Abstract
The discharge planning process can be successful when information is shared among the patient, caregiver, and provider from admission through post discharge. The objective of this paper was to evaluate the association of information sharing among patients, caregivers, and health care providers and the impact on the discharge process. The authors identified reports of the discharge planning process through systematic electronic database searches. The eligibility criteria were 1) usual discharge planning process, and 2) patient, caregiver, or provider perception or feedback. Of the eligible articles, all voiced concern about a broken discharge planning process that affected the information exchanged among all involved in patient care. Outcomes related to satisfaction, knowledge transfer, and communication were identified. The initial evidence suggests information sharing through interdisciplinary patient care can play a significant role in the future.
INTRODUCTION
There were 38 million hospital discharges in the United States in 2003, at a total cost of over $753 billion.1 The hospital discharge process is poorly standardized and is characterized by discontinuity and fragmentation of care. In addition, many processes place patients at high risk of post discharge adverse events and rehospitalization: lack of coordination in the handoff 2 from the hospital to community care, social support gaps, high rates of low health literacy, and poor delineation of discharge responsibilities among hospital staff. 3
Sometimes it seems as though discharge from the hospital happens all at once, and in a hurry. Discharge planning is a process, not a single event. Medicare defines discharge planning as: “A process used to decide what a patient needs for a smooth move from one level of care to another.” 4
The objective of this paper was to evaluate the association of information sharing among patients, caregivers, and health care providers and the impact on the discharge process. The authors systematically reviewed articles to evaluate the impact of the lack of a viable discharge planning process on health outcomes. This review is a preliminary step to a larger project.
METHODS
Data Sources
The authors searched MEDLINE (1998-present) and CINAHL (1995-present) for relevant studies using combinations of the following search terms: (i) patients (MeSH), caregivers (MeSH), health care personnel (MeSH); (ii) discharge planning (MeSH), patient discharge (MeSH), hospitals (MeSH); (iii) case management (MeSH), patient care team (MeSH), interdisciplinary communication (MeSH), delivery of care (MeSH); and (iv) clinical audit (MeSH), healthcare quality assessment (MeSH). The authors also systematically searched the reference lists of included studies and relevant reviews.
Inclusion and Exclusion Criteria
The inclusion criteria were any articles evaluating the discharge planning process with outcomes related to satisfaction, knowledge transfer, and communication. The excluded studies are those that were not published in English, published prior to 1995, or did not involve a usual discharge planning process.
Study Selection and Data Extraction
The authors reviewed the titles and abstracts of the identified citations and applied a screening algorithm based on the inclusion and exclusion criteria described above. The two investigators rated each paper as “potentially relevant” or “potentially not relevant.” The authors collected the following information from each “potentially relevant” article: patient sample, methods, outcome measures, and conclusions. The authors grouped the outcomes by satisfaction, knowledge transfer, and communication.
RESULTS
Comprehensive literature searches identified 60 articles. After reading the full articles, 50 articles were excluded. Ten articles met the eligibility criteria. 5–14 (Table 1)
Table 1.
Eligible Discharge Planning Studies
| Authors | Sample | Methods | Conclusions |
|---|---|---|---|
| Armitage S et al.5 | 29 chronic cardiology and respiratory patients | Semi-structured telephone interview; 20–90 minutes to complete; qualitative / quantitative format; completed post discharge at home (5–36 days) | Delays waiting on medication and letters No written information regarding their condition and prognosis; Short term (3 days) medication supply was not enough; Poor warning regarding discharge times given to family; Patient not prepared to manage at home |
| Atwal A6 | 9 orthopedic nurses; 6 acute medicine nurses; 4 elder care nurses | Case study design interview and direct observation study; 30–90 minutes to complete; critical incident approach format; nonparticipant approach format; 45–60 minutes to complete; completed 12 months post-discharge | Time restraints --Discharge aspects ignored, neglected and rarely co-ordinated; Handoff hindered communication |
| Bull M et al.7 | 139 congestive heart failure family caregivers | Telephone and face-to-face interviews; 40–50 minutes to complete; longitudinal design-client satisfaction (8 items) and continuity of care questionnaire (12 items); completed pre-discharge (baseline) and post discharge (2 weeks & 2 months) | Lack of involvement -- Low scores on satisfaction; Feelings of preparedness; Perception of care continuity; Less acceptance of role |
| Burkey Y et al.8 | 45 patients | Semi-structured or in-depth pilot interviews; qualitative format; completed post discharge (2 weeks & 3 months) | Discharging doctor did not know them Vague about reason for discharge, condition and future care; Patient input ignored |
| Clemens E 9 | 37 caregiver-discharge planners; 3 patient-discharge planners | Survey questionnaire & face-to-face interview; 60–90 minutes to complete; open/closed ended format; completed post discharge (1 week) | Very little or no information received; Too few choices or no choice at all |
| Clever S et al. 10 | 3123 patients | Face-to-face interview & surveys; 15 minutes & 10 minutes completion time; qualitative format (30 items) & quantitative format (20 items 5-point scale); completed pre-discharge (baseline) & post discharge (1 month) | Positive relationship between overall satisfaction and overall ratings of physicians’ communication behaviors |
| Tyson S et al. 11 | 55 stroke patients; 176 general practitioners, hospital doctors, therapists and nurses | Patient satisfaction and staff opinion surveys (postal); Likert (13 items, 4 point scale); completed post-discharge (0–6 weeks) | Dissatisfied – Poor level of service; Poor communication between staff and patient/caregivers; Liaison between staff, and narrow focus of rehabilitation; Support received from community services; Information received |
| Tennier L et al. 12 | 81 clinicians; 15 mangers/administrators | Generic and social worker questionnaires (internal mail) & face-to-face interview; 30 minutes to complete; descriptive design; completed post discharge (0–2 weeks) | Discharge date not predicted in advance; Lack communication, coordination documentation, clear hospital policy and palliative and long term care resources; Community resources expensive and not often inaccessible to families; Patient and family not adequately informed; Failure to include patient and family |
| Watts R et al. 13 | 12 registered nurses | Semi-structured face-to-face interviews; 30–40 minutes to complete; qualitative (open ended) format; completed post discharge (2 weeks) | Communication between nursing and medical staff either enhanced or impeded; Different level of involvement perceived; Discharge plan inconsistent |
| Watts R et al. 14 | 218 critical care nurses | Semi-structured interview; 30–40 minutes to complete; explorative descriptive approach (qualitative - open ended 31 items) | No agreement on how to define discharge planning (“next level of care”); Discharge process not well understood; Discharge education needed |
These studies took place in the United States, 7–10 Australia, 5, 13–14 United Kingdom, 6,11 and Canada. 12 The discharge planning process problems are not limited to a particular local or regional area. It is an international issue. Patients were surveyed in five (5) studies (3255 patients); caregivers were surveyed in two (2) studies (176 caregivers); and health care providers were surveyed in six (6) studies (521 providers). Patients, caregivers and health care providers are invaluable stakeholders; therefore, possessing a vested interest in creating a strong information sharing and real-time communication environment.
All articles involved cross-sectional or survey methods. Ten (10) articles used face to face or interview survey methods; two (2) articles used telephone surveys; and two (2) articles use paper and pencil surveys. The length of time it took to complete the surveys ranged from 10 minutes to 90 minutes. The number of survey items ranged from 12 to 31. Three (3) studies indicated they used an open / closed format of questions. The discharge questionnaires were administered from pre-discharge (baseline) to post discharge (up to 12 months).
Twenty-three (23) different outcomes were measured in the eligible articles (Table 2). The number of outcomes per article ranged from 1 to 4. Of the types of outcome measures, seven (7) measured satisfaction (30.4%),5–9,13–14 (ten) 10 measured knowledge transfer (43.5%),5,7–8,10,12,14 and six (6) measured communication (26.1%).7,9–10.12–14
Table 2.
Outcome Measures
Satisfaction |
Knowledge transfer |
Communication |
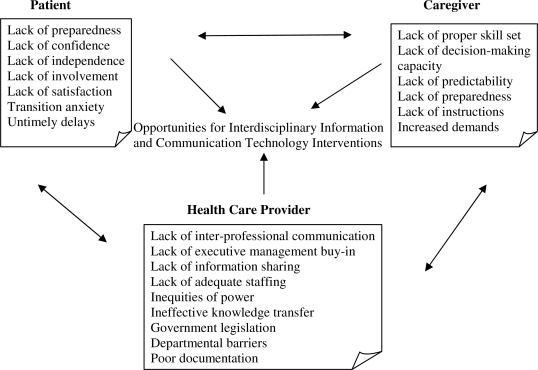
Many factors affect the discharge process for patients, caregivers, and health care providers. These factors that lead to opportunities for interdisciplinary information and communication technology interventions are presented in Figure 1.
Figure 1.
Factors Impacting Satisfaction, Knowledge Transfer, and Communication in the Discharge Process
DISCUSSION
In this systematic review, the authors analyzed the discharge planning process by measuring health outcomes evaluated in the eligible articles. In 2001, the Institute of Medicine (IOM) 15 outlined six overarching “Aims for Improvement” for health care (shown in italics below). These are tangible benefits that can be realized if information sharing and communication occurs as part of an efficient and effective discharge planning process.
The organization’s benefits are: (1) resource utilization is more efficient and leads to higher quality of life, (2) value-added service delivery among the local community by building team relationships, (3) patient, caregiver and health care provider satisfaction, and (4) evidence based medicine or standard protocols are adhered and provide more seamless patient care transitions.
The patient’s benefits are: (1) gaps or needs in the care process are identified and addressed earlier (2) patient empowerment or preferences in an informed decision-making process to maximize independence (3) stronger possibilities of adherence of the proposed care plan (4) consumer driven health care (5) continuum of equitable care ensures better health outcomes and safe environment.
The caregiver’s benefits are: (1) relationships are strengthened and feel valued as partners, (2) appropriate information input heightens future patient care and warrants additional community support, and (3) choices regarding their role and responsibilities.
The health care provider’s benefits are: (1) expertise knowledge willingly shared and allows patient-centered care, (2) disseminate key information in a timely manner, and (3) precise role delineation and effective discharge planning.
In 2000, Joint Commission on Accreditation for Health Care Organizations (JCAHO) Standards mandated interdisciplinary care in the standards on Care of Patients and Continuum of Care.16 The time spent working in individual disciplines or departmental silos has caused detriment and hindered the “whole patient” approach associated with discharge planning process. Upon establishing a seamless standardization protocol by information sharing and communication, the perceptions or satisfaction by the patient, caregiver and health care provider will build confidence and rapport.
Information sharing helps to bridge boundaries, mend fragmentation of roles and responsibilities, minimize inter professional conflict, encourage idea exchanges, decrease duplication of effort, increase pooling of knowledge, maximize smoother transitions or handoffs, heighten clinical input and decrease gaps and problems in patient care, and unify hospital protocol awareness. Communication helps breaks down professional barriers, plan care coordination better, change stagnate professional and organizational culture, build inter relationships among all involved in patient care, delineate roles and responsibility, encourage patient and caregivers active involvement, promote accurate and clear documentation, maximize timely discharge planning, minimize fragmented discharge planning, and inspire respectful professional behaviors.
Well-coordinated collaboration across professions has the potential to allow comprehensive, population-based, cost-effective patient care and a new emphasis on health promotion and disease prevention, essential in meeting contemporary health care challenges. 17 The ultimate patient-centered goal is to provide the right time, right place, 18 right care, right information, right communication and right solution.
Acknowledgments
This research was supported by the National Library of Medicine (Grant # 5T15LM007087-18).
REFERENCES
- [1].Jack B, Greenwald J, Forsythe S, et al. Developing the tools to administer a comprehensive discharge program: the reEngineered discharge (RED) programAvailable at http://www.ahrq.gov/downloads/pub/advances2/vol3/Advances-Jack_28.pdf Accessed February 10, 2009. [PubMed]
- [2].Pantilat SZ, Lindenauer PK, Katz PP. Primary Care Physician attitudes regarding communication with hospitalists. Dis Mon. 2002;48:218–229. doi: 10.1016/s0011-5029(02)90029-5. [DOI] [PubMed] [Google Scholar]
- [3].Weissman JS, Stem R, Fielding SL, et al. Delayed access to healthcare: risk factors, reasons and consequence. Ann Intern Med. 1991;114:325–331. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- [4].Caregiving Organization A Family Caregiver Guide to Hospital Discharge PlanningAvailable at http://www.caregiving.org/pubs/brochures/familydischargeplanning.pdf Accessed November 20, 2008.
- [5].Armitage SK, Kavanagh KM. Consumer-oriented outcomes in discharge planning: a pilot study. Journal of Clinical Nursing. 1998;7(1):67–74. doi: 10.1046/j.1365-2702.1998.00136.x. [DOI] [PubMed] [Google Scholar]
- [6].Atwal A. Nurses’ Perceptions of Discharge Planning in Acute Health Care: A case study in one British teaching hospital. Journal of Advanced Nursing: Issues and Innovations in Nursing Practice. 2002;39(5):450–458. doi: 10.1046/j.1365-2648.2002.02310.x. [DOI] [PubMed] [Google Scholar]
- [7].Bull MJ, Hansen HE, Gross CR. Components of a proper hospital discharge for elders. Journal of Advanced Nursing. 2000;35:571–581. doi: 10.1046/j.1365-2648.2001.01873.x. [DOI] [PubMed] [Google Scholar]
- [8].Burkey Y, Black M, Reeve H. Patients’ view on their discharge from follow up in outpatient clinics: qualitative study. BMJ. 1997;315:1138–1141. doi: 10.1136/bmj.315.7116.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Clemens E. Multiple perceptions of discharge planning in one urban hospital. Health & Social Work. 1995;20(4):254–262. doi: 10.1093/hsw/20.4.254. [DOI] [PubMed] [Google Scholar]
- [10].Clever SL, Jin L, Levinson W, Meltzer DO. Does doctor-patient communication affect patient satisfaction with hospital care? Results of a analysis with a novel instrumental variable. Health Service Research. 2008;43(5):1505–1519. doi: 10.1111/j.1475-6773.2008.00849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tyson S, Turner G. Discharge and follow-up for people with stroke: what happens and why. Clin Rehabil. 2000;14:381–392. doi: 10.1191/0269215500cr331oa. [DOI] [PubMed] [Google Scholar]
- [12].Tennier L. Discharge planning: an examination of the perceptions and recommendations for improved discharge planning at the Montreal General Hospital. Social Work Health Care. 1997;26(1):41–60. doi: 10.1300/J010v26n01_03. [DOI] [PubMed] [Google Scholar]
- [13].Watts R, Gardner H. Nurses’ perceptions of discharge planning. Nursing and Health Sciences. 2005;7:175–183. doi: 10.1111/j.1442-2018.2005.00229.x. [DOI] [PubMed] [Google Scholar]
- [14].Watts RJ, Pierson J, Gardner H. How do critical care nurses define the discharge planning process? Intensive and Critical Care Nursing. 2005;21:39–46. doi: 10.1016/j.iccn.2004.07.006. [DOI] [PubMed] [Google Scholar]
- [15].Institute of Medicine Crossing the Quality Chasm; A New Health System for the 21st CenturyAvailable at http://www.iom.edu/Object.File/Master/27/184/Chasm-8pager.pdf Accessed February 10, 2009.
- [16].Halm MA, Goering M, Smith M. Interdisciplinary rounds: Impact on patients, families, and staff. Clinical Nurse Specialist. 2003;17(3):133–142. doi: 10.1097/00002800-200305000-00013. [DOI] [PubMed] [Google Scholar]
- [17].Health Resources and Services Administration Bureau of Health Professions and Interdisciplinary Teamwork in HealthcareAvailable at http://www.med.unc.edu/epic/module4/m4to.htm/ Accessed February 10, 2009.
- [18].Steen P. The most appropriate health care in the right place, at the right time. Home Care Provider. 1998;3(1):25–27. doi: 10.1016/s1084-628x(98)90152-6. [DOI] [PubMed] [Google Scholar]