Abstract
OBJECTIVES:
To establish the prevalence of fetal alcohol exposure; to compare physical, behavioural and learning patterns of children with significant alcohol exposure in utero with those of a group of children exposed to minimal alcohol; to assess the usefulness of a fetal alcohol syndrome (FAS)/fetal alcohol effect (FAE) score; and to provide feedback to parents, schools and communities.
DESIGN:
Parent questionnaire, complete physical examinations of children, psychometric tests of the children using elements of the Pediatric Early Elementary Examination (PEEX) and the Pediatric Examination of Educational Readiness (PEER), ADD-H comprehensive teachers rating scale (ACTeRS) score, the newly developed FAS/FAE Score, and the Brigance Comprehensive Inventory of Basic Skills to assess language and mathematical achievement. Testers were blinded to the results of the assessments and questionnaires.
SETTING:
Grades 1 to 3 at Sir Alexander MacKenzie School in Inuvik, Northwest Territories.
RESULTS:
Twenty-four per cent of mothers reported frequent or binge drinking, and 76% of mothers reported abstinence or moderate alcohol intake. There were significant ethnic differences; none of the Caucasian mothers reported frequent or binge drinking during pregnancy compared with 40% of Inuvialuit and 33% of Indian mothers. Children with exposure to frequent or binge drinking in utero had smaller palpebral fissures (2.3±0.1 cm versus 2.5±0.3 cm, P<0.01), smaller palpebral fissure to intercanthal distance ratios (0.77±0.05 versus 0.86±0.10, P<0.01) and smaller head circumferences (52.1±1.6 cm versus 53.6±1.6 cm, P<0.01) than those exposed to moderate drinking or abstinence. Children exposed to frequent or binge drinking in utero also demonstrated poorer coordination (P<0.005) and cortical function (P<0.01), attention problems, hyperactivity (ACTeRS), and poorer scholastic achievement in language (P<0.001) and mathematics (P<0.01) than their minimally exposed counterparts. In children in grades 2 and 3, a significant negative correlation was found between FAS/FAE scores and language (r=–0.55, P<0.001) and mathematical achievement (r=–0.28, P=0.20).
CONCLUSIONS:
The prevalence of drinking during pregnancy in the northern population studied was high, and exposure in utero was associated with physical abnormalities, difficulties with coordination and cortical function, and significant delays in language and mathematical achievement. The FAS/FAE score may be useful in predicting success or failure in language development.
Keywords: Aboriginal health, Alcohol-related birth defects, Alcohol-related neurodevelopmental defects, Attention deficit hyperactivity disorder, Fetal alcohol syndrome, Fetal alcohol effect, Learning difficulties
Abstract
OBJECTIFS :
Établir la prévalence de l’exposition fœtale à l’alcool, comparer les profils physiques, de comportement et d’apprentissage des enfants très exposés à l’alcool in utero à ceux d’un groupe d’enfants qui y étaient très peu exposés, évaluer l’utilité d’un indice du syndrome d’alcoolisme fœtal (SAF) ou de l’effet de l’alcoolisme sur le fœtus (EAF) et transmettre l’information aux parents, aux écoles et aux collectivités.
MÉTHODOLOGIE :
Questionnaires aux parents, examen physique complet des enfants, tests psychométriques des enfants à l’aide d’éléments de l’examen élémentaire pédiatrique précoce et de l’examen pédiatrique de réceptivité à l’éducation. Indice ACTeRs, nouvel indice SAF-EAF et de l’inventaire Brigance détaillé des aptitudes de base pour évaluer le succès linguistique et mathématique. Les examinateurs ne connaissaient pas l’identité des enfants qui avaient répondu aux évaluations et aux questionnaires.
EMPLACEMENT :
Niveaux 1 à 3 à l’école Sir Alexander MacKenzie d’Inuvik, dans les Territoires du Nord-Ouest.
RÉSULTATS :
Vingt-quatre pour cent des mères ont déclaré être de grandes buveuses ou des buveuses faisant des virées irrégulières, et 76 % des mères ont indiqué avoir opté pour l’abstinence ou une consommation modérée d’alcool. Les différences ethniques étaient importantes; aucune mère caucasienne n’fait état d’une grande consommation ou consommation irrégulière d’alcool pendant leur grossesse, par rapport à 40 % des mères Inuvialuit et 33% des mères indiennes. Les enfants exposés à une grande consommation ou à une consommation irrégulière importante in utero présentaient une fente palpébrale plus petite (2,3±0,1 cm par rapport à 2,5±0,3 cm, P<0,01), un coefficient de fente palpébrale par rapport à la distance intercanthale plus faible (0,77±0,05 cm par rapport à 0,86±0,10 cm, P<0,01) et une circonférence crânienne plus petite (52,1±1,6 cm par rapport à 53,6±1,6 cm, P<0,01) que ceux exposés à une consommation modérée d’alcool in utero ou dont la mère avait opté pour l’abstinence. Ils présentaient également une coordination (P<0,005) et une fonction corticale (P<0,01) moindres, des troubles d’attention, de l’hyperactivité (ACTeRs) et des résultats scolaires moins satisfaisants du point de vue du langage (P<0,001) et des mathématiques (P<0,01) que les enfants très peu exposés. Chez les enfants de deuxième et troisième année, on remarquait une corrélation négative significative entre les indices SAF-EAF et les succès relatifs au langage (r=–0,55, P<0,001) et aux mathématiques (r=–0,28, P=0,20).
CONCLUSIONS :
La prévalence de consommation d’alcool pendant la grossesse au sein de la population nordique étudiée était élevée, et l’exposition in utero s’associait à des anomalies physiques, à des troubles de coordination et de fonction corticale et à d’importants retards du langage et des apprentissages mathématiques. L’indice SAF-EAF peut être utile pour prédire le succès ou l’échec dans le développement du langage.
It is only since the classic descriptions of the malformations associated with fetal exposure to alcohol were reported by Jones and Smith (1) in 1973 that the full scope of the devastation brought on by alcohol exposure during pregnancy was realized. A diagnosis of fetal alcohol syndrome (FAS) is based on a history of prenatal alcohol consumption combined with a group of characteristics in the infant. These include growth deficiencies, specific dysmorphic features such as characteristic facies (small palpebral fissures, widened intercanthal distances with a decreased ratio of palpebral fissure size to intercanthal distance [2], a short nose, a depressed nasal bridge, epicanthal folds, a hypoplastic philtrum, a thin upper lip and a bow-shaped mouth) and central nervous system defects, including microcephaly (1). Significant problems, such as hyperactivity, lifelong learning difficulties and behaviour problems, may also occur (1,3,4). With the reshaping of the face that occurs with adolescence, FAS becomes more difficult to diagnose on clinical grounds (4). A diagnosis of fetal alcohol effect (FAE) originally denoted alcohol exposure, and nonspecific physical and psychological manifestations. The diagnosis of ‘FAE’ has been largely replaced by a new classification system that specifies whether effects are physical (alcohol-related birth defects [ARBD]) or related to the development of the nervous system or brain (alcohol-related neurodevelopmental defects [ARND]) (5). Although ARBD and ARND do not necessarily accompany full-blown FAS, their effects can be as severe (6).
Abel (7) estimated the incidence of FAS at 0.97/1000 (0.097%) live births and 43/1000 (4.3%) among heavy drinkers. More recently, on the basis of three population studies, Sampson et al (8) estimated the incidence of FAS to be between 2.8 and 4.8/1000 live births, and the incidence of a combination of FAS and ARND to be at least 9.1/1000 live births. Although all races are susceptible, FAS appears with disproportionately high frequency in American Indian offspring (9). There is an increasing awareness of the extent of FAS and FAE in native communities in Canada (10), and especially the relationship of these conditions with developmental delay and difficulty in learning (11). Robinson et al (12) identified 22 (16%) of 116 children with FAS in one Aboriginal community in British Columbia.
Apart from the characteristic facies, the most consistent physical finding in newborns with FAS is growth retardation, especially a small head circumference (13,14). Increased motor activity, and alterations in motor tone and orientation behaviour have also been found (15,16). Throughout early childhood, decreased cognitive (17), motor and speech development have been noted, with more serious defects occurring in children whose mothers drank heavily throughout the pregnancy (3,10,12,13,18). Attention deficits, hyperactivity and impulsive behaviours similar to those found in children with attention deficit hyperactivity disorder (ADHD) who were not exposed to alcohol were also documented in children with FAS or FAE (19). Children’s intelligence quotient (IQ) has also been found to be affected. Russell et al (20) noted a mean decrease of seven intelligence quotient (IQ) points in the six-year-old offspring of mothers with ‘problem’ drinking during pregnancy. Streissguth et al (21) found a similar decrease in six-year-old children who had been exposed to ‘binge’ drinking (greater than five drinks at one time) in utero. In a study by LaDue et al (22), adolescents and adults with FAS were found to have intellectual functioning in the mild to moderate range of impairment, with 46% scoring less than an IQ of 69. There was a marked discrepancy between mean verbal IQ of 65 and performance IQ of 79, with significant specific deficits in academic and adaptive function. Specific impairment of number processing has also been found (23).
Although heavy drinking, and especially ‘binge’ drinking, appears to have an effect on cognition, behaviour and development, several studies suggest that behavioural abnormalities and language deficits may be minimal in the absence of the physical features of FAS or FAE. Greene et al (24) followed a cohort of infants exposed to alcohol prenatally up to the age of three years and found no significant relationship between alcohol exposure and language difficulties unless craniofacial effects of FAS were present. Similarly, Russell et al (20) found no significant difference in the intellectual development or auditory processing in children of moderate or ‘social’ drinkers who had no stigmata of FAS or FAE. Abel (6) gives convincing arguments that low alcohol consumption levels are unlikely to cause FAS, that effects depend on high blood alcohol levels and that the number of drinks consumed at a time are more important than the ‘average’ alcohol consumption. Similarly, Godel et al (14) found that moderate drinking (less than five drinks less than once per week) had no measurable effect on the newborn compared with frequent or binge drinking, which was associated with microcephaly.
Individuals exposed to alcohol in utero may have long term sequelae requiring life-long care and attention. LaDue et al (22), Olson et al (25) and others (26) have established a profile of psychological and behavioural manifestations of FAS and FAE that do not improve with age. Poor judgment and the inability to appreciate the possible consequences of an action are common; if these characteristics are combined with frustration with poor school performance or a tendency to impulsive behaviour, conduct leading to conflict with society may result. Excessive familiarity and friendliness even toward strangers, combined with a lack of inhibitions, can lead to exploitation and abuse. Other problems with long term implications, such as poor social skills, difficulty with organization, and difficulty with recognizing and setting boundaries, make day-to-day living difficult and hazardous (22). These continuing defects distinguish individuals with fetal exposure to alcohol from individuals with attention deficit disorders and learning disabilities that are not associated with alcohol exposure. There is, however, evidence that adequate and early intervention can minimize the effects of behaviours related to FAS or FAE (25,27). Thus, it is important to recognize individuals with FAS or FAE early.
From 1987 to 1991, the nutrition of a cohort of pregnant women and their infants was studied in the Inuvik zone of the Northwest Territories (14). Details of alcohol intake during pregnancy were included in the study. The present study is a follow-up of a cohort of women of the same age, and included some of the participants in the original study to determine whether there are recognizable physical, cognitive or psychological sequelae in their children that can be used for diagnosis of exposure to alcohol in utero.
The present study had several objectives. One goal was to establish the prevalence of learning disorders and their associations in individuals with intrauterine exposure to alcohol. Another goal was to establish the prevalence of fetal alcohol exposure. The study also sought to identify characteristic physical, behavioural and learning patterns of children with documented intrauterine exposure to alcohol. Researchers also aimed to assess the usefulness of the FAS/FAE Score, and provide feedback to parents, the community and schools in order to stimulate discussion, and help plan interventions and solutions.
PATIENTS AND METHODS
Study population
The study group included all elementary school children who were born between June 1, 1987 and May 31, 1989, and who were attending school in Inuvik. Mother-child pairs were not considered for inclusion in the study if information about alcohol intake was vague or not quantifiable, or if it was based on anecdotal evidence that was not verified by parents or foster parents. Although alcohol intake was based mainly on questionnaires filled out by biological parents, other sources were also considered. Some of the adoptive parents were family members who had intimate knowledge of maternal alcohol intake; heavy alcohol exposure was often the reason for removal from the birth family. Children whose parents refused to participate, children with chronic illness, or children who had suffered illnesses or injuries that could affect either their growth or cognition were excluded. The study did not control for factors such as a poor home environment, differences in maternal IQ, socioeconomic status and cultural differences.
Data collection
Information collected before the physical examination included a parent questionnaire, based on one developed by the Glenrose Rehabilitation Hospital in Edmonton, Alberta, that provided relevant background information, including family history, the mother’s pregnancy history and relevant lifestyle issues. Examiners were blinded to all background information when performing the physical examination and psychometric testing.
Questions relating to drinking explored abstinence, the frequency of drinking (once per week, two or more times per week) and the amount consumed each time (one to two drinks, three to five drinks, more than six drinks). Patterns of drinking during pregnancy were stratified as follows: abstinence; moderate (less than five drinks less than once a week); frequent (less than five drinks more than once a week); and binge (more than five drinks at any time). A ‘drink’ referred to a bottle of beer, a 120 mL glass of wine or a 30 mL shot of liquor with or without a mixer. This classification enabled comparison with previous responses to a questionnaire administered during pregnancy to a number of the mothers (14).
Physical and psychometric examinations, which the parents were encouraged to attend, were carried out. Physical examination included facial as well as anthropometric measurements. Neurodevelopmental testing included elements of the Pediatric Examination of Educational Readiness (28) and the Pediatric Early Elementary Examination (29) that are standardized for seven- to nine-year-old children. The tests were selected to allow the assessment of coordination and cortical function. Tests of coordination consisted of tests of gross motor function (motor stance, rapid pronation and supination, stand and hop in place) and fine motor function (imitative finger movements and finger opposition). Tests of cortical function consisted of tests of perception (double simultaneous touch), visual memory (copying a four block based pyramid from memory), auditory memory (digit span, word span and sound patterns), visual symbol association (visual to verbal with comprehension) and sound-symbol association (auditory to graphic). To diminish cultural bias, test items were selected that were mainly nonverbal and that had been used in the past by psychologists at the Glen-rose Rehabilitation Hospital to test Aboriginal children. Test components were graded from 0 to 3, depending on how well they were performed. Coordination and cortical indices were means calculated from individual scores in each group of tests.
Checklists to supplement the above tests were filled out by homeroom teachers, one of whom was Aboriginal. Checklists included the ADD-H comprehensive teachers raing scale (ACTeRS) (30), which scores attention, hyper-activity, and social and oppositional behaviour. Test scores are converted into percentiles, and the result may be used to support a diagnosis of ADHD. Low percentiles, especially below the 15th percentile in a particular field, may indicate significant problems. An FAS/FAE Score (Table 1) developed especially for this study scored behavioural characteristics that have been found to be associated with FAS or FAE (22,25,26). No standards have been established for the FAS/FAE Score.
TABLE 1:
Fetal Alcohol Syndrome/Fetal Alcohol Exposure (FAS/FAE) checklist
| None | Severe | ||||
|---|---|---|---|---|---|
| Attention problems | 1 | 2 | 3 | 4 | 5 |
| Impulsiveness | 1 | 2 | 3 | 4 | 5 |
| Hyperactivity | 1 | 2 | 3 | 4 | 5 |
| Lack of judgment | 1 | 2 | 3 | 4 | 5 |
| Lack of initiative | 1 | 2 | 3 | 4 | 5 |
| Sequencing problems | 1 | 2 | 3 | 4 | 5 |
| Organization problems | 1 | 2 | 3 | 4 | 5 |
| Difficulty making decisions | 1 | 2 | 3 | 4 | 5 |
| Inappropriate behaviour | |||||
| Excessive friendliness | 1 | 2 | 3 | 4 | 5 |
| Lack of inhibitions | 1 | 2 | 3 | 4 | 5 |
| Difficulty with abstract thinking | 1 | 2 | 3 | 4 | 5 |
| Inability to transfer lessons learned | 1 | 2 | 3 | 4 | 5 |
| Inability to anticipate consequences of actions | 1 | 2 | 3 | 4 | 5 |
| Total | 65 | ||||
Finally, a Brigance Comprehensive Inventory of Basic Skills test (31), which measures basic skills in language and math and gives a score of grade equivalence, was administered individually to each child by three members of the special needs department of the school, two of whom were Aboriginal. The Brigance test is a text-referenced and field-tested criteria referenced assessment instrument designed for use with a wide range of students from prekindergarten to grade 9. Results from this test can be used to determine the effectiveness of an instructional program and to assess competence for placement and promotion. It was selected for this study in part because it has been recognized to be useful in assessing academic skills by school personnel in the north. It can be administered easily and scored objectively by special education and classroom teachers, as well as by clinically trained personnel such as school psychologists. Furthermore, the Brigance test’s ability to gather academic data that provide a sampling of skills that go beyond simple word recognition in reading and numerical operations in mathematics was deemed to be important. Although reliability data for the Brigance test are limited, research has verified acceptable reliability for this instrument (32).
Statistical analysis
Results were analyzed to establish the prevalence of learning problems and to see whether there were features that could, either alone or in combination, identify children exposed to alcohol in utero. The authors realized that some comparisons may be based on relatively small samples. Nevertheless, it was determined that significant comparisons may be found if means or proportions showed important and clinically significant differences among groups. Therefore, anthropometric, psychological and psychometric variables were compared among groups using ANOVA for continuous variables, χ2 for categorical variables and logistic regression for dichotomous variables.
Consent
Parents or guardians of children who were to be involved in the study were approached, the purpose of the study was explained and informed consent was obtained. A research licence was obtained from the Aurora Research Institute in Inuvik, Northwest Territories. Letters of endorsement were solicited from the Inuvik Regional Health Board, the Community Corporation of Inuvik and the Gwich’in Native Band Councils in Aklavik. The following agencies were informed of the proposed study: the Dene Cultural Institute, the Dene Nation, the Inuvialuit Social Development Corporation, the Gwich’in Tribal Council and the Sahtu Tribal Council.
RESULTS
One hundred children were in the age group selected for the study. Eight were excluded because their parents chose not to participate. None of the children were excluded on the basis of illness or accident. Thus, 92 children were enrolled in the study, 55 males and 37 females. There were 31 Causasian, 33 Inuvialuit, 26 Dene and 10 children of mixed ethnic origin. Twenty-five children were in grade 1, 55 in grade 2 and 12 in grade 3. Teachers identified 46% of the 92 children as having learning problems.
No significant differences in any of the measured parameters were found among the children of mothers who abstained or drank moderately during their pregnancies, or among children of mothers who drank frequently or engaged in binge drinking during their pregnancies. Thus, for analysis, the data from each of these similar groups were combined (group 1 and group 2, respectively).
Quantifiable information about alcohol exposure during pregnancy was obtained for 70 children. Seventeen (24%) of the mothers reported frequent or binge drinking during pregnancy and 53 (76%) reported abstinence or moderate intake only. The prevalence of frequent or binge drinking among 21 Caucasian mothers, 26 Inuvialuit mothers, 15 Indian mothers and nine mothers of mixed race was 0%, 40%, 33% and 22%, respectively.
Thirty-nine (73.6%) of the 53 children exposed minimally had no reported school difficulty compared with only one child (5.6%) of the 17 with significant alcohol exposure. The rest of the children had various conditions that could affect learning. One (2%) of the children exposed minimally had criteria suggestive of FAS or FAE compared with 13 (76%) of the group with significant exposure. Of the other eight children, seven were males (six were in the minimally exposed group and two were in the moderate to heavy exposure group), and all had criteria based on classifications in the Diagnostic and Statistical Manual of Mental Disorders: DMS-IV, 4th edition (33) that were suggestive of ADHD. Six children in the minimally exposed group and two in the moderate to heavily exposed group had factors, such as perinatal difficulties and difficult home situations, that may account for learning difficulties.
Overall, children exposed in utero to frequent or binge drinking had significantly smaller mean palpebral fissures (2.3±0.1 cm versus 2.5±0.3 cm, P<0.01), smaller palpebral fissure to intercanthal distance ratios (0.77±0.05 cm versus 0.86±0.10 cm, P<0.01) and smaller mean head circumferences (52.1±1.6 cm versus 53.6±1.6 cm, P<0.01) than children exposed to no drinking or moderate drinking. However, the results of facial measurements were influenced by the fact that even among children in group 1, significant ethnic differences were found. The mean palpebral fissure length among Indian children in group 1 (2.18+0.20 cm) was significantly less than that of either Caucasian (2.54±0.22 cm, P<0.001) or Inuvialuit children (2.51±0.23 cm, P<0.001). Similarly, the mean palpebral fissure to epicanthal distance ratio of nonalcohol-exposed Dene children in group 1 (0.77±0.07), was significantly less than that of either of their Caucasian (0.90±0.08, P<0.001) or Inuvialuit counterparts (0.85±0.09, P<0.05). When children within each ethnic group were considered separately, no significant differences in measurements were found between children exposed to no alcohol and children exposed to alcohol within the ethnic groups.
The mean coordination index for all children was 2.28±0.31 (25th percentile 2.11, fifth percentile 1.79). Only one of 50 (2%) children in group 1 had indices at or below the fifth percentile compared with four of 19 (21%) children in group 2. There was a significant difference in the mean coordination index among group 1 and group 2-exposed, even when controlled for age (Table 2). Using multiple regression, a small but not significant age effect was noted. The mean cortical index for all children was 2.06±0.59 (25th percentile 1.70, fifth percentile 1.20). Only one of 50 (2%) of children in Group 1 had indices below the fifth percentile compared with three of 19 (16%) of the children in group 2. The child in group 1 had an extremely low cortical index (0.1), marked hyperactivity and attention problems, and a severe learning disability. A significant difference was found in the mean cortical index between the two groups (Table 2). In a multiple regression model, age had a slight and nonsignificant effect on the cortical index when the four outliers who had indices below 0.8 (three of whom had been exposed to alcohol) and who were all younger than seven years of age were excluded from the calculation.
TABLE 2:
Results of neurodevelopmental tests, ADD-H Comprehensive Teachers Rating Scale (ACTeRS) and the Fetal Alcohol Syndrome/Fetal Alcohol Exposure (FAS/FAE) Score relative to alcohol exposure during pregnancy
| Test | Alcohol exposure in utero | P | |
|---|---|---|---|
| None or moderate (group 1, n=50) mean | Frequent or binge (group 2, n=19) mean | ||
| Neurodevelopmental | |||
| Coordination Index (range) | 2.34±0.24 (1.79 to 2.74) | 2.06±0.44 (0.94 to 2.78) | <0.005 |
| Cortical Index (range) | 2.16±0.55 (0.60 to 3.00) | 1.6±0.66 (0.10 to 2.50) | <0.001 |
| ACTeRS | |||
| Attention (percentile) | 51.2±26.2 | 18.1±16.7 | <0.0001 |
| Hyperactivity (percentile) | 50.4±18.4 | 20.2±18.5 | <0.0001 |
| Social (percentile) | 53.8±25.6 | 26.3±24.3 | <0.0001 |
| Oppositional (percentile) | 37.7±15.1 | 25.3±17.0 | <0.005 |
| FAS/FAE Score | |||
| Score | 22.1±10.0 | 41.7±13.8 | <0.001 |
Highly significant differences attributable to alcohol exposure were found in the mean percentile results from all four elements of the ACTeRS assessment (Table 2). Furthermore, a significantly higher percentage of children had scores below the 15th percentile, six of 50 (12%) among children in group 1 compared with 11 of 19 (58%) among children in group 2 (χ2=15.6, P=0.0001). There were, however, some racial differences. Mean percentiles for Attention among participants in group 1 were significantly higher for Caucasian children (63.0±20.8) than for either of their Inuvialuit (34.1±25.1, P<0.001) or Dene counterparts (41.5±26.2, P=0.05). Nevertheless, when only the Aboriginal groups were considered, there was still a marked contrast in mean percentiles for attention between groups 1 and 2 (37.0±25.2 versus 16.1±15.1, P<0.005). Similar but less marked ethnic differences were found when percentiles for hyperactivity, social and oppositional scores were compared. Again, when ethnicity was taken into consideration, differences due to alcohol exposure were still present.
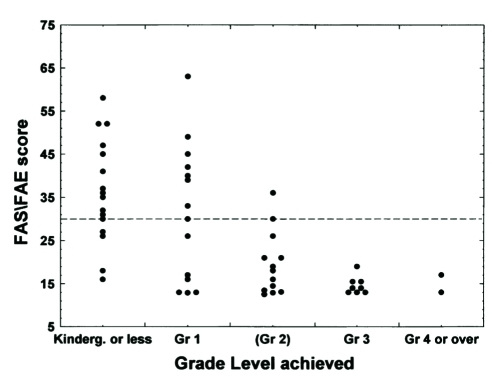
Differences in the FAS/FAE Scores were also found (Table 2), suggesting a much higher frequency of behavioural disturbances among children in group 2 than among those in group 1. Some differences were found between ethnic groups. Caucasian children in group 1 had FAS/FAE scores significantly lower (18.0±6.7) than Inuvialuit (24.7±11.1, P=0.05) or Dene children (28.0±13.0, P<0.01) ) in group 1, who were also exposed to minimal amounts of alcohol. However, when only the Aboriginal children were considered, the difference in the mean FAS/FAE Scores between groups 1 and 2 was significant once again (29.1±1.7 versus 39.7±12.7, P<0.005), suggesting a definite fetal alcohol effect. A high FAS/FAE score was also highly predictive of grade level achievement. Significant negative correlations were found between the FAS/FAE Score and both language (r=–0.55, P<0.001) and math achievement (r=–0.28, P<0.02). Only one child with a score of over 30 achieved standards at the expected grade level in language (Figure 1). All of the other children achieved standards one or two grades below the expected level.
Figure 1).
Relationship between Fetal Alcohol Syndrome/Fetal Alcohol Exposure (FAS/FAE) Score of grade 2 children and language grade level achieved on the Brigance test. The points to the left indicate achievement below the norm; to the right achievement above the norm. Kinderg Kindergarten; Gr Grade
Table 3 indicates the relationship of intrauterine alcohol exposure to language and math achievement in grade 2 children. The effect on language development was most marked. The mean grade level achieved by grade 2 children exposed in utero to frequent or binge drinking was equivalent to kindergarten or less compared with the appropriate grade level for their less exposed counterparts. Indeed, many of the children in group 2 were unable to recognize even simple words. A similar although smaller effect was noted in math. It is noteworthy that the achievement of children least affected by alcohol exposure was also below the norm. Table 4 shows the degree of language difficulty experienced by children in grades 2 and 3 related to the alcohol intake of parents. Eleven of 13 children (85%) in group 2, reflecting the highest fetal alcohol exposure, were at least two grade levels behind in language development. Only one of these children achieved language standards for his grade; more than half of his peers in group 1 achieved expected grade level language standards. Binge drinking seemed to have the greatest effect on achivement. All nine children exposed prenatally to ‘binge’ drinking showed little, if any, ability to read or spell. There was a slight but not significant ethnic difference in language skills among children in group 1.
TABLE 3:
Relationship of alcohol exposure during pregnancy to language and math achievement in grade 2 on the Brigance Comprehensive Inventory of Basic Skills
| Alcohol exposure | P | ||
|---|---|---|---|
| None or moderate (group 1, n=33) grade equivalent | Frequent or binge (group 2, n=11) grade equivalent | ||
| Language | |||
| Word recognition | 1.78±1.00 | 0.73±0.83 | 0.01 |
| Reading – oral | 2.06±1.12 | 0.55±0.75 | 0.001 |
| Comprehension | 2.05±1.10 | 0.77±0.72 | 0.001 |
| Spelling | 1.86±1.01 | 0.82±0.60 | 0.01 |
| Mean grade equivalent | 1.94±0.98 | 0.72±0.67 | 0.001 |
| Mathematics | |||
| Number recognition | 1.84±0.80 | 1.00±0.45 | 0.01 |
| Math problems | 1.08±0.40 | 1.09±0.30 | N/S |
| Money | 1.85±0.87 | 0.95±0.79 | 0.01 |
| Time | 1.15±1.00 | 0.81±0.40 | N/S |
| Mean grade equivalent | 1.48±0.54 | 0.97±0.54 | 0.01 |
TABLE 4:
Relationship of fetal alcohol exposure to language achievement in grades 2 and 3
| Alcohol intake | Language achievement | Total | |||
|---|---|---|---|---|---|
| More than one grade less n (%) | One grade less n (%) | At grade level n (%) | Above grade level n (%) | ||
| None or moderate (group 1) | 7 (18.9) | 11 (29.8) | 14 (37.8) | 5 (13.5) | 37 |
| Frequent or binge (group 2) | 11 (84.6) | 1 (7.7) | 1 (7.7) | 0 (0.0) | 13 |
| Total | 18 (36.0) | 12 (24.0) | 15 (30.0) | 5 (10.0) | 50 |
DISCUSSION
The present study underlined the extent of learning problems and the severity of abnormalities associated with prenatal exposure to alcohol. Even with the relatively small numbers in each subgroup, which tended to reduce the power of the study for conclusion making, significant physical, neurodevelopmental, behavioural and academic problems were found. The children labelled with ADHD tended to be different. For example, 11 of the 12 children with ADHD were male, and had fewer difficulties with interpersonal relationships, life skills, judgment and appreciation of consequences of action than those found in children in group 2. Our data suggest that because facial proportions tend to vary with race, differences in facial measurements cannot be cited as characteristics of FAS, unless each ethnic group is considered separately. Standards need to be established for each ethnic group.
The definitions of light, moderate and heavy drinking are controversial, with the tendency to define consumption on the basis of ‘average’ intake (34). However, the total alcohol intake and the resultant blood alcohol level, especially among ‘alcoholic’ women, may be the most important determinant of whether the fetus will be affected (6). There are other concerns related to drinking during pregnancy. Self-reporting of alcohol consumption tends to underestimate intake. Furthermore, some of the parents who refused to participate in the study may have done so because of guilt due to drinking during pregnancy. Thus, the prevalence of drinking during pregnancy may still be underestimated. It may be argued that after many years, it is difficult for mothers to remember the amount that they drank during pregnancy. However, in the group that had been in the original NINS study (14), the concordance rate between the intake reported during pregnancy and the intake reported in this study seven to nine years later was greater than 90%. Confounding factors such as poor home environment, differences in maternal IQ, socioeconomic status and cultural differences were not controlled for and may have contributed to some of the differences seen. Some of the ethnic differences seen with the ACTeRS and FAS/FAE scores may reflect cultural differences. With regard to nomenclature, the newer terms ARBD and ARND were not commonly used at the time of the study, hence the use of the old terms FAS or FAE. However, the neurodevelopmental, behavioural and the learning difficulties demonstrated by children in alcohol-exposed group can be classified as ARND.
With regard to the home environment, a number of the most highly affected children had been in adoptive or foster homes since infancy. No information regarding the home situation, housing or family income was obtained. Cultural differences in upbringing and the presence of teachers from a southern culture have been suggested as factors influencing the short attention span and hyperactivity in the children. However, both Aboriginal and Caucasians teachers taught math and language to these children.
Although the effects of fetal alcohol exposure reflect irreversible brain damage, early diagnosis and remediation can result in improved prognosis. Behavioural problems are the most devastating of all effects. Early intervention can help FAS/FAE-affected children function within their limitations, learn how to make proper choices, develop acceptable interpersonal skills, master basic life skills and, most important, maintain self-esteem. This often means scaling down academic expectations and putting an emphasis on training for future self-sufficiency. Programming for success can result in improved learning and enhanced self-image, which in turn can decrease ‘acting out’ behaviours. Because there is no ‘blood test’ for FAS/FAE, diagnosis must be based on a strong index of suspicion based on known physical and behavioural characteristics, many of which were apparent in this study. The FAS/FAE Score seems promising as a diagnostic tool but needs further evaluation. A score of 30 seems a reasonable break point for the FAS/FAE Score.
Prevention is the key to the elimination of FAS/FAE. It is very important that communities become aware of the extent of the problem, and the resulting financial and human costs. Awareness is followed by acknowledgement and ‘ownership’ of the problem, and an appreciation of the role of the community in prevention. To improve awareness in the community studied, meetings were held with individual parents to discuss findings related to their children. Meetings with teachers and educators followed to discuss the implications of the overall findings and the role of the school in remediation. Discussions also began with community leaders, tribal councils, women’s groups, health boards and school boards to foster community awareness and to encourage development of prevention programs.
Because FAS/FAE and its sequelae – ARBD and the more devastating ARND – are completely preventable, knowing the extent and morbidity of this problem may give impetus to community-based programs to counter alcohol abuse, especially drinking during pregnancy. This paper outlines only the first steps; further measures must come from the community itself. Changes in attitude may already be occurring. Anecdotal evidence from health workers involved with pregnant women in the Inuvik area suggests a shift in attitude away from drinking during pregnancy.
Acknowledgments
This study was funded in part by the Inuvik Regional Health and Social Services Board, Inuvik, Northwest Territories.
REFERENCES
- 1.Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early pregnancy. Lancet. 1973. pp. iipp. 999–1001. [DOI] [PubMed]
- 2.Clarren SK, Astley SJ. Diagnostic Guide for Fetal Alcohol Syndrome and Related Conditions: The 4-Digit Diagnostic Code. 2nd edn. Seattle: University of Washington; 1999. [Google Scholar]
- 3.Conry J. Neuropsychological deficits in fetal alcohol syndrome and fetal alcohol effects. Alcohol Clin Exp Res. 1990;14:650–5. doi: 10.1111/j.1530-0277.1990.tb01222.x. [DOI] [PubMed] [Google Scholar]
- 4.Spohr HL, Willms J, Steinhausen HC. Prenatal alcohol exposure and long-term developmental consequences. Lancet. 1993;341:907–10. doi: 10.1016/0140-6736(93)91207-3. [DOI] [PubMed] [Google Scholar]
- 5.Stratton K, Howe C, Battaglia FC, editors. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Diagnosis and Treatment: Committee to Study Fetal Alcohol Syndrome. Washington: National Academy Press; 1996. [Google Scholar]
- 6.Abel EL. What really causes FAS? Teratology. 1999;59:4–6. doi: 10.1002/(SICI)1096-9926(199901)59:1<4::AID-TERA3>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 7.Abel EL. An update on incidence of FAS: FAS is not an equal opportunity birth defect. Neurotoxicol Teratol. 1995;17:437–43. doi: 10.1016/0892-0362(95)00005-c. [DOI] [PubMed] [Google Scholar]
- 8.Sampson PD, Streissguth AP, Bookstein FL, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56(5):317–26. doi: 10.1002/(SICI)1096-9926(199711)56:5<317::AID-TERA5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 9.Aase JM. The fetal alcohol syndrome in American Indians: A high risk group. Neurobehav Toxicol Teratol. 1981;3:153–6. [PubMed] [Google Scholar]
- 10.Carney LJ, Chermak GD. Performance of American Indian children with fetal alcohol syndrome on the test of language development. J Commun Disord. 1991;24:123–34. doi: 10.1016/0021-9924(91)90016-c. [DOI] [PubMed] [Google Scholar]
- 11.Asante KO, Nelms-Matzke J. Report on the survey of children with chronic handicaps and fetal alcohol syndrome in the Yukon and Northwest British Columbia. Terrance: Mills Memorial Hospital; 1985. [Google Scholar]
- 12.Robinson GC, Conry JL, Conry RF. Clinical profile and prevalence of fetal alcohol syndrome in an isolated community in British Columbia. CMAJ. 1987;137:203–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Russell M, Skinner JB. Early measures of maternal alcohol misuse as predictors of adverse pregnancy outcomes. Alcohol Clin Exp Res. 1988;12:824–30. doi: 10.1111/j.1530-0277.1988.tb01354.x. [DOI] [PubMed] [Google Scholar]
- 14.Godel JC, Pabst HF, Hodges PE, Johnson KE, Froese GJ, Joffres MR. Smoking and caffeine and alcohol intake during pregnancy in a northern population: Effect on fetal growth. CMAJ. 1992;147:181–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Walpole I, Zubrick S, Ponte J, Lawrence C. Low to moderate maternal alcohol use before and during pregnancy, and neurobehavioural outcome in the newborn infant. Dev Med Child Neurol. 1991;33:875–83. doi: 10.1111/j.1469-8749.1991.tb14796.x. [DOI] [PubMed] [Google Scholar]
- 16.Coles CD, Smith I, Fernhoff PM, Falek A. Neonatal neurobehavioural characteristics as correlates of maternal alcohol use during gestation. Alcohol Clin Exp Res. 1985;9:454–60. doi: 10.1111/j.1530-0277.1985.tb05582.x. [DOI] [PubMed] [Google Scholar]
- 17.Kerns KA, Don A, Mateer CA, Streissguth AP. Cognitive defects in non-retarded adults with fetal alcohol syndrome. J Learn Disabil. 1997;30:685–93. doi: 10.1177/002221949703000612. [DOI] [PubMed] [Google Scholar]
- 18.Becker M, Warr-Leeper GA, Leeper HA. Fetal alcohol syndrome: A description of oral motor, articulatory, short term memory, grammatical, and semantic abilities. J Commun Disord. 1990;23:97–124. doi: 10.1016/0021-9924(90)90016-r. [DOI] [PubMed] [Google Scholar]
- 19.Nanson JL, Hiscock M. Attention deficits in children exposed to alcohol prenatally. Alcohol Clin Exp Res. 1990;14:656–61. doi: 10.1111/j.1530-0277.1990.tb01223.x. [DOI] [PubMed] [Google Scholar]
- 20.Russell M, Czarnecki DM, Cowan R, McPherson E, Mudar PJ. Measures of maternal alcohol use as predictors of development in early childhood. Alcohol Clin Exp Res. 1991;14:991–1000. doi: 10.1111/j.1530-0277.1991.tb05200.x. [DOI] [PubMed] [Google Scholar]
- 21.Streissguth AP, Barr HM, Sampson PD. Moderate prenatal alcohol exposure: effects on child IQ and learning problems at age 7 1/2 years. Alcohol Clin Exp Res. 1990;14:662–9. doi: 10.1111/j.1530-0277.1990.tb01224.x. [DOI] [PubMed] [Google Scholar]
- 22.Ladue RA, Streissguth AP, Randels SP. Clinical considerations pertaining to adolescents and adults with fetal alcohol syndrome. In: Sonderegger TB, editor. Perinatal Substance Abuse: Research Findings and Clinical Implications. Baltimore: The Johns Hopkins University Press; 1993. pp. 104–31. [Google Scholar]
- 23.Kopera-Frye K, Dehaene S, Streissguth AP. Impairments of number processing induced by fetal alcohol exposure. Neuropsychologia. 1996;34:1187–96. doi: 10.1016/0028-3932(96)00043-7. [DOI] [PubMed] [Google Scholar]
- 24.Greene T, Ernhart CB, Martier S, Sokol R, Ager J. Prenatal alcohol exposure and language development. Alcohol Clin Exp Res. 1990;14:937–45. doi: 10.1111/j.1530-0277.1990.tb01842.x. [DOI] [PubMed] [Google Scholar]
- 25.Olson HC, Burgess DM, Streissguth AP. Fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE): A lifespan view, with implications for early intervention. Zero to Three/National Center for Clinical Infant Programs. 1992;13:24–9. [Google Scholar]
- 26.Streissguth AP, Aase JM, Claren SK, Randels SP, LaDue RA, Smith DF. Fetal alcohol syndrome in adolescents and adults. JAMA. 1991;265:1961–7. [PubMed] [Google Scholar]
- 27.Burgess DM, Streissguth AP. Fetal alcohol syndrome and fetal alcohol effects: Principles for educators. Phi Delta Kappan. 1992;74:24–9. [Google Scholar]
- 28.Levine MD, Schneider EA. Pediatric Examination of Educational Readiness (PEER) Cambridge: Educators Publishing Service Inc; 1982. [Google Scholar]
- 29.Levine MD. The Pediatric Early Elementary Examination (PEEX) Cambridge: Educators Publishing Service Inc; 1992. [Google Scholar]
- 30.Ullmann RK, Sleator EK, Sprague RL. ACTeRs. Champaign: MetriTech Inc; 1991. [Google Scholar]
- 31.Brigance AH. Comprehensive Inventory of Basic Skills. North Billerica: Curriculum Associates Inc; 1983. [Google Scholar]
- 32.Linkous LW. A reliability study of the Brigance CIBS. Annual Meeting of the Council for Exceptional Children; March 31 to April 4, 1986.New Orleans: [Google Scholar]
- 33.4th edn. Washington: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 34.Abel EL, Kruger ML, Friedl J. How do physicians define “light”, “moderate” and “heavy” drinking? Alcohol Clin Exp Res. 1998;22:979–84. doi: 10.1111/j.1530-0277.1998.tb03692.x. [DOI] [PubMed] [Google Scholar]