Abstract
Background
Computer simulations have demonstrated that excessive hip and knee flexion during gait, as frequently seen in ambulatory children with cerebral palsy (CP), can reduce the ability of muscles to provide antigravity support and increase the tendency of hip muscles to internally rotate the thigh. These findings suggest that therapies for improving upright posture during gait also may reduce excessive internal rotation.
Objective
The goal of this study was to determine whether strength training can diminish the degree of crouched, internally rotated gait in children with spastic diplegic CP.
Design
This was a pilot prospective clinical trial.
Methods
Eight children with CP participated in an 8-week progressive resistance exercise program, with 3-dimensional gait analysis and isokinetic testing performed before and after the program. Secondary measures included passive range of motion, the Ashworth Scale, and the PedsQL CP Module. To identify factors that may have influenced outcome, individual and subgroup data were examined for patterns of change within and across variables.
Results
Strength (force-generating capacity) increased significantly in the left hip extensors, with smaller, nonsignificant mean increases in the other 3 extensor muscle groups, yet kinematic and functional outcomes were inconsistent. The first reported subject-specific computer simulations of crouch gait were created for one child who showed substantial benefit to examine the factors that may have contributed to this outcome.
Limitations
The sample was small, with wide variability in outcomes.
Conclusions
Strength training may improve walking function and alignment in some patients for whom weakness is a major contributor to their gait deficits. However, in other patients, it may produce no change or even undesired outcomes. Given the variability of outcomes in this and other strengthening studies in CP, analytical approaches to determine the sources of variability are needed to better identify those individuals who are most likely to benefit from strengthening.
The long-term goal of this research collaboration is to determine whether targeted strengthening of the hip and knee extensors, alone or in combination with other treatments, can effectively diminish the excessive knee flexion, hip flexion, and hip internal rotation commonly observed in children with spastic diplegia who walk with a crouched gait pattern. Cerebral palsy (CP) is the most prevalent physical disability originating in childhood, with the largest proportion of this patient population having spastic diplegia,1 characterized by involvement primarily in the lower extremities. Nearly all children with spastic diplegia will ambulate, although often at a later age and with greater hip and knee flexion than children without neuromotor disabilities.2 Much therapeutic effort is directed at promoting and maintaining upright ambulation in these children, including regular physical therapy and bracing, as well as more invasive methods of spasticity reduction (eg, intramuscular injections, orthopedic surgery). Unfortunately, the outcomes of strength training and of many of the other interventions for improving walking in these individuals remain inconsistent.
There are several reasons to hypothesize that strengthening the hip and knee extensors might improve the gait kinematics of children with spastic diplegia. Perry's pioneering work demonstrated electromyographic (EMG) activity of the hip and knee extensors during the early stance phase of normal gait,3 and computer-based simulations of walking dynamics have revealed that the gluteus maximus and vastus muscles play an important role in early stance by supporting body weight and controlling hip and knee extension.4 (For a review of principles associated with human locomotion, refer to Kuo and Donelan in this issue.5) Simulations analyzing the roles of these muscles during crouch gait have revealed that the capacity of gluteus maximus and other muscles to extend the hip and knee may be diminished substantially by hip and knee flexion.6 The presence of weakness in children with spastic diplegia is now well documented, with even the most functional individuals demonstrating substantial generalized muscle weakness.7,8 Together, these observations suggest that the crouched postures of some children with CP may be exacerbated by lower-extremity extensor weakness. Musculoskeletal modeling and anatomical studies also have shown that excessive hip flexion alters the balance of the muscles that rotate the hip. With excessive hip flexion, the moment arms (ie, the lever arms or mechanical advantage) of some hip external rotators are diminished and the moment arms of hip internal rotators are increased, potentially contributing to excessive hip internal rotation.9 For example, the capacity of the gluteus maximus muscle to generate external rotation of the hip is compromised when the hip is flexed. This finding suggests that improvement of excessive hip flexion in people with crouch gait might improve hip rotation.
Despite this rationale, the potential for strength training to improve the gait mechanics of people with spastic diplegia remains unclear. Strength training was briefly a part of early physical therapy management of CP and has experienced a resurgence over the past 10 to 15 years. This resurgence was preceded by decades during which resistance training was contraindicated for people with CP because of clinical concerns that it would exacerbate spasticity. Some studies have demonstrated that short-term progressive resistance exercise programs can safely increase strength (force-generating capacity) in targeted muscles in people with CP without increasing spasticity.10,11 Positive effects on gait and gross motor function also have been reported,12 although less consistently than gains in strength.13 A recent meta-analysis, however, failed to provide evidence that strength training is effective in improving strength, increasing gait speed, or producing a clinically meaningful change in gross motor function in people with CP.14 The potential for strength training to improve the gait kinematics of people with CP has been evaluated in only a few studies, and findings have been equivocal. Most of these studies averaged data over a small number of subjects (ie, 11–21 subjects) and revealed only modest mean changes in the subjects’ joint angles during walking.15–19
The variability in outcomes reported in previous studies may be due to a range of factors, including methodological factors that may have limited the effectiveness of the training (eg, insufficient muscle loads, insufficient training durations) or, in some cases, impairments other than weakness that may have limited the subjects’ functional gains following strengthening (eg, difficulties with balance). We believe new approaches are needed to rigorously evaluate the biomechanical effects of resistance exercise programs, to help explain the reasons for inconsistent outcomes across subjects, and to identify individuals who are most likely to benefit from strengthening.
This article presents the results from a pilot strength training study in which we used a combination of physical examination, gait analysis, and state-of-the-art computer simulation to evaluate the effects of an 8-week progressive resistance exercise program on participants’ hip and knee angles (kinematics) during walking. We hypothesized that strengthening the hip and knee extensor muscles would decrease the exaggerated hip and knee flexion and hip internal rotation of children with spastic diplegia during the stance phase of gait. Secondary hypotheses were that strengthening would improve temporal spatial gait parameters, such as walking speed and stride length, and lead to improved physical functioning and related quality of life. Our main objective was to assess whether strength training could improve lower-extremity alignment during walking and, if so, use simulation to provide biomechanical insights into the reasons for these improvements.
Method
Participants
The goal of this pilot study was to enroll 10 children with spastic diplegia, based on a power analysis using data from 2 previous studies,15,17 within the age range of 5 to 17 years and diagnosed at Gross Motor Functional Classification System (GMFCS) levels I to III. The children had to be more than 1 year postsurgery and 6 months post–botulinum toxin injections in the lower extremity. Additional inclusion criteria, based on physical examination, included bilateral passive hip extension to neutral with the other hip flexed to 90 degrees, passive knee extension within 5 degrees of full extension while positioned supine, and passive hip external rotation of at least 20 degrees as assessed in a prone position with hip extended and knees flexed to 90 degrees. These criteria were chosen in an effort to exclude children whose gait deviations were predominantly constrained by musculoskeletal contracture. Previous orthopedic surgery or neurosurgery were not considered a reason for exclusion, with the exception of previous rotational osteotomies.
Children were screened visually to determine whether they exhibited a crouched internal rotation gait pattern, and these kinematic criteria were confirmed by gait analysis. In particular, children had to satisfy the following requirements bilaterally prior to participating in the strengthening portion of the study: (1) hip and knee flexion greater than 1 standard deviation above the mean normative value at initial contact; (2) excessive adduction and internal rotation of the hip at mid stance; and (3) less than 20 degrees of ankle dorsiflexion at mid stance, because excessive weakness of the plantar flexors or overlengthening of the calf muscles alone may contribute to crouch gait.
Participants were recruited from the neurology and neurosurgery cerebral palsy clinics and the physical therapy clinic at St. Louis Children's Hospital associated with Washington University. Informed consent and pediatric assent were obtained from all participants prior to the initial assessment.
Eight children (3 male, 5 female) met the inclusion criteria and completed the 8-week strengthening program during the study period (eTab. 1). The children ranged in age from 5.5 to 13.4 years. Five children were classified at GMFCS level III and used an assistive device to walk, 2 children were classified at GMFCS level II, and 1 child was classified at GMFCS level I.
Strength Training Program
Each child participated one-on-one with a therapist in a community-based physical therapy program, attending three 1-hour sessions per week for 8 weeks. Each therapist-guided session consisted of a progressive resistance exercise program using free weights or weight machines that targeted the gluteus maximus and quadriceps muscles bilaterally, with at least 1 day of rest between sessions (examples shown in Fig. 1). The program used a combination of open- and closed-chain exercises for maximum transfer to both the stance and swing phases of gait, and these exercises were designed to work the muscles in the most extended portion of the range. Examples include the use of cuff weights attached to the distal thigh during prone hip extension exercises with the knee kept flexed throughout the motion, the use of a resisted leg press, and the use of a weight machine that resisted knee extension in a reclined sitting position.
Figure 1.
Two examples of hip extensor strengthening exercises performed during training using weight machines. Other exercises also were performed (see text).
The intensity and difficulty of the program were adjusted individually. The amount of resistance applied was based on the number of repetitions each child could perform before fatiguing; the target was 8 to 10 repetitions, with the total number of repetitions consistent across participants (30 repetitions per muscle group). Passive stretching exercises at the hip and knee and a 5-minute walk at a relaxed pace on a treadmill or indoor track (depending on the child's ability and preference) were performed for warm-up before and cool-down after the strengthening exercises.
Functional Assessment
Each child received an assessment consisting of the following: (1) a physical examination; (2) a 3-dimensional (3-D) gait analysis; (3) an isokinetic strength assessment, as measured by maximum hip and knee extensor concentric torque at 30°/s; and (4) a validated self-report measure of physical functioning and related quality of life, as quantified by the parent-proxy version of the PedsQL 3.0 Cerebral Palsy Module.20 The exercise program was started within a week after the initial assessment, and an identical assessment was conducted within a week of completing the program. The physical examination was performed to assess range of motion at the hip, knee, and ankle (to ensure that the child met the inclusion and exclusion criteria) and to assess spasticity in the hamstring and quadriceps muscles. Spasticity was measured using the Ashworth Scale (ranging from 0 to 4, with a score of 1 indicating normal tone [resistance to passive stretch] and a score of 0 indicating less-than-normal tone). The 3-D gait analysis was performed to determine the child's lower-extremity joint angles during walking, with data from 5 trials collected at both freely selected and “as fast as possible without running” speeds. Fifteen retroreflective markers were placed on the skin overlying specific anatomic locations on the pelvis and bilateral lower extremities. The 3-D locations of these markers were tracked using an 8-camera Vicon system,* and the data were processed using Plug-In-Gait.† The isokinetic strength assessment enabled comparison of each child's isokinetic peak torque before and after strengthening. The peak torque data were expressed as the actual value and also were divided by body weight and multiplied by 100 to facilitate comparisons across children of varying sizes. Paired t tests (P<.05) were used to evaluate changes in selected assessment measures for the children before and after strengthening. Due to the small sample and the pilot nature of this study, no correction for multiple tests was applied.
Subject-Specific Simulations of Crouch Gait
Additional data were collected on children who were independent ambulators with the aim of creating subject-specific computer simulations of each child's crouched gait. To enable dynamic simulations, these data must include “clean” consecutive forceplate strikes during the gait analysis. These data were available, from both prestrengthening and poststrengthening training assessments, for one individual in this sample. In this case, the gait assessments included full-body 3-D kinematics, ground reaction forces and moments from forceplates, and surface EMG recordings from the tibialis anterior, gastrocnemius, rectus femoris, medial hamstring, adductor longus, vastus medialis, gluteus medius, and gluteus maximus muscles.
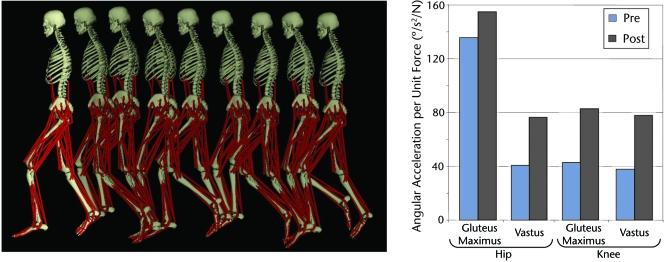
Computer simulations of the stance phase were generated that reproduced this child's 3-D gait kinematics and kinetics before and after strengthening. This process provided one of the first subject-specific simulations of an individual with a crouched, internal rotation gait pattern and is the first such model to evaluate changes in the actions of muscles as a result of strength training. To generate the simulations, we first created a computer model of the child that included 3-D representations of the bones, joints, and muscles scaled to the child's anthropometric dimensions.
Next, we used OpenSim biomechanics software21 to estimate the muscle activation patterns and muscle forces that, when applied to the model, produced joint angles and ground reaction forces that corresponded closely to the experimental measurements of the child's gait kinematics and kinetics. This software uses an optimization algorithm, called Computed Muscle Control,22 to determine the excitation patterns for each of the 92 muscle compartments in the model. We used the child's measured EMG data to verify that the simulated muscle excitations reflected the child's activation patterns. We generated 2 simulations: one that reproduced the child's gait dynamics before strengthening and another that reproduced the gait dynamics after strengthening.
Lastly, we analyzed the simulations to identify factors that enabled this individual to walk more upright after strengthening. In particular, we performed a perturbation analysis4 to assess the capacity of the gluteus maximus, vastus, and other muscles to support the body and extend the hip and knee during the stance phase. This analysis makes small adjustments (ie, perturbations) to the force in each muscle and measures the resulting changes in the hip and knee angles to determine the role that each muscle plays in extending or flexing the joints throughout the movement.
Results
Effects of Strength Training on Peak Isokinetic Torque
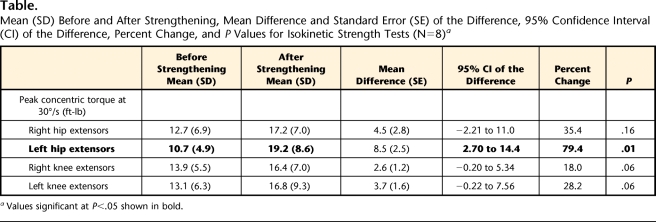
Most of the participants’ hip and knee extensor muscles were stronger after training, as measured by the change in isokinetic peak torque. The mean percentage gains in strength (ie, change in peak torque divided by initial peak torque value) ranged from 18.0% for the right knee extensors to 79.4% for the left hip extensors (Table); however, the percentage gains varied widely across participants. The magnitude and consistency of the strength changes generally were greater at the hip than at the knee (eTab. 2). Four children achieved appreciable increases in peak torque in at least 3 of the 4 muscle groups (Fig. 2). The other 4 children responded less dramatically to the strengthening program, showing either a negligible change or a small decrease in peak torque in one or both limbs and joints.
Table.
Mean (SD) Before and After Strengthening, Mean Difference and Standard Error (SE) of the Difference, 95% Confidence Interval (CI) of the Difference, Percent Change, and P Values for Isokinetic Strength Tests (N=8)a
Values significant at P<.05 shown in bold.
Figure 2.
Change in isokinetic peak torque divided by body weight and multiplied by 100 for each participant for the (A) right and left hip extensors and (B) right and left knee extensors. A positive change indicates an increase in strength. (C) Change in minimum knee flexion angle during stance. A positive change indicates an increase in knee flexion (ie, greater crouch).
Effects of Strength Training on Gait Kinematics
Some, but not all, of the children walked with improved hip and knee extension during stance following the exercise program (Fig. 2). The changes in hip extension generally were correlated to the changes in knee extension (r>.75, P<.05). Several of the children walked with improved hip rotation; however, we did not detect a correlation between the changes in hip rotation and the changes in either hip or knee extension.
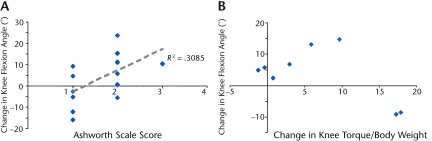
The 2 children who achieved the greatest gains in knee extensor strength (participant 1, classified at GMFCS level I, and participant 2, classified at GMFCS level III) also showed the greatest improvements in knee extension during the stance phase. However, for the other 6 children, knee flexion appeared to worsen with increasing strength gains, so no general conclusions could be made (Fig. 3).
Figure 3.
Scatterplot of change in minimum knee flexion angle (average for right and left legs) against (A) Ashworth Scale score and (B) change in knee extensor strength. Positive correlation between change in minimum knee flexion angle during stance and Ashworth Scale score of the hamstring muscles. Note that the Ashworth Scale score was not collected for one participant.
Effects of Strength Training on Gait Temporal-Spatial Parameters
Gait speed, stride length, and cadence were not significantly changed, on average, in either the self-selected or fast speed conditions following the strengthening program (eTab. 2). However, changes in all 3 measures varied across subjects; for example, self-selected walking speed improved 18% for participant 7, but diminished 25% for participant 5. No significant correlations were found between change in strength and change in these temporal-spatial parameters.
Effects of Strength Training on Perceived Physical Function and Related Quality of Life
A secondary outcome measure was the parent-proxy version of the PedsQL 3.0 Cerebral Palsy Module. These data showed trends toward a small amount of improvement (eTab. 3), but none of the changes were statistically significant when averaged across the participants.
Secondary Measures of Impairment
Mean passive knee extension was −2 degrees at the start of the program. A small, but significant, decrease (increased tightness) in passive knee extension was found as a result of the training (P<.05 for both right and left sides), with a mean change of about 3 degrees. The popliteal angle also worsened slightly, but the change was not significant on either side. No significant correlation was found between changes in passive and active knee extension. Spasticity did not change significantly before and after the training, but the degree of spasticity was directly related to the change in knee position (r=.55, P<.05). Figure 3 shows the initial Ashworth Scale score for each leg plotted against the change in minimum knee flexion, indicating that the greater the spasticity, the worse the response to strengthening.
Analysis of the Subject-Specific Simulations
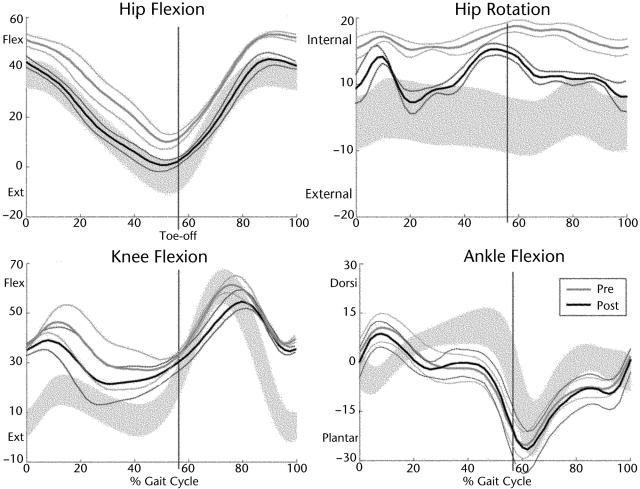
Participant 1 responded well to the strengthening program, demonstrating notable improvements in knee extension, hip extension, and hip rotation throughout the gait cycle (Fig. 4). Analysis of the subject-specific computer simulations and the associated clinical data provided insights into why this child's gait improved.
Figure 4.
Joint angles (with standard deviation bands), obtained from gait analysis, from the left side of one participant who responded well to the strengthening program (one for whom computer simulation was created). Note that the participant's excessive knee flexion, hip flexion, and internal hip rotation were diminished after strengthening. Pre=before strengthening, Post=after strengthening, Flex=flexion, Ext=extension, Dorsi=dorsiflexion, Plantar=plantar flexion.
Prior to the strengthening program, participant 1 had lower than normal strength of the hip and knee extensors, with the left side slightly weaker than the right side, and he walked in a moderate crouch gait pattern. As reported in previous studies, this posture puts greater than normal demands on the vastus muscles to support the body weight and diminishes the potential of the gluteus maximus and vastus muscles to extend the hip and knee.4,6,23 Although this child walked with excessive knee flexion, analysis of the computer simulation revealed that his hamstring muscles were operating at muscle-tendon lengths sufficient for normal walking,24 so a surgical lengthening of the hamstring muscles was not needed to release excessively tight muscles. He had normal range of motion at the hip and knee, with popliteal angles of 126 and 132 degrees on the right and left sides, respectively. He had undergone a selective dorsal rhizotomy at age 5 years and exhibited good selective control, as demonstrated by the ability to dorsiflex bilaterally without evidence of hip flexion. Thus, for this participant, an increase in strength was sufficient to improve his gait, and the resulting functional gains were not limited by other confounding impairments.
Our analysis of the child's gait dynamics supports this explanation. After the strengthening program, he demonstrated a substantial increase (from 20% to 85% of peak isometric torque) in the strength of his hip and knee extensors, with the left extremity values now exceeding those of the right extremity. The simulations suggested that the force generated by the left gluteus maximus muscle during early stance was increased, restoring an important mechanism that promotes hip and knee extension in normal gait. Furthermore, the capacity for the gluteus maximus and vastus muscles to accelerate the hip and knee into extension was increased (ie, angular acceleration per unit muscle force) (Fig. 5). Thus, after strengthening, the child's excessive knee flexion was diminished, which reduced the demands on the vastus muscles and increased the capacity of the gluteus maximus, vastus, and other muscles to support the body weight and to produce hip and knee extension. The decrease in hip flexion in stance also shifted the moment arms of the gluteus maximus, gluteus medius, and other hip muscles toward external rotation; this may have contributed to this individual's small improvement in hip rotation.
Figure 5.
(Left) The 3-dimensional musculoskeletal model in poses corresponding to key events in the gait cycle. The musculoskeletal model used to create a simulation of one of the participants has 10 body segments and 92 muscle compartments. (Right) Capacity of the gluteus maximus and vastus muscles to accelerate the hip and knee into extension before (Pre) and after (Post) strengthening for the participant on whom the simulation was performed.
Discussion
The goal of our pilot strengthening program, guided by previous studies and insights from musculoskeletal models, was to improve the children's lower-extremity alignment during walking. Unfortunately, the program did not produce systematic decreases in excessive hip flexion or knee flexion during the stance phase. Furthermore, because stance-phase hip extension was improved in only a few children, we were unable to test our hypothesis that improving hip extension would decrease hip internal rotation. We made an effort to exclude children whose gait deviations may have been caused primarily by other factors, such as weak or over-lengthened plantar flexors, muscle contractures, or bone deformities. Nonetheless, responses to the strength training were variable, similar to previous studies.15,16,18 The large variability in response, combined with the small sample size, likely affected our ability to detect significant mean group responses to strengthening. Although the conclusions we can draw from analysis of only 8 participants are limited, examination of these results is informative for clinical practice and for guiding future research.
Consistent with previous studies, we showed that gains in hip and knee extensor strength are possible in ambulatory children with CP, although some children achieved larger gains, and responded differently to those gains, than others. It is difficult to explain why some children did not make appreciable strength gains, given the fairly long (8-week) duration and the design of this program, whereby a therapist closely monitored each individual and progressively increased the amount of resistance used during training. Possible explanations include neurological factors, such as a primary agonist insufficiency that was not amenable to training, or pre-existing muscle adaptations that may have limited the capacity of some muscles to change in response to loading. At present, these explanations remain hypothetical and warrant further investigation. The children's strength changes were less consistent and smaller at the knee than at the hip, which may be related to increases in hamstring muscle strength. Greater strength in the hamstring muscles would contribute to increased extension torque at the hip, but could be a potential source of greater antagonist restraint when producing extension torque at the knee.
Previous studies have shown that resistance training, in some cases, can produce positive effects on gross motor functional abilities, including self-selected and maximum walking speed.10,13 In the present study, although there was a nonsignificant trend toward improvement on the questionnaire that measured the children's perception of physical performance and related quality of life, we did not detect a systematic improvement in walking speed or other gait parameters. This finding is not surprising, given the limited response to strength training for some of the children, as we suspect that improvements in strength may be needed to stimulate changes in these functional measures.
Only a few studies have evaluated the effects of increased strength on gait kinematics in people with CP, and findings have been equivocal. For example, Damiano and colleagues15 examined the effectiveness of a 6-week isotonic quadriceps muscle strengthening program for improving crouch gait in 14 children with spastic diplegia. Knee extensor strength improved significantly, as did stride length at free and fast speeds. However, the only significant change in the gait kinematics was a more extended knee position, on average, at initial contact. Six of the children also achieved greater knee extension at mid stance, but 2 children developed a slightly worsened crouch gait (ie, knee flexion increased approximately 5°) (unpublished observation).
In a subsequent strength study, Damiano and Abel17 targeted the 2 weakest muscles per individual and found significant changes in walking speed and function in a sample of 11 children with hemiplegia or diplegia, but no consistent improvement in gait kinematics, which was not surprising given the variability in the target muscles across subjects. Unger and colleagues16 evaluated the effects of an 8-week, generalized lower-extremity strengthening program for 21 adolescents with CP and reported a significant improvement in their gait kinematics of 5.1 degrees at mid stance only by summing up changes at the hip, knee, and ankle. Eek and colleagues18 trained the 4 weakest muscles per subject in 16 independently ambulatory children with CP and observed improvements in stride length and hip and ankle kinetics, but no systematic change in the gait kinematics. Lee and colleagues19 conducted a generalized functional lower-extremity training program in 16 children, ages 4 to 12 years, and found no changes in the gait kinematics.
Previous studies10,12,15–19 generally have reported mean changes in gait measures and have provided little insight into subject-specific factors that may have influenced the functional or kinematic outcomes. One potential precipitating factor often mentioned clinically is growth. As children grow, their strength must keep pace, or else their posture is compromised, as often is apparent in normal adolescence, suggesting that crouch in individuals with CP may be exacerbated by growth. However, Wren and colleagues25 recently evaluated the influence of age, among other factors, on different types of malalignment in nearly 1,000 patients with CP and found that rotational malalignment was associated with advancing age, but interestingly, crouch did not emerge as being significantly affected by age. It is likely that the natural history of crouch is altered by surgical procedures or botulinum toxin injections on the hamstrings and other muscles, which may have affected their analyses.
Given the variability of responses observed here, the reasons why some children in the present study walked with exaggerated knee flexion or internal rotation following the program remain unclear. In the subgroup analysis comparing independent ambulators with those who used an assistive device, the children who were more functional showed a small improvement in comparison with an appreciable worsening in the children who required an assistive device to walk; however, this difference did not reach significance, and the subgroup sample sizes were small. We did find decreased passive knee extension as a result of the program, as well as a relationship between greater hamstring muscle spasticity and poorer kinematic outcomes. We believe that unavoidable strengthening of the hamstring muscles during the hip extensor training may be responsible for the decrease in active and passive knee extension, despite the greater extensor strength, with those children with greater hamstring muscle spasticity at greater risk. More stringent muscle length or spasticity criteria, as well as closer monitoring of hamstring muscle length during the intervention, may be warranted in future studies. Interestingly, the child who had the most positive outcome was an independent ambulator and had undergone a selective dorsal rhizotomy several years prior to the study.
In their review of the role of strength training for improving gait in ambulatory children and adolescents with CP, Mockford and Caulton13 noted that the wide range of gait-related outcomes within and across studies occurs because individuals have shown such a wide variety of abnormalities and compensations; therefore, they concluded that no general conclusions can be drawn. Indeed, the heterogeneity of the motor disorder in people with CP makes it difficult to predict outcomes of any intervention in this population. One study in the adult orthopedic literature supports the premise that an 8-week strengthening program—in this case, targeting the hip abductors and lateral rotators in 15 female runners who were healthy—can alter kinematics in a clinically significant and predictable way.26 Based on our own observations and data from the literature, we remain cautiously optimistic about the potential for strength training to improve walking in some patients. One hypothesis that emerges from these results is that strengthening may be more beneficial for children with milder involvement, which seems reasonable because those patients are likely to have less spasticity and fewer motor control deficits that could limit their response to strengthening. It also is possible that programs need to be of longer duration or coupled with other interventions to address all of the factors that potentially contribute to excessive hip flexion, knee flexion, and hip internal rotation during walking.
Conclusion
The effect of strength training on gait kinematics in people with CP remains unpredictable at the level of the individual patient, and the current approach of mean group analysis of heterogeneous samples will not resolve this dilemma. We contend that studies with larger samples that can more adequately examine patient and intervention factors that could influence outcome, large-scale regression analyses, or subject-specific computer simulations of walking are needed to help explain the variability in outcomes and to identify individuals who are most likely to benefit from strengthening. More research also is needed to determine how strength training might complement or interact with other treatments, especially those interventions that tend to further weaken patients. Subject-specific musculoskeletal models and simulations of walking are currently labor- and technology-intensive efforts, but they hold promise for identifying the impairments that impede locomotor function, thereby refining and improving treatment approaches in CP.
Supplementary Material
Footnotes
Dr Damiano was the principal investigator and project director of the clinical trial. Dr Arnold and Dr Delp provided concept/idea/research design and project management. Dr Arnold, Ms Steele, and Dr Delp provided writing and data analysis. Ms Steele provided consultation (including review of manuscript before submission).
The authors acknowledge the United Cerebral Palsy Research & Education Foundation for funding this project. This research also was supported, in part, by the intramural program at the National Institutes of Health. The authors thank Julie Anderson for her assistance in all aspects of the study and Tom Nuzum and Dave Reddy for conducting the training sessions for all participants.
Human subjects approval was obtained from the Washington University Human Studies Committee prior to study initiation.
Vicon, 7388 S Revere Pkwy, Suite 901, Centennial, CO 80112.
Oxford Metrics, 14 Minns Business Park, West Way, Oxford OX2 0JB, United Kingdom.
References
- 1.Hirtz D, Thurman DJ, Gwinn-Hardy K, et al. How common are the “common” neurologic disorders? Neurology 2007;68:326–337 [DOI] [PubMed] [Google Scholar]
- 2.Sussman M. ed. The Diplegic Child Evaluation and Management Rosemont, IL: American Academy of Orthopaedic Surgeons; 1992 [Google Scholar]
- 3.Perry J. Determinants of muscle function in the spastic lower extremity. Clin Orthop Relat Res 1993;(288):10–26 [PubMed] [Google Scholar]
- 4.Arnold AS, Anderson FC, Pandy MG, Delp SL. Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J Biomech 2005;38:2181–2189 [DOI] [PubMed] [Google Scholar]
- 5.Kuo AD, Donelan JM. Dynamic principles of gait and their clinical implications. Phys Ther 2010;90:157–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hicks JL, Schwartz MH, Arnold AS, Delp SL. Crouched postures reduce the capacity of muscles to extend the hip and knee during the single-limb stance phase of gait. J Biomech 2008;41:960–967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Damiano DL, Vaughan CL, Abel MF. Muscle response to heavy resistance exercise in spastic cerebral palsy. Dev Med Child Neurol 1995;37:731–739 [DOI] [PubMed] [Google Scholar]
- 8.Wiley ME, Damiano DL. Lower extremity strength profiles in spastic cerebral palsy. Dev Med Child Neurol 1998;40:100–107 [DOI] [PubMed] [Google Scholar]
- 9.Delp SL, Hess WE, Hungerford DS, Jones LC. Variation of rotation moment arms with hip flexion. J Biomech 1999;32:493–501 [DOI] [PubMed] [Google Scholar]
- 10.Andersson C, Grooten W, Hellsten M, et al. Adults with cerebral palsy: walking ability after progressive strength training. Dev Med Child Neurol 2003;45:220–228 [DOI] [PubMed] [Google Scholar]
- 11.Fowler EG, Ho TW, Nwigwe AI, Dorey FJ. The effect of quadriceps femoris muscle strengthening exercises on spasticity in children with cerebral palsy. Phys Ther 2001;81:1215–1223 [PubMed] [Google Scholar]
- 12.Dodd KJ, Taylor NF, Damiano DL. A systematic review of the effectiveness of strength-training programs for people with cerebral palsy. Arch Phys Med Rehabil 2002;83:1157–1164 [DOI] [PubMed] [Google Scholar]
- 13.Mockford M, Caulton JM. Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Pediatr Phys Ther 2008;20:318–333 [DOI] [PubMed] [Google Scholar]
- 14.Scianni A, Butler JM, Ada L, Teixeira-Salmela LF. Muscle strengthening is not effective in children and adolescents with cerebral palsy: a systematic review. Aust J Physiother 2009;55:81–87 [DOI] [PubMed] [Google Scholar]
- 15.Damiano DL, Kelly LE, Vaughn CL. Effects of quadriceps femoris muscle strengthening on crouch gait in children with spastic diplegia. Phys Ther 1995;75:658–667 [DOI] [PubMed] [Google Scholar]
- 16.Unger M, Faure M, Frieg A. Strength training in adolescent learners with cerebral palsy. Clin Rehabil 2006;20:469–477 [DOI] [PubMed] [Google Scholar]
- 17.Damiano DL, Abel MF. Functional outcomes of strength training in spastic cerebral palsy. Arch Phys Med Rehabil 1998;79:119–125 [DOI] [PubMed] [Google Scholar]
- 18.Eek MN, Tranberg R, Zügner R, et al. Muscle strength training to improve gait function in children with cerebral palsy. Dev Med Child Neurol 2008;50:759–764 [DOI] [PubMed] [Google Scholar]
- 19.Lee JH, Sung IY, Yoo JY. Therapeutic effects of strengthening on gait function in cerebral palsy. Disabil Rehab 2008;30:1439–1444 [DOI] [PubMed] [Google Scholar]
- 20.Varni JW, Burwinkle TM, Berrin SJ, et al. The PedsQL in pediatric cerebral palsy: reliability, validity, and sensitivity of the Generic Core Scales and Cerebral Palsy Module. Dev Med Child Neurol 2006;48:442–449 [DOI] [PubMed] [Google Scholar]
- 21.Delp SL, Anderson FC, Arnold AS, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans Biomed Eng 2007;55:1940–1950 [DOI] [PubMed] [Google Scholar]
- 22.Thelen DG, Anderson FC, Delp SL. Generating dynamic simulations of movement using computed muscle control. J Biomech 2003;36:321–328 [DOI] [PubMed] [Google Scholar]
- 23.Liu MQ, Anderson FC, Pandy MG, Delp SL. Muscles that support the body also modulate forward progression during walking. J Biomech 2006;39:2623–2630 [DOI] [PubMed] [Google Scholar]
- 24.Arnold AS, Asakawa DJ, Delp SL. Do the hamstrings and the adductors contribute to excessive internal rotation of the hip in persons with cerebral palsy? Gait Posture 2000;11:181–190 [DOI] [PubMed] [Google Scholar]
- 25.Wren TA, Rethlefsen S, Kay RM. Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Orthop 2005;25:79–83 [DOI] [PubMed] [Google Scholar]
- 26.Snyder KR, Earl JE, O'Connor KM, Ebersole KT. Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running. Clin Biomech (Bristol, Avon) 2009;24:26–34 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.