Abstract
We report a case of ciliary body melanocytoma in a Korean patient, which presented as an intermittently painful pigmented iris mass and was successfully managed by iridocyclectomy. A 52-year-old healthy man presented with an irregularly-shaped and heavily-pigmented mass at the iris root of his right eye. Visual acuity of the right eye was 20/20 with normal intraocular pressure. Ultrasound biomicroscopy showed a 1.5x1.3-mm ciliary-body mass with extension into the iris root. Iridocyclectomy with scleral resection under a lamellar scleral flap was performed, and the histopathologic features of the resected tissue were consistent with melanocytoma of the ciliary body. The patient's visual acuity remained 20/20 with good postoperative cosmesis. During one year of follow-up, no signs of tumor recurrence were seen, and the patient reported resolution of the intermittent ocular pain in the involved eye.
Keywords: Ciliary body, Iridocyclectomy, Melanoma, Uveal neoplasms
Although melanocytomas are classically located in the optic nerve head, they can also be found anywhere along the uveal tract, including the iris [1], choroid [2], and ciliary body [3]. Melanocytoma is a variant of melanocytic nevi, and its occurrence in the uveal tract is relatively uncommon. Until 1999, 40 cases of ciliary-body melanocytomas had been described [4]; since that time, ten more cases have been reported in the English literature [5-9]. We report a case of ciliary body melanocytoma in a Korean patient which was successfully managed with surgery.
Case Report
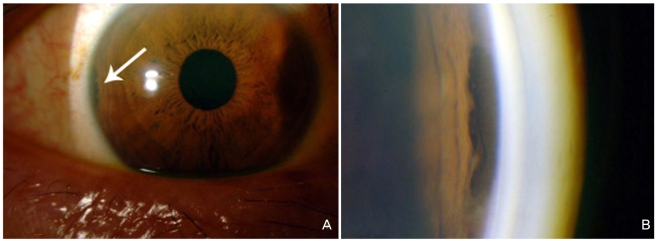
A 52-year-old healthy man presented with intermittent ocular pain of indistinct duration in his right eye. His best-corrected visual acuity (BCVA) was 20/20, and the intraocular pressure in the right eye was 10 mmHg. Ophthalmic examination of his left eye was unremarkable. Slit-lamp and gonioscopic examination of the right eye showed an irregularly-shaped pigmented mass at the temporal iris root (Fig. 1). Ultrasound biomicroscopy showed a ciliary body mass with extension into the iris root and medium internal reflection (Fig. 2A). The basal diameter of the mass was 1.5 mm and the height was 1.3 mm. Magnetic resonance imaging of the head and orbit was unremarkable, and positron emission tomography of the ciliary body identified no significant fluorodeoxyglucose uptake in the orbit or the imaged body to suggest malignancy.
Fig. 1.
(A) Colored slit-lamp photograph showing a dark-pigmented and irregularly-shaped mass at the temporal iris root (white arrow) in the right eye. (B) Gonioscopic examination showing the mass in an enlarged view.
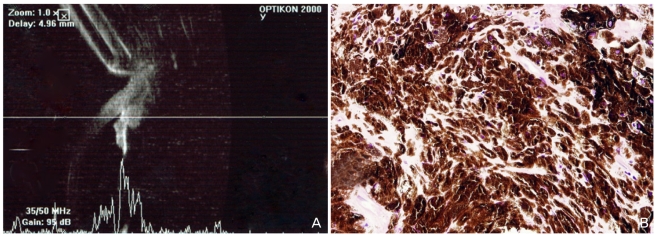
Fig. 2.
(A) Ultrasound biomicroscopy shows a ciliary body mass with extension into the iris root. Medium internal reflection of the mass was seen with a basal diameter of 1.5 mm and a height of 1.3 mm. (B) Microscopic appearance of the specimen showing polyhedral cells filled with dark melanin granules, typical features of a melanocytoma.
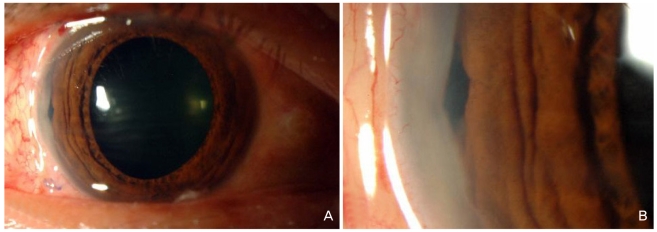
The patient received iridocyclectomy with scleral resection under a lamellar scleral flap. Microscopic examination showed a tumor of heavily-pigmented polyhedral cells (Fig. 2B), and the tumor was positive for melanocytic markers (Melan A and HMB-45). A macrophage marker (CD 68) confirmed the presence of melanophages in a scattered pattern. The proliferative activity, estimated by the Ki-67 labeling index, was less than 1.0%, implying a benign tumor. Histopathologic features were consistent with melanocytoma of the ciliary body with extension into the iris root. Slit-lamp photography taken on postoperative day 7 showed a small iridectomy site with good overall cosmesis (Fig. 3). The patient's BCVA remained 20/20 with an intraocular pressure of 12 mmHg. During one year of follow-up, no signs of tumor recurrence were seen, and the patient reported resolution of the intermittent ocular pain in the involved eye.
Fig. 3.
Slit-lamp photograph taken on postoperative day 7. (A) Note a small opening at the iris root with good overall postoperative cosmesis. (B) Enlarged view of the iridectomy site.
Discussion
Melanocytoma of the ciliary body is typically identified at a late stage, as its location behind the iris eludes early detection with routine ophthalmic examination. Only after ciliary body melanocytomas extend into the iris root can they be visualized on anterior segment examination. In a report of ten patients with ciliary body melanocytomas, including a review of 30 additional cases [4], 85% of patients displayed extension into the iris root or the trabecular meshwork, but only 12% had elevated intraocular pressure. Our patient exhibited extension of his ciliary-body melanocytoma into the iris root, but his preoperative intraocular pressure was within the normal range.
In this series of ten patients [4], three were symptomatic, one of which reported soreness of the involved eye. Likewise, our patient presented with intermittent ocular pain, which could have been related to the presence of tumor in the ciliary body. The intermittent pain disappeared following the removal of the mass.
The differential diagnosis of a pigmented tumor of the ciliary body includes adenoma, adenocarcinoma, medulloepithelioma and, most importantly, malignant melanoma. Although melanocytoma can usually be distinguished histopathologically, it can be difficult to clinically differentiate before surgery, especially from a malignant melanoma. LoRusso et al. [4] advised surgical removal rather than observation for management of pigmented lesions of the ciliary body due to both the difficulty in clinically distinguishing a melanocytoma from a malignant melanoma and the frequent occurrence of necrosis (36%) seen in ciliary body melanocytomas. If serious intraocular complications are not present, such as massive necrosis of a large tumor, severe destruction of chamber angle structures, or massive hemorrhage, and if technically feasible, iridocyclectomy under lamellar scleral flap seems an apt choice for the surgical treatment of ciliary body tumors.
In summary, melanocytoma of the ciliary body is a rare tumor that can invade chamber angle structures and present as a pigmented mass at the iris root. We present a case of ciliary body melanocytoma which presented as an iris mass with intermittent pain that was successfully managed with an iridocyclectomy.
References
- 1.Demirci H, Mashayekhi A, Shields CL, et al. Iris melanocytoma: clinical features and natural course in 47 cases. Am J Ophthalmol. 2005;139:468–475. doi: 10.1016/j.ajo.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Brownstein S, Dorey MW, Mathew B, et al. Melanocytoma of the choroid: atypical presentation and review of the literature. Can J Ophthalmol. 2002;37:247–252. doi: 10.1016/s0008-4182(02)80117-x. [DOI] [PubMed] [Google Scholar]
- 3.Shields JA, Shields CL, Eagle RC., Jr Melanocytoma (hyperpigmented magnocellular nevus) of the uveal tract: the 34th G. Victor Simpson lecture. Retina. 2007;27:730–739. doi: 10.1097/IAE.0b013e318030e81e. [DOI] [PubMed] [Google Scholar]
- 4.LoRusso FJ, Boniuk M, Font RL. Melanocytoma (magnocellular nevus) of the ciliary body: report of 10 cases and review of the literature. Ophthalmology. 2000;107:795–800. doi: 10.1016/s0161-6420(99)00151-7. [DOI] [PubMed] [Google Scholar]
- 5.Capeans C, Pineiro A, Blanco MJ, et al. Ultrasound biomicroscopic findings in a cavitary melanocytoma of the ciliary body. Can J Ophthalmol. 2003;38:501–503. doi: 10.1016/s0008-4182(03)80030-3. [DOI] [PubMed] [Google Scholar]
- 6.Haruta M, Miyamoto K, Horii T, et al. Iridociliary melanocytoma with suspected pulmonary metastasis. Jpn J Ophthalmol. 2005;49:545–547. doi: 10.1007/s10384-005-0235-7. [DOI] [PubMed] [Google Scholar]
- 7.Hiscott P, Campbell RJ, Robertson DM, Damato B. Intraocular melanocytoma in association with bone formation. Arch Ophthalmol. 2003;121:1791–1794. doi: 10.1001/archopht.121.12.1791. [DOI] [PubMed] [Google Scholar]
- 8.Mohamed MD, Gupta M, Parsons A, Rennie IG. Ultrasound biomicroscopy in the management of melanocytoma of the ciliary body with extrascleral extension. Br J Ophthalmol. 2005;89:14–16. doi: 10.1136/bjo.2004.048967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei WB, Yang WL, Hu SM, Li B. Local excision of ciliary body tumors: a long-term prospective cohort study in China. Chin Med J. 2008;121:2152–2156. [PubMed] [Google Scholar]