Abstract
Osteonecrosis (ON) has been reported in femoral remnants removed after failure of hip resurfacing arthroplasty. Experimental and clinical studies have further described thermal effects of the cementation technique, damage of extraosseous blood vessels, and intraoperative hypoxemia as possible causative factors. We analyzed histologically a series of 123 retrieved specimens with a preoperative diagnosis other than ON to investigate the incidence and extent of advanced ON. ON was found in 88% of cases and associated with 60% (51 of a total of 85) of periprosthetic fractures. The fracture incidence correlated with the extent of ON. Collapse of necrotic tissue in three (2%) cases resulted in disconnection of the bone stock-femoral component. We observed smaller regions of superficial ON in the majority of the remaining femoral remnants with periprosthetic fractures and in hips that failed for reasons other than fracture.
Introduction
Conventional ON is a multifactorial debilitating disease that typically affects patients between 20 and 50 years of age. This disease, which often leads to destruction of the hip, most commonly affects the femoral head [11].
In previous retrieval studies, the occurrence of necrotic changes in retrieved femoral remnants was seen in cases with a preoperatively histologically proven absence of conventional ON at the dome of the femoral remnant [10, 16, 17]. Furthermore, ON was described mostly in failures attributable to fractures [14, 16, 17] and was suggested as a cause of the fracture [3, 5, 16]. Several causes of ON, particularly those related to surgical techniques, such as the effects of cementation [1, 7–9] or intraoperative extraosseous vascular injury [2, 4, 15, 18, 21], have been discussed.
Our primary objective was to describe (1) the incidence, morphologic features, and extent of ON after failed hip resurfacing arthroplasty. Furthermore, we asked whether there was a relationship between the extent of osteonecrotic lesions and (2) the distinct failure modes of this modern replacement technique and (3) characteristics of patients who underwent surgery.
Material and Methods
We retrospectively reviewed 123 specimens from patients undergoing revision of hip resurfacing femoral systems from January 2004 to July 2008. To minimize the possible influence of preoperative ON on our results, we excluded patients with primary ON. We examined the specimens macroscopically and histologically and also examined their contact radiographs; we determined the vertical size of the ON of the femoral remnant bone. Only complete specimens removed at revision surgery with the femoral component in situ were examined and fragmented specimens or those without bone in the femoral components were excluded. Detailed clinical information was available for all patients. Demographic data including age and gender of the patient, body mass index (BMI), and indication for arthroplasty were recorded. The cohort included 63 (51%) men (mean age ± standard deviation, 56.9 ± 9.0 years) and 60 (49%) women (age, 54.2 ± 9.2 years). Most hips were treated for advanced stages of osteoarthritis (n = 96). Other conditions were developmental hip dysplasia (n = 13), posttraumatic arthritis (n = 7), and rheumatoid arthritis (n = 7). Nine specimens from patients with known primary ON of the femoral head were excluded.
Eighty-five of the 123 revisions (69%) were performed for periprosthetic fractures, 10 (8%) for acetabular loosening, and the remaining 28 (23%) for other causes such as groin pain or femoral component loosening. Fifty-one of the 85 specimens (60%) with periprosthetic fractures had complete ON of bone tissue proximally from the fracture line and thus were defined as postnecrotic fractures. The remaining 34 (40%) fractures had some vital bone tissue in the fractured bone segment and were considered biomechanical fractures.
The specimens came from patients with five hip resurfacing femoral systems: 98 Articular Surface Replacements (ASR™; DePuy Orthopaedics, Inc, Warsaw, IN), nine Birmingham Hip Resurfacing (BHR™; Smith & Nephew, London, UK), five Cormet™ (Corin Group PLC, Cirencester, UK), six DUROM® (Zimmer Inc, Warsaw, IN), and five ReCAP® (Biomet Inc, Warsaw, IN). Data regarding surgical approach were not available.
All specimens were formalin-fixed femoral head remnants. A central 4-mm-thick slice was cut from the revised hips with the femoral component in situ in the femoral neck plane using a water-cooled diamond-coated saw (Exakt Apparatebau GmbH, Norderstedt, Germany) [12, 13]. The central slice was photographed macroscopically, radiographed (Faxitron X-Ray LLC, Wheeling, IL), completely embedded in methylmethacrylate (Technovit 7200 VLC®; Heraeus Kulzer, Wehrheim, Germany) ground, and stained with toluidine blue (MH). Another section in the anteroposterior (AP) plane perpendicular to the former was removed from the implantation device using acetone and completely embedded in methylmethacrylate. Undecalcified processed histopathologic slides were stained with toluidine blue, Goldner trichrome, and von Kossa staining. The remaining bone tissue of the femoral head and neck remnant was stored in buffered formalin.
Macroscopically, necrotic bone tissue appeared pale and white-yellowish with scattered chalky white precipitations. Intraosseous cement penetrations were recognized by their hard consistency, fine granular structure, and white color. At the border of ON, a zone of hyperemia and bone sclerosis was apparent in some cases. Soft tan-brown fibrous masses distal to the ON were characteristic for collapsed fibrous tissue. Pseudarthrosis was characterized by an irregular thin bluish-white line in the vital bone tissue.
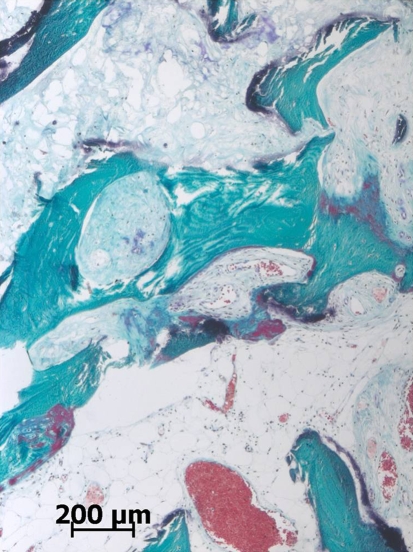
Using contact radiography, two of us (JZ, MA) independently identified ON by adjacent sclerosis and condensation of bone structure distal to the lesion, similar with Ficat Stages II–III ON [6]. A thin radiolucent zone between the proximal necrotic area and bordering sclerosis of the vital bone suggested ongoing resorptive changes. A thick radiolucent area was considered collapsed fibrocartilaginous tissue. A thinner horizontal radiolucent line in the bone tissue was typical for pseudarthrosis. The remaining bone tissue was stored in formalin to enable future analysis, if needed. Cement mantle and intraosseous cement penetrations were observed as less opaque fine granular areas at the bone-implant interface. Superficial cemented bone cysts and additional drill holes were differentiated owing to their size, shape, and regularity of the margins of the lesions. To confirm the macroscopically and radiographically suggested diagnosis of ON, two of us (JZ, MA) independently examined histologically the cutting plane from each of three quadrants of the femoral bone remnant embedded in its full length. Microscopically, we defined an advanced lesion [20] by the presence of trabeculae without stainable osteocytes, disorganized bone marrow, and bordering fibrosis (Fig. 1). Weighted kappa analysis was used to calculate the reliability of interobserver (JZ, MA) agreement for diagnosing advanced ON. Interobserver agreement on diagnosis of the presence or absence of ON was observed in 93% (kappa = 0.728). Although interrater agreement clearly was weaker in the group with failed results who had revision surgery within the first 6 months after the index surgery (kappa = 0.314), the diagnosis of advanced ON was not problematic in the remaining specimens (kappa = 0.940).
Fig. 1.
The typical features of the bordering fibrosis between ON (top) and vital bone tissue (bottom) are shown. No sharp border of ON is seen in the partly necrotic bone trabeculae. Moderate hyperemia and appositional new bone formation (center) are visible at the border of the lesion. The adjacent bone marrow shows marked hyperemia and absence of hematopoiesis (Stain, Goldner; original magnification, ×400).
The extent of ON was quantified as follows. The most representative cutting plane was chosen for subsequent metric analysis. For patients with clinical fractures, we recorded a minimal vertical distance between the proximal surface of the femoral head and fracture line. For patients with failed results not attributable to fracture, we recorded a minimal vertical distance between the surface of the femoral head and bordering fibrosis.
Descriptive statistics were performed to describe means and standard deviations. As time to revision surgery and size of ON deviated clearly from a normal distribution, a nonparametric analytic method was used (Kruskal-Wallis test). Analysis of data was performed using SPSS® 15.0 for Windows® software (SPSS Inc, Chicago, IL).
Results
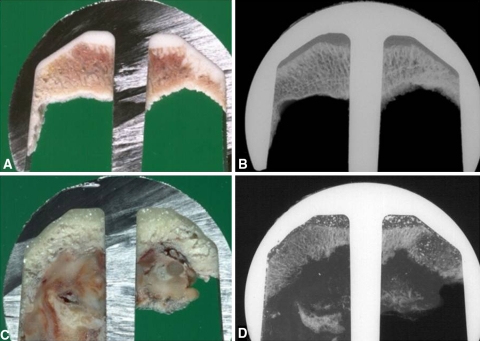
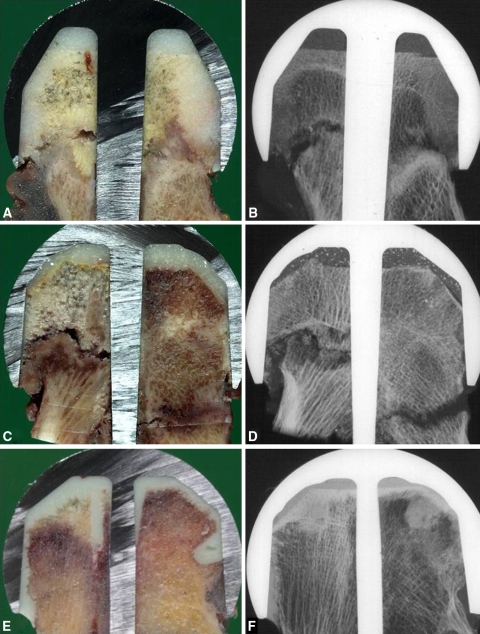
We observed ON of the femoral remnant tissue in 108 (88%) of 123 cases. In typical cases, we detected more or less similar zones of bone necrosis in all three analyzed quadrants. Femoral remnant bone tissue of 51 patients (60%) who had revision surgery for periprosthetic fractures showed histologically advanced ON proximal to the fracture line (Fig. 2A–B). Three (2%) patients had collapsed fibrous tissue leading to bone-implant disconnection (Fig. 2C–D). Patients with a less typical pattern of ON had progression of the fracture line throughout the bone necrosis and bordering fibrosis (Fig. 3A–B). Rarely, but predominantly in patients with large asymmetric necrosis, the fracture line was detected in the zone of bordering fibrosis at one side and located more distally in the vital bone tissue on the other side. Similarly to the former, two other patients had collapsed ON at one side leading to fracture nonunion with pseudarthrosis on the other side (Fig. 3C–D). Three (2%) patients had triangle-shaped segmental ON (Fig. 3E–F) associated with deep fixation drill holes.
Fig. 2A–D.
(A) The typical pattern of failure caused by a periprosthetic fracture associated with superficial dome-shaped ON after a hip resurfacing arthroplasty is characterized by yellowish bone tissue without vital reaction. (B) A corresponding contact radiograph illustrates the absence of lytic or sclerotic changes. (C) A similar ON lesion with adjacent elastic brownish fibrosis reveals (D) multiple small collapsed bone fragments in the fibrosis in a hip revised for loosening of the femoral component.
Fig. 3A–F.
(A) A large area of ON after hip resurfacing arthroplasty shows propagation of the fracture line throughout the bordering fibrosis and ON lesion. (B) A corresponding contact radiograph reveals typical bordering fibrosis. (C) An asymmetric segmental ON lesion was observed in hips with partial collapse and a contralateral irregular zone of fibrocartilaginous tissue. (D) A contact radiograph shows several bone fragments in the collapsed tissue and contralateral nonunion. (E) A small triangle-shaped ON lesion with its base at the dome and one side touching a thin deep additional fixation drill hole is seen proximally. (F) Sclerosis is evident at the border of the triangle-shaped ON lesion.
Clearly, the vertical size of the ON lesion was larger (p < 0.0001) in the 51 hips with postnecrotic fractures (20.7 ± 8.6 mm) than in the remaining 34 biomechanical fractures (6.4 ± 7.2 mm) and the 38 hips revised for reasons other than fractures (2.9 ± 5.3 mm) (Table 1). Hips with ON failed earlier (p = 0.0369) than hips with vital bone tissue (in situ time, 229.9 ± 291.7 days versus 511.5 ± 485.0, respectively) (Table 2).
Table 1.
Relationship between failure modes, characteristics, and vertical size
| Characteristic | Number | Vertical size of osteonecrosis (mm)* | p Value |
|---|---|---|---|
| Failure pattern | < 0.0001 | ||
| No fracture | 38 | 2.9 ± 5.3 | |
| Biomechanical fracture | 34 | 6.4 ± 7.2 | |
| Postnecrotic fracture | 51 | 20.7 ± 8.6 | |
| Clinical diagnosis | 0.4925 | ||
| Hip dysplasia | 13 | 7.5 ± 8.0 | |
| Primary osteoarthritis | 96 | 11.3 ± 10.9 | |
| Rheumatoid arthritis | 7 | 12.8 ± 16.4 | |
| Posttraumatic arthritis | 7 | 15.9 ± 8.6 | |
| Gender | 0.0074 | ||
| Men | 63 | 13.8 ± 11.5 | |
| Women | 60 | 8.6 ± 9.6 | |
| Total | 123 | 11.3 ± 10.9 |
* Values are expressed as mean ± standard deviation.
Table 2.
Relationship between the duration of implantation, age, and BMI
| Variable | Gender | Osteonecrosis present | Osteonecrosis absent | p Value |
|---|---|---|---|---|
| In situ time (days) | 0.0369 | |||
| Men | 207.4 ± 303.3 | 353.5 ± 200.9 | ||
| Women | 257.5 ± 277.4 | 574.7 ± 557.5 | ||
| Age (years) | 0.6836 | |||
| Men | 56.7 ± 9.0 | 57.3 ± 10.1 | ||
| Women | 54.3 ± 9.0 | 53.6 ± 11.1 | ||
| BMI (kg/m2) | 0.3008 | |||
| Men | 27.4 ± 3.2 | 25.2 ± 4.3 | ||
| Women | 25.4 ± 4.3 | 25.4 ± 4.7 |
Values are expressed as mean ± standard deviation; BMI = body mass index.
Patients with posttraumatic arthritis had more extensive (p = 0.0357) ON than patients with dysplastic hips (15.9 ± 8.6 mm versus 7.5 ± 8.0 mm, respectively). We found no relationship between the size of the ON lesion and other clinical diagnoses. Even though there was a similar (p = 0.3359) frequency of patients of both genders in the entire cohort (63 men of 123 patients) and in the group of patients with histologically proven ON (59 men of 108 patients), we found a higher (p = 0.0357) proportion of men (33 of 51) in the group of patients with postnecrotic fractures. Furthermore, the mean size of the ON lesions in the femoral remnants of men (13.8 ± 11.5 mm) was larger (p = 0.0074) than that of women (8.6 ± 9.6 mm) (Table 1). The incidence of ON did not correlate with age of patients or their BMI (Table 2).
Discussion
Retrieval analyses of femoral remnants of failed hip resurfacing arthroplasties attributable to either fracture [3, 5, 9, 12, 16, 17] or loosening [3] suggest the presence of ON. ON reportedly occurs predominantly in early- and midterm hip failures and may relate to impaired blood supply to the femoral head [2, 15, 18] or heat injury [7, 8] at the time of surgery. We therefore analyzed the incidence, extent, and morphologic features of ON in a large series of retrieval specimens. Furthermore, we explored a possible relationship between the extent of osteonecrotic lesions with distinct failure modes and the characteristics of patients with failed arthroplasties.
We recognize several limitations to the current retrieval study. First, as we analyzed only failed replacements, the real incidence of ON after hip resurfacing arthroplasty remains unclear. Second, we had minimal clinical data for statistical analysis of the relationship between the incidence of ON and surgical technique. However, we obtained specimens from multiple international practicing orthopaedic surgeons, mostly from smaller institutions. Therefore, our cohort may reflect a routine experience away from specialized university or design centers. Third, the heterogeneity and asymmetry of pathologic changes in some bone remnants might constitute another limitation to our study. However, as we morphologically analyzed radial sections from three quadrants of each specimen in its full length and quantified the most representative one of them, we suggest our observations are relevant for assessing the vertical extent of ON. This highly standardized sampling method also helped us identify hips with asymmetric and/or only focal lesions. Finally, the interindividual variability between patients and osseous changes related to the preoperative hip disease also should be taken into account.
Previous studies have suggested ON is related to failure of resurfacing arthroplasty in some cases. Treacy et al. supposed its incidence in one or two per thousand cases [19]. Contrary to their suggestion, Campbell et al. assumed ON induced seven failures of 98 studied retrieval specimens [3]. Little et al. found ON in 12 of 13 retrieved specimens (after 377 implantation procedures) [10], and Steffen et al. found ON in all nine histologically analyzed postoperative fractures of 842 procedures [16]. These studies suggested ON was secondary to implantation in causing these failures. We found histologically advanced ON in the majority of analyzed femoral remnants. More than ½ of all fractures and five hips with collapsed tissue seemed to be caused by ON. Hips with ON failed earlier and fractured more frequently than the remaining hips. A similar association has not been described before. Similar to Little et al. [10] and Campbell et al. [3], we also experienced considerable difficulties in identifying ON during the first weeks or months after the implantation surgery. At this time, reactive changes of bone tissue after implantation or fracture might exhibit histologic findings similar to those with early or minimal ON. After the implantation, advanced ON lesions [20] were associated with characteristic morphologic changes previously described as extensive [3] or established [10], and the diagnosis was straightforward.
The extent of ON described by Campbell et al. (45 cases) varied as much as several millimeters [3], but the authors did not describe any possible relationship of extent with distinct failure patterns. Treacy et al. [19] (one hip) and Steffen et al. [16] (nine fractural failures) described even larger lesions in the femoral neck but did not further quantify their extent. We measured vertical extension of ON in all 108 positive cases (of 123 retrievals) and found lesions as much as 42-mm. As the region of ON was larger in specimens from hips with postnecrotic fractures than in hips with biomechanically caused fractures and those revised for reasons other than fractures, we suggest the extent of the lesion might relate to its outcome. An association of lesion size of ON with its outcome would be similar to that proposed in most classification systems for conventional ON of the femoral head [11]. We found larger lesions were associated with periprosthetic fractures and larger lesions collapsed more frequently than smaller ones. However, other mechanical factors such as the stabilizing effect of the femoral component in smaller lesions and edge loading in large ones also may influence the risk of this type of periprosthetic fracture. Even though we found several asymmetric wedge-shaped lesions, the majority of lesions were symmetric and located superficially at the dome. Although the fracture line in postnecrotic fractures associated with smaller lesions occurred typically in the areas of adjacent resorption, we observed the fracture line in larger periprosthetic lesions directly in the osteonecrotic area or partly outside the lesion.
The most surprising outcome was that men dominated in the group with postnecrotic fractures and had larger lesions than women. As we had more than 100 specimens with ON, this was not likely a chance association from a small number of analyzed specimens. Consistent with our finding, seven of eight patients with fractures and histologically documented ON described by Little et al. were men [10]. We found the largest mean size of ON in hips with posttraumatic arthritis, probably caused by inadequately restored intraosseous blood circulation after the trauma.
We found histologically advanced ON in the majority of specimens in a series of retrievals from metal-on-metal hip resurfacing arthroplasties. ON appeared to be causative in 46% of all failures attributable to postnecrotic periprosthetic fractures and collapse. Typical symmetric lesions were seen at the dome of the femoral remnant. We identified ON more frequently in men, whose lesions were larger than those of women.
Acknowledgments
We thank Michael Hahn, PhD, for assistance with processing the specimens. We also thank all cooperating orthopaedic surgeons who provided us with cases.
Footnotes
One or more of the authors received from DePuy Orthopaedics, Inc, Warsaw IN (MM, MA); Smith & Nephew, London, UK (MM, MA); Corin Group PLC, Cirencester, UK (MM, MA); Zimmer Inc, Warsaw, IN (MM, MA); and Biomet Inc, Warsaw, IN (MM, MA).
This work was performed at University Medical Center Hamburg-Eppendorf and TUHH University of Technology Hamburg-Harburg.
References
- 1.Amstutz HC, Campbell PA, Le Duff MJ. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg Am. 2004;86:1874–1877. doi: 10.2106/00004623-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Beaule PE, Campbell PA, Hoke R, Dorey F. Notching of the femoral neck during resurfacing arthroplasty of the hip: a vascular study. J Bone Joint Surg Br. 2006;88:35–39. doi: 10.2106/JBJS.F.00592. [DOI] [PubMed] [Google Scholar]
- 3.Campbell P, Beaule PE, Ebramzadeh E, Le Duff M, Smet K, Lu Z, Amstutz HC. A study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46. doi: 10.1097/01.blo.0000238777.34939.82. [DOI] [PubMed] [Google Scholar]
- 4.Capello WN, Ireland PH, Trammel TR, Eicher P. Conservative total hip arthroplasty: a procedure to conserve bone stock Part I: analysis of sixty-six patients. Part II: analysis of failures. Clin Orthop Relat Res. 1978;134:59–74. [PubMed] [Google Scholar]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 6.Ficat RP. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 7.Gill HS, Campbell PA, Murray DW, Smet KA. Reduction of the potential for thermal damage during hip resurfacing. J Bone Joint Surg Br. 2007;89:16–20. doi: 10.1302/0301-620X.89B1.18369. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh PH, Tai CL, Liaw JW, Chang YH. Thermal damage potential during hip resurfacing in osteonecrosis of the femoral head: an experimental study. J Orthop Res. 2008;26:1206–1209. doi: 10.1002/jor.20639. [DOI] [PubMed] [Google Scholar]
- 9.Little CP, Gray HA, Murray DW, Beard DJ, Gill HS. Thermal effects of cement mantle thickness for hip resurfacing. J Arthroplasty. 2008;23:454–458. doi: 10.1016/j.arth.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty. J Bone Joint Surg Br. 2005;87:320–323. doi: 10.2106/JBJS.D.02927. [DOI] [PubMed] [Google Scholar]
- 11.Mont MA, Marulanda GA, Jones LC, Saleh KJ, Gordon N, Hungerford DS, Steinberg ME. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(suppl 3):16–26. doi: 10.2106/JBJS.F.00457. [DOI] [PubMed] [Google Scholar]
- 12.Morlock M, Bishop N, Ruether W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proc Inst Mech Eng H. 2006;220:333–344. doi: 10.1243/095441105X69015. [DOI] [PubMed] [Google Scholar]
- 13.Morlock MM, Bishop N, Zustin J, Hahn M, Rüther W, Amling M. Modes of implant failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg Am. 2008;90(suppl 3):89–95. doi: 10.2106/JBJS.H.00621. [DOI] [PubMed] [Google Scholar]
- 14.Shimmin AJ, Bare J, Back DL. Complications associated with hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:187–193, ix. [DOI] [PubMed]
- 15.Steffen RT, Fern D, Norton M, Murray DW, Gill HS. Femoral oxygenation during hip resurfacing through the trochanteric flip approach. Clin Orthop Relat Res. 2009;467:934–939. doi: 10.1007/s11999-008-0390-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steffen RT, Foguet PR, Krikler SJ, Gundle R, Beard DJ, Murray DW. Femoral neck fractures after hip resurfacing. J Arthroplasty. 2009;24:614–619. doi: 10.1016/j.arth.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90:436–441. doi: 10.1302/0301-620X.90B4.19648. [DOI] [PubMed] [Google Scholar]
- 18.Steffen RT, Smith SR, Urban JP, McLardy-Smith P, Beard DJ, Gill HS, Murray DW. The effect of hip resurfacing on oxygen concentration in the femoral head. J Bone Joint Surg Br. 2005;87:1468–1474. doi: 10.1302/0301-620X.87B11.16780. [DOI] [PubMed] [Google Scholar]
- 19.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 20.Berg BE, Malghem JJ, Labaisse MA, Noel HM, Maldague BE. MR imaging of avascular necrosis and transient edema of the femoral head. Radiographics. 1993;13:501–520. doi: 10.1148/radiographics.13.3.8316660. [DOI] [PubMed] [Google Scholar]
- 21.Whiteside LA, Lange DR, Capello WR, Fraser B. The effects of surgical procedures on the blood supply to the femoral head. J Bone Joint Surg Am. 1983;65:1127–1133. [PubMed] [Google Scholar]