Abstract
Objective
The aim of this study was to investigate the morphological characteristics of the thalamoperforating arteries that arise from the P1 segment of the posterior cerebral artery.
Methods
Thalamoperforating arteries located in the interpeduncular fossa were dissected in 26 formalin-fixed human cadaver brains. We investigated the origin site of thalamoperforating arteries from the P1 segment, number and diameter, and variations in their origin.
Results
Thalamoperforating arteries arose from the superior, posterior or posterosuperior surfaces of the P1 segment at the mean 1.93 mm (range, 0.41-4.71 mm) distance from the basilar apex and entered the brain through the posterior perforated substance. The average number was 3.6 (range 1-8) and mean diameter was 0.70 mm (range 0.24-1.18 mm). Thalamoperforating arteries could be classified into five different types according to their origin at the P1 segment : Type I (bilateral multiple), 38.5%; Type II (unilateral single, unilateral multiple), 26.9%; Type III (bilateral single), 19.2%; Type IV (unilateral single), 11.5%; Type V (unilateral multiple), 3.8%. In 15.4% of all specimens, thalamoperforating arteries arose from the only one side of P1 segment and were not noted in the other side. In such cases, the branches arising from the one side of P1 segment supplied the opposite side.
Conclusion
Variations in the origin of the thalamoperforating arteries should be keep in mind to perform the surgical clipping, endovascular treatment or operation involving the interpeduncular fossa. In particular, unilateral single branch seems to be very risky and significant for surgical technique or endovascular treatment.
Keywords: Morphology, Cadaver, Thalamoperforating artery, Posterior cerebral artery
INTRODUCTION
The perforating arteries arising at the base of the brain from the posterior communicating arteries and the basilar bifurcation, which contribute part of the blood supply to the thalamus, are designated as thalamoperforating arteries. These arteries have a close relationship with many important neural structures during its course. A number of studies of the vascular structures and variations of the thalamoperforating arteries have been published1-11). This suggests that there are several variations of the perforating arteries on their origin and distribution.
Knowledge of the microvascular features of the thalamoperforating arteries is of paramount importance for surgeons approaching vascular lesions of this area, particularly basilar top aneurysms, and also importance for neurologist and neurointerventionist for ischemic lesion involving basilar artery (BA) and P1 segment of posterior cerebral arteries (PCA).
We investigated the microvascular anatomy of this region using formalin-fixed human cadaver brains and measured the outer diameter and length of these vessels, definition of their branching patterns and variations of the vessels.
MATERIALS AND METHODS
Twenty-six formalin-fixed human cadaver brains were used. The brains were very carefully removed from the skull, in order to avoid damage to the brain stems, as well as to the BA, PCA and superior cerebellar artery. The brain was placed upside down, and the ventral surface of the brain stem was examined from anterior to posterior to permit direct viewing of the interpeduncular fossa. Thalamoperforating arteries arising from the P1 segment of the PCA were carefully dissected in the interpeduncular fossa under a Zeiss NC4 microscope (×40) (Carl Zeiss Inc., Germany). We investigated the following items : 1) site of the P1 segment from that thalamoperforating artery originates; 2) distance from the bifurcation of the BA to the 1st origin of the thalamoperforating artery in P1 segment; 3) length of the P1 segment from the bifurcation of the BA; 4) outer diameter and numbers of the perforating arteries at both P1 segment and upper BA; 5) Morphological variations in the origin of the thalamoperforating arteries at P1 segment origin (Fig. 1). In addition, perforating arteries arising from the ventral surface of upper potion of BA were also investigated. During the measurements a digimatic caliper (Mitutoyo Co., Tokyo, Japan) was used, and photographs were taken by using a digital camera.
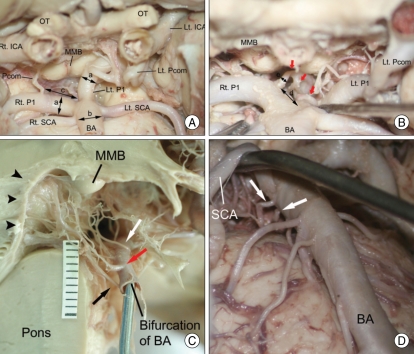
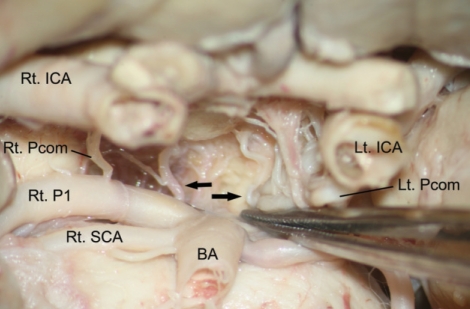
Fig. 1.
Photographs showing the anatomical structures in the interpeduncular fossa. The measured vascular structures are visible on the anteroinferior view of the interpeducular fossa (A and B). On the midsagittal section of the brain stem (C), thalamoperforating arteries arise from the superior (white arrow), posterosuperior (red arrow) and posterior surfaces (black arrow) of the P1 segment and enter the midbrain through the posterior perforated substance (arrowheads). There are visible two perforating arteries (white arrows) arising from the ventral surface of BA on the anteroinferior view of the interpeduncular fossa (D). a, diameter of the P1 segment; b, diameter of the BA; c, distance of the P1 segment; d, distance between the bifurcation of BA and the 1st origin of the thalamoperforating artery (red arrows); e, diameter of the thalamoperforating artery. BA : basilar artery, ICA : internal carotid artery, Lt : left, MMB : mamillary body, OT : optic nerve, Pcom : posterior communicating artery, P1 : P1 segment of posterior cerebral artery, Rt : right, SCA : superior cerebellar artery.
RESULTS
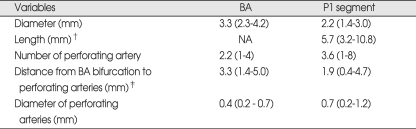
Thalamoperforating arteries were seen in all specimens. Thalamoperforating arteries arose from the superior, posterior or posterosuperior surfaces of the P1 segment at the mean 1.93 mm (range, 0.41-4.71 mm; median 1.95 mm) distance from the basilar apex and entered the midbrain through the posterior perforated substance (Fig. 1). The average number of these arteries was 3.6 (range 1-8) and mean diameter was 0.70 mm (range 0.24-1.18 mm; median 0.67 mm). The mean length of P1 segment from the apex of BA was 5.76 mm (rage, 3.15-10.83 mm; median 5.8 mm). Mean diameters of the BA and P1 segment of PCA were 3.34 mm (range, 2.28-4.16 mm; median 3.36 mm) and 2.24 mm (range, 1.36-3.03; median, 2.32 mm). One to four fine perforators (mean 2.2) with the mean diameter of 0.42 mm (range, 0.16-0.71 mm; median 0.4 mm) were also observed to arise from the ventral surfaces of the BA at the last 1.4 to 5.0 mm (mean 3.34 mm) of the basilar apex (Table 1).
Table 1.
Morphological characteristics of perforating arteries arising from the upper BA and P1 segment in 26 cadaveric specimen*
*Values and parentheses indicate average and range, respectively, †Length of the P1 segment means the distance between the BA bifurcation and the junction of the posterior communicating and posterior cerebral arteries, ‡Distance in BA was measured from the BA bifurcation to the perforators arising from ventral surface and just below BA bifurcation. In P1 segment, distance was measured from the BA bifurcation to the 1st origin of thalamoperforating artery of P1 segment. BA : basilar artery, NA : not applicable
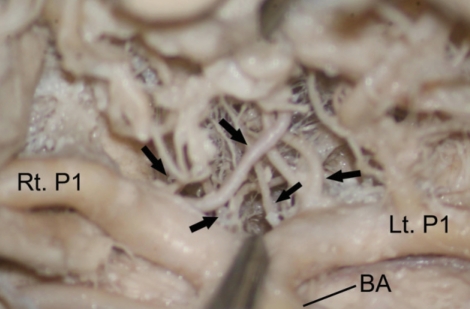
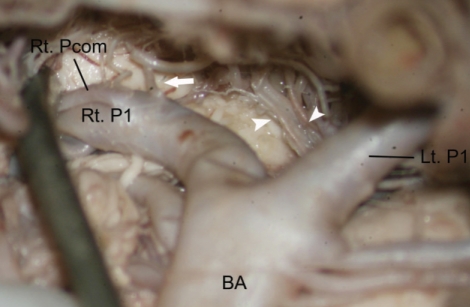
Thalamoperforating arteries were classified into five different types according to their origin at the P1 segment : Type I (Bilateral multiple), multiple branches arose from the P1 segment on each side (10 cases, 38.5%) (Fig. 2); Type II (Unilateral single, unilateral multiple), a single branch on one side of P1 segment and multiple branches on the other side (7 cases, 26.9%) (Fig. 3); Type III (Bilateral single), a single thick branch on each P1 segment (5 cases, 19.2%) (Fig. 4); Type IV (Unilateral single), unilateral single branch and the other with no branch (3 cases, 11.5%) (Fig. 5); Type V (Unilateral multiple) : unilateral multiple and the other with no branch (1 case, 3.8%) (Fig. 6).
Fig. 2.
Photograph showing the bilateral multiple thalamoperforating arteries (black arrows). BA : basilar artery, Lt : left, P1 : P1 segment of posterior cerebral artery, Rt : right.
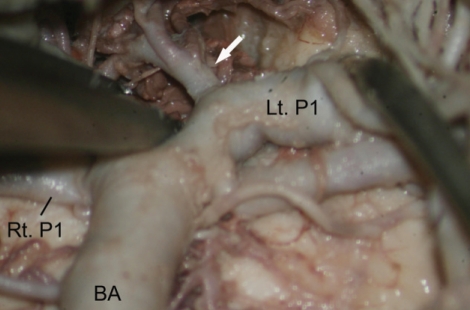
Fig. 3.
Photograph showing the unilateral single and unilateral multiple type of thalamoperforating artery. Single thalamoperforating artery (white arrow) arising from the superior surface of the right P1 segment is visible. Multiple thalamoperforating arteries (arrow heads) arising from the posterior surface of the left P1 segment is also visible. BA : basilar artery, Lt : left, P1 : P1 segment of posterior cerebral artery, Rt : right.
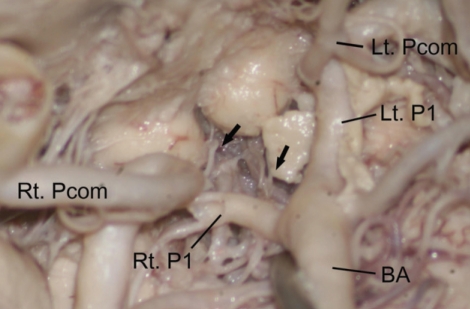
Fig. 4.
Photograph showing the bilateral single type of thalamoperforating arteries (black arrows). BA : basilar artery, ICA : internal carotid artery, Lt : left, Pcom : posterior communicating artery, P1 : P1 segment of posterior cerebral artery, Rt : right, SCA : superior cerebellar artery.
Fig. 5.
Photograph showing the unilateral single thalamoperforating artery (white arrow). BA : basilar artery, Lt : left, P1 : P1 segment of posterior cerebral artery, Rt : right.
Fig. 6.
Photograph showing the unilateral multiple thalamoperforating arteries (black arrows). Prominent posterior communicating artery is visible on right side. Thalamoperating artery arising from the left P1 segment is not visible. BA : basilar artery, Lt : left, Pcom : posterior communicating artery, P1 : P1 segment of posterior cerebral artery, Rt : right.
In bilateral 52 P1 segments of 26 specimens, multiple thalamoperforating arteries more than two arising from the P1 segment were noted in 28 P1 segments (53.8%) and single thalamoperforating artery was noted in 20 P1 segments (38.5%). In 3 specimen (11.5%), P1 segment had a single thick branch on one side and had no branch on the other side. If this branch arises as a single thick artery, damage to this artery during surgery may cause serious neurological insufficiency.
DISCUSSION
The perforating arteries arising at the base of the brain from the posterior communicating arteries and the basilar bifurcation, which contribute part of the blood supply to the thalamus, are designated as thalamoperforating arteries. The thalamoperforating arteries were identified by both Duret1) and Heubner6) in the latter part of the 19th century, described as "optic arteries" supplying part of the thalamus and the optic pathways. George et al.3) also reported that the posterior thalamoperforating arteries may be divided into interpeduncular, mesencephalic and thalamic segments in the study of microangiographic and microscopic dissections with 63 freshly autopsied brains. Zeal20), Saek and Rhoton17) reported that these arteries are a group of branches that arise from the P1 segment of this artery and the posterior communicating artery. These authors referred to the arteries that arise from the posterior communicating artery as anterior thalamoperforating arteries, and the branches that arise from the P1 segment as the posterior thalamoperforating arteries. They named the thickest thalamoperforating artery as the premamillary artery, and the thickest posterior thalamoperforating artery as the thalamoperforating artery. On the one hand, Pedroza et al.13) reported that the vessels that penetrate the posterior perforating substance and the anterior mesencephalic tegmentum were classified as, inferior paramedian mesencephalic arteries, branches of the P1 segment or sometimes the BA, superior paramedian mesencephalic arteries which systematically originate on the P1 segment and follow their course to the posterior half of the posterior perforated substance, and finally paramedian thalamic arteries which also stem from the P1 segment in every case, and vascularize the anterior half of the posterior perforated substance.
The thalamoperforating arteries consist of one or more arteries usually originating on the central segment of P1, but occasionally originating from the medial 1 mm P1 (8%) or the lateral 1 mm (5%) or rarely even arising from the posterior portion of the posterior communicating artery9). Marinkovic and Milisavljevic10) found the most proximal perforating artery to arise as close as 2.1 mm to the basilar bifurcation, and the most distal vessel to branch off at a distance of 2.6 mm from the junction with the posterior communicating artery. Average number and diameter of these arteries have been reported to be 2-2.7 (range, 0-10) and 0.32 mm (range 0.1-1 mm)10,11,13,20). They usually arise from the posterior or superior surface of the P1 segment4,20). In our study, the mean distance to the basilar bifurcation from the origin of perforating arteries was similar as 1.93 mm (range 0.16-4.71 mm; median 1.95 mm), the average number of these arteries was 3.6 (range 1-8) and mean diameter was 0.70 mm (range 0.24-1.18 mm; median 0.67 mm). They arose from the superior, posterior or posterosuperior surfaces of the P1 segment. This fits with our finding that no perforators were located on the anterior surface of the basilar bifurcation and thus surgical results are better with anterior aneurysms because the less tendency for vital perforators to be involved.
Also, the posterior and lateral surfaces of the upper centimeter of the BA were rich source of perforating arteries. Saeki and Rhoton17) noted that an average eight (range 3-18) branches of 0.1 to 0.5 mm diameter arose from the upper centimeter; approximately one-half arose from the posterior surface and one-fourth from each side, and intermixed with the medial P1 branches forming a complex arterial plexus in the interpeduncular fossa. No perforating branches arose from the anterior surface of the basilar apex, but one or two perforators arose from the anterior surface of one-third P1 segments. In our study, one to four fine perforators (mean 2.2) with the mean diameter of 0.42 mm (range, 0.16-0.71 mm; median 0.4 mm) arose from the ventral surfaces of the BA at the last 1.4 to 5.0 mm (mean 3.34 mm) of the basilar apex.
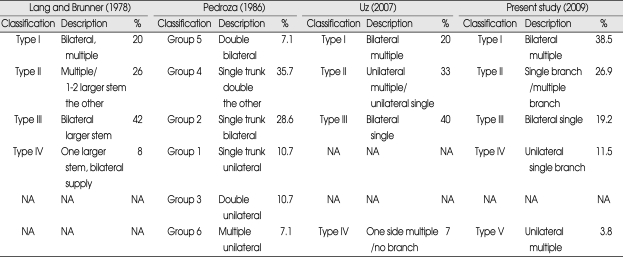
Lang and Brunner8) described four patterns of thalamoperforating arteries in an examination of 50 cadaver brains (Table 2). In type IV of their classifications, one P1 had no thalamoperforating branches, while the other had a large stem thalamoperforator that supplied branches bilaterally. Similar cases of unilaterally aplastic thalamoperforators with contralateral crossover have been described by Westberg, Percheron and Saeki and Rhoton14-17,19). Other studies of the variations of thalamoperforating arteries summarized in Table 2.
Table 2.
Summary of the studies on the classification of the thalamoperforating arteries
NA : not appilicable
Pedroza et al.13) reported that about 10% of P1 segments the perforators originated from only one trunk, so occlusion would always cause bilateral thalamopeduncular infarct. In the present study, five (19.2%) of cases, these arteries arose from the P1 segment on each side as a single thick branch. There was only a single thick branch on one side in 11.5% of cases. In such cases the opposite side was supplied by this branch. If this branch arises as a single thick artery, damage to this artery during surgery may cause serious neurological insufficiency. The number and diameter of perforating branches were relatively constant, regardless of the P1 segment size; therefore, a hypoplastic posterior communicating artery or P1 segment supplied the same perforating area as a larger vessel despite its smaller size. This fits with our finding, so the importance of preservation of these vessels deserves emphasis because of the important role of a hypoplastic vessel in supply of the local area. If hypoplastic segments are divided in case of clipping on basilar apex aneurysm, care should be taken not to sacrifice any small perforators17).
The thalamoperforating arteries enter the brain after passing from the posterior perforated substance, interpeduncular fossa and from the medial side of the cerebral peduncle. These arteries supply the posterior part of the thalamus, the hypothalamus, subthalamus, substantia nigra, red nucleus, oculomotor nucleus, trochlear nucleus, reticular formation of the midbrain, pretectum, rhomboid fossa and posterior part of the internal capsule. Occlusion of the posterior thalamoperforating arteries may produce a variety of syndromes including : contralateral hemiplegia, cerebellar ataxia, or a "rubral" tremor associated with ipsilateral oculomotor nerve paresis. If the lesion affects the subthalamus it may produce contralateral hemiballismus, which abates into choreiform movements with time or treatment.
Percheron14-16) described three possible variations involving the paramedian thalamic-mesencephalic arterial supply : small branches arising from both P1 segments, an asymmetrical common trunk arising from a P1 segment (this variation is called "the artery of Percheron", or an arterial arcade emanating from an artery bridging the two P1 segments. Bilateral thalamic infarcts are uncommon. The paramedian thalamic region is the most commonly affected location, and usually the infarcts are asymmetrical and caused by multiple emboli or small artery disease. Occlusion of "the artery of Percheron" results in bilateral medial thalamic and rostral mesencephalic infarctions with a relatively symmetrical distribution. When "the artery of Percheron" is occluded, the thalamic infarcts are always bilateral and medial. Matheus and Castillo12) propose that, when bilateral medial thalamic infarcts are found, occlusion of "the artery of Percheron" should be considered as the main diagnosis.
Knowledge of the microvascular features of the thalamoperforating arteries is of paramount importance for surgeons approaching vascular lesions of this area, particularly basilar top aneurysms, and also importance for neurologist and neurointerventionists for ischemic lesion involving BA and P1 segment of PCA. Awareness of variations in the basilar and posterior cerebral arteries is important for the treatment of aneurysms of these arteries because their number arising from the P1 segment is variable. They can arise as a single thick branch or one, two or multiple small branches.
CONCLUSION
Variations in the origin of the thalamoperforating arteries should be keep in mind to perform the surgical clipping, endovascular treatment or operation involving the interpeduncular fossa. Particularly, unilateral single branch seems to be very risky and significant for surgical technique or endovascular treatment.
References
- 1.Duret M. Recherches anatomiques sur la circulation de l'encéphale. Arch Phys Norm Path. 1874;1:60–91. (Cited from George AE, Raybaud C, Salamon G, Kricheff II : Anatomy of the thalamoperforating arteries with special emphasis on arteriography of the third ventricles : Part I. Am J Roentgenology 124 : 220-230, 1975) [Google Scholar]
- 2.Duvernoy HM. Human brainstem vessels. Berlin, Heidelberg, New York: Springer-Verlag; 1978. pp. 16–23. [Google Scholar]
- 3.George AE, Raybaud C, Salamon G, Kricheff II. Anatomy of the thalamoperforating arteries with special emphasis on arteriography of the third ventricles : Part I. Am J Roentgenol Radium Ther Nucl Med. 1975;124:220–230. doi: 10.2214/ajr.124.2.220. [DOI] [PubMed] [Google Scholar]
- 4.Grand W, Hopkins LN. The microsurgical anatomy of the basilar artery bifurcation. Neurosurgery. 1977;1:128–131. doi: 10.1227/00006123-197709000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Hara K, Fujino Y. The thalamoperforate artery. Acta Radiol Diagn (Stockh) 1966;5:192–200. doi: 10.1177/02841851660050p122. [DOI] [PubMed] [Google Scholar]
- 6.Heubner Zur topographie der Ernähungsgabiete der einzelnen hirnarterien. Zbl Med Wiss. 1872;52:817–821. (Cited from George AE, Raybaud C, Salamon G, Kricheff II : Anatomy of the thalamoperforating arteries with special emphasis on arteriography of the third ventricles : Part I. Am J Roentgenology 124 : 220-230, 1975) [Google Scholar]
- 7.Kaplan HA, Ford DH. The brain vascular system. Amsterdam: Elsevier; 1966. pp. 70–81. [Google Scholar]
- 8.Lang J, Brunner FX. Über die rami centrales der aa. Cerebri anterior and media. Gegenbaurs Morph Jb. 1978;124:364. [PubMed] [Google Scholar]
- 9.Marinkovic SV, Gibo H. The surgical anatomy of the perforating branches of the basilar artery. Neurosurgery. 1993;33:80–87. doi: 10.1227/00006123-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Marinkovic SV, Milisavljevic M. The surgical anatomy of relationships between the perforating and the leptomeningeal arteries. Neurosurgery. 1996;39:72–83. doi: 10.1097/00006123-199607000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Marinkovic SV, Milisavljevic M, Kovacevic M. Interpeduncular perforating branches of the posterior cerebral artery : the microsurgical anatomy of their extracerebral and intracerebral segments. Surg neurol. 1986;26:349–359. doi: 10.1016/0090-3019(86)90135-7. [DOI] [PubMed] [Google Scholar]
- 12.Matheus MG, Castillo M. Imaging of acute bilateral paramedian thalamic and mesencephalic infarcts. Am J Neuroradiol. 2003;24:2005–2008. [PMC free article] [PubMed] [Google Scholar]
- 13.Pedroza A, Dujovny M, Ausman JI, Diaz FG, Artero JC, Berman SK, et al. Microvascular anatomy of the interpeduncular fossa. J Neurosurg. 1986;64:484–493. doi: 10.3171/jns.1986.64.3.0484. [DOI] [PubMed] [Google Scholar]
- 14.Percheron G. [Arteries of the human thalamus. I. Artery and polar thalamic territory of the posterior communicating artery] Rev Neurol (Paris) 1976;132:297–307. [PubMed] [Google Scholar]
- 15.Percheron G. [Arteries of the human thalamus. II. Artery and paramedian thalamic territory of the communicating basilar artery] Rev Neurol (Paris) 1976;132:309–324. [PubMed] [Google Scholar]
- 16.Percheron G. The anatomy of the arterial supply of the human thalamus and its use for the interpretation of the thalamic vascular pathology. Z Neurol. 1973;205:1–13. doi: 10.1007/BF00315956. [DOI] [PubMed] [Google Scholar]
- 17.Saeki N, Rhoton AL., Jr Microsurgical anatomy of the upper basilar artery and the posterior circle of Willis. J Neurosurg. 1977;46:563–578. doi: 10.3171/jns.1977.46.5.0563. [DOI] [PubMed] [Google Scholar]
- 18.Uz A. Variations in the origin of the thalamoperforating arteries. J Clin Neurosci. 2007;14:134–137. doi: 10.1016/j.jocn.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 19.Westberg G. Arteries of the basal ganglia. Acta Radiol Diagn (Stockh) 1996;5:581–596. doi: 10.1177/02841851660050p163. [DOI] [PubMed] [Google Scholar]
- 20.Zeal AA, Rhoton AL., Jr Microsurgical anatomy of the posterior cerebral artery. J Neurosurg. 1978;48:534–559. doi: 10.3171/jns.1978.48.4.0534. [DOI] [PubMed] [Google Scholar]