Abstract
To explore how patients and providers respond to Tailored Lifestyle Conversations (TLC), an evidence-based decision aid to help patients set priorities for selecting among multiple health behavior change goals, we conducted a study utilizing key informant interviews. Based on patient level assessment data, TLC presents tailored outputs that include 1) behavioral and clinical risk; 2) readiness and confidence scores for changing each of four behaviors; and 3) qualitative equations to elicit patient priorities for change. Patient priorities are documented in an action plan to be discussed with their provider during a clinical encounter. Interview questions probed how patients and providers responded to this output, and how heavily they valued the chance of success versus health benefit in deciding which behavior to work on first. The interviews also revealed how TLC might mediate the conversation around behavior change between patients and providers. TLC has potential to drive a more evidence based and patient centric approach to behavioral counseling in clinical settings.
Keywords: Health behavior, Health promotion, Computer-based tailoring, Decision support
Introduction
A patient centered approach to changing the health behaviors of Americans has the greatest potential of any current approach for decreasing morbidity and mortality and for improving the quality of life across diverse populations.1 2 The 1996 edition of the Guide to Clinical Preventive Services by the USPSTF concluded: “Effective interventions that address personal health practices … [for] … primary prevention … hold greater promise for improving overall health than many secondary preventive measures, such as routine screening for early disease. Therefore, clinician counseling that leads to improved personal health practices may be more valuable than conventional clinical activities, such as diagnostic testing.3 Yet, rates of behavioral counseling in primary care fall far below national targets. In fact, gaps in the delivery of clinical preventive services are greater for behavioral counseling than for screening or chemoprophylaxis.4
Research suggests that only 35% of patients have ever been counseled to exercise regularly 5, only 42% of overweight and obese patients had been counseled to lose weight6, and only 37% of smokers had been advised by their physicians to quit7. Provider-centric alerts and decision support have been linked to EHRs to increase counseling in primary care, however results are beginning to emerge and generally are disappointing. For example, in a national survey, EHR use and the association of EHR with 17 ambulatory quality indicators there was no improved performance on any of the 5 counseling indicators.8 Results from a recent systematic review of information technology to support self-management in chronic care show that most research in this area focus on the use of technology by individuals for self education, and a critical lack of applications to enable collaboration of providers and individuals in self management activities. This pattern is “incongruent with the Chronic Care Model”, which emphasizes collaboration of informed activated patients with the health care system.9
The Tailored Lifestyle Conversations (TLC) system suggests an alternative approach to the use of provider-centric EHR alerts and decision support tools to increase behavioral counseling services in clinical care. TLC emphasizes that legitimate patient choice exists when there are a range of behavioral recommendations, such as loosing weight, quitting smoking, and physical inactivity. The choice about which behavior to prioritize first is itself preference sensitive and based on personal goals and priorities. TLC is designed as a transaction decision aid, which prior to a visit with their provider prepares the patient to consider their preferences for behavior change goals. Subsequently, a pre-activated patient is ready to engage in a conversation with their provider about behavioral change, incorporating both their understanding of clinical risk and priorities for choosing among multiple behavior change goals.
Patient Choice for Health Behavior Change
A number of false assumptions are made by providers in behavioral counseling: that achieving good health is the patient’s main motivation for change, that patients want to change, that now is always the right time to change, and that the physician knows best how the patient should change.10 Contrary to these assumptions, patients do not necessarily choose to work on the risk factor most harmful to their health.11 Since patient and provider priorities may often lack concordance, a transactional decision aid, between patient and provider presents a viable option to incorporate patient choice together with medical importance in coming to a decision that will accommodate both perspectives. Aside from ethical reasons to incorporate patient choice, doing so leads to better outcomes: higher stages of behavior change12, stronger intention to adhere to recommendations13, faster recovery, improved emotional health, fewer diagnostic tests, and improved overall health status. 14
TLC taps into self-regulatory theories such as Bandura’s self-efficacy model 15, the theory of reasoned action of Ajzen and Fishbein16, The Transtheoretical Model17 and Motivational Interviewing (MI).18 MI is a patient centered approach that can be used by providers to help their patients prioritize behavior change goals. A core strategy of MI incorporates the concepts of importance, confidence and readiness. Rollnick argue that for someone to be ready to change they must feel both confident and that change is important to them. However, having a high level of confidence but not feeling that the change is important, or feeling that the change is important but not being confident, are presumed to be insufficient for successful change.18
While there is ample evidence for the motivational interviewing across various health behaviors19, and in clinical settings to structure brief counseling interventions10, TLC represents a novel informatics approach to motivational interviewing that enables patient assessments and the pre- activation of patients to select behavior change priorities before engaging in health behavior change conversations during the clinical encounter.
Description of the TLC intervention components
TLC integrates clinical data elements (height, weight, waist circumference, total cholesterol, HDL cholesterol, diastolic blood pressure, and systolic, diabetic) with patient assessment data to run its’ decision logic for the tailored outputs. Patient assessment consists of five standardized questionnaires pertaining to 1) diet, 2) weight 3) physical activity 4) tobacco use and 5) psychosocial issues. Each of the four behavioral assessment instruments contains from 8 to 22 multiple choice or Likert questions. For each of the four behaviors, we also assess the level of engagement in the unhealthy behavior (i.e., number of cigarettes smoked and level of nicotine dependence) as well as the patient’s transtheoretical stage of change for improving the behavior and self-efficacy in their ability to sustain the behavior change. The psychosocial issues assessment (labeled more about you) consists of 3 brief subsections: education level, and questions about financial status with reference to their ability to afford gym membership, purchase medications, purchase health foods and see a doctor. There are also questions on computer use and a brief health literacy assessment. All assessment questions were selected with consideration of quality and feasibility characteristics, such as validation, suitability to purpose, comprehensibility for patients, length, and adequate scoring algorithm.
The output report given to the patient contains four components: 1) behavioral risk and clinical risk; 2) readiness and confidence scores for changing each of the four behaviors; 3) qualitative equations to elicit patient priorities for change and 4) an action plan to affirm their behavior change priorities and goals. While the four health behaviors increase risk for many chronic diseases, focus in the output is on cardiovascular disease.
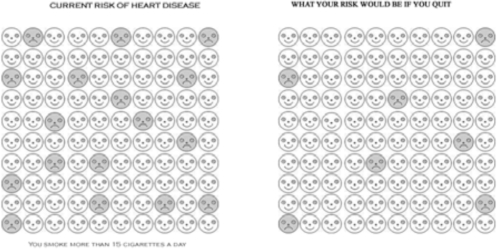
The behavioral and clinical risk section was designed to help patients understand their risk factors, and how their risk for heart disease could be reduced if they made lifestyle changes. The risk information is displayed in a visual representation (Figure 1), developed in prior research on visuals to aid low numeracy populations in parsing probability-based risk information20.
Figure 1.
Visual depiction of risk of health behavior of individual compared to risk from healthy behavior
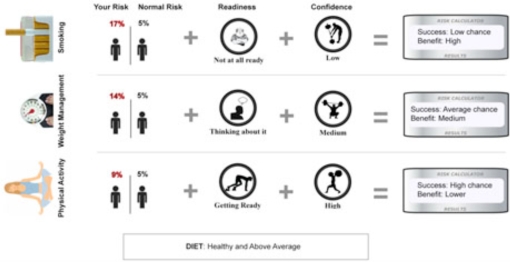
The second section visually displays the readiness and confidence of the individual for each behavior on a “ladder” to represent the progress for each behavior Summarization occurs at two levels. First, overall risk as calculated by the Framingham algorithm is presented to the patient. Second, TLC output presents a qualitative equation that combines risk, readiness and confidence. The sum in this equation is calculated based chance of success (readiness + confidence) as well as the level of health benefit the patient would achieve if they elect to work on that specific behavior. For example in Figure 2, whereas quitting smoking would produce the highest health benefit, the patient would also have the lowest chance of success in quitting at this point in time. On the other hand, although physical activity would produce the lowest benefit, they would also have the highest chance of success in maintaining regular physical activity in their lives.
Figure 2:
TLC Output Summary Equations
The report also contains two pages that serve as the “Doctors report”. These two pages contain the summary output as shown in Figure 2 and also a sheet containing “talking points”. These talking points include important behavioral points derived from the assessment (such as “patient has high fat foods and not enough fruits and vegetables).
Methods
Key informant interviews were conducted among a convenience sample of patients who lived and worked in the Washington Heights community, as well as a sample of family practice physicians who served the Washington Heights and Harlem communities through community clinics or small family practice offices (n=13). Interviewees were shown a sample TLC output based on mock patient data. Patients were asked to imagine that the output reflected their personal health information, and respond to questions accordingly. Providers were first asked to imagine that the report reflected tailored feedback on one of their patients and asked a series of questions, and were then asked to pretend that it was their own health information.
The mock health information included in the sample output included three health behaviors: quitting smoking, for which the patient would have a low chance of success (based on their low confidence and readiness for change) but would achieve a high health benefit; weight management, for which the patient would have an average chance of success and would achieve a moderate health benefit; and finally physical activity, for which the patient would have a high chance of success but the lowest health benefit (Figure 2). Patients were then asked, “If these were your personal results, which behavior would you choose to work on first?” Providers were asked this question as well as, “If this were your patient, which behavior would you want them to work on first?”
Results
Results showed a clear dichotomy in how both patients and providers approached and interpreted the decision support tool, and were almost evenly divided in their decisions. When asked which behavior they would choose, eight chose smoking (the highest benefit, lowest chance of success), while five chose physical activity (the lowest benefit, highest chance of success). Interestingly, no one chose weight management, showing a distinct divide between those who most valued the highest level of benefit to their health versus those who valued starting with a behavior they believed they could succeed in changing first. This divide was also reflected in the physician’s choice of behaviors for the patients to work on, with three choosing smoking and three choosing physical activity as their preferences for their patients’ behavior change.
Patients and providers who chose smoking as the behavior they would work on first focused on how important the behavior change would be for their health, rather than focusing on their chance of success. Many who chose smoking did not address the fact that they would have to overcome low confidence and low readiness in order to accomplish this behavior, commenting instead on how important or how big the impact would be on their health. Physicians were likely to look at the problem clinically, for example commenting, “If those were my results, I would always choose smoking cessation – smoking is the number one cause of preventable death,” while patients seemed to respond on a more “gut level” to the high risk (“I would do the smoking faster than physical activity. You have more of a survival chance if you quit first” and “Smoking would be my number one priority.”) Others did address the low success rating, and viewed it as an important barrier to overcome. One patient commented, “It’ll be hard, but it’s gonna get done.” A physician took it even further by seeing the “low chance” rating as a further incentive to choose that behavior, responding, “Me personally, I would choose smoking. I would see it as a challenge, and I would overcome it.” Similarly, another patient said, “You see the numbers, ‘low chance,’ it’s sobering… You have a low chance, but it still comes back to you. In reality, this is possible. It can be done. It should be done.”
Those who chose physical activity described this behavior change as a stepping stone to building confidence before tackling other behaviors. These respondents tended to see behavior change as an ongoing process, and recognized that all three behaviors were important to change – it was just a matter of where to start. One patient told us, “ “Even though it’s the smallest benefit, I would try to tackle something I’m ready and confident I can change first. Then maybe I’d move on to the other behaviors,” and finally another respondent noted that starting with physical activity “would help build up my confidence.”
Physicians who chose physical activity were also concerned about the consequences of the first change attempt, and how its outcomes could color their future attempts at change. They expressed worry that their patients would start trying to quit smoking and fail because they were not ready, and then become demoralized and less likely to pursue other behavioral changes. One physician told us, “I’m all about baby steps… I’d start with something I thought they could accomplish.” Another noted, “I would go for the low-hanging fruit, the easiest behavior.” Another physician viewed the chance of success as a proxy measure for motivation as well, and viewed the decision support tool as way to hone in on the area in which the patient was most motivated to change. This physician said, “Here the most motivation is in exercise, so I would really push that up. I would get them to come back in [to the office] and reinforce that [behavior change]. If they get into the exercise, even though the benefit is lower, they can do it… Once you get them moving they’re going to see changes in their weight and they’ll see they’ll feel a lot better if they stop smoking too.”
Though physicians were split evenly on the behavior they would want their patients to work on, in our sample they were also more inclined to choose smoking as the behavior they would work on for themselves. This may be because physicians are highly educated on the risks of smoking, and see firsthand the deadly consequences of this behavior in their patients. Another explanation may be that since physicians are primed to appreciate delayed gratification – through the process of their education – they may be more apt to risk significant hardship now (the difficulty of quitting cigarettes) for the promise of an even greater benefit in the distant future (reduced risk of heart disease and lung cancer 10 or 15 years from now).
Patients and providers were also asked to comment on how helpful the information provided in the decision support tool (risk/benefit level, readiness, confidence & chance of success) would be in making a choice about behavior change. All of the respondents, among both patients and providers, thought the tool would be useful in the decision-making process in some way, but they differed on the reasoning for how it would help. Many of the respondents thought the tool was useful in its clear, concrete conceptualization of factors that would influence their decision. Respondents recognized that most smokers know that this behavior puts them at high risk, but seeing the information laid out visually and directly, in a personalized way, made it more salient. “They could tell you you’re gonna die in two weeks, but when you see it [on paper like this], it’s another story,” said one patient. “It’s sobering. Answering questions doesn’t mean you see that… Seeing this [the report] is very concrete,” said another. A provider added, “In the course of a visit we are mentally thinking of these things. Here it’s very clearly visualized and conceptualized. It would save a lot of time; it gives you everything right up front and helps you know how to approach it.”
Others thought the importance of the decision support tool was not in the risk and readiness details themselves, but in the process that the tool would enable. One patient commented that the tool was helpful because it would actually get them thinking about all of these behaviors in a concrete way. A provider, when discussing which behavior should be chosen, made the observation, “I’m not sure it matters though– it matters that they choose something.” The decision support tool becomes not just an informational tool then, but also a jumping off point for an important conversation that needs to happen between a patient and his or her provider. One provider commented that it is “almost like a contract,” in that it documents the conversation about behavioral risks, which the provider speculated would be more powerful than his verbal recommendation alone, since that could easily be forgotten or ignored.
The final element we explored in the interviews with physicians was how TLC might change the dynamic of a behavioral counseling session. The goal of the tool is to foster more of a conversation, rather than provider-driven, top-down advice without patient input. We sought to explore provider’s reactions to the idea that the patient would provide the primary direction around where the behavior change conversation would start. To understand reactions to this shift, we asked providers, “If your patient chose to work on a different behavior than the one you wanted them to work on, what would you say?”
In response, most physicians embraced the patient preference model, believing that the behavior change discussion should be driven by the patient’s beliefs, motivations and values. Two providers took a complete patient-centric approach, giving the patient the reins in deciding which health behaviors to pursue. One of these providers had very strong feelings about the importance of tobacco cessation counseling, even when the success rate for change is low, but when it came to patient preference she commented, “I would gear it towards what the patient is most focused on working on. Gear everything toward the patient’s needs and desires,” rather than pushing her preference to start with tobacco cessation. Several other providers described a shared decision-making approach, primarily driven by patient preference but also allowing them the opportunity to mention other risks. For example, one provider responded, “If they were my patient’s results and they chose one of the other activities, I would support their choice. But I would still at least mention smoking cessation at their visits.”
Conclusion
This study provides preliminary evidence that a behavior change decision support tool based on risk, readiness and confidence may be an effective method to help patients choose a behavior change plan that most appropriately suits their values and psychosocial attributes, while also facilitating a more productive conversation with their provider. However, this study employed hypothetical scenarios and this may have influenced their choices. We are currently doing a preliminary validation study with 30 patients and their providers.
The dichotomous results in behavior change preference suggest that there are two very different approaches to health behavior change: the approach that focuses almost exclusively on the level of benefit the behavior change would afford in the future versus the approach that focuses on chance of success in the present and the ability to build confidence for future successes. The wide variety of responses suggests that a personalized tool emphasizing patient preference would be effective, since it would allow the patient to approach behavior change in a way that best suits their own values and perspective on lifestyle changes. The preliminary feedback also suggests that the tool would positively affect the dynamic in the behavior change discussion between patient and provider.
References
- 1.Whitlock EP, Orleans CT, et al. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–84. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 2.Koop EC. Health promotion and disease prevention in clinical practice. In: Lawrence RS, Woolf SH, Jonas S, editors. Health promotion and disease prevention in clinical practice. Williams & Wilkins; Baltimore, MD: 1996. pp. vii–ix. [Google Scholar]
- 3.US Preventive Services Task Force Guide to clinical preventive services. 2nd ed. Williams & Wilkins; 1996. [Google Scholar]
- 4.Partnership for Prevention . Why invest in disease prevention? Partnership for Prevention; Washington, DC: 1999. [Google Scholar]
- 5.Wee CC, McCarthy EP, Davis RB, Phillips RS.Physician counseling about exercise JAMA 19992821583 8. [DOI] [PubMed] [Google Scholar]
- 6.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 7.Thorndike AN, et al. Rates of U.S. physicians counseling adolescents about smoking. J Nat Cancer Inst. 1999;91(21):1857–62. doi: 10.1093/jnci/91.21.1857. [DOI] [PubMed] [Google Scholar]
- 8.Stafford J, et al. Electronic Health Record Use and the Quality of Ambulatory Care in the United States”. Arch Intern Med. 2007;167(13):1400–1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 9.Solomon MR. Information Technology to Support Self-Management in Chronic Care: A Systematic Review. Disease Management & Health Outcomes. 2008;16(4):391–401. [Google Scholar]
- 10.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 11.Levenkron JC. Patient priorities for behavioral change: selecting from multiple coronary disease risk factors. J Gen Int Med. 1988;3(3):224–229. doi: 10.1007/BF02596336. [DOI] [PubMed] [Google Scholar]
- 12.O'Connor PJ, et al. Professional advice and readiness to change behavioral risk factors among members of a managed care organization. Am J Manag Care. 2001;7(2):125–30. [PubMed] [Google Scholar]
- 13.Street RL, et al. 2008 Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart M, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;(49):796–804. [PubMed] [Google Scholar]
- 15.A Bandura Social foundations of thought and action: a social cognitive theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 16.Ajzen I, Fishbein M. Understanding attitudes and social behavior. Prentice-Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- 17.Prochaska JO, Di Clemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 18.Rollnick S, et al. Health behavior change: a guide for practitioners. Churchill Livingston; Edinburgh, Scotland: 1999. [Google Scholar]
- 19.Martins K. Review of motivational interviewing in promoting health behaviors. Clinical psychology review. 2009 doi: 10.1016/j.cpr.2009.02.001. In Press. [DOI] [PubMed] [Google Scholar]
- 20.Ancker J, Senathirajah Y, Kukafka R, Starren J. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc. 2006;13(6):608–18. doi: 10.1197/jamia.M2115. [DOI] [PMC free article] [PubMed] [Google Scholar]