Abstract
The purpose of this study was to develop and test a structural model explaining medication compliance of schizophrenia. From a review of the literature, a hypothetical model was developed based on the conceptual framework of the Health Belief Model with medication knowledge, symptom severity and social support as the exogenous variables, and perceived benefits, perceived barriers, substance use and medication compliance as the endogenous variables. Data was collected at various mental health facilities, including psychiatric outpatient clinics of general hospitals and community mental health centers, between March and May, 2001. A structured questionnaire was used by one- on- one interviews to collect data on 208 schizophrenic patients. Well established measurement instruments, with confirmed reliability, were used to assess each method variable. As a result of covariance structural analysis, the hypothetical model was found not to fit the empirical data well, so a parsimonious model was adopted after modifying the model. The final model was able to explain the 33% medication compliance. Medication knowledge, social support and perceived benefits had significant effects on medication compliance. The findings of this study address the importance of medication education and social support to promote medication compliance. It is also suggested that various education programs and support groups are needed to enhance medication compliance.
Keywords: Medication compliance, schizophrenia
INTRODUCTION
Medication compliance is essential in managing the psychotic symptoms of schizophrenic patients. However, it has been reported that 65.8% of mentally ill patients had experiences of taking their medication at different times and with different dosages from those prescribed by their doctor.1 Medication noncompliance leads to a relapse of symptoms and rehospitalization. A relapse rate of 16% over one year was reported when schizophrenic patients took their medication as their doctors ordered, but this was 74% when the prescribed regimen was not followed.2
Many variables influencing medication compliance in the mentally ill have been identified from prior studies. Medication knowledge,3-5 symptom severity,6-8 social support,9-11 perceived benefits12-14 and barriers,15-17 and substance abuse18-19 have all been well identified as variables influencing medication noncompliance. When patients had no knowledge of their medication, their psychiatric symptoms were serious, but when social support was received from their family, friends and health care providers, medication noncompliance was higher. Alcohol and drug use also interfere with medication compliance.
Even though these variables are well known, prior studies have only revealed the direct effects of these variables on medication compliance; thus, which variables are most influential and important remain unknown. Therefore, the factors influencing medication compliance, and to what degree, either direct or indirect, needs to be examined.
Thus, the development of a comprehensive model explaining chronic schizophrenic patients' medication compliance is required. The more variables included in the model, the higher the explanation power. However, to develop a precise and concise model, it is necessary to involve the most influential variables.
The purpose of this study was to develop a comprehensive and parsimonious model explaining a schizophrenic patients' medication compliance. The model should have a theoretical basis, so that it will be possible to enhance intervention for increased medication compliance.
CONCEPTUAL FRAMEWORK AND A HYPOTHETICAL MODEL
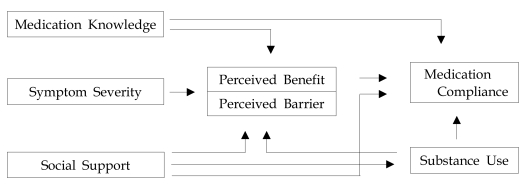
Conceptual framework
The conceptual framework of this study consisted of variables identified through a review of the literature as major factors directly or indirectly influencing medication compliance. The concept of Becker's (1974) health belief model,20 in which medication compliance is seen as a behavior for improving one's health, was used (Fig. 1). This model has two assumptions: First, that one has a need to avoid or recover from illness; second, one performs a specific behavior to prevent an illness. The Health Belief Model is applicable and useful for psychiatric patients as they perform specific behaviors, such as taking their medication to get over their mental illness.
Fig. 1.
Conceptual framework.
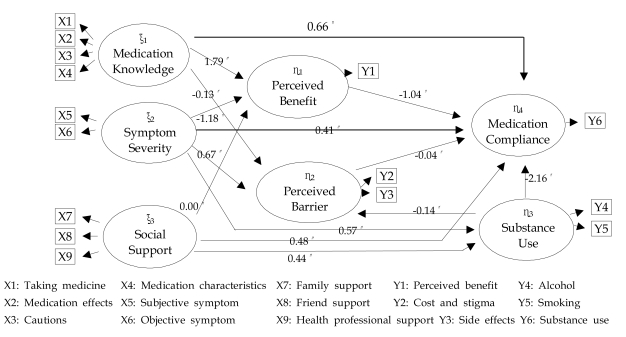
Hypothetical model
The hypothetical model consisted of three exogenous variables (medication knowledge, symptom severity, and social support) and four endogenous variables (perceived benefit, perceived barrier, substance use, and medication compliance). The exogenous variables were independent variables influencing the endogenous variables either directly or indirectly. A total of 14 hypothetical paths were established (Fig. 2).
Fig. 2.
Path coefficient of the hypothetical model.
MATERIALS AND METHODS
Subjects
The criteria for the study subjects were as follows:
1) Adult schizophrenic patients between the age of 18 and 65 years, diagnosed with a schizophrenia for at least 6 months.
2) A total score on the MMSE (Mini Mental State Examination) over 25 in order to understand the questions and correctly answer the questionnaire.
3) Patients currently receiving psychiatric treatment and taking medication.
4) Those currently residing in the community. Hospitalized patients were not involved in the sample as hospitalization affects medication compliance.
5) Patients had to verbally agreed to participate in the study
Data collection
A pilot study was undertaken to ascertain if all of the questions were understandable, then the questionnaire was administered, on a on-to-one basis, to 34 patients meeting the sample selection criteria before further study was conducted. Participants were asked which questions they found difficult or did not understand, with feedback on those items used to modify the questions of easier understanding.
Data were collected between March and May, 2001 through one-on-one interviews. To decrease the sample error, eight provinces were used for data, which was carried out in three general hospital out patients' clinics, five community mental health centers in different provinces, one community public health center, one day care center, one doctor's clinic, and in patients' homes. Before going to the mental health care facilities for data collection, the purpose and method of the study was explained to representatives of each facility by letter and phone, and permission received for collecting the data. The purpose of the study was explained to each participant, and those agreeing to participate were interviewed by the researcher.
A total of 244 patients meeting the subject selection criteria were interviewed and completed the questionnaire. However, 36 participants' family members were unable to be reached by phone to measure medication compliance; thus, a total of 208 participant's questionnaires were used for the analysis. A one-on-one interview for the questionnaire was undertaken by the researcher, which took 30-40 minutes to complete.
Instruments
Medication knowledge
A total of 14 questions were asked relating to medication knowledge, which was initially presented by Harbor et al. (1996).21 Each question was answered either 'yes', 'no', or 'don't know', with total scores ranging from 0 to 14; the higher the score, the greater the stress.
Symptom severity
Symptom severity was measured on the BPRS (Brief Psychiatric Rating Scale) developed by Overall et al. (1962).22 This questionnaire consisted of 18 questions, divided into two parts. One part measured the subjective symptoms, such as degree of anxiety and depression, which consisted of 9 questions. The second part also consisted of 9 questions, and measured the researchers' observations relating to slow movement and non cooperation, etc. The score range of each question was from 1 to 7, with the total scores ranging from 18 to 126; the higher the score, the greater the severity of the symptom. The Cronbach's alpha was 0.95 in this study.
Social support
Sarason's (1983) social support questionnaire23 was used to measure family, friend and health care provider support. A total of 8 questions were asked, including the degree of satisfaction about people they can trust, with each question having a 6-point Likert style answer, from 'very unsatisfied' to 'very satisfied'. The total scores ranged from 8 to 48; the higher the score, the greater the degree of social support. The Cronbach's alpha in the study was 0.92.
Perceived benefit
The perceived benefit refers to the good things that can be attained by medication compliance, which was measured using a modified Korean version of Moon's (1990) health belief questionnaire24 for Korean adults; 6 questions were included in this questionnaire: symptom improvement, decreasing the chance for relapse and improvement of interpersonal relationship, etc. having a 5-point Likert scale. The total scores ranged from 6 to 30; the higher the score, the greater the perceived benefits. The Cronbach's alpha in this study was 0.84.
Perceived barrier
The perceived barriers refer to the difficulties experienced by a person, which were addressed by five items: medication side effects, price, avoiding people's eye, visiting the hospital regularly and trying to follow medication times. This was measured using a modified Korean version of Moon's (1990) health belief questionnaire24 for Korean adults. Each question had a 5-point Likert scale; with the answers ranging from 'very likely' to 'unlikely'. The total scores ranged from 5 to 25; the higher the score, the greater the perceived barriers. The Cronbach's alpha in this study was 0.65.
Substance use
Substance refers to the psychoactive chemical agents. The substance use questionnaire, developed by the Ministry of Culture and Athletics (1996), was used.25 The amount of alcohol and cigarette uses per day and per month were measured, with the degree of alcohol use converted to alcohol content; the higher the score, the greater the participant's use of alcohol and cigarettes.
Medication compliance
Medication compliance refers to the behavior of taking the correct medication and dose at the correct time, as prescribed the participant's doctors. This was measured in two ways, by selfreporting and from family member's report. The question, 'what age percent have you taken your medication in the past one month? Answer 100% if you took all medication as your doctor prescribed', was asked to the patient. The question, 'what age percent has your ill family member taken his/her medication in the past month? Answer 100% if they took the medication as their doctor prescribed', was asked to the participant's family. When it was not possible to contact the participant's family, a data collection phone interview of the participant's family member was carried out, with the patients' consent. The mean of the two scores (patient and family) was the participant's final medication compliance score; the higher the score, the greater the medication compliance.
Data analysis
The SPSS PC 11.0 Program was used for descriptive statistics, and LISREL 8.12 for covariance analysis for coincidence testing of the hypothetical and modified models.
RESULTS
Demographic characters
There were 126 males (60.8%) and 82 females (39.2%), with a mean age of 38.89 years and a mean age at the onset of schizophrenia of 24.47 years. The mean illness and medication periods were 11.4 and 9.4 years, respectively.
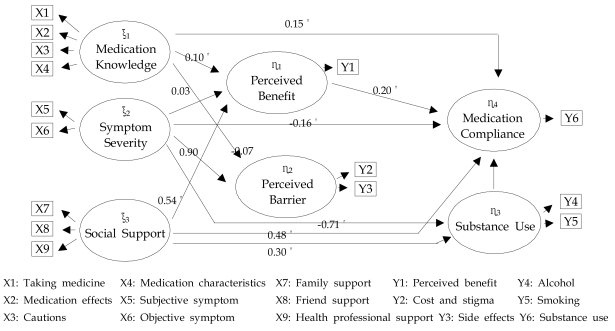
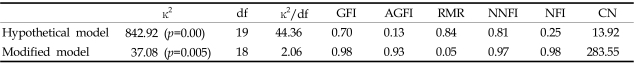
The effects and squared multiple correlation of the hypothetical model
Medication knowledge, symptom severity, perceived benefit and substance use had significant direct effects on medication compliance, with an explanation power of 89%; however, the indices of the hypothetical model did not fit well. Therefore, the model was modified (Table 1).
Table 1.
Effects of Endogenous Variables for the Hypothetical Model
*p<.05 (|T|>1.96)
Testing hypothesis
The hypotheses including perceived benefits as endogenous variables were:
Hypothesis 1 : 'The greater the medication knowledge, the greater the perceived benefit' was supported as a direct effect (r=0.10, t=3.18); significant.
Hypothesis 2 : 'The more severe the symptoms, the greater the perceived benefit' was not supported as a direct effect (r=0.03, t=0.29) ; not significant.
Hypothesis 3 : 'The greater the social support, the greater the perceived benefits' was supported as a direct effect (r=0.54, t=8.08) ; significant.
The hypotheses including perceived barriers as endogenous variables were:
Hypothesis 4 : 'The greater the medication knowledge, the lower the perceived barriers' was not supported as a direct effect (r=-0.07, t=-1.95); significant.
Hypothesis 5 : 'The more severe the symptoms, the greater the perceived barriers' was supported as a direct effect (r=0.90, t=13.76); significant.
Hypothesis 6 : 'The greater the substance use, the greater the perceived barriers' was not supported, as this path was removed.
The hypotheses including substance use as an endogenous variable were:
Hypothesis 7 : 'The more severe the symptoms, the greater the substance use' was supported as a direct effect (r=0.71, t=11.41); significant.
Hypothesis 8 : 'The greater the social support, the lower the substance use' was not supported (r=0.30, t=5.45) ; even though the statistical value was effective, the direction of the effect coefficient did not coincide.
The hypotheses including medication compliance as an endogenous variable were:
Hypothesis 9 : 'The greater the medication knowledge, the greater the medication compliance' was supported as a direct effect (r=0.15, t=3.63); significant.
Hypothesis 10 : 'The more severe the symptoms, the greater the medication compliance' was not supported as a direct effect (r=-0.16, t=-1.80); not significant.
Hypothesis 11 : 'The greater the social support, the greater the medication compliance' was supported as a direct effect (r=0.48, t=7.72); significant.
Hypothesis 12 : 'The greater the perceived benefit, the greater the medication compliance' was supported as a direct effect (r=0.20, t=2.14); significant.
Hypothesis 13 : 'The lower the perceived barriers, the greater the medication compliance' was not supported, as this path was removed.
Hypothesis 14 : 'The greater the substance use, the greater the medication compliance' was not supported as a direct effect (r=0.07, t=1.87); not significant.
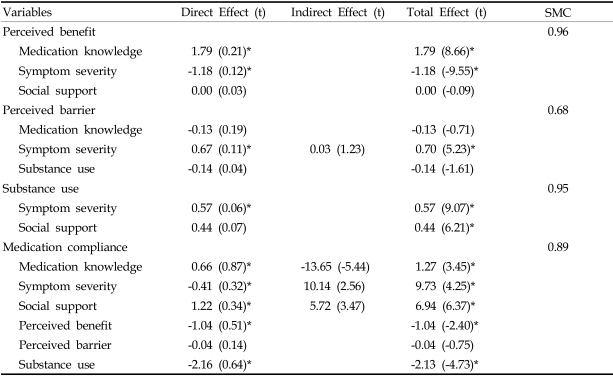
Modifying the hypothetical model
The modifying process or the model considered the conciseness, suitability, statistical significance and theoretical meaning. The variables with a correlation above 0.45 were used in the final analysis, which was the case with most of the variables in this study. Two paths were removed as their effects were weak and insignificant, and were found to decrease the suitability. These were 'how substance use affected perceived barriers' and 'how perceived barriers affected medication' (Fig. 3).
Fig. 3.
Path coefficient of the modified model.
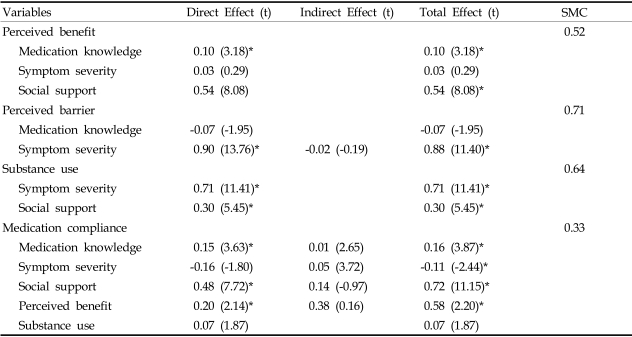
Fitness of the modified model
The chi-square value of the hypothetical model was too high (842.92), and the other indices also necessitated model modification. After modification, all indices indicating suitability and conciseness fitted to the model well, with all ×2 (37.08, df=18, p=0.005), GFI (0.98), AGFI (0.93), RMR (0.05), NNFI (0.97) and CN (283.55) values (Table 2).
Table 2.
Fitness of Indices
The effects and squared multiple correlation of the modified model
Among the medication knowledge, symptom severity and social support variables, which predict perceived benefits, medication knowledge and social support had significant direct effects, with an explanation power of 52%. Among the medication knowledge, symptom severity and substance use variables, which predict the perceived barriers, only symptom severity had a significant direct effect, with an explanation power of 71%. Both symptom severity and social support had significant direct effects on substance use, and both variables listed substance use as 64%. The endogenous variables, which predict medication compliance, were medication knowledge, symptom severity, social support, perceived benefits and substance use. Three variables of medication knowledge, social support, and perceived benefits had significant direct effects on medication compliance, with an explanation power of 33%; social support had the strongest direct effect among these variables (Table 3).
Table 3.
Effects of Endogenous Variables for the Modified Model
*p<.05 (|T|>1.96).
DISCUSSION
The model developed by structural equation analysis has to reflect reality and have theoretical validity.26 The aim of this study was to develop a concise, well fitted model to predict factors and explain their direct and indirect effects on medication compliance. Many variables influencing medication compliance in the mentally ill were identified through an extensive literature review.
Among the variables identified, six were found to have the most influence on medication compliance. The endogenous variables were medication knowledge, symptom severity and social support, with perceived benefits, perceived barriers and substance use as mediating variables. Medication compliance of chronic schizophrenic patients was directly affected by medication knowledge, social support and perceived benefits, with an explanation power for these variables of 33%.
Prior study results have not been consistent with regards to medication knowledge directly affecting medication compliance. One research report suggested that medication knowledge increased after a medication education program, which led to an increase in medication compliance.5 However, another study reported that medication education to schizophrenic patients did not change medication compliance, even though their medication knowledge had increased.27 Medication compliance was found to be directly affected by medication knowledge in this study. It is thought that most participants attended an outpatient treatment care center, where they were repeatedly educated about the effects and side effects of the medication and the importance of taking medication for preventing a relapse; thus, they knew about their medication and it increased compliance.
Social support has consistently been identified as a reinforcement factor for medication compliance through prior studies.28,29 However, the extent to which social support predicts medication compliance has not been identified. The finding of this study, that social support was the most powerful predictor of influences on medication compliance in chronic schizophrenic patients, is new. Thus, strengthen social support is suggested, for which various strategies need to be developed that involve families, friends and health care professionals.
Perceived benefits come from the therapeutic effects of the antipsychotic agents, improvement in the symptoms, and relapse and rehospitalization prevention, and are determining factors of health behaviors. They can also be heightened by medication education, and complying patients have higher perceived benefits than noncompliant patients.30 From the findings in this study, it was clear that the perceived benefits are the second strongest variables for predicting medication compliance. Thus, it is also suggested that the medication's positive rather than negative effects, such as side effects, have to be reinforced.
Unlike other diseases, schizophrenic patients do not take their medication, as they lose their insight into illness and treatment. It was reported that the degree of insight was consistently related to the degree of medication compliance,31 so is suggested a variable that should be included in further study.
Also, severe psychotic symptoms lead to increases in medication dose and frequency, which impede medication compliance.32 Thus, symptom severity was an important factor that could decrease medication compliance in schizophrenia. However, this variable did not significantly predict medication compliance in this study. The mean BPRS score in this study was 27.45, which was very low in comparison to the original median BPRS score of 72.0, suggesting the symptoms were not that severe in most of the participants. The reason the BPRS was low was due to all the study participants residing in the community, not a hospital, so their symptoms were manageable and less severe. Thus, a very low BPRS did not have a significant effect on medication compliance in this study.
Substance use has been identified in prior studies as a major factor leading to medication noncompliance and most patients in psychiatric hospitals have a substance abuse history.33,34 With alcohol abuse, 62% of patients discontinued their medication, which increased the medication noncompliance eight fold.35 The study participants' amount of substance use was very low, so did not significantly affect medication compliance in this study. A small number of participants drank alcohol at a social drinking level. Cigarette smoking was not that significant either. Because most patients were involved in treatment settings, such as community mental health centers, outpatient clinics and public health centers, they knew it was harmful to use substances while on medication therapy.
Perceived barriers, such as health care cost, fear, side effects and accessibility,36 need to be overcome before beginning healthy behavior. Perceived barriers lead patients to believe that their medication is not helpful and has no benefits.37 However, perceived barriers did not significantly influence medication compliance in this study. The different results compared to prior studies were due to the study participants characteristics and cultural aspects. Chronic patients usually know how to deal with the side effects, and were under Medicaid support from the Korean government, so payment for medicine was not a major problem. Thus, it can be said that the difficulties encountered with taking medication for chronic schizophrenic patients were not significant enough to decrease medication compliance.
In this study, medication knowledge, social support and perceived benefits predicted both direct and indirect medication compliance. Thus, to strengthen medication compliance of chronic schizophrenic patients residing in the community, continuous education needs to be enhanced to increase medication knowledge and social support from families, health care persons, and friends.
The significance of this study lies in the development of a basis for theory for schizophrenic patients' medication compliance. However, our results are limited, and do not apply to hospitalized schizophrenics or those not involved in a treatment setting. Also, those patients that stay at home, without the involvement of a treatment setting, were not included in the study sample. Thus, the model developed in the study can only be applied to schizophrenic patients involved in a treatment setting. It is suggested that these patients should be included in a future study and a model developed that can be applied to all schizophrenic patients, irrespective of their environment. Developing various programs to enhance patients' medication compliance, and many intervention programs to heighten social support, have been suggested.
References
- 1.Ruscher SM, Wit R, Mazmanian D. Psychiatric patients' attitudes about medication and factors affecting noncompliance. Psychiatr Serv. 1997;48:82–85. doi: 10.1176/ps.48.1.82. [DOI] [PubMed] [Google Scholar]
- 2.Kissling W. Ideal and reality of neuroleptic relapse prevention. Br J Psychiatry Suppl. 1992;161:133–139. [PubMed] [Google Scholar]
- 3.Bond WS, Hussar DA. Detection methods and strategies for improving medication compliance. Am J Hosp Pharm. 1991;48:1978–1988. [PubMed] [Google Scholar]
- 4.Oh HJ. The burden and professional help for the family of the mental illness. J Korean Acad Nurs. 2000;30:202–212. [Google Scholar]
- 5.Harvey NS, Peet M. Lithium maintenance: Effects of personality and attitude on health information acquisition and compliance. Br J Psychiatry. 1991;158:200–204. doi: 10.1192/bjp.158.2.200. [DOI] [PubMed] [Google Scholar]
- 6.Drain J, Solomon P. Explaining attitudes toward medication compliance among a seriously mentally ill population. J Nerv Ment Dis. 1994;182:50–54. doi: 10.1097/00005053-199401000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz RC, Skaggs JL, Peterson S. Critique of recent empirical research on insight and symptomology in schizophrenia. Psychol Rep. 2000;86:471–474. doi: 10.2466/pr0.2000.86.2.471. [DOI] [PubMed] [Google Scholar]
- 8.Gao X, Nau DP, Rosenbluth VS, Woodward C. The relationship of disease severity, health beliefs and medication adherence among HIV patients. AIDS Care. 2000;12:387–398. doi: 10.1080/09540120050123783. [DOI] [PubMed] [Google Scholar]
- 9.Scott CS, Lore C, Owen RG. Increasing medication compliance and peer support among psychiatrically diagnosed students. J Sch Health. 1992;62:478–480. doi: 10.1111/j.1746-1561.1992.tb01227.x. [DOI] [PubMed] [Google Scholar]
- 10.Buchanan A. A two-year prospective study of treatment compliance in patients with schizophrenia. Psychol Med. 1992;22:787–797. doi: 10.1017/s0033291700038228. [DOI] [PubMed] [Google Scholar]
- 11.Razali MS, Yahya H. Compliance with treatment in schizophrenia: A drug intervention program in a developing program. Acta Psychiatr Scand. 1995;91:331–335. doi: 10.1111/j.1600-0447.1995.tb09790.x. [DOI] [PubMed] [Google Scholar]
- 12.Shon KH. A comparative study on relationship of social support, life events, and depression between psychiatric patients and normal subjects. Nurs Science. 1997;9:59–86. [Google Scholar]
- 13.Adams J, Scott J. Predicting medication adherence in severe mental disorders. Acta Psychiatr Scand. 2000;101:119–124. doi: 10.1034/j.1600-0447.2000.90061.x. [DOI] [PubMed] [Google Scholar]
- 14.Budd RJ, Hughes I, Smith JA. Health beliefs and compliance with antipsychotic medication. Br J Clin Psychol. 1996;35:393–397. doi: 10.1111/j.2044-8260.1996.tb01193.x. [DOI] [PubMed] [Google Scholar]
- 15.Janz NK, Becker MH. The Health belief model: A decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 16.Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: Empirical and clinical findings. Schizophr Bull. 1997;23:637–651. doi: 10.1093/schbul/23.4.637. [DOI] [PubMed] [Google Scholar]
- 17.Richardson MA, Simons-Morton B, Annegers JF. Effect of perceived barriers on compliance with antihypertensive medication. Health Educ Q. 1993;20:489–503. doi: 10.1177/109019819302000409. [DOI] [PubMed] [Google Scholar]
- 18.Reiger DA, Farmer ME, Rae DS. Comorbidity of mental disorders with alcohol and other drug abuse. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 19.Lee CS, Han ES, Hwang TY. Public mental health and community: psychosocial rehabilitation program for mentally ill. Kyoungido: Yongin psychiatric hospital; 1996. [Google Scholar]
- 20.Becker MH. The health belief model and personal health behavior. Health Educ Mono. 1974;2:324–473. [Google Scholar]
- 21.Harber J, Krainovich-Miller B, McMahon LA, Price-Hoskins P. Comprehensive Psychiatric Nursing. 5th ed. St. Louis: Mosby; 1996. [Google Scholar]
- 22.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 23.Sarason IG. Measuring health: A guide to rating scales and questionnaires. New York: Oxford Univ. Press; 1983. The social support questionnaire; pp. 867–869. [Google Scholar]
- 24.Moon JS. A study of instrument development for health belief of Korean adults[dissertation] Seoul: Yonsei Univ.; 1990. [Google Scholar]
- 25.Korean Ministry of Culture and Athlete. Current status of adolescent drug misuse and prevention strategies. Ministry of culture and athlete press; 1996. [Google Scholar]
- 26.Cho SB. LISREL structural equation model. Seoul: Young-Ji Press; 1996. [Google Scholar]
- 27.Hwang MS. The effects of medication education to schizophrenia patients medication knowledge and medication compliance[dissertation] Seoul: Yonsei Univ.; 1998. [Google Scholar]
- 28.Collins-Colon T. Do it yourself: Medication management for community based clients. J Psychosoc Nurs Ment Health Serv. 1990;28:25–29. doi: 10.3928/0279-3695-19900601-07. [DOI] [PubMed] [Google Scholar]
- 29.Ku MO, Lee EO. Health belief model and Korean chronic patients' sick role. J Korean Academy. 1990;29:49–63. [PubMed] [Google Scholar]
- 30.Shon KH, Park SS. Medication and symptom management education program for the rehabilitation of psychiatric patients in Korea: the effects of promoting schedule on self-efficacy theory. Yonsei Med J. 2002;43:579–589. doi: 10.3349/ymj.2002.43.5.579. [DOI] [PubMed] [Google Scholar]
- 31.Kim BY, Lee CW, Park CW. The relationship among insight, psychopathology and drug compliance in the schizophrenic patient. J Korean Neuropsychiatric Association. 1993;32:373–380. [Google Scholar]
- 32.Perkins DO. Adherence to antipsychotic medications. J Clin Psychiatry. 1999;60:25–30. [PubMed] [Google Scholar]
- 33.Owen RR, Fischer EP, Booth BM, Cuffel BJ. Medication noncompliance and substance abuse among patients with schizophrenia. Psychiatr Serv. 1996;47:853–858. doi: 10.1176/ps.47.8.853. [DOI] [PubMed] [Google Scholar]
- 34.Olfson M, Mechanic D, Hansell S, Boyer AC, Walkup J, Weiden PJ. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2000;51:216–222. doi: 10.1176/appi.ps.51.2.216. [DOI] [PubMed] [Google Scholar]
- 35.Pristach CA, Smith CM. Medication compliance and substance abuse among schizophrenia patients. Hosp Community Psychiatry. 1990;41:1345–1348. doi: 10.1176/ps.41.12.1345. [DOI] [PubMed] [Google Scholar]
- 36.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 37.Colom F, Vieta E, Martinez-Aran A, Reinares M, Benabarre A, Gasto C. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549–555. doi: 10.4088/jcp.v61n0802. [DOI] [PubMed] [Google Scholar]