Abstract
Patient empowerment is considered to be one of the key factors in improving and maintaining a patient’s health status. Patient empowerment in chronic illnesses involves educating the patient after the initial diagnosis and then keeping the patient motivated to adhere to the treatment in the follow up period. The aim of this research is creating an interactive framework to improve adherence to treatment in type 1 diabetic (T1D) patients based on an existing theoretical behavioral change model. The proposed framework learns from the patient’s situation based on the patient’s adherence to treatment and the patient’s personal profile; and then the framework adapts itself to the new situation and creates new strategies to motivate the patient in order to reinforce positive behavior on the part of the patient. Thus, the embedded self-care interactive framework empowers T1D patients in achieving improved health outcomes by adhering to long term treatments.
Keywords: Interactive Frameworks, Self-care Health Games, Behavioral Change Models, Patient Empowerment, Compliance to Treatment, Adherence to Treatment
1. Introduction
1.1. Empowerment
Patient empowerment is the enhanced ability of patients to actively understand and influence their health status [1]. Effective ‘Patient Empowerment’ would not be achieved unless the patient can receive the necessary information and be educated about his/her situation which implies the necessity of ‘Patient Education’ [2].
Although traditional clinical care is still the main core in treating patients and relieving their morbidities, when it comes to chronic diseases the patient’s role in self-controlled health status becomes more prominent [3]. Thus ‘Patient Empowerment’ and ‘Patient Education’ together are essential and crucial elements in managing ‘Chronic Diseases’ [4]. Furthermore, ‘Chronic Diseases’ are increasing dramatically in modern societies compared to other types of diseases [5].
1.2. Behavioral Change Models
The main aim of ‘Patient Empowerment’ and ‘Patient Education’ is to change the patient’s view, concept and finally the patient’s act and behavior about his/her disease. The ultimate goal for the patient is to assume responsibility for managing the disease and to behave accordingly in order to improve the health status. Passive education without any patient interactivity would not lead to the desired results [6].
Positive behavioral changes would reinforce the patients in order to increase their role in the treatment procedure. Providing information alone, without the necessary incentives, would not insure a positive effect [7]. As an instance, many of the young diabetic patients are well informed about their situation but most of them are not acting well about their regular injection times [8].
The traditional approaches may not change the patients’ behavior as these approaches do not have sufficient incentives for the patients to affect them based on their unique situations [9]. The existing interactive frameworks are not suited to target the real change in the patients’ behavior to ensure an effective change in their personal lifestyles [10].
2. Background
2.1. Health Games
Games are targeted for increasing the motivation of patients in three areas [11]: (1) To increase a patient’s motivation to engage in learning the ins and outs of their condition and its treatment; (2) To be used as a tool in distraction therapy for pain and anxiety; and (3) To encourage young patients to continue with their treatments over longer treatment regimes.
2.2. Theory of Planned Behavior (TPB)
According to the theory of planned behavior, human action is guided by three components: “beliefs about the likely outcomes of the behavior and the evaluations of these outcomes (behavioral beliefs), beliefs about the normative expectations of others and motivation to comply with these expectations (normative beliefs), and beliefs about the presence of factors that may facilitate or impede performance of the behavior and the perceived power of these factors (control beliefs)” [12]. Based on this model, behavioral changes can be achieved by targeting any of the factors: attitudes, subjective norms, or perceptions of behavioral control. The result of such an intervention should produce changes in behavioral intentions and, given adequate control over the behavior, the new intentions will be carried out under appropriate circumstances [12].
3. Methodology
3.1. Current Study
A game framework was developed based on the TPB model to increase the adherence rate to treatment. The main research question of this study is “Can games change the behavior of patients with Type 1 diabetes?” Parents reported adherence rates of their children and children (patients) were awarded in the game based on their adherence to treatment. Health points collected by adherence were used in the game to acquire new items or play additional embedded games (i.e. mini-games). The user studies showed a significant improvement in attitude toward healthy behaviors and a significant increase in adherence rates [13]. The significant results indicate the effectiveness and potential of the implemented conceptual interactive framework in changing the behavior of the patients.
3.2. Conceptual Framework
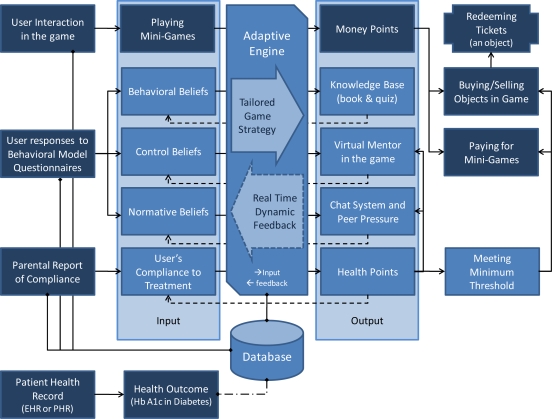
The purpose of developing a conceptual framework is to match the foundational basis of treatment adherence and behavioral models to the elements of games. In this study, theoretical models of adherence and behavioral changes were broken down into its constructs and then possible matching framework elements were identified (Figure 1):
Fig. 1:
Interactive Framework based on the TPB model. Darker boxes represent features used in both treatment and control group. Lighter boxes were only functional in the treatment group.
Knowledgebase and Educational Content
This element was represented by an embedded book. The content was customized based on the patient’s current beliefs and actions. A quiz was administered in the framework and if the patient’s responses showed that s/he did not believe taking medication has an effect on health outcome, more information in this regard was provided.
Motivational Factors
It is important to keep the patients motivated in engaging with the game while improving their behavioral beliefs. For example, if a patient does not believe taking an insulin-shot on time makes any difference, an element in the game has to motivate him/her by showing the results of such an action. The following approaches were considered: Pointing system: The user (patient) was rewarded based on his/hers actions in the real world and also in the game. The user was rewarded by acquiring points while playing the game (e.g. mini-games) and also by acting in a healthy manner in real world (e.g. adherence to treatment). In order to differentiate these two mechanisms, while keeping them inter-related, two pointing systems were used in the proposed framework: (1) Health points were awarded only when the user behaved accordingly such as adhering to treatment. On the other hand, users lost health points when not complying with treatment. Minimum health points were necessary to enter different sections of the game and accessing different objects. (2) Money points were acquired by adhering to treatment, playing the game or correctly answering a quiz in the game; however, users lost money when they used it in the game to purchase different objects including redeemable prizes. Virtual mentoring system: In order to keep the patients motivated and encourage their positive behavioral beliefs while diminishing their negative beliefs, a virtual mentor acted as a reminder and as an external representation of the possible long term effect of a certain act. Indeed, the health of the virtual mentor in the game changed by the reported adherence rates of the patients. The mentor also reminded the patients to take their medication on time.
Peer Pressure
Normative belief of TPB is the beliefs about the normative expectations of others. One way to approach this factor is to facilitate the communication between the patient and other patients. The proposed framework in this research included both a real time chat system and an internal message relaying system.
Measurements
A periodical questionnaire was implemented to determine the current behavioral, normative and control beliefs of the patient. This helped the researcher in measuring the effect of the proposed interventions; plus, the adaptation of the framework to the patient’s behavioral model. For example, based on the questionnaire’s result, the game could find out that the patient is lacking in normative beliefs and therefore promoted the game’s chat system by prompting the patient to use it more often.
3.3. Study Design
The study implemented a mixed between-group and within-subject methodology (repeated-measurements along with longitudinal crossovers). 42 Type 1 diabetic patients (7 to 13 yrs) were randomly assigned to either G1 (starting as the test group) or G2 (starting as the control group). The weekly treatment plan was acquired from the parents and entered for each participant in the framework’s database prior to the start of the study. As the study progressed, the participants interacted with the game while their parents entered their adherence data based on the given treatment plan. Participants who played EH (the game framework with the behavioral change features) were rewarded in the game based on their adherence data and had access to the game’s book, virtual mentor and chat system, while participants who played EO (the game framework without the behavioral change features) did not have these features.
G1 played EH for three weeks while G2 started the study by playing EO for the same amount of time. After three weeks, the condition reversed, where each group experienced the other type of the game. Participants were blinded regarding their initial assignment to either the test (EH) or the control group (EO).
The TPB questionnaire was targeted for treatment adherence and adapted from previous studies that showed an acceptable internal validity [14]. However, the questionnaire’s internal validity was tested again due to its modification for treatment adherence. Cronbach’s alpha, which represents the internal validity, was 0.72 for attitude, 0.86 for subjective norm, 0.79 for perceived behavior control, and 0.82 for intention. The questionnaire was administered on a weekly basis. At the end of the study a usability questionnaire was also administered. Adherence reports were entered by the parents and adherence rates were calculated in the game on a daily basis, although a weekly rate was used for statistical calculations.
4. Results
4.1. Behavioral Change Results
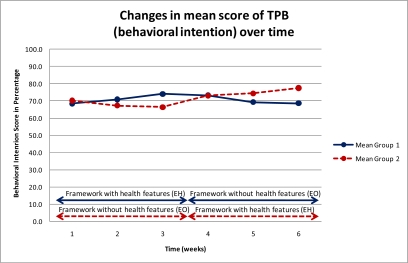
Each subject answered the questionnaire 6 times (3 times while playing EH and 3 times while playing EO). The following chart (Figure 2) depicts the transformation of the TPB average score for behavioral intention during the study for both G1 and G2. Both G1 and G2 experienced EH and EO but in different stages due to the crossover design.
Fig. 2:
Changes in the mean score of TPB (behavioral intention) over time
In figure 2, the solid line indicates G1 who experienced EH in the first three weeks and then EO for the rest of the study. The dotted line represents G2 who experienced EO before EH. The arrow lines on the bottom of the chart indicate the within-subjects crossover of EO and EH. As depicted by the solid line, the mean TPB’s behavioral intention score rises in the first three weeks while it decreases and finally becomes plateau at the end of the study. In contrast, the dotted line decreases in the first half of the study and then starts to rise in the second half.
The simplest test to explore the data is a paired t-test that compares each pair of the measures. The null hypothesis can be redefined for each of the comparisons. For example the null hypothesis can assume that the mean of TPB score in week two is not different from week one. If the paired t-test shows an acceptable p-value while having a favorable CI-95 then the hypothesis can be rejected; and inferred that a significant difference exists. A paired t-test between mean scores of each week compared to its previous week showed significant change in all weeks except the last week (the plateau at the end of the diagram). The paired t-test results are: week 2 versus week 1 (p=.031), week 3 versus week 2 (p=.000), week 4 versus week 3 (p=.000), week 5 versus week 4 (p=.000) and week 6 versus week 5 (p=.355: not significant). The insignificant difference for the last two weeks can be interpreted as a stabilizing form of the learning effect, but it cannot be studied unless the interaction of game type and subject is calculated.
Although paired t-test is a suitable test to explore the differences within-subjects, it does not explore the differences between the groups (G1 and G2). An alternative is the application of an unpaired t-test for G1 and G2 in the first half and another one for the second half. After applying an unpaired t-test to the differences of means between G1 and G2 in the first and second half of the study a significant change was detected (p=.000, CI95= 6.50–12.33 and p=.000, CI95= 6.39–11.93). These results were interpreted as a significant difference between the mean TPB scores of G1 and G2 in the first half and second half of the study; however this test ignores the within-subject design.
Although these t-test results show the changes in the mean score over time, these changes should be analyzed while considering within-subject and between-group designs concurrently to imply significance. An approach to measure the significance of a difference in a mixed within-subjects and between-groups design is GLM-ANOVA. Subject is assumed a random factor. After applying the GLM models of TPB versus Subject, Game and Subject*Game (interaction) the following p-values were detected: .000 (F=87.38) for subject, .000 (F=16.65) for game and .001 (F=2.10) for the interaction of subject and game. R2(adj) was determined at 91.79% which shows a low contribution of errors in the results that is mainly because of the subject’s effect in absorbing the errors associated with the variability between subjects. The results were interpreted as a significant difference is TPB’s behavioral intention scores due to the effect of the subjects and the game type (EH versus EO).
The t-test of the difference between mean TPB score of week 1 versus week 6 between G1 and G2 resulted in an insignificant p-value (p=0.467). This can be interpreted as an insignificance effect of EH in long term (e.g. G1 has lost its TPB score when encountered with EO). This may indicate that keeping a high TPB score requires frequent interaction between the user and EH. A regression analysis of the effect of TPB score on missing medications showed a significant effect (p=.000); however the small R2(adj) (36.6%) implies the effect of control factors in the conversion of an intention (TPB score) to an actual behavior.
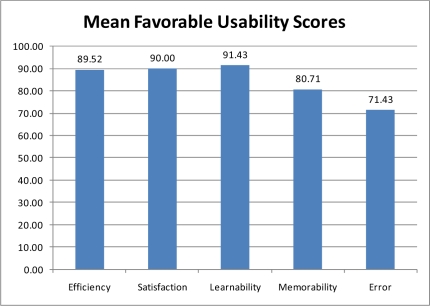
4.2. Usability Results
Usability questions were included only at the end of the study. Some of the questions were Likert-scale while some others were comment based. Usability questions were categorized as: Efficiency which reflects the goal of the game in affecting adherence; Satisfaction which indicates how much fun the game has been; Leanability that indicates how easy learning the game was; and Memorability which refers to the ease of memorizing game features (Figure 3):
Fig. 3:
Mean usability score based on various categories.
5. Conclusion
The proposed framework provided support for children and families to engage in games and game-like scenarios to reinforce lessons and skills and to encourage adherence to long term treatments for chronic diseases such as Type 1 diabetes.
This research has not tried to create a complete game but rather to develop a framework that supports a behavioral model. Due to the change in the patient’s behavior in the course of interaction with the game, the game itself adapted to the particular stage of the patient in order to keep him/her motivated.
Despite the exciting results, the researcher concludes that longer term parallel studies are needed. The research should be replicated for different chronic conditions to increase its generalizability. Multiple centers can be involved and different age ranges can be investigated. Different game elements may be studied separately to identify the most effective ones.
References
- 1.D’Alessandro D, Dosa N. Empowering children and families with information technology. Arch Ped Adolesc Med. 2001;155(10):1131–1136. doi: 10.1001/archpedi.155.10.1131. [DOI] [PubMed] [Google Scholar]
- 2.Johansson K, Leino-Kilpi H, Salantera S, Lehtikunnas T, Ahonen P, Elomaa L. Need for change in patient education: a Finnish survey from the patient’s perspective. Pat Edu and Coun. 2003;51(3):239–245. doi: 10.1016/s0738-3991(02)00223-9. [DOI] [PubMed] [Google Scholar]
- 3.Luban-Plozza B. Empowerment techniques: from doctor-centered (Balint approach) to patient-centred discussion groups. Pat Edu and Couns. 1995 Sep;26(1–3):257–263. doi: 10.1016/0738-3991(95)00756-p. [DOI] [PubMed] [Google Scholar]
- 4.Paterson B. Myth of empowerment in chronic illness. J of Adv Nurs. 2001 Jun;34(5):574–581(8). doi: 10.1046/j.1365-2648.2001.01786.x. [DOI] [PubMed] [Google Scholar]
- 5.Gagnon J, Grenier R.Evaluation and validation of quality care indicators relative to empowerment in complex chronic disease., l’Universite Laval, Quebec2004 [PubMed]
- 6.Prochaska J, DiClemente C. Self change processes, self efficacy and decisional balance across five stages of smoking cessation. Prog in Clin and Biol Res. 1984;156:131–140. [PubMed] [Google Scholar]
- 7.Fawcett S, White G, Balcazar F, Balcazar Y, Mathews R, Andrews A. A contextual-behavioral model of empowerment: case studies involving people with physical disabilities. Amer J Com Psyc. 1994;22(4):471–496. doi: 10.1007/BF02506890. [DOI] [PubMed] [Google Scholar]
- 8.Keers J, Blaauwwiekel E, Hania M, Bouma J, Scholten-Jaegers S, Sanderman R. Diabetes rehabilitation: development and first results of a Multidisciplinary Intensive Education Program for patients with prolonged self-management difficulties. Pat Edu and Coun. 2004;52:151–157. doi: 10.1016/s0738-3991(03)00019-3. [DOI] [PubMed] [Google Scholar]
- 9.Hewitt-Taylor J. Challenging the balance of power: patient empowerment. Nurs Stand. 2004;18(22):33–37. doi: 10.7748/ns2004.02.18.22.33.c3546. [DOI] [PubMed] [Google Scholar]
- 10.Rapley P. Self-care: re-thinking the role of compliance. AJAN. 1997;15(1):20–25. [PubMed] [Google Scholar]
- 11.Watters C, Kharrazi H, Oore S, Shepherd M, Abouzied A, Cox A, Kellar M. Extending the Use of Games in Health Care. HICSS. 2006;5:88.2. [Google Scholar]
- 12.Ajzen I. The theory of planned behavior. Org Beh & Hum Dec Proc. 1991;2(50):179–211. [Google Scholar]
- 13.Kharrazi H, Watters C, Oore S. Improving behavioral stages in children by adaptive applications. JITH. 2008;6(1) [Google Scholar]
- 14.Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: How useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS. BMC Public Health. 2007 Jun;7(104):1–16. doi: 10.1186/1471-2458-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]