Abstract
Patient experience was assessed by survey as part of a large, randomized controlled trial of a secure, practice-linked personal health record called Patient Gateway at Partners HealthCare in Boston, MA. The subjects were patients with Type 2 diabetes who prepared for their upcoming primary care visit using a previsit electronic journal. The journal generated a diabetes care plan using patient chart information and patient responses to questions in preparation for a scheduled office visit. Review of 37 surveys revealed that a diabetes care plan took 5–9 minutes (modal) to be created by the patient and helped many patients to feel more prepared for their visit (60%) and give more accurate information to their provider (53%). Study limitations included small numbers of survey participants and a bias toward white, better educated patients with better controlled diabetes. Nevertheless, the electronic journal is a promising tool for visit preparation and process improvement.
Introduction
Patient medical chart information is available electronically via secure patient portal at a number of leading healthcare organizations1,2, including Partners HealthCare, where over 70,000 patients have enrolled in Patient Gateway (PG), a secure, electronic health record (EHR) connected personal health record (PHR) in use since 20023.
Patient-entered information collected electronically for use in ambulatory care has become more commonplace4, and advocates believe it promises to save time, improve information accuracy and completeness, increase patient understanding of their own chart data, and engage the patient as a partner in care5. Adoption of these approaches remains a significant challenge for many reasons, including patient access, security and confidentiality concerns, literacy, EHR data limitations, interoperability challenges, and human factors2,6.
The Prepare for Care study, a large, multipractice randomized clinical trial (clinicaltrials.gov Identifier: NCT00251875), was conducted from 2005–2007 to evaluate the impact of a PHR that was linked directly to the ambulatory EHR. It offered patients and providers a novel electronic journal for visit preparation by patients, who reviewed key clinical topics in advance of a face-to-face office visit. The previsit electronic journal completed by diabetes patients and shared with their provider was developed with feedback from a variety of stakeholders, including patients, providers, practice staff, and informatics specialists.
This paper reports on patient journal use and survey feedback from patients about their experience using the previsit diabetes journal.
Methods
Eleven primary care practices within Partners HealthCare staffed by 230 primary care providers (PCPs) in hospital and community-based settings were randomized into either an intervention or an active control group. All patients of these practices were eligible to enroll in PG prior to and during the study. Patients received an electronic message via PG’s secure mail system inviting participation in the study. If the patient consented, was a member of the intervention group, and had type 2 diabetes mellitus (DM) based on a review of problem lists, HbA1c > 7.0% in the prior year, and/or an active prescription for a DM-specific medication, they were offered the diabetes module of the electronic journal, along with the medication and allergy module 2 weeks before a scheduled visit with their PCP.
Mailed postcards, practice signs, and telephone voice messages at each practice were used to recruit patients to use Patient Gateway. Practice physicians and staff were trained in use of the electronic journal, which was made accessible via a web link in the ambulatory electronic health record, the LMR (Longitudinal Medical Record), on the provider schedule page, and in the electronic patient chart.
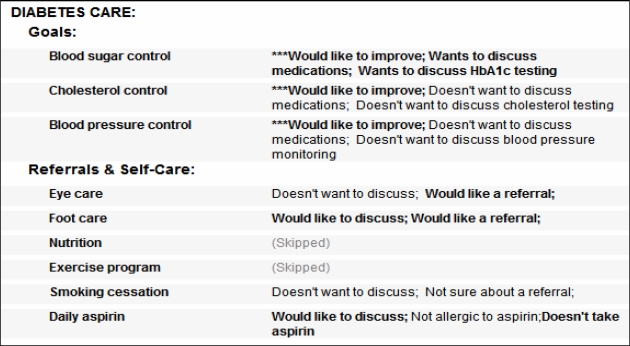
The electronic journal for DM patients consisted of several topics: Medications, Allergies, Diabetes Goals, and Diabetes Referrals and Self-Care. The journal incorporated the most recent values for HbA1c, LDL-C, and blood pressure, along with current medications and allergies from the LMR. Patients were invited to enter: 1) structured concerns and requests about their glucose, cholesterol, and blood pressure control; 2) requests for referrals or education for eye care, foot care, nutrition, aspirin use, smoking cessation, and exercise; and 3) corrections or changes to their medication list and allergy list. Run-time decision support was integrated into the journal to communicate if the patient had reached their diabetes management goal (e.g. for glucose control) or not, and to suggest actions for improvement. A patient-generated care plan is shown in Figure 1, and additional details about the design and features of the DM PHR module are published 8.
Figure 1.
Screen shot of a completed diabetes care plan.
Patient and physician use of the electronic journal was monitored. In addition, a 10-item journal experience survey was administered online to patients between July 2006 and March 2007, two weeks after opening the journal, to record patient attitudes about use of the electronic previsit journal. Survey items are shown in Table 1.
Table 1.
Journal life-cycle activity.
| Journal status | # Journals (%) |
|---|---|
| Journal created | 300 (100%) |
| Patient-opened | 173 (58%) |
| Patient-edited | 164 (56%) |
| Patient-submitted | 140 (48%) |
| Physician-opened | 114 (31%) |
Results
Levels of participation of diabetes patients in the study were moderate (39%) for PG users (126 out of 323 PG enrollees) but low for all intervention patients (126 of 2525 diabetes patients eligible to participate in the trial, or 5%), as reported previously7.
Journal activity
The 126 patients who consented to the study were offered a total of 300 visit-based journals during the study period (Table 1). Fifty-eight percent of those journals were opened by the patient, 56% were edited, and 48% were submitted. Physicians electronically opened 31% (114 journals submitted by 53 patients). Physicians were asked to review submitted journals if an appointment was kept. Physician viewing of journals printed by the patient was not tracked.
Most (81%) of patient-opened journals were submitted, and most (81%) of patient-submitted journals were physician-opened.
Survey
The journal experience survey was offered to 55 patients who opened an electronic diabetes journal between July 2006 and March 2007. Thirty-seven patients (67%) completed the survey, 30 of whom had completed a journal before July 2006. Survey respondents had similar characteristics to intervention arm patients: 59.4 years (mean age); 42% female; 7% non-white; 60% at goal (<7.0) for HbA1c; 73% at goal for LDL-C (<100 mg/dL); and 51% at goal for systolic blood pressure (<130/80 mmHg).
Results for the ten journal experience survey questions (Q1–Q10) are found in Table 2. The modal time (Q3) reported to complete the electronic journal was 5–9 minutes, with 80% of respondents completing it within 20 minutes. Most (62%) reported the journal to be Very easy or Easy to complete (Q4), while 34% said it was Neither easy nor difficult and 3% said it was Difficult.
Table 2.
Journal experience survey items and responses (intervention arm, patients with diabetes).
| 1. For your recent appointment, did you submit a journal to your provider? (n=37) |
Yes 31 (84%) |
No 5 (13%) |
Don’t know 1 (3%) |
||
| [If “No” to #1] 2. Why did you not submit the journal? (n=7) | Free text response | ||||
| 3. How many minutes did you spend completing the journal? (n=36) |
<5m 3 (8%) |
5–9m 17 (47%) |
10–19m 9 (25%) |
20–29m 3 (8%) |
>29m 4 (11%) |
| 4. How would you rate your experience of completing the journal online? (n=32) |
V. Easy 3 (9%) |
Easy 17 (53%) |
Neither 11 (34%) |
Difficult 1 (3%) |
V. Difficult 0 (0%) |
| 5. Did you discuss your journal information with your provider at your recent visit? (n=33) |
Yes 20 (61%) |
No 10 (30%) |
No visit 3 (9%) |
||
| 6. How strongly do you agree or disagree with the following statements? With use of the journal… |
Strongly Agree | Agree | Neither | Disagree | Strongly Disagree |
| A) my communication with my provider during the visit improved (n=32) | 3 (9%) | 11 (34%) | 17 (53%) | 1 (3%) | 0 (0%) |
| B) the quality of care I received at my visit improved (n=31) | 3 (10%) | 3 (10%) | 21 (68%) | 4 (13%) | 0 (0%) |
| C) my provider had more accurate information about me (n=32) | 3 (9%) | 14 (44%) | 11 (34%) | 4 (13%) | 0 (0%) |
| D) I felt more prepared for my visit (n=32) | 5 (16%) | 14 (44%) | 12 (38%) | 1 (3%) | 0 (0%) |
| E) I felt more satisfied with my visit (n=31) | 4 (13%) | 8 (26%) | 17 (55%) | 2 (6%) | 0 (0%) |
| 7. What topics would you like to have in the journal you submit to your provider? | Topics list + Free text response | ||||
| 8. Based on your experience using the journal, are you interested in completing a journal again for another visit? (n=35) |
Yes 22 (63%) |
No 5 (14%) |
Not sure 8 (23%) |
||
| 9. Based on your experience using the journal, would you recommend it to a friend or relative? (n=36) |
Yes 22 (56%) |
No 5 (14%) |
Not sure 11 (30%) |
||
| 10. Any other feedback? Please comment. | Free text response | ||||
Eighty-four percent of survey respondents reported submitting a journal for their appointment with their provider (Q1), and 61% reported they talked with their provider about journal information (Q5). Thirty percent said they did not discuss it with their provider, and 9% said they had not had their appointment yet. One patient commented, “[my] dr. did not have survey info available”, suggesting that physician access did not always occur.
Improvements in some measures of visit experience were reported with use of the journal (Q6). Patients agreed or strongly agreed with the statements: I felt more prepared for my visit (60%); My provider had more accurate information about me (53%); “Communication with my provider improved” (44%); and “I felt more satisfied with my visit” (39%). Almost two-thirds (63%) reported they would like to complete a journal again for another visit (Q8), and 56% would recommend it to a friend or relative (Q9).
Other measures of the visit experience were not increased according to survey results (Q6). Most participants reported the journal did not improve “quality of care during the visit” (81%), “my satisfaction with the visit” (61%); or “communication with my provider” (56%). Several themes from patient narrative comments in the survey emerged.
Enthusiasm for the journal
Patient comments indicated that use of the journal had a positive impact in a number of ways. “It helps me prepare and get myself organized”; “It helps save time during [the] visit”; “In fact I mentioned it to my mom, sister, cousin & aunt yesterday”; “I want to show [my wife] how to use our computer to complete the surveys you sent, [since] it does help [the] appointment go better”; “the Patient Gateway is an excellent idea, much needed”; “This is new to me. I think it is a wonderful way to keep in touch with health issues.” Low enthusiasm was shared by one respondent: “I have been seeing my doctor for many years. I don't need a journal to aid in conversations.”
Content and usability
Some participants criticized journal content as too narrow, saying the journal should “provide an opportunity to let my Dr. know about something new I want to discuss”, “allow for topics of my own choosing”, and “let me write questions I would like answered”. From a list of topics, patients identified the most important ones as: test results (68%), reason for visit (45%), screening & prevention (42%), and medications/allergies (39%).
Some users of the medications/allergies section described it as “clumsy and not flexible”, “tedious”, and suggested the patient “deal only with exceptions”. “It’s silly to ask me if I know what I use ‘syringes’ for – I’m a diabetic”. “I said in the last journal ‘why’ I was taking my medicines – there’s no need to ask me again.”
Access
Some access concerns were identified through patient comments, such as: “Internet Explorer as the only option for access is very restrictive”; and “Not sure I’d be able to do [the journal] at home [if I didn’t have] a job with access to the internet”.
Usefulness to the doctor
Some patients expressed concern about the value of the journal to the physician. “I expect that my doctor knows all this stuff. She always brings my test results up on her computer. Isn't this just wasting her time? I find the med information useful for me but I don't think the doctors need to see it twice”; “She will ask me why I am seeing her even if it is recorded so why duplicate this question?”; “I did take the time to fill out the journal - but at the time of the visit the computers were offline so that my M.D. could not access them.”
Discussion
The electronic previsit journal for diabetes appears to benefit patients in a number of ways. As reported elsewhere7, a major finding for patients in the intervention group was that they were more likely to have their medication regimens adjusted at the office visit, suggesting reduced clinical inertia and the potential for better outcomes.
Survey and usage data in this study showed that the diabetes journal has the potential, in the view of patients, to improve their experience of care during a visit. Half or more of patients surveyed felt the journal improved their visit preparation and the information their physician had about them, said they would like to complete another journal at a future visit, would recommend it to a friend or relative, and found it was not difficult to complete the journal. However, more global measures were not highly endorsed, such as visit satisfaction and the perceived quality of care in the visit. There are several possible explanations for this.
First, the journal limited the patient’s ability to address other topics – such as asking about test results, giving a reason for the visit, etc. This led to some patient frustration. The journal design, which favored structured over free-text patient responses, made topics falling outside of medications, allergies, and diabetes care difficult if not impossible for patients to enter. Whereas even paper forms offer the option to “write in the margin” if necessary, this electronic journal did not. Early in patient user testing, this limitation of the journal was identified as a problem. But concern that physicians could not guarantee timely review of every submitted journal led to the decision for the free-text limitations to remain. Not only is patient frustration reflected in the survey comments, but this design decision may have narrowed the amount of useful information in the journal for physicians, as well. Compensation for non-visit-based care, which is missing in this environment, might have reduced physician objections to receiving free-text journal information.
Second, journal content tailoring had limitations. Journal content was not tailored based on visit type from the scheduling system, or based on physician, even though both of these factors could be used to guide the selection of content. Tailoring did not occur with the presence of non-diabetes conditions. Subsequent visit journals did not adapt questions or prefill data from similar questions in a previous journal, which made some patients complain of unnecessary work. Achieving a useful balance between collecting consistent provider-requested journal content, and fostering flexible patient-driven content, is a significant challenge and an important area for future work.
Third, patients expected journal information to be useful to the physician – and expressed concern when that did not seem to be the case. Patients were explicitly requested to submit the journal and to review it with the physician during the visit. But this did not always happen. Many submitted journals were not opened by the physician, according to tracking data. Many physicians had only one or two patients with journals, and having received training months before the first journal arrived, could have forgotten what to do. Notification of a submitted journal was passive (i.e. an icon next to the patient name on the schedule) rather than active (e.g. a notification message or alert). Patients might have forgotten about the journal as well, having submitted it several weeks prior to the visit. Visits might have been rescheduled or canceled, causing submitted journals to remain unread or to wait longer than two weeks. Thus, a combination of timing, workflow, user interface, and usability factors likely contributed to drop-off in patient and physician use of the journal, in addition to content limitations.
The small number of responess to the survey could have biased the study findings, but it’s unclear if that led to a more positive or a more critical response, given the many factors that affect journal experience.
As EHR systems and practice-linked PHRs mature, next-generation systems such as the diabetes journal in the Prepare for Care study are becoming more feasible. By leveraging multiple clinical system components such as the ambulatory electronic record, the clinical data repository, and expert systems that apply rules to EHR-captured and PHR-captured data, the electronic journal can share historical patient chart information, ask tailored health history questions, provide relevant educational information, and offer personalized decision support. It can remind patients about appointments, facilitate patient data capture, improve information-sharing, streamline documentation, and identify patient visit priorities. For interactive electronic journals to be adopted more broadly, challenges like those identified in this and other investigations6 must be addressed.
Conclusions
Many benefits of use of an electronic journal as part of a practice-linked PHR were reported by patients in this survey. Limitations were also identified in the areas of content, workflow, access, and usability.
With advanced journal capabilities come a number of challenges, including complexity of design, iterative user testing, content tailoring, and the need to engage both patients and physicians in workflow changes.
Research to identify and overcome barriers of adoption should focus on: engaging patients and physicians in use of an electronic journal; tailoring content to provide more value; improving usability; fitting the electronic journal more seamlessly into a collaborative care workflow; and supporting patient-provider dialogue beyond the boundaries of a visit.
References
- 1.Gearon C, Barret M, Brennan P, et al. Perspectives on the future of personal health records. California HealthCare Foundation. 2007 [Google Scholar]
- 2.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wald JS, Middleton B, Bloom A, et al. A patient-controlled journal for an electronic medical record: issues and challenges Medinfo 200411(pt 2):1166–1170. [PubMed] [Google Scholar]
- 4.Kim MI, Johnson KB. Personal health records: evaluation of functionality and utility. J Am Med Inform Assoc. 2002;9:171–180. doi: 10.1197/jamia.M0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bachman JW. The patient-computer interview: a neglected tool that can aid the clinician. Mayo Clin Proc. 2003;78:67–78. doi: 10.4065/78.1.67. [DOI] [PubMed] [Google Scholar]
- 6.Nijland N, van Gemert-Pijnen J, Boer H, et al. Evaluation of internet-based technology for supporting self-care: problems encountered by patients and caregivers when using self-care applications. J Med Internet Res. 2008 May 15;10(2):e13. doi: 10.2196/jmir.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant RW, Wald JS, Poon EG, et al. Design and implementation of a Web-based patient portal linked to an ambulatory care electronic health record: patient gateway for diabetes collaborative care. Diabetes Technol Ther. 2006;8(5):576–586. doi: 10.1089/dia.2006.8.576. [DOI] [PMC free article] [PubMed] [Google Scholar]