spectrum antifungal frequently employed for the long-term management of chronically immunosuppressed patients. It has been associated with photosensitivity, accelerated photoaging, and aggressive squamous cell carcinoma (SCC).
In this series, 51 cutaneous SCC were identified in 8 patients treated with chronic voriconazole in the setting of graft-versus-host disease, HIV, and Wegener’s granulomatosis.
A high index of suspicion for photosensitivity and SCC may be warranted with voriconazole use in the setting of concurrent immunosuppression.
REFERENCES
- 1.Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–415. doi: 10.1056/NEJMoa020191. [DOI] [PubMed] [Google Scholar]
- 2.Patel AR, Turner ML, Baird K, Gea-Banacloche J, Mitchell S, Pavletic SZ, et al. Voriconazole-induced phototoxicity masquerading as chronic graft-versus-host disease of the skin in allogeneic hematopoietic cell transplant recipients. Biol Blood Marrow Transplant. 2009;15:370–376. doi: 10.1016/j.bbmt.2008.12.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wingard JR, Carter SL, Walsh JT, Kurtzberg J, Small TN, Gersten ID, et al. Results of a randomized, double-blind trial of fluconazole (FLU) vs. voriconazole (VORI) for the prevention of invasive fungal infections (IFI) in 600 allogeneic blood and marrow transplant (BMT) patients. ASH Annual Meet Abstr 110. 2007:163. [Google Scholar]
- 4.Voriconazole (Vfend®) product labeling information. http://media.pfizer.com/files/products/uspi_vfend.pdf. June 27, 2009.
- 5.Denning DW, Griffiths CE. Muco-cutaneous retinoid-effects and facial erythema related to the novel triazole antifungal agent voriconazole. Clin Exp Dermatol. 2001;26:648–653. doi: 10.1046/j.1365-2230.2001.00909.x. [DOI] [PubMed] [Google Scholar]
- 6.Dolan CK, Hall MA, Blazes DL, Norwood CW. Pseudoporphyria as a result of voriconazole use: a case report. Int J Dermatol. 2004;43:768–771. doi: 10.1111/j.1365-4632.2004.02177.x. [DOI] [PubMed] [Google Scholar]
- 7.Kwong WT, Hsu S. Pseudoporphyria associated with voriconazole. J Drugs Dermatol. 2007;6:1042–1044. [PubMed] [Google Scholar]
- 8.Tolland JP, McKeown PP, Corbett JR. Voriconazole-induced pseudoporphyria. Photodermatol Photoimmunol Photomed. 2007;23:29–31. doi: 10.1111/j.1600-0781.2007.00263.x. [DOI] [PubMed] [Google Scholar]
- 9.Brunel AS, Fraisse T, Lechiche C, Pinzani V, Mauboussin JM, Sotto A. Multifocal squamous cell carcinomas in an HIV-infected patient with a long-term voriconazole therapy. AIDS. 2008;22:905–906. doi: 10.1097/QAD.0b013e3282f706a9. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy KL, Playford EG, Looke DF, Whitby M. Severe photosensitivity causing multifocal squamous cell carcinomas secondary to prolonged voriconazole therapy. Clin Infect Dis. 2007;44:e55–e56. doi: 10.1086/511685. [DOI] [PubMed] [Google Scholar]
- 11.Vanacker A, Fabre G, Van Dorpe J, Peetermans WE, Maes B. Aggressive cutaneous squamous cell carcinoma associated with prolonged voriconazole therapy in a renal transplant patient. Am J Transplant. 2008;8:877–880. doi: 10.1111/j.1600-6143.2007.02140.x. [DOI] [PubMed] [Google Scholar]
- 12.Rubenstein M, Levy ML, Metry D. Voriconazole-induced retinoid-like photosensitivity in children. Pediatr Dermatol. 2004;21:675–678. doi: 10.1111/j.0736-8046.2004.21614.x. [DOI] [PubMed] [Google Scholar]
- 13.Racette AJ, Roenigk HH, Jr, Hansen R, Mendelson D, Park A. Photoaging and phototoxicity from long-term voriconazole treatment in a 15-year-old girl. J Am Acad Dermatol. 2005;52:S81–S85. doi: 10.1016/j.jaad.2004.07.034. [DOI] [PubMed] [Google Scholar]
- 14.Feist AA, Osborne SL, Thistlethwaite PA, Madani M, Reed S, Yung G. Voriconazole use increases the incidence of skin cancer in lung transplant recipients. J Heart Lung Transplant. 2009;28:S242. [abstract] [Google Scholar]
- 15.Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation.[see comment] N Engl J Med. 2003;348:1681–1691. doi: 10.1056/NEJMra022137. [DOI] [PubMed] [Google Scholar]
- 16.Murayama N, Imai N, Nakane T, Shimizu M, Yamazaki H. Roles of CYP3A4 and CYP2C19 in methyl hydroxylated and N-oxidized metabolite formation from voriconazole, a new anti-fungal agent, in human liver microsomes. Biochem Pharmacol. 2007;73:2020–2026. doi: 10.1016/j.bcp.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Bruggemann RJ, Alffenaar JW, Blijlevens NM, Billaud EM, Kosternik JG, Verweij PE, et al. Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents. Clin Infect Dis. 2009;48:1441–1458. doi: 10.1086/598327. [DOI] [PubMed] [Google Scholar]
- 18.Halliday GM, Lyons JG. Inflammatory doses of UV may not be necessary for skin carcinogenesis. Photochem Photobiol. 2008;84:272–283. doi: 10.1111/j.1751-1097.2007.00247.x. [DOI] [PubMed] [Google Scholar]
- 19.Stern RS. Psoralen and ultraviolet a light therapy for psoriasis. N Engl J Med. 2007;357:682–690. doi: 10.1056/NEJMct072317. [DOI] [PubMed] [Google Scholar]
- 20.Klecak G, Urbach B, Urwyler H. Fluoroquinolone antibacterials enhance UVA-induced skin tumors. J Photochem Photobiol B. 1997;37:174–181. doi: 10.1016/s1011-1344(96)07424-6. [DOI] [PubMed] [Google Scholar]
- 21.Jensen AO, Thomsen HF, Engebjerg MC, Olesen AB, Sorensen HT, Karagas MR. Use of photosensitising diuretics and risk of skin cancer: a population-based case-control study. Br J Cancer. 2008;99:1522–1528. doi: 10.1038/sj.bjc.6604686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karagas MR, Stukel TA, Umland V, Tsoukas MM, Mott LA, Sorensen HT, et al. Reported use of photosensitizing medications and basal cell and squamous cell carcinoma of the skin: results of a population-based case-control study. J Invest Dermatol. 2007;127:2901–2903. doi: 10.1038/sj.jid.5700934. [DOI] [PubMed] [Google Scholar]
- 23.Curtis RE, Metayer C, Rizzo JD, Socié G, Sobocinski KA, Flowers ME, et al. Impact of chronic GVHD therapy on the development of squamous-cell cancers after hematopoietic stem-cell transplantation: an international case-control study. Blood. 2005;105:3802–3811. doi: 10.1182/blood-2004-09-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leisenring W, Friedman DL, Flowers ME, Schwartz JL, Deeg HJ. Nonmelanoma skin and mucosal cancers after hematopoietic cell transplantation. J Clin Oncol. 2006;24:1119–1126. doi: 10.1200/JCO.2005.02.7052. [DOI] [PubMed] [Google Scholar]
- 25.Marcil I, Stern RS. Squamous-cell cancer of the skin in patients given PUVA and ciclosporin: nested cohort crossover study. Lancet. 2001;358:1042–1045. doi: 10.1016/S0140-6736(01)06179-7. [DOI] [PubMed] [Google Scholar]




