Abstract
Heart failure patients require complex, long-term care. Research shows that self-care education improves health outcomes of these patients. This study reports the results of a randomized trial which compared the effects of two remote educational interventions on heart failure patients’ knowledge of self-care practices. The first group reviewed self-care content on a Web site and had email access to a cardiac nurse. The second group had access to the Web site, and participated in four telephone-based sessions with the cardiac nurse. The test scores of both groups significantly improved following the intervention. However, the post-intervention test scores of the group that included telephone sessions were significantly higher than the scores for the group that had access to the Web site only. These results show a benefit to learning of a teleconferencing intervention that is over and above the benefit of an intervention based on Web information and email access alone.
Introduction
Heart failure is the most common cause of hospitalization for adults over the age of 65 years: the estimated number of those afflicted in North America exceeds five million1. Approximately 59% of men and 45% of women with heart failure will die within five years of the first onset of the symptoms2. Additionally, 54% of these patients will be readmitted to the hospital within 6 months of initial discharge3. Persons with heart failure require lifelong monitoring, and must make complex lifestyle changes in order to prevent their condition from worsening and to avoid being readmitted to hospital. Many strategies attempt to reduce the complexities associated with long-term care of heart failure patients. Most, such as disease and case management interventions, involve multiple medical roles in patient care or dedicated additional resources to patient monitoring and discharge planning. By contrast, self-care or self-management strategies aim to strategically reduce the involvement of medical professionals, and to enable patients to assume care of their condition.
Health Canada defines self-management as: “decisions and actions taken by someone who is facing a health problem or issue in order to cope with it and improve his or her health”4. Self-management interventions may involve teaching patients to monitor symptoms, administer medication and recognize when to seek help. According to the definition of health informatics, self-management interventions may also employ information and communication technologies5. As documented below, self-management interventions have been shown to improve health outcomes of patients with heart failure. Given that self-management can be effective, the associated health informatics research questions concern how, when, and to whom to deliver health informatics applications designed to promote better self management.
The research presented below contrasts two educational interventions for heart failure patients. In this research, we test the hypothesis that teleconferencing with other patients and a cardiac nurse improves self-management knowledge more than an intervention that involves Web information and email access alone. Finding a statistically significant benefit to adding teleconferencing to the intervention in this case would provide scientific support for the use of teleconferencing to promote self-management of heart failure patients, with the ultimate aim of reducing the number of readmissions and thus the overall cost of care for these patients.
Background
Our previous systematic review has demonstrated that self-management interventions improve health outcomes of patients with heart failure6. The study showed a reduction in the number of hospitalizations both for heart failure and for all causes. The intervention was shown to have the potential to prevent one out of seven readmissions that were due to heart failure. The importance of structured self-management education was also highlighted in a systematic review7, and a meta-analysis of 21 studies8 which sought to identify components of interventions that improved health outcomes.
Although information technologies have the capacity to deliver self-management education to patients afflicted with conditions that require complex care, their use for this purpose has remained relatively unexplored. For example, only one randomized controlled trial of self-management education for heart failure patients was identified at the time of this study9; it did not improve health outcomes. In addition, most previous research involving remote communication technologies (typically telephone) focused on enabling physicians to monitor patients’ vital signs, as reported in two systematic reviews3,10. However, physician-led approaches are not consistent with the principles of self-management.
The study reported in this paper sought to cast further light on the issue of whether or not remote education can lead to improvements in patient self-management by delivering self-management education remotely using validated educational content.
Method
The study compared two methods of self-care education for heart failure patients. The “Web group” had access to a Web site with educational content and had email access to the cardiac nurse. The “Live group” had access to the Web site and the cardiac nurse, but also had four additional telephone-based sessions that covered the same educational content.
Knowledge about heart failure management was assessed at baseline and following the intervention using a validated self-care test11. The test had been selected by the study team by consensus following a literature review of relevant knowledge tests.
The educational content was adapted from the Heart Failure Society of America’s self-care education modules for patients with heart failure12. The content was modified to a Grade 8 reading level and revised to include metric measures, consistent with Canadian standards. The resulting content was incorporated into the study Web site. The Web site was reviewed for usability using the heuristic evaluation method13. Heuristic evaluation was conducted by four usability experts, consistent with the research-based principles of discount usability engineering14. A medical team consisting of two physicians and a cardiac nurse reviewed the overall content prior to use with patients.
Patients 18 years of age or older diagnosed with congestive heart failure were recruited from the University Health Network (UHN) hospitals, Sunnybrook Hospital, Toronto Rehab institutes (all in Toronto), and the Trillium hospital in Mississauga, Ontario, Canada. Consistent with the UHN ethics guidelines, patients were recruited through advertisements posted in hospital common areas. Advertisements were also posted on two Toronto-based community web sites. Participants who reported a diagnosis of congestive heart failure, were able to communicate in English, and had access to a personal computer equipped with Internet access were eligible to participate in the study. Patients who were cognitively impaired, as assessed by the Short Portable Mental Status Questionnaire15, were excluded from the study if they answered one or more questions incorrectly. One patient was excluded for this reason.
A statistician determined a randomization schedule using permuted blocks that were not known to the investigators. A randomized sequence was generated for each site from which participants were recruited in order to ensure that the patient allocation was balanced for each site. Sealed individual opaque envelopes were used to conceal the allocation sequence. Patients who consented to participate were assigned to one of the two study groups, based on the next number in the randomized sequence. The study team (education provider, data assessor) remained blinded to participant allocation until the end of the study. A research assistant randomly assigned the patients who consented to participate, and who met the inclusion criteria, to a Web or a Live group. The study information and the initial data collection forms were mailed to the patients after their consent was obtained. The patients had to return the consent form and the completed baseline self-care knowledge test prior to being given access to the study Web site and, if applicable, prior to the start of the live (teleconferencing) intervention. The responsiveness rating of the test (0.75) was used to calculate the required sample size of 38 participants16.
Participants in the Web group were asked to review, over a period of two weeks, the educational content on self-care, which was posted on the study web-site. One week into this period, the participants were reminded that one week remained to review the material. Participants in the Live group attended four teleconference educational sessions led by a cardiac nurse. The sessions were held twice a week for two weeks. They consisted of the nurse’s presentation on two self-care topics and a question-and-answer period following each topic. Participants in the Live group had access to the same Web site as the Web group. All participants were able to email questions to the cardiac nurse at any time.
The second knowledge test was mailed one week following the intervention, along with a series of statements about the study. Patients were asked to indicate their level of agreement with the statements on a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree). Following the receipt of the second knowledge test, participants were contacted by telephone and additional feedback on the study was solicited.
Baseline knowledge scores between the two groups were compared using a t-test in order to determine whether the groups differed at baseline. Post-intervention scores for each group were compared using paired t-tests. An unpaired t-test was used to compare the differences between the pre- and post-intervention scores between the two groups.
Results
A total of 31 participants was enrolled in the study. All but two of the participants had a personal computer, used email and had internet access; two participants used a friend’s computer or public library. The average age of participants was 50.25. Seven participants had a high school degree or less, 21 participants had completed some or all of university or college, and three had postgraduate education. Three participants withdrew prior to completion of the study (one from the Live and two from the Web group).
The scores of the two groups were not significantly different at baseline, as assessed using a t-test (p = 0.50). Paired t-tests were used for each of the groups (Live, and Web) to determine if scores improved significantly from the first to the second test.
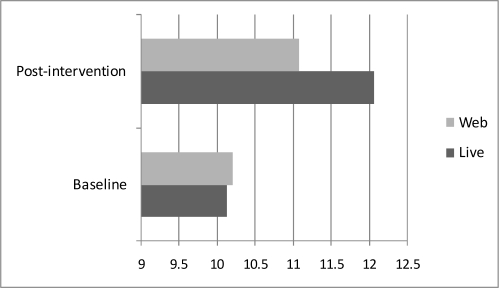
Mean post-intervention scores of the Live group participants (12.06) were significantly higher (t[15]=4.29, p<.001)) than the corresponding mean of baseline scores (10.125). Mean post-intervention scores were also significantly higher (t[14]=2.1, p<.05)) than the corresponding mean baseline scores in the Web group (10.20 vs. 11.07). The score improvement was significantly higher (t[29]=1.72, p<.05)) in the Live group (1.94) than in the Web group (0.87). The differences in the test scores among the two groups are summarized in the Figure 1.
Figure 1.
Test score improvement in two groups (scores out of 14)
The participants who completed the study were also asked to rate their level of agreement with a series of statements on a 5-point Likert scale. Mean scores were calculated from the returned questionnaires (29 in total), and the scores between the two groups were compared using unpaired t-tests. Correlations between the feedback and the study variables were also computed. The Live group had a significantly higher (p<0.05) mean rating of agreement with the statement “I got a response to most of my queries about heart failure.” (Live: 4.38; Web: 3.92) The Live group also had a higher mean agreement with the statement “I have already implemented several things which I learned in this study in my own self care”; the difference approached statistical significance (Live: 4.33, Web: 3.75; p=0.06).
There was no significant difference between the groups in the ratings of the following statements:
“I felt I could trust the educational material in the study web site” (Live: 4.82; Web: 4.67, p=0.41)
“This study did not teach me anything new” (Live: 2.08; Web: 2.08, p=0.49)
“This study only left me more concerned about my health” (Live: 2.54; Web: 2.17; p=0.24)
“I would rather take advice from a doctor than a web site” (Live: 2.54; Web: 2.17; p=0.40)
“What I learned in this study was useful to me personally” (Live: 4.25; Web: 4.08; p=0.22), and
“This kind of education was appropriate for patients with heart failure” (Live: 4.25; Web: 4.17, p=0.35).
Participation rates among the two groups were compared. The Live group participated more extensively in the study than the Web group, as expressed in terms of the number of questions, emails and accesses to the Web site. While the Live group sessions involved many questions and discussions, only two questions were emailed by the participants in the Web group. From the post-intervention comments, it appears that the group learning experience and the ability to seek personalized advice motivated the participants in the Live group to engage more actively with the study material. By contrast, Web group participants commented that they did not email any questions to the nurse because they had no relevant questions, or because the Web site content was sufficiently clear.
Discussion
The results indicate that knowledge scores of both groups increased significantly after the intervention. The increase in scores of the Live group was significantly higher than the increase in the Web group. However, the increases in both groups were limited to 1 or 2 points, which may be due to the higher baseline scores (10.2 out of 14) and the test’s potential “ceiling effect”11. When the results for which baseline scores were within 2 points of the maximum were removed from the analysis, the difference in the improvement in the live group scores was greater with the mean improvement being 2.73 (p=0.02). This suggests that the patients who stand to benefit most from the intervention are those who score lower on the baseline test.
Since live educational sessions facilitate discussions more easily than email communication, it was expected that more patients in the Live group than in the Web group would rate the study information as “useful to them personally”. However, level of agreement with this statement did not significantly differ between the groups.
Participants in both groups indicated that they had implemented several strategies that they had learned in the study in their own self-care. Examples include following weighing guidelines, paying attention to sodium content of foods and salt substitutes, restricting fluid intake, keeping track of symptoms, avoiding exertion that puts strain on the heart, and discussing care options with healthcare practitioners. These statements could not be independently verified.
Credibility of information found on the Internet has been frequently questioned. Since the participants were aware that the content in this study was prepared by a medical team, trustworthiness scores may not be the same as those for medical Internet sites in general. In the context of this study, it was expected that participants would rate information on the study Web site as very trustworthy. The results were consistent with this expectation: the mean ratings for the Live and the Web group were 4.82 and 4.67 out of 5 respectively.
The patients also indicated that they were open to Web-based learning. The participants in the Web group disagreed with the statement that such educational approaches were inappropriate. In addition, the participants indicated that they would trust the information on a web site to which their physician referred them.
It should be noted that participants in the study tended to be younger and likely more highly educated than heart failure patients in general. The average age of study participants was 50.13, while the average age of heart failure patients across the Canadian province of Ontario is 75.817. The results therefore may not be generalizable to the entire population of patients with heart failure, but are likely relevant to those who are comfortable using a computer and Internet.
One important consideration is that more Live group participants than Web group participants indicated that they had adopted the newly learned self-care practices. When contacted for feedback on the study, these patients commented that other participants’ questions helped them to consider new issues, or to consider an existing issue from a new angle. They also commented that other patients’ experiences with certain medications or treatments helped them to make decisions about their own care. Several patients indicated that they had a better understanding of their symptoms and the appropriate response. These comments may illustrate a potentially important component of learning that is absent from Web-based education.
Conclusion
This paper presents the results of a randomized trial which compared the effects of two types of online educational interventions on heart failure patients’ knowledge of self-care practices. The results indicate that the test scores of the Live group participants and the Web group participants significantly improved following the intervention, but the increase in test scores was significantly higher in the Live than in the Web group. Patients in both groups adopted some of the suggested strategies in their own self-care. These results should provide useful information to decision-makers who need to devise educational interventions for heart failure patients.
Acknowledgments
The authors would like to thank Vaska Micevski for her contribution in running the patient education sessions in this study.
References
- 1.Smith ER. Heart failure – are we making progress? Can J Card. 2002;18:1124–25. [PubMed] [Google Scholar]
- 2.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KKL, Murabito JM, Vasan RS. Long term trends in the incidence of and survival with heart failure. New England J Med. 2002;347(18):1397–402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 3.Louis AA, Turner T, Gretton M, Baksh A, Cleland JGF. A systematic review of telemonitoring for the management of heart failure. Eur J Heart Fail. 2003;5:583–90. doi: 10.1016/s1388-9842(03)00160-0. [DOI] [PubMed] [Google Scholar]
- 4.Health Canada Supporting self-care: The contribution of nurses and physicians: An exploratory study. URL: http://www.hcsc.gc.ca/hppb/healthcare/pubs/selfcare/index.htm l (Accessed Sept 2005).
- 5.Bath PA. Health informatics: current issues and challenges. J Info Sci. 2008;34:501–18. [Google Scholar]
- 6.Jovicic A, Holroyd-Leduc JM, Straus SE.Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomised controlled trials BioMed Central Cardiovasc Dis 2006. 6:43. URL: http://www.biomedcentral.com/1471-2261/6/43 (Accessed Jul 2009). [DOI] [PMC free article] [PubMed]
- 7.Windham BG, Bennet RG, Gottlieb S. Care management interventions for older patients with congestive heart failure. Am J Managed Care. 2003;9(6):47–59. [PubMed] [Google Scholar]
- 8.Yu DS, Thompson DR, Lee DT. Disease management programmes for older people with heart failure: crucial characteristics which improve post-discharge outcomes. Eur Heart J. 2006;27(5):596–612. doi: 10.1093/eurheartj/ehi656. [DOI] [PubMed] [Google Scholar]
- 9.Ross SE, Moore LE, Earnest ME, Wittevrongel L, Chen-Tan L. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res. 2004;6(2):e12. doi: 10.2196/jmir.6.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: The evidence base. J Am Med Inform Assoc (JAMIA) 2007;14:269–77. doi: 10.1197/jamia.M2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gwadry-Sridhar F, Guyatt GH, Arnold MO, Massel D, Brown J, Nadeau L, Lawrence S. Instruments to measure acceptability of information and acquisition of knowledge in patients with heart failure. Eur J Heart Fail. 2003;v. 5:783–91. doi: 10.1016/s1388-9842(03)00158-2. [DOI] [PubMed] [Google Scholar]
- 12.Heart Failure Society of America Heart failure education modules. URL: http://www.hfsa.org/hf_modules.asp
- 13.Nielsen J. Usability Engineering. Academic Press; Boston, Massachusetts: 1993. [Google Scholar]
- 14.Nielsen J, Landauer TK. A mathematical model of the finding of usability problems; Proc ACM/IFIP INTERCHI’93 Conf; 1993. pp. 206–13. [Google Scholar]
- 15.Pfeiffer E. A short portable mental status questionnaire for assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;10:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 16.Guyatt G, Walter S, Norman G. Measuring change over time: Assessing the usefulness of evaluative instruments. J Chronic Dis. 1987;v40(2):171–6. doi: 10.1016/0021-9681(87)90069-5. [DOI] [PubMed] [Google Scholar]
- 17.Institute for Clinical and Evaluative Sciences (ICES) ‘Precious time’: Scientists discover how long heart failure patients are expected to live. Online resource. URL: http://www.biomedicine.org/medicine-news-1/Precious-Time---Scientists-discover-how-long-heart-failure-patients-can-expect-to-live-11662-1/ (Accessed April 4, 2008).