Abstract
Background:
Despite increasing awareness of the long-term impact of pediatric stroke, there are few estimates of the costs of care. We examined acute and 5-year direct costs of neonatal and childhood stroke in a population-based cohort in Northern California.
Methods:
We obtained electronic cost data for 266 children with neurologist-confirmed strokes, and 786 age-matched stroke-free controls, within the population of all children (<20 years) enrolled in a large managed care plan from 1996 through 2003. Cost data included all inpatient and outpatient health service costs including care at out-of-plan facilities. Costs were assessed for 5 years after stroke, expressed in 2003 US dollars, and stratified by age at stroke onset (neonatal, defined as <29 days of life, vs childhood). Stroke costs were adjusted for costs in stroke-free age-matched controls.
Results:
Average adjusted 5-year costs for pediatric stroke are substantial: $51,719 for neonatal stroke and $135,161 for childhood stroke. The average cost of a childhood stroke admission was $81,869. The average birth admission cost for a neonatal stroke was $39,613; adjustment for control birth admission costs reduced this by only $4,792, suggesting the stroke accounted for 88% of costs. Even among neonates whose strokes were not recognized until later in childhood (“presumed perinatal strokes”), admission costs exceeded those of controls. Chronic costs were highest in the first year poststroke, but continued to exceed control costs even in the fifth year by an average of $2,016.
Conclusions:
The economic burden of neonatal and childhood stroke is both large and sustained.
GLOSSARY
- IQR
= interquartile range;
- IVH
= intraventricular hemorrhage;
- KPMCP
= Kaiser Permanente Medical Care Program;
- KPSS
= Kaiser Pediatric Stroke Study;
- LOS
= length of stay.
With the advent of noninvasive neuroimaging, stroke has been increasingly recognized and studied in children.1–8 Historical impressions that children recover well from stroke have been contradicted by recent studies that document a high rate of lifelong morbidity.1,6–9 Despite increasing awareness of poor long-term outcomes, data measuring the burden of this disease remain sparse.10–14
The cost of stroke has been extensively studied in adults, including analyses of hospital charges, direct costs, indirect costs, and lifetime costs of adult stroke.10,11,15 Such studies have been the basis for many important cost-effectiveness analyses for stroke prevention and treatment modalities.16–18 Childhood stroke cost data, however, are limited: there has been one published US cost analysis from a single children's hospital.19 The costs of neonatal stroke have yet to be addressed. The goal of this study was to measure the acute and long-term direct costs of childhood and neonatal stroke in a population of children enrolled in a large Northern Californian managed care plan that maintains comprehensive cost databases.
METHODS
Setting/study population.
We used a previously identified sample of confirmed pediatric stroke cases from the Kaiser Pediatric Stroke Study (KPSS).20,21 KPSS is a retrospective population-based cohort study that included all neonates and children (0–19 years of age) diagnosed with an ischemic or hemorrhagic stroke within the cohort of all 2.3 million children enrolled in Kaiser Permanente Medical Care Program (KPMCP) from January 1993–December 2003. Because individual-level cost data have been available only since 1996, the study period for this cost analysis was restricted to January 1996–December 2003. KPMCP is the largest nonprofit managed care organization in the United States, with 17 hospitals and 36 outpatient facilities in Northern California. It provides care for 30% of the population in the region and shares the general sociodemographic distribution of California except for an underrepresentation of socioeconomic extremes.22
Standard protocol approvals and patient consent.
We obtained approval from institutional review boards at both KPMCP and UCSF prior to initiation of the study; waiver of consent was approved.
Case ascertainment.
Cases were obtained through electronic searches of inpatient and outpatient diagnostic databases (including diagnoses related to out-of-plan care), text string searches of all electronic head imaging reports, and cross-referencing with prior KPMCP studies of cerebral palsy.20,21 Cases were confirmed through independent chart review by 2 neurologists, with adjudication by a third. The criteria for stroke were 1) documented clinical presentation consistent with stroke, such as a sudden onset focal neurologic deficit, headache, or seizure; and 2) CT or MRI showing a focal infarct or hemorrhage in a location and of a maturity consistent with the neurologic signs and symptoms. Neonatal strokes were those occurring between 28 weeks gestation and 28 days of life.3 Strokes occurring after 28 days were defined as childhood strokes. Presumed perinatal strokes were defined as those strokes diagnosed in later infancy or childhood, but presumed to have occurred around the time of birth.3 These were included within the definition of neonatal stroke. Hemorrhagic stroke included intracerebral hemorrhage, subarachnoid hemorrhage, or intraventricular hemorrhage (IVH), except for neonatal IVH, which was excluded. Ischemic stroke included arterial ischemic stroke and venous sinus thrombosis.
Control selection.
To determine the costs of a pediatric stroke borne by the health care system that are in excess of routine health care for a child, we collected cost data for randomly identified stroke-free control patients. Three controls per case were randomly selected from the entire KPMCP cohort, and pairwise matched for age, year of enrollment in the KPMCP system, and the facility within KPMCP at which they first received routine health care. Health care status of the controls was not used in the selection process.
Clinical data abstraction.
Case clinical data were abstracted from electronic and traditional medical records by a single pediatric RN medical records analyst using a standardized protocol. A single pediatric vascular neurologist (H.J.F.) reviewed all available records to classify stroke type (hemorrhagic vs ischemic) and etiology.
Cost data.
Costs for all services provided by KPMCP, or paid for by KPMCP (in the instances of out-of-plan medical care), were directly obtained from KPMCP's Cost Management Information System, an automated system that integrates health care utilization databases with the financial ledgers of the system.23,24 Because KPMCP is a comprehensive health care plan that both insures and provides medical care to its members, these data are true costs (as opposed to charges) that were generated for individual services using standard accounting methods and program-specific relative value units. The costs include program and facility overhead.
For the cases, we collected all health care costs incurred within 5 years of the stroke event date. Admission costs were available for both hospitalizations that were “within plan” (i.e., at a KPMCP facility) and “out of plan.” These included all admission-related costs: emergency department costs, hospital costs, professional fees, and radiology, laboratory, and pharmacy costs. Costs of outpatient stroke-related care included visits to primary care and specialty physicians, medications, imaging studies, laboratory studies, rehabilitation, assistive devices, and other spasticity-related treatments provided by KPMCP.
For the pair-matched controls, we collected all health care costs incurred within 5 years of the “index date.” The index date for each control was defined as the stroke event date for the case paired with that control.
Cost analysis.
We performed a 5-year cost analysis using a microcosting approach, directly tabulating the actual cost of every individual component. Only direct costs were measured in this study; we did not account for “productivity costs” (i.e., lost economic productivity due to morbidity or mortality). All costs were adjusted for inflation to 2003 dollars, using the consumer price index. Because mean (average) costs reflect the overall societal burden and are used for economic analyses, we primarily summarized our results using means. However, because the cost data were not normally distributed, with positive skewness, we also expressed our results in medians and interquartile ranges (IQR).
We defined acute costs as all costs of the acute admission for stroke. The acute admission for a neonatal stroke is the birth admission. To isolate admission costs attributable to the stroke itself, the costs of birth admissions were individually “adjusted” by subtracting the mean birth admission costs for each case's trio of pair-matched controls. We report summary data of both the unadjusted and adjusted acute costs of neonatal stroke.
We defined chronic costs as all costs (inpatient and outpatient) incurred after the initial hospitalization. These were annualized and estimated for 5 years. To estimate the costs attributable to the stroke alone, we used control cost data to individually calculate “adjusted” chronic costs accounting for the costs of stroke-free childhood health care. We calculated the average annualized cost of health care for each trio of pair-matched controls over the same 5 years of observation as that trio's paired case. These annualized averages were subtracted from the annualized chronic cost for each case to estimate the excess cost related to childhood stroke.
Five-year-total costs were the sum of acute and chronic costs in those children with 5 years of follow-up data. In children who were never admitted for their stroke, total costs equaled chronic costs. “Adjusted” 5-year-total costs included both the adjustments made to neonatal birth admission costs and those made to all chronic costs.
Statistical analysis.
Because our cost data were skewed, precluding the use of linear regression techniques without transformation, we performed stratified analyses of both acute and chronic costs to determine whether stroke costs varied by predictors such as stroke type, age at onset (neonatal vs later childhood), and neurologic deficits at discharge. We used Mann-Whitney rank-sum tests to determine the significance of observed differences in cost, as well as length of stay. For comparisons of proportions, we employed χ2 tests. Alpha was set at 0.05 for all comparisons. All statistical analyses were done with Stata 9.0 or 10.0 (College Station, TX).
RESULTS
Of the 370 childhood stroke subjects identified in KPSS (1993–2003), 283 had their stroke in 1996 or after, when electronic cost data were available. Sixteen cases (5.6%) were excluded because of missing cost data, leaving a final cohort size of 266. We compared those with (n = 266) vs without (n = 16) available cost data and found no significant differences in gender, ethnicity, stroke type, or length of stay (data not shown). The final stroke cohort was ethnically diverse (15% black, 40% non-Hispanic white, 24% Hispanic, 11% Asian, 1% Native American, and 9% other), with a preponderance of males (60%). It included 81 (30%) neonatal strokes and 185 (70%) childhood strokes. Five neonates missing birth admission cost data were excluded from the analysis of acute and 5-year total costs, but included in the analysis of chronic costs. Of the childhood strokes, 101 (55%) were hemorrhagic and 84 (45%) ischemic, including 11 with venous sinus thrombosis. Fourteen (8%) of the childhood cases were already inpatients at the time of their stroke, while 149 (80%) were admitted after the stroke, and 22 (12%) were never admitted. Among the neonates, 25 (31%) had presumed perinatal strokes.
Five-year-total costs.
The mean 5-year-total cost of a pediatric stroke was $118,644, with an adjusted mean of $110,921 (table 1). Stroke itself therefore accounted for 93.5% of the total health care costs in these children, and increased the total health care costs 15-fold compared to stroke-free controls. The maximum 5-year-total cost, after adjustment for control costs, was $984,210 for childhood and $792,648 for neonatal stroke.
Table 1 Five-year-total costs for 186 children with stroke and ≥5 years of follow-up in Kaiser Permanente Medical Care Program P (1996–2003), stratified by age and stroke type, in 2003 US dollars

Acute costs.
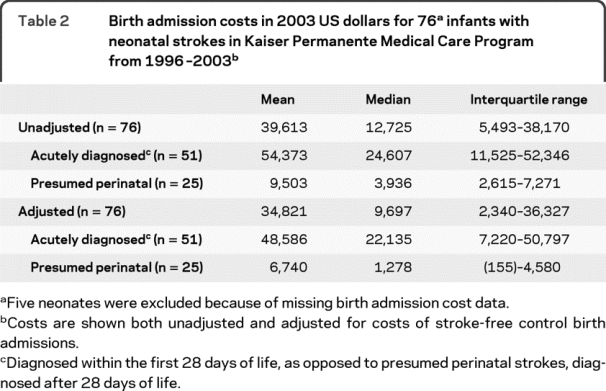
Admission costs for neonatal stroke are shown in table 2. The mean adjusted cost was 88% of the unadjusted cost, suggesting that the majority of the total birth admission costs can be attributed to the stroke. Although the median adjusted cost was only $9,697, the mean adjusted cost was $34,821, reflecting the positively skewed distribution, with a maximum adjusted birth admission cost of $453,298. Acute costs for the presumed perinatal strokes were lower than those for acutely diagnosed neonatal strokes (p < 0.001), but still exceeded controls' birth admission costs, with a mean adjusted cost of $6,740.
Table 2 Birth admission costs in 2003 US dollars for 76 infants with neonatal strokes in Kaiser Permanente Medical Care Program from 1996–2003
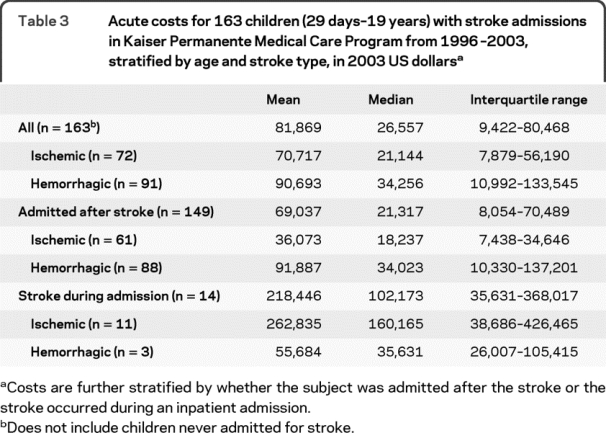
The average acute cost of a childhood stroke exceeded that of neonatal stroke (p < 0.0001 for the comparison of adjusted neonatal stroke admissions and childhood stroke admissions). Acute costs tended to be higher for hemorrhagic stroke compared to ischemic stroke (p = 0.12, table 3). Children with hemorrhagic stroke had a similar length of stay (LOS; median 7, IQR 2–16, mean 12) compared to those with ischemic stroke (median 6, IQR 2–17, mean 16; p > 0.99). However, the proportion of children requiring an intensive care unit admission was higher for hemorrhagic (72%) than ischemic stroke (51%; p = 0.001). Admission costs were higher when the stroke occurred during a hospital admission, as compared to when a child was admitted after a stroke (p = 0.001); the latter is likely a better reflection of costs attributable to the stroke itself. We again observed positive skewness due to extreme outliers with a maximum admission cost of $806,096 for a stroke during an admission and $660,318 for an admission after stroke.
Table 3 Acute costs for 163 children (29 days–19 years) with stroke admissions in Kaiser Permanente Medical Care Program from 1996–2003, stratified by age and stroke type, in 2003 US dollars
Chronic costs.
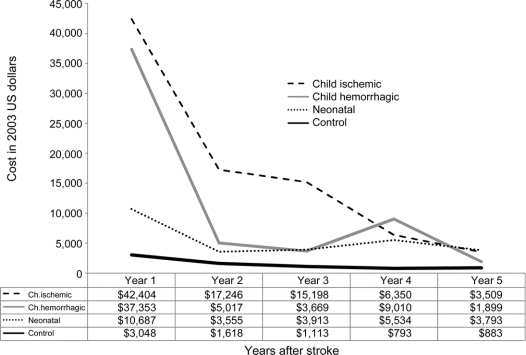
Mean chronic costs were highest in the first year after stroke, and then gradually declined. However, they failed to fall to the level of mean control health care costs even 5 years after the stroke (figure). Median chronic costs approximated median control costs more closely: by year 5, the median of the stroke costs that had been adjusted for costs in age-matched controls dropped to $220 (table e-1 on the Neurology® Web site at www.neurology.org). This suggests that the bulk of the long-term financial burden is due to a subgroup of more severely affected children with high ongoing health care costs. The maximum year 5 cost was $47,942 in a child with an ischemic stroke.
Figure Mean chronic costs after childhood stroke
Annualized mean chronic costs in pediatric stroke subjects in Kaiser Permanente Medical Care Program from 1996 to 2003. Subjects are stratified into 3 groups: childhood ischemic stroke, childhood hemorrhagic stroke, and neonatal stroke (including presumed perinatal strokes). Year 1 costs exclude acute (admission) costs. Chronic costs of age-matched stroke-free control subjects are also shown. Values are in 2003 US dollars. Sample sizes, means, medians, and interquartile ranges for each data point are shown in table e-1.
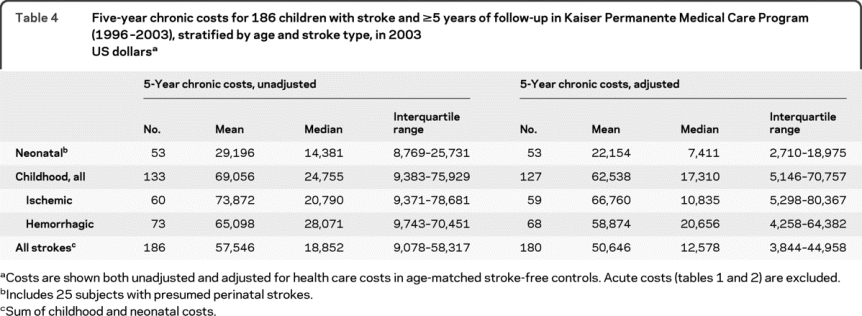
A total of 186 subjects had complete cost data through 5 years of follow-up and could therefore be included in the analysis of 5-year-total chronic costs. Compared to the 80 subjects excluded for missing data, these subjects were similar in terms of stroke length of stay (p = 0.58), intensive care admission (p = 0.84), and neurologic deficit at discharge (p = 0.14). As observed for acute costs, 5-year-total chronic costs were generally higher for childhood compared to neonatal stroke (p = 0.005), although there was considerable overlap (table 4). There was no significant difference in 5-year-total chronic costs between the hemorrhagic and ischemic stroke subgroups (p = 0.98). The maximum adjusted 5-year-total chronic cost was $749,147 in a childhood ischemic stroke case, $564,253 in a childhood hemorrhagic case, and $339,350 in a neonatal case. It was higher for children with neurologic deficits at discharge (n = 67: mean $71,434; median $25,551; IQR $5,807–$89,239) compared to those with normal neurologic examination results at discharge (n = 60: mean $52,604; median $10,579; IQR $2,444–$36,023; p = 0.03).
Table 4 Five-year chronic costs for 186 children with stroke and ≥5 years of follow-up in Kaiser Permanente Medical Care Program (1996–2003), stratified by age and stroke type, in 2003 US dollars
DISCUSSION
Pediatric stroke impacts long-term functioning, leading to physical disabilities, cognitive impairment, and other neurologic disorders, such as epilepsy and dystonia.25 Stroke-related direct costs provide one measure of the societal burden of this disease. Our study measured 5-year direct medical costs in a population-based cohort of children with stroke. We found that the financial burden of strokes in neonates and children is both substantial and long term, increasing 5-year health care costs 15-fold compared to age-matched children without stroke. Although chronic costs declined after the first year, they continued to exceed costs of the age-matched stroke-free control children, even 5 years poststroke. Because we did not measure indirect costs, or costs beyond 5 years, the total lifetime cost of a childhood stroke remains unknown. However, it is likely substantial, particularly given the potential for lost productivity of both the parents (caring for the afflicted child) and the child who matures into a disabled adult.
The average 5-year cost of a neonatal stroke in our cohort, after adjustment for control costs, was approximately $50,000. Childhood stroke was even more costly, with an average 5-year-total of $135,000, and a maximum approaching $1 million. Although few adult studies have measured costs beyond the first year poststroke,26 available data suggest that, during a similar time window, childhood stroke may be more costly than stroke in adults. For strokes diagnosed in US Medicare beneficiaries (age ≥65 years) in 1997, average Medicare expenditures at 4 years poststroke were $48,327 for subarachnoid hemorrhage, $38,023 for intracerebral hemorrhage, and $39,396 for ischemic stroke.27 Other studies have similarly reported a lower 5-year cost for adult stroke.28,29 Because pediatric strokes are occurring at a young age, the cumulative lifetime direct costs of a stroke in a child may greatly exceed that of a stroke in an adult.
Costs of acute stroke care in children are not only substantial but highly skewed, with an average childhood stroke admission cost of more than $80,000, median of $27,000, and maximum of $800,000. The only prior cost analysis of childhood stroke studied a retrospective sample from an academic children's hospital in Ohio and derived costs from hospital charges.19 Despite several methodologic differences, they reported comparable median inpatient costs: $22,000 for ischemic stroke and $50,000 for hemorrhagic stroke.
Some of the high stroke admission costs may reflect a serious underlying disease that predisposed to stroke. We were able to distinguish children who had a stroke during an acute hospitalization from those who were admitted because of the stroke; indeed, admission costs were higher in the former group. However, even among the children admitted for the stroke itself, the mean admission cost was more than $90,000 for hemorrhagic stroke and $36,000 for ischemic stroke. These costs are substantially higher than those previously reported for community hospital stroke admissions in adults: mean of approximately $24,000 for subarachnoid hemorrhage, $10,000 for intracerebral hemorrhage, and $6,000 for ischemic stroke (all in 1998 US dollars).11 Although the higher costs we observed in children may reflect differences in research methods, they may also reflect differences in the disease itself. For example, children predominantly have large artery infarctions, lacunar strokes being rare,30 which could lead to greater critical care needs and longer lengths of stay than adults, who have more lacunar strokes. In our study, 51% of children with ischemic stroke required an intensive care unit admission, compared to 14% of adults11 in the same community hospital report.
Although acute costs for neonatal stroke were lower than for childhood stroke, these events increased birth admission costs, relative to controls, by an average of almost $35,000. Presumed perinatal strokes are those not recognized in the acute phase, but diagnosed later, typically when a child presents with focal motor impairment during infancy or seizures. The birth admission costs for these babies still exceeded those of stroke-free controls by an average of almost $7,000, suggesting that these children have greater medical needs in the perinatal period, prior to diagnosis.
The primary limitation of our study is that the setting within a health maintenance organization may not be fully generalizable; costs may be different in an academic setting, among uninsured patients, or outside of California. However, because children were transferred to tertiary care hospitals as necessary, and the costs of these referrals were captured, our data are likely fairly representative of stroke costs within an insured population. Another limitation is that we had complete 5-year follow-up data on only 186 of the original 266 cases (70%). However, the cases with missing data were no different from those with complete data in terms of hospital length of stay, intensive care admissions, or neurologic deficits at discharge. A further limitation is that we did not have data on long-term disability, and therefore could not determine how degree of disability correlated with costs. Advantages of our study include the direct measurement of costs, as opposed to deriving cost estimates from hospital charges. Charges (as well as actual payments) tend to reflect provider cost shifting and other factors that decrease the validity of using charges to represent the true costs of providing care.31,32 Other advantages are the randomly selected controls, and the population-based sample, preventing the referral bias that might affect convenience samples from tertiary care institutions.
We measured the direct cost of childhood stroke during the acute hospitalization and 5 years poststroke, and demonstrated that costs are both substantial and long term. However, this is only one measure of the burden of this disease: we did not measure lifetime costs, indirect costs (lost productivity), or quality of life. Future studies should address these other important measures to better estimate the true burden of childhood stroke.
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. Nancy K. Hills.
DISCLOSURE
Dr. Gardner and Dr. Hills report no disclosures. Dr. Sidney serves on an external scientific advisory committee for the MESA Air Study; receives funding for travel to NIH Study Section meetings; serves as a Women's Health Initiative Study Case Adjudicator; and receives research support from the Eli Lilly and Company and from the NIH [NHLBI R01 HL078972 (PI), NHLBI N01 HC-48050 (PI), NINDS K23 NS049230 4 (Co-I), NINDS K02NS053883 (Co-I), NCI R01 CA103974 (Co-I), NHLBI R01 HL077618 (Co-I)] and the FDA. Dr. Johnston serves on a scientific advisory board for Daiichi Sankyo; serves as Vice Editor of Annals of Neurology; and receives research support from Boehringer Ingelheim, the NIH [NCRR Clinical and Translational Science Award (PI)], and the American Heart Association/American Stroke Association. Dr. Fullerton serves on a data safety monitoring board for Berlin Heart; serves on the editorial board of Pediatric Neurology; and receives research support from the NIH [R01 NS062820 A2 (contact PI), K02 NS053883 (PI), and R01 NS050488 R (Co-I/local PI)] and the American Heart Association.
Supplementary Material
Address correspondence and reprint requests to Dr. Heather J. Fullerton, University of California, San Francisco, Department of Neurology, Box 0114, 505 Parnassus Avenue, San Francisco, CA 94143-0114 fullertonh@neuropeds.ucsf.edu
Supplemental data at www.neurology.org
e-Pub ahead of print on January 6, 2010, at www.neurology.org.
Study funding: Supported by a Beginning Grant-In-Aid to Dr. Heather Fullerton from the American Heart Association, Western States Affiliates.
Disclosure: Author disclosures are provided at the end of the article.
Received May 7, 2009. Accepted in final form August 11, 2009.
REFERENCES
- 1.deVeber GA, MacGregor D, Curtis R, Mayank S. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 2000;15:316–324. [DOI] [PubMed] [Google Scholar]
- 2.Hartel C, Schilling S, Sperner J, Thyen U. The clinical outcomes of neonatal and childhood stroke: review of the literature and implications for future research. Eur J Neurol 2004;11:431–438. [DOI] [PubMed] [Google Scholar]
- 3.Lee J, Croen LA, Backstrand KH, et al. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. JAMA 2005;293:723–729. [DOI] [PubMed] [Google Scholar]
- 4.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: ethnic and gender disparities. Neurology 2003;61:189–194. [DOI] [PubMed] [Google Scholar]
- 5.Fullerton HJ, Chetkovich DM, Wu YW, Smith WS, Johnston SC. Deaths from stroke in US children, 1979 to 1998. Neurology 2002;59:34–39. [DOI] [PubMed] [Google Scholar]
- 6.Lanthier S, Carmant L, David M, Larbrisseau A, de Veber G. Stroke in children: the coexistence of multiple risk factors predicts poor outcome. Neurology 2000;54:371–378. [DOI] [PubMed] [Google Scholar]
- 7.De Schryver EL, Kappelle LJ, Jennekens-Schinkel A, Boudewyn Peters AC. Prognosis of ischemic stroke in childhood: a long-term follow-up study. Dev Med Child Neurol 2000;42:313–318. [DOI] [PubMed] [Google Scholar]
- 8.Chabrier S, Husson B, Lasjaunias P, Landrieu P, Tardieu M. Stroke in childhood: outcome and recurrence risk by mechanism in 59 patients. J Child Neurol 2000;15:290–294. [DOI] [PubMed] [Google Scholar]
- 9.Ganesan V, Hogan A, Shack N, Gordon A, Isaacs E, Kirkham FJ. Outcome after ischaemic stroke in childhood. Dev Med Child Neurol 2000;42:455–461. [DOI] [PubMed] [Google Scholar]
- 10.Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke 1996;27:1459–1466. [DOI] [PubMed] [Google Scholar]
- 11.Reed SD, Blough DK, Meyer K, Jarvik JG. Inpatient costs, length of stay, and mortality for cerebrovascular events in community hospitals. Neurology 2001;57:305–314. [DOI] [PubMed] [Google Scholar]
- 12.Friefeld S, Yeboah O, Jones JE, deVeber G. Health-related quality of life and its relationship to neurological outcome in child survivors of stroke. CNS Spectr 2004;9:465–475. [DOI] [PubMed] [Google Scholar]
- 13.Broderick J, Brott T, Kothari R, et al. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary first-ever and total incidence rates of stroke among blacks. Stroke 1981;1998;29:415–421. [DOI] [PubMed] [Google Scholar]
- 14.Adelman SM. The National Survey of Stroke: economic impact. Stroke 1981;12(suppl 1):I6–I87. [PubMed] [Google Scholar]
- 15.Brown DL, Boden-Albala B, Langa KM, et al. Projected costs of ischemic stroke in the United States. Neurology 2006;67:1390–1395. [DOI] [PubMed] [Google Scholar]
- 16.Sinclair SE, Frighetto L, Loewen PS, et al. Cost-Utility analysis of tissue plasminogen activator therapy for acute ischaemic stroke: a Canadian healthcare perspective. Pharmacoeconomics 2001;19:927–936. [DOI] [PubMed] [Google Scholar]
- 17.Marissal JP, Selke B. Economic assessment of the secondary prevention of ischaemic stroke with dipyridamole plus aspirin (Aggrenox/Asasantin) in France. Pharmacoeconomics 2004;22:661–670. [DOI] [PubMed] [Google Scholar]
- 18.Lightowlers S, McGuire A. Cost-effectiveness of anticoagulation in nonrheumatic atrial fibrillation in the primary prevention of ischemic stroke. Stroke 1998;29:1827–1832. [DOI] [PubMed] [Google Scholar]
- 19.Lo W, Zamel K, Ponnappa K, et al. The cost of pediatric stroke care and rehabilitation. Stroke 2008;39:161–165. [DOI] [PubMed] [Google Scholar]
- 20.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Recurrent hemorrhagic stroke in children: a population-based cohort study. Stroke 2007;38:2658–2662. [DOI] [PubMed] [Google Scholar]
- 21.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics 2007;119:495–501. [DOI] [PubMed] [Google Scholar]
- 22.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ray GT, Levine P, Croen LA, Bokhari FA, Hu TW, Habel LA. Attention-deficit/hyperactivity disorder in children: excess costs before and after initial diagnosis and treatment cost differences by ethnicity. Arch Pediatr Adolesc Med 2006;160:1063–1069. [DOI] [PubMed] [Google Scholar]
- 24.Ray GT, Butler JC, Black SB, Shinefield HR, Fireman BH, Lieu TA. Observed costs and health care use of children in a randomized controlled trial of pneumococcal conjugate vaccine. Pediatr Infect Dis J 2002;21:361–365. [DOI] [PubMed] [Google Scholar]
- 25.Broderick J, Talbot GT, Prenger E, Leach A, Brott T. Stroke in children within a major metropolitan area: the surprising importance of intracerebral hemorrhage. J Child Neurol 1993;8:250–255. [DOI] [PubMed] [Google Scholar]
- 26.Luengo-Fernandez R, Gray AM, Rothwell PM. Costs of stroke using patient-level data: a critical review of the literature. Stroke 2009;40:e18–e23. [DOI] [PubMed] [Google Scholar]
- 27.Lee WC, Christensen MC, Joshi AV, Pashos CL. Long-term cost of stroke subtypes among Medicare beneficiaries. Cerebrovasc Dis 2007;23:57–65. [DOI] [PubMed] [Google Scholar]
- 28.Hass SL, Ransom JE, Brown RD, Jr., O'Fallon WM, Whisnant JP, Leibson CL. The impact of stroke on the cost and level of care in nursing homes: a retrospective population-based study. Mayo Clin Proc 2001;76:493–500. [DOI] [PubMed] [Google Scholar]
- 29.Kolominsky-Rabas PL, Heuschmann PU, Marschall D, et al. Lifetime cost of ischemic stroke in Germany: results and national projections from a population-based stroke registry: the Erlangen Stroke Project. Stroke 2006;37:1179–1183. [DOI] [PubMed] [Google Scholar]
- 30.Williams LS, Garg BP, Cohen M, Fleck JD, Biller J. Subtypes of ischemic stroke in children and young adults. Neurology 1997;49:1541–1545. [DOI] [PubMed] [Google Scholar]
- 31.Price KF. Pricing Medicare's diagnosis-related groups: charges versus estimated costs. Health Care Financ Rev 1989;11:79–90. [PMC free article] [PubMed] [Google Scholar]
- 32.Shwartz M, Young DW, Siegrist R. The ratio of costs to charges: how good a basis for estimating costs? Inquiry 1995;32:476–481. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.