Abstract
Depression and chronic physical illness are in reciprocal relationship with one another: not only do many chronic illnesses cause higher rates of depression, but depression has been shown to antedate some chronic physical illnesses. Depression associated with physical illness is less well detected than depression occurring on its own, and various ways of improving both the detection and treatment of depression accompanying physical illness are described. This paper is in four parts, the first dealing with the evidence for depression having a special relationship with physical disorders, the second dealing with detection of depression in physically ill patients, the third with the treatment of depression, and the fourth describing the advantages of treating depression among physically ill patients.
Keywords: Depression, chronic physical illness, prospective studies, collaborative care, improved detection
Depression among those with chronic physical illnesses is both a major public health challenge, and likely to be missed by professionals who care for physically sick patients. This is because health professionals are understandably concerned with the physical disorder which is usually the reason for the consultation, and may not be aware of the accompanying depression. However, untreated depression is a cause of much unnecessary suffering, and effective treatment has been shown to decrease disability, prolong survival and increase the quality of life.
EVIDENCE FOR A SPECIAL RELATIONSHIP
Incidence and prevalence of depression in those with physical illness
The prevalence of depression is significantly higher in those with physical illnesses both in the USA 1 and internationally 2. The American study compared the one year prevalence of depression in 10,500 patients with chronic disease with 19,460 age matched healthy controls and found that as a group the former were almost three times more likely to be depressed: the odds ratio (OR) was 2.6 (CI 2.31-2.94). Rates for depression were double in diabetes, hypertension, coronary artery disease and heart failure, and three times in endstage renal failure, chronic obstructive pulmonary disease and cerebrovascular disease 1. Broadly similar results are reported in the international study of the one year prevalence of depression among 245,400 patients in 60 countries: in this study those with two or more chronic physical disorders experienced a prevalence of depression of 23%, whereas healthy controls only reported depression in 3.2% of cases 2.
Patients with “comorbid” depression and anxiety disorders – who by definition have a greater number of symptoms than either depression or anxiety disorders on their own – have a stronger relationship with chronic physical diseases than those with either depression or anxiety on their own 3.
Physical disease causing depression
Two population-based prospective cohort studies found that physical illness was a risk factor for the later development of depression. A study by Patten et al 4 followed up for 2 years 11,859 people who had been free of depression at baseline, and found that 3.5% had developed a new episode of major depressive disorder. Physical illness was a risk factor for the development of such depressive disorder (OR=2.5, CI 1.3-4.6). The risk was similar for a wide range of physical illnesses, namely hypertension, asthma, arthritis and rheumatism, back pain, diabetes, heart disease and chronic bronchitis. In a study by Smit et al 5 in a population of 4,664 who had never had depressive disorder, 2.7% of the population had developed depression after one year. The presence of two of three illnesses (migraine, respiratory or abdominal problems) predicted the later development of depressive disorder (incident RR 2.85) after adjusting for confounders.
In clinical populations, the year after the diagnosis of cancer 6, and after first hospitalisation with a heart attack 7, are associated with a particularly high rate of new onset of depression or anxiety – approximately 20%. There is also consistent evidence for depression being a consequence of coronary heart disease, stroke and HIV/AIDS 8.
There are at least three distinct ways in which a chronic physical disease causes depression.
First, the number of different pains an individual experiences is directly proportional to the prevalence of depression: in the study by Dworkin et al 9, primary care patients with a single pain had no increased risk of depression, those with two pains had double the risk, but those with three or more had five times the risk. Pain in turn causes emotional distress and poor sleep, irrespective of whether pain has a known cause 10.
Second, chronic physical illness carries with it the risk of disability, and this can be very depressing for an adult who has previously been healthy. For example, Prince et al 11 showed that the population attributable fraction of disability or handicap to the prediction of onset of depression among the elderly was no less than 0.69, and similar findings have been reported by Ormel et al 12.
Third, there are physical changes in some diseases which may underlie the development of depression, such as changes in the allostatic load. Allostasis refers to the ability of the body to adapt to stressful conditions. It is a dynamic, adaptive process. Tissue damage, degenerative disease (like arthritis) and life stress all increase allostatic load and can induce inflammatory changes which produce substances such as bradykinin, prostaglandins, cytokines and chemokines. These substances mediate tissue repair and healing, but also act as irritants that result in peripheral sensitization of sensory neurons, which in turn activate central pain pathways 13. In stroke – especially left sided – cerebral ischaemia may favour development of depression, and in degenerative dementias the same processes may account for increased rates of depression.
Other features of physical illness that may lead to depression include disfigurement, the necessity for undergoing stressful investigations, and the fear of impending death.
Depression causing physical disease
A depressive illness can also precede a new episode of physical disease. Systematic reviews of eleven prospective cohort studies in healthy populations showed that depression predicted later development of coronary heart disease in all of them (OR 1.18 to 5.4, median=2.05; for new cardiovascular events, after adjustment for traditional risk factors: OR=1.90, 95% CI=1.48-2.42) 14-15. Three prospective studies have shown that depression is an independent risk factor in stroke 16,17,18.
In prospective population-based cohort studies, depression has been shown to predict the later development of colorectal cancer 19, back pain 20,21,22, irritable bowel syndrome 23, multiple sclerosis 24. There is inconsistent evidence that depression may precede the onset of type 2 diabetes 8. Prince et al 8 argue that there is consistent evidence for depression leading to physical ill-health in coronary heart disease and stroke, and depression in pregnancy leading to infant stunting and infant mortality.
The following are among the ways in which depression may cause physical illness. First, increases in proinflammatory cytokines in depression and increased adrenocortical reactivity may lead to atherosclerosis, and consequently to an increased risk for both stroke and coronary artery disease. Second, autonomic changes in depression may cause ECG changes which favour development of coronary disease. Third, immune changes that occur during depression may be relevant: they include an increase in white cell counts and a relative increase in neutrophils, increases in measures of immune activation, and a suppression of mitogen-induced lymphocyte proliferation, with a reduction in natural killer (NK) cells 25. Changes in NK cells and T-lymphocytes in depression may also lead to lowered resistance to AIDS in HIV infections. Menkes and McDonald 26 have argued that exogenous interferons cause both depression and increased pain sensitivity in susceptible individuals, by suppressing tryptophan availability and therefore serotonin synthesis.
Consequences of depression accompanying physical disease
Prince et al 8 argue that there is consistent evidence for depression affecting the outcome of coronary heart disease, stroke and diabetes.
Depression leads to a shorter expectancy of life 27 and therefore treatment might be expected to prolong life. However, the studies required to demonstrate this have not been done, as they would require long follow-up periods accompanied by prolonged treatment of depression, with the control group denied such treatment. Di Matteo et al 28, in a meta-analysis of factors related to non-compliance, found that depressed patients were three times as likely to be non-compliant with treatment recommendations as non-depressed patients, suggesting that there may be real advantages in treating depression among the physically ill. In heart disease, van Melle et al 29(29) showed a more than double greater risk of death with comorbid depression.
As the severity of depression increases, the subjective quality of life decreases. One of the reasons for persevering with active treatment for depression is that, even if the outlook for survival is not improved, the quality of survival will be greatly improved. In the large study by Moussavi et al 2, especially low health status scores were found in those with depression comorbid with physical illness.
DETECTION OF DEPRESSION ACCOMPANYING PHYSICAL DISEASE
Depression among those with physical illnesses is defined in the same way as depression occurring on its own. Thus, standard case finding screening measures such as the PHQ-9 30 or the Hospital Anxiety and Depression scale 31 are recommended in order to detect depression in all cases.
However, several of the defining symptoms of depression in both the DSM and the ICD classifications can sometimes be produced by the physical disorder rather than depressive illness – for example, poor energy, loss of weight or poor appetite, and sleep disturbance. When psychiatrists interview physically ill patients, they typically report no difficulty in ignoring these symptoms if they consider that the physical disorder may be causing them. Nevertheless, when other health professionals are assessing patients, the presence of these symptoms is likely to cause confusion, if the critical number of symptoms to justify a diagnosis of depression is applied in a rigid fashion.
It has been shown that in the UK general practitioners are very much less likely to detect depression in physically sick patients than they are among physically well patients – the detection rates being 24% and 95% respectively 32.
It is possible to use a reduced set of symptoms that does not include those mentioned above, and still achieve a high degree of agreement with researchers using the full set of nine symptoms. This is fortunate, since many non-psychiatrists have difficulty remem-bering the full list of symptoms. Zimmerman et al 33 have shown that a set of only five symptoms is sufficient – depressed mood, low interest, worthlessness, poor concentration and thoughts of death. These important findings have been replicated 34.
It is likely that if internists and family physicians were encouraged to use this modified scale, the detection rate of depression in chronic physical illness would greatly increase. The criteria are easier to remember, almost equally valid as the longer list, and much less likely to be produced by physical disease. In developing countries, where nurses, assistant medical officers and multi-purpose health workers are often responsible for case finding, and where even medical officers may not be skilled in detection of depression, the proposal has even greater merit.
TREATMENT OF DEPRESSION ACCOMPANYING PHYSICAL DISEASE
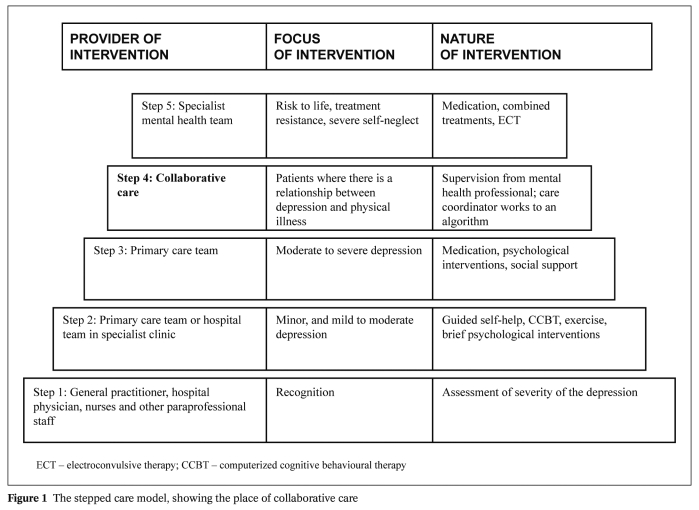
The stepped-care model provides a framework in which to organize the provision of services supporting both patients and carers, and healthcare professionals in identifying and accessing the most effective interventions (Figure 1). The aim of a stepped care programme is to provide the least intrusive, most effective intervention first and to promote the organization and delivery of care in a way which is understandable to patients and carers, as well as professionals.
Figure 1 The stepped care model, showing the place of collaborative care.
Gilbody et al 35 define collaborative care as that where the primary care physician maintains overall responsibility for the patient, but where there is a case manager to follow up patients and assess adherence to treatment, and a mental health specialist (psychiatrist or clinical psychologist) providing support and consultation to the physician. They find that not only is there evidence that collaborative care is effective in reducing depressive symptoms in those who are physically ill, but also emerging evidence that such model may be cost effective.
Collaborative care requires: a) a dedicated coordinator of the intervention located in and receiving support from a multiprofessional team; b) joint determination of the plan of care; c) longterm coordination and follow up; d) coordination of mental and physical health care.
Those with less severe depression may be helped by active monitoring combined with other interventions, including sleep hygiene and structured physical activity programmes. Physical activities must be modified to take account of any physical disabilities, and may take place either individually or in groups, with weekly sessions over a 12 week period. Other treatments based upon cognitive behavioural principles include individually based self-help programmes, and computerized cognitive behavioural therapy (CCBT).
Cognitive behaviour therapy (CBT), or components of it called behavioural activation, are the treatments of choice for those who prefer and have available suitably qualified therapists. These treatments can be delivered either in small groups of patients with similar physical health problems over about 8 weeks, or individually delivered for up to 18 weeks, with additional booster sessions over the next 12 months.
There is no good evidence that one antidepressant is superior to another in the treatment of depression among those with physical illnesses, and perhaps the most important consideration when choosing an antidepressant for these patients is the nature of the treatment being given for the physical illness. It should be recalled that sertraline is the antidepressant of choice in conjunction with β-blockers, and sertraline, mirtazapine, moclobemide or mianserin are drugs of choice in cardiac arrythmias.
Selective serotonin reuptake inhibitors (SSRIs) are recommended as the first line of drug treatment for the majority of physically ill patients, but should not be used in migraine treated with 5HT1 agonists (for example, sumatriptan, zolmitriptan), where they increase risk of central nervous system (CNS) toxicity and serotonergic effects, or with ergotamine, where they increase the risk of serotonin syndrome. They are also contraindicated in Parkinson’s disease treated with MAO-B inhibitors such as selegiline or rasagiline, because of increased risk of CNS excitation and hypertension.
Venlafaxine, fluvoxamine, and duloxetine should be avoided in the treatment of cardiac arrhythmias; hypertension treated with β-blockers, methyldopa and ACE inhibitors; and migraine treated with 5HT1 antagonists. In addition, venlafaxine should be avoided when viral infections are being treated with indinavir, because of decreased plasma levels. Trazodone is not recommended in those receiving digoxin for heart failure, since it increases its plasma levels. Mianserin should be avoided in conjunction with drugs used for cancer, including cytotoxic drugs, antiproliferatives and protein kinase inhibitors, and also in cases of organ transplantation treated with immuno-suppressants. Reboxetine should be avoided in conjunction with thiazide diuretics like bendroflumethiazide, because of the risk of hypokalaemia. It should also be avoided in the treatment of bacterial infections with erythromycin or clairthromycin. Older antidepressants, such as tricyclics and MAO inhibitors, and St. John’s wort, should be avoided in physically ill patients, since they are each associated with a wide range of interactions with other drugs.
ADVANTAGES OF TREATMENT OF DEPRESSION ACCOMPANYING CHRONIC PHYSICAL DISEASE
While generally reporting beneficial effects on depression, randomized trials have generally failed to show a significant effect of treatment of depression on concomitant heart disease 36-37 or diabetes 38-39. A systematic review of enhanced/collaborative care for depression in the physically ill concluded, on the basis of a meta-analysis, that depression can be treated effectively but there does not appear to be consistent evidence that such treatment improves physical outcomes 40-41.
Treatment for depression does have other beneficial effects on outcomes other than measures of depression. Simon et al 42 showed improvements in social and emotional functioning, and disability in a mixed group of chronic physical disorders in primary care. Mohr et al 43 showed improvements in both disability and fatigue with a CBT intervention for depression in patients with multiple sclerosis. Lin et al 44 showed that treatment of depression in patients with arthritis resulted in improved arthritis-related pain and functional outcomes and better general health status and overall quality of life. von Korff 45 argues that the weight of the evidence suggests that, in addition to reducing depressive symptoms, treatment of depression is effective in reducing functional disability.
As the severity of depression increases, the subjective quality of life decreases. One of the reasons for persevering with active treatment for depression is that even if the outlook for survival is poor, quality of life may still be improved.
Acknowledgement
This paper is based upon work carried out by the author and colleagues for the National Institute for Clinical Excellence (NICE) or the UK government. The full NICE guidance can be found at http://guidance.nice.org.uk/CG91.
References
- 1.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29:409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Moussavi S, Chatterji S, Verdes W. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:852–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 3.Scott KM, Bruffaerts R, Tsang A. Depression – anxiety relationships with chronic physical conditions: results from the World Mental Health surveys. J Affect Disord. 2007;103:113–120. doi: 10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Patten SB. Longterm medical conditions and major depression in a Canadian population study at waves 1 and 2. J Affect Disord. 2001;63:35–41. doi: 10.1016/s0165-0327(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 5.Smit F, Beekman A, Cuijpers P. Selecting key variables for depression prevention: results from a population-based prospective epidemiological study. J Affect Disord. 2004;81:241–249. doi: 10.1016/j.jad.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Burgess C, Cornelius V, Love S. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ. 2005;330:702–702. doi: 10.1136/bmj.38343.670868.D3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickens CM, Percival C, McGowan L. The risk factors for depression in first myocardial infarction patients. Psychol Med. 2004;34:1083–1092. doi: 10.1017/s0033291704001965. [DOI] [PubMed] [Google Scholar]
- 8.Prince M, Patel V, Saxena S. No health without mental health. Lancet. 2007;370:879–883. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin S, von Korff M, LeResche L. Multiple pains, psychiatric and psychosocial disturbance: an epidemiologic association. Arch Gen Psychiatry. 1990;47:1025–1037. doi: 10.1001/archpsyc.1990.01810150039007. [DOI] [PubMed] [Google Scholar]
- 10.von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry. 1996;30:101–108. [PubMed] [Google Scholar]
- 11.Prince M, Harwood RH, Blizard RA. Impairment, disability and handicap as risk factors for late life depression. Psychol Med. 1998;27:311–321. doi: 10.1017/s0033291796004473. [DOI] [PubMed] [Google Scholar]
- 12.Ormel J, Kempen GI, Penninx BW. Chronic medical conditions and mental health in old people. Psychol Med. 1997;27:1065–1067. doi: 10.1017/s0033291797005321. [DOI] [PubMed] [Google Scholar]
- 13.Rittner HL, Brack A, Stein C. Proalgesic and analgesic actions of immune cells. Curr Opin Anaesthesiol. 2003;16:527–533. doi: 10.1097/00001503-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–1467. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 16.Everson SA, Roberts RE, Goldberg DE. Depressive symptoms and increased risk of stroke mortality in a 29 year period. Arch Intern Med. 1998;158:1133–1138. doi: 10.1001/archinte.158.10.1133. [DOI] [PubMed] [Google Scholar]
- 17.Ohira T, Iso H, Satoh H. Prospective study of stroke among Japanese. Stroke. 2001;32:903–908. doi: 10.1161/01.str.32.4.903. [DOI] [PubMed] [Google Scholar]
- 18.Larson SL, Owens PL, Ford D. Depressive disorder, dysthymic disorder and risk of stroke. 13 year follow up study from Baltimore ECA study. Stroke. 2001;32:1979–1983. doi: 10.1161/hs0901.094623. [DOI] [PubMed] [Google Scholar]
- 19.Kroenke CH, Bennett GG, Fuchs C. Depressive symptoms and prospective incidence of colorectal cancer in women. Am J Epidemiol. 2005;162:839–848. doi: 10.1093/aje/kwi302. [DOI] [PubMed] [Google Scholar]
- 20.Larson SL, Clark MR, Eaton WW. Depressive disorder as a long-term antecedent risk factor for incident back pain: a 13-year follow-up study from the Baltimore Epidemiological Catchment Area sample. Psychol Med. 2004;34:211–219. doi: 10.1017/s0033291703001041. [DOI] [PubMed] [Google Scholar]
- 21.Jarvik JG, Hollingworth W, Heagerty PJ. Three-year incidence of low back pain in an initially asymptomatic cohort: clinical and imaging risk factors. Spine. 2005;30:1541–1548. doi: 10.1097/01.brs.0000167536.60002.87. [DOI] [PubMed] [Google Scholar]
- 22.Reid MC, Williams CS, Concato J. Depressive symptoms as a risk factor for disabling back pain in community-dwelling older persons. J Am Geriatr Soc. 2003;51:1710–1717. doi: 10.1046/j.1532-5415.2003.51554.x. [DOI] [PubMed] [Google Scholar]
- 23.Ruigómez A, Rodriguez LA, Panes J. Risk of irritable bowel syndrome after an episode of bacterial gastroenteritis in general practice. Clin Gastroenterol Hepatol. 2007;5:465–469. doi: 10.1016/j.cgh.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Grant I, McDonald I, Patterson T. Multiple sclerosis. In: Brown GW, Harris T, editors. Life events. London: Unwin; 1989. pp. 295–312. [Google Scholar]
- 25.Irwin M. Immune correlates of depression. Adv Exper Med Biol. 1999;461:1–24. doi: 10.1007/978-0-585-37970-8_1. [DOI] [PubMed] [Google Scholar]
- 26.Menkes DB, McDonald JA. Interferons, serotonin and neurotoxicity. Psychol Med. 2000;30:259–268. doi: 10.1017/s0033291799001774. [DOI] [PubMed] [Google Scholar]
- 27.Evans DL, Charney DS, Lewis L. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Di Matteo MR, Lepper HS, Croghan TW. Depression is a risk factor for non-compliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Ann Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 29.van Melle JP, de Jonge P, Spijkerman TA. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL. The PHQ-9: a new depression and diagnostic severity measure. Psychiatr Ann. 2002;32:509–521. [Google Scholar]
- 31.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 32.Bridges KW, Goldberg DP. Somatic presentation of DSM-III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- 33.Zimmerman M, Chelminski I, McGlinchey JB. A clinically useful depression outcome scale. Compr Psychiatry. 2008;49:131–140. doi: 10.1016/j.comppsych.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 34.Andrews G, Anderson TM, Slade T. Classification of anxiety and depressive disorders: problems and solutions. Depress Anxiety. 2008;25:274–281. doi: 10.1002/da.20489. [DOI] [PubMed] [Google Scholar]
- 35.Gilbody S, Bowers P, Gask L. Is collaborative care effective for depression in the presence of physical illness? Psychol Med. in press. [Google Scholar]
- 36.Glassman AH, O’Connor CM, Califf RM. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 37.Berkmann LF, Blumenthal J, Burg M. Effects of treating depression and low perceived social support on clinical events after myocardial infarction. The Enhancing Recovery in Coronary Heart Disease (ENRICHD) randomised trial. JAMA. 2003;289:3106–3106. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 38.Williams JW, Katon W, Lin E. The effectiveness of depression care management on depression and diabetes related outcomes in older patients with both conditions. Ann Intern Med. 2004;140:1015–1024. doi: 10.7326/0003-4819-140-12-200406150-00012. [DOI] [PubMed] [Google Scholar]
- 39.Katon W, Unutzer J, Fan MY. Cost-effectiveness and net benefit of enhanced treatment for depression for older adults with diabetes and depression. Diabetes Care. 2006;29:265–270. doi: 10.2337/diacare.29.02.06.dc05-1572. [DOI] [PubMed] [Google Scholar]
- 40.Bower P, Gilbody S, Richards D. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 41.Christensen H, Griffiths KM, Gulliver A. Models in the delivery of depression care: a systematic review of randomised and controlled intervention trials. BMC Family Practice. 2008;9:25–25. doi: 10.1186/1471-2296-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simon GE, von Korff M, Lin E. Clinical and functional outcomes of depression treatment in patients with and without chronic medical illness. Psychol Med. 2005;35:271–279. doi: 10.1017/s0033291704003071. [DOI] [PubMed] [Google Scholar]
- 43.Mohr DC, Hart S, Vella L. Reduction in disability in a randomized controlled trial of telephone-administered cognitive-behavioral therapy. Health Psychol. 2007;26:554–563. doi: 10.1037/0278-6133.26.5.554. [DOI] [PubMed] [Google Scholar]
- 44.Lin EHB, Katon W, von Korff M. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290:2428–2434. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 45.von Korff M, Scott K, Gureje O. Mind, body and health: global perspectives in mental disorders and physical illness from the WHO World Mental Health Surveys. Manuscript in preparation. [Google Scholar]