The risks of a first occurrence and a recurrence of neural tube defects have been shown to be reduced by periconceptionalfolic acid supplementation—that is by taking folic acid from 3 months before conception to 3 months after conception.1,2 The Expert Advisory Group in the United Kingdom recommended in 1992 that women who were trying to conceive should take 0.4 mg folic acid per day.3 We assessed whether there had been any change in the incidence of neural tube defects since this recommendation was made.
Methods and results
The number of live births, stillbirths, and pregnancies terminated because the fetus had a neural tube defect (spina bifida, anencephaly, or encephalocele) as well as the total number of live births, stillbirths, and abortions among residents of England and Wales from 1972 to 1996 were obtained from the Office for National Statistics. The true incidence of these abnormalities was defined as the number of affected infants (born alive or dead) plus the number of pregnancies terminated after prenatal diagnosis of a neural tube defect and expressed as a proportion of 100 000 live births, stillbirths, and terminations for neural tube defects. The number of prescriptions dispensed and the number of preparations sold over the counter containing 400 μg to 500 μg folic acid were provided by the Department of Health and Self Medication UK, a department of Intercontinental Medications Statistics-Health, (Pinner, Middlesex), respectively. The total number of prescriptions dispensed was available but data for over the counter sales do not include information from Boots pharmaceutical stores because they do not provide this information.
The incidence of each defect was modelled against the calendar year using a logarithmic transformation of the incidence. To assess whether rates of decline have been more rapid since 1992, a term was added to the model to reflect the number of years since 1992. Further analyses in which a square root was used instead of logarithmic transformation gave similar results. All models were fitted using the sas statistical package.
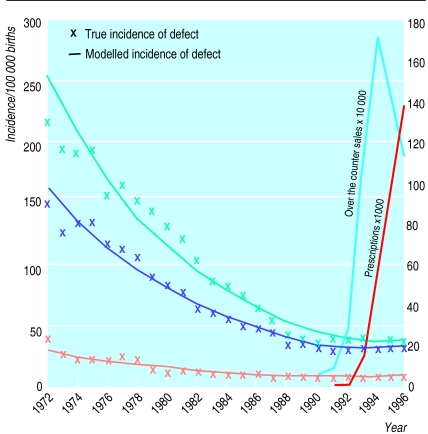
Before 1992 there was a significant drop in the incidence of each of the defects (P=0.0001 for each abnormality) (figure). The incidence of spina bifida fell from 215/100 000 in 1972 to 38/100 000 in 1991; the incidence of anencephaly fell from 149/100 000 to 29/100 000; and the incidence of encephalocele fell from 39/100 000 to 9/100 000. Since 1992 the rates of decline have stabilised and the decline was significantly less rapid than before 1992 (P=0.002 for spina bifida, P=0.0001 for anencephaly, and P=0.03 for encephalocele). The number of prescriptions of folic acid dispensed increased between 1992 and 1996, and over the counter sales increased between 1990 and 1994 and declined in 1995-6.
Comment
The incidence of neural tube defects has been decreasing since the early 1970s. Our study shows that although there has been a large increase in the number of prescriptions dispensed and preparations sold over the counter of folic acid since 1992 in England and Wales, the rate of decline in the true incidence of neural tube defects has slowed. Although periconceptional supplementation with folic acid has been shown to be effective in randomised controlled trials, no reduction in the incidence of neural tube defects has yet occurred. Supplementation may not be taken at the right time,4 or may not be taken by those women who are at the highest risk, or the recommended dose may be too low. It is also possible that the incidence of these defects has reached such a low level that it is not possible to achieve further reduction through supplementation or that a longer interval is required to show the true effect of supplementation on the incidence. Our study is observational, and we do not know what the incidence would have been in the absence of folic acid supplementation. Additionally, sales and prescriptions may not represent the actual use of folic acid. There is a need for continued health education on the use of folic acid before pregnancy or immediately after conception in unplanned pregnancies.
Figure.
True incidence and modelled incidence of spina bifida (blue), anencephaly (purple), and encephalocele (orange) per 100 000 births in England and Wales, 1972-96, and number of prescriptions dispensed and preparations sold over the counter containing 400μg to 500 μg of folic acid, 1992-6
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council vitamin study. Lancet. 1991;338:131–137. [PubMed] [Google Scholar]
- 2.Czeizel AE. Prevention of congenital abnormalities by periconceptional multivitamin supplementation. BMJ. 1993;306:1645–1649. doi: 10.1136/bmj.306.6893.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Report from an Expert Advisory Group (1992) on folic acid and the prevention of neural tube defects. London: Department of Health; Scottish Office Home and Health Department; Welsh Office; Department of Health and Social Services, Northern Ireland, 1992.
- 4.McGovern E, Moss H, Grewal G, Taylor A, Bjornsson S, Pell J. Factors affecting the use of folic acid supplements in pregnant women in Glasgow. Br J Gen Pract. 1997;47:635–637. [PMC free article] [PubMed] [Google Scholar]