Abstract
Background
There is a high volume of unmet needs for knee arthroplasty in the population despite the increase in surgery rates. Given the long waiting times to have a knee arthroplasty, some governments have proposed prioritization systems for patients on waiting lists based on their level of need.
Questions/Purposes
We therefore estimated the needs and demand of knee arthroplasty in four regions of Spain during a 5-year period.
Methods
We developed a discrete event simulation model to reproduce the process of knee arthroplasty. The prioritization system was compared with the usual waiting list management strategy (by waiting time only).
Results
Under the prioritization system, patients saved an average of 4.5 months (95% confidence interval, 4.4–4.6 months) adjusted by level of need. The proportion of patients who experienced excessive waiting times was small and was associated with low levels of priority. The 5-year projection of the volume of unmet needs for knee arthroplasty remained stable; however, although the volume of need for the first knee arthroplasty decreased by 12%, the volume of need for an arthroplasty in the contralateral knee increased by 50%.
Conclusions
The data suggested the prioritization system was more beneficial than assigning surgery by waiting time only. The 5-year projection of the volume of unmet needs for knee arthroplasty remained stable, despite the increase in the need for contralateral knee arthroplasty.
Level of Evidence
Level II, economic and decision analyses. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
In recent years, rates of knee arthroplasty have increased in most Western countries because of aging, reduced surgical risk, and broader criteria for surgery [12]. In Spain, the knee arthroplasty rate increased from 22.28 surgeries per 10,000 population aged 65 years or older in 2000 to 40.47 surgeries in 2007. However, this increase is still insufficient to meet the volume of demand, and the length of time on waiting lists continues to increase gradually in the public health service [2].
Several governments (such as those from New Zealand, Canada, and Spain) have considered the need to prioritize patients on waiting lists for elective surgery, instead of allocating surgery according to the time waited [4, 13, 18, 21, 26, 27]. Prioritization is based on the fact that the need for surgery differs even in patients with appropriate surgical indication and introduces levels of need; in this context, we define “need” as the state in which a patient would benefit from the surgery but the surgery is not urgently required. In Spain, a prioritization system for patients on the waiting list for knee and hip arthroplasties has been developed and has been implemented for patients on waiting lists for knee arthroplasty [27]. The conjoint analysis technique was used and the general population, patients and relatives, clinical specialists, and related health professionals were involved in developing the prioritization system. The prioritization system showed acceptable construct validity (level of correlation with instruments that measure similar or different aspects) and reliability (interobserver reliability: degree to which the instrument is free from random error) in establishing priority for surgery [1]. This prioritization system assumes an appropriate indication including clinical (pain, severity of the disease, and prognosis), functional (difficulty in performing daily activities and work limitations), and social (providing or receiving caregiving) criteria to score needs for an arthroplasty. Possible scores range between 0 and 100, with higher scores representing greater need. The highest-weighted criterion is pain, followed by difficulty in performing activities of daily living. By using this prioritization system, need can be measured through the priority score.
The introduction of the prioritization system in clinical practice would modify the current management of waiting lists, which are ordered according to time waited, known as the first-in, first-out (FIFO) principle. Allocating surgery according to patients’ need for surgery could improve equity, as patients with a higher level of need would have their knees operated on in less time. However, patients entering the waiting list with a lower level of need may have excessive waiting times and this could raise concern among patients or surgeons if a delayed surgery could decrease the benefit from surgery. Thus, the benefits and disadvantages of waiting list prioritization should be analyzed by taking into account all patients who enter the waiting list (patients who had surgery, patients still waiting, patients who switched to the private sector, and patients who died while waiting) rather than only patients who had surgery, as it would overestimate the effect of the prioritization system. In addition, the population’s overall need for knee arthroplasty should be taken into account because the proportion of persons waiting for an arthroplasty among the overall population with prevalence of knee osteoarthritis who could benefit from surgery may be small [15]. Waiting lists cannot be used as an indicator of unmet needs (reflecting patients who would benefit from but who do not have surgery), as they may represent a small proportion of the overall need (people who have accessed the health services only) and might underestimate the volume of unmet needs.
Our objectives were (1) to compare two waiting list management strategies in terms of waiting time related to level of need and (2) to calculate the 5-year variation of the volume of the population with unmet needs of knee arthroplasty in Spain.
Materials and Methods
We built a simulation model to represent the entire process of knee arthroplasty from incidence of knee osteoarthritis severe enough to require arthroplasty to the surgery. A similar model was developed for cataract surgery and the methodology was described by Comas et al. [6]. The development of a model for knee arthroplasty is summarized below. The study complied with the Declaration of Helsinki and was approved by the ethics committee of Hospital del Mar-IMIM (Barcelona).
The model was based on individuals from the general population, 50 years or older, because knee arthroplasty rarely is indicated in persons younger than 50 years, and focused on demand in the public health system of Spain, which provides universal coverage. Patients have access to knee arthroplasty without copayment. Information was obtained from four regions of Spain (Andalusia, Aragon, the Canary Islands, and Catalonia), with a population of 16.6 million people (40.6% of the Spanish population).
The need for knee arthroplasty was defined as the prevalence of need for surgery according to indication criteria. The criteria for surgical indication were defined as radiographically confirmed osteoarthritis and the presence of sufficiently severe local symptoms (pain, stiffness) and functional limitations clinically evaluated by an orthopaedic surgeon, with no response to nonsurgical treatments or failure of other previous surgical interventions [23].
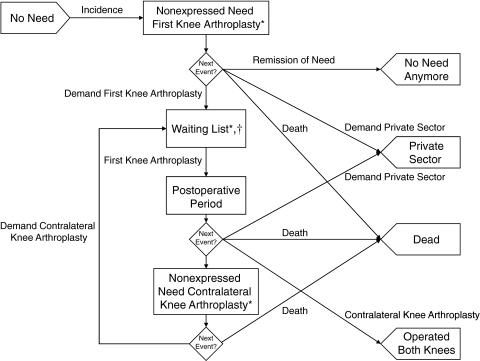
The conceptual model (Fig. 1) shows the events the target population may experience. The population was divided between patients with no need for knee arthroplasty (ie, patients with no knee osteoarthritis or patients who adequately benefit from medical treatments and/or lifestyle changes and need no surgery) and patients needing the procedure (ie, patients who would benefit from the surgery). Need for knee arthroplasty was divided between “waiting list,” indicating need for surgery has been expressed, and “nonexpressed need,” indicating, although they would benefit from knee arthroplasty, they have not demanded this surgery for whatever reason (including not accessing the healthcare system) and thus they are not included on a waiting list. Because knee osteoarthritis is an age-related disease, and assuming most patients have the bilateral form [23] and undergo arthroplasty on one knee at a time, “nonexpressed need” was divided according to the knee requiring surgery, ie, “nonexpressed need first knee arthroplasty” and “nonexpressed need for contralateral knee arthroplasty.” We included a postoperative period after arthroplasty on the first knee and before the decision to operate on the contralateral knee was made. People may experience a need for knee arthroplasty, request a first knee arthroplasty in the public sector, have this surgery, and then, given that a small proportion of patients have an arthroplasty on both knees, request a contralateral knee arthroplasty or not. Finally, an event called “remission of need” was added to represent the possible competing risks that may contraindicate a knee arthroplasty with time.
Fig. 1.
A flowchart illustrates the conceptual model.* = prevalence of need was divided among these three groups. † = patients on the waiting list had a priority score as an additional attribute.
Because 10.3% of the inhabitants of Spain have double healthcare coverage (public and private) [8], and thus a proportion of patients have knee arthroplasty in the private sector, the activity performed in the private sector was taken into account (“private sector” in Fig. 1).
The model was implemented as a discrete-event simulation model [3, 6]. Discrete-event simulation, or queuing theory, is a technique in operations research that is gaining popularity because of its flexibility in representing real systems by taking into account patient characteristics and the scarcity of resources present in health services provision. Real systems are reproduced through mathematical models in a computer, and executions can be performed to simulate a period of time to obtain results. These results are useful to analyze the evolution of the real system given several specifications and assumptions.
The time units were months and the simulation horizon was 60 months (5 years). The model took into account the possible changes during the 5-year horizon in the parameters related to supply and demand. Nevertheless, a 5-year horizon was sufficiently long to determine the evolution of the system without compromising accuracy of the estimations that remained unchanged with time.
The model’s parameters were estimated from several sources, including administrative and research databases, and included the values for 2003 to 2004 (Table 1). Information was obtained for the four regions of Spain included (Andalusia, Aragon, the Canary Islands, and Catalonia).
Table 1.
Sources of information and values of the model parameters
| Parameter | Source | Value | Note |
|---|---|---|---|
| Related to need for surgery | |||
| Overall population | Census data* | 16,599,360 | |
| Overall population 50 years or older | Census data* | 5,214,119 | |
| Overall volume of need | Vizcaya study [23] | 576,534 | |
| Nonexpressed need first knee surgery backlog | Vizcaya study [23] | 490,054 | |
| Nonexpressed need contralateral knee surgery backlog | Vizcaya study [23] | 86,480 | |
| Incident cases per month | Vizcaya study [23] | 1,577 | |
| Related to surgery | |||
| Number of surgeries per month | Hospital discharge minimum data set† | s(t) = 855 + 105 ln(36 + t) | ‡ |
| Probability of contralateral knee surgery | Hospital discharge minimum data set† | p(t) = 0.1047 + 0.0315 ln(16 + t) | § |
| Postoperative time distribution | Opportunistic | Normal distribution Mean, 6 months (SD, 0.2 months) | |
| Number of cases performed in the private sector per month | Hospital discharge minimum data set† | 225 | |
| Related to the waiting list | |||
| Waiting list backlog (December 2004) | Waiting lists register† | 15,005 | |
| Proportion of patients waiting for contralateral knee surgery | Pilot test [1, 9] | 15% | |
| Number of bilateral cases entering the waiting list per month | Waiting lists register† | d(t) = s(t − 1) + 256.14 | || |
| Proportion of patients who switch to the private sector | Pilot test [1, 9] | 14% | |
| Priority score distribution | Pilot test [1, 9] | Mean, 47.6 points (SD, 21.8 points) | |
| Increase in priority score (points per month) | Pilot test [1, 9], field work | 0.67 | |
| Time between revisions of priority score (months) | Pilot test [1, 9], field work | 1 | |
* Data obtained from the National Statistics Institute (INE); †data obtained from the Health Services of each region; ‡from 1,231.27 at the beginning of the simulation to 1,334.26 at the end of the simulation; §from 19.2% at the beginning of the simulation to 24.1% at the end of the simulation; ||from 1,484.45 at the beginning of the simulation to 1,589.30 at the end of the simulation; pilot test = pilot test of the introduction of the prioritization system in clinical practice.
All calculations were performed by stratifying by age (yearly) and gender. Census data regarding the number of inhabitants of the regions studied were obtained from the National Statistics Institute (INE). Information from a population-based study on the prevalence of knee osteoarthritis in the Basque Country (Vizcaya study) was used [23], and prevalence was calculated, dividing it by prevalence of need of first or contralateral knee surgery. Prevalence estimations were projected to the census population of the regions included in the study. By projecting, the estimated amount of people with the need for a knee arthroplasty was obtained. The number of patients waiting for a knee arthroplasty in the public health system was obtained from the waiting list registers. The estimation of prevalence of nonexpressed need was calculated as the difference between the overall volume of need and the number of patients included on the waiting list.
In the absence of incidence data, prevalence also was used to estimate incidence [22]. Prevalence and incidence were projected into the population, by age (yearly) and gender. To simulate deaths of the subjects included in the model, the lifetime distribution (the probability distribution of the time until death conditioned on current age), was obtained through Gompertz models for men and women [25]. The lifetime distribution was used to schedule the time a subject within the model will die. A Gompertz model was fitted to estimate the instantaneous risk of death, and through survival analysis theory, the Gompertz distribution, which is a mathematical model used to describe the probability of dying during a period of time, was derived. The estimated overall prevalence for individuals 50 years or older was 11.3%, being higher for women between 70 and 79 years old. The estimated number of surgeries corresponded to a knee arthroplasty rate of 305.3 surgeries per 100,000 inhabitants 50 years or older.
To calculate the number of knee arthroplasties per month and the probability of contralateral knee arthroplasty, the Hospital Discharge Minimum Data Set of the Spanish health system was used. The procedures of knee arthroplasty (according to the ICD-9-CM classification) from 1999 to 2003 were included. The database structure allowed the public and private sectors to be differentiated and bilateral surgeries to be identified. Linear models were used to estimate future numbers of surgeries and the probability of contralateral knee arthroplasty from December 2003 onward [14]. Based on expert opinion, a normal distribution with a mean of 6 months and a SD of 0.2 months was chosen to simulate the postoperative time distribution, ie, the time after the first knee surgery before which the decision on operating on the contralateral knee cannot be made.
The initial number of patients on the waiting list was obtained from the waiting list registers of each region. These were divided into first or contralateral knees by applying the proportion of patients waiting for contralateral knee surgery obtained from a pilot study of the waiting lists of eight hospitals in the regions studied [1, 9]. The number of entries on the waiting list also was obtained from the waiting list registers of each region and it was modeled to increase at the same speed as the number of surgeries. The proportion of patients who switch from the waiting list to the private sector was obtained by analyzing the reasons to leave the waiting list of patients participating in the pilot test [1, 9].
To estimate the priority score distribution of patients on waiting lists, the sample from the pilot test was used [1, 9]. A subsample from this study was further analyzed to estimate the increase in priority with time (worsening of clinical and functional criteria). The relationship between time waited and the increase in priority score could not be adjusted through a regression model but was modeled as an increase of 10 points (the mean increase) divided by 15 months (the mean time between assessments) each month. Then, the priority score of patients on the waiting list was increased by 0.67 points every month to take into account possible worsening of clinical and functional criteria with time.
The results were analyzed by comparing two waiting list management alternatives: the prioritization system (operating according to the order given by the priority score) versus the FIFO discipline (operating according to time waited). Because the impact of the time waited depended on the level of need, we had to find a combined measure to make comparisons. This measure allowed waiting times to be compared between alternatives by taking into account how those times were assigned according to each patient’s priority score. Thus, waiting time was weighted by priority score for all the patients (knees) who entered the waiting list during the simulation horizon (patients operated on in the public sector, patients still waiting at the end of the simulation, patients who switched to the private sector from the public waiting list, and patients who died while waiting). The weight was calculated as the priority score of each patient divided by the sum of the priority scores of all patients entering the waiting list. Therefore, interpreting the priority score as a measure of need, the difference between the two waiting list management alternatives can be interpreted as the time, weighted by need, saved or lost with one alternative versus the other (ie, the prioritization system versus the FIFO discipline). This comparison allows the benefit associated with the prioritization system to be quantified in terms of need-adjusted lifetime, giving greater importance to the time waited by patients with greater need, although lower-weighted waiting times mean patients with higher need waited for less time.
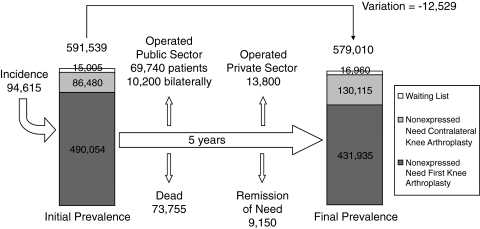
The 5-year evolution of the population with unmet needs of a knee arthroplasty in Spain was analyzed through the volume of need for a knee arthroplasty and its evolution in the simulation model. Nonexpressed need first knee arthroplasty, with a volume of 490,054 individuals, represented 82.8% of overall initial need; nonexpressed need of contralateral knee arthroplasty, with a volume of 86,480, represented 14.6%; and the waiting list represented 2.5%.
A sensitivity analysis was performed to test the impact of different estimations of the volume of need on the model results. In addition to the estimated volume of need, two scenarios were simulated: one reducing prevalence (and thus incidence) to 50% and the other reducing to 16%, which was the portion of subjects found to have an appropriate indication for surgery as reported by Quintana et al. in the Vizcaya study [23].
Owing to the complexity of the system we modeled, the diversity of the sources, and the quality of the information used to estimate the parameters, the face validation method [3] was used. This method consisted of presenting known results of the real system and the results of the model to a panel of experts that included the research team, orthopaedic surgeons, and experts in simulation. The model’s results were considered valid and credible, as the mean waiting time of patients who had surgery (12.6 months; 95% confidence interval [CI], 12.3–12.8 months) (Table 2) under the FIFO discipline was considered acceptable according to the values published by the regional health systems for the mean waiting time for knee arthroplasty in each region. The results also were validated by changing the waiting list management strategy from FIFO to the prioritization system to assess the impact of prioritization on the system’s behavior, and the resulting differences were in the expected direction, ie, patients who had surgery had lower waiting times and patients who did not have surgery had higher waiting times, as the sum of waiting times should be the same in both management strategies, given that the number of surgeries is the same.
Table 2.
Waiting times of patients on waiting list stratified by exit route and overall weighted waiting time
| Patients | FIFO | Prioritization system | Benefit | |||
|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Unweighted waiting times (months) | ||||||
| Patients who had surgery | 12.55 | 12.33, 12.76 | 6.74 | 6.58, 6.89 | 5.81 | 5.53, 6.08 |
| Patients still waiting | 6.13 | 5.91, 6.35 | 17.45 | 16.93, 17.97 | −11.32 | −11.91, −10.72 |
| Patients who switched to the private sector | 12.96 | 12.72, 13.2 | 7.25 | 6.08, 8.42 | 5.71 | 4.30, 7.11 |
| Patients who died while waiting | 6.54 | 6.32, 6.77 | 12.11 | 11.19, 13.02 | −5.56 | −6.73, −4.40 |
| Waiting time weighted by priority score (months) | 10.39 | 10.24, 10.54 | 5.90 | 5.79, 6.01 | 4.49 | 4.39, 4.59 |
Results are based on 20 replications using independent chains of random numbers; FIFO = first-in, first-out; benefit = difference in waiting time; 95% CI = 95% confidence interval.
Results
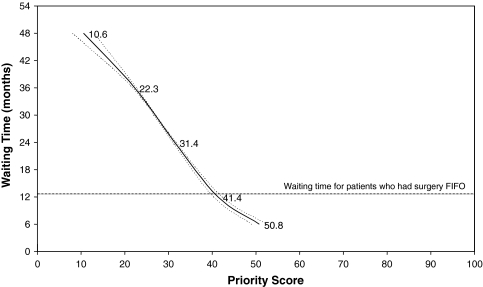
When comparing the two waiting list management strategies in terms of waiting time related to level of need, we found applying a prioritization system reduced the unweighted mean waiting time for patients undergoing knee arthroplasty in the public sector from 12.6 months (under the FIFO discipline) to 6.7 months (95% CI, 6.6–6.9 months) (Table 2). However, patients still waiting at the end of the simulation under the prioritization system had an unweighted mean waiting time of 17.5 months (95% CI, 16.9–18.0 months), which was 11.3 months longer than that for the FIFO system (95% CI, 10.7–11.9 months) (Table 2). The waiting time weighted by priority score was reduced by 4.5 months (95% CI, 4.4–4.6 months) weighted by need under the prioritization system. Patients with a priority score (at entry to the waiting list) greater than 50.8 points (95% CI, 49.0–52.6 points) underwent arthroplasty in less than 6 months (Fig. 2). Conversely, patients with fewer than 22.3 points (95% CI, 21.9–22.7 points) underwent arthroplasty after 36 months. Patients with priority scores greater than 40 points had waiting times lower than the reference waiting time for the FIFO system and patients with priority scores lower than 40 points had higher waiting times. The mean priority score of patients on the waiting list was 47.6 points (SD, 21.8 points).
Fig. 2.
A graph shows the negative relationship between the priority score and the waiting time (months) of patients having surgery under the prioritization system compared with the waiting time under the FIFO system, which has no relationship with the priority score. The 95% CIs are represented by the dotted lines.
After 5 years, overall need decreased by 12,529 patients (a 2% decrease): nonexpressed need first knee arthroplasty” decreased by 12% and “nonexpressed need contralateral knee arthroplasty increased by 50%. After 60 months, the number of patients on the waiting list was stable at approximately 17,000. Of the 73,755 patients who died during the 5-year period, 2610 (3.5%) did so while waiting for surgery. Of the 13,800 patients who underwent knee arthroplasty in the private sector, 1620 (11.7%) switched from the public waiting list (Fig. 3).
Fig. 3.
A flowchart illustrates the 5-year evolution of the population with the need for knee arthroplasty. The overall volume of unmet needs remains stable although, as the need for a first knee arthroplasty decreased, that for contralateral knee arthroplasty substantially increased.
For the scenario using ½ the prevalence of need, the overall volume decreased by 5.6% (286,370 subjects after 5 years), nonexpressed need first knee arthroplasty decreased by 27%, and nonexpressed need for contralateral knee arthroplasty doubled its volume. For the scenario considering patients with appropriate indication only, the overall volume increased by 50% (from 107,250 to 156,550 subjects after 5 years), nonexpressed need first knee arthroplasty decreased by 8%, and nonexpressed need for contralateral knee arthroplasty increased almost fivefold.
Discussion
There is a high volume of unmet needs for knee arthroplasty in the population despite the increase in surgery rates. Given the long waiting times to undergo a knee arthroplasty, some governments have proposed prioritization systems for patients on waiting lists based on their level of need. We used a simulation model to assess the benefit of introducing a prioritization system, based on need for knee arthroplasty, to knee arthroplasty waiting lists and to estimate the future requirement of knee arthroplasty in four Spanish regions with more than 16 million inhabitants.
We have several notes of caution. First, the results of a discrete-event simulation model are only estimations that depend on the input values and thus on their quality. The principle of “garbage in-garbage out” applies. Moreover, the apparent clarity and transparency of any simulation model may lead readers to overestimate their credibility as models are always simplifications of reality. Second, our definition of need was relatively wide, which could have led to an overestimation of the volume of need for knee arthroplasty. However, given the wide variability in the priority score at entry on the waiting list and the ranges covered by the priority score (from mild to severe pain, or from some difficulties to inability to perform most daily activities, for example), we can conclude a knee arthroplasty is indicated in patients with fairly different levels of need. In fact, only 16% of the cases labeled as prevalent of need for knee arthroplasty according to our indication criteria were found to have an appropriate indication for surgery in the Vizcaya study [23]. When testing this scenario under a sensitivity analysis, overall need increased substantially, owing to the increase in need for contralateral surgery only. When testing a scenario with ½ the original volume of need, the same pattern of a substantial, although lower, increase in need for contralateral surgery was observed, but need for first knee surgery decreased by 27%, resulting in a slight decrease of overall need. Third, our simulation of a pure FIFO system may not match the real practice of surgeons facing patients with severe pain, as they may jump the waiting list. If these patients and practice were frequent, this would overestimate the benefit of the prioritization system. Finally, the relationships among some parameters of the model, such as the relationship between surgery and demand, were difficult to assess, and mathematical functions were defined to approximate their behavior. These relationships were not based on real data because the information needed to estimate them comes from sources with different levels of robustness and data must be compared with time. They were considered reasonable, and thus valid, by the panel of experts.
The model suggests the prioritization system was more beneficial than allocating arthroplasties by waiting time only. Given the same number of surgeries, the prioritization system distributes waiting time according to priority; thus, patients with greater need wait less time. Although the prioritization system was more beneficial at a population level, patients with lower priority scores had excessive waiting times, even though the priority score was increased with time. The mean priority score of patients on entry to the waiting list was 47.6 points (SD, 21.8 points). According to our results, all patients with a score higher than the mean priority score would have a knee arthroplasty earlier with the prioritization system than with the FIFO system. However, patients with, for example, fewer than 22.3 points (16% of patients with mild pain and some or great difficulty in performing daily activities) would wait for 36 months or longer. Unless supply is increased, an excess waiting time of 3 years would exclude these patients from the system. Moreover, in our model, if the priority score had not been increased to take worsening of clinical criteria with time into account, these patients would never have undergone a knee arthroplasty. The studies that analyzed prioritization of waiting lists for other procedures concluded allocating surgery according to a priority score was more beneficial than doing so by waiting time only [10, 11, 24, 28].
Knee arthroplasty is an elective, highly cost-effective procedure [16, 17]. However, even though the rates of knee arthroplasty in Spain are similar to the US rates [12], a substantial volume of need for knee arthroplasty remains in the population, in addition to waiting lists. Waiting lists cannot be used as an indicator of unmet needs, as they represent a small proportion of the overall need, ie, waiting lists include only persons who have accessed the health services and thus substantially underestimate the volume of unmet need. Identifying the level of need for the population meeting the indication criteria is important, as there is evidence of absence of prioritization of persons with unmet need. Waiting lists arise in countries with national health services, such as Spain and the UK. However, beyond waiting lists, there is an important volume of nonexpressed need that would benefit from explicit prioritization at the indication stage. Therefore, the problem does not exclusively concern waiting list management, but rather how to approach the unmet need in the population. Given that a knee arthroplasty is indicated at a wide range of priority levels, the level of need in the population with unmet need also could be expected to vary widely. Nevertheless, this wide range of levels of need also may be caused by broadening of the indication criteria, given the benefit of a knee arthroplasty. The difficulty of defining the concept of need in elective orthopaedic surgeries is reflected in the wide variations found in its use [19, 30] and the high level of inappropriate indication [23].
Regardless of the waiting list discipline, the volume of unmet need for a knee arthroplasty was stable at approximately 585,000 inhabitants (11.2% of the population 50 years or older) during the 5-year horizon. Nevertheless, although unmet need for a first knee arthroplasty decreased, that for contralateral knee arthroplasty substantially increased. Need for a contralateral knee arthroplasty is obviously a consequence of previously performed first knee arthroplasties. Thus, these patients are persons whose disease has been partially treated and who could benefit from a contralateral knee arthroplasty; moreover, these individuals are more conscious of their need and have greater knowledge of how to access treatment. However, given that a small proportion of patients have an arthroplasty in both knees, assuming all patients need an arthroplasty in both knees could overestimate the volume of need for contralateral knee arthroplasty. Study of needs and demand for health services is important as substantial unmet needs are observed. The gap between needs and services provision may be too great to be resolved, but models assessing the impact of changes on the amount of resources used or the impact of health policies on the management of need and demand are useful in decision making [29]. Several studies have taken advantage of simulation to assess needs for health services [5, 7, 20]. Jüni et al. [15] used a cross-sectional population-based sample to estimate the requirement for knee arthroplasty but made no forward projection of the population need for knee arthroplasty.
Our study represents the flow of patients between need, waiting lists, and knee arthroplasty, considering elective surgery is a scarce resource for which patients compete and prioritization systems may be used to assign surgery according to need. Moreover, discrete-event simulation could be used as a tool for shared decision making, as patients could be presented with the expected waiting time according to their priority score and could decide whether they would be willing to accept it. Introducing a prioritization system for waiting lists was more beneficial than allocating arthroplasty by waiting time only (FIFO) and the proportion of patients who experienced with excessive waiting times was small and had low priority. In view of current data regarding waiting lists, testing the prioritization system through the simulation model allows definition of a (justifiable) level of need above which the public health system could appropriately meet demand. This alternative would make waiting list management transparent, would substantially reduce the waiting time for the most disabled patients, and could be a less costly and more sustainable option than shock plans. Our results suggest, under the prioritization system, patients with a priority score of 41.4 points or greater (57.1% of patients) would have a waiting time of 12 months or less whereas patients with a priority score of 31.4 points or lower (29.2% of patients) would wait 24 months or more.
Acknowledgments
IRYSS Modeling Group: Lorena Hoffmeister, Francesc Cots (Hospital del Mar-IMIM); Javier Mar (Hospital Alto Deba, Mondragón); Mireia Espallargues, Alejandro Allepuz (Catalan Agency for Technology Assessment and Research); Enrique Bernal (Instituto Aragonés de Ciencias de la Salud, Aragón); Alberto Jiménez-Puente (Hospital Costa del Sol, Andalusia); Virginia Yanes, Santiago Gutiérrez-Moreno (Servicio Canario de la Salud, Canary Islands). We thank Drs. Josep Martí-Valls and Luis Azorín, from Hospital Vall d’Hebron, Barcelona, and Dr. Lluís Puig, from Hospital del Mar, Barcelona, for their advice on the conceptual model.
Footnotes
This work was supported by grants from the Catalan Agency for Health Technology Assessment and Research (CAHTA) (089/07/2000) and the Fondo de Investigación Sanitaria (FIS) (PI020365, RedIRYSS [G03/202, PI052403], and RCESP [C03/09, PI052302]).
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Hospital del Mar-IMIM (Barcelona).
References
- 1.Allepuz A, Espallargues M, Moharra M, Comas M, Pons JM; Research Group on Support Instruments–IRYSS Network. Prioritisation of patients on waiting lists for hip and knee arthroplasties and cataract surgery: instruments validation. BMC Health Serv Res. 2008;8:76. [DOI] [PMC free article] [PubMed]
- 2.Allepuz A, Serra-Sutton V, Espallargues M, Salvador X, Pons JMV. Artroplastias de cadera y rodilla en Cataluña desde 1994 a 2005. Gac Sanit. 2008;22:534–540. doi: 10.1016/S0213-9111(08)75351-2. [DOI] [PubMed] [Google Scholar]
- 3.Banks J, editor. Handbook of Simulation: Principles, Methodology, Advances, Applications, and Practice. New York, NY: John Wiley & Sons, Inc.; 1998. [Google Scholar]
- 4.Waiting List Prioritisation Scoring Systems: A Discussion Paper. London, UK: British Medical Association; 1999. [Google Scholar]
- 5.Burkell J, Wright A, Hoffmaster B, Webb K. A decision-making aid for long-term care waiting list policies: modelling first-come, first-served vs. needs-based criteria. Healthc Manage Forum. 1996;9:35–39. doi: 10.1016/S0840-4704(10)60942-8. [DOI] [PubMed] [Google Scholar]
- 6.Comas M, Castells X, Hoffmeister L, Roman R, Cots F, Mar J, Gutierrez-Moreno S, Espallargues M. Discrete-event simulation applied to analysis of waiting lists: evaluation of a prioritization system for cataract surgery. Value Health. 2008;11:1203–1213. doi: 10.1111/j.1524-4733.2008.00322.x. [DOI] [PubMed] [Google Scholar]
- 7.Davies R, Roderick P. Predicting the future demand for renal replacement therapy in England using simulation modelling. Nephrol Dial Transplant. 1997;12:2512–2516. doi: 10.1093/ndt/12.12.2512. [DOI] [PubMed] [Google Scholar]
- 8.Encuesta Nacional de Salud 2001. Madrid, Spain: Ministerio de Sanidad y Consumo; 2001. [Google Scholar]
- 9.Espallargues M, Comas M, Sampietro-Colom L, Castells X. Prova pilot del sistema de priorització de pacients en llista d’espera per a cirurgia de cataracta, artroplàstia de maluc i artroplàstia de genoll (setembre 2003). Barcelona, Spain: Agència d’Avaluació de Tecnologia i Recerca Mèdiques. Servei Català de la Salut. Departament de Salut. Generalitat de Catalunya. January 2005 (IN04/2004). Available from: http://www.gencat.net/salut/depsan/units/aatrm/pdf/in0404ca.pdf. Accessed April 27, 2009.
- 10.Everett JE. A decision support simulation model for the management of an elective surgery waiting system. Health Care Manag Sci. 2002;5:89–95. doi: 10.1023/A:1014468613635. [DOI] [PubMed] [Google Scholar]
- 11.Fantini MP, Negro A, Accorsi S, Cisbani L, Taroni F, Grilli R. Development and assessment of a priority score for cataract surgery. Can J Ophthalmol. 2004;39:48–55. doi: 10.1016/s0008-4182(04)80052-8. [DOI] [PubMed] [Google Scholar]
- 12.Grupo de Variaciones en la Práctica Médica de la Red temática de Investigación en Resultados y Servicios de Salud (Grupo VPM-IRYSS) Variaciones en cirugía ortopédica y traumatología en el Sistema Nacional de Salud. Atlas Var Pract Med Sist Nac Salud. 2005;1:17–36. [Google Scholar]
- 13.Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 1: Overview. BMJ. 1997;314:131–134. doi: 10.1136/bmj.314.7074.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmeister L, Roman R, Comas M, Cots F, Bernal-Delgado E, Castells X. Time-trend and variations in the proportion of second-eye cataract surgery. BMC Health Serv Res. 2007;7:53. doi: 10.1186/1472-6963-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juni P, Dieppe P, Donovan J, Peters T, Eachus J, Pearson N, Greenwood R, Frankel S. Population requirement for primary knee replacement surgery: a cross-sectional study. Rheumatology (Oxford) 2003;42:516–521. doi: 10.1093/rheumatology/keg196. [DOI] [PubMed] [Google Scholar]
- 16.Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997;345:134–139. doi: 10.1097/00003086-199712000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–1121. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lundstrom M, Stenevi U, Thorburn W. Assessment of waiting time and priority setting by means of a national register. Int J Technol Assess Health Care. 1996;12:136–140. doi: 10.1017/S0266462300009454. [DOI] [PubMed] [Google Scholar]
- 19.Lurie JD, Weinstein JN. Shared decision-making and the orthopaedic workforce. Clin Orthop Relat Res. 2001;385:68–75. doi: 10.1097/00003086-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Minassian DC, Reidy A, Desai P, Farrow S, Vafidis G, Minassian A. The deficit in cataract surgery in England and Wales and the escalating problem of visual impairment: epidemiological modelling of the population dynamics of cataract. Br J Ophthalmol. 2000;84:4–8. doi: 10.1136/bjo.84.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinto JL, Rodríguez E, Castells X, Gracia X, Sánchez FI. El Establecimiento de Prioridades en la Cirugía Electiva. Madrid, Spain: Ministerio de Sanidad y Consumo; 2000. [Google Scholar]
- 22.Podgor MJ, Leske MC. Estimating incidence from age-specific prevalence for irreversible diseases with differential mortality. Stat Med. 1986;5:573–578. doi: 10.1002/sim.4780050604. [DOI] [PubMed] [Google Scholar]
- 23.Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168:1576–1584. doi: 10.1001/archinte.168.14.1576. [DOI] [PubMed] [Google Scholar]
- 24.Ratcliffe J, Young T, Buxton M, Eldabi T, Paul R, Burroughs A, Papatheodoridis G, Rolles K. A simulation modelling approach to evaluating alternative policies for the management of the waiting list for liver transplantation. Health Care Manag Sci. 2001;4:117–124. doi: 10.1023/A:1011405610919. [DOI] [PubMed] [Google Scholar]
- 25.Roman R, Comas M, Hoffmeister L, Castells X. Determining the lifetime density function using a continuous approach. J Epidemiol Community Health. 2007;61:923–925. doi: 10.1136/jech.2006.052639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romanchuk KG, Sanmugasunderam S, Hadorn DC, Steering Committee of the Western Canada Waiting List Project Developing cataract surgery priority criteria: results from the Western Canada Waiting List Project. Can J Ophthalmol. 2002;37:145–154. doi: 10.1016/s0008-4182(02)80056-4. [DOI] [PubMed] [Google Scholar]
- 27.Sampietro-Colom L, Espallargues M, Rodriguez E, Comas M, Alonso J, Castells X, Pinto JL. Wide social participation in prioritizing patients on waiting lists for joint replacement: a conjoint analysis. Med Decis Making. 2008;28:554–566. doi: 10.1177/0272989X08315235. [DOI] [PubMed] [Google Scholar]
- 28.Tuft S, Gallivan S. Computer modelling of a cataract waiting list. Br J Ophthalmol. 2001;85:582–585. doi: 10.1136/bjo.85.5.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vissers JM, Bij JD, Kusters RJ. Towards decision support for waiting lists: an operations management view. Health Care Manag Sci. 2001;4:133–142. doi: 10.1023/A:1011409711828. [DOI] [PubMed] [Google Scholar]
- 30.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 2006;31:2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]