Summary
Mucous membrane pemphigoid includes chronic autoimmune sub-epithelial blistering diseases that predominantly affect mucous membranes, with varying combinations of oral, ocular, cutaneous, genital, nasopharyngeal, oesophageal and laryngeal lesions. The case is reported of a man with multiple manifestations of mucous membrane pemphigoid. A 53-year-old male presented at our Department with a 4-year clinical history of diagnosed cicatricial pemphigoid. The patient was affected by ocular and urinary symptoms and presented with nasal obstruction and dysphonia. Nasal endoscopy revealed crusting and synechiae with pale and atrophic mucosa. Computed tomography examination showed hypodense-hyperdense material occupying all paranasal sinuses and nasal fossae. Laryngoscopy showed anterior para-commessural and inter-arytenoidal synechiae. The patient underwent functional endoscopic sinus surgery for incision of synechiae and removal of scars and inflammatory material from all sinuses. Nasal splints were then inserted. A wait-and-see policy was adopted for the laryngeal lesion. One year later, the splints were removed; the upper airways were still free and there were no signs of nasal obstruction. An endoscopic approach appears to be efficacious in the surgical treatment of nasal cicatricial pemphigoid, and long-term stenting may be necessary to avoid recurrence. Although surgery has not a curative role in long-term therapeutic strategies, it may, nonetheless, improve the quality of life and ensure good nasal respiration.
Keywords: Nose, Larynx, Cicatricial pemphigoid, Synechia
Riassunto
Il pemfigoide mucosinechiante è un disordine autoimmune cronico caratterizzato da manifestazioni mucose spesso multiple. Questa rara condizione colpisce prevalentemente alcuni organi, quali, ad esempio, il cavo orale, gli occhi, la cute, i genitali, la mucosa nasale, faringea, esofagea e laringea. Presentiamo il caso di un paziente con coinvolgimento multiorgano. Un uomo di 53 anni è giunto alla nostra attenzione, presso il Dipartimento di Otorinolaringoiatria dell’Ospedale San Raffaele di Milano, con diagnosi antecedente di pemfigoide mucosinechiante e una storia clinica di circa 4 anni, caratterizzata da un intervento di odontocheratoprotesi all’occhio destro. Il paziente presentava sintomi oculari e urinari associati a ostruzione respiratoria nasale e disfonia. All’indagine endoscopica nasale era evidente un quadro di rinite crostosa e sinechie diffuse su una mucosa nasale pallida e atrofica. L’imaging radiologico confermava la presenza di materiale infiammatorio occupante i seni paranasali e le fosse nasali. In fibrolaringoscopia erano presenti una sinechia laringea localizzata in sede paracommissurale e una in sede interaritenoidea. Il paziente è stato sottoposto a chirurgia endoscopica naso-sinusale allo scopo di rimuovere il materiale cicatriziale e infiammatorio dai seni paranasali e lisare le sinechie con posizionamento di splints parasettali. Per quanto riguarda il coinvolgimento laringeo si è deciso di effettuare un follow-up stretto sulla lesione senza intervenire chirurgicamente. Gli splints parasettali sono stati lasciati in sede per circa un anno. Al controllo le vie aeree risultavano pervie, senza segni di ostruzione nasale. L’approccio endoscopico nel trattamento chirurgico delle forme di pemfigoide mucosinechiante con coinvolgimento nasale sembra essere efficace soprattutto se associato all’utilizzo di splints nasali a lunga permanenza.
Introduction
Mucous Membrane Pemphigoid (MMP) includes chronic, autoimmune, inflammatory sub-epithelial blistering diseases that predominantly affect the mucous membranes, with or without skin involvement as defined by the first international consensus conference 1. Any mucosa might be affected, with varying combinations of oral, ocular, cutaneous, genital, naso-pharyngeal, oesophageal and laryngeal lesions. MMP is typically a disease of the elderly. It occurs most frequently in the sixth and seventh decades of life, although it has been reported to range between the third and ninth decades 2 3. Females are affected twice as often as males, and there is no geographic or racial predominance 4. MMP is not a common disease. The annual incidence is reported to be 1.16 and 0.87 per million, in France and Germany, respectively 5 6.
Although the exact patho-physiological mechanisms have not yet been fully elucidated, experimental data suggest that humoral and cellular immune mechanisms may play a role in the pathogenesis of the disorder 7–9. Direct immunofluorescence investigations show continuous linear deposits of IgG and C3, in addition to IgA, in the epithelial basement membrane zone in all MMP patients 1 10. Clinical onset varies as it may appear as vescicolo-bullous lesions, with progressive erosion and healing with scars or as erythema, oedema or crusty ulcers that occasionally evolve into scarring and adhesions 11. The heterogeneous clinical picture can make diagnosis of MMP difficult. Diagnosis of the condition requires a combination of clinical and immuno-pathological findings together with histological evidence 11. Medical therapy is the treatment of choice. Both local and systemic measures may be used to achieve symptomatic control and delay disease progression, but since the aetiology is unknown, treatment is neither specific nor curative. According to the data in the literature, surgery plays a marginal role being used mainly in the presence of complications. Herewith, the case is presented of a multiple mucous involvement, focusing on ENT lesions.
Case report
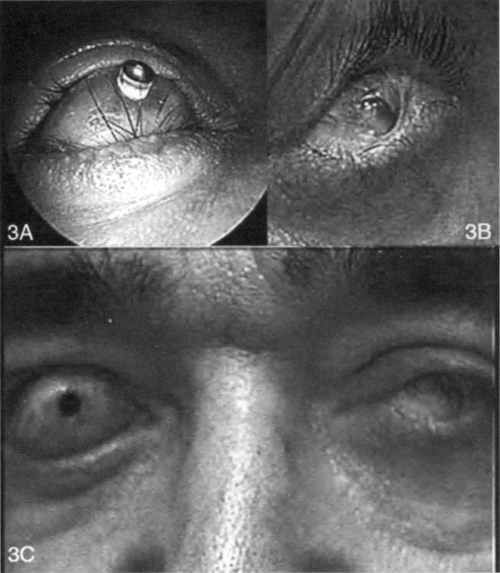
A 53-year-old male presented at the Department of Otorhinolaryngology at the Vita-Salute University of Milan, in 2002, with a 4-year clinical history and diagnosis of Cicatricial Pemphigoid (CP). He was affected by scarring of the tarsal conjunctiva with symblepharon and ankyloblepharon formation (Fig. 1A). This condition had progressed until total blindness. He also reported urinary disorders, correlated with the presence of urethral synechiae requiring endoscopic surgery followed by placement of a foley for 50 days in order to ensure diuresis. He came to our attention complaining of nasal obstruction, hyposmia and headache. He also reported having dysphonia since 2001.
Fig. 1.
A: Left eye with conjuctival synechiae. B: Right eye treated by osteo-odonto-keratoprosthesis. C: General view of eyes.
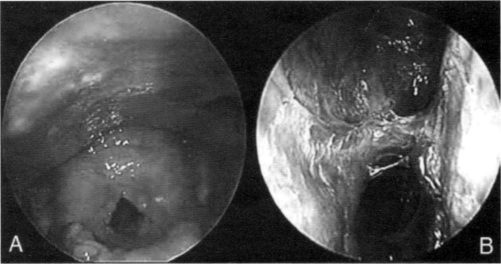
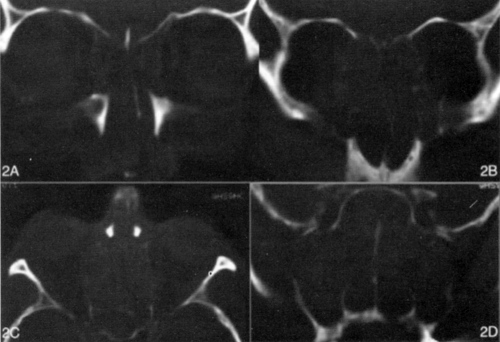
Nasal examination using a 30° rigid endoscope revealed crusting and synechiae between the nasal septum and inferior turbinates, which also led to choanal stenosis. Evidence of a pale nasal mucosa confirmed atrophic rhinitis (Fig. 2B). Laryngeal involvement was evaluated with a 70° endoscope showing anterior para-commessural and inter-arytenoidal synechiae (Fig. 2A). Computerized tomography (CT) examination (in 2002) was performed on axial and coronal views, 3 mm thickness (Fig. 3A-D). CT showed hysodense-hyperdense material occupying the left maxillary sinus, ethmoidal cavities, sphenoidal and left frontal sinus. Material was also present in the right maxillary sinus. Nasal fossae, especially the left, were totally filled. Bone structures were hyperdense, on CT scans, for lateral walls and thin for medial walls that were not easily detected at nasal fossae level, similar to findings observed in chronic inflammatory reactions. Pathological tissue extended anteriorly to the nasal fossae and posteriorly to the choana, particularly on the right side.
Fig. 2.
A: Laryngeal involvement was evaluated with a 70° endoscope showing anterior para-commessural and inter-arytenoidal synechiae. B: Nasal endoscopy shows pale nasal mucosa with atrophic rhinitis, synechiae and crusting.
Fig. 3.
A-B-D: CT scan (coronal views) shows inflammatory material occupying ethmoid, maxillary, sphenoid sinuses and nasal fossae. C: Axial view of CT examination shows pathological tissue that extends to obliterate the paranasal sinuses.
Due to the patient’s clinical and radiological picture, functional endoscopic sinus surgery (FESS) with diode laser was performed, in order to incise synechiae, remove scars and inflammatory material from all sinuses. Nasal splints were then inserted. One year later, the splints were removed; the upper airways were still free and there were mild signs of nasal obstruction. A wait-and-see policy was adopted for laryngeal lesions. Between 2003 and 2004, the patient underwent ocular surgery, and his right eye was treated using an osteo-odonto-keratoprosthesis (Fig. 1B).
Discussion
Cicatricial pemphigoid is a chronic, progressive, sub-epithelial blistering disease that may affect several mucous sites. According to the literature, this condition involves, in decreasing frequency, the oral cavity (90%), eye (65%), nose, nasopharynx, anogenitals, skin (20-30%), larynx (8-9%) and oesophagus 12. In a recent prospective study, Alexandre et al. investigated the nose and throat manifestations of MMP and reported several symptoms, such as epistaxis (26%), pharyngalgia (24%), dysphagia (40%), dysphonia (18%), dyspnoea (13%), nasal obstruction (37%) and nasal crusting (82%) 13. Our patient showed nasal obstruction and crusting in addition to dysphonia.
Very limited data concerning ENT involvement by blistering are available, and the frequency of such lesions and correlated symptoms is not well known 13. Indeed, it should not be forgotten that agreement between symptoms and lesions was only partial. Some symptomatic patients have no lesions at physical examination. At the same time, it cannot be excluded that asymptomatic patients might have lesions. In the literature, clinical lesions have been reported in 25% of cases involving the nose and in 5% and 17% involving the pharynx and larynx, respectively 13.
Atrophic rhinitis is the most frequent nasal lesion (58%) 13. In our patient, this condition was associated with crusting and synechiae, which have been reported to represent 26% and 11%, respectively, of nasal lesions 13. These nasal manifestations lead to choanal or nasal valve stenosis, symptoms which give rise to great discomfort
Postbullous erosions of the pharynx and larynx, associated with erythema and/or oedema, have been reported to occur in 13% and 42% of previously reported cases, respectively 13. The most frequent laryngeal lesion is erosion of the epiglottal laryngeal surface (34% of the cases) 13. These lesions are also seen on arytenoids, interarytenoids and aryepiglottic folds. Synechiae may be observed joining the epiglottis, aryepiglottic folds, arytenoids and false vocal cords resulting in severe obstruction of the laryngeal inlet. Laryngeal involvement is particularly dangerous since it exposes the patient to the permanent risk of acute dyspnoea and death. Our patient presented dysphonia related to two synechiae in the paracommissural and interarytenoidal space.
Severe laryngeal involvement, severe ocular lesions or more than 3 affected sites, other than nose and throat mucous membranes, can be potentially life-threatening 13. In patients with nasal disease, regular irrigation with isotonic sodium chloride solution and an intra-nasal lubricant are important 14. Atrophic rhinitis requires specific treatment based on local corticosteroid instillations. Vasoconstrictors are contra-indicated due to the increased risk of mucous atrophy 13.
Use of nasal surgery is highly controversial. In the literature, surgical procedures have been considered both unnecessary and detrimental on account of the high risk of relapse 13. Surgical approaches require repeated divisions and insertion of nasal splints 11. Our patient underwent functional endoscopic sinus surgery to improve nasal obstruction removing synechiae, scarring and inflammatory material in addition to splint insertion. The splits were removed one year later and the upper airway was still free. Although surgery does not play a curative and long-term therapeutic role, in this case it improved the patient’s quality of life and ensured good nasal respiration.
Laryngeal synechiae and stenosis can result from the typical evolution of the pathological condition or as a consequence of routine intubation. This latter event explains why surgery, to repair the upper aerodigestive tract, should be delayed until MMP is stabilized; anaesthesiologists should be forewarned regarding the fragility of the upper aerodigestive tract to guarantee scrupulous care when intubation is necessary.
The discovery of laryngeal involvement orientates the clinician towards an aggressive systemic therapeutic approach, combining immunosuppressive drugs and inhaled corticosteroids 13. All previous reports focusing on the surgical treatment of laryngeal stenosis stress the reluctance of surgeons to excise the scarred tissue on account of the recurrent nature of MMP 15. Tracheostomy may, however, be a life-saving procedure in order to stabilize the airway whilst the appropriate therapy is undertaken. Excision of scarring is not recommended in the acute period. Once the disease is stabilized, the laryngeal airway can be restored with a carbon dioxide laser 11. This surgical procedure can be repeated during management of the disease and also associated with adjuvant use of mitomycin-C, which appears to reduce the severity of stenosis and prolong the symptom-free interval 16–18. On the basis of the above considerations, it was decided not to treat this patient with conventional surgical techniques since he presented only dysphonia and not dyspnoea.
In conclusion, an endoscopic approach appears to be efficacious in the surgical treatment of nasal cicatricial pemphigoid and long-term stenting is required to avoid acute relapse.
References
- 1.Chan LS, Ashmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol 2002;138:370-9. [DOI] [PubMed] [Google Scholar]
- 2.Laskaris G, Sklavounou A, Stratigos J. Bullous pemphigoid, cicatricial pemphigoid, and pemphigus vulgaris. A comparative clinical survey of 278 cases. Oral Surg Oral Med Oral Pathol 1982;54:656-62. [DOI] [PubMed] [Google Scholar]
- 3.Mantich NM, Craig RM, Glass BJ. Red, blistering, and erosive lesions of the oral mucosa. J Am Dent Assoc 1987;115:457-8. [DOI] [PubMed] [Google Scholar]
- 4.Lever WF. Pemphigus. Medicine 1953;32:1-123. [DOI] [PubMed] [Google Scholar]
- 5.Bernard P, Vaillant L, Labeille B, Bedane C, Arbeille B, Denoeux JP, et al. Incidence and distribution of subepidermal autoimmune bullous skin diseases in three French regions. Bullous Diseases French Study Group. Arch Dermatol 1995;131:48-52. [PubMed] [Google Scholar]
- 6.Zillikens D, Weyer S, Roth A, Weidenthaler-Barth B, Hashimoto T, Brocker EB. Incidence of autoimmune subepidermal blistering dermatoses in a region of central Germany. Arch Dermatol 1995;131:957-8. [DOI] [PubMed] [Google Scholar]
- 7.Liu Z, Diaz LA, Troy JL, Taylor AF, Emery DJ, Fairley JA, et al. A passive transfer model of the organ-specific autoimmune disease, bullous pemphigoid, using antibodies generated against the hemidesmosomal antigen, BP180. J Clin Invest 1993;92:2480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazarova Z, Yee C, Darling T, Briggaman RA, Yancey KB. Passive transfer of anti-laminin 5 antibodies induces subepidermal blisters in neonatal mice. J Clin Invest 1996;98:1509-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Budinger L, Borradori L, Yee C, Eming R, Ferencik S, Grosse-Wilde H, et al. Identification and characterization of autoreactive T cell responses to bullous pemphigoid antigen 2 in patients and healthy controls. J Clin Invest 1998;15;102:2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan LS, Hammerberg C, Coope KD. Significantly increased occurrence of HLA-DQB1*0301 allele in patients with ocular cicatricial pemphigoid. J Invest Dermatol 1997;108:129-32. [DOI] [PubMed] [Google Scholar]
- 11.Whiteside OJ, Martinez Devesa P, Ali I, Capper JW. Mucous membrane pemphigoid: nasal and laryngeal manifestations. J Laryngol Otol 2003;117:885-8. [DOI] [PubMed] [Google Scholar]
- 12.Eschle-Meniconi ME, Ahmad SR, Foster CS. Mucous membrane pemphigoid: an update. Curr Opin Ophthalmol 2005;16:303-7. [DOI] [PubMed] [Google Scholar]
- 13.Alexandre M, Brette MD, Pascal F, Tsianakas P, Fraitag S, Doan S, et al. A prospective study of upper aerodigestive tract manifestations of mucous membrane pemphigoid. Medicine (Baltimore) 2006;85:239-52. [DOI] [PubMed] [Google Scholar]
- 14.Egan CA, Yancey KB. The clinical and immunopathological manifestations of anti-epiligrin cicatricial pemphigoid, a recently defined subepithelial autoimmune blistering disease. Eur J Dermatol 2000;10:585-9. [PubMed] [Google Scholar]
- 15.el-Sayed Y, al-Muhaimeed H. Cicatricial pemphigoid of the larynx: a case report of surgical treatment. Ear Nose Throat J 1996;75:658-60, 665, 668. [PubMed] [Google Scholar]
- 16.Rahbar R, Shapshay SM, Healy GB. Mitomycin: effects on laryngeal and tracheal stenosis, benefits, and complications. Ann Otol Rhinol Laryngol 2001;110:1-6. [DOI] [PubMed] [Google Scholar]
- 17.Correa AJ, Reinisch L, Sanders DL, Huang S, Deriso W, Duncavage JA, et al. Inhibition of subglottic stenosis with mitomycin-C in the canine model. Ann Otol Rhinol Laryngol 1999;108:1053-60. [DOI] [PubMed] [Google Scholar]
- 18.Eliashar R, Eliashar I, Esclamado R, Gramlich T, Strome M. Can topical mitomycin prevent laryngotracheal stenosis? Laryngoscope 1999;109:1594-600. [DOI] [PubMed] [Google Scholar]