Abstract
Asthma is the leading chronic childhood disease with exacerbations resulting in urgent and emergency care visits. Guidelines adherence improves patient care but is suboptimal. A computerized guideline system can help improve compliance through automatic initiation and reminders to increase adherence. We designed a computerized management system for asthma care in the pediatric emergency department (ED). The system will be evaluated in two phases. The first phase evaluates a computerized diagnostic prompt using the ED’s existing asthma protocol. The second phase evaluates a computerized asthma management system including temporal reminder elements for scoring and medication orders. The system was developed in conjunction with the pediatric ED multidisciplinary care team. The computerized system is entirely automatic and a prospective evaluation of the diagnostic component is ongoing.
INTRODUCTION
Asthma is the leading chronic childhood disease affecting 6.8 million children (9.4%)1. Asthma exacerbations account for an estimated 14 million missed school days2 and more than 1.8 million emergency department (ED) visits annually2. Asthma disproportionately affects minority populations and adverse outcomes including ED visits are higher for black children3. The chronic characteristic of asthma carries a considerable economic burden and accounts for >60% of asthma-related costs4. Uncontrolled asthma can lead to exacerbations requiring the patient to seek immediate care, frequently in an ED setting.
Asthma care in the ED is complex, involving a temporal element of evaluation and reevaluation to adjust asthma medications and make disposition decisions. Standardized care is challenging to provide in a hectic, fast-paced environment like the ED. An implemented guideline can help provide this standardization. The overall goal of this study was to design and implement a computerized detection and reminder system for asthma care in the pediatric ED and embed it in the clinicians’ workflow.
BACKGROUND
Asthma Guidelines
Utilization of and adherence to asthma guidelines improves patients’ clinical care4,5. Several asthma guidelines exist to support clinicians in providing adequate treatment including the guideline from the National Heart Lung and Blood Institute (NHLBI)6. However, guideline adherence remains suboptimal. The NHLBI guidelines for asthma focus on the outpatient setting but include information about emergency management in the ED setting. The guidelines are general rules clinicians should follow for optimal care. The emergency management guidelines direct treatment through peak flow readings, forced expiratory volume, and oxygen saturation. However, the flow diagram provides general principals and requires local customization to account for individual ED variations including for medications and scoring. Peak flow measurements, for example, are not performed in all EDs or a different scoring metric may be applied.
Asthma treatment should be started quickly and its response must be evaluated repeatedly and adjusted to the new assessment level leading to a discharge decision within a few hours. The temporal nature of the guideline makes it more difficult to keep up with the patient’s position on the flow diagram. A computerized approach could help alleviate some of these challenges.
Approaches for implementing guidelines
In the ED early identification and accurate assessment of the severity of airway obstruction and response to therapy are fundamental to the improvement of health for patients with asthma. The NHLBI guidelines emphasize early recognition and treatment of asthma exacerbations6, as well as appropriate treatment stratified by severity. Identification of patients presenting with an asthma exacerbation is often an issue. Among studies that identified asthma patients few were intended for real-time identification and none were integrated with other information systems. One ED-based study implemented a computerized, kiosk-like application to obtain patient information from parents7. In a prospective study8 the kiosk-generated care recommendations were presented on paper to the clinicians caring for the patients. The study had only marginal effects on patient care, which was primarily due to physicians’ nonuse of the provided, paper-based information.
Challenges and opportunities for asthma care
When a patient presents with an asthma exacerbation in the pediatric ED, their care can take several hours. During this time, the care is driven by a team-oriented approach. Upon arrival, patients are given an initial asthma severity rating using either an asthma scoring metric9, peak flow measurement, or oxygen saturation reading. Once treatment has begun, the patient’s asthma severity should be reevaluated every 1–2 hours, but this is challenging in the ED which is fraught with delays. In the ED treatment decisions are made every 2–4 hours and the asthma medications are modified to best suit treatment. The goal is to reach a disposition decision within 4 hours.
DESIGN OBJECTIVES
The design objectives were influenced by the team-oriented workflow of asthma care in the pediatric ED and local adaptation of the NHLBI guidelines. The design included the following steps: developing a conceptual framework, establishing guideline eligibility using a Bayesian network (BN) system10,11, providing an electronic or paper-based flow diagram and protocol, and evaluating guideline adherence. In consideration of the workflow-embedded system, the ED management system had three main design objectives that we considered critical for a successful implementation.
Integration with clinical workflow: The approach should be embedded in the clinical workflow of the ED by making relevant patient information available when the health care provider is asked to make a decision. The system should avoid unnecessary interruptions of workflow. All data used are already collected during triage. The computer application queries the electronic medical record for any additional information including the patient’s past history of asthma.
Informatics approach: The informatics approach should take full advantage of the ED information technology infrastructure, allowing for a fully computerized solution for each step in the process without prompting for additional information. In an integrated approach, the information systems should support the ED staff and facilitate following the guidelines with limited additional work required. This should provide the basis for a completely integrated, computer-based approach.
Information display and data capture: Information should be available at the right time, presented to the right individuals, and in the right format. Data entry and navigation should be minimal. Patients and providers should be able to easily opt out at any time during the process, if deemed appropriate.
Following the design objectives, a multidisciplinary team developed the system, including ED nurses, physicians, respiratory therapists, and leadership members from both the ED and the hospital.
The proposed study examines the benefits of a novel approach for reminding clinicians in an ED setting to use guideline-driven care. The overall approach will apply a workflow-embedded process taking advantage of an advanced information technology infrastructure. It will include two elements:
A diagnostic component consisting of a computerized, real-time reminder system, which will automatically detect guideline-eligible patients without requiring additional data entry, evaluated in phase I.
An asthma management component consisting of a computerized, workflow-embedded guideline implementation, evaluated in phase II.
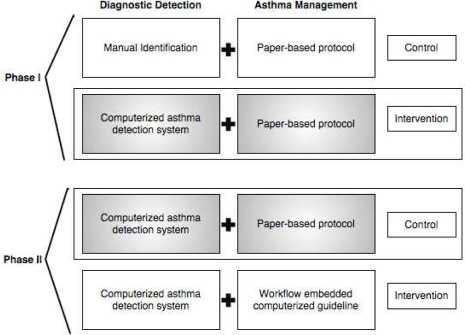
The primary premise is that the combination of the reminder system with the guideline implementation will increase utilization and adherence of guideline-driven care, leading to improved patient outcomes. To examine separately the effects of the computerized reminder system and the computerized guideline on the utilization of and adherence to the guidelines the study will be conducted in two phases (Figure 1). The study includes two hypotheses:
An automatic, computerized reminder system for detecting asthma patients in the pediatric ED will increase paper-based guideline use compared to paper-based guideline without the system.
The creation of an integrated asthma management informatics system that combines the reminder system with workflow-embedded guideline implementation will further increase guideline utilization compared to the reminder system combined with paper-based guideline delivery.
Figure 1:
Study design for phases I and II for asthma management system.
The goals of the computerized asthma system are:
Phase I: Implement and evaluate a real-time, computerized asthma detection system in the ED information system.
Phase II: Implement the asthma guideline in the ED infrastructure and evaluate the effect of the detection system combined with the computerized guideline versus the asthma detection system combined with the paper-based guideline.
SYSTEM DESCRIPTION
Setting
The Vanderbilt pediatric ED provides care for >40,000 patient visits annually. The ED has 48 physicians, 87 nurses, and 18 respiratory therapists. Approximately 7–10% of ED patients present with asthma exacerbations10. A paper-based guideline including a validated asthma severity metric9 is available for guiding asthma care including reassessment and treatment suggestions; however, the guideline is used in only 7–10% of the asthma cases presenting to the pediatric ED10.
Informatics infrastructure
The ED information system infrastructure includes five information systems that were the basis for the computerized guideline system. The five information systems include the electronic medical record (EMR)12, the computerized triage application13, the computerized provider order entry system (CPOE)14, the computerized whiteboard application15, and the computerized respiratory therapy documentation system. The EMR and triage application provide the basis for the diagnostic detection system, phase I, and the CPOE system, whiteboard, and respiratory therapy system provide the basis for the computerized asthma management system, phase II.
Electronic Medical Record
Vanderbilt’s longitudinal EMR includes patient information since 199412. It represents the institution’s primary repository for all patient information, including problem list, clinic notes, procedure notes, scanned documents, exam reports, and caregiver team communications.
Computerized Triage Application
The triage system13 captures triage data in mostly coded format. In addition to capturing the usual triage information (current and past medical history, current medication, pain assessment, vital signs, acuity level, chief complaint, etc.), the triage nurse completes an initial screening for diseases, domestic violence, and cultural needs, and assigns the patient a coded chief complaint. After triage, an asthma probability is calculated using the BN diagnostic system. If the patient has findings compatible with asthma, a check-box appears on the triage exit page asking the nurse to acknowledge that there will be additional asthma documentation to print. When triage is completed, a patient summary page is displayed. The paper-based guideline will print automatically at the end of the summary page including the protocol and flow diagram.
Computerized Provider Order Entry System
Vanderbilt’s CPOE system is used in all inpatient wards and the ED14. Physicians enter more than 90% of all medication orders. The computerized asthma management system will trigger automatically using the computerized detection system. The system will be used to provide a summary page to clinicians including the patient’s prior asthma scores, previous orders, and local guideline recommendations for order or discharge decisions.
Respiratory Therapy System
The respiratory therapy documentation system allows the respiratory therapists to document the asthma score9 using a semi-structured format. The respiratory therapists can easily record the patient’s asthma score as well as any notes about the patient’s breathing or auscultations. The system is integrated with the EMR.
Computerized whiteboard system
The computerized whiteboard allows clinicians an overview of the ED’s clinical and operational statistics15. The whiteboard lists ED patients and relevant information about orders and labs. The whiteboard is a highly used reference for physicians accessing the patient’s EMR or the CPOE system. Using the existing workflow element, the whiteboard will be used to provide an alert notification for asthma reassessment.
Applied Technology
The technology infrastructure used to connect the information systems for the application were Perl and Java programming languages, and Oracle® and MySQL® databases.
RESEARCH DESIGN
Diagnostic Detection
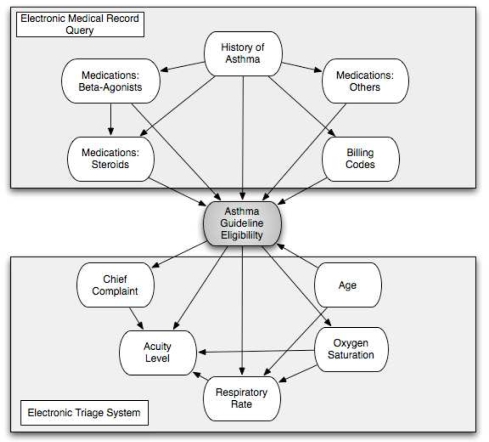
Phase I addresses hypothesis 1. An existing asthma detection algorithm consisting of a BN (Figure 2)10 has been integrated with the ED information system including the EMR and electronic triage application. The algorithm is used in real-time to determine based on the information available in triage, whether a patient has findings suggestive of an asthma exacerbation. At the end of the electronic triage, an exit screen suggests any immediate actions, reminders, or potential resources the patient may require. The effect of the detection algorithm on prompting clinicians to use the paper-based guideline is being evaluated in a currently ongoing randomized controlled trial. The control group will receive no electronic reminder. For the intervention group a prompt is displayed at the triage exit screen asking the nurse to acknowledge that she has seen the prompt and that the patient is eligible for the asthma guideline. Immediately following the triage summary page, the triage nurse prints the locally customized flow diagram and the ED’s asthma protocol. The triage nurse can then easily attach the protocol to the chart. This allows the paper-based flow diagram to be available when it is needed. It also “tags” the patient as having asthma to help initiate treatment earlier.
Figure 2:
Bayesian Network used for determining asthma guideline eligibility.
Asthma Management
Phase II will address hypothesis 2. The asthma guideline component will be implemented and integrated with the different information systems available in the ED, including the CPOE system, the respiratory therapy system, and the ED whiteboard. Clinical workflow considerations will drive the implementation approaches and reminder methods. The effect of combining the asthma detection algorithm with the computerized guideline on guideline adherence and compliance will be examined in a second randomized clinical trial. The detection algorithm will prompt providers for all eligible patients. The control is equivalent to the intervention group in the previous study and includes the computerized asthma prompt for adding the paper-based guideline to the patient’s chart. The intervention group will receive no triage prompt, but the prompt is passed on to the ED information systems, which will prompt the ED physicians to initiate the computerized guideline. In addition, the information systems will remind physicians about the repetitive assessments when they are due, which is expected to increase adherence. The computerized application will be available for use for all physicians, but will only be automatically triggered for patients in the intervention group.
Outcome measures
The outcome variables for both studies include the time to disposition decision, the frequency of guideline use and the adherence to guideline treatment recommendations. The staggered implementation will demonstrate the isolated effects of the detection system and the computerized guideline on changes in guideline compliance.
STATUS REPORT
The diagnostic asthma identification system was put into place in November 2008 to begin a comprehensive run-in period to test the informatics systems. We evaluated four weeks of data from 01/01/2009 to 01/31/2009. The pediatric ED saw 3,986 patients during the test period. Patient demographics are in table 1.
Table 1:
Characteristics for patients in which an alert was triggered.
| Asthma (n=129) | Not Asthma (n=48) | |
|---|---|---|
| Age, mean (standard deviation) | 5.8 (3.9) | 6.1 (4.6) |
| Admission | 38% | 21% |
| At least 1 asthma score | 87% | 33% |
| Respiratory Therapy | 76% | 33% |
| Repeated Scoring |
Patients were included in the analysis if they were between 2–18 years of age, had an ED diagnosis, and were not “fast-tracked.” Fast track patients are moved quickly through the ED for care and do not get placed in the rooms for extended treatment. Patients were also excluded if they had an Emergency Severity Index of 1 (most severe) or did not undergo computerized triage documentation. The system identified 245 as asthma patients with 177 meeting inclusion criteria. A chart review of all the asthma patients identified 48 false positive and 129 true positive asthma cases. Patients were considered to have an asthma exacerbation if their primary or secondary diagnosis was “bronchiolitis,” “status asthmaticus,” “asthma exacerbation,” or “reactive airway disease.” Patients misclassified by the BN diagnostic system included respiratory complaints in 60% of the cases (Table 2).
Table 2:
Diagnoses of patients misclassified by the Bayesian network diagnostic system.
| Diagnosis | (n=48) |
|---|---|
| Pneumonia | 8 |
| Upper Respiratory Infection | 6 |
| Fever | 4 |
| Cough | 3 |
| Respiratory Syncytial Virus | 3 |
| Croup | 3 |
| Tachypnea | 2 |
| Other | 19 |
To help test the accuracy of the diagnostic detection system we queried asthma diagnosis codes (ICD9 493.*) for all patients with an ED visit during the study period. We compared the patients with at least one diagnosis code to those the diagnostic system identified. During the study period, there were 185 patients with an asthma diagnosis code. Of these, 102 were identified by our system. From the 83 patients missed 53 did not meet the inclusion criteria because of age, fast track, or had a comorbidity and unrelated asthma visit that was not ED related. The system missed 27 asthma exacerbations, and of these two patients had asthma as a secondary diagnosis. The system’s real-time impact on ED asthma care is currently being examined in a randomized prospective interventional study.
DISCUSSION
We described the design, development, and implementation of a team-oriented computerized asthma management system that used available information systems to create an informatics solution in a challenging environment. The system is embedded in the ED workflow. The detection system is currently being evaluated in a randomized prospective study. During the pre-implementation study period, the diagnostic system ran in an unobtrusive manner; the system was thoroughly evaluated and fully functional. The computerized asthma management system is currently being developed with the multidisciplinary ED team.
Limitations
The pediatric ED utilizes several information systems for patient care; this information system environment may not be typical for other EDs, limiting the generalizability of the findings. However, the project examines a new approach to increase guideline utilization and adherence, which may provide additional insights for potential approaches for delivering guideline-based care.
The system demonstrates that it is possible to leverage different information technology applications to create an integrated approach for an asthma reminder system. Having access to such an infrastructure allows the design of processes that may be easier to use, “simple,” and “do not stop clinicians,” but rather change a clinician’s direction16. In addition, the user-driven development created a workflow-suitable approach that supported the acceptance among the busy ED clinicians.
Acknowledgments
This work was supported by LM 009747-01 and NHLBI K23 HL80005. The first author was supported by a Training Grant from the NLM (T15 LM 007450-03).
REFERENCES
- 1.http://www.cdc.gov/nchs/FASTATS/asthma.htm [Accessed 9 March 2009]
- 2.Allergy & Asthma Advocate. Quarterly patient newsletter of the American Academy of Allergy, Asthma and immunology. 2004.
- 3.Akinbami LJ.The State of childhood asthma, United States, 1980–2005 Advance data from vital and health statisticsno. 381Hyattsville, MD: National Center for Health Statistics; 2006 [PubMed] [Google Scholar]
- 4.Grimshaw JM, Eccles MP, Walker AE, Thomas RE. Changing physicians' behavior: what works and thoughts on getting more things to work. J Contin Educ Health Prof. 2002;22:237–243. doi: 10.1002/chp.1340220408. [DOI] [PubMed] [Google Scholar]
- 5.Scribano PV, Lerer T, Kennedy D, Cloutier MM. Provider adherence to a clinical practice guideline for acute asthma in a pediatric emergency department. Acad Emerg Med. 2001;8:1147–1152. doi: 10.1111/j.1553-2712.2001.tb01131.x. [DOI] [PubMed] [Google Scholar]
- 6.National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the diagnosis and management of asthma. 1997.
- 7.Porter SC, Cai Z, Gribbons W, et al. The asthma kiosk: a patient–centered technology for collaborative decision support in the emergency department. J Am Med Inform Assoc. 2004;11:458–67. doi: 10.1197/jamia.M1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Porter SC, Forbes P, Feldman HA, Goldmann DA. Impact of patient-centered decision support on quality of asthma care in the emergency department. Pediatrics. 2006 Jan;117(1):e33–42. doi: 10.1542/peds.2005-0906. [DOI] [PubMed] [Google Scholar]
- 9.Qureshi F, Pestian J, Davis P, Zaritsky A. Effect of nebulized ipratropium on the hospitalization rates of children with asthma. N Engl J Med. 1998 Oct 8;339(15):1030–5. doi: 10.1056/NEJM199810083391503. [DOI] [PubMed] [Google Scholar]
- 10.Sanders DL, Aronsky D. Detecting asthma exacerbations in a pediatric emergency department using a Bayesian network. Proc AMIA Symp. 2006:684–688. [PMC free article] [PubMed] [Google Scholar]
- 11.Sanders DL, Gregg W, Aronsky D. Identifying asthma exacerbations in a pediatric emergency department: A feasibility study. Int J Med Inform. 2007 Jul;76(7):557–64. doi: 10.1016/j.ijmedinf.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Giuse DA. Supporting communication in an integrated patient record system. AMIA Annu Symp Proc. 2003:1065. [PMC free article] [PubMed] [Google Scholar]
- 13.Levin S, France D, Aronsky D. The Effects of Computerized Triage on Nurse Work Behavior. AMIA Annu Symp Proc. 2006:1005. [PMC free article] [PubMed] [Google Scholar]
- 14.Miller RA, Waitman LR, Chen S, et al. The anatomy of decision support during inpatient care provider order entry (CPOE): empirical observations from a decade of CPOE experience at Vanderbilt. J Biomed Inform. 2005;38:469–85. doi: 10.1016/j.jbi.2005.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aronsky D, Jones I, Lanaghan K, Slovis CM. Supporting patient care in the emergency department with a computerized whiteboard system. J Am Med Inform Assoc. 2008;15:184–94. doi: 10.1197/jamia.M2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10:523–30. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]