Abstract
Patient falls are serious problems in hospitals. Risk factors for falls are well understood and nurses routinely assess for fall risk on all hospitalized patients. However, the link from nursing assessment of fall risk, to identification and communication of tailored interventions to prevent falls is yet to be established. The Fall TIPS (Tailoring Interventions for Patient Safety) Toolkit was developed to leverage existing practices and workflows and to employ information technology to improve fall prevention practices. The purpose of this paper is to describe the Fall TIPS Toolkit and to report on strategies used to drive adoption of the Toolkit in four acute care hospitals. Using the IHI “Framework for Spread” as a conceptual model, the research team describes the “spread” of the Fall TIPS Toolkit as means to integrate effective fall prevention practices into the workflow of interdisciplinary caregivers, patients and family members.
Keywords: fall prevention, patient safety, fall risk assessment, acute care, caregiver
Background and Significance
Patient falls in hospitals are a leading cause of preventable injury. Patient falls and patient falls with injury are considered “nursing sensitive” and are employed nationally as standard metrics of nursing care quality. [1] The unfamiliar environment, acute illness, surgery, bed rest, medications, treatments and the placement of various tubes and catheters are common challenges that put patients at risk for falls. Falls are devastating to patients, family members, and providers. A single fall may result in a fear of falling that can begin a downward spiral of reduced mobility, leading to loss of function and elevated risk for falls. The most rigorous research to date has been in the area of fall risk assessment. As a result, risk factors associated with falls are well established. However, the link from nursing assessment of fall risk to identification and communication of tailored interventions to prevent falls is yet to be established.[2]
Rethinking Fall Prevention in hospitals: Fall TIPS
Reducing patient falls is a high priority goal for Partners HealthCare System (PHS) in Eastern, MA. Over the past five years, nurses from the PHS Fall Prevention Task Force have worked to standardize fall risk assessment and evaluation metrics across PHS hospitals. In 2007, a nurse led research team was awarded a Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative grant to develop and test a fall prevention toolkit (e. g., “Fall TIPS”). Fall TIPS aims to establish evidence based linkages between routine nursing fall risk assessment, and structured communication and tailored interventions to prevent patient falls in acute care hospitals.
Early in the study, a nurse scientist conducted focus group interviews of professional and paraprofessional caregivers to explore existing barriers, facilitators and interventions used to prevent falls. In addition, interviews were conducted with patients who had fallen while in the hospital. A content analysis of interview transcripts revealed that while nurses routinely assess their patients’ risk for falls, communication related to fall risk status and communication of the plan to prevent falls was inconsistent. [3] Variable communication was identified as a major barrier to the collaboration and teamwork that participants said was needed to prevent patient falls. “High risk for fall” signs were routinely hung in patient rooms to alert caregivers of a patient’s risk status. However, nurses and paraprofessional caregivers reported that these signs were too common and too generic to be useful. Even when a fall prevention plan did exist in the patient record, this information was not available to all caregivers or patients at the bedside. Neither nursing assistants who may provide care before receiving report nor family members who often spend a great deal of time with patients had access to the patient’s fall prevention plan. Therefore, they did not know how to assist the patient with routine activities such as toileting or what they could do to prevent falls. In addition, patients identified the loss of balance in the context of an urgent need to reach the bathroom as a common reason for falling. [4]
The Fall TIPS Toolkit: Bringing fall prevention guidelines to the bedside
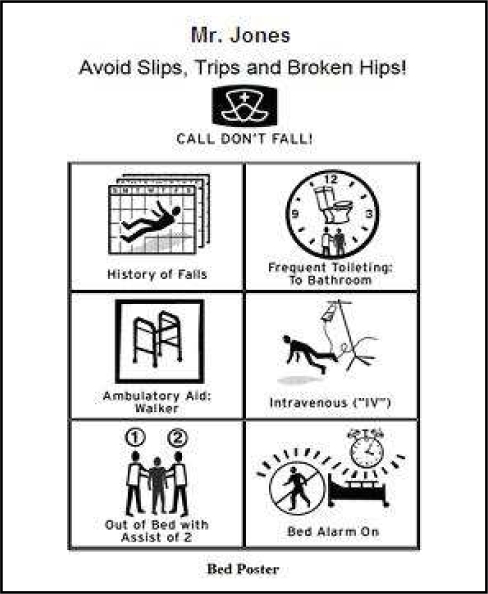
Based on the requirements gathered in the interviews, the research team worked with programmers and end users to build Fall TIPS, a platform-independent fall prevention toolkit. Fall TIPS leverages existing practices and workflows (e. g., routine nursing fall risk assessment, use of signs to alert caregivers to fall risk status) and makes use of information technology to promote the use of evidence based fall prevention practices (e.g., tailoring display of alerts based on risk status). Using the Fall TIPS toolkit, nurses document the fall risk assessment online. The Fall TIPS software identifies a core set of evidence-based interventions directly linked to the patient-specific risk factors. The nurse has the ability to further tailor interventions based on knowledge of the patient. The nursing assessment data and the associated tailored interventions are then processed by the Fall TIPS software to generate three patient-specific fall prevention tools; a bed poster, a plan of care and an educational handout for patients and family members. In hospitals where there is a paper record in place, all three forms automatically print when the nurse completes the initial fall risk assessment. In hospitals where an electronic record is in place, the bed poster and educational handout are printed and the interdisciplinary plan of care populates the electronic record. Figure 1 is an example of a tailored bed poster for a patient who is at high risk for falls. Note that in addition to conveying risk status, the bed poster includes actionable alerts that relate to patient-specific areas of risk; the need for frequent toileting, assistance with getting out of bed and cognitive limitations. The icons were developed and validated with professional and paraprofessional caregivers to ensure that images communicate actionable alerts related to risk status and tailored interventions across literacy levels. This feature distinguishes the “Fall TIPS bed posters” from the typical “high risk for falls signs” used in many hospitals.
Figure 1:
Fall TIPS Bed Poster
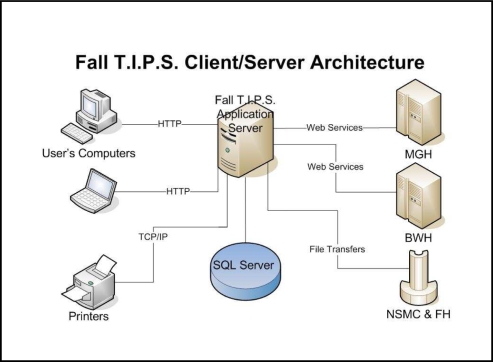
The Fall TIPS Technology
The Fall TIPS toolkit application employs HTML, JavaScript and .NET technologies. In addition, DHTML (e.g., “Dynamic” HTML) and JavaScript are used to dynamically build the patient-specific fall prevention tools. Fall TIPS is a web-based ASP.NET application. OAP (Simple Object Access Protocol) web services are used to retrieve patient information from the study entities. Data selected in the Fall TIPS toolkit at each site are stored in a SQL server database. A file transfer protocol is used to retrieve fall risk assessment data recorded in vendor-based applications at the community hospitals and client side printing technology is used at the medical centers (see Figure 2).
Figure 2:
Fall TIPS Client/Server Architecture
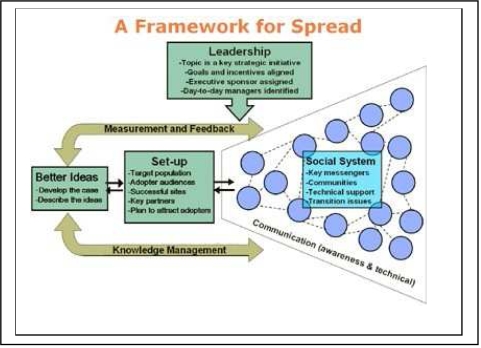
Conceptual Framework: Framework for Spread
The conceptual framework used for the Fall TIPS Toolkit implementation was the Institute for Healthcare Improvement’s Framework for Spread. The Framework for Spread[5] is based on Roger’s Diffusion of Innovations theory[6] which holds that diffusion of innovations is a process and requires the communication or spread of messages over time to members of a social system. The Framework for Spread occurs over three phases (1) planning and setup, 2) spread within the target population and 3) continuous monitoring and feedback of the spread process. The underpinnings of the Framework for Spread include leadership, set-up for spread, better ideas, communication, social system, knowledge management, and measurement and feedback. (See Figure 3). Use of these factors to promote effective spread of the Fall TIPS Toolkit is outlined in Table 1.
Figure 3:
Framework for Spread [5]
Table 1:
Fall TIPS Toolkit (FTTK) Spread Strategy
| “Spread for Change” Component1 | Fall TIPS Toolkit (FTTK) Spread Strategy |
|---|---|
| Leadership: Setting the agenda and assigning responsibility for spread |
|
| Set-Up for Spread: Identifying the target population and the initial strategy to reach all sites in the target population with the new ideas |
|
| Better Ideas: A description of the new ideas and evidence to “make the case” to others |
|
| Communication: Methods to share awareness and technical information about the new ideas |
|
| Social System: Understanding the relationships among the people who will be adopting the new ideas |
|
| Knowledge Management: Observing and using the best methods for spread as they emerge from the practice of the organization |
|
| Measurement and Feedback: Collecting and using data about process and outcomes to better monitor and make adjustments to spread progress |
|
“Framework for Spread” Fall TIPS Toolkit Adoption Measures
The Fall TIPS Toolkit has been in place on experimental units in four PHS hospitals since November 2008. To evaluate “spread” or adoption of the Fall TIPS Toolkit, we are evaluating the following:
percent of patients for whom a fall risk assessment was completed within the past 24 hours (assessed during weekly safety rounds)
percent of patients for whom one or more of the Fall TIPS tools are printed
percent of patients with a tailored Fall TIPS poster hanging above their bed (assessed during weekly safety rounds)
percent of patients for whom the nurse uses the Fall TIPS toolkit to tailor fall prevention interventions (automatic and manual)
frequency with which nurses use the toolkit to complete a fall risk assessment
Additional long term outcome measures being tracked are included in Table 2. These measures will provide information about nurse satisfaction with the toolkit and identify recommendations for improvement from the perspectives of professional and paraprofessional caregivers, patients and family members. Moreover, data derived from these measures will provide a means to evaluate the effectiveness of the Fall TIPS toolkit for improving nurses’ and paraprofessionals’ self-efficacy (e.g., confidence that they can prevent patient falls), and for reducing patient falls and fall with injury.
Table 2:
Fall TIPS Outcome Measures
| Measure | Method for data capture |
|---|---|
| 1. Patient falls/1000 patient days | Standard measure. Data submitted by each hospital’s quality department |
| 2. Patient falls with injury/1000 patient days | Standard measure. Data submitted by each hospital’squality department |
| 3. Nurse “Fall Prevention Self-efficacy” | Survey |
| 4. Paraprofessional “Fall Prevention Self-efficacy” | Survey |
| 5. Nurse Satisfaction | Survey |
| 6. Recommendations for improvement of Fall TIPS toolkit | Focus groups (Professional, paraprofessional caregivers, patients/family members) |
To test its efficacy, a cluster randomization design was utilized in four Partners hospitals. In particular, we have two units within each of the four hospitals, with one unit within a hospital randomized to the intervention, and the other unit within the hospital randomized to usual care.
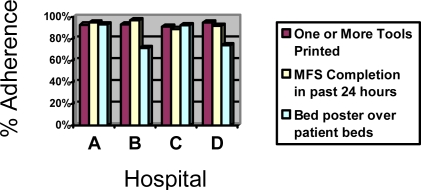
Results to Date
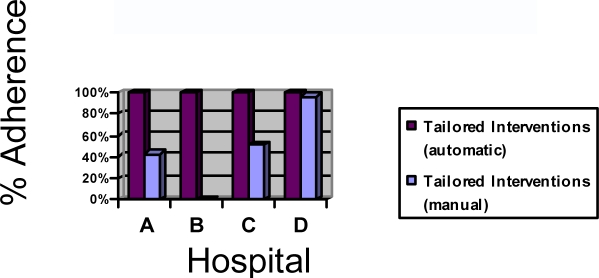
At this time, N=685 patients have been on the units using the Fall TIPS toolkit (N=142 in Hospital A, N=208 in Hospital B, N=170 in Hospital C, N=165 in Hospital D), Adherence with the “Framework for Spread” Toolkit adoption measures ranges from 72% (percent of patients with a tailored Fall TIPS poster hanging above their bed, Hospital B) to 97% (% patients for whom a fall risk assessment was completed within the past 24 hours during weekly safety rounds, Hospital B). In addition, we are tracking the percent of patients where the interventions are tailored to individual patient determinants of risk. The Fall TIPS toolkit automatically tailors interventions for all patients based on fall risk assessment, but in hospitals A, C and D, nurses can further tailor, based on their knowledge of the patient. For example, based on the toolkit logic, if the nurse identifies “Intravenous (IV)/Heparin Lock” as a risk factor, “provide assistance with IV pole” is generated as a tailored intervention. For patients who have a heparin lock only, the nurse can de-select this intervention so that the icon to alert caregivers to provide assistance with the IV pole is not included on the bed poster and other Fall TIPS tools. In hospital B, this functionality is not available due to constraints of the vendor software. Results for all “spread” or adoption measures are included in Figures 4–5. In addition, significant improvement has been noted across hospitals as the mean number of fall risk assessments completed by nurses using the Fall TIPS Toolkit per patient, per day has increased by 25% across sites from first month after implementation to current practice (from 1.7 pre to 2.0 the first month, p<. 003).
Figure 4–5:
“Framework for Spread” Fall TIPS Adoption Measure Results
Discussion
The Fall TIPS Toolkit was developed using an iterative approach with toolkit requirements coming directly from end-users including professional and paraprofessional caregivers, patients and family members. Since implementation of the Fall TIPS Toolkit on experimental units, feedback from end-users is positive. However, even well designed innovations which are successful in one location, may fail in different organizations or settings. [7] Due to the complex, fast paced work flows that exist in acute care hospitals, adoption and spread of new innovations is often challenging for even well designed systems. The Fall TIPS toolkit was implemented on experimental units in four acute care hospitals, each with unique communication and information systems. A key challenge was to identify a framework for implementation that would facilitate spread and adoption across diverse sites.
The IHI Framework for Spread provided an organized approach to implementation and a multifaceted Fall TIPS Toolkit adoption strategy that promotes engagement across all levels of the organization. Key components of the Framework for Spread including an expectation for adoption communicated by PHS leaders, chief nursing officers, and unit leadership set the tone for successful diffusion. Involvement of unit-based “peer champions” in usability and pilot testing supported the “set-up for spread” efforts by communicating and demonstrating the advantages of using the Fall TIPS toolkit in the context of typical patient care workflows. Regular measurement and consistent feedback to end-users about performance serves as a means to reinforce effective fall prevention practices and further integrate the Fall TIPS Toolkit into the workflow.
As with all new innovations, there are challenges associated with implementing the Fall TIPS Toolkit. Changing behavior and practice is difficult, even when the rationale and methods for change are embraced by caregivers. Nurses and other caregivers in acute care hospitals are busy. The patients are sick and the workflows are complex. In addition to the Fall TIPS toolkit, professional and paraprofessional caregivers are continuously barraged with new policies, systems and innovations that they are pressured to implement. This type of environment demands that if innovations are to be adopted, they must be thoughtfully introduced using a framework that provides the communication, peer support, feedback and time needed to assure an effective transition to adoption, culture change and sustained improvement.
There are several limitations associated with this work. While the “Framework for Spread” Fall TIPS Adoption Measure results suggest that the toolkit is being used, it has been in place for a relatively short period of time and is currently on experimental units only. Once the randomized evaluation of the Fall TIPS Toolkit is complete, it will be made available across all PHS hospitals. It is unknown whether the same techniques will have similar results with a larger implementation over a long period of time.
Conclusion
Patient falls are serious problems in hospitals. The Fall TIPS Toolkit was developed to leverage existing practices and workflows and to employ information technology to promote the use of evidence based interventions to prevent falls. The IHI “Framework for Spread” was employed as a means to “spread” the Fall TIPS Toolkit and to integrate effective fall prevention practices into the workflow of interdisciplinary caregivers, patients and family members at PHS hospitals. Early results based on the “Framework for Spread” Fall TIPS Adoption Measure set suggest that the level of adoption on experimental units is reasonable. However, the degree to which sustained adoption and practice changes will be maintained over time is unknown. It is hoped that the “Framework for Spread” strategies will maintain toolkit adoption and sustain best fall prevention practices and ultimately prevent patient falls in PHS hospitals.
Acknowledgments
The authors would like to thank the Robert Wood Johnson Foundation support of this research and the nurses and nursing leadership across PHS hospitals for their role in spread and adoption of the Fall TIPS Toolkit.
References
- 1.Patient Safety, National Patient Safety Goals 2009[cited 2/28/09]; Available from: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals
- 2.Oliver D. Preventing falls among older people in hospital: interpreting the null result. BMJ. 2008;336(7649):847. doi: 10.1136/bmj.39549.430162.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dykes P, et al. Why do Patients in Acute Hospitals Fall? Can Patient Falls be Prevented? JONA. 2008. In press. [DOI] [PMC free article] [PubMed]
- 4.Carroll D, Dykes P, Hurley A. Patients’ Perspectives of Falling While in an Acute Care Hospital and Suggestions for Prevention. Journal of Applied Nursing Research. 2008. In press. [DOI] [PMC free article] [PubMed]
- 5.IHI A Framework For Spread 2009[cited2/28/09]; Available from: http://www.ihi.org/IHI/Topics/Improvement/SpreadingChanges/Changes
- 6.Rogers E. Diffusion of Innovations. 5th ed. New York: Free Press; 2003. [Google Scholar]
- 7.Berwick DM. Disseminating innovations in health care. Jama. 2003;289(15):1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]