Abstract
Although very rare, a few cases of intradural extramedullary (IDEM) spinal tumor migration have been reported since Tomimatsu first reported a mobile schwannoma of the cervical cord in 1974. Schwannoma is a neurogenic tumor which originates from nerve sheath that it is relatively well-marginated tumor with little attachment or adhesion to surrounding tissue. Mobility of tumor in spinal canal sometimes can result in negative exploration at the expected area. We found three interesting cases in which different tumor locations observed in repeated magnetic resonance image (MRI) findings. All tumors were intradural and extramedullary schwannoma. We reviewed the literature about moving tumor in the spine through PUBMED search.
Keywords: Intradural extramedullary, Schwannoma, Mobility
INTRODUCTION
Migration of intradural and extramedullary neurogenic tumors has been reported in many countries since 1963; however, there have been a very small number of cases and the incidence has been very rare. The migration of tumors in the spinal canal was also observed at our institute. Therefore, in this report, we document three rare cases with brief literature review. A systemic review of reports about mobile intradural extramedullary (IDEM) spinal tumor through PUBMED search from 1963 to 2008 was done. All of the original articles were rechecked to confirm the moving distance of the tumor, their diagnostic methods and medical records. The most common tumor type among the mobile IDEM tumors was schwannoma, although there have been two reports, one for the neurenteric cyst and one for the ependymoma. Therefore, we excluded non-schwannoma cases in order to focus on the nature and characteristics of the homogeneous schwannoma group.
CASE REPORT
Case 1
Presentation and Examination
A 45-year-old male patient presented with bilateral leg pain which started one year ago and aggravated one month prior to admission. His leg symptom was worsened with positional change and he experienced sleep disturbance due to the pain. There was no motor weakness or sensory change. Bowel and bladder functions were normal. He took magnetic resonance image (MRI) at another hospital, and we checked the enhanced MRI. The preoperative visual analog score (VAS) was 6 for back pain and 10 for leg pain.
Radiologic finding
The MRI from another hospital, which was taken on January 8, 2008, showed an IDEM tumor at the L3-4 level (from L3 mid-body to L4 upper endplate). It was a relatively well-marginated oval mass. The conus medullaris terminated at the T12-L1 disc level. The rechecked MRI showed migration of the tumor up to the L2-3 level (from L2 mid-body level to L3 upper endplate). The tumor was heterogeneous and multi-septated. Some loculations showed cystic change. Enhanced MRI showed strong peripheral enhancement. The approximate size was 16 × 30 mm. There was no calcification within the tumor on simple radiographs or CT scan.
Operation
He underwent a partial laminectomy at L2-3 level for tumor removal on January 15, 2008. After a midline dural incision, the tumor was carefully dissected from the surrounding root and completely removed. The biopsy determined it to be a schwannoma.
Case 2
Presentation and Examination
A 32-year-old male patient visited for his bilateral leg weakness. The symptom developed about one year ago and aggravated recently. He felt radiating pain along the posterior thigh and paresthesia on the bilateral inguinal area. Motor and sensory abnormality was not found. Needle electromyography showed no abnormal finding. We reviewed the MRI which was taken 2 weeks previously at another institution. The preoperative VAS for leg was 8.
Radiologic findings
There was a huge round neurogenic tumor on MRI taken on July 7, 2008. The tumor was a relatively well-marginated IDEM neurogenic tumor located at T10-11 disc level to upper half of T11 body. A long ellipsoidal mass was positioned at the ventral side of thoracic cord. We checked the contrast enhanced MRI. It showed tumor migration to lower half of T11 body level. The tumor was relatively homogenous and its size was 10 × 16 × 20 mm.
Hospital course
During operation, T10 total laminectomy was performed and the tumor was not found, so additional T11 laminectomy was done. The tumor was deeply situated ventral to the cord at lower body level of T11. It was not connected to dural membrane. After resection of dentate ligaments, the cord was mobilized. Cystic bluish well-capsulated mobile tumor was exposed. The mass was attached to somewhat redundant nerve roots at both rostral and caudal ends. The tumor was completely removed. Histological examination revealed it to be a schwannoma. The patient was discharged uneventfully.
Case 3
Presentation and Examination
A 27-year-old male patient visited due to his lower back and leg pain which were started three months ago. Recently, he felt a motor weakness of his right leg. Upon physical examination, there was grade 4 motor weakness of the right ankle and great toe dorsiflexion. A sensory disturbance was found at right inguinal area and along the bilateral L5, S1 dermatome, but autonomic function was intact. The needle electromyography showed increased insertion amplitude along the bilateral tibialis anterior.
Radiologic examination and hospital course
In the preoperative T2-weighted sagittal view, a round tumor mass was located at the L3-4 level (from the lower L3 body to the L3-4 disc level). The tumor size was approximately 14 mm in length and 12 mm in diameter. The content looked relatively homogenous and the tumor was well-enhanced. An L3-L4 laminectomy was done to remove the tumor. According to the operation record, there was no tumor found after the dural incision. The immediate postoperative MRI was checked. Unfortunately, the tumor was up-migrated to the L2 body level. The migration distance was about 40 mm, so L2 hemi-laminectomy and tumor removal were performed at following day. The IDEM tumor was well-encapsulated, dark-reddish and hard in nature. After tumor resection, the preoperative symptoms were much relieved. The biopsy result revealed a schwannoma. The final MRI showed a complete removal of the tumor mass.
DISCUSSION
Tavy el al.9) decribed this type of tumor as 'elusive' tumor. According to their report, there were two cases in which the first operation failed to find the original tumor. One of this study's aims was to avoid unnecessary additional laminectomy or second operation. Several preventive measures were suggested, such as pre-operative repeated MRI or myelography, intra-operative myelography, ultrasonography or even MRI. Intraoperative myelography has a shortcoming that it should be done before dural incision1). Furthermore, injection of dye itself can cause displacement of tumor. Intraoperative MRI can be done only in equipped hospital. Therefore, intraoperative ultrasound seems to be the most convenient diagnostic method to find hidden or moved tumors.
Schwannoma is a neurogenic tumor originating from nerve sheath cell. It is the most common intradural extramedullary neurogenic tumor at spine. In most cases, there are no attachments to dural membrane. Only motion-limitating structures are just two never roots at each end of tumor mass. In the lumbar region, tumor attached to redundant root of the cauda equina gives more chance of mobility in comparison with cervical or thoracic region, where cord exists and allows less space for mobility. Pau et al.7) demonstrated tumor migration according to positional change between Trendelenburg's position and upright position using lipiodol myelography. Preoperative pressure-related symptoms such as pain aggravation by coughing, sneezing and position-related symptom such as pain-easing by lying were described in some articles2,9). Some authors mentioned about intraoperative tumor migration during laminectomy6) or tumor movement up and down in the operative field11). Tomimatsu demonstrated intraoperative movement of a cervical tumor by photographs. Although mechanism of mobility is not definitely proven until now, the mobility of tumors mentioned by most authors appears to be related to intrathecal pressure or spine posture.
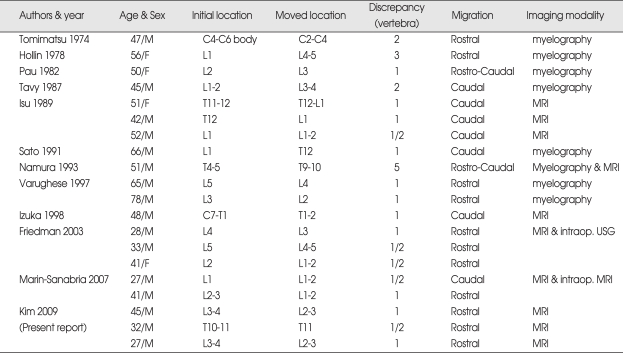
Reported mobile schwannomas from literatures including our three cases are summarized at Table 1. Prevalent sites were lumbar area (65%) where cauda equina exists, but mobility can occur at cervical (5%), cervicothoracic (5%), thoracic (10%) cord region or thoracolumbar junction (15%). According to the data, the sex ratio of males to females was 16 : 4. The migrated location and distance were retrieved from figures of next myelography, MRI or intraoperative ultrasound, if there was no exact description in the content of article. Rostral (60%) or caudal (30%) and even with to-and-from (10%) motion were all observed. Migration distance was most commonly within one level vertebral distance (80%). Maximum of five level vertebral distance was also reported at thoracic cord lesion6). There was tumor migration even up to cervical C2-3 cord level by two level vertebral distance10).
Table 1.
Summary of published cases of mobile schwannomas in the spine
MRI : magnetic resonance image
CONCLUSION
Though unusual, IDEM tumor has tendency to move within spinal canal. Therefore, spine surgeons must always aware of the possibility of mobility. To prevent unnecessary additional laminectomy or secondary operation, intraoperative myelography before dural incision is considered to be one of the easy and useful detection methods; ultrasound or MRI also can help to find hidden or moved tumor.
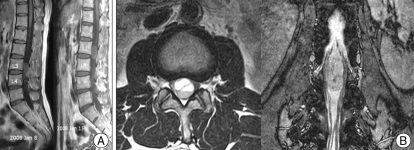
Fig. 1.
Magnetic resonance (MR) image of the first case. A : Outside T1-weighted sagital view shows mass lesion at L3-4 level. However, rechecked MR image shows mass upmigrated at L2-3 level. B : In T2 axial image, some portion of tumor show cystic change with septum formation. MR myelography showing intradural extramedullary location.
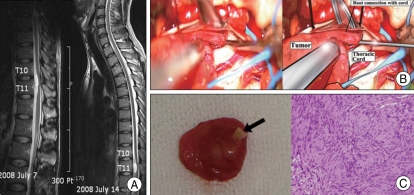
Fig. 2.
Magnetic resonance (MR) image of the 2nd case. A : MR image taken at another hospital shows mass lesion at T10-T11 disc level to upper portion of T11 body. Rechecked MR image shows mass migration caudally to lower portion of T11 body. Tumor is located to ventral side of thoracic cord. B : Intraoperative tumor exposure with some root attached to it. C : Gross : Excised tumor mass with some remnant of nerve root connection (black arrow). Microscopic view (H&E staing, ×40) : Moderate cellularity with cell elongation. The typical finding of Antoni A area is noted.
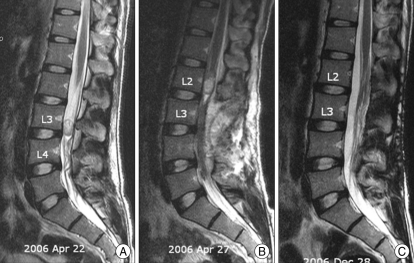
Fig. 3.
Magnetic resonance (MR) image of the 3rd patient. A : Preoperative T2-weighted sagittal MR image shows round mass at the L3-4 level. B : But, immediate postoperative MR image shows tumor migration up to the L2 body level. C : After repeated surgery, tumor is completely removed at the final MR image.
Acknowledgements
The authors thanks to pathologist, Sung Suk Paeng, M.D. for her kind cooperation and nice and delicate comments on pathologic findings, and Mr. Kim Ho for editing service and Je Min, Son for illustration.
This study was supported by a grant from the Wooridul Spine Foundation.
References
- 1.Friedman JA, Wetjen NM, Atkinson JL. Utility of intraoperative ultrasound for tumors of the cauda equina. Spine. 2003;28:288–290. doi: 10.1097/01.BRS.0000042271.75392.E4. discussion 291. [DOI] [PubMed] [Google Scholar]
- 2.Hollin SA, Drapkin AJ, Wancier J, Huang YP. Mobile schwannoma of the cauda equina. Case report. J Neurosurg. 1978;48:135–137. doi: 10.3171/jns.1978.48.1.0135. [DOI] [PubMed] [Google Scholar]
- 3.Iizuka H, Iida T, Akai T. Mobile neurinoma of the cervicothoracic junction. Surg Neurol. 1998;50:492–493. doi: 10.1016/s0090-3019(98)00125-6. [DOI] [PubMed] [Google Scholar]
- 4.Isu T, Iwasaki Y, Akino M, Nagashima M, Abe H. Mobile schwannoma of the cauda equina diagnosed by magnetic resonance imaging. Neurosurgery. 1989;25:968–971. doi: 10.1097/00006123-198912000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Marin-Sanabria EA, Sih IM, Tan KK, Tan JS. Mobile cauda equina schwannomas. Singapore Med J. 2007;48:e53–e56. [PubMed] [Google Scholar]
- 6.Namura S, Hanakita J, Suwa H, Mizuno M, Ohtsuka T, Asahi M. Thoracic mobile neurinoma. Case report. J Neurosurg. 1993;79:277–279. doi: 10.3171/jns.1993.79.2.0277. [DOI] [PubMed] [Google Scholar]
- 7.Pau A, Orunesu G, Sehrbundt Viale E, Turtas S, Zirattu G. Mobile neurinoma of the cauda equina. Case report. Acta Neurochir (Wien) 1982;60:115–117. doi: 10.1007/BF01401756. [DOI] [PubMed] [Google Scholar]
- 8.Satoh T, Kageyama T, Kamata I, Date I. [Mobile neurinoma of the cauda equina; a case report] No Shinkei Geka. 1991;19:891–896. [PubMed] [Google Scholar]
- 9.Tavy DL, Kuiters RR, Koster PA, Hekster RE. Elusive tumor of the cauda equina. Case report. J Neurosurg. 1987;66:131–133. doi: 10.3171/jns.1987.66.1.0131. [DOI] [PubMed] [Google Scholar]
- 10.Tomimatsu T, Yanamura I, Kawaguchi N, Fujii K, Isobe Y. A mobile tumor of the cervical spinal cord. A case report. Kantoh Seisaisi. 1974;5:213–218. [Google Scholar]
- 11.Varughese G, Mazagri R. Mobile tumours in the lumbar spinal canal : a diagnostic problem. Can J Surg. 1997;40:59–63. [PMC free article] [PubMed] [Google Scholar]