Abstract
AIM: To characterize clinical features, surgery, outcome, and survival of malignant melanoma (MM) of the gastrointestinal (GI) tract in a surgical training center in Bangkok, Thailand.
METHODS: A retrospective review was performed for all patients with MM of the GI tract treated at our institution between 1997 and 2007.
RESULTS: Fourteen patients had GI involvement either in a metastatic form or as a primary melanoma. Thirteen patients with sufficient data were reviewed. The median age of the patients was 66 years (range: 32-87 years). Ten patients were female and three were male. Seven patients had primary melanomas of the anal canal, stomach and the sigmoid colon (5, 1 and 1 cases, respectively). Seven patients underwent curative resections: three abdominoperineal resections, two wide local excisions, one total gastrectomy and one sigmoidectomy. Six patients had distant metastatic lesions at the time of diagnosis, which made curative resection an inappropriate choice. Patients who underwent curative resection exhibited a longer mean survival time (29.7 mo, range: 10-96 mo) than did patients in the palliative group (4.8 mo, P = 0.0006).
CONCLUSION: GI MM had an unfavorable prognosis, except in patients who underwent curative resection (53.8% of cases), who had a mean survival of 29.7 mo.
Keywords: Melanoma, Gastrointestinal tract, Neoplasm metastasis
INTRODUCTION
Malignant melanoma (MM) of the gastrointestinal (GI) tract is a rare condition, especially in Eastern countries. However, its incidence is rising with unclear reason[1]. It may be either primary or metastatic. GI metastasis of MM is frequently found during autopsy (50%-60% of cases), but a small proportion of melanoma patients are diagnosed with GI metastasis while living (2%-5% of patients)[2,3]. The most common sites of the metastasis are the stomach and small intestine. Meanwhile, primary MM can arise in any GI mucosal site, but is most common in the anorectal region and esophagus.
The prognosis of GI MM is very poor with a 5-year survival of < 10%[4]. Surgery is still the mainstay of treatment. Recent studies have reported a trend toward less radical resection because there is no significant advantage of aggressive surgery over limited surgery in terms of local disease control, recurrence, and survival time[4,5].
In Thailand, MM is less common than in western countries and the data are limited. This study, therefore, was conducted to evaluate clinical features, surgical options, and outcome including recurrence and survival of MM of the GI tract in a surgical training center in Bangkok, Thailand.
MATERIALS AND METHODS
A retrospective review was conducted on patients diagnosed with MM of the GI tract who were admitted to Siriraj Hospital between 1997 and 2007. Patients were identified from the hospital computer database using an ICD-10 system. Patients’ charts were reviewed retrospectively for patient characteristics, presenting symptoms, physical examination findings, imaging results, operative records, presence of complications, recurrence, follow-up time, survival time, and cause of death. Diagnosis was confirmed in all patients by histological study and immunochemistry for S-100 protein or HMB45 monoclonal antibody. Survival time was defined as the number of months from the time of diagnosis of GI MM to the time of death or the last follow-up evaluation. The long-term follow-up data were collected by direct contact with patients or their relatives. A Kaplan-Meier method was used for statistical analysis of survival outcome. This study was approved by Siriraj ethics committee, Mahidol University (EC1 2550/307).
RESULTS
Between 1997 and 2007, there were 14 patients diagnosed with MM of the GI tract in Siriraj Hospital. One patient was excluded from this study due to insufficient data in the medical records; thus, only 13 cases were included in this study. Ten patients were female and three were male. The median age of the patients at presentation was 66 years (range: 32-87 years). Seven patients had a primary GI MM (anorectal, n = 5; sigmoid colon, n = 1; and stomach, n = 1), whereas the others (three patients, 23.1%) had metastatic MM of the GI tract. The primary melanoma sites of these three patients were ocular, thumb, and ovary. There were three patients who had advanced GI MM of unknown primary origin.
The most common presenting symptom was abdominal pain (5 patients, 38.5%), followed by intra-abdominal mass in four patients (30.8%). Other presenting symptoms included obstructive jaundice, small bowel obstruction, bowel habit change, and tenesmus. The anorectal region was the most common site of GI MM (7 patients, 53.8%), followed by the stomach (3 patients, 23.1%) (Table 1).
Table 1.
Characteristic of patients with MM of the GI tract
| Curative group | Palliative group | All | |
| n | 7 | 6 | 13 |
| Median age (range) (yr) | 66 (32-87) | 57 (42-78) | 66 (32-87) |
| Gender (M/F) | 2/5 | 1/5 | 3/10 |
| Presenting symptoms n (%) | |||
| Abdominal pain | 1 | 4 | 5 (38.5) |
| Intra-abdominal mass | 4 | 0 | 4 (30.8) |
| Obstructive jaundice | 0 | 1 | 2 (15.4) |
| Small bowel obstruction | 0 | 1 | 1 (7.7) |
| Bowel habit change | 1 | 0 | 1 (7.7) |
| Tenesmus | 1 | 0 | 1 (7.7) |
| Investigation n (%) | |||
| Abdominal CT | 5 | 3 | 8 (61.5) |
| Endoscopy | 1 | 1 | 2 (15.1) |
| Upper GI study | 0 | 1 | 1 (7.7) |
| Barium enema | 1 | 0 | 1 (7.7) |
| Origin of GI MM n (%) | |||
| Primary | 7 | 0 | 7 (53.8) |
| Secondary | 0 | 3 | 3 (23.1) |
| Unknown primary | 0 | 3 | 3 (23.1) |
| Site of the tumor n (%) | |||
| Anorectal | 5 | 2 | 7 (53.8) |
| Stomach | 1 | 2 | 3 (23.1) |
| Jejunum | 0 | 1 | 1 (7.7) |
| Pancreas | 0 | 1 | 1 (7.7) |
| Sigmoid colon | 1 | 0 | 1 (7.7) |
| Survival times (mo) | |||
| Mean | 29.7 | 4.8 | 17 |
| Range | 10-96 | 4-12 | 4-96 |
MM: Malignant melanoma; GI: Gastrointestinal; CT: Computed tomography.
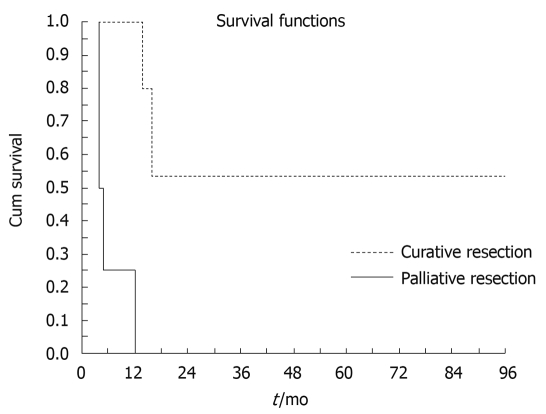
Seven patients (53.8%) underwent curative resection, which consisted of three abdominoperineal resections, two wide local excisions, one total gastrectomy, and one sigmoidectomy. There was no perioperative mortality in this study. Meanwhile, another six patients (46.2%) had distant metastatic lesions at the time of diagnosis. They therefore received only palliative surgical treatment such as colostomy, small bowel resection, and enteroenterostomy anastomosis. Patients who underwent curative resection exhibited a longer mean survival time (29.7 mo, range: 10-96 mo) than patients in the palliative group (4.8 mo, range: 4-12 mo) (Figure 1). Survival was significantly increased in patients who underwent curative resection (P = 0.0006).
Figure 1.
Kaplan-Meier curve demonstrating survival of patients with malignant melanoma of the gastrointestinal tract, who underwent curative resection and palliative resection.
DISCUSSION
In Thailand, MM is a rare disease. The estimated incidence rate of cutaneous melanoma in Thailand is 0.4 and 0.1 per 100 000 in men and women, respectively[5]. Incidence of MM of the GI tract is exceedingly rare[6]. There have been only a few reported cases of documented anorectal MM in Thailand[7]. MM of the GI tract can be either primary or metastatic. Primary GI melanoma must be differentiated from metastatic disease by previous history of melanoma and complete physical examination.
Patients often present with bleeding, pain or intestinal obstruction. If the patients present with GI bleeding, an endoscopy with magnification might be the procedure of choice to diagnose MM of the GI tract[8-10]. Multiple black, depressed lesions (1 ± 5 mm in diameter) with a “bull’s eye” appearance are usually viewed in the GI mucosa[9]. In the present study, approximately half of the patients presented with pain. A lower number of patients presented with gross GI bleeding and obstruction.
MM of the GI tract remains a fatal disease. Patients often present with advanced disease. In our study, almost half of the patients had metastatic disease at the time of presentation. The prognosis of GI MM is poor. The mean survival time of patients with a local or locoregional disease who underwent curative resection was only 29.7 mo. Several investigators have reported that the overall survival varies from 12 to 18 mo, with a 5-year survival of < 10%[11]. When systemic metastasis has occurred, mean survival is only 6-8 mo[12,13].
As a result of the poor prognosis of this disease, operative intervention has been discouraged. However, several recent studies have demonstrated better survival outcome in the patients who had complete surgical resection[14-19]. Our experiences compare favorably with those of other centers. Our study demonstrated seven patients with GI MM who underwent curative resection with a mean survival comparable to that in other centers. Several adjuvant treatment of GI MM such as chemotherapy, radiotherapy and immunotherapy have been utilized in many countries, but no such treatment was given in our center because of their unclear effectiveness. One recent randomized trial has demonstrated no survival benefit of adjuvant therapy[20].
In conclusion, patients with GI MM had a poor prognosis, especially in nonoperable cases. Surgical resection of the tumor resulted in a longer survival time. In selected patients with local or locally advanced disease, surgery should be performed where possible.
COMMENTS
Background
Gastrointestinal (GI) malignant melanoma (MM) is a rare malignancy. As a result of the paucity of cases, the available data about its clinical features, treatment options, and outcomes are very limited, especially in Eastern countries.
Research frontiers
As a result of the poor prognosis of GI MM, improvement of its treatment options is an area that is in need of research. However, in order to reach that point, some basic understanding of the clinical characteristics and treatment outcomes of current surgical approaches is required. This study provides a picture of clinical experience with this rare disease from one surgical training center in Thailand.
Innovations and breakthroughs
This study revealed that the nature of MM of the GI tract and its treatment outcomes in Thailand were similar and comparable to those from other centers.
Applications
With a better understanding of GI MM and its poor prognosis, future research should look at how to improve the treatment outcome, through early diagnosis, selection of patients undergoing surgery, and improvement of surgical techniques.
Peer review
This is a retrospective study on surgical management of MM of the GI tract. Patients who underwent curative resection exhibited a longer mean survival time than patients in the palliative group. Survival was significantly increased in patients who underwent curative resection.
Footnotes
Peer reviewers: Nadia Peparini, MD, PhD, Department of General Surgery “Francesco Durante”, La Sapienza University, Viale del Policlinico, 155, Rome, 00161, Italy; Dr. Oliver Mann, MD, Senior Attending Physician and Deputy Director, Department of General, Visceral and Thoracic Surgery, University of Hamburg, Martini Str. 52, D-20246 Hamburg, Germany; Dr. Yuk Him Tam, Department of Surgery, Prince of Wales Hospital, Shatin, Hong Kong, China
S- Editor Tian L L- Editor Kerr C E- Editor Ma WH
References
- 1.Klaase JM, Kroon BB. Surgery for melanoma metastatic to the gastrointestinal tract. Br J Surg. 1990;77:60–61. doi: 10.1002/bjs.1800770121. [DOI] [PubMed] [Google Scholar]
- 2.Dasgupta T, Brasfield R. Metastatic melanoma. A clinicopathological study. Cancer. 1964;17:1323–1339. doi: 10.1002/1097-0142(196410)17:10<1323::aid-cncr2820171015>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 3.Cagir B, Whiteford MH, Topham A, Rakinic J, Fry RD. Changing epidemiology of anorectal melanoma. Dis Colon Rectum. 1999;42:1203–1208. doi: 10.1007/BF02238576. [DOI] [PubMed] [Google Scholar]
- 4.Bullard KM, Tuttle TM, Rothenberger DA, Madoff RD, Baxter NN, Finne CO, Spencer MP. Surgical therapy for anorectal melanoma. J Am Coll Surg. 2003;196:206–211. doi: 10.1016/S1072-7515(02)01538-7. [DOI] [PubMed] [Google Scholar]
- 5.Promtatvethi V, Gojaseni P, Buri P, Censarn N. Malignant melanoma: a clinical experience in a Thai hospital. J Med Assoc Thai. 1978;61:210–216. [PubMed] [Google Scholar]
- 6.Crombie IK. Racial differences in melanoma incidence. Br J Cancer. 1979;40:185–193. doi: 10.1038/bjc.1979.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Somran J, Kanngurn S, Porncharoenpong S, Lertkajornsin O. Anorectal malignant melanoma: report of two cases from Buddhachinnaraj Hospital. J Med Assoc Thai. 2005;88:1128–1133. [PubMed] [Google Scholar]
- 8.Pommer B, Probst A, Messmann H. Gastric metastases from malignant melanoma. Endoscopy. 2008;40 Suppl 2:E30–E31. doi: 10.1055/s-2007-995434. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka K, Toyoda H, Hamada Y, Aoki M, Kosaka R, Noda T, Katsurahara M, Nakamura M, Ninomiya K, Inoue H, et al. Duodenal metastasis of malignant melanoma observed by magnification endoscopy. Endoscopy. 2008;40 Suppl 2:E6–E7. doi: 10.1055/s-2007-966566. [DOI] [PubMed] [Google Scholar]
- 10.Galloro G, Inzirillo A, Magno L, Diamantis G, Inzirillo M, Pastore A, Ruggiero S, Mosella G. Multiple nodular lesions by colonic metastatic malignant melanoma. Dig Liver Dis. 2009;41:169. doi: 10.1016/j.dld.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 11.Yang JI, Byun HJ, Kang JM. Education and imaging. Gastrointestinal: anorectal malignant melanoma. J Gastroenterol Hepatol. 2009;24:697. doi: 10.1111/j.1440-1746.2009.05816.x. [DOI] [PubMed] [Google Scholar]
- 12.Liang KV, Sanderson SO, Nowakowski GS, Arora AS. Metastatic malignant melanoma of the gastrointestinal tract. Mayo Clin Proc. 2006;81:511–516. doi: 10.4065/81.4.511. [DOI] [PubMed] [Google Scholar]
- 13.Lens M, Bataille V, Krivokapic Z. Melanoma of the small intestine. Lancet Oncol. 2009;10:516–521. doi: 10.1016/S1470-2045(09)70036-1. [DOI] [PubMed] [Google Scholar]
- 14.Berger AC, Buell JF, Venzon D, Baker AR, Libutti SK. Management of symptomatic malignant melanoma of the gastrointestinal tract. Ann Surg Oncol. 1999;6:155–160. doi: 10.1007/s10434-999-0155-8. [DOI] [PubMed] [Google Scholar]
- 15.Agrawal S, Yao TJ, Coit DG. Surgery for melanoma metastatic to the gastrointestinal tract. Ann Surg Oncol. 1999;6:336–344. doi: 10.1007/s10434-999-0336-5. [DOI] [PubMed] [Google Scholar]
- 16.Ishizone S, Koide N, Karasawa F, Akita N, Muranaka F, Uhara H, Miyagawa S. Surgical treatment for anorectal malignant melanoma: report of five cases and review of 79 Japanese cases. Int J Colorectal Dis. 2008;23:1257–1262. doi: 10.1007/s00384-008-0529-6. [DOI] [PubMed] [Google Scholar]
- 17.Sanki A, Scolyer RA, Thompson JF. Surgery for melanoma metastases of the gastrointestinal tract: indications and results. Eur J Surg Oncol. 2009;35:313–319. doi: 10.1016/j.ejso.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Huang YJ, Wu MH, Lin MT. Multiple small-bowel intussusceptions caused by metastatic malignant melanoma. Am J Surg. 2008;196:e1–e2. doi: 10.1016/j.amjsurg.2007.05.062. [DOI] [PubMed] [Google Scholar]
- 19.Slaby J, Suri U. Metastatic melanoma with multiple small bowel intussusceptions. Clin Nucl Med. 2009;34:483–485. doi: 10.1097/RLU.0b013e3181a7d25e. [DOI] [PubMed] [Google Scholar]
- 20.Spitler LE, Grossbard ML, Ernstoff MS, Silver G, Jacobs M, Hayes FA, Soong SJ. Adjuvant therapy of stage III and IV malignant melanoma using granulocyte-macrophage colony-stimulating factor. J Clin Oncol. 2000;18:1614–1621. doi: 10.1200/JCO.2000.18.8.1614. [DOI] [PubMed] [Google Scholar]