Abstract
Acetabular retroversion (AR) alters load distribution across the hip and is more prevalent in pathologic conditions involving the hip. We hypothesized the abnormal orientation and mechanical changes may predispose certain individuals to stress injuries of the femoral neck. We retrospectively reviewed the anteroposterior (AP) pelvic radiographs of 54 patients (108 hips) treated for a femoral neck stress fracture (FNSF) and compared these radiographs with those for a control group of patients with normal pelvic radiographs. We determined presence of a crossover sign (COS), femoral neck abnormalities, and neck shaft angle. The prevalence of a positive COS was greater in patients with stress fractures than in the control subjects (31 of 54 [57%] versus 17 of 54 [31%], respectively) and higher than for control subjects reported in the literature. Thirteen patients had radiographic changes of the femoral neck consistent with femoroacetabular impingement (FAI). These radiographic abnormalities were seen more commonly in retroverted hips. A greater incidence of AR was noted in patients with FNSF. Potential implications include more aggressive screening of military recruits with AR and the new onset of hip pain. Finally, we present an algorithm we use to diagnose and treat these relatively rare FNSFs.
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Abnormalities of acetabular orientation are increasingly implicated in the etiology of various disorders of the hip [5, 8, 10, 13, 15]. Recent research suggests higher rates of AR in patients with hip osteoarthritis (15%–20%) [5, 8, 10], hip dysplasia (16%–37%) [13, 15], and Legg-Calve-Perthes disease (42%) [5] when compared with the healthy population (5%–16%) [5, 8, 10]. AR is also an etiologic factor in FAI [23]. Although well-designed biomechanical studies have yet to be performed, an accepted theory in the literature proposes that AR results in decreased articular contact area, eccentric loading of the joint, and abnormal contact between the proximal femur and the acetabular rim during terminal motion of the hip, which in turn may lead to various hip disorders [7]. The diagnosis of AR can be made by the presence of a COS on standard AP pelvic radiographs [21] (Fig. 1). This radiographic sign is a reliable and validated indicator of AR [9].
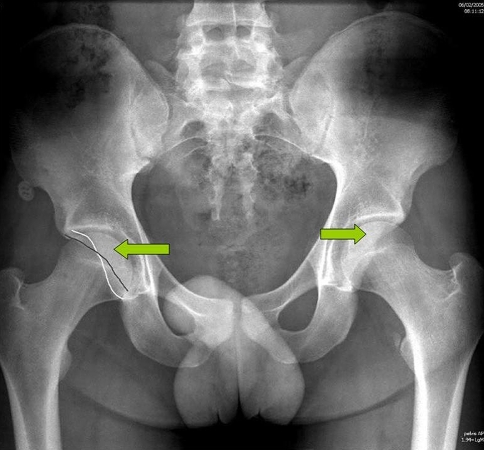
Fig. 1.
An AP radiograph shows a bilateral COS (arrows). The white line represents the posterior wall and the gray line represents the anterior wall.
FNSFs are relatively rare, accounting for less than 10% of all stress fractures [14]. Stress fractures result from the failure of normal bone to react quickly enough and with sufficient reparative response to counter repetitive or supraphysiologic loads [11]. Because forces across the femoral neck nearly triple with running activities, military recruits and endurance athletes are at risk for FNSFs owing to the prolonged running and marching required in their training [6, 22]. It stands to reason that any biomechanical factor further elevating such forces might hasten the development of stress fractures across the femoral neck.
It seems intuitive that increased cumulative load transmission across the femoral neck in highly active individuals might contribute to FNSF. This study was performed at a large military medical facility where a relatively large volume of patients with this uncommon injury are treated. As our awareness of FAI and AR has increased in recent years, we increasingly have noted the COS in patients with FNSF. We therefore hypothesized AR alters the distribution of forces on the femoral neck and increases the risk of having a FNSF develop in certain high-risk populations.
The purposes of our study were: (1) to present an algorithm for diagnosing and treating FNSF; (2) to determine if there is an increased incidence of AR in patients with FNSFs compared with healthy control subjects; (3) to determine if patients with FNSF have radiographic changes of the femoral neck that are suggestive of FAI; and (4) to report the incidence of AR in a healthy military population and compare it with the incidence of AR in the general population as reported in the literature.
Materials and Methods
We retrospectively identified and reviewed the medical records and imaging studies of all patients seen at the Naval Medical Center San Diego between January 2001 and August 2006 who were diagnosed with a FNSF. We included patients between 17 and 30 years of age with closed physes with stress fractures diagnosed by plain radiographs, bone scintigraphy, or MRI. Our hospital is a major military medical treatment facility, and all patients were active-duty military personnel. The majority of patients were US Marine Corps recruits or involved in special warfare training programs. All patients had passed entry-level military physical examinations and had no known preexisting diagnosis of a hip disorder. We identified 66 patients with FNSFs. Of these 66 patients, we excluded 12 owing to excessive pelvic tilt or rotation observed on the radiographs. The remaining 54 patients (108 hips) comprised our study group. The average age of these patients was 21.9 years (95% CI, 21.1–22.7 years), and all were male. The stress fracture involved the right hip in 33 patients and the left in 20 patients. One patient had bilateral stress fractures. We obtained prior Institutional Review Board approval.
The diagnosis of FNSF was made through a modified protocol previously described [24]. At-risk patients with hip pain initially are evaluated by clinical examination and plain radiography consisting of AP and frog-leg lateral pelvic films taken with the patient in a supine position. If radiographs are normal but suspicion for a stress fracture remains high, a bone scan is obtained. Patients with negative bone scans are treated conservatively and followed until symptoms resolve. In the presence of a positive bone scan, MRI is obtained to determine fracture location and degree of femoral neck involvement (Fig. 2). Patients with compression-sided fractures measuring less than 50% of the femoral neck width are treated with protected weightbearing. Those with compression-sided fractures measuring 50% or greater of the femoral neck width, any tension-sided fracture, or completed fractures are offered surgical stabilization (Fig. 3).
Fig. 2.
A coronal MR STIR image shows a right femoral neck stress fracture (arrow) with greater than 50% neck involvement.
Fig. 3.
An AP radiograph taken after prophylactic fixation of a femoral neck stress fracture shows a bilateral COS. The white line represents the posterior wall and the gray line represents the anterior wall.
Twenty-nine patients were treated operatively and 25 were treated nonoperatively. Two patients had completed stress fractures at the time of diagnosis and underwent urgent operative fixation.
We examined all AP pelvic radiographs for the presence of a COS and radiographic abnormalities of the femoral neck indicative of FAI, namely, decreased femoral head-neck offset and subcapital synovial herniation pits located on the anterolateral region of the femoral neck [1, 7]. One of us (KMK) measured femoral neck shaft angles using a digital goniometer on two separate occasions. The presence of a COS is influenced by the inclination or rotation of the pelvis [24]. Therefore, before inclusion in the study, all radiographs were assessed for adequacy using the technique described by Mast et al. [14]. We measured the distance between the tip of the coccyx and the pubic symphysis with digital calipers. If this distance was greater than 2 cm, the radiograph was considered to have excessive pelvic inclination and was excluded from the study. Pelvic rotation was evaluated by measuring the horizontal distance between the sacral midpoint and the center of the pubic symphysis. We considered a distance greater than 2 mm as indicating excessive pelvic rotation and these radiographs were eliminated from the study [24].
Our control group consisted of male patients aged 17 to 30 years evaluated at the Naval Medical Center San Diego’s emergency department for trauma between 2001 and 2006. We excluded patients with radiographic evidence of prior congenital or traumatic hip disorders and patients without a radiographically normal AP pelvic radiograph per the official radiologist report. Our radiologists do not routinely report on acetabular version on plain radiographs. We initially identified 700 consecutive normal AP radiographs of the pelvis. We subsequently excluded all patients not within the study’s age parameters, leaving 120 patients (120 radiographs) that met inclusion criteria. These were reviewed for adequacy using the previously described parameters for excessive tilt and rotation. Those not within study parameters were excluded, leaving 54 patients (108 hips). All patients were males, and the average age was 23.6 years (95% CI, 22.9–24.4 years). We evaluated these radiographs for the presence of a COS and radiographic femoral neck abnormalities. Neck shaft angles were measured using a digital goniometer and were recorded for both hips.
Neck shaft angles were compared in the study group for the affected and unaffected hips using a two-sample Wilcoxon rank sum test. Neck shaft angles of the affected hips were also compared with the neck shaft angles of both hips in the control group using a two-sample Wilcoxon rank sum test. The study and control groups were compared for the presence of a COS using Fisher’s exact test. Finally, we compared the proportion of subjects with the COS in our control group with the proportion of AR reported for healthy subjected using Fisher’s exact test. The proportion of radiographic abnormalities of the femoral neck was compared between groups with and without a positive COS using Fisher’s exact test.
Results
In the study group, 31 patients (57%) had a positive COS on the affected hip, which, when present, was detected bilaterally in each of these patients. The average neck shaft angle of the affected hip was 132°, which mirrored the neck shaft angle of the unaffected hip. Seven of 54 patients (13%) in the study group showed radiographic abnormalities of the femoral neck consistent with FAI, including decreased head-neck offset and synovial herniations. Five of these seven patients (71%) had a positive COS (Figs. 4, 5). Seventeen patients (31%) in the control group had a COS. When identified, the COS was present bilaterally in all patients. The average neck shaft angle was 135°. Six of 54 patients (11%) had radiographic abnormalities of the femoral neck consistent with FAI. Five of these six patients (83%) had a positive COS.
Fig. 4.
An AP radiograph shows the pelvis of a 21-year-old patient with bilateral COS (black arrow) and synovial herniations (gray arrow) on the left which correspond to a left-sided femoral neck stress fracture.
Fig. 5A–C.

(A) An AP radiograph shows a positive COS (gray arrow) and right-sided femoral neck stress fracture (black arrow). (B) The lateral radiograph of the right hip from same patient shows decreased head-neck offset (arrow). (C) An MR image from the same patient shows a compression-sided femoral neck fracture (arrow).
The average neck shaft angle of hips in the control group was greater (p = 0.001) than that of hips in the study group (Table 1). (Although this value achieved statistical significance, the difference was very small [3°] and we do not consider this difference clinically important.) The average neck shaft angles in the study group of the affected and unaffected hips were similar (p = 0.60). We observed a greater (p = 0.01) incidence of femoral neck radiographic abnormalities in individuals with a COS than those without regardless of the presence of a FNSF (Table 2).
Table 1.
Summary of group comparison
| Group | Number of patients | Average age (years) | Positive crossover sign | Femoral neck shaft angle (degrees) | Femoral neck radiographic abnormalities |
|---|---|---|---|---|---|
| FNSF group | 54 | 21.9 | 31 | 132 | 7 |
| Control group | 54 | 23.6 | 17 | 135 | 6 |
| P value | 0.009 | 0.001 |
FNSF = femoral neck stress fracture.
Table 2.
Radiographic signs of femoroacetabular impingement
| Crossover sign | Femoral neck radiographic abnormalities present | Femoral neck radiographic abnormalities absent | Total |
|---|---|---|---|
| Present | 10 (77%) | 38 (40%) | 48 |
| Absent | 3 (23%) | 57 (60%) | 60 |
| Total | 13 | 95 | 108 |
The incidence of a COS was greater (p = 0.009) in the study group.
Discussion
Increased incidences of AR in patients with various pathologic conditions of the hip have been reported in numerous studies [5, 8, 13, 21, 23, 25]. It is believed that variations in acetabular orientation alter contact pressures across the hip predisposing patients to these myriad disorders. Much previous work shows the pathologic consequences of AR on the acetabulum, although it stands to reason that the proximal femur is also affected by the abnormal orientation [5, 8, 21, 25]. The purposes therefore were to: (1) to present our algorithm for diagnosing and treating FNSF; (2) determine if there is an increased incidence of AR in patients with FNSFs compared with healthy control subjects; (3) determine if patients with FNSF have radiographic changes of the femoral neck that are suggestive of FAI; and (4) report the incidence of AR in a healthy military population and compare it with the reported incidence of AR in the general population.
There are several limitations to our study. First, because this study is a radiographic review only, no physical examination data were obtained for the study group to determine if these patients had clinical signs of FAI. Second, although the study group is small, it represents a fairly large group of patients with a rather rare injury. Third, we were unable to control for other risk factors for FNSF such as hormonal and nutritional factors or bone mineral density. Finally, all patients were male. This is secondary to the inherent gender bias of the military population and the fact that the recruit training facility in the area of our facility is male only. We therefore are unable to extrapolate our findings to female patients.
FNSFs occur most commonly in military recruits and endurance athletes who are subjected to prolonged, high-stress repetitive lower extremity loading activities [6, 22]. Proposed risk factors include coxa vara, female gender, hormonal factors, nutritional deficiencies, and bone mineral density [3, 4, 16, 17]. Symptoms often develop after initiating or increasing the intensity of a conditioning program [6]. Although nondisplaced FNSFs almost uniformly heal with appropriate treatment, there have outcomes do not always correlate with radiographic union [19, 26]. Some patients have long-term hip pain and decreased functional scores despite radiographic resolution [26]. Unrecognized or untreated, this injury will progress, resulting in fracture displacement. The consequences can be devastating and include nonunion, femoral head osteonecrosis, and secondary osteoarthritis resulting in long-term morbidity [12, 18]. The diagnostic algorithm described for detecting a FNSF has been used for 6 years at our institution and is successful in detecting most FNSFs before they displace. Bone scans reportedly have a sensitivity of 93% to 100% and specificity of 75% to 95% [20]. Although not as specific as MRI, it is still a sensitive diagnostic tool and more cost effective when dealing with a relatively large number of patients being screened for this diagnosis.
The data show that individuals with FNSFs have a greater incidence of AR than individuals without FNSFs. Although the retrospective nature of our study prevents us from identifying a causal relationship, the difference certainly delineates a clear association between AR and a FNSF. This association may be secondary to altered load distribution across the femoral neck. When the bony architecture of the femoral neck is weakened by high-frequency repetitive loading, additional stress caused by abnormal hip mechanics may result in further microdamage, which can overwhelm the bone’s reparative capabilities.
Although the relationship between AR and FAI has been well established [23], the contribution of mechanical impingement to the development of a FNSF has not. FAI can occur when a retroverted acetabulum acts as an obstacle to flexion and internal rotation of the hip resulting in impingement of the anterosuperior aspect of the head and neck against the proximal medial aspect of the acetabular rim. Radiographic findings seen in the proximal femur that are indicative of FAI include decreased femoral head-neck offset and subcapital synovial herniation pits on the anterolateral femoral neck [1, 7]. Our data show that these radiographic findings were seen more commonly in patients with AR, but not necessarily more commonly observed in patients with FNSFs. The case series by Beck et al. [2] lends further credence to the theory that FAI may contribute to altered forces across the femoral neck. They describe the mechanical effects of FAI resulting in nonunions in three patients with femoral neck fractures. All patients had radiographic union after surgical restoration of a more anatomic femoral head-neck offset and resolution of FAI.
The incidence of the COS in our control group (31%) was greater than has been reported (5%–16%) [5, 8, 10]. Using standardized radiographic techniques and established criteria to account for pelvic tilt and rotation, it is unlikely this finding is spurious. There may be a higher incidence of AR in the general population than has been observed: combined data from healthy patients show the COS to be present in 12 of 211 healthy subjects (6%) [6, 11], whereas the incidence of the COS in our control group (31%) was greater than the reported incidence (Table 3). A larger group of healthy subjects with good-quality AP radiographs is required to confirm this finding.
Table 3.
Comparison of historic controls with a control group
| Crossover sign | Historic controls | Study controls | Total |
|---|---|---|---|
| Present | 12 (6%) | 17 (31%) | 29 |
| Absent | 199 (94%) | 37 (59%) | 236 |
| Total | 211 | 54 | 265 |
AR appears more commonly in patients with a FNSF than in control subjects. Despite this association, it is unclear whether the presence of AR is a true risk factor for development of a FNSF. Additionally, our control group had an increased incidence of AR than was previously reported. Radiographic findings of FAI also were observed in patients with AR. Additional biomechanical and prospective studies are needed to investigate whether AR leads to increased stresses across the proximal femur and predisposes individuals to a FNSF. Potential implications of this study include more liberal use of advanced imaging screening modalities in military recruits with AR and the new onset of hip pain. Early recognition and treatment cannot be emphasized enough to prevent the devastating complications of a displaced FNSF.
Acknowledgments
We thank Joseph R. Carney, MD, and Robert H. Riffenburgh, PhD, for gracious assistance with the statistical analysis and data interpretation for this study. We also thank Waine Macallister for assistance with manuscript preparation.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical researchers at the Naval Medical Center San Diego operate under the auspices of The Office of Research Integrity and Ethics (ORIE) Responsible Conduct of Research Programs (BUMED), Bethesda, MD.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government.
References
- 1.Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691–701. doi: 10.1007/s00256-005-0932-9. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Leunig M, Clarke E, Ganz R. Femoroacetabular impingement as a factor in the development of nonunion of the femoral neck. J Orthop Trauma. 2004;18:425–430. doi: 10.1097/00005131-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Brudvig TJ, Gudger TD, Obermeyer L. Stress fractures in 295 trainees: a one-year study of incidence as related to age, sex and race. Mil Med. 1983;148:666–667. [PubMed] [Google Scholar]
- 4.Carpintero P, Leon F, Zafra M, Serrano-Trenas JA, Roman M. Stress fractures of the femoral neck and coxa vara. Arch Orthop Trauma Surg. 2003;123:273–277. doi: 10.1007/s00402-003-0514-z. [DOI] [PubMed] [Google Scholar]
- 5.Ezoe M, Naito M, Inoue T. The incidence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 6.Fullerton LR., Jr Femoral neck stress fractures. Sports Med. 1990;9:192–197. doi: 10.2165/00007256-199009030-00006. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 9.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of “cross-over sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 10.Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88:727–729. doi: 10.2106/JBJS.E.00550. [DOI] [PubMed] [Google Scholar]
- 11.Koch JC. The laws of bone architecture. Am J Anat. 1917;21:177–298. doi: 10.1002/aja.1000210202. [DOI] [Google Scholar]
- 12.Lee CH, Huang GS, Chao KH, Jean JL, Wu SS. Surgical treatment of displaced stress fractures of the femoral neck in military recruits: a report of 42 cases. Arch Orthop Trauma Surg. 2003;123:527–533. doi: 10.1007/s00402-003-0579-8. [DOI] [PubMed] [Google Scholar]
- 13.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 14.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53. doi: 10.1097/00003086-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15:46–58. doi: 10.1177/036354658701500107. [DOI] [PubMed] [Google Scholar]
- 16.Muldoon MP, Padgett DE, Sweet DE, Deuster PA, Mack GR. Femoral neck stress fractures and metabolic bone disease. J Orthop Trauma. 2001;15:181–185. doi: 10.1097/00005131-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Niva MH, Kiuru MJ, Haataja R, Pihlajamaki HK. Fatigue injuries of the femur. J Bone Joint Surg Br. 2005;87:1385–1390. doi: 10.1302/0301-620X.87B10.16666. [DOI] [PubMed] [Google Scholar]
- 18.Pihlajamaki HK, Ruohola JP, Kiuru MJ, Visuri TI. Displaced femoral neck fatigue fractures in military recruits. J Bone Joint Surg Am. 2006;88:1989–1997. doi: 10.2106/JBJS.E.00505. [DOI] [PubMed] [Google Scholar]
- 19.Pihlajamaki HK, Ruohola JP, Weckstrom M, Kiuru MJ, Visuri TI. Long-term outcome of undisplaced fatigue fractures of the femoral neck in young male adults. J Bone Joint Surg Br. 2006;88:1574–1579. doi: 10.2106/JBJS.E.00505. [DOI] [PubMed] [Google Scholar]
- 20.Prather JL, Nusynowitz ML, Snowdy HA, Hughes AD, McCartney WH, Baggs RJ. Scintographic findings in stress fractures. J Bone Joint Surg Am. 1977;59:869–874. [PubMed] [Google Scholar]
- 21.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 22.Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293–302. doi: 10.5435/00124635-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 25.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Weistroffer JK, Muldoon MP, Duncan DD, Fletcher EH, Padgett DE. Femoral neck stress fractures: outcome of analysis at minimum five-year follow-up. J Orthop Trauma. 2003;17:334–337. doi: 10.1097/00005131-200305000-00003. [DOI] [PubMed] [Google Scholar]