Abstract
How does paper usage change following the introduction of Computerized Physician Order Entry and the Electronic Medical Record (EMR/CPOE)? To answer that question we analyzed data collected from fourteen sites across the U.S. We found paper in widespread use in all institutions we studied. Analysis revealed psychological, ergonomic, technological, and regulatory reasons for the persistence of paper in an electronic environment. Paper has unique attributes allowing it to fill gaps in information timeliness, availability, and reliability in pursuit of improved patient care. Creative uses have led to “better paper.”
INTRODUCTION
Like the paperless business office, the paperless hospital or medical office is currently a myth. Business Week predicted the paperless office in 19751 when it was thought that computer records would completely replace paper. In the next two decades after that pronouncement, paper use doubled.2“Going paperless,” that is, eliminating paper, thereby creating a paperless office or hospital is often a highly visible institutional goal of implementing Computerized Provider Order Entry (CPOE) and Electronic Medical Record (EMR) systems. CPOE is defined as a computer application healthcare providers use to enter orders for medications, diagnostic tests, and ancillary services into a computer system. The EMR refers to a computerized record of patient data. Because of their close interrelation, we will consider them as one, EMR/CPOE. Shifting to an electronic system from a paper-based system is widely expected to improve the efficiency, quality, and safety of medical care.3–6
Our research team however, identified “persistent paper,” that is, continued paper use in an electronic environment -as one type of unintended consequence of EMR/CPOE implementation7. To identify reasons for this phenomenon, we analyzed all descriptions of continued paper use in our data.
METHODS
Site Selection
We selected sites based primarily on their reputations for excellence in the implementation and use of EMR/CPOE as determined by a panel of experts. We sought broad geographic variation, types of systems and healthcare organizations, and length of EMR/CPOE use. Although each institution was, and is, a model of EMR/CPOE use, none was truly “complete” in every aspect of EMR/CPOE.
Data Collection
The multidisciplinary Provider Order Entry Team (POET) includes librarians, physicians, nurses, a pharmacist, medical informaticists, and trained informatics graduate students. The team collected data on visits to multiple sites over nine years. To gather data, we used observation, informal interviews, focus groups, and oral history interviews. Subjects included clinicians, medical and IT staff, and administrators. We shadowed participants unobtrusively to observe interactions with clinical systems. Interviews let us elicit each institution’s history with electronic systems as well as the implementation process.
We obtained institutional review board approval at Oregon Health & Science University, Kaiser Permanente Northwest, and each study site.
Data Analysis
Data analysis has been ongoing since 1998. Initial analysis of data from the University of Virginia, Veterans Affairs of Puget Sound, and El Camino Hospital investigated EMR/CPOE implementation success factors. As our investigation progressed, we realized that implementation of clinical systems could produce unintended consequences. We then visited six more sites (Kaiser Permanente Northwest, Regenstrief, Alamance Hospital, and three hospitals in the Boston area) to learn more about unintended consequences. We used a card sort analysis to identify categories of unintended consequences. One such category was “paper persistence,” or, the continued use of substantial amounts of paper in organizations that had committed to the reduction or elimination of paper. These observations prompted interim analysis and spurred additional discussion and evaluation.
RESULTS
Eliminating paper, thus creating a paperless environment was a highly visible goal at all institutions. We observed much paper still in use. One medium-sized institution (a 300 bed hospital) uses “1.6 million pieces of paper per month – printed or copied …we print and destroy 40% of that paper.” Why is there such continued use of so much paper in a potentially “paperless” environment? First, because old uses are still valued, second because there are new uses for paper, and third, because of regulatory factors.
Old Uses are Still Valued
Clinicians and institutions may use paper because there is still value in old uses.
Psychological factors: paper is familiar and comforting. People and paper have had a long and close relationship. Paper interweaves medical practice and the social fabric of teams.
Some people value the palpable presence of paper, needing or wanting a paper document they can see and hold: "’I like to have a handle on it. I like to have the information on paper where I can hold on to it,’ (as he clutches his sheaf of papers to his chest.)” In our study, participants also stated they found the electronic replacements for comfortable established paper-based processes discomforting:
Users often mentioned difficulties understanding information presented in electronic form compared with paper, so they print paper copies: “I have to put it down, look at it, and then think about it.”
Many clinicians continue to use paper notes because of discomfort using the computer and typing when with the patient. They felt it degraded both the patient’s and their own experience by diverting eye contact, distracting attention from the central patientdoctor relationship, and was rude as well.
Paper is part of some social systems in care delivery. In the Intensive Care Unit, for example, activity historically centers on the patient care flowsheets. A nurse told us: “It's just the nature of a critical care unit to use a flow sheet.” We observed other medical teams, hospitalists, intensivists, and other specialists organizing work around paper charts as a group activity. The teams divided the work and assigned tasks to individuals who then developed individual to-do lists. Developing the checklist was part of the medical team’s social structure and functional hierarchy.
Some continued paper use is due to clinician or institutional “inertia.” At several sites clinicians were provided with a bundle of papers for a clinic visit or an admission but discarded them almost immediately, stating that they really didn’t know why the pages were printed since they were no longer used or useful: “They told us we'd be paperless, each night all this stuff is printed, we never look at these papers, I don't know why we have them."
New Uses of Paper
Paper is often used to fill gaps in electronic systems. Systems are not always complete when implemented and may also be only partly implemented. These uses disappear with further development of systems.
Technology Factors: Paper Fills Gaps. Electronic systems, particularly billing and Admission-Discharge-Transfer (ADT) systems, are widespread, with more than 95% of even critical access hospitals employing them8. Utilization of EMR/CPOE, representing computerization of the care delivery side, is slowly increasing9. Because many hospitals and clinics take an incremental approach to electronic system implementation, moving bit by bit, unit by unit, they may bypass some units or functions temporarily, resulting in systems that are part paper, part electronic, with paper filling the gaps. Often, paper ordering and reporting are necessary for ancillary services such as labs and imaging. Pharmacy routing in some institutions is another place where paper persisted: “A printout is also produced in the inpatient pharmacy with every order entered…This process necessitates the use of an unbelievable amount of paper.”
Systems may not allow EMR/CPOE activation until the patient has inpatient status. Rather than delay delivery of patient care, in this circumstance, some institutions supported a paper-based admission process that allowed paper orders initially with later entry into the EMR/CPOE system.
In addition, there are numerous other reasons why paper was needed: “We continue to maintain a hybrid documentation environment…the following continue to exist wholly or in part as paper: consents, emergency trip records, progress notes…nursing assessment and, code blue records.” During emergent situations such as acute cardiovascular collapse and other urgent situations EMR/CPOE systems did not replace paper in our study institutions: “…all of that documentation still goes on paper. The paper is then put in the [paper] chart.”
Unique Attributes of Paper: “Better Paper”
Paper does have some rather unique attributes that give it value, such as flexibility and tailorability. Paper may act as a temporary computer interface, a portable database (as in rounding reports), or a repository of information a patient will take home with them, none of which require a logon, electricity or the web. These uses of “better paper”, some of which are quite creative, may never be replaced.
Human and Ergonomic Factors: Paper is versatile and useful Ergonomics is the science of designing products to optimize them for human use10. Ergonomics also includes a product’s existing characteristics such as accessibility and ease of use11. Sticky notes are a prime example of ergonomic flexibility observed in all institutions in our study, where they festooned charts, door posts, and computer terminals. Sticky notes held simple requests: “Patient would like order for throat lozenges”, as well as more complex requests or comments, and unfortunately, computer passwords.
As we noted earlier, everyone from clerks to clinicians used paper reminder lists and checkbox lists: “On her census pages…her patients have check boxes. She crosses them off after she’s seen them.” These notes and lists often employed color-coding to denote new orders, changes, and plans.
Hybrid computer-paper instruments: Some EMR/CPOE systems generated patient lists as well as succinct thumbnail descriptions of a patient’s diagnoses, problems, pending orders, labs, etc. Clinicians then wrote more information on them, producing hybrid documents. These documents were frequently observed in the pockets of clinical staff members: “Each of the participants has a bundle of paper. Most have the Long rounds, Dr-Pt list and chart notes.” Participants expressed confidence in these paper reports: “We use these reports to write progress notes. The synopses are really accurate.”
Hospital discharges can often be time-consuming. Here, the computer–paper connection can lead to time savings by reducing the time needed for a discharge summary: “If the patient is in for less than a week, it [the EMR] will auto-populate a discharge summary.” A timely discharge summary saves time for the discharging doctor and can be a boon for outpatient follow-up care.
In the institutions included in our study, we often saw heterogeneous “bundles” of documents from different sources. For doctors and nurses, as well as for support services, the bundle often consisted of a EMR/CPOE-generated “census” document with multiple entries for a team or floor, pages for individual patients, and other pages for beepers and contact information. Clinicians expressed their perceived value: “They’re wonderful to have. If I lose them in the day, I’m totally lost through the rest of the day…I have to go all over to get information.”
When Paper may be Best
There are conditions under which paper may be the best solution, at least for the near future.
Regulatory Factors: Paper use may be required, at least for now. The regulatory environment can have significant effects on computer and paper use. States may require paper copies of documents such as informed consent, resuscitation status, or advancedhealth directives to physicians. Narcotic prescriptions still often require a “wet signature.”
Institutional policies often require verbal orders be written and placed in the chart if the transcriber cannot enter the order directly into the computer. Sometimes official order sheets are not available. One participant described the unauthorized use of a hastily-grabbed napkin or paper towel as the “paper towel interface,[noting] You just can’t file that in the chart.”
Downtime Procedures Individual offices and groups may have informal contingency plans for times when their EMR does not work. They may print hard copies of lab and recent visits for the next day’s patients. Other locations file that day’s visit bundle in a paper chart so that at least that information is available.
Hospitals and other facilities with patients in ongoing critical treatment can ill afford to ignore the probability of a network or other system outage. Paper back-up processes are essential to ensure continuity of care and avoid lapses in care during system downtime, whether expected or unexpected. Our subject institutions often had formal processes for immediate reversion to paper-based systems when EMR/CPOE went down and furthermore, regularly practiced downtime drills. An anecdote illustrates the disorder: “when a server went down; ‘we had nothing; couldn’t get labs, anything…no effective paper back-up. It was terrible.’”
DISCUSSION
The practice of medicine has developed using paper as a record and as a communication tool. As Harper and Sellen observed: “Paper has helped to shape work practices, and work practices have been designed around the use of paper.”12 Although some paper persistence may be inevitable, there are also good reasons to be cautious about its continued use.
Paper’s Positives: Reasons for Persistence Paper has physical attributes that make it particularly effective in collaborative work. Luff described “tailorability,” or rapid customizability that allows, for example, convenient use of various colored markers and freehand annotations11. Ecological “flexibility” describes paper’s attributes: small, foldable, and easily moved about11. Paper even works without power or access to an information infrastructure. The observed flexibility of sticky notes may delay their electronic replacement.
Where systems do not allow EMR/CPOE before the patient arrives, paper is needed to bridge the gap and allow care to begin without delay. Without such plans, there have been significant patient-care problems.13 Paper is still needed to communicate information between electronic and paper-based institutions, though hopefully not for long since scanning and faxing have their own problems.
Paper back-up processes can help an institution avoid grinding to a halt during downtime attributable due to system failure or maintenance. It is critical that institutions implement carefully designed procedures detailing how temporary paper records will later merge with computer records.
Paper’s negatives: A Reason for moving to electronic media. Paper documents hold static information that loses timeliness with age. Participants told us that although documents are current when printed, they “age rapidly during the day.” Similarly, “versioning,” occurs when multiple versions of a paper document exist, leading clinicians to wonder which document has the latest information. “We feel it’s safer to go to the original document in the computer.”
Paper documents containing patient information constitute an information security hazard. HIPAA addressed this problem, defining protected health information and how to handle it in exquisite detail. Despite HIPAA, a misplaced patient information sheet or chart becomes an untraceable breach of confidentiality because those paper documents have no secure audit trail of those who have seen the document.
Paper’s Replacements
We use the term “inertia” to describe resistance to change, or a desire to continue the current process. This kind of paper persistence is the most human of factors: we simply do things we always have, although those processes are a vestige of times past.
As digital systems evolve, new capabilities should allow replacement of paper. For example, digital technologies are steadily becoming more paper-like by becoming smaller, lighter, less expensive, and more portable. Paper documentation is still required in many locations for advanced directives and narcotic prescriptions. Consents for procedures or surgeries often persist in paper form but electronic replacements are being developed14. Federal legislation has encouraged digital signatures in place of some “wet signatures”15. What remains is to employ electronic signatures on a large scale in systems, policies, procedures, laws and by-laws.
Berg points out that work tasks are completed by an interrelation of workers and artifacts together16. The artifact (paper order sheet or EMR/CPOE) does not just support the work but, by actually “taking part” in the work brings about task completion. Replacement of an element, like paper, of this co-developed process is not trivial, and will take time and patience. Given enough time, the screen may become as useful as a piece of paper, and an electronic signature as forceful as a handwritten signature.
Paper’s future: what next? Paper is increasingly a temporary medium in healthcare settings: rather than being archived at the end of a session, it is simply shredded, similar to industry practices17. Some medical institutions file little paper, others have no official paper record at all. Where paper continues to be generated for office visits or hospital admissions it is often shredded at the end of the encounter. In a move that may possibly circumvent the shred-recycle process, Xerox is developing a paper that will erase itself in approximately 16 hours17.
Finding ways to accomplish tasks in the new electronic milieu may require adapting old methods to fit the emerging environment 18. As improved digital devices take on more of the ecological flexibility of paper, we may also expect them to take on more of paper’s current roles. Meanwhile, paper will continue to fill many gaps, from psychological to technological, to legal. These system gaps leading to continued use of paper may point to opportunities for increased functionality and usefulness of systems.
CONCLUSIONS
We observed paper to have a prominent place,filling vital roles. Although many such uses will become electronic with time, right now paper in those roles make care happen. Our observations indicate that “going paperless” is a journey, not an event. Going forward, as institutions introduce electronic systems, they should not expect paper to totally disappear overnight. We found paper use generally had a very positive impact on patient care by serving as a portable, disposable computer interface, supporting information transfer between clinicians and patients, allowing care to go on during outages, and filling gaps in the system to support clinicians. Our observations lead us to believe that as electronic systems assume the archival role, the role of paper will continue changing from an archival medium to an active and vital communication medium, filling gaps in current technology. As gaps close, paper may go away—but not anytime soon.
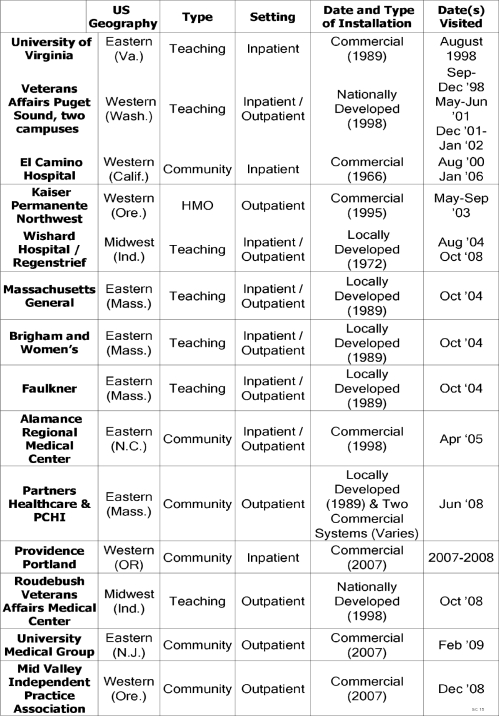
Table 1.
Attributes of Selected Sites
Acknowledgments
This work was supported by NLM grant LM06942 and AHRQ contract HHSA290200810010. Special thanks to Cody Curtis for help preparing this paper.
REFERENCES
- 1.The Office of the Future. Business Week z1975 June 30. 1975:48–70. [Google Scholar]
- 2.Abramovitz J, Mattoon A. Paper Cuts: Recovering the Paper Landscape.: WorldWatch Paper 149 December 1999
- 3.Mekhjian HS, Kumar RR, Kuehn L, et al. Immediate Benefits Realized Following Implementation of Physician Order Entry at an Academic Medical Center. Journal of the American Medical Informatics Association. 2002;9(5):529–39. doi: 10.1197/jamia.M1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuperman GJ, Gibson RF. Computer Physician Order Entry: Benefits, Costs, and Issues.[See Comment] Annals of Internal Medicine. 2003;139(1):31–9. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 5.Bates DW, Teich JM, Lee J, et al. The Impact of Computerized Physician Order Entry on Medication Error Prevention. Journal of the American Medical Informatics Association. 1999;6(4):313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Leapfrog Group Factsheet: Computer Physician Order Entry. 2006 [Accessed September 17, 2006] Available from: http://www.leapfroggroup.org/for_hospitals/leapfrog_safety_practices/cpoe
- 7.Campbell EM, Sittig DF, Ash JS, et al. Types of Unintended Consequences Related to Computerized Provider Order Entry. J Am Med Inform Assoc. 2006;13(5):547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flex Monitoring Team The Current Status of Health Information Technology Use in Cahs 2006[Accessed Mar 13, 2008] Available from: http://www.flexmonitoring.org/documents/BriefingPaper11_HIT.pdf
- 9.Health Information Technology in the United States: The Information Base for Progress2006 [Accessed March 3, 2008 ] Available from: http://www.rwjf.org/files/publications/other/EHRReport0609.pdf
- 10.SearchWebServices Definitions. Human Factors. 2007 [Accessed June 2, 2007 ] Available from: http://searchwebservices.techtarget.com/sDefinition/0,290660,sid26_gci214386,00.html
- 11.Luff P, Heath C, Greatbatch D. Tasks-in-Interaction: Paper and Screen Based Documentation in Collaborative Activity. In: Turner J, Baecker R, editors. Proceedings of the 1992 ACM Conference on Computer Supported Cooperative Work. New York: ACM Press; 1992. pp. 163–170. [Google Scholar]
- 12.Harper R, Sellen A.Paper-Supported Collaborative WorkXerox Technial Report EPC-1995-109 1996
- 13.Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected Increased Mortality after Implementation of a Commercially Sold Computerized Physician Order Entry System. Pediatrics. 2005;116(6):1506–12. doi: 10.1542/peds.2005-1287. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Medicine. Va Pateint Consent Goes Electronic. 2005 [Accessed February 17, 2007] Available from: http://www.usmedicine.com/article.cfm?articleID=1012&issueID=71
- 15.Electronic Signatures in Global and National Commerce Act (Esign)Pub. L. No. 106–229 (June 30, 2000) [Google Scholar]
- 16.Berg M. Accumulating and Coordinating: Occasions for Information Technologies in Medical Work. Computer Supported Cooperative Work. 1999;8:373–401. [Google Scholar]
- 17.Markoff J.New York Times. Xerox Seeks Erasable Form of Paper for Copiers. 2006 [Accessed Available from: http://www.nytimes.com/2006/11/27/technology/27xerox.html?_r=1&scp=1&sq=&st=nyt
- 18.The College of Healthcare Information Management Executives (CHIME) Printing Still Common after Ehr. 2007 [Accessed 7/17/07] Available from: http://www.healthdatamanagement.com/html/news/NewsStory.cfm?articleId=15454