Abstract
It is often difficult to predict postoperative radiographic curve magnitude and balance parameters while performing intraoperative correction during scoliosis surgery. We asked whether there was a radiographic correlation between intraoperative long-cassette scoliosis film and postoperative standing radiographs of adolescent idiopathic scoliosis with pedicle screw instrumentation. We retrospectively reviewed 44 patients with adolescent idiopathic scoliosis who underwent posterior instrumentation with pedicle screws. We made preoperative, intraoperative (after instrumentation and correction), and standing postoperative radiographic measurements (eg, curve magnitudes, coronal and sagittal balance, disc angles) and compared those for the intra- and postoperative radiographs. The intraoperative long-cassette scoliosis film correlated with the immediate postoperative standing film for all curve correction and balance parameters. The routine use of a long-cassette intraoperative scoliosis film provides the surgeon with a valuable tool to guide intraoperative decision-making and foreshadows the correction and balance obtained on the immediate postoperative film.
Level of Evidence: Level IV, retrospective study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Pedicle screw fixation has gained in popularity to surgically correct adolescent idiopathic scoliosis (AIS). Pedicle screws offer three-column fixation and reportedly provide curve correction, maintenance of correction, lower pseudarthrosis rates, fewer implant failures, and fewer postoperative bracing requirements than conventional hook and wire constructs [7, 9, 16, 22]. Additionally, the safety of pedicle screws has been well documented with several large series of patients with AIS undergoing correction with minimal neurologic or visceral complications [13, 23, 24]. Kim et al. [5] reported no neurologic or vascular complications with the placement of over 3000 thoracic pedicle screws. When pedicle screws are placed accurately, they should be completely contained within the pedicle, whereas hook insertion necessitates canal intrusion of approximately 30% [2]. Also, hooks are more prone to shift during correction maneuvers [8, 9]. Another benefit of the more rigid stabilization offered by pedicle screw fixation is the ability to use shorter constructs to achieve deformity correction, thus preserving more motion segments than other techniques and potentially decreasing postoperative back pain [3, 16, 22].
Radiographic studies are essential to evaluate deformity correction and implant placement. Computed tomography (CT) scans have superior accuracy in assessing pedicle morphology to aid in preoperative planning along with identifying malpositioned screws [2]. However, CT scans are limited by cost, radiation exposure, and lack of intraoperative availability [4, 19]. Another concern for the use of CT is the supine position masks the true extent of the deformity, because the Cobb angle spontaneously corrects approximately 30% when performed in the supine position [10, 25]. Although the intraoperative film is taken prone and all postoperative images are standing, passive correction on the nonweightbearing film is minimized by rigid fixation. For these reasons, plain radiographs are used more routinely for serial postoperative examinations to assess correction parameters and to assess the accuracy of pedicle screw placement. Obtaining postoperative CT scans is not routine at most centers, because the concern for radiation to the patient as well as the cost are taken into consideration. However, the implications of a malpositioned screw or incomplete/improper correction evaluation on a postoperative radiograph can be considerable, because a surgeon may be obligated to return to the operating room to redirect an errant screw or perform additional corrective maneuvers (Fig. 1A–C).
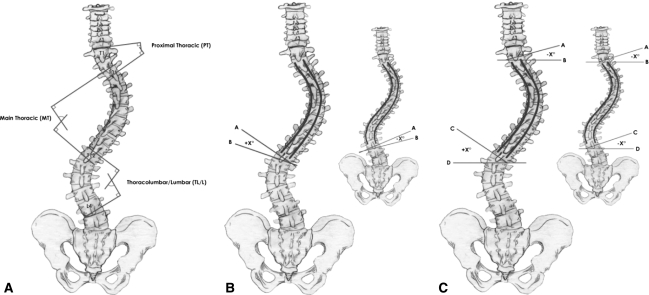
Fig. 1A–D.
Example of a case in which obtaining the intraoperative film allowed us to change the nature/extent of the correction and allowed us to properly address/correct the curve pattern. Images from left to write demonstrate preoperative (A), intraoperative after initial corrective action (B), intraoperative after final correction (C), and postoperative films (D)
Kim et al. [5], comparing CT with plain films, reported using long-cassette intraoperative radiographs to assess the accuracy of pedicle screw placement with a 95% confidence interval. However, they did not confirm whether the findings on the intraoperative radiographs reflected those on the postoperative radiographs. In virtually all orthopaedic arenas, it is imperative to be able to assess alignment intraoperatively and have it correlate to postoperative imaging. Intraoperative fluoroscopy correlates well with standing radiographs when assessing lower limb alignment [20]. However, it is unknown whether the apparent deformity correction on the intraoperative, prone radiographs correlates with the correction seen on postoperative, standing images.
Therefore, the purposes of our study were to (1) determine if radiographic parameters on long-cassette, prone intraoperative films correlate with the postoperative standing radiographs; and (2) determine if additional clinical benefit would be afforded by an intraoperative radiograph during the treatment of AIS with pedicle screw instrumentation.
Materials and Methods
We retrospectively reviewed all 44 patients with AIS who underwent posterior instrumentation with pedicle screws from two centers from August 2000 through July 2007. The average age at the time of surgery was 15.1 ± 2.21 years. We included all patients with the diagnosis of AIS that had radiographs taken at all three time points: (1) preoperative long-cassette standing radiographs; (2) intraoperative, prone full-length scoliosis films; and (3) postoperative, standing radiographs. Nine patients were excluded as a result of the inability to adequately visualize the pelvis on the intraoperative images, which was necessary to assess all coronal balance parameters. We measured radiographic measurements, including curve magnitudes, coronal and sagittal balance, shoulder and pelvic balance, and disc angles, on all three films. The intraoperative, prone scoliosis film was obtained after instrumentation and correction were completed.
All surgeries were performed by the two senior authors (LGL, RAL) using a free-hand technique and stainless steel pedicle screw instrumentation as espoused by Kim et al. [5]. Pedicle screws were placed segmentally with the major corrective maneuver being direct vertebral derotation using linked vertebral column manipulators (VCMs) (Medtronic Spinal and Biologics, Minneapolis, MN). Per routine, the VCM device was attached to the screw heads that did not allow for toggle in the mediolateral plane (ie, fixed head or uniplanar screws), and direct derotation was performed followed by placement of the correcting rod. The correcting rod was precontoured in the sagittal plane only. The rod was placed and set plug screws were captured at the three cephalad levels. The set plugs were left loose, and then the rod was rotated 180° and placed into the distal screw heads. Then in a stepwise fashion, set plugs were placed with the use of “rockers” or rod-manipulating devices in a caudad to cephalad direction. During the rod capture procedure, the assistant placed a direct, thoracic force on the rib cage while maintaining the derotation force through the VCM devices. After rod placement, set plugs were locked in place in a caudal to cephalad manner using various rod reduction tools. Then, in situ coronal bending was performed simultaneously on the correcting and/or holding rods, and compression or distraction maneuvers were used at the cephalad and caudad aspects of the construct to obtain proper shoulder balance and horizontalization of the lowest instrumented level (LIV). After final correction maneuvers, an intraoperative long-cassette prone radiograph was obtained to assess our correction and balance parameters. Three patients in our study group had inadequate curve correction based on intraoperative imaging and required revision correction maneuvers and repeat intraoperative imaging. We then decorticated and placed our crosslinks in a standard fashion at the cephalad and caudad aspect of our construct.
Postoperative standing films were obtained before discharge within 4 to 7 days after surgery when the patient was able to stand for the film with minimal discomfort. All films were routinely taken with the patient approximately 72 inches from the radiographic source as is standard protocol for scoliosis imaging at both centers. This was accomplished intraoperatively by placing the cassette on a sitting stool and lowering the operating table. The portable radiographic machine was then elevated to achieve the appropriate distance from the source to the cassette. An intraoperative, long-cassette lateral film is not possible secondary to arm positioning and shoulder overlap. Intraoperative lateral images were taken on two short cassettes and were thus only used to assess implant position and not useful for assessing sagittal alignment. We then compared all radiographic parameters on intraoperative film with the postoperative, standing film.
A single, independent reviewer (MDH) not involved in any of the surgeries measured all radiographs. Initially, all preoperative films were measured and the end vertebrae were noted for all curves. The intraoperative films were then reviewed at a separate sitting without the availability of the preoperative or postoperative films to avoid any personal bias with the measurements. All curves were measured using the same end vertebra noted from the preoperative films to ensure consistency with measurement techniques. Similarly, the postoperative films were measured at a separate time, again without any of the previous images available. One center uses plain film radiography, necessitating use of a digital protractor (x-caliper; Eisenlohr Technologies, Wilton, CA) to obtain curve measurements, whereas the other center uses all digital imaging (AGFA Impax 4.5). The same digital protractor was used for all plain film measurements.
Coronal measurements included Cobb angles, lowest instrumented vertebra tilt to the horizontal (LIV-H), angulation of disc below lowest instrumented level (LIV-α), the alignment of the C7 plumb line in relation to the center sacral vertical line (C7-CSVL), apical vertebral translation (apex-CSVL), and the coronal position of the lowest instrumented level (LIV-CSVL) (Fig. 2A–C). The most widely used measurement parameter in scoliosis is the Cobb angle, which is determined by the intersection of a line drawn from the superior end plate of the cephalad end vertebra and the inferior end plate of the caudal end vertebra for each curve, which measures curvature in the coronal plane. The LIV-H measures the angle of a line along the caudal end plate of the LIV and a horizontal intersecting line assessing the tilt of the LIV. Similarly, LIV-α measures the coronal angulation of the disc below the LIV by computing the angle between tangential lines drawn from the inferior end plate of the LIV and the superior end plate of the level below. Overall coronal balance is measured by the distance between the C7 plumb line and the CSVL. The C7 plumb line is a line from the middle of the C7 body parallel to the edge of the radiograph, and the CSVL is drawn from the midbody of S1 parallel to the radiograph edge. Finally, the coronal translation of the LIV and curve apex were also measured [18].
Fig. 2A–C.
Preoperative (A), intraoperative (B), and postoperative (C) radiographs show correlation between intraoperative and postoperative films
We classified the curves using the system of Lenke et al. [15]. The system has three components: (1) a curve type (1 through 6), (2) a modifier for the lumbar spine (A, B, or C), and (3) a modifier for the thoracic spine on the sagittal radiograph (−, N, or +). The system reportedly has high reliability [15].
We determined the difference in the postoperative and intraoperative parameters for all patients (Table 1). Correlation between intraoperative and postoperative radiographic parameters was tested through computation of a Pearson’s coefficient. Frequency data were evaluated to determine percent of patients with less than 5° difference. Statistical analysis was performed using SPSS 14.0 for Windows (SPSS Inc, Chicago, IL) statistical software program.
Table 1.
Difference between intraoperative and postoperative measurements
| Lenke curve type | Proximal thoracic ΔIO/PO | Main thoracic ΔIO/PO | TL/lumbar ΔIO/PO | LIV-H ΔIO/PO | LIV-disc ΔIO/PO | C7-CSVL ΔIO/PO | Apex-CSVL ΔIO/PO | LIV-CSVL ΔIO/PO | Lumbar-CSVL ΔIO/PO |
|---|---|---|---|---|---|---|---|---|---|
| 1AN | 0 | 13 | −8 | 0 | −4 | −26 | −27 | −11 | −24 |
| 3AN | −2 | −3 | 6 | −2 | 0 | 24 | −6 | 11 | −1 |
| 6CN | −1 | −2 | −4 | −3 | 8 | −57 | −30 | 4 | −17 |
| 2AN | 3 | −2 | 4 | −6 | 3 | −31 | −35 | −12 | −18 |
| 1AN | 0 | −5 | 4 | 2 | 5 | 3 | 2 | 10 | 0 |
| 1AN | −3 | −2 | 6 | 6 | 2 | 17 | −5 | −6 | −9 |
| 1CP | 0 | 8 | 17 | −13 | −3 | −79 | −52 | −52 | −40 |
| 1CN | 3 | 1 | 1 | 2 | −4 | 15 | 7 | 15 | 0 |
| 2AN | 7 | −2 | −11 | −2 | −8 | −13 | −8 | 0 | −1 |
| 1AN | −1 | −17 | −5 | −2 | 2 | −57 | −46 | −3 | −33 |
| 3BN | 4 | −3 | −5 | 1 | −1 | 29 | 16 | 25 | 18 |
| 1AN | 0 | −5 | −4 | −3 | 2 | 24 | −9 | −10 | −29 |
| 3CN | 0 | 4 | 2 | −15 | −6 | −81 | −61 | −23 | −34 |
| 3CN | −1 | −1 | 2 | 5 | 0 | −43 | −32 | 2 | 3 |
| 1AN | −9 | −4 | −9 | 0 | −5 | −64 | −48 | 9 | −10 |
| 1CN | 1 | −4 | −12 | 27 | 15 | 26 | −29 | 17 | 8 |
| 1CN | −5 | −9 | −2 | 3 | −2 | 71 | 22 | −5 | 10 |
| 1AN | 0 | −2 | 10 | 6 | 2 | 50 | 21 | 3 | 1 |
| 4CN | 0 | 0 | −4 | −5 | 0 | 16 | 13 | −1 | 8 |
| 1AN | −3 | 0 | 1 | −4 | 0 | −46 | −25 | −8 | −21 |
| 1AN | 1 | −1 | 11 | 0 | 1 | −9 | −16 | −13 | −17 |
| 1AN | 0 | 6 | 8 | −4 | 5 | −33 | −24 | −14 | −23 |
| 1AN | −3 | −8 | −6 | 2 | 1 | −18 | 14 | 13 | 8 |
| 1AN | −6 | 0 | −4 | −2 | −2 | −11 | −18 | −14 | −11 |
| 1AN | 3 | 2 | 2 | −4 | 2 | 0 | −8 | −8 | −10 |
| 1AN | 2 | −5 | −3 | 2 | −2 | −54 | −52 | −7 | 0 |
| 1AN | 10 | 2 | 1 | −8 | 0 | 6 | 14 | 8 | 1 |
| 5CN | −8 | 0 | −11 | 3 | −7 | 27 | 8 | 9 | 24 |
| 3CN | 5 | −2 | −3 | 5 | −10 | −73 | −45 | −2 | −6 |
| 5CN | −5 | 0 | 5 | 4 | −2 | 5 | 3 | 3 | 5 |
| 3CN | −12 | 3 | 1 | −3 | −7 | 42 | 5 | −3 | −4 |
| 3CN | 1 | −12 | −12 | −6 | −2 | 11 | −2 | 2 | 10 |
| 3CN | −2 | 0 | −1 | 5 | 0 | −49 | −37 | −13 | −19 |
| 1AN | −8 | −1 | 1 | 0 | 0 | 39 | 14 | 10 | 17 |
| 1AN | −3 | −4 | 0 | 1 | 0 | 32 | 21 | 13 | 0 |
| 3CN | −4 | −2 | 6 | 3 | −1 | −5 | −10 | −16 | −10 |
| 6CN | 10 | −2 | 7 | 3 | 1 | −7 | −12 | −2 | −2 |
| 1AN | −7 | −6 | 0 | −5 | 1 | −42 | −11 | −7 | 0 |
| 2AN | −2 | 0 | 1 | 5 | 1 | 25 | 15 | 13 | 0 |
| 6CN | 2 | −6 | −7 | −2 | 4 | −13 | −13 | −3 | 8 |
| 3CN | −1 | −3 | 15 | 12 | 8 | −42 | −41 | −20 | −32 |
| 3CN | −6 | −3 | 7 | 5 | 10 | −7 | −2 | 0 | 2 |
| 1AN | −3 | −6 | 0 | 3 | 3 | −37 | −35 | −18 | −12 |
| 3CN | 1 | 0 | 4 | 0 | −2 | 19 | 11 | 15 | 10 |
Δ = change from intraoperative (IO) to postoperative (PO), + indicates higher number postoperatively and − indicates lower number postoperatively; LIV-H = lowest instrumented vertebra-horizontal; LIV = lowest instrumented vertebra; CSVL = center sacral vertical line.
Results
The curve magnitude on the intraoperative films for the proximal thoracic, main thoracic, and thoracolumbar/lumbar curves correlated (r = 0.748, 0.847, and 0.775, respectively; p < 0.005) with those on the postoperative films. The higher propensity of correlation with the main curve from intraoperative to postoperative is likely a result of the thoracic curve being instrumented in a large majority of the cases (Fig. 3A–C). The Lenke Type 1 curve pattern was the most common (n = 23 [52.3%]) followed by Lenke Type 3 curves (n = 12 [27.3%]) (Table 2). The proximal curve and TL/LC were not always instrumented depending on the particular curve pattern of each patient.
Fig. 3A–C.
Cobb angle difference between intraoperative and postoperative radiograph in proximal thoracic (A), main thoracic (B), and thoracolumbar/lumbar (C) curves
Table 2.
Measurements based on curve pattern
| Lenke curve type | Number of subjects | Proximal thoracic ΔIO/PO | Main thoracic ΔIO/PO | TL/lumbar ΔIO/PO | LIV-H ΔIO/PO | LIV-disc ΔIO/PO | C7-CSVL ΔIO/PO | Apex-CSVL ΔIO/PO | LIV-CSVL ΔIO/PO | Lumbar-CSVL ΔIO/PO |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 23 | 3.1 | 4.8 | 5 | 4.3 | 2.7 | 33 | 22.6 | 11.9 | 12.3 |
| 2 | 3 | 4 | 1.3 | 5.3 | 4.3 | 4 | 23 | 19.3 | 8.3 | 6.3 |
| 3 | 12 | 3.3 | 3 | 5.3 | 5.2 | 3.9 | 35.4 | 22.3 | 11 | 12.4 |
| 4 | 1 | 0 | 0 | 4 | 5 | 0 | 16 | 13 | 1 | 8 |
| 5 | 2 | 6.5 | 0 | 8 | 3.5 | 4.5 | 16 | 5.5 | 6 | 16.3 |
| 6 | 3 | 4.3 | 3.3 | 6 | 2.7 | 4.3 | 25.7 | 18.3 | 3 | 9 |
Δ = change from intraoperative (IO) to postoperative (PO), LIV-H = lowest instrumented vertebra-horizontal; LIV = lowest instrumented vertebra; CSVL = center sacral vertical line.
The caudal balance parameters (LIV-H and LIV-α) correlated with the intraoperative to postoperative radiographs (r = 0.497, p = 0.001 and r = 0.43, p = 0.004, respectively). The LIV to CSVL as well as the apex of the lumbar curve to the CSVL correlated (r = 0.57, p < 0.0005 and r = 0.50, p = 0.001, p = 0.001, respectively). We observed no correlation between C7 to CSVL distance (r = −0.012, p = 0.937) or from apex to CSVL distance (r = 0.132, p = 0.399) when comparing intraoperative with postoperative radiographs.
Seventy-seven percent of the main thoracic curve showed a difference (p < 0.005) of 5° or less from the intraoperative to the postoperative standing film (Fig. 4A–C). We observed a similar pattern with the proximal curve with 76.7% of curves differing by 5º or less from intraoperative to postoperative films. Additionally, 59.1% of thoracic and lumbar curves were within 5° on intraoperative and postoperative measurements. For LIV-α, we observed a correlation (p = 0.001) between intraoperative and postoperative radiographs of less than 5° in 84.1% of cases. The intraoperative LIV to CSVL distance was within 20 mm of the postoperative film 93.2% of the time, and the intraoperative lumbar curve to the CSVL was within 20 mm of the postoperative measurement 79.5% of the time. With C7 to CSVL and apex to CSVL, only 38.6% and 56.8% of measurements were within 20 mm of each other, respectively.
Fig. 4A–C.
Sample measurement parameters illustrated to include Cobb angles (A), lowest instrumented vertebra-angle (LIV-α) (B), and lowest instrumented vertebra-horizontal (LIV-H) (C). Images provided by Medtronic Sofamor Danek USA, Inc.
Discussion
Given surgeons make decisions based on the apparent deformity correction on intraoperative prone radiographs, it is important to know whether the measurements will reflect the correction on postoperative, standing images. The purposes of our study were therefore to (1) determine if a correlation existed between radiographic parameters on long-cassette, prone intraoperative films and the postoperative standing radiographs; and (2) determine what additional clinical benefit would be afforded by an intraoperative radiograph during the treatment of AIS with pedicle screw instrumentation.
The limitations of our study include the relatively small sample size as well as the retrospective nature of this study. Although the data were assessed retrospectively, all data were collected per our standard operating procedure for the performance of deformity correction surgery and had no missing data. Another potential weakness of our study is imaging was not standard between both study centers with one using all plain film radiography and the other using all digital imaging. While we had only one individual conduct all the radiographic measurements, two studies have demonstrated an intraobserver variability of less than 3° on both digital and manual measurements, whereas we consider a change of 5° as clinically important [11, 17].
The usefulness of intraoperative radiographs in spine surgery has been well established with regard to analyzing implant placement. In the cervical spine, the position of C2 intralaminar screws was correctly identified 77% of the time using intraoperative plain radiographs [14]. A study by Learch et al. [12] identifying pedicle screw placement found 63% of the screws were correctly identified with plain films. Given the relatively low incidence of neurovascular injury, intraoperative plain radiographs remain a cost-effective, reliable method for assessing implant position, particularly in recognizing screws that may need to be revised [1, 6, 21]. However, there is a paucity of literature evaluating intraoperative imaging to determine overall alignment. Our main purpose was to determine if these intraoperative radiographs could reliably assess alignment. We found curve magnitude correlated between the intraoperative and postoperative films for instrumented curves. There was also a statistically significant correlation in four of the six coronal balance parameters measured. A recent study of 114 patients with AIS demonstrated maintenance of main curve correction and TL/LC correction from the immediate postoperative films to the 3-year followup radiographs [13]. Therefore, if the intraoperative film strongly correlates with the immediate postoperative film, which it did in our study, the surgeon can get an appreciation of the ultimate correction of the deformity.
Additionally, we intended to determine what additional clinical benefit was afforded by intraoperative imaging. By obtaining intraoperative radiographs, the surgeon is able to affect immediate change in the construct as opposed to discovering on the postoperative film that the construct is not optimal. This occurred in only three patients in our current study. Although not statistically significant, these patients were spared both the cost and associated risks of an additional operative procedure.
Intraoperative radiographs facilitate recognition of any asymmetry, unacceptable residual deformity, or malpositioned implants that can be addressed during the index procedure, thereby avoiding the risks and costs associated with having to return to the operating room for a revision procedure. Based on our data, we conclude routine use of a long-cassette intraoperative film provides the surgeon with a valuable tool to guide intraoperative decision-making and foreshadows the ultimate correction and balance obtained on the immediate postoperative film.
Footnotes
One or more of the authors (LGL) has received funding from Medtronic, DePuy, Axial Biotech, and Quality Medical Publishing.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Walter Reed Army Medical Center, Washington, DC, and Washington University School of Medicine, St Louis, MO.
The views expressed in this manuscript are those of the authors and do not reflect the official policy of the Department of Army, Department of Defense, or the US Government. Three authors are employees of the US Government. This work was prepared as part of their official duties and as such there is no copyright to be transferred.
References
- 1.Acikbas SC, Tuncer MR. New method for intraoperative determination of proper screw insertion or screw malposition. J Neurosurg. 2000;93:40–44. doi: 10.3171/spi.2000.93.1.0040. [DOI] [PubMed] [Google Scholar]
- 2.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 3.D’Andrea LP, Betz RR, Lenke LG, Clements DH, Lowe TG, Merola A, Haher T, Harms J, Huss GK, Blanke K, McGlothlen S. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine. 2000;25:1795–1802. doi: 10.1097/00007632-200007150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Jamieson D, Perdios A, Varghese R, Reilly CW. The use of CT in the development and implementation of a preoperative protocol to aid in pedicle screw placement during scoliosis surgery. Pediatr Radiol. 2008;38:452–456. doi: 10.1007/s00247-008-0776-2. [DOI] [PubMed] [Google Scholar]
- 5.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, Lenke LG, Cheh G, Riew KD. Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine. 2005;30:2084–2088. doi: 10.1097/01.brs.0000178818.92105.ec. [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 8.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, Sides B. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 9.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Jr, Polly DW, Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90º. Spine. 2005;30:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 10.Kuklo TR, Potter BK, Lenke LG. Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis: what is the best radiographic correlate? J Spinal Disord Tech. 2005;18:139–147. doi: 10.1097/01.bsd.0000159033.89623.bc. [DOI] [PubMed] [Google Scholar]
- 11.Kuklo TR, Potter BK, Schroeder TM, O’Brien MF. Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine. 2006;31:1240–1246. doi: 10.1097/01.brs.0000217774.13433.a7. [DOI] [PubMed] [Google Scholar]
- 12.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: a proposed systematic approach to improve accuracy of interpretation. Spine. 2004;29:767–773. doi: 10.1097/01.BRS.0000112071.69448.A1. [DOI] [PubMed] [Google Scholar]
- 13.Lehman RA, Jr, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, Kuhns CA, Bridwell KH. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs; minimum three-year follow-up of one hundred fourteen cases. Spine. 2008;33:1598–1604. doi: 10.1097/BRS.0b013e318178872a. [DOI] [PubMed] [Google Scholar]
- 14.Lehman RA, Jr, Sasso RC, Helgeson MD, Dmitriev AE, Gill NW, Rosner MR, Riew DK. Accuracy of intraoperative plain radiographs to detect violations of intralaminar screws placed into the C2 vertebrae: a reliability study. Spine. 2007;32:3036–3040. doi: 10.1097/BRS.0b013e31815cdab9. [DOI] [PubMed] [Google Scholar]
- 15.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 16.Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, Hyman JE, Roye DP., Jr Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 17.Mok JM, Berven SH, Diab M, Hackbarth M, Hu SS, Deviren V. Comparison of observer variation in conventional and three digital radiographic methods used in the evaluation of patients with adolescent idiopathic scoliosis. Spine. 2008;33:681–686. doi: 10.1097/BRS.0b013e318166aa8d. [DOI] [PubMed] [Google Scholar]
- 18.O’Brien MF, Kuklo TR, Blanke KM, Lenke LG, editors. Spinal Deformity Study Group Radiographic Measurement Manual. Minneapolis, MN: Medtronic Sofamor Danek, Inc; 2005. [Google Scholar]
- 19.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke type I adolescent idiopathic scoliosis curves. Spine. 2005;30:1859–1866. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 20.Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am. 2008;90:43–51. doi: 10.2106/JBJS.F.01514. [DOI] [PubMed] [Google Scholar]
- 21.Sapkas GS, Papadakis SA, Stathakopoulos DP, Papagelopoulos PJ, Badekas AC, Kaiser JH. Evaluation of pedicle screw position in thoracic and lumbar spine fixation using plain radiographs and computed tomography. A prospective study of 35 patients. Spine. 1999;24:1926–1929. doi: 10.1097/00007632-199909150-00011. [DOI] [PubMed] [Google Scholar]
- 22.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–526. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 23.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 24.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YBl. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 25.Yazici M, Acaroglu ER, Alanay A, Deviren V, Cila A, Surat A. Measurement of vertebral rotation in standing versus supine position in adolescent idiopathic scoliosis. J Pediatr Orthop. 2001;21:252–256. doi: 10.1097/00004694-200103000-00025. [DOI] [PubMed] [Google Scholar]