Abstract
THA in young patients is challenging regarding restoration and survival because patients are young, active, and tend to have disturbed anatomy. We asked whether a three-dimensional custom cementless stem could restore hip function, decrease osteolysis and wear, and enhance stem survival in young patients. We retrospectively reviewed 212 patients (233 hips) younger than 50 years (mean, 40 years) at a followup of 5 to 16 years (mean, 10 years). The Merle D’Aubigné-Postel and Harris hip scores improved at last followup. No thigh pain was recorded for any of the patients; 187 of the 212 patients (88%) had full activity recovery, 206 had full range of motion, and 151 had a score greater than 80 points for all five categories of the Hip disability and Osteoarthritis Outcome score. Five patients had femoral osteolysis not associated with pain. With revision for any reason as an end point, the survivorship was 87% (range, 77%–97%) at 15 years, and considering stem revision only, the survivorship was 93% (confidence interval, 90%–97%) at 15 years. Our data compare favorably with those from series using standard cementless stems at the same followup with a high percentage of patients achieving functional restoration and a low rate of complications.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The success of THA in older patients inevitably has led to its increased use in young and active patients. It generally is expected that THA in this population will have higher rates of femoral loosening and osteolysis compared with those in the general population [11, 14, 33]. As a result of increased life expectancy and functional demand, patients younger than 50 years present new challenges, including restoration of full ROM, quick and complete return to physical activity, long-term bone-implant fixation, and a low rate of revision for polyethylene wear or osteolysis [34, 41].
On the femoral side, the durability of cementless components may be at least as good as for cemented implants, particularly in young patients [23], but depend on the design, the material, or the type of coating used [6, 9, 10]. Several major issues must be addressed when using cementless stems: initial implant stability, durable long-term bone-implant fixation, strain transmission to the proximal femur, and restoration of hip mechanics (ie, the design of the extramedullary portion of the implant including variations of femoral anteversion, femoral offset, and neck-shaft angle). Primary stability of the stem is a prerequisite to secondary bone ingrowth and proper long-term fixation. Initial stability depends either on filling the proximal femur with intimate contact between the stem and the anatomic shape of the proximal femur (an anatomic fit) or filling the femoral diaphysis [56]. In previous anatomic studies, important anatomic variations in the upper femur intramedullary shape and the femoral neck (femoral anteversion, femoral offset, and neck-shaft angle) were described for primary hip osteoarthritis (OA) [29] or developmental dysplasia of the hip (DDH) [3, 4]. Proximally porous-coated stems not anatomic in shape reportedly have a revision rate resulting from aseptic loosening of 0.9% at 15 to 18 years followup [11]. However, when proximal fixation on cancellous bone is favored with an anatomic stem, optimal fit-and-fill of the metaphysis can be difficult to obtain with commercially available marketed prostheses, even with various anatomic designs and sizes [40]. Furthermore, abnormal femoral anatomy affects not only the intramedullary canal, but also the extramedullary part of the femur [29]. Considering intramedullary and extramedullary expected anatomic variations, we presumed custom cementless stems might restore and maintain hip function and result in less osteolysis and a high survival rate in patients younger than 50 years. In a midterm study of patients younger than 65 years [56] treated with custom implants, the mean Harris hip score was 98.8 points (range, 84-100) and the survival rate was 100% without complications or reoperations, but no published data were available for a custom stem in patients younger than 50 years.
We then asked whether (1) a custom cementless stem in patients younger than 50 years restores hip function as measured by the Harris hip score, the Hip disability and Osteoarthritis Outcome score (HOOS), and return to previous activity level; (2) the stems would remain stable with a low rate of osteolysis and wear; and (3) custom cementless stems would provide high survivorship.
Patients and Methods
We retrospectively reviewed all 233 uncemented first-time THAs performed in 212 patients younger than 50 years using a custom hydroxyapatite (HA)-coated stem and an HA-coated acetabular component with a ceramic on ultrahigh-molecular-weight-polyethylene (UHMWPE) liner at our institution between January 1990 and September 2002. We included patients with first-time custom cementless THAs performed for primary OA, avascular necrosis (AVN), or Grades 1 and 2 DDH according to the classification of Crowe et al. [15], age between 18 and 50 years, and a minimum followup of 5 years. The indications were 115 secondary hip OA (49.4%) with 27 posttraumatic and 88 resulting from DDH (according to Crowe et al. [15]: Groups I and II, excluding Groups III and IV), 77 AVN (33%), and 41 primary hip OA (11.6%). Twenty-four patients (10.3%) had previous surgery on the affected hip, including 12 isolated shelf arthroplasties, seven isolated intertrochanteric osteotomies (ITO), and five combined shelf arthroplasties with ITO. The preoperative Charnley’s patient category [12] was Category A (single hip with OA) for 194 patients, Category B (bilateral hips with arthritis) for 34 patients, and Category C (multiple joints affected with arthritis or a chronic disease that affects health-related quality of life, specifically walking) for five patients. According to the activity score of Devane et al. [19], all patients were higher than Grade 3. Patients included in the current series represented 19.4% of the total THAs performed during the same period. Their mean age at surgery was 42.6 ± 4 years (range, 20–50 years). Their mean weight was 71 ± 15 kg (range, 42–120 kg), and mean height was 170 ± 10 cm (range, 142–192 cm) for a mean body mass index (BMI) of 25 ± 5 kg/m2 (range, 16–48 kg/m2); 112 patients (48.1%) were then overweight, including 27% who were obese. The minimum clinical followup was 5 years (mean, 10 years; range, 5–16 years), 162 patients (69.5%) with followups greater than 10 years and 28 (12%) with followups greater than 15 years. No patients were lost to followup. Approval of the local ethical committee was obtained.
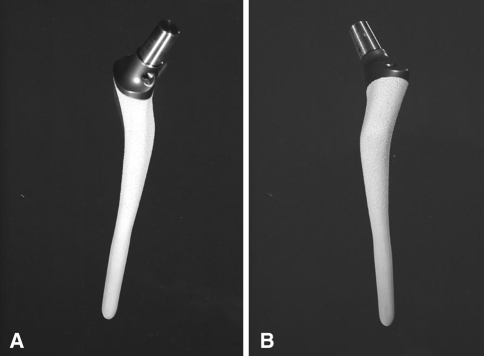
All the procedures were performed by the two senior surgeons (JNA, JMA) using the anterolateral Watson-Jones approach with the patient in the supine position. The same uncemented custom Ti-alloy HA fully coated stem (Symbios®, Yverdon, Switzerland) was used in all patients (Fig. 1). The custom femoral stem design was based on preoperative radiographs and CT scan analysis and individually customized for each patient. The radiographs include AP and lateral views of the hip, an AP view of the pelvis, and full-length views of the two lower limbs (with the patient in the supine position), which enables estimation of lengthening and offset correction necessary during the definitive surgery. A CT scan is performed to plan the three-dimensional design of the stem for its intramedullary fit, promoting cancellous bone contact without cortical bone contact. This is allowed by the use of a smooth custom stainless steel rasp of the same shape to compact the cancellous bone. The CT scan also allows evaluating the correction needed for the prosthetic neck’s appropriate offset and anteversion [29]. The surgeon provides the engineer with the correction to be made laterally for each patient based on the contralateral side when normal or on the lever arm ratio described by Amstutz and Sakai [2] and the abductor angle [24] when abnormal or in the case of bilateral disease. Regarding the additional information provided by the CT scan (femoral neck anteversion) and the lengthening to be realized (based on the full-leg view of the limbs), the prosthetic three-dimensional neck then can be calculated (Table 1). A hemispheric uncemented Ti-alloy HA-coated cup (Hilock; Symbios®) was used in all patients. In all cases, the insert was an UHMWPE liner. The mean acetabular component diameter was 53 mm (range, 44–64 mm) and a 28-mm diameter alumina-made femoral head routinely was inserted.
Fig. 1A–B.
(A) Medial and (B) lateral views of the the custom titanium alloy hydroxyapatite-coated stem are shown.
Table 1.
Population characteristics
| Population group | Whole series | Osteoarthritis | Posttraumatic | Developmental dysplasia of the hip | Avascular necrosis |
|---|---|---|---|---|---|
| Number of hips | 233 | 41 | 27 | 88 | 77 |
| Mean age (years) | 42.6 (20 to 50) | 44 (28 to 50) | 43.1 (23 to 50) | 41.9 (20 to 49) | 43.7 (31 to 50) |
| Lengthening to be realized (mm) | 6.8 (0 to 52) | 3 (0 to 25) | 8.7 (0 to 30) | 10.7 (0 to 20) | 4.3 (0 to 25) |
| Lateral correction (mm) | 2.5 (−30 to 25) | 2.3 (−20 to 20) | 2.1 (0 to 12) | 3.4 (−30 to 20) | 1.7 (−12 to 25) |
| Femoral anteversion (°) | 19 (−22 to 85) | 14 (−14 to 50) | 20 (−15 to 53) | 26 (−22 to 85) | 13 (−14 to 50) |
| Anteversion correction (°) | −4 (−70 to 37) | 1.2 (−35 to 29) | −5 (−38 to 30) | −11.5 (−70 to 37) | 1.4 (−35 to 29) |
Postoperative rehabilitation protocols included immediate weightbearing protected by crutches during the first 2 or 3 weeks according to patient tolerance, and exercises focused on passive and then active recuperation of ROM. All patients received routine thromboprophylaxis with low-molecular-weight heparin preoperatively and postoperatively for 21 days.
All patients were clinically evaluated preoperatively, 3 months postoperatively, at yearly intervals, and at last followup by the treating surgeons. The last clinical and radiographic reviews were performed by one orthopaedic surgeon not involved in the treatment (XF). Clinical outcomes were evaluated preoperatively and postoperatively using the Merle D’Aubigné-Postel score [17] and the Harris hip score [27] to determine the patient’s functional level. The presence or absence of thigh pain also was recorded at each visit. A subjective postoperative functional evaluation was performed using the HOOS [45]. The HOOS is a self-administered hip-related quality-of-life questionnaire including five dimensions scored separately: pain (nine items); symptoms (seven items); activities of daily life function (17 items); sport and recreation function (five items); and quality of life (four items). All items are scored from 0 to 4, and each of the five scores is calculated as the sum of the items included. Scores then are transformed using free calculation software available online (www.koos.nu) to a 0 to 100 scale with zero representing extreme hip problems and 100 representing no hip problems. We did not determine the HOOS score preoperatively because it had not yet been published. The patients’ level of activity was evaluated using the UCLA score [7]. The patients were asked to indicate his or her current level of activity.
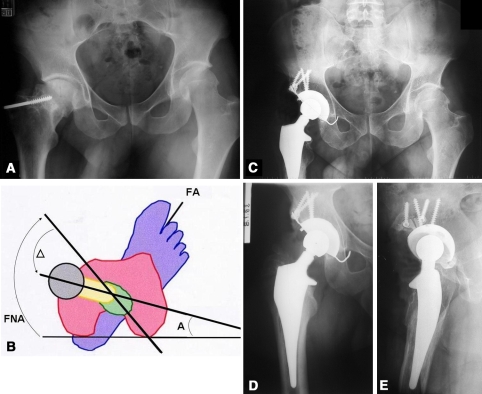
Radiographic postoperative evaluations were made on AP views of the hip and pelvis and a true lateral view of the hip (Fig. 2). The first postoperative radiograph then was used as a baseline from which subsequent radiographs were interpreted. One of us (XF) measured the distance from the acetabular teardrop to the lesser trochanter as a reflection of postoperative leg lengths. No intraobserver or interobserver variability assessment was performed. The femur was analyzed using the seven zones described by Gruen et al. [26] and the corresponding seven zones on the lateral radiograph. We recorded progressive radiolucencies, radiolucencies greater than 2 mm in width, and the presence of osteolysis. The femoral component stability was evaluated according to the criteria of Engh and Bobyn [21]. We considered a stem loose if subsidence was greater than 2 mm or if the angular position of the stem shifted more than 2°. Polyethylene wear was measured using IMAGIKATM software (View tech®; CMC Corp, Edison, NJ). Three points were required to measure the head diameter and three others for the cup. The linear penetration then was determined by the distance from the cup center to the femoral head center.
Fig. 2A–E.
(A) A preoperative frontal view of the pelvis shows left hip osteoarthritis. The patient was a 49-year-old woman who subsequently underwent a left THA. (B) The values for femoral neck anteversion (FNA = 50°), the desired final prosthetic anteversion (anteversion, A = 15°), and the correction made in the prosthetic neck (∆ = −35°) are shown. FA = foot axis (25°). A postoperative (C) AP view of the pelvis. (D) AP and (E) mediolateral views of the hip obtained at the 9-year followup show satisfactory leg length equalization and femoral offset restoration.
We described patient demographics using means and standard deviations or medians and ranges for continuous variables (age, weight, height, body mass index [BMI], Merle D’Aubigné-Postel score, Harris hip score, HOOS, postoperative leg lengths, polyethylene wear) and counts (percent) for categorical variables (gender, side, indication for THA, Charnley’s patient category, activity score of Devane et al., BMI category; presence of thigh pain, radiolucencies, or osteolysis). We determined descriptive statistics for the postoperative HOOS and UCLA scores and the radiographic outcomes using means and standard deviations to describe stem stability and osteolysis. We performed a 15-year survival analysis using the Kaplan-Meier technique [31] (with 95% confidence intervals) for all patients considering revision for any reason or radiographic loosening as the end point and stem revision only as the end point. Analysis was performed using SPSS software (Version 12; SPSS Inc, Chicago, IL). All calculations assumed two-tailed tests.
Results
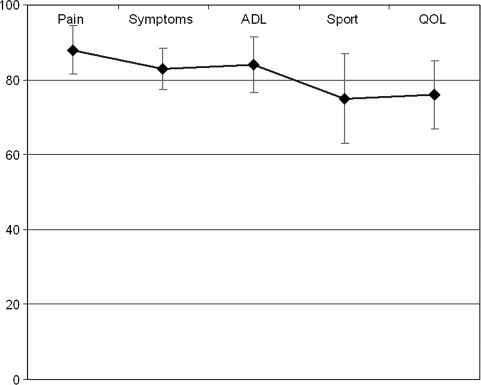
The Merle D’Aubigné-Postel and Harris hip scores improved from preoperatively to final followup (Table 2). No patient described thigh pain on questioning; 172 patients (74%) had no pain, 187 (81%) had full activity recovery, and 206 (89%) had full ROM. Sixty-eight percent of the patients had a HOOS score greater than 80 points for all five categories (Fig. 3). At the most recent followup, the mean UCLA score improved (p = 0.007) from 5.2 ± 1.6 points to 7.2 ± 2 points and 198 (85%) patients had a score greater than 6 (indicating regular involvement in moderate physical activities).
Table 2.
Comparison of preoperative and postoperative Harris hip and Merle D’Aubigné-Postel scores
| Mean | Preoperative | Postoperative | p Value |
|---|---|---|---|
| Harris hip score | |||
| Total | 54.2 (26–87) | 97 (50–100) | < 0.001 |
| Pain | 18.2 (10–44) | 42.6 (20–44) | 0.001 |
| Walking | 9.2 (1–14) | 31.7 (9–33) | 0.01 |
| Activity | 7.1 (0–12) | 13.5 (6–14) | 0.009 |
| Deformity | 4.3 (0–4) | 4 (3–4) | 0.08 |
| Range of motion | 2.8 (0–5) | 4.8 (2–5) | 0.07 |
| Merle D’Aubigné-Postel score | |||
| Total | 7.6 (0–13) | 16.3 (12–18) | < 0.001 |
| Pain | 1.6 (0–3) | 5.1 (3–6) | 0.03 |
| Walking | 2.4 (0–6) | 5.2 (4–6) | 0.01 |
| Mobility | 3.6 (0–5) | 5.9 (3–6) | 0.02 |
Fig. 3.
Distribution of the postoperative hip disability and Osteoarthritis Outcome scores are shown. ADL = activities of daily living; QOL = quality of life.
The postoperative leg length discrepancy averaged 2.3 mm (range, 0-13 mm), 73% of which were lengthened by the mean value of 1.8 mm, whereas 94% of patients had less than 5 mm of discrepancy. No patient had subsidence or varus malalignment. We found radiographic abnormalities around the femur in 13 patients (5.6%): four cortical hypertrophies (three in Gruen Zone 4, one in Zone 2, one in Zone 3), five patients with femoral osteolysis (1.6%; three in Gruen Zone 1, two in Zones 1 and 8), three stem-cortical contacts (one in Gruen Zone 13, two in Zone 4) without thigh pain, and one cortical pedestal without pain. Study of bone remodeling, as described by Engh and Bobyn [21], showed no stress shielding. Additionally, we observed radiographic anomalies in the acetabulum in four patients (1.7%): one with migration and three with complete radiolucent lines. The mean annual wear was 0.09 ± 0.05 mm/year (range, 0.003–0.29 mm/year).
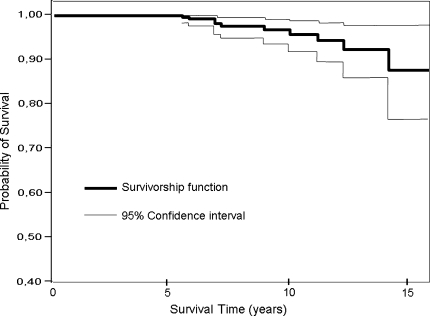
Taking revision for any reason as an end point, the survivorship was 96.7% (range, 93.7%–100%) at 10 years and 87% (range, 77%–97%) at 15 years. Considering stem revision for any reason or stem revision for aseptic loosening as end points, the survivorship was, respectively, 92.6% (range, 89.6%–97.2%) and 97.6% (range, 96%–100%) at 15 years (Fig. 4). Eleven hips (4.7%) underwent revision of the implants. Five were isolated cup revisions, including four for loosening and one for isolated polyethylene wear. Two were isolated stem revisions for loosening. The four remaining hips were revised for deep infections with a two-stage procedure with removal of all components and insertion of a cement spacer. All the infections healed and the Harris hip score averaged 79 points (range, 62–92 points).
Fig. 4.
Kaplan-Meier survivorship analysis curves with revision for any reason as the end point are shown. The 15-year survivorship rate was 87% (95% confidence interval, 77%–97%).
There were no intraoperative femoral fractures. Six patients (1.9%) experienced dislocation, including one having revision surgery. Twelve hips (5.2%) had reoperations without revision of the implants: four for infections requiring surgical washout; three for symptomatic heterotopic ossification; one for a diaphyseal femoral fracture (a 41-year-old man who did not have any intraoperative crack with a BMI of 30 kg/m2 who fell trying to walk without crutches on the third postoperative day) for which we performed plate fixation; one for polyethylene liner-cup dislocation for which the liner was replaced in the retained cup; one for painful trochanteric wire with subsequent wire removal; one for greater trochanteric fracture nonunion (the fracture having occurred at the time of the index procedure fixed with cerclage wires) for which refixation was done; and one for the hip dislocation previously mentioned.
Discussion
THA is challenging in young and active patients [13]. This population has an increased life expectancy and an increased functional demand requiring, after THA, full ROM, quick and complete return to physical activity, long-term bone-implant fixation, and limited polyethylene wear and osteolysis [34, 41]. In previous anatomic studies, it was shown the upper femoral anatomy may be distorted, particularly in young patients with frequent secondary forms of osteoarthritis [4, 29, 50]; consequently optimal fit-and-fill of the metaphysis and extramedullary adaptation may be difficult to achieve in every case. A mean survival rate of 100% at 10 years was reported for a series of patients younger than 65 years without thigh pain, migration, or reoperation [56]. For these reasons, we presumed custom cementless stems would provide high function and high survival in this population. We asked whether a custom cementless stem would restore hip function, remain stable with a low rate of osteolysis, and provide high 15-year Kaplan-Meier survivorship.
Some limitations should be mentioned. First, we made no attempt to correlate polyethylene wear and postoperative position of the femur in the frontal and horizontal planes. Although this would require radiograph and CT scan evaluation, it is difficult to clearly evaluate the role in wear reduction of the custom neck, theoretically also designed for optimizing the load on the bearing surface. Second is the absence of a control group. Third, because we aim to have an individual offset correction or reproduction, it was not possible to separate the patient population in subgroups regarding the postoperative femoral offset value and then to correlate postoperative offset with clinical function. However, a postoperative CT scan study to confirm whether we achieved the preoperative desired value is ongoing in a limited number of patients. Fourth, we had only 162 patients (69.5%) with followups longer than 10 years and 28 (12%) with followups longer than 15 years. Finally, the extra cost of the custom THA is approximately 40% greater than a THA using a conventional cementless stem. However, there are some cost savings because there is a reduced need for keeping stock room shelves of various-sized prostheses, their associated hire/purchase costs, and specific equipment for implantation of each stem.
Function was improved with 80.8% of patients recovering full activity at last followup, 88.8% having full ROM, and 85% involved in regular moderate physical activities; these figures compare with those from long-term studies using cementless conventional stems in this population (Table 3) [1, 16, 41, 52, 53]. Additionally, 68% of the patients had a HOOS score greater than 80 points for all five categories and 85% of patients had postoperative regular involvement in moderate physical activities for the return to previous physical activities, a new demand in this type of population [18, 38, 43]. No patient reported thigh pain when asked, whereas numerous studies of conventional cementless stems showed some rates of thigh pain as much as 27% [8, 25, 35, 44]. This can be related to the design with a fit-and-fill with cementless custom stems. Bargar [5] reported a higher Harris hip score (less pain) compared with a prior series of conventional stems, and Stulberg et al. [54] found less residual and recurrent thigh pain than with conventionally ready-made components, whereas Reize and Wülker [49] used a square cross-section custom titanium-alloy stem but described a 24% rate of leg length discrepancy related to the impossibility to achieve correct implantation depth. We speculate the absence of thigh pain in our patients may be the result of the tapered design of the custom stem with individualized metaphyseal fit-and-fill, whereas restoration of hip function may be related to the three-dimensional prosthetic neck design.
Table 3.
Comparison of middle to long-term followups of cementless polyethylene-bearing THAs
| Study | Year | Number of hips | Number of patients | Mean age (years) | Mean followup (years) | Mean Harris hip score (points) | Thigh pain (%) | Aseptic femoral loosening (%) | Survivorship |
|---|---|---|---|---|---|---|---|---|---|
| Kim et al. [35] | 2003 | 118 | 80 | 46.8 (21–49) | 9.8 (8–11) | 92 | 10 | 0 | 99 at 10 years |
| Reigstad [48] | 2008 | 75 | 70 | 52 (24–68) | 16 (15–18) | 89 (54-100) | — | 1.3 | 88 at 18 years |
| Schramm et al. [52] | 2000 | 89 | 80 | 51 (20–77) | 10 | 98 | 17 | 0 | — |
| Zenz et al. [56] | 1995 | 56 | 56 | 56 | 10 | 91 | 47 | 0.7 | 97.96 at 10 years |
| Duffy et al. [20] | 2004 | 84 | 73 | 38 (16–50) | 10 | 88 (48–100) | — | 6 | 87.9 at 10 years |
| Capello et al. [11] | 2003 | 123 | 106 | 39 (18–49) | > 10 | 91.5 | 0.8 | 0.9 | 94.6 at 10 years |
| McLaughlin and Lee [42] | 2000 | 108 | 91 | 37 (20–50) | 10.2 (8-13) | 92 (62–100) | 2 | 7 | 98 at 12.5 years |
| McAuley et al. [41] | 2004 | 561 | 488 | 40 (16–50) | 6.92 (0–19) | — | — | — | 89% at 10-year 60% at 15-year |
| Current study | 2009 | 233 | 212 | 42.6 (20–50) | 10 (5–16) | 97 (50–100) | 0 | 0.8 | 96.7 at 10 years 87% at 15 years |
To decrease femoral osteolysis around THA in young patients, the use of uncemented stems has been considered an alternative to cement fixation, but aseptic femoral loosening as much as 7% at midterm followup has been reported (Table 3) [1, 11, 20, 28, 41]. Distally supported prostheses have been introduced to increase initial and long-term stability [22, 39] but may increase the risk of proximal osteopenia [46], whereas proximally fitting designs may lead to subsidence and early loosening [37, 46]. The use of a femoral component with a tapered design adapted to each proximal femoral anatomy (a custom stem) may resolve this conflicting issue, as we report, with no subsidence and limited femoral osteolysis (1.6%). However, bone ingrowth around custom stems has been controversial and may depend on the design. Kawate et al. [32] described the use of cementless custom-made stems made of Ti-6Al-4 V with the proximal one-third covered with hydroxyapatite in 55 hips of 53 patients with dysplastic hips whose average age at surgery was 60 years and with an average followup of 7 years. They described bone-ingrown fixation in all but 9% of hips with severe stress shielding related to inadequacy of the stem to the canal flare index. Conversely, Koulouvaris et al. [36] reported no cases of aseptic loosening in a series of 48 custom THAs in young adults at a mean followup of 6 years, and in the preliminary series by Wettstein et al. [55] using the same custom stem used in our patients, all 62 stems were considered stable without stress shielding at a mean followup of 94.9 months.
Although it was suggested in one finite element study [47] that excessive combined lateralization and anteversion may have an adverse effect on initial implant stability and bone-implant interface stresses, Sakalkale et al. [51] reported a certain amount of lateralization may decrease wear. In their study the mean preoperative offset of the femur was 38.8 mm. On the side with a standard femoral component (radiologic offset 31.5 mm), the linear wear rate was 0.21 mm per year, whereas on the side with a lateralized femoral component (radiologic offset 40.1 mm), the linear wear rate was 0.10 mm per year [51]. We found a mean annual wear of 0.09 ± 0.05 mm/year which compared favorably with those of conventional polyethylene metal-backed cups in young patients [25, 30, 35]. We also suspect individual three-dimensional femoral offset restoration may decrease polyethylene wear.
Few studies report long-term survivorship of cementless stems in patients younger than 50 years. Considering stem revision only, the survivorship was 93% (90%–97%) at 15 years in the current series, whereas the 15-year survivorship was 87% (77%–97%) taking revision for any reason as the end point. McAuley et al. [41] reported a survivorship of 60% at 15-years followup in a series of 488 THAs performed in patients 50 years or younger. Reigstad et al. [48] studied 75 cementless Zweymüller stems with titanium-backed threaded cups in 70 patients with a mean age of 52 years (range, 24–68 years) and the overall survival rate was 88% at 18 years followup. Aldinger et al. [1] reported a survivorship of the stem of 90% at 20 years in 154 THAs performed with an uncemented grit-blasted straight tapered titanium femoral stem combined with a threaded socket in patients younger than 55 years.
We believe the greatest advantage of using a femoral custom stem for young patients is to provide an individual three-dimensional preoperative plan to analyze and correct the parameters “outside the bone,” especially in a population with a wide range of indications and disturbed anatomy. Our data suggest custom stems based on preoperative CT scans achieved anatomic reconstruction while avoiding intraoperative complications and with limited osteolysis at an average of 10 years followup. Hip function, a key factor in this high-demand population, was restored as shown by the quality-of-life scores. Additional comparative studies with revision rate and wear analysis are necessary in this population with a long life expectancy, but the concept of three-dimensional planning used for custom stems could be applied to monoblock or modular stems for a wider range of the population requiring THAs.
Footnotes
The institution of the authors has received funding from Symbios, Yverdon, Switzerland.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aldinger PR, Thomsen M, Mau H, Ewerbeck V, Breusch SJ. Cementless Spotorno tapered titanium stems: excellent 10–15-year survival in 141 young patients. Acta Orthop Scand. 2003;74:253–258. doi: 10.1080/00016470310014157. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Sakai DN. Total joint replacement for ankylosed hips: indications, technique, and preliminary results. J Bone Joint Surg Am. 1975;57:619–625. [PubMed] [Google Scholar]
- 3.Argenson JN, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–45. doi: 10.1097/BLO.0b013e3181576052. [DOI] [PubMed] [Google Scholar]
- 4.Argenson JN, Ryembault E, Flecher X, Brassart N, Parratte S, Aubaniac JM. Three-dimensional anatomy of the hip in osteoarthritis after developmental dysplasia. J Bone Joint Surg Br. 2005;87:1192–1196. doi: 10.1302/0301-620X.87B9.15928. [DOI] [PubMed] [Google Scholar]
- 5.Bargar WL. Shape the implant to the patient: a rationale for the use of custom-fit cementless total hip implants. Clin Orthop Relat Res. 1989;249:73–78. [PubMed] [Google Scholar]
- 6.Barrack RL, Jasty M, Bragdon C, Haire T, Harris WH. Thigh pain despite bone ingrowth into uncemented femoral stems. J Bone Joint Surg Br. 1992;74:507–510. doi: 10.1302/0301-620X.74B4.1624506. [DOI] [PubMed] [Google Scholar]
- 7.Beaule PE, Dorey FJ, Hoke R, Leduff M, Amstutz HC. The value of patient activity level in the outcome of total hip arthroplasty. J Arthroplasty. 2006;21:547–552. doi: 10.1016/j.arth.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Bourne RB, Rorabeck CH, Ghazal ME, Lee MH. Pain in the thigh following total hip replacement with a porous-coated anatomic prosthesis for osteoarthrosis: a five-year follow-up study. J Bone Joint Surg Am. 1994;76:1464–1470. doi: 10.2106/00004623-199410000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Bugbee WD, Culpepper WJ, II, Engh CA, Jr, Engh CA., Sr Long-term clinical consequences of stress-shielding after total hip arthroplasty without cement. J Bone Joint Surg Am. 1997;79:1007–1012. doi: 10.2106/00004623-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Capello WN, D’Antonio JA, Feinberg JR, Manley MT. Hydroxyapatite-coated total hip femoral components in patients less than fifty years old: clinical and radiographic results after five to eight years of follow-up. J Bone Joint Surg Am. 1997;79:1023–1029. doi: 10.2106/00004623-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Capello WN, D’Antonio JA, Feinberg JR, Manley MT. Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old: a concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:885–889. doi: 10.2106/00004623-200305000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Charnley GJ. Numerical grading of clinical results. In: Charnley J, editor. Low Friction Arthroplasty of the Hip. Berlin, Germany: Springer Verlag; 1979. pp. 20–24. [Google Scholar]
- 13.Charnley J. Low Friction Arthroplasty of the Hip. Theory and Practice. New York, NY: Springer; 1979. [Google Scholar]
- 14.Collis DK. Long-term (twelve to eighteen-year) follow-up of cemented total hip replacements in patients who were less than fifty years old: a follow-up note. J Bone Joint Surg Am. 1991;73:593–597. [PubMed] [Google Scholar]
- 15.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 16.D’Antonio JA, Capello WN, Manley MT, Geesink R. Hydroxyapatite femoral stems for total hip arthroplasty: 10- to 13-year followup. Clin Orthop Relat Res. 2001;393:101–111. doi: 10.1097/00003086-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 17.D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 18.Davis AM, Perruccio AV, Canizares M, Tennant A, Hawker GA , Conaghan PG , Roos EM , Jordan JM, Maillefert JF, Dougados M , Lohmander LS. The development of a short measure of physical function for hip OA HOOS-Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16:551–559. doi: 10.1016/j.joca.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 19.Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis: factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–266. doi: 10.1016/S0883-5403(97)90021-8. [DOI] [PubMed] [Google Scholar]
- 20.Duffy GP, Prpa B, Rowland CM, Berry DJ. Primary uncemented Harris-Galante acetabular components in patients 50 years old or younger: results at 10 to 12 years. Clin Orthop Relat Res. 2004;427:157–161. doi: 10.1097/01.blo.0000142286.73328.28. [DOI] [PubMed] [Google Scholar]
- 21.Engh CA, Bobyn JD. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res. 1988;231:7–28. [PubMed] [Google Scholar]
- 22.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 23.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register: 4, 661 primary replacements followed for 0–22 years. Acta Orthop. 2005;76:28–41. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 24.Flecher X, Argenson JN, Parratte S, Ryembault E, Aubaniac JM. [Custom cementless stem for osteoarthritis following developmental hip dysplasia] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:332–342. doi: 10.1016/s0035-1040(06)75763-4. [DOI] [PubMed] [Google Scholar]
- 25.Giannikas KA, Din R, Sadiq S, Dunningham TH. Medium-term results of the ABG total hip arthroplasty in young patients. J Arthroplasty. 2002;17:184–188. doi: 10.1054/arth.2002.29394. [DOI] [PubMed] [Google Scholar]
- 26.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 27.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 28.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73, 000 arthroplasties. Acta Orthop Scand. 2000;71:337–353. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 29.Husmann O, Rubin PJ, Leyvraz PF, Roguin B, Argenson JN. Three-dimensional morphology of the proximal femur. J Arthroplasty. 1997;12:444–450. doi: 10.1016/S0883-5403(97)90201-1. [DOI] [PubMed] [Google Scholar]
- 30.Jialiang T, Zhongyou M, Fuxing P, Zongke Z, Bin S, Jing Y. Primary total hip arthroplasty with Duraloc cup in patients younger than 50 years: a 5- to 7-year follow-up study. J Arthroplasty. 2009 Feb 3. [Epub ahead of print] [DOI] [PubMed]
- 31.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 32.Kawate K, Ohneda Y, Ohmura T, Yajima H, Sugimoto K, Takakura Y. Computed tomography-based custom-made stem for dysplastic hips in Japanese patients. J Arthroplasty. 2009;24:65–70. doi: 10.1016/j.arth.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 33.Keener JD, Callaghan JJ, Goetz DD, Pederson DR, Sullivan PM, Johnston RC. Twenty-five-year results after Charnley total hip arthroplasty in patients less than fifty years old: a concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:1066–1072. doi: 10.2106/00004623-200306000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Kim SY, Kyung HS, Ihn JC, Cho MR, Koo KH, Kim CY. Cementless Metasul metal-on-metal total hip arthroplasty in patients less than fifty years old. J Bone Joint Surg Am. 2004;86:2475–2481. doi: 10.1302/0301-620X.86B7.15255. [DOI] [PubMed] [Google Scholar]
- 35.Kim YH, Oh SH, Kim JS. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am. 2003;85:109–114. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 36.Koulouvaris P, Stafylas K, Sculco T, Xenakis T. Custom-design implants for severe distorted proximal anatomy of the femur in young adults followed for 4–8 years. Acta Orthop. 2008;79:203–210. doi: 10.1080/17453670710014987. [DOI] [PubMed] [Google Scholar]
- 37.LaPorte DM, Mont MA, Hungerford DS. Proximally porous-coated ingrowth prostheses: limits of use. Orthopedics. 1999;22:1154–1160. doi: 10.3928/0147-7447-19991201-09. [DOI] [PubMed] [Google Scholar]
- 38.Lavigne M, Masse V, Girard J, Roy AG, Vendittoli PA. [Return to sport after hip resurfacing or total hip arthroplasty: a randomized study] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:361–367. doi: 10.1016/j.rco.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 39.Mahomed N, Schatzker J, Hearn T. Biomechanical analysis of a distally interlocked press-fit femoral total hip prosthesis. J Arthroplasty. 1993;8:129–132. doi: 10.1016/S0883-5403(06)80051-3. [DOI] [PubMed] [Google Scholar]
- 40.Massin P, Geais L, Astoin E, Simondi M, Lavaste F. The anatomic basis for the concept of lateralized femoral stems: a frontal plane radiographic study of the proximal femur. J Arthroplasty. 2000;15:93–101. doi: 10.1016/S0883-5403(00)91337-8. [DOI] [PubMed] [Google Scholar]
- 41.McAuley JP, Szuszczewicz ES, Young A, Engh CA., Sr Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. doi: 10.1097/00003086-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 42.McLaughlin JR, Lee KR. Total hip arthroplasty in young patients: 8- to 13-year results using an uncemented stem. Clin Orthop Relat Res. 2000;373:153–163. doi: 10.1097/00003086-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 43.Naal FD, Schmied M, Munzinger U, Leunig M, Hersche O. Outcome of hip resurfacing arthroplasty in patients with developmental hip dysplasia. Clin Orthop Relat Res. 2009;467:1516–1521. doi: 10.1007/s11999-008-0456-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nercessian OA, Wu WH, Sarkissian H. Clinical and radiographic results of cementless AML total hip arthroplasty in young patients. J Arthroplasty. 2001;16:312–316. doi: 10.1054/arth.2001.21503. [DOI] [PubMed] [Google Scholar]
- 45.Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS): validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nourbash PS, Paprosky WG. Cementless femoral designing concerns: rationale for extensive porous coating. Clin Orthop Relat Res. 1998;355:189–199. doi: 10.1097/00003086-199810000-00020. [DOI] [PubMed] [Google Scholar]
- 47.Ramaniraka NA, Rakotomanana LR, Rubin PJ, Leyvraz P. [Noncemented total hip arthroplasty: influence of extramedullary parameters on initial implant stability and on bone-implant interface stresses] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2000;86:590–597. [PubMed] [Google Scholar]
- 48.Reigstad O, Siewers P, Røkkum M, Espehaug B. Excellent long-term survival of an uncemented press-fit stem and screw cup in young patients: follow-up of 75 hips for 15–18 years. Acta Orthop. 2008;79:194–202. doi: 10.1080/17453670710014978. [DOI] [PubMed] [Google Scholar]
- 49.Reize PK, Wülker N. The Adaptiva custom-made stem: our reasons for not using it anymore. Int Orthop. 2007;31:217–222. doi: 10.1007/s00264-006-0160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rubin PJ, Leyvraz PF, Aubaniac JM, Argenson JN, Esteve P, Roguin B. The morphology of the proximal femur: a three-dimensional radiographic analysis. J Bone Joint Surg Br. 1992;74:28–32. doi: 10.1302/0301-620X.74B1.1732260. [DOI] [PubMed] [Google Scholar]
- 51.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–134. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 52.Schramm M, Keck F, Hohmann D, Pitto RP. Total hip arthroplasty using an uncemented femoral component with taper design: outcome at 10-year follow-up. Arch Orthop Trauma Surg. 2000;120:407–412. doi: 10.1007/PL00013771. [DOI] [PubMed] [Google Scholar]
- 53.Sinha RK, Dungy DS, Yeon HB. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg Am. 2004;86:1254–1261. doi: 10.1302/0301-620X.86B3.14392. [DOI] [PubMed] [Google Scholar]
- 54.Stulberg SD, Stulberg BN, Wixson RL. The rationale, design characteristics, and preliminary results of a primary custom total hip prosthesis. Clin Orthop Relat Res. 1989;249:79–96. [PubMed] [Google Scholar]
- 55.Wettstein M, Mouhsine E, Argenson JN, Rubin PJ, Aubaniac JM, Leyvraz PF. Three-dimensional computed cementless custom femoral stems in young patients: midterm followup. Clin Orthop Relat Res. 2005;437:169–175. doi: 10.1097/01.blo.0000163001.14420.3a. [DOI] [PubMed] [Google Scholar]
- 56.Zenz P, Pospisil C, Fertschak W, Schwäger [10 years of cementless implantation of total hip endoprosthesis using Zweymüller’s stem] [in German] Z Orthop Ihre Grenzgeb. 1995;133:558–561. doi: 10.1055/s-2008-1039939. [DOI] [PubMed] [Google Scholar]