Abstract
While a wide variety of approaches to engineering orthopedic tissues have been proposed, less attention has been paid to the interfaces, the specialized areas that connect two tissues of different biochemical and mechanical properties. The interface tissue plays an important role in transitioning mechanical load between disparate tissues. Thus, the relatively new field of interfacial tissue engineering presents new challenges—to not only consider the regeneration of individual orthopedic tissues, but also to design the biochemical and cellular composition of the linking tissue. Approaches to interfacial tissue engineering may be distinguished based on if the goal is to recreate the interface itself, or generate an entire integrated tissue unit (such as an osteochondral plug). As background for future efforts in engineering orthopedic interfaces, a brief review of the biology and mechanics of each interface (cartilage–bone, ligament–bone, meniscus–bone, and muscle–tendon) is presented, followed by an overview of the state-of-the-art in engineering each tissue, including advances and challenges specific to regenerating the interfaces.
Introduction
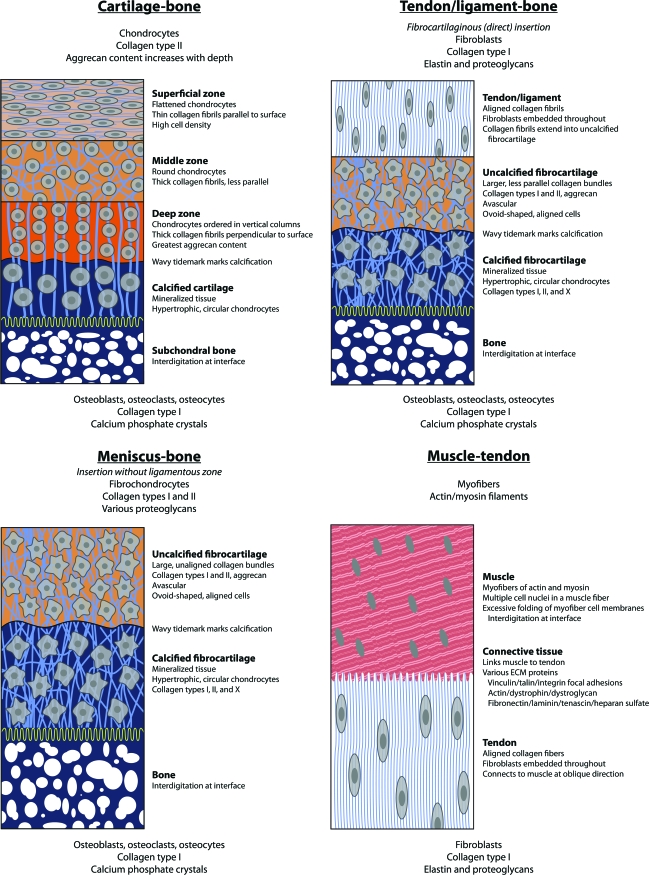
Recent advances in tissue engineering have led to a myriad of therapeutic approaches for a variety of orthopedic diseases and injuries. However, much less work has been done to engineer orthopedic tissue interfaces. Interfaces bridge the gap between two dissimilar tissues, usually with physical and biological properties that separate them from the tissues they connect. Interfaces in orthopedics are crucial in that they transfer load between bone, cartilage, tendon, ligament, and muscle tissue1 and therefore are required to restore full patient function after the application of tissue engineering strategies to regenerate these tissues. A gradual transition in mechanical properties may reduce stress concentrations at the interface, preventing failure.1 In light of these mechanical considerations, the interfaces have unique biochemical compositions that are distinguishable from both tissues they connect. Many utilize a shift in extracellular matrix (ECM) composition while maintaining ECM continuity to allow for repeated and durable load transfer.1 These biochemical and mechanical design parameters present the field of regenerative medicine with a new challenge—not only to create homogeneous tissues, but also to develop methods and techniques for linking different tissues together. Figure 1 provides an overview of the cartilage–bone, tendon/ligament–bone, meniscus–bone, and muscle–tendon interfaces.
FIG. 1.
A diagram depicting the cartilage–bone, tendon/ligament–bone, meniscus–bone, and muscle–tendon interfaces and their compositions. In the color version of this figure, orange indicates levels of aggrecan concentration, light blue indicates collagen fibers, while dark blue indicates mineralized tissue. Red indicates muscle fibers. Gradients of matrix composition, interdigitation of tissue zones, and interconnecting collagen fibers all enable load transfer between disparate tissues. Color images available online at www.liebertonline.com/ten.
Approaches to interfacial tissue engineering may be distinguished based on if the goal is to engineer the interface itself, or generate an entire integrated tissue unit (such as an osteochondral plug). In both cases, an interface is developed, but tissue engineering–related considerations of scaffold, cell source, bioactive factors, and other stimuli are affected by the overall design paradigm. Accordingly, we present a synopsis of current knowledge in the areas of cartilage–bone, tendon/ligament–bone, meniscus–bone, and muscle–tendon interfaces as background for future efforts in engineering orthopedic interfaces. A summary of the biology and mechanics of each tissue, as well as the interfaces themselves, is provided. Additionally, a review of the state-of-the-art in engineering each tissue is included, and current advances and challenges specific to regenerating interfaces are highlighted.
Cartilage–Bone
Tissue properties
The cartilage–bone interface, otherwise known as the osteochondral interface, has been most extensively studied in orthopedics due to the rising demand for new therapies to diseases such as osteoarthritis, which causes degeneration of hyaline cartilage. In 2008, 27 million people in the United States suffered from clinical osteoarthritis.2 Structurally, the osteochondral interface is the interface between a layer of hyaline cartilage and underlying bone. Hyaline cartilage is a dense, avascular, connective tissue that provides smooth articular surfaces for joint motion and is found at all joints.3 Cartilage can be further distinguished into three zones—the superficial, middle, and deep zones. The superficial zone lies at the joint surface, the deep zone connects to the calcified cartilage zone (and subsequently, subchondral bone), and the middle zone lies between these two.3–5
Biochemically, cartilage tissue is largely comprised of water, chondrocytes (1–10%), type II collagen, and the aggregating proteoglycan aggrecan.3–5 Each zone is defined by a particular composition and organization of cells and ECM molecules.6 However, in all areas of the tissue, collagen fibrils form a dense, highly interconnected matrix. Within this matrix, aggrecan, a highly glycosylated molecule with net negative charge, is bound in large numbers to hyaluronic acid chains to form proteoglycan aggregates. These aggregates raise the osmolarity of the tissue, which triggers an influx of water. The resultant swelling is countered by the resistance of the collagen matrix, generating a large internal pressure and giving cartilage its unique mechanical properties.3 Each zone in cartilage exhibits a characteristic makeup and organization of cells and ECM components. The superficial zone is characterized by flattened chondrocytes and thin collagen fibrils that are parallel to the articulating surface.5 Cell density is at its highest point in this zone.5 In the middle zone, chondrocytes are round in shape, and collagen fibrils are larger in diameter and less parallel.3,5 In the deep zone, both chondrocytes and fibers are organized perpendicular to the articular surface, with chondrocytes ordered in vertical columns.3,7 Collagen fibril diameter is maximal in this region, but collagen content is also at its lowest.5 Across all three zones, aggrecan concentration greatly increases with tissue depth.8
The differential proportions in ECM composition, as well as the arrangement of those components, significantly influence the mechanical properties of each section of the tissue. For example, the superficial zone is strong in tension along the alignment of its collagen fibrils, which assists the tissue in resisting shear at the surface.5,7 Over the depth of the tissue, the deep zone is over an order of magnitude stiffer in compression relative to the superficial zone.6
Bone is a complex tissue designed to provide mechanical support to the body. Briefly, bone tissue can be separated into trabecular and cortical bone types. Trabecular bone is approximately 80% porous.9 It is filled with marrow, which is involved in generation of red and white blood cells, and is characterized by plates or struts called trabeculae.9 In contrast, compact bone is dense and characterized by cylindrical elements called osteons (also known as Haversian systems) surrounded on both sides by inner and outer circumferential lamellae.9 Bone tissue can also be characterized as primary or secondary, with secondary bone arising from active bone resorption and subsequent replacement with new bone.9 Three cell types exist within cortical bone: osteoclasts resorb bone, osteoblasts produce calcified tissue, and osteoblasts eventually become osteocytes, which continue to assist in calcification of the matrix in which they are encased.9 Bone primarily consists of water, collagen type I, and hydroxyapatite crystals, which provide the tissue's stiffness and compressive strength.9
The osteochondral interface describes the interaction of calcified cartilage and the subchondral bone underneath. Structurally, collagen fibers extend from the deep zone to calcified cartilage through a wavy tidemark, marking calcification, that dissipates forces through the vertical orientation of collagen fibrils.10 Endochondral ossification (tissue calcification) continues in calcified cartilage throughout a person's lifetime.10 However, even though calcified cartilage is mineralized tissue, its mechanical strength is still an order of magnitude lower than that of the subchondral bone beneath it.11 Subchondral bone can be classified into two types: immediately below the cartilage lies the cortical bone, with low porosity and vascularity, followed by subchondral trabecular bone further beneath, which contains trabeculae oriented in random directions.8 Calcified cartilage is interdigitated with subchondral bone, but fibers do not extend across the zone into the bone.10,12 These interdigitations presumably provide for tighter adherence at the interface, eliminating lateral tissue strain. It is proposed that this reduces the possibility of cartilage cracking in this area.13 The wavy tidemark and vertically oriented fibers at the tidemark, as well as interdigitations present at the interface, may allow for reduction of stress concentrations as well as better integration with the underlying bone.10
Each zone of tissue contains significantly different mechanical properties: the compressive modulus varies on orders of magnitude between each zone. The approximate moduli of the superficial zone, deep zone, calcified cartilage, and subchondral bone are 0.079, 2.1, and 320 MPa, and 5.7 GPa, respectively.6,11 Given the complexity of the biology and mechanics of this interface, the challenges for osteochondral tissue engineering include developing a low-friction surface that integrates with surrounding cartilage tissue, ensuring proper integration with surrounding tissues and maintaining the mechanical properties of the implant.
Current tissue engineering approaches
With those challenges in mind, a number of methods are currently being developed to mimic the complete osteochondral interface. This section will focus on summarizing advances in osteochondral tissue engineering; the reader is encouraged to see other reviews for more information on tissue engineering of either bone or cartilage as a single tissue.14–17 It is important to note that in most of the current methods, formation of the interface tissue itself is generally a by-product, rather than a conscious aim of the approach. Instead, the focus for the osteochondral interface is in recreating a replacement tissue unit (osteochondral plug).
Four current approaches to scaffold design for osteochondral tissue engineering have been outlined: first, a scaffold designed for bone and a scaffold-free approach for cartilage; second, separate bone and cartilage scaffolds that are combined at implantation; third, a heterogeneous composite scaffold; and fourth, a homogeneous composite scaffold.18 Generally, scaffold types can be divided into two categories—either derived from hydroxyapatite or derived from synthetic/natural polymers. Hydroxyapatite and calcium phosphate–derived scaffolds exhibit high mechanical strength and offer excellent bone integration.18 However, typical implantation uses multiple cylindrical plugs to fill irregular cartilage defects, which leads to limited integration and increased contact pressures due to nonuniformity in the articular surface.18 Synthetic and natural polymers are comparatively weaker materials, but offer the advantage of adaptability to various defect geometries through a variety of molding and casting techniques.18 Once the scaffold is chosen, it can be loaded with a combination of cells with chondrogenic and/or osteogenic capacity, or simply nothing at all.18 Finally, constructs can optionally undergo additional in vitro conditioning, with additional bioactive factors and/or mechanical stress, before in vivo implantation.18 The summary below reflects this diversity in approach—each study uses its own cocktail of scaffold, cell source, and additional stimuli in engineering the osteochondral interface. Given the myriad of possibilities, the scaffold seems to represent the main differentiating factor between techniques.
Hydroxyapatite or its derivatives (including natural bone matrix) are the most popular components chosen for the osseous layer.19–21 Due to bone's intrinsic repair ability, as well as its capacity to infiltrate and remodel hydroxyapatite scaffolds, osteogenic cells are typically not required.18 Usually, however, hydroxyapatite is linked with a separate scaffold to replicate the avascular cartilage layer.18 Natural components such as chitosan, gelatin, and collagen have previously been employed for the cartilage portion.22–24 Some studies have also been performed using stem cells and hyaluronic acid scaffolds.25–27 In one approach, researchers stimulated rat MSCs with transforming growth factor-β1 (TGF-β1), and then encapsulated them in a hyaluronic acid sponge on top of a hydroxyapatite/calcium phosphate layer.26 After subcutaneous implantation, results demonstrated fibrocartilage tissue in the sponge, with bone tissue noted in the ceramic component. A subsequent experiment replaced the bony layer with injectable calcium phosphate in a rat medial femoral condyle implantation study.27 Results at 12 weeks indicated zonal areas of growth in addition to good integration with surrounding cartilage. Columnar arrangements of chondrocytes were seen, along with a calcified cartilage layer in some specimens. Although no significant differences in staining for ECM were observed, replacement tissue in cell-free controls appeared to display reduced cell density and increased surface irregularity.27 However, another investigation underlines the importance of eliminating possible immunogenic responses. In one 52-week experiment with a cell-free dual layer bovine collagen I/III–calcium phosphate scaffold, the collagen layer failed to show significant cellularity near the articular surface, likely due to immunogenic reaction to the bovine collagen.28
Hydroxyapatite and related ceramics have also frequently been used in tandem with synthetic polymers.29 The family of poly-L-lactide (PLLA), poly-D,L-lactide (P(D,L)LA), poly(DL-lactic-co-glycolide) (PLGA), polylactic (PLA), and polyglycolic (PGA) acid has been most extensively studied, due to the ability to tailor the specific chemical properties of the resulting network, including biodegradation time.30–33 Results have varied widely depending on the particular formulation of polymer and ceramic. One experiment demonstrated good cartilage integration at 12 weeks with a hybrid acellular calcium phosphate/PLLA scaffold incorporating basic fibroblast growth factor (bFGF).32 Another study implanted a biphasic PLGA/calcium phosphate construct into mini-pigs for 6 months. Histology revealed excellent bone integration and a tidemark noted between cartilage and bone, with the chondral phase of all samples producing mineralization near the tidemark. However, integration with surrounding cartilage tissue was poor.33
Solid free-form (SFF) fabrication is a new technology that has been used with some success to create custom geometry calcium phosphate–based scaffolds using a liquid binder, thus bypassing traditional limitations to calcium phosphate matrices.34–39 One experiment used a proprietary SFF method with sodium chloride and tricalcium phosphate as the solid components.34 The fabrication process was also instructed to form a gradient between the 55% porous bone component and a 90% porous, PLA/PLGA component for cartilage ingrowth; chondrocytes preferentially populated the 90% porous layer and deposited ECM over 4 weeks in vitro.34 Another procedure using SFF fabrication methods developed a separate hydroxyapatite scaffold, with a porous PLA scaffold pressed onto the hydroxyapatite layer. PLA rods were required to stabilize the adhesion between the two layers.35 After seeding with fibroblasts in the hydroxyapatite layer and chondrocytes in the PLA layer, the constructs were subcutaneously implanted in mice. Microcomputed tomography demonstrated a mineralized cartilage layer at the interface after 4 weeks in vivo.35
In contrast to the previous studies, some methods forego the cartilage scaffolding component entirely, simply culturing cells on top of a ceramic scaffold, with promising results.40,41 One investigation seeded ovine chondrocytes on top of a porous calcium phosphate scaffold, culturing the cells for 8 weeks in vitro before implanting them in sheep for up to 9 months. Generated cartilage tissue integrated well with surrounding cartilage, and bone tissue grew into the scaffold. Moreover, as measured by compression testing, a significant increase in equilibrium elastic modulus was reported at 3 and 9 months after implantation. However, there was no difference noted between samples at 3 and 9 months.40
Other approaches do not use hydroxyapatite-based scaffolds at all, but instead employ purely synthetic or natural polymers.31,42–47 One study utilizing natural polymers molded anatomically shaped constructs using a bovine-chondrocyte–loaded agarose gel and a demarrowed bovine trabecular bone substrate. After 2 weeks in vitro, researchers reported tight integration with the bone substrate, increased glycosaminoglycan (GAG) content, and increased aggregate modulus relative to the initial time point.42 In another use of natural matrices, a fibronectin-coated hyaluronic acid scaffold was infiltrated with rat bone marrow, and then implanted in rabbit osteochondral defects for 24 weeks.43 Histology revealed a layer of cartilage on the surface that integrated well with surrounding cartilage tissue; no histological difference was found between scaffolds seeded with or without bone marrow at any time point. However, the researchers concluded that bone marrow loading appeared to expedite the initial repair process.43
Synthetic polymers that have been explored for osteochondral tissue engineering include PLLA and polyethylene glycol (PEG) as along with their derivatives.31,44–47 One strategy seeded either side of a P(D,L)LA scaffold with MSCs for cartilage or osteogenically induced MSCs for bone, and then cultured the entire scaffold in a specialized medium designed to maintain osteogenic and chondrogenic phenotypes for up to 10 weeks.44 Staining for sulfated GAG (Alcian blue) content, as well as aggrecan, collagen type II, and proteoglycan link protein, all markers of cartilage tissue, exhibited heavy staining in the cartilage layer, with a gradient in staining at the interface. However, staining for bone sialoprotein and collagen I, both markers of bone tissue, revealed a sharp demarcation at the interface.44 In studies using photopolymerizable PEG, separate layers containing MSCs precultured in osteogenic media and chondrogenic media were polymerized sequentially using long-wave UV light and implanted subcutaneously in immunodeficient mice. Although neither component matched the mechanical properties of native tissue, scaffold stiffness increased, and both layers demonstrated specific markers for their respective tissues.46 Finally, oligo(poly(ethylene glycol) fumarate) (OPF), a hydrolyzable PEG derivative, has been used to fill cartilage defects in a rabbit medial femoral condyle model.47,48 OPF was supplanted with gelatin microparticles containing TGF-β1 and cross-linked in situ. After 14 weeks, the initially acellular polymer matrix had been infiltrated by cells and degraded, with trabecular bone tissue in the bone layer, and hyaline cartilage-like tissue in the cartilage layer.47
Design considerations for osteochondral tissue engineering
Particular sets of experiments have underlined the importance of properly altering material composition to ensure more effective healing. In one study, four different implants were seeded with autologous chondrocytes—all were PLGA-based for the cartilage layer, but included PLGA, bioactive glass, or calcium sulfate in the bony layer. It was found that stiffer materials in both layers promoted increased healing in Spanish goats.30 Thus, matrix mechanical properties may play a role in ensuring proper integration. Great care should also be taken to properly tailor the degradative properties of PLLA-based scaffolds. In a separate in vitro experiment, some of the PLLA scaffolds utilized in the bioreactor study degraded by 15 weeks, leading to scaffold collapse.31 This work highlights the necessity of tuning scaffold degradability to allow for sufficient tissue replacement, which can assist in improving mechanical properties. Overall, the mechanical strength and integrity of both bone and cartilage layers of the implant can affect long-term implant stability and tissue healing.30,31
Another salient issue in osteochondral tissue engineering is long-term fusion with native cartilage tissue; results seem to vary widely from study to study. For example, one procedure first cultured chondrocytes in PGA scaffolds, and then sutured the scaffold together with a commercial scaffold composed of calcium phosphate, hydroxyapatite, and collagen shortly before implantation.22 Results after 6 months showed good integration with bone tissue and regeneration of the tidemark between cartilage and bone, but indicated little fusion with native cartilage.22 Without proper integration, the articular surface may be prone to instability and failure.18,22 This remains a future challenge for osteochondral constructs, as integration of the cartilage layer will be required for the overall success of any approach.
An additional area of integration to be considered in osteochondral tissue engineering lies at the cartilage–bone interface with the calcified cartilage zone. Although many published studies have demonstrated a region of calcified cartilage, this region has traditionally been considered less of a priority in osteochondral tissue engineering. However, the emerging importance of creating a transition in mechanical properties has generated experiments that specifically examine the calcified cartilage zone. One investigation of this kind specifically isolated chondrocytes from the deep zone of bovine articular cartilage and cultured them on a calcium phosphate scaffold.49 After 8 weeks of culture in 10 mM β-glycerophosphate, engineered tissues showed a calcified cartilage region, with an uncalcified region at the surface of the tissue. Shear mechanical testing revealed that tissues with a calcified region (i.e., cultured in β-glycerophosphate) exhibited much higher resistance to shear forces than scaffolds not cultured in β-glycerophosphate; however, the shear strength was still an order of magnitude less than native tissue.49
Summary and future challenges
From these studies, there is limited consensus on tissue engineering of the osteochondral interface, but many researchers agree that the basic presence of a scaffold may be sufficient for bone tissue infiltration and remodeling. Calcium phosphate–based scaffolds have been preferred for the bone component due to greater mechanical properties compared to pure polymeric matrices, although synthetic and natural polymers have also demonstrated success as scaffolds. General agreement has not yet been reached on the type of cells or scaffold that is most optimal for cartilage regeneration. However, an important challenge for the future is to ensure integration with native cartilage tissue, as well as appropriately modulating scaffold stiffness and degradative properties for mechanical stability and tissue regeneration. Of the literature reviewed, it is also clear that the eventual goal of osteochondral tissue engineering is to replicate the zonal structure of cartilage; initial results indicate that a calcified cartilage zone may greatly assist in resisting commonly experienced forces such as shear.
Tendon/Ligament–Bone
Tissue properties
While most attention in interfacial orthopedic tissue engineering has focused on the formation of osteochondral constructs, the tendon/ligament–bone interface has been explored more recently.50 Tendons and ligaments are responsible for linking the musculoskeletal system; tendons transfer loads between muscles and bones, while ligaments bind bone to bone to restrict their motion.9 Ligaments are especially necessary in the knee, which, as an inherently unstable joint, relies on ligaments such as the anterior cruciate ligament (ACL) and the medial collateral ligament (MCL) to restrict tibiofemoral motion and maintain joint stability.9,51 The aligned organization of collagen fibers gives tendon and ligament its characteristic hierarchical structure. Collagen fibers assemble to form microfibrils (4 nm diameter), which further aggregate to form subfibrils (20 nm) and fibrils (50–500 nm). Collagen fibrils are organized along with fibroblasts to form fascicles. Finally, multiple fascicles form a whole tendon or ligament. Electron microscopy has shown that collagen fibers in tendon and ligament display a wavy crimp structure without load.9,51–53 Biochemically, the main components of tendon and ligament tissue include collagen (primarily type I), elastin, and proteoglycans.9 In both ligament and tendon, proteoglycans (including decorin, biglycan, fibromodulin, lumican, aggrecan, and versican) comprise 1–3% of the overall dry weight; ligament tissue generally contains 10–15% elastin, whereas tendon contains less than 3%.9
Mechanically, the crimp structure of collagen fibers in tendon and ligament permits small deformations without actual tissue tension and can be seen in the stress–strain curve of tendon/ligament tissue, which displays a toe region at low deformations.52,53 When under deformation, the alignment of individual collagen fibers gives tendons/ligament its extremely high tensile strength.9
Insertions of tendon or ligament into bone vary considerably depending on the particular attachment. However, insertions can generally be characterized as either direct or indirect.54 From a histological viewpoint, indirect and direct insertions are also known as fibrous or fibrocartilaginous entheses, respectively.55 One example of a fibrous enthesis (indirect insertion) is the tibial insertion of the MCL.56 In fibrous insertions, a tendon or ligament attaches at acute angles to the bone through Sharpey's fibers, collagen fibers that extend directly through to the bone. On the other hand, fibrocartilaginous entheses, or direct insertions, are also found; one example is the femoral insertion of the MCL.56 Generally, this type of tendon/ligament–bone insertion is characterized by a transition zone of four general types of tissue. The first zone is fibrous connective tissue, generally similar to normal tendon/ligament. This tissue contains aligned collagen fibrils with fibroblasts embedded throughout the collagen matrix. Collagen fibrils insert from this zone into the next zone, uncalcified fibrocartilage. Here, collagen fibril bundles are larger and less parallel than in the first region. Type II collagen and aggrecan are found in this matrix. This zone is relatively avascular, with ovoid-shaped, aligned cells. A tidemark has been found separating uncalcified fibrocartilage and the next zone of calcified fibrocartilage.55 Calcified fibrocartilage contains hypertrophic, highly circular chondrocytes, with collagen X found only in this region.1 Between the calcified fibrocartilage and the fourth zone, bone, there is an interlocking region of tissue interdigitation, providing secure attachment between tissues.1,55 Bone tissue, as reviewed earlier, contains osteoblasts, osteoclasts, and osteocytes, with mineralized collagen I fibers. Collagen type II is not present.1
The mechanics of the interface involve two materials of vastly different mechanical properties; tendons and ligaments are very strong in tension, while bone is optimized for compressive loading.9,57 Without a gradual transition in mechanical properties, as in indirect/fibrous insertions, stress concentrations may form at regions where two materials of significantly different mechanical properties are joined.1 However, in fibrocartilaginous (direct) insertions, uncalcified and calcified fibrocartilage tissues at the interface are superior in transferring compressive load, and the insertion site shows an increase in Young's modulus across the transition.1,50 Thus, fibrocartilaginous insertions provide the transitional zones of tissue to bridge the gap between the mechanical properties of ligament and bone.58
As with the cartilage–bone interface, engineering of the tendon/ligament–bone interface requires strategies that ensure mechanical stability. Additionally, design constraints must also be applied based on the overall approach to insertion point regeneration. In general, work in this area can be divided based on whether the objective is to build an entire composite tissue unit (e.g., formation of a tissue-engineered bone–ligament–bone graft), or whether the objective is to assist in recreating individual interfaces, such as improving integration of autografts with surrounding bone. Most current work in interface engineering has focused on assisting graft anchorage.1 Because approaches to interface repair can be based on tendon/ligament tissue engineering, an overview of the state of the art in tendon/ligament regeneration is provided, followed by a discussion of the means explored to recreate the insertion points. This is not meant to be an exhaustive review of tendon/ligament tissue engineering; please see other reviews1,53,59 for more in-depth discussion.
Current tissue engineering approaches
In tendon/ligament tissue engineering, silk, collagen, and the PLLA family of synthetic polymers are the most widely explored scaffolds, while MSCs and tendon/ligament fibroblasts are typically chosen as cell sources.53,59 It has been proposed that MSCs may be an optimal cell source due to their increased proliferation rates and increased collagen deposition.60 After the choice of a proper scaffold and cell source, additional growth factors can be added to either MSC or fibroblast-populated scaffolds to induce further ECM deposition, such as TGF-β, insulin growth factor-1, platelet-derived growth factor, and bFGF.61
Because tendon/ligament tissue is primarily composed of collagen type I, collagen gels have been widely explored as scaffolds for engineering ligament tissue.59 Although many studies report success with cell infiltration, tissue ingrowth, and enhanced mechanical strength, most attempts do not generate matrices with mechanical properties similar to native tendon/ligament tissue.59,62–66 Some studies, however, have produced scaffolds with mechanical properties similar to ligament. One experiment reported elastic moduli similar to native ligament tissue after 20 days in culture, with the presence of cells increasing construct peak stress.67
Thus, due to the overall issues with collagen gel mechanical strength, many researchers use fibers or hydrophobic scaffolds. One natural material that has been widely explored is silk; silk fibers can be woven into a rope-like structure and have been tailored to match the stiffness of normal tendon/ligament tissue without reduction of ultimate tensile strength.59,68,69 After seeding on these fibers, MSCs demonstrated proliferation and ECM secretion over 14 days in culture.69 Scaffolds using synthetic polymers, typically PLLA and PGA, have also been utilized in tendon/ligament tissue engineering.53,70–75 Like silk, several studies have woven PLLA fibers into 3D braids.53,70,71,73,75 The 3D braiding technique, along with the use of PLLA, allows for close control of mechanical properties, pore sizes, degradation properties, and overall geometry; a single braid can contain both a porous intraarticular zone and less porous bony attachment zones.73
Some groups have established multiphase matrices to engineer the tendon/ligament–bone insertion point.76–79 In two recent experiments, three distinct scaffolding phases were formed (one for ligament, bone, and a fibrocartilage interface) using mixtures of PLGA and bioactive glass. A study with bovine fibroblasts and osteoblasts seeded on either side of the middle phase demonstrated cells migrating into the middle layer.77 The subsequent subcutaneous implantation in athymic rats using a triculture of bovine fibroblasts, chondrocytes, and osteoblasts revealed the development of a fibrocartilaginous layer, with collagen type X observed between the fibroblast and chondrocyte layer; mineralization was confined to the osteoblast layer.78 Another approach involved modification of a collagen scaffold with a gradient of retrovirus encoding the osteogenic transcription factor Runx2.80 These scaffolds were then seeded with dermal fibroblasts to create a single construct with heterogeneous cell phenotype and biochemical properties, including mineralized matrix deposition from cells undergoing osteoblastic differentiation. Constructs maintained their heterogeneity even after ectopic implantation in vivo.80 These investigations indicate the potential of using tissue engineering principles to create zonal tissues that resemble the mechanical and biochemical properties of the native tendon/ligament interface. Further, this platform could be expanded to regenerate an entire tissue unit, much like the approaches to developing osteochondral tissue plugs described in the previous section.
Other tissue engineering techniques have focused instead on recreating an interface between an existing graft and bone. These methods are designed to assist current means of ligament and tendon reconstruction after injury, especially for ACL defects. The current accepted standard for ACL replacement is autologous ligament transplantation, where an existing autologous tendon is removed during surgery and used to replace the torn ACL. The surgery is performed using either the central third of the patellar ligament or the gracilis and semitendinosus (hamstring) tendons with fairly similar outcomes regardless of the graft tissue used.81–85 To perform the surgery, bone tunnels are drilled into the tibial and femoral heads and the tendon is affixed inside each tunnel with a metal fastener or degradable PLLA screw, the type of which can greatly affect graft success rates.86,87 The screw effectively pins the tissue against the side of the bone tunnel, generating a tight fit. Depending on the patient, bone–ligament–bone transplants have also been performed.88 Results within the bone tunnel have largely been positive, with Sharpey's fibers typically noted at the ligament–bone interface.89,90 Clinical research strongly indicates, however, that restoration of a zonal insertion site, with regions of uncalcified and calcified fibrocartilage, is the optimal outcome.91,92
Consequently, tissue engineering paradigms have recently been applied to bone tunnel healing to increase the mechanical strength of the interface, often by generating an insertion site similar to that of a direct, fibrocartilaginous insertion. In some studies, natural materials have been used. One approach used autologous periosteal tissue to envelop rabbit bone tunnel tendon grafts. At 8 and 12 weeks, a fibrocartilaginous zone was observed at the interface, and maximal failure load significantly increased at 8 and 12 weeks.93 A later investigation, similar in concept, used fibrin glue to wrap MSCs around hamstring tendon autografts during ACL reconstruction in rabbits. After 8 weeks, distinct zones of tendon, uncalcified fibrocartilage, calcified fibrocartilage, and bone were observed in experimental samples, with extensive collagen type II staining in the fibrocartilaginous region and cells arranged in columns perpendicular to the tidemark. In contrast, control grafts without MSCs showed Sharpey's fibers, but no collagen II staining or other indications of fibrocartilaginous tissue. MSC-enhanced grafts also displayed higher failure load and higher stiffness than MSC-untreated controls.94
Promising work has also recently been demonstrated using synthetic materials. One study constructed a graft comprised of two PLLA 3D braids on either side of a bFGF-releasing gelatin hydrogel. The entire construct was then wrapped with a collagen membrane before subsequent implantation in bone tunnels in rabbits. This cell-free approach induced cell migration and bone formation into the tunnel, as well as cell migration in and around the intraarticular braid. Increased failure load and stiffness compared to controls without bFGF or the collagen membrane were also reported. However, grafts failed after 8 weeks due to overall lack of integration with the bone tunnel.95 This underlines the importance of ensuring proper biological fixation. In a separate strategy intended to recreate interface fibrocartilage, a contractile PLGA nanofiber mesh with a PLGA/bioactive glass collar was employed. After wrapping the mesh and collar around explanted bovine tendons for 2 weeks to induce compression, results indicated upregulation of fibrocartilage-related genes.79 Such a device could potentially be deployed in situ in a bone tunnel to assist in rebuilding the native interface from ligament to bone.
The growth factor bone morphogenetic protein 2 (BMP-2) has also been used to stimulate tendon/ligament–bone interface healing.96–98 One study covalently linked BMP-2 to hyaluronic acid and blended the tethered BMP-2 with a photopolymerizable PEG hydrogel solution containing periosteal progenitor cells,97 subsequently polymerizing the solution at the tendon–bone insertion in rabbits. After 12 weeks in vivo, a fibrocartilaginous interface and higher pullout strength was observed.97 Another study retrovirally infected autologous semitendinosus tendons ex vivo with a gene expressing BMP-2 and monitored graft outcomes through 8 weeks in rabbits.98 Although gene expression of BMP-2 by graft cells lasted only through 6 weeks, a four-zonal interface region was generated, along with significantly greater failure load and stiffness at 8 weeks.98
Summary and future challenges
From the approaches explored above, it is clear that the design methodology depends on the desired therapy objectives. Several studies have recognized the importance of generating proper interface tissue after graft fixation to improve implant success. A major future challenge in this area is the development of the optimal scaffold, cell source, and extracellular stimuli to recreate the zonal, fibrocartilaginous tissue that bridges tendon/ligament and bone. Addressing this issue may require the development and linkage of separate homogeneous components, or, alternatively, the presence of continually gradiated scaffold properties may remove this need by providing heterogeneity in a single construct. Solutions for recreating the interface can improve surgical outcomes in bone tunnel healing during autologous transplantation. Finally, accumulated knowledge will guide expanding efforts in generating whole tissue units, such as a bone–ligament–bone substitute, that can be implanted in the place of current auto- or allograft transplants.
Meniscus–Bone
Compared to the cartilage–bone and ligament–bone interfaces, less work has been completed in the area of meniscus–bone interface tissue engineering. However, increasing attention to meniscus tissue engineering in recent years suggests that this interface may become an important topic of future study.99–103 Accordingly, a brief review of the biology and mechanics of the meniscus will be presented, followed by an overview of general meniscus tissue engineering strategies to provide background for those who may be interested in exploring this area of research.
Tissue properties
Structurally, the meniscus is a semicircular, wedge-shaped piece of cartilage-like tissue that provides an articulating surface for the femur. The knee contains two menisci, one medial and one lateral. In humans, a transverse ligament connects both menisci via the anterior horns; either a Humphry or a Wrisberg ligament (or both) may connect the lateral posterior horn to the medial femoral condyle (this varies between patients).100
Biochemically, the meniscus can be divided into two regions—the outer region is largely vascularized, whereas the inner region is avascular.100 Additionally, meniscus tissue shows zonal arrangement of collagen fibers; superficial layers contain randomly oriented fibers, while the deep zone contains mostly circumferentially arranged fibers, with some fibers oriented radially to tie the framework together.104 Dry meniscus tissue contains approximately 80% collagen type I, with types II, III, and V also present (mostly type II).104,105 Less is known about proteoglycan composition in meniscus tissue, but it appears to vary with species; in porcine menisci, decorin and biglycan were found, while in bovine menisci, aggrecan, fibromodulin, and biglycan were found, with aggrecan as the main component.104,105 The predominant cell type in meniscus tissue is the fibrochondrocyte, a cell whose naming has generated some controversy, but nevertheless displays characteristics of both fibroblasts and chondrocytes, such as collagen I deposition, a pericellular matrix, and consistent staining for proteoglycans.102
Mechanically, the menisci distribute force over the entire surface of the tibia and also act as a shock absorber.104 Due to the semicircular shape of the menisci, the forces imparted by the femur are transferred to hoop stresses within the menisci, which are anchored at the insertion points.104 Because of the shock-absorbing capacity of the tissue, meniscectomy can result in articular cartilage degradation and subsequent bone remodeling with osteoarthritic effects.100 It has been shown that if the ligament attachments are excised, the menisci easily move apart, directing load transfer over a smaller region of articular cartilage rather than the entire tibial surface and increasing average stress threefold.104 Thus, engineering meniscus tissue, as well as its attachment to bone, is critical for avoiding the detrimental osteoarthritic effects of either meniscal defect or removal.
As mentioned earlier, the ends of the horns of each meniscus are connected via ligaments that insert into the tibia, although in bovine and rabbit knees, the posterior lateral meniscus horn inserts into the medial femoral condyle.104 Almost all of these insertions occur via a fibrocartilaginous transition zone resembling the tendon/ligament–bone insertion.106 Collagen fibers connect through zones of uncalcified fibrocartilage and calcified fibrocartilage directly into the bone.104 Collagen type I is found throughout the interface, collagen type II is localized to the fibrocartilaginous areas, and collagen type X is localized specifically to the calcified fibrocartilage zone.104,106 How mechanical forces in each insertion point influence insertion site composition has been examined, but results are conflicting; little is known about the specific compressive forces observed at the meniscus–bone interface.104,107
Current tissue engineering approaches
Considerably less literature exists in the area of meniscus tissue engineering when compared to cartilage or bone tissue engineering. Nevertheless, significant advances have been made in the past decade to engineer meniscus tissue.99–101,103,105,108 A short summary is presented here, as many of these approaches may be starting points for the generation of integrated meniscal constructs that include bony insertions. These fully integrated tissue units may be easier to implement clinically, although innovative designs may allow for regeneration of the interface separately from the meniscus, similar to bone tunnel healing after ligament reconstruction.
Scaffolds for meniscus tissue engineering include both natural and synthetic polymers. Many natural scaffolds have been studied.109–112 One scaffold of note is a collagen-based, acellular implant that is currently undergoing phase II clinical trials.109–111 Results at 12 months and 5–6 years after implantation showed no adverse immunogenic or wear-related issues, with statistically significant Lysholm knee scores and Tegner activity scores compared to before the initial surgery. Biopsy samples detailed fibrocartilage-like tissue and uniform ECM in the constructs.110,111 In another approach, an acellular gelatin hydrogel infiltrated with autologous, platelet-rich plasma was implanted in rabbit meniscus defects for 12 weeks. Semiquantitative scoring described a significant increase in tissue integration, Safranin O staining, and fibrochondrocyte-like cells in the gels with platelet-rich plasma, as opposed to gelatin hydrogels with either platelet-poor plasma or no plasma at all.112 Another investigation explored enzymatically processed allogeneic meniscus tissue as a possible matrix.113 Menisci were treated with trypsin, collagenase, and protease solutions, then sterilized, and successfully seeded the scaffolds with meniscal cells in vitro for 28 days. Testing for immunogenicity using MHC I/II antibodies did not indicate any immunogenic response.113
Other natural gels are comprised of hyaluronic acid and, optionally, another natural or synthetic polymer.114–117 Some in vivo studies have been conducted with a hybrid hyaluronic acid/polycaprolactone (PCL) scaffold, augmented with circumferentially arranged PLA fibers.114,115 Both experiments demonstrated tissue ingrowth and vascularization after either 6-week or 4-month implantation of the acellular scaffold in a total meniscus replacement in sheep.114,115 In addition, the latter study found cartilaginous ECM only in constructs seeded with articular chondrocytes at 4 months, compared to cell-free controls.115 A hyaluronic acid/gelatin matrix was also recently investigated.116 Rabbit marrow stromal cells were precultured in chondrogenic media, then seeded into the hybrid scaffolds, and implanted in rabbit meniscal defects for 12 weeks. Defects that were treated with a cell-free scaffold displayed mostly fibrous tissue in the defect area, while defects treated with the seeded scaffold demonstrated a fibrocartilaginous tissue response. Additionally, repair tissue from the seeded implant indicated a greater mean cross-sectional area than control implants.116
Similar to other orthopedic applications, synthetic scaffolds have also been used for meniscus tissue engineering. One study demonstrated the ability to control matrix alignment using aligned PCL nanofiber scaffolds over 10 weeks, more closely mimicking the mechanical properties of the native tissue.118 Polyurethane and PLLA-based scaffolds have also been explored as scaffold materials.119–123 In one early study, an acellular polyurethane porous implant was used to repair lesions in canine menisci.119 After 2 months, fibrocartilage was observed developing inside the implant; vascularity was noted initially, but decreased after 16 weeks as the fibrocartilage tissue matured. Menisci without implants remained occupied by vascularized fibrous tissue through 24 weeks.119 A more recent study tested a derivatized polyurethane scaffold, implanting scaffolds into dogs for 6 months. Histology revealed a heterogeneous collagen distribution, with fibrous collagen I in the periphery and collagen II in the cartilaginous center.120
One well-studied scaffold is agarose, although it is used in what is referred to as a scaffoldless approach.124–126 Because agarose is generally cell nonadhesive, the general mechanism is believed to be that the nonadhesiveness of agarose directs cells to favor cell–cell interactions—a self-assembly technique.124–126 One in vitro experiment used this approach with a ring-shaped agarose construct and a 1:1 ratio of chondrocytes and meniscal fibrochondrocytes to generate replacement tissue with circumferential fiber bundles, which were stronger in tension when compared to a similarly seeded PGA control.125
Many cell types have been explored for meniscus tissue engineering. Several studies use fibrochondrocytes isolated from meniscus tissue.102,113,118,124–128 Due to the heterogeneity of the meniscus, some issues have been raised regarding the location from which cells should be harvested. In one inquiry, meniscal fibrochondrocytes showed changes in differentiation potential depending on the particular meniscal region chosen for cell isolation.128 Another study indicated decreased expression of chondrocytic genes during monolayer expansion of harvested fibrochondrocytes.129 Fibrochondrocytes are further limited by their preference for producing collagen type I, which neglects collagen type II production. To resolve the issue of matrix deposition, several studies have been published using cocultures of chondrocytes and fibrochondrocytes, citing data showing that chondrocytes establish matrix more rapidly than fibrochondrocytes—especially, collagen and GAG content.124–126 One of these investigations found that coculture improved the biochemical composition and mechanical properties of the resultant tissue, relative to results when using a homogeneous fibrochondrocyte population.126 However, some effort has focused on using MSCs as a potential cell source.116,118 One approach using a PCL nanofiber scaffold found little difference between using meniscal fibrochondrocytes and MSCs, concluding instead that the fiber alignment played a larger role in improving scaffold mechanical properties.118 Thus, further investigation is required to determine the relative merits of differentiated versus undifferentiated cell sources for this application.
To date, the most characterized growth factor in meniscus tissue engineering has been TGF-β1, with BMP-4 and TGF-β3 also showing promising results.127,130,131 In contrast, studies indicate that bFGF does not assist in ECM deposition or protein production.131,132 Many experiments have used adenovirus and retrovirus techniques to express TGF-β1 and other growth factors in implanted cells, though long-term expression remains an issue.98,130,133
Summary and future challenges
Given the diversity of the aforementioned strategies, it is clear that a consensus has yet to be developed regarding optimal meniscal tissue engineering strategies, including the ideal cell source and growth factors for ensuring mechanical stability and matrix deposition. However, current research has also indicated that graft fixation greatly influences the overall outcome of the graft; thus, the meniscus–bone interface is clearly important in ensuring the success of meniscal replacements.108,134–136 Given this link between mechanical fixation and graft effectiveness, investigating this issue may prove essential for future meniscal tissue engineering efforts. Fortunately, due to the similarity between the meniscus–bone insertion and the tendon/ligament–bone insertion, advances in ligament–bone interface regeneration may shed important insights into engineering the meniscus–bone interface. Challenges in the meniscal insertion mirror those for the ligament–bone interface—the need for proper fixation through a fibrocartilaginous transition zone, as well as the expansion of tissue engineering efforts to create an entire integrated tissue unit.
Muscle–Tendon
Similar to the meniscus–bone interface, the muscle–tendon interface has not been extensively studied. However, the myotendinous junction (MTJ) is an important interface in the musculoskeletal system because it acts as the mechanical bridge between skeletal muscle and bone. In muscle injury, failures most often occur near the MTJ.137,138 Successful tissue engineering of the MTJ would bridge the gap between tendon/ligament and muscle tissue engineering, creating new opportunities for the development of regenerative techniques as well as the creation of entire muscle tissue units. To enable potential further work in this field, a review of muscle tissue structure and mechanics of the muscle–tendon interface will be presented, followed by an overview of existing methodologies to regenerate both muscle tissue as well as the interface itself.
Tissue properties
Structurally, a muscle is a collection of muscle fibers; each fiber is considered an individual cell but contains multiple nuclei. Each fiber contains many myofibrils, which are bundles of actin/myosin filaments. These actin/myosin filaments constrict upon stimulation from the peripheral nervous system to effect movement.139 The MTJ is characterized histologically by excessive folding of myofiber cell membranes at the interface, increasing the interfacial area by about an order of magnitude.140–142 Bridging the gap between tendon and muscle is a small bridge of connective tissue, containing fibroblasts, that links the dense collagen fibers of the tendon to muscle fibers at an oblique direction.141 Mechanically, the excessive folding of membranes at the MTJ serves two functions. First, folding reduces the stress on the MTJ membrane during contraction by distributing stress over a wider area to minimize the possibility of tearing. Second, the folding decreases the angle of loading on the interface, which places the interface primarily under shear stress.140,141,143 The success of this structure is seen in muscle failure, which rarely occurs directly at the MTJ but usually in the muscle fibers immediately proximal to it.137,144
At the MTJ, some details concerning muscle fiber force transmission to the tendon ECM are unclear. Generally, there are two accepted biochemical systems. In the first, a vinculin/talin/integrin focal adhesion system links the actin cytoskeleton of a muscle fiber to the ECM, which contains collagen, laminin-1, and laminin-2.142,145 The second system involves dystrophin, the protein that is typically absent in muscular dystrophy.142,145,146 Actin binds to dystrophin, which is linked to the dystroglycan complex; dystrophin binds the intramembrane dystroglycan-β subunit, and the dystroglycan-α subunit binds laminin-2 in the ECM.146 Additional studies have identified paxillin as localized to the MTJ and distributed much like other focal adhesion proteins such as talin or vinculin.147 On the tendon side of the MTJ, fibronectin, laminin, tenascin, and heparan sulfate have all been identified distinctly in the MTJ ECM.142
Current tissue engineering approaches
It is likely that strategies for building the muscle–tendon interface will arise from existing efforts in muscle tissue engineering as well as tendon/ligament tissue engineering. As the latter has been covered previously, here, we present a brief overview of the work that has been completed to date in muscle tissue engineering, as well as a discussion of approaches to engineering the interface. Extended information regarding skeletal muscle tissue engineering can be found elsewhere.148
While cardiac muscle tissue engineering has been researched in great detail, fewer investigations have been performed for skeletal muscle. Fibrinogen hydrogels and other scaffolds made from natural materials (alginate and collagen) have been frequently used.148 A fibrinogen gel was used to culture myoblasts and generated multinucleated myotubes after 3 weeks in culture. Through electrical excitation, the procedure verified several parameters in the engineered tissue that were similar to native muscle. These tests included the characterization of the relationship between muscle lengthening and force generation, as well as the force generated in response to variation of excitation voltage or excitation frequency.149 One experiment, using synthetic polymer constructs, seeded rat skeletal muscle myoblasts in PGA scaffolds and noted vascularized tissue after 6 weeks postperitoneal cavity implantation.150 While myoblasts were adequately supported within these scaffolds, no subsequent evaluations were performed to determine whether the resulting constructs had any muscle functionality. Other studies in engineering muscle tissue include a scaffoldless coculture of rat skeletal myoblasts and fibroblasts for 31 days, which also demonstrated the ability to respond to electrical excitation.151 Despite the noted successes in engineered muscle response to electrical stimuli, however, the above constructs could only generate a small percentage of the forces that a muscle in vivo would generate.148,149,151
As with the meniscus–bone interface, minimal work has been performed to engineer the MTJ itself. One investigation describes the creation of an MTJ analog using constructs formed by rat Achilles tendon fibroblasts and soleus muscle myoblasts.152 Cells from both tissues were cultured separately and formed either self-organized tendon constructs or multinucleated myotubes. The tissues were then pinned together and cocultured for approximately 2 weeks. Results indicated no difference in contractile force between engineered tendon constructs and using segments of adult and fetal rat-tail tendon as the tendon linkages. Additionally, immunostaining revealed the presence of paxillin and talin, which indicated the presence of focal adhesions to the surrounding ECM.152
Summary and future challenges
Based on these studies, a great amount of work remains to be completed to successfully engineer skeletal muscle tissue as well as its connection to tendon tissue. A main issue in engineering muscle tissue remains the lack of force generated in comparison to native muscle. Moreover, as size increases, the issue of construct vascularization may inhibit muscle tissue construct development.153 Additionally, engineered muscle must be efficiently interfaced with tendon to provide proper load transfer to bone, which may prove difficult given the task of replicating the natural membrane interdigitation and folding at the MTJ (or a mechanically comparable analog). This challenge highlights the need for increased expertise in creation of the MTJ interface alone, or as a part of composite muscle–tendon construct.
Conclusions
The four interfaces reviewed here have unique issues to be addressed, but all four share a set of guiding principles in their structure and mechanics. The overall goal in each case is to provide a smooth transition between tissues of varying mechanical properties, which reduces stress concentrations at the interface and thus protects against mechanical failure. Generally, interfaces accomplish this in four ways. First, interface surface area is maximized to reduce stress across the tissue. Second, interface zones are gradual, using calcification and increased proteoglycan content to increase the compressive strength near a stiffer tissue. Third, interdigitation is employed to provide better mechanical integration and adhesion between two tissue types. Fourth, forces are redirected into hoop stresses and shear stresses when possible.
Because these transitions occur within small distances (in the order of millimeters in many cases54,104,141), recreating the gradients of structure and function that occur at these interfaces can present particular difficulties for tissue engineers. To best design new approaches to regenerating orthopedic tissue interfaces, more knowledge is required in the basic developmental biology of these interfaces to better understand when and in response to what stimuli these unique transition tissues are created. In particular, detailed knowledge of how the different cell types involved interact via soluble and insoluble cues at different stages of development may prove interesting. Additionally, more information on the exact spatial distribution of matrix molecules and the relation of tissue structure and mechanical properties on a submillimeter scale would provide insight into what key components are required to effect load transfer. To begin to explore these issues, creation of new techniques for interface tissue characterization, as well as methods for simultaneously culturing multiple cell types, may be required.
While the basic biological and mechanical information gained from the above experiments should serve to better determine design parameters for interfacial tissue engineering, unique tools must also be developed to create the complex tissue templates that are required for these applications. These include biomaterials with capabilities to temporally and spatially control the application of cells and soluble factors, as well as bioreactors that better mimic the anisotropic stresses that are imparted at these interfaces. Finally, outcome measures may need to be reassessed to assure that a suitable level of interface structure and biochemistry has been recapitulated to promote appropriate load transfer across tissue-engineered orthopedic implants. Although, as outlined above, numerous challenges do exist, the necessity of forming proper interfaces for the long-term success of orthopedic tissue engineering strategies makes interfacial tissue engineering both an essential and exciting field of future research.
Acknowledgments
The authors acknowledge funding from the National Science Foundation (NSF Graduate Research Fellowship to P.J.Y. and NSF CAREER Award to J.S.T.) and the National Institutes of Health (1R21EB008918).
Disclosure Statement
No competing financial interests exist.
References
- 1.Lu H.H. Jiang J. Interface tissue engineering and the formulation of multiple-tissue systems. Adv Biochem Eng Biotechnol. 2006;102:91. [PubMed] [Google Scholar]
- 2.Lawrence R.C. Felson D.T. Helmick C.G. Arnold L.M. Choi H. Deyo R.A. Gabriel S. Hirsch R. Hochberg M.C. Hunder G.G. Jordan J.M. Katz J.N. Kremers H.M. Wolfe F. National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ulrich-Vinther M. Maloney M.D. Schwarz E.M. Rosier R. O'Keefe R.J. Articular cartilage biology. J Am Acad Orthop Surg. 2003;11:421. doi: 10.5435/00124635-200311000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Stockwell R.A. Meachim G.T. The chondrocytes. In: Freeman M.A.R., editor. Adult Articular Cartilage. Tunbridge Wells, England: Pitman Medical; 1979. pp. 69–144. [Google Scholar]
- 5.Poole A.R. Kojima T. Yasuda T. Mwale F. Kobayashi M. Laverty S. Composition and structure of articular cartilage: a template for tissue repair. Clin Orthop Relat Res. 2001;391S:S26. doi: 10.1097/00003086-200110001-00004. [DOI] [PubMed] [Google Scholar]
- 6.Schinagl R.M. Gurskis D. Chen A.C. Sah R.L. Depth-dependent confined compression modulus of full-thickness bovine articular cartilage. J Orthop Res. 1997;15:499. doi: 10.1002/jor.1100150404. [DOI] [PubMed] [Google Scholar]
- 7.Hunziker E.B. Articular cartilage structure in humans and experimental animals. In: Kuettner K.E., editor; Schleyerbach R., editor; Peyron J.G., editor; Hascall V.C., editor. Articular Cartilage and Osteoarthritis. New York: Raven Press; 1992. pp. 183–199. [Google Scholar]
- 8.Burr D.B. Anatomy and physiology of the mineralized tissues: role in the pathogenesis of osteoarthrosis. Osteoarthritis Cartilage. 2004;12 Suppl A:S20. doi: 10.1016/j.joca.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Martin R.B., editor; Burr D.B., editor; Sharkey N.A., editor. Skeletal Tissue Mechanics. New York: Springer; 1998. [Google Scholar]
- 10.Oegema T.R. Carpenter R.J. Hofmeister F. Thompson R.C. The interaction of the zone of calcified cartilage and subchondral bone in osteoarthritis. Microsc Res Tech. 1997;37:324. doi: 10.1002/(SICI)1097-0029(19970515)37:4<324::AID-JEMT7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 11.Mente P.L. Lewis J.L. Elastic modulus of calcified cartilage is an order of magnitude less than that of subchondral bone. J Orthop Res. 1994;12:637. doi: 10.1002/jor.1100120506. [DOI] [PubMed] [Google Scholar]
- 12.Clark J.M. Huber J.D. The structure of the human subchondral plate. J Bone Joint Surg Br. 1990;72:866. doi: 10.1302/0301-620X.72B5.2211774. [DOI] [PubMed] [Google Scholar]
- 13.Zizak I. Roschger P. Paris O. Misof B.M. Berzlanovich A. Bernstorff S. Amenitsch H. Klaushofer K. Fratzl P. Characteristics of mineral particles in the human bone/cartilage interface. J Struct Biol. 2003;141:208. doi: 10.1016/s1047-8477(02)00635-4. [DOI] [PubMed] [Google Scholar]
- 14.Temenoff J.S. Mikos A.G. Review: tissue engineering for regeneration of articular cartilage. Biomaterials. 2000;21:431. doi: 10.1016/s0142-9612(99)00213-6. [DOI] [PubMed] [Google Scholar]
- 15.Burg K.J. Porter S. Kellam J.F. Biomaterial developments for bone tissue engineering. Biomaterials. 2000;21:2347. doi: 10.1016/s0142-9612(00)00102-2. [DOI] [PubMed] [Google Scholar]
- 16.Chung C. Burdick J.A. Engineering cartilage tissue. Adv Drug Delivery Rev. 2008;60:243. doi: 10.1016/j.addr.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan Y. Yaszemski M.J. Mikos A.G. Laurencin C.T. Tissue engineering of bone: material and matrix considerations. J Bone Joint Surg Am. 2008;90 Suppl 1:36. doi: 10.2106/JBJS.G.01260. [DOI] [PubMed] [Google Scholar]
- 18.Martin I. Miot S. Barbero A. Jakob M. Wendt D. Osteochondral tissue engineering. J Biomech. 2007;40:750. doi: 10.1016/j.jbiomech.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Kreklau B. Sittinger M. Mensing M.B. Voigt C. Berger G. Burmester G.R. Rahmanzadeh R. Gross U. Tissue engineering of biphasic joint cartilage transplants. Biomaterials. 1999;20:1743. doi: 10.1016/s0142-9612(99)00061-7. [DOI] [PubMed] [Google Scholar]
- 20.Gao J. Knaack D. Goldberg V.M. Caplan A.I. Osteochondral defect repair by demineralized cortical bone matrix. Clin Orthop Relat Res. 2004;427S:S62. doi: 10.1097/01.blo.0000143819.82510.0d. [DOI] [PubMed] [Google Scholar]
- 21.Li X. Jin L. Balian G. Laurencin C.T. Anderson D.G. Demineralized bone matrix gelatin as scaffold for osteochondral tissue engineering. Biomaterials. 2006;27:2426. doi: 10.1016/j.biomaterials.2005.11.040. [DOI] [PubMed] [Google Scholar]
- 22.Schaefer D. Martin I. Jundt G. Seidel J. Heberer M. Grodzinsky A. Bergin I. Vunjak-Novakovic G. Freed L.E. Tissue-engineered composites for the repair of large osteochondral defects. Arthritis Rheum. 2002;46:2524. doi: 10.1002/art.10493. [DOI] [PubMed] [Google Scholar]
- 23.Oliveira J.M. Rodrigues M.T. Silva S.S. Malafaya P.B. Gomes M.E. Viegas C.A. Dias I.R. Azevedo J.T. Mano J.F. Reis R.L. Novel hydroxyapatite/chitosan bilayered scaffold for osteochondral tissue-engineering applications: scaffold design and its performance when seeded with goat bone marrow stromal cells. Biomaterials. 2006;27:6123. doi: 10.1016/j.biomaterials.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 24.Chang C.H. Lin F.H. Lin C.C. Chou C.H. Liu H.C. Cartilage tissue engineering on the surface of a novel gelatin-calcium-phosphate biphasic scaffold in a double-chamber bioreactor. J Biomed Mater Res B Appl Biomater. 2004;71:313. doi: 10.1002/jbm.b.30090. [DOI] [PubMed] [Google Scholar]
- 25.Angele P. Kujat R. Nerlich M. Yoo J. Goldberg V. Johnstone B. Engineering of osteochondral tissue with bone marrow mesenchymal progenitor cells in a derivatized hyaluronan-gelatin composite sponge. Tissue Eng. 1999;5:545. doi: 10.1089/ten.1999.5.545. [DOI] [PubMed] [Google Scholar]
- 26.Gao J. Dennis J.E. Solchaga L.A. Awadallah A.S. Goldberg V.M. Caplan A.I. Tissue-engineered fabrication of an osteochondral composite graft using rat bone marrow-derived mesenchymal stem cells. Tissue Eng. 2001;7:363. doi: 10.1089/10763270152436427. [DOI] [PubMed] [Google Scholar]
- 27.Gao J. Dennis J.E. Solchaga L.A. Goldberg V.M. Caplan A.I. Repair of osteochondral defect with tissue-engineered two-phase composite material of injectable calcium phosphate and hyaluronan sponge. Tissue Eng. 2002;8:827. doi: 10.1089/10763270260424187. [DOI] [PubMed] [Google Scholar]
- 28.Gotterbarm T. Richter W. Jung M. Berardi Vilei S. Mainil-Varlet P. Yamashita T. Breusch S.J. An in vivo study of a growth-factor enhanced, cell free, two-layered collagen-tricalcium phosphate in deep osteochondral defects. Biomaterials. 2006;27:3387. doi: 10.1016/j.biomaterials.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 29.Fukuda A. Kato K. Hasegawa M. Hirata H. Sudo A. Okazaki K. Tsuta K. Shikinami Y. Uchida A. Enhanced repair of large osteochondral defects using a combination of artificial cartilage and basic fibroblast growth factor. Biomaterials. 2005;26:4301. doi: 10.1016/j.biomaterials.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Niederauer G.G. Slivka M.A. Leatherbury N.C. Korvick D.L. Harroff H.H. Ehler W.C. Dunn C.J. Kieswetter K. Evaluation of multiphase implants for repair of focal osteochondral defects in goats. Biomaterials. 2000;21:2561. doi: 10.1016/s0142-9612(00)00124-1. [DOI] [PubMed] [Google Scholar]
- 31.Wang X. Grogan S.P. Rieser F. Winkelmann V. Maquet V. Berge M.L. Mainil-Varlet P. Tissue engineering of biphasic cartilage constructs using various biodegradable scaffolds: an in vitro study. Biomaterials. 2004;25:3681. doi: 10.1016/j.biomaterials.2003.10.102. [DOI] [PubMed] [Google Scholar]
- 32.Huang X. Yang D. Yan W. Shi Z. Feng J. Gao Y. Weng W. Yan S. Osteochondral repair using the combination of fibroblast growth factor and amorphous calcium phosphate/poly(L-lactic acid) hybrid materials. Biomaterials. 2007;28:3091. doi: 10.1016/j.biomaterials.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 33.Jiang C.C. Chiang H. Liao C.J. Lin Y.J. Kuo T.F. Shieh C.S. Huang Y.Y. Tuan R.S. Repair of porcine articular cartilage defect with a biphasic osteochondral composite. J Orthop Res. 2007;25:1277. doi: 10.1002/jor.20442. [DOI] [PubMed] [Google Scholar]
- 34.Sherwood J.K. Riley S.L. Palazzolo R. Brown S.C. Monkhouse D.C. Coates M. Griffith L.G. Landeen L.K. Ratcliffe A. A three-dimensional osteochondral composite scaffold for articular cartilage repair. Biomaterials. 2002;23:4739. doi: 10.1016/s0142-9612(02)00223-5. [DOI] [PubMed] [Google Scholar]
- 35.Schek R.M. Taboas J.M. Segvich S.J. Hollister S.J. Krebsbach P.H. Engineered osteochondral grafts using biphasic composite solid free-form fabricated scaffolds. Tissue Eng. 2004;10:1376. doi: 10.1089/ten.2004.10.1376. [DOI] [PubMed] [Google Scholar]
- 36.Shao X. Goh J.C. Hutmacher D.W. Lee E.H. Zigang G. Repair of large articular osteochondral defects using hybrid scaffolds and bone marrow-derived mesenchymal stem cells in a rabbit model. Tissue Eng. 2006;12:1539. doi: 10.1089/ten.2006.12.1539. [DOI] [PubMed] [Google Scholar]
- 37.Cao T. Ho K.H. Teoh S.H. Scaffold design and in vitro study of osteochondral coculture in a three-dimensional porous polycaprolactone scaffold fabricated by fused deposition modeling. Tissue Eng. 2003;9 Suppl 1:S103. doi: 10.1089/10763270360697012. [DOI] [PubMed] [Google Scholar]
- 38.Swieszkowski W. Tuan B.H. Kurzydlowski K.J. Hutmacher D.W. Repair and regeneration of osteochondral defects in the articular joints. Biomol Eng. 2007;24:489. doi: 10.1016/j.bioeng.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 39.Sachs E. Cima M. Williams P. Brancazio D. Cornie J. 3-dimensional printing - rapid tooling and prototypes directly from a CAD model. J Eng Ind-Trans ASME. 1992;114:481. [Google Scholar]
- 40.Kandel R.A. Grynpas M. Pilliar R. Lee J. Wang J. Waldman S. Zalzal P. Hurtig M. CIHR-Bioengineering of Skeletal Tissues Team. Repair of osteochondral defects with biphasic cartilage-calcium polyphosphate constructs in a sheep model. Biomaterials. 2006;27:4120. doi: 10.1016/j.biomaterials.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Waldman S.D. Spiteri C.G. Grynpas M.D. Pilliar R.M. Hong J. Kandel R.A. Effect of biomechanical conditioning on cartilaginous tissue formation in vitro. J Bone Joint Surg Am. 2003;85-A Suppl 2:101. doi: 10.2106/00004623-200300002-00013. [DOI] [PubMed] [Google Scholar]
- 42.Hung C.T. Lima E.G. Mauck R.L. Takai E. Taki E. LeRoux M.A. Lu H.H. Stark R.G. Guo X.E. Ateshian G.A. Anatomically shaped osteochondral constructs for articular cartilage repair. J Biomech. 2003;36:1853. doi: 10.1016/s0021-9290(03)00213-6. [DOI] [PubMed] [Google Scholar]
- 43.Solchaga L.A. Gao J. Dennis J.E. Awadallah A. Lundberg M. Caplan A.I. Goldberg V.M. Treatment of osteochondral defects with autologous bone marrow in a hyaluronan-based delivery vehicle. Tissue Eng. 2002;8:333. doi: 10.1089/107632702753725085. [DOI] [PubMed] [Google Scholar]
- 44.Tuli R. Nandi S. Li W.J. Tuli S. Huang X. Manner P.A. Laquerriere P. Nöth U. Hall D.J. Tuan R.S. Human mesenchymal progenitor cell-based tissue engineering of a single-unit osteochondral construct. Tissue Eng. 2004;10:1169. doi: 10.1089/ten.2004.10.1169. [DOI] [PubMed] [Google Scholar]
- 45.Alhadlaq A. Elisseeff J.H. Hong L. Williams C.G. Caplan A.I. Sharma B. Kopher R.A. Tomkoria S. Lennon D.P. Lopez A. Mao J.J. Adult stem cell driven genesis of human-shaped articular condyle. Ann Biomed Eng. 2004;32:911. doi: 10.1023/b:abme.0000032454.53116.ee. [DOI] [PubMed] [Google Scholar]
- 46.Alhadlaq A. Mao J.J. Tissue-engineered osteochondral constructs in the shape of an articular condyle. J Bone Joint Surg Am. 2005;87:936. doi: 10.2106/JBJS.D.02104. [DOI] [PubMed] [Google Scholar]
- 47.Holland T.A. Bodde E.W. Baggett L.S. Tabata Y. Mikos A.G. Jansen J.A. Osteochondral repair in the rabbit model utilizing bilayered, degradable oligo(poly(ethylene glycol) fumarate) hydrogel scaffolds. J Biomed Mater Res A. 2005;75:156. doi: 10.1002/jbm.a.30379. [DOI] [PubMed] [Google Scholar]
- 48.Jo S. Shin H. Shung A.K. Fisher J.P. Mikos A.G. Synthesis and characterization of oligo(poly(ethylene glycol) fumarate) macromer. Macromolecules. 2001;34:2839. [Google Scholar]
- 49.Allan K.S. Pilliar R.M. Wang J. Grynpas M.D. Kandel R.A. Formation of biphasic constructs containing cartilage with a calcified zone interface. Tissue Eng. 2007;13:167. doi: 10.1089/ten.2006.0081. [DOI] [PubMed] [Google Scholar]
- 50.Moffat K.L. Sun W.H. Pena P.E. Chahine N.O. Doty S.B. Ateshian G.A. Hung C.T. Lu H.H. Characterization of the structure-function relationship at the ligament-to-bone interface. Proc Natl Acad Sci USA. 2008;105:7947. doi: 10.1073/pnas.0712150105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pedowitz R.A., editor; O'Connor J.J., editor; Akeson W.H., editor. Daniel's Knee Injuries: Ligament and Cartilage Structure, Function, Injury and Repair. Philadelphia, PA: Lippincott, Williams and Wilkins; 2003. [Google Scholar]
- 52.Goh J.C. Ouyang H.W. Teoh S.H. Chan C.K. Lee E.H. Tissue-engineering approach to the repair and regeneration of tendons and ligaments. Tissue Eng. 2003;9 Suppl 1:S31. doi: 10.1089/10763270360696969. [DOI] [PubMed] [Google Scholar]
- 53.Laurencin C.T. Freeman J.W. Ligament tissue engineering: an evolutionary materials science approach. Biomaterials. 2005;26:7530. doi: 10.1016/j.biomaterials.2005.05.073. [DOI] [PubMed] [Google Scholar]
- 54.Woo S.L. Buckwalter J.A. AAOS/NIH/ORS workshop. Injury and repair of the musculoskeletal soft tissues. Savannah, Georgia, June 18–20, 1987. J Orthop Res. 1988;6:907. doi: 10.1002/jor.1100060615. [DOI] [PubMed] [Google Scholar]
- 55.Benjamin M. Ralphs J.R. Fibrocartilage in tendons and ligaments—an adaptation to compressive load. J Anat. 1998;193:481. doi: 10.1046/j.1469-7580.1998.19340481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Woo S.L. Abramowitch S.D. Kilger R. Liang R. Biomechanics of knee ligaments: injury, healing, and repair. J Biomech. 2006;39:1. doi: 10.1016/j.jbiomech.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 57.Wang J.H. Mechanobiology of tendon. J Biomech. 2006;39:1563. doi: 10.1016/j.jbiomech.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 58.Benjamin M. Kumai T. Milz S. Boszczyk B.M. Boszczyk A.A. Ralphs J.R. The skeletal attachment of tendons—tendon “entheses”. Comp Biochem Physiol A Mol Integr Physiol. 2002;133:931. doi: 10.1016/s1095-6433(02)00138-1. [DOI] [PubMed] [Google Scholar]
- 59.Vunjak-Novakovic G. Altman G. Horan R. Kaplan D.L. Tissue engineering of ligaments. Annu Rev Biomed Eng. 2004;6:131. doi: 10.1146/annurev.bioeng.6.040803.140037. [DOI] [PubMed] [Google Scholar]
- 60.Ge Z. Goh J.C. Lee E.H. Selection of cell source for ligament tissue engineering. Cell Transplant. 2005;14:573. doi: 10.3727/000000005783982819. [DOI] [PubMed] [Google Scholar]
- 61.Molloy T. Wang Y. Murrell G. The roles of growth factors in tendon and ligament healing. Sports Med. 2003;33:381. doi: 10.2165/00007256-200333050-00004. [DOI] [PubMed] [Google Scholar]
- 62.Awad H.A. Boivin G.P. Dressler M.R. Smith F.N. Young R.G. Butler D.L. Repair of patellar tendon injuries using a cell-collagen composite. J Orthop Res. 2003;21:420. doi: 10.1016/S0736-0266(02)00163-8. [DOI] [PubMed] [Google Scholar]
- 63.Butler D.L. Awad H.A. Perspectives on cell and collagen composites for tendon repair. Clin Orthop Relat Res. 1999;367S:S324. doi: 10.1097/00003086-199910001-00031. [DOI] [PubMed] [Google Scholar]
- 64.Cornwell K.G. Lei P. Andreadis S.T. Pins G.D. Crosslinking of discrete self-assembled collagen threads: effects on mechanical strength and cell-matrix interactions. J Biomed Mater Res A. 2007;80:362. doi: 10.1002/jbm.a.30893. [DOI] [PubMed] [Google Scholar]
- 65.Meaney Murray M. Rice K. Wright R.J. Spector M. The effect of selected growth factors on human anterior cruciate ligament cell interactions with a three-dimensional collagen-GAG scaffold. J Orthop Res. 2003;21:238. doi: 10.1016/S0736-0266(02)00142-0. [DOI] [PubMed] [Google Scholar]
- 66.Torres D.S. Freyman T.M. Yannas I.V. Spector M. Tendon cell contraction of collagen-GAG matrices in vitro: effect of cross-linking. Biomaterials. 2000;21:1607. doi: 10.1016/s0142-9612(00)00051-x. [DOI] [PubMed] [Google Scholar]
- 67.Gentleman E. Livesay G.A. Dee K.C. Nauman E.A. Development of ligament-like structural organization and properties in cell-seeded collagen scaffolds in vitro. Ann Biomed Eng. 2006;34:726. doi: 10.1007/s10439-005-9058-4. [DOI] [PubMed] [Google Scholar]
- 68.Altman G.H. Diaz F. Jakuba C. Calabro T. Horan R.L. Chen J. Lu H. Richmond J. Kaplan D.L. Silk-based biomaterials. Biomaterials. 2003;24:401. doi: 10.1016/s0142-9612(02)00353-8. [DOI] [PubMed] [Google Scholar]
- 69.Altman G.H. Horan R.L. Lu H.H. Moreau J. Martin I. Richmond J.C. Kaplan D.L. Silk matrix for tissue engineered anterior cruciate ligaments. Biomaterials. 2002;23:4131. doi: 10.1016/s0142-9612(02)00156-4. [DOI] [PubMed] [Google Scholar]
- 70.Cooper J.A. Bailey L.O. Carter J.N. Castiglioni C.E. Kofron M.D. Ko F.K. Laurencin C.T. Evaluation of the anterior cruciate ligament, medial collateral ligament, Achilles tendon and patellar tendon as cell sources for tissue-engineered ligament. Biomaterials. 2006;27:2747. doi: 10.1016/j.biomaterials.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 71.Lu H.H. Cooper J.A. Manuel S. Freeman J.W. Attawia M.A. Ko F.K. Laurencin C.T. Anterior cruciate ligament regeneration using braided biodegradable scaffolds: in vitro optimization studies. Biomaterials. 2005;26:4805. doi: 10.1016/j.biomaterials.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 72.Ouyang H.W. Toh S.L. Goh J. Tay T.E. Moe K. Assembly of bone marrow stromal cell sheets with knitted poly (L-lactide) scaffold for engineering ligament analogs. J Biomed Mater Res B Appl Biomater. 2005;75:264. doi: 10.1002/jbm.b.30281. [DOI] [PubMed] [Google Scholar]
- 73.Cooper J.A. Lu H.H. Ko F.K. Freeman J.W. Laurencin C.T. Fiber-based tissue-engineered scaffold for ligament replacement: design considerations and in vitro evaluation. Biomaterials. 2005;26:1523. doi: 10.1016/j.biomaterials.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 74.Qin T.W. Yang Z.M. Wu Z.Z. Xie H.Q. Qin J. Cai S.X. Adhesion strength of human tenocytes to extracellular matrix component-modified poly(DL-lactide-co-glycolide) substrates. Biomaterials. 2005;26:6635. doi: 10.1016/j.biomaterials.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 75.Cooper J.A. Sahota J.S. Gorum W.J. Carter J. Doty S.B. Laurencin C.T. Biomimetic tissue-engineered anterior cruciate ligament replacement. Proc Natl Acad Sci USA. 2007;104:3049. doi: 10.1073/pnas.0608837104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lu H.H. El-Amin S.F. Scott K.D. Laurencin C.T. Three-dimensional, bioactive, biodegradable, polymer-bioactive glass composite scaffolds with improved mechanical properties support collagen synthesis and mineralization of human osteoblast-like cells in vitro. J Biomed Mater Res A. 2003;64:465. doi: 10.1002/jbm.a.10399. [DOI] [PubMed] [Google Scholar]
- 77.Spalazzi J.P. Doty S.B. Moffat K.L. Levine W.N. Lu H.H. Development of controlled matrix heterogeneity on a triphasic scaffold for orthopedic interface tissue engineering. Tissue Eng. 2006;12:3497. doi: 10.1089/ten.2006.12.3497. [DOI] [PubMed] [Google Scholar]
- 78.Spalazzi J.P. Dagher E. Doty S.B. Guo X.E. Rodeo S.A. Lu H.H. In vivo evaluation of a multiphased scaffold designed for orthopaedic interface tissue engineering and soft tissue-to-bone integration. J Biomed Mater Res A. 2008;86:1. doi: 10.1002/jbm.a.32073. [DOI] [PubMed] [Google Scholar]
- 79.Spalazzi J.P. Vyner M.C. Jacobs M.T. Moffat K.L. Lu H.H. Mechanoactive scaffold induces tendon remodeling and expression of fibrocartilage markers. Clin Orthop Relat Res. 2008;466:1938. doi: 10.1007/s11999-008-0310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Phillips J.E. Burns K.L. Le Doux J.M. Guldberg R.E. García A.J. Engineering graded tissue interfaces. Proc Natl Acad Sci USA. 2008;105:12170. doi: 10.1073/pnas.0801988105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marder R.A. Raskind J.R. Carroll M. Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med. 1991;19:478. doi: 10.1177/036354659101900510. [DOI] [PubMed] [Google Scholar]
- 82.Aglietti P. Buzzi R. Zaccherotti G. de Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:211. doi: 10.1177/036354659402200210. [DOI] [PubMed] [Google Scholar]
- 83.Brown C.H. Steiner M.E. Carson E.W. The use of hamstring tendons for anterior cruciate ligament reconstruction. Technique and results. Clin Sports Med. 1993;12:723. [PubMed] [Google Scholar]
- 84.Jansson K.A. Linko E. Sandelin J. Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:12. doi: 10.1177/03635465030310010501. [DOI] [PubMed] [Google Scholar]
- 85.Beynnon B.D. Johnson R.J. Abate J.A. Fleming B.C. Nichols C.E. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33:1751. doi: 10.1177/0363546505279922. [DOI] [PubMed] [Google Scholar]
- 86.Webster K.E. Feller J.A. Hameister K.A. Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9:86. doi: 10.1007/s001670100191. [DOI] [PubMed] [Google Scholar]
- 87.Kousa P. Järvinen T.L. Vihavainen M. Kannus P. Järvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med. 2003;31:174. doi: 10.1177/03635465030310020401. [DOI] [PubMed] [Google Scholar]
- 88.Kessler M.A. Behrend H. Henz S. Stutz G. Rukavina A. Kuster M.S. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16:442. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 89.Rodeo S.A. Arnoczky S.P. Torzilli P.A. Hidaka C. Warren R.F. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993;75:1795. doi: 10.2106/00004623-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 90.Grana W.A. Egle D.M. Mahnken R. Goodhart C.W. An analysis of autograft fixation after anterior cruciate ligament reconstruction in a rabbit model. Am J Sports Med. 1994;22:344. doi: 10.1177/036354659402200309. [DOI] [PubMed] [Google Scholar]
- 91.Brand J. Weiler A. Caborn D.N. Brown C.H. Johnson D.L. Graft fixation in cruciate ligament reconstruction. Am J Sports Med. 2000;28:761. doi: 10.1177/03635465000280052501. [DOI] [PubMed] [Google Scholar]
- 92.Weiler A. Hoffmann R.F. Bail H.J. Rehm O. Südkamp N.P. Tendon healing in a bone tunnel. Part II: Histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002;18:124. doi: 10.1053/jars.2002.30657. [DOI] [PubMed] [Google Scholar]
- 93.Chen C.H. Chen W.J. Shih C.H. Yang C.Y. Liu S.J. Lin P.Y. Enveloping the tendon graft with periosteum to enhance tendon-bone healing in a bone tunnel: a biomechanical and histologic study in rabbits. Arthroscopy. 2003;19:290. doi: 10.1053/jars.2003.50014. [DOI] [PubMed] [Google Scholar]
- 94.Lim J.K. Hui J. Li L. Thambyah A. Goh J. Lee E.H. Enhancement of tendon graft osteointegration using mesenchymal stem cells in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. 2004;20:899. doi: 10.1016/j.arthro.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 95.Kimura Y. Hokugo A. Takamoto T. Tabata Y. Kurosawa H. Regeneration of anterior cruciate ligament by biodegradable scaffold combined with local controlled release of basic fibroblast growth factor and collagen wrapping. Tissue Eng C Methods. 2008;14:47. doi: 10.1089/tec.2007.0286. [DOI] [PubMed] [Google Scholar]
- 96.Rodeo S.A. Suzuki K. Deng X.H. Wozney J. Warren R.F. Use of recombinant human bone morphogenetic protein-2 to enhance tendon healing in a bone tunnel. Am J Sports Med. 1999;27:476. doi: 10.1177/03635465990270041201. [DOI] [PubMed] [Google Scholar]
- 97.Chen C.H. Liu H.W. Tsai C.L. Yu C.M. Lin I.H. Hsiue G.H. Photoencapsulation of bone morphogenetic protein-2 and periosteal progenitor cells improve tendon graft healing in a bone tunnel. Am J Sports Med. 2008;36:461. doi: 10.1177/0363546507311098. [DOI] [PubMed] [Google Scholar]
- 98.Martinek V. Latterman C. Usas A. Abramowitch S. Woo S.L. Fu F.H. Huard J. Enhancement of tendon-bone integration of anterior cruciate ligament grafts with bone morphogenetic protein-2 gene transfer: a histological and biomechanical study. J Bone Joint Surg Am. 2002;84-A:1123. doi: 10.2106/00004623-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 99.Schoenfeld A.J. Landis W.J. Kay D.B. Tissue-engineered meniscal constructs. Am J Orthop. 2007;36:614. [PubMed] [Google Scholar]
- 100.Aufderheide A.C. Athanasiou K.A. Mechanical stimulation toward tissue engineering of the knee meniscus. Ann Biomed Eng. 2004;32:1161. doi: 10.1114/b:abme.0000036652.31658.f3. [DOI] [PubMed] [Google Scholar]
- 101.Buma P. Ramrattan N.N. van Tienen T.G. Veth R.P. Tissue engineering of the meniscus. Biomaterials. 2004;25:1523. doi: 10.1016/s0142-9612(03)00499-x. [DOI] [PubMed] [Google Scholar]
- 102.Arnoczky S.P. Building a meniscus. Biologic considerations. Clin Orthop Relat Res. 1999;367S:S244. [PubMed] [Google Scholar]
- 103.Sweigart M.A. Athanasiou K.A. Toward tissue engineering of the knee meniscus. Tissue Eng. 2001;7:111. doi: 10.1089/107632701300062697. [DOI] [PubMed] [Google Scholar]
- 104.Messner K. Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193:161. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Almarza A.J. Athanasiou K.A. Design characteristics for the tissue engineering of cartilaginous tissues. Ann Biomed Eng. 2004;32:2. doi: 10.1023/b:abme.0000007786.37957.65. [DOI] [PubMed] [Google Scholar]
- 106.Gao J. Immunolocalization of types I, II, and X collagen in the tibial insertion sites of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2000;8:61. doi: 10.1007/s001670050013. [DOI] [PubMed] [Google Scholar]
- 107.Upton M.L. Guilak F. Laursen T.A. Setton L.A. Finite element modeling predictions of region-specific cell-matrix mechanics in the meniscus. Biomech Model Mechanobiol. 2006;5:140. doi: 10.1007/s10237-006-0031-4. [DOI] [PubMed] [Google Scholar]
- 108.Setton L.A. Guilak F. Hsu E.W. Vail T.P. Biomechanical factors in tissue engineered meniscal repair. Clin Orthop Relat Res. 1999;367S:S254. doi: 10.1097/00003086-199910001-00025. [DOI] [PubMed] [Google Scholar]
- 109.Stone K.R. Rodkey W.G. Webber R. McKinney L. Steadman J.R. Meniscal regeneration with copolymeric collagen scaffolds. In vitro and in vivo studies evaluated clinically, histologically, and biochemically. Am J Sports Med. 1992;20:104. doi: 10.1177/036354659202000202. [DOI] [PubMed] [Google Scholar]
- 110.Rodkey W.G. Steadman J.R. Li S.T. A clinical study of collagen meniscus implants to restore the injured meniscus. Clin Orthop Relat Res. 1999;367S:S281. doi: 10.1097/00003086-199910001-00027. [DOI] [PubMed] [Google Scholar]
- 111.Steadman J.R. Rodkey W.G. Tissue-engineered collagen meniscus implants: 5- to 6-year feasibility study results. Arthroscopy. 2005;21:515. doi: 10.1016/j.arthro.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 112.Ishida K. Kuroda R. Miwa M. Tabata Y. Hokugo A. Kawamoto T. Sasaki K. Doita M. Kurosaka M. The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng. 2007;13:1103. doi: 10.1089/ten.2006.0193. [DOI] [PubMed] [Google Scholar]
- 113.Maier D. Braeun K. Steinhauser E. Ueblacker P. Oberst M. Kreuz P.C. Roos N. Martinek V. Imhoff A.B. In vitro analysis of an allogenic scaffold for tissue-engineered meniscus replacement. J Orthop Res. 2007;25:1598. doi: 10.1002/jor.20405. [DOI] [PubMed] [Google Scholar]
- 114.Chiari C. Koller U. Dorotka R. Eder C. Plasenzotti R. Lang S. Ambrosio L. Tognana E. Kon E. Salter D. Nehrer S. A tissue engineering approach to meniscus regeneration in a sheep model. Osteoarthritis Cartilage. 2006;14:1056. doi: 10.1016/j.joca.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 115.Kon E. Chiari C. Marcacci M. Delcogliano M. Salter D.M. Martin I. Ambrosio L. Fini M. Tschon M. Tognana E. Plasenzotti R. Nehrer S. Tissue engineering for total meniscal substitution: animal study in sheep model. Tissue Eng A. 2008;14:1067. doi: 10.1089/ten.tea.2007.0193. [DOI] [PubMed] [Google Scholar]
- 116.Angele P. Johnstone B. Kujat R. Zellner J. Nerlich M. Goldberg V. Yoo J. Stem cell based tissue engineering for meniscus repair. J Biomed Mater Res A. 2008;85:445. doi: 10.1002/jbm.a.31480. [DOI] [PubMed] [Google Scholar]
- 117.Marsano A. Wendt D. Quinn T.M. Sims T.J. Farhadi J. Jakob M. Heberer M. Martin I. Bi-zonal cartilaginous tissues engineered in a rotary cell culture system. Biorheology. 2006;43:553. [PubMed] [Google Scholar]
- 118.Baker B.M. Mauck R.L. The effect of nanofiber alignment on the maturation of engineered meniscus constructs. Biomaterials. 2007;28:1967. doi: 10.1016/j.biomaterials.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Klompmaker J. Veth R.P. Jansen H.W. Nielsen H.K. de Groot J.H. Pennings A.J. Kuijer R. Meniscal repair by fibrocartilage in the dog: characterization of the repair tissue and the role of vascularity. Biomaterials. 1996;17:1685. doi: 10.1016/0142-9612(96)87648-4. [DOI] [PubMed] [Google Scholar]
- 120.Tienen T.G. Heijkants R.G. de Groot J.H. Schouten A.J. Pennings A.J. Veth R.P. Buma P. Meniscal replacement in dogs. Tissue regeneration in two different materials with similar properties. J Biomed Mater Res B Appl Biomater. 2006;76:389. doi: 10.1002/jbm.b.30406. [DOI] [PubMed] [Google Scholar]
- 121.Tienen T.G. Heijkants R.G. de Groot J.H. Pennings A.J. Schouten A.J. Veth R.P. Buma P. Replacement of the knee meniscus by a porous polymer implant: a study in dogs. Am J Sports Med. 2006;34:64. doi: 10.1177/0363546505280905. [DOI] [PubMed] [Google Scholar]
- 122.Ibarra C. Jannetta C. Vacanti C.A. Cao Y. Kim T.H. Upton J. Vacanti J.P. Tissue engineered meniscus: a potential new alternative to allogeneic meniscus transplantation. Transplant Proc. 1997;29:986. doi: 10.1016/s0041-1345(96)00337-5. [DOI] [PubMed] [Google Scholar]
- 123.Kang S.W. Son S.M. Lee J.S. Lee E.S. Lee K.Y. Park S.G. Park J.H. Kim B.S. Regeneration of whole meniscus using meniscal cells and polymer scaffolds in a rabbit total meniscectomy model. J Biomed Mater Res A. 2006;78:659. doi: 10.1002/jbm.a.30904. [DOI] [PubMed] [Google Scholar]
- 124.Hoben G.M. Hu J.C. James R.A. Athanasiou K.A. Self-assembly of fibrochondrocytes and chondrocytes for tissue engineering of the knee meniscus. Tissue Eng. 2007;13:939. doi: 10.1089/ten.2006.0116. [DOI] [PubMed] [Google Scholar]
- 125.Aufderheide A.C. Athanasiou K.A. Assessment of a bovine co-culture, scaffold-free method for growing meniscus-shaped constructs. Tissue Eng. 2007;13:2195. doi: 10.1089/ten.2006.0291. [DOI] [PubMed] [Google Scholar]
- 126.Hoben G.M. Athanasiou K.A. Creating a spectrum of fibrocartilages through different cell sources and biochemical stimuli. Biotechnol Bioeng. 2008;100:587. doi: 10.1002/bit.21768. [DOI] [PubMed] [Google Scholar]
- 127.Hoben G.M. Willard V.P. Athanasiou K.A. Fibrochondrogenesis of hESCs: growth factor combinations and co-cultures. Stem Cells Dev (Epub ahead of print); 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mauck R.L. Martinez-Diaz G.J. Yuan X. Tuan R.S. Regional multilineage differentiation potential of meniscal fibrochondrocytes: implications for meniscus repair. Anat Rec. 2007;290:48. doi: 10.1002/ar.20419. [DOI] [PubMed] [Google Scholar]
- 129.Gunja N.J. Athanasiou K.A. Passage and reversal effects on gene expression of bovine meniscal fibrochondrocytes. Arthritis Res Ther. 2007;9:R93. doi: 10.1186/ar2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Steinert A.F. Palmer G.D. Capito R. Hofstaetter J.G. Pilapil C. Ghivizzani S.C. Spector M. Evans C.H. Genetically enhanced engineering of meniscus tissue using ex vivo delivery of transforming growth factor-beta 1 complementary deoxyribonucleic acid. Tissue Eng. 2007;13:2227. doi: 10.1089/ten.2006.0270. [DOI] [PubMed] [Google Scholar]
- 131.Pangborn C.A. Athanasiou K.A. Effects of growth factors on meniscal fibrochondrocytes. Tissue Eng. 2005;11:1141. doi: 10.1089/ten.2005.11.1141. [DOI] [PubMed] [Google Scholar]
- 132.Imler S.M. Doshi A.N. Levenston M.E. Combined effects of growth factors and static mechanical compression on meniscus explant biosynthesis. Osteoarthritis Cartilage. 2004;12:736. doi: 10.1016/j.joca.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 133.Hidaka C. Ibarra C. Hannafin J.A. Torzilli P.A. Quitoriano M. Jen S.S. Warren R.F. Crystal R.G. Formation of vascularized meniscal tissue by combining gene therapy with tissue engineering. Tissue Eng. 2002;8:93. doi: 10.1089/107632702753503090. [DOI] [PubMed] [Google Scholar]
- 134.Alhalki M.M. Howell S.M. Hull M.L. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27:320. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 135.Chen M.I. Branch T.P. Hutton W.C. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12:174. doi: 10.1016/s0749-8063(96)90007-9. [DOI] [PubMed] [Google Scholar]
- 136.Goertzen D. Gillquist J. Messner K. Tensile strength of the tibial meniscal attachments in the rabbit. J Biomed Mater Res. 1996;30:125. doi: 10.1002/(SICI)1097-4636(199601)30:1<125::AID-JBM16>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 137.Tidball J.G. Salem G. Zernicke R. Site and mechanical conditions for failure of skeletal muscle in experimental strain injuries. J Appl Physiol. 1993;74:1280. doi: 10.1152/jappl.1993.74.3.1280. [DOI] [PubMed] [Google Scholar]
- 138.Garrett W.E. Muscle strain injuries: clinical and basic aspects. Med Sci Sports Exerc. 1990;22:436. [PubMed] [Google Scholar]
- 139.Lieber R.L. Skeletal Muscle Structure, Function and Plasticity: The Physiological Basis of Rehabilitation. Philadelphia, PA: Lippincott, Williams and Wilkins; 2002. [Google Scholar]
- 140.Trotter J.A. Structure-function considerations of muscle-tendon junctions. Comp Biochem Physiol A Mol Integr Physiol. 2002;133:1127. doi: 10.1016/s1095-6433(02)00213-1. [DOI] [PubMed] [Google Scholar]
- 141.Tidball J.G. Myotendinous junction injury in relation to junction structure and molecular composition. Exerc Sport Sci Rev. 1991;19:419. [PubMed] [Google Scholar]
- 142.Benjamin M. Ralphs J.R. The cell and developmental biology of tendons and ligaments. Int Rev Cytol. 2000;196:85. doi: 10.1016/s0074-7696(00)96003-0. [DOI] [PubMed] [Google Scholar]
- 143.Tidball J.G. Force transmission across muscle cell membranes. J Biomech. 1991;24 Suppl 1:43. doi: 10.1016/0021-9290(91)90376-x. [DOI] [PubMed] [Google Scholar]
- 144.Garrett W.E. Tidball J.G. Myotendinous junction: structure, function, and failure. In: Woo S.L., editor; Buckwalter J.A., editor. Injury and Repair of Musculoskeletal Soft Tissues. Park Ridge: IL American Academy of Orthopaedic Surgeons; 1988. [Google Scholar]
- 145.Monti R.J. Roy R.R. Hodgson J.A. Edgerton V.R. Transmission of forces within mammalian skeletal muscles. J Biomech. 1999;32:371. doi: 10.1016/s0021-9290(98)00189-4. [DOI] [PubMed] [Google Scholar]
- 146.Cohn R.D. Campbell K.P. Molecular basis of muscular dystrophies. Muscle Nerve. 2000;23:1456. doi: 10.1002/1097-4598(200010)23:10<1456::aid-mus2>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 147.Turner C.E. Kramarcy N. Sealock R. Burridge K. Localization of paxillin, a focal adhesion protein, to smooth muscle dense plaques, and the myotendinous and neuromuscular junctions of skeletal muscle. Exp Cell Res. 1991;192:651. doi: 10.1016/0014-4827(91)90090-h. [DOI] [PubMed] [Google Scholar]
- 148.Bach A.D. Stem-Straeter J. Beier J.P. Bannasch H. Stark G.B. Engineering of muscle tissue. Clin Plast Surg. 2003;30:589. doi: 10.1016/s0094-1298(03)00077-4. [DOI] [PubMed] [Google Scholar]
- 149.Borschel G.H. Dow D.E. Dennis R.G. Brown D.L. Tissue-engineered axially vascularized contractile skeletal muscle. Plast Reconstr Surg. 2006;117:2235. doi: 10.1097/01.prs.0000224295.54073.49. [DOI] [PubMed] [Google Scholar]
- 150.Saxena A.K. Willital G.H. Vacanti J.P. Vascularized three-dimensional skeletal muscle tissue-engineering. Biomed Mater Eng. 2001;11:275. [PubMed] [Google Scholar]
- 151.Kosnik P.E. Faulkner J.A. Dennis R.G. Functional development of engineered skeletal muscle from adult and neonatal rats. Tissue Eng. 2001;7:573. doi: 10.1089/107632701753213192. [DOI] [PubMed] [Google Scholar]
- 152.Larkin L.M. Calve S. Kostrominova T.Y. Arruda E.M. Structure and functional evaluation of tendon-skeletal muscle constructs engineered in vitro. Tissue Eng. 2006;12:3149. doi: 10.1089/ten.2006.12.3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Levenberg S. Rouwkema J. Macdonald M. Garfein E.S. Kohane D.S. Darland D.C. Marini R. van Blitterswijk C.A. Mulligan R.C. D'Amore P.A. Langer R. Engineering vascularized skeletal muscle tissue. Nat Biotechnol. 2005;23:879. doi: 10.1038/nbt1109. [DOI] [PubMed] [Google Scholar]