Abstract
Study Objectives:
To explore whether employment in industries likely to have non-standard work schedules (e.g., manufacturing and service) and occupations with long work-weeks (e.g., managerial/ professional, sales, and transportation) is associated with an increased risk of short sleep duration.
Design:
Cross-sectional epidemiologic survey.
Setting:
Household-based face-to-face survey of civilian, non-institutionalized US residents.
Participants:
Sample adults interviewed for the National Health Interview Survey in 1985 or 1990 (N = 74,734) or between 2004 and 2007 (N = 110,422). Most analyses focused on civilian employed workers interviewed between 2004 and 2007 (N = 66,099).
Interventions:
N/A
Measurements and Results:
The weighted prevalence of self-reported short sleep duration, defined as ≤6 h per day, among civilian employed workers from 2004-2007 was 29.9%. Among industry categories, the prevalence of short sleep duration was greatest for management of companies and enterprises (40.5%), followed by transportation/warehousing (37.1%) and manufacturing (34.8%). Occupational categories with the highest prevalence included production occupations in the transportation/warehousing industry, and installation, maintenance, and repair occupations in both the transportation/warehousing industry and the manufacturing industry. In the combined sample from 1985 and 1990, 24.2% of workers reported short sleep duration; the prevalence of short sleep duration was significantly lower during this earlier time period compared to 2004–2007 for 7 of 8 industrial sectors.
Conclusions:
Self-reported short sleep duration among US workers varies by industry and occupation, and has increased over the past two decades. These findings suggest the need for further exploration of the relationship between work and sleep, and development of targeted interventions for specific industry/occupation groups.
Citation:
Luckhaupt SE; Tak S; Calvert GM. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. SLEEP 2010;33(2):149-159
Keywords: Sleep duration, occupational groups, work
THE NATIONAL SLEEP FOUNDATION (NSF) RECOMMENDS THAT HEALTHY ADULTS SLEEP 7-9 H/DAY; BUT EPIDEMIOLOGICAL STUDIES SUGGEST THAT mean sleep duration among American adults has decreased substantially over time, with an increased percentage of adults who report an average sleep duration of ≤ 6 h/day.1,2 Recent surveys indicate that American workers average 6.7 to 7.6 h of sleep per workday.3,4
Both short and long habitual sleep time have been found to be associated with increased risks of mortality,5,6 hypertension,7,8 coronary heart disease,9 and diabetes.10 In addition, short sleep duration has been found to be associated with self-rated poor health11 and elevated body mass index (BMI).12 Among workers, insufficient sleep can affect job performance and workplace safety, which are important occupational health considerations.13–15
In addition to understanding the effects of sleep duration, it is important to study determinants that predict or influence an individual's sleep duration.16 This issue is important because: 1) understanding the primary determinants of sleep duration will allow for the design of studies that can appropriately control for confounders and effect modifiers; and 2) knowledge of the determinants of sleep duration will allow for identification of subgroups at highest risk for sleep related morbidity, so that these subgroups can be targeted with appropriate interventions.
Non-occupational factors that have been associated with short sleep duration include demographic factors: being male,17–20 being non-Hispanic black,18,21 being divorced or widowed,18,19 low levels of education,7,18,19 and urban residence.18 Some studies have found a U-shaped relationship between age and short sleep duration, with lower prevalence of short sleep duration among young adults and older adults, compared to middle-aged adults2,17; while other studies have suggested a more linear increase in prevalence of short sleep duration with age.7 High self-reported stress,18 smoking,18,20,22,23 activity limitations and leisure-time physical inactivity,18,23 and alcohol consumption18,22,23 have also been associated with short sleep duration. Employed persons tend to have a higher prevalence of short sleep duration than unemployed persons18; and, with regard to work schedules, early morning start times,24 rotating shifts,25 night shifts,26 and long work hours17 are associated with short sleep duration.
Relationships between Work and Sleep
Decreases in mean sleep duration have been attributed, in part, to the expanded possibilities of nighttime activities that accompanied the introduction of electric light and other technologies, and to the more recent trend toward expansion of both manufacturing and service sectors to 24-h/day operations.1 In addition, cell phones, beepers, and other communication devices have had the effect of putting some workers in a perpetual “on-call” status, increasing the likelihood that sleep will be interrupted for rapid decision-making or other duty-related tasks. The increasing role of computing and the internet in work may also influence sleep patterns, as people literally bring their laptops, and thus work, to bed with them. Observational studies have suggested that work may impact both quantity and quality of sleep as a result of long working hours,3,17 shift work,3,24–26 and job stress.27–30 Although the effects of work may interact with lifestyle factors and stress at home, work factors remain important after adjusting for many potential confounders.25,30
Worldwide, annual working hours for most workers have gradually declined from the latter part of the 19th century until recently, when they began increasing again. The US now has the longest annual working hours of any of the wealthy industrialized countries,31 although data from the US Bureau of Labor Statistics indicate that the average length of the American work week has changed little, and possibly even declined since the 1960s-1970s.32,33 The prevalence of workers who work > 48 h per week has increased, and there is evidence that long working hours vary by occupation, with a high prevalence among managerial and professional, sales, and transportation workers.32,34
In addition to the quantity of hours worked affecting the opportunity for sleep, the timing of hours available for sleep affects sleep duration through circadian disruption. Attempts to sleep during daylight hours, when melatonin is falling and body temperature is rising, usually result in shorter sleep episodes and more awakening.35–37 Thus, working non-traditional shifts, especially night shifts, can negatively affect sleep duration independently of long working hours.
In order to identify groups of workers at increased risk of short sleep duration for targeted interventions and future studies, we used data from the National Health Interview Survey (NHIS) to examine the prevalence of short sleep duration among US workers by industry and occupation. We hypothesized that workers in the manufacturing and service sectors would be at increased risk of short sleep duration due to 24-h/day operations leading to non-standard work schedules; and that, within these industry sectors, managerial and professional, sales, and transportation workers would be at increased risk of short sleep duration due to long work weeks. We also hypothesized that the prevalence of short sleep duration among US workers has increased significantly over time. We defined short sleep duration as a self-reported average ≤ 6 h of sleep per 24-h period, based on the NSF recommendation that adults should sleep 7-9 h/day (http://www.sleepfoundation.org/site/c.huIXKjM0IxF/b.2419131/k.6C23/How_Much_Sleep_is_Enough.htm), and well controlled experimental studies that have shown both neurobehavioral performance and memory impairment with chronic sleep reductions to ≤ 6 h.38,39
METHODS
Study Sample
Publicly available data collected through the National Health Interview Survey (NHIS) were utilized in the present analyses. The NHIS has been conducted annually by the National Center for Health Statistics in collaboration with the US Census Bureau since 1957 to monitor the health of the nation, as described elsewhere.40,41 The target population is the US civilian, non-institutionalized population, and interviews are conducted face-to-face in the participants' homes. A representative sample of households is selected using a multistage cluster sample design. Trained interviewers from the US Census Bureau annually visit 35,000 to 40,000 households across the country and collect data on about 75,000 to 100,000 individuals. A sample adult and sample child are chosen from each family to answer detailed questions. The data used to analyze sleep duration and the relevant SAS program statements are publicly available (http://www.cdc.gov/nchs/nhis.htm).
Variables of interest for this study included demographic variables – sex, age, race, ethnicity, marital status, and educational attainment, which have previously been associated with sleep duration. Data on urban vs. rural residence are collected for the NHIS but are not publicly available for recent years. Work-related variables of interest included employment status, industry, occupation, number of current jobs, and total hours worked in the last week. (The latter 2 variables were only available for 2004-2007.) Data on health behaviors (smoking, alcohol consumption, physical inactivity, and obesity) and self-rated health status were also included in some analyses.
Since work hour data were not available in the 1985 or 1990 NHIS, we utilized work hour data from the 1990 Current Population Survey (CPS) to provide a comparison to the 2004-2007 NHIS work hour data. The CPS data was obtained from the website of the National Bureau of Economic Research (http://www.nber.org/data/cps_basic.html).
Study Definitions
The NHIS sample adult questionnaire included a question about the average hours of sleep per day in 1985, 1990, and 2004-2007: “On average, how many hours of sleep do you get in a 24-hour period?” Answers were recorded as whole numbers of hours, so we used the categorical variable “short sleep duration” for all analyses. We defined short sleep duration as ≤ 6 h of sleep in a 24-h period, on average.
Employment status in the week prior to the interview was ascertained for all adults. We classified employment status into 5 categories: employed (“working for pay at a job or business” or “with a job or business but not at work”), unemployed (“looking for work”), unpaid worker (“working, but not for pay, at a family-owned job or business”), non-worker (“not working at a job or business and not looking for work”), and unknown.
Verbatim responses were obtained from each employed sample adult (≥ 18 years old) respondent regarding his/her industry (employer's type of business) and occupation (employee's type of work). These responses were reviewed by US Census Bureau coding specialists who assigned 4-digit industry and occupation codes. For data prior to 2004, industry and occupation codes were based on the prevailing versions of the Standard Industrial Classification (SIC) and the Standard Occupational Classification (SOC) systems. For industry and occupation data collected since 2004, the 1997 North American Industrial Classification System (NAICS) and 2000 SOC system were used. Due to concerns that the level of detail contained in the Census codes could compromise respondent confidentiality, detailed industry and occupation codes are restricted to in-house NHIS data files, and only 2-digit industry and occupation recodes are included in public use data files. Since 2004, the occupation recodes include 94 detailed categories and 23 simple categories, and the industry recodes include 79 detailed categories and 21 simple categories.
Data Analyses
First, we pooled data from NHIS sample adults interviewed from 2004 through 2007 to analyze the prevalence of short sleep duration by employment status. We excluded respondents coded to the military specific occupation category or the Armed Forces industry category (N = 42) from further analyses because the NHIS sample is not designed to provide accurate estimates of persons in the Armed Forces. Next we analyzed the prevalence of short sleep duration among currently employed civilian workers by simple industry categories. Within industry categories with a high prevalence of short sleep duration, we performed additional analyses to identify occupational groups with the highest prevalence of short sleep duration. We also examined the prevalence of short sleep duration by demographic variables, health behaviors, health status, and job characteristics, which are all hypothesized to be potential confounders in the relationship between work and short sleep duration.
Four different models were developed to calculate prevalence ratios (PRs) for industry groups using an industry group with a median prevalence of short sleep duration as a reference group. In the first model, we only adjusted for demographic factors (age, sex, race, ethnicity, marital status, and education), in order to avoid potential “overadjustment” by factors likely to be consequences of short sleep, which could result in underestimation of the relationship between job and sleep duration.42,43 In the second model, we adjusted for both demographic factors and health behaviors (smoking, alcohol consumption, physical inactivity, and obesity) which have previously been shown to be associated with short sleep duration and vary by industry. In the third model, we added a measure of overall health status that has been shown to be associated with short sleep duration and vary by industry. Finally, in the fourth model, we added job characteristics (long work hours and multiple jobs) hypothesized to affect sleep duration. We used the fourth model for the additional analyses of occupational groups within the high-prevalence industry categories. Results for industry and occupation groups with sample sizes < 30 were not reported because of confidentiality concerns and instability of estimates generated from samples this small.
In order to compare the prevalence of short sleep duration by industry over time, we compared NHIS data from 2004-2007 to NHIS data from 1985 and 1990. Although the differences in the NCHS industry and occupation recode systems used before 2004 and those used since 2004 precluded us from making comparisons with earlier time periods at the level of the 21 simple industry recode categories, we were able to sort the industry codes from each time period into 8 broad industry sectors corresponding to the NIOSH National Occupational Research Agenda (NORA) industrial sectors (See http://www.cdc.gov/niosh/NORA/).
We tested the hypothesis that the prevalence of short sleep duration among US workers has increased significantly over time by comparing NHIS data from 1985 and 1990 to data from 2004-2007 within NORA industry categories using the Wald χ2 test. Sleep hour data was available for 1985, 1990, and 2004 to 2007, but was not available between these dates. Weighted mean weekly work hours by industry sector were calculated from 1990 CPS data and 2004-2007 NHIS data.
All analyses were completed using the Software for the Statistical Analysis of Correlated Data (SUDAAN v9.0) package to take into account sample weights and design effects due to the complex sample survey design.44 This allowed us to estimate the total number of employed US civilian workers represented by each individual in the sample. Variance estimates were adjusted for the population survey units, strata, and sampling weights assigned by NCHS.
RESULTS
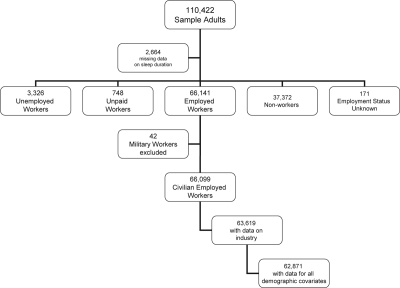
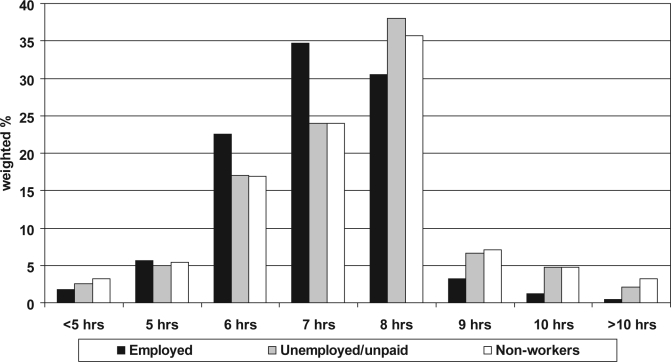
Data were available for 110,422 sample adults in the 2004-2007 NHIS, who represent approximately 219 million non-institutionalized US adults per year. We excluded 2,664 respondents with missing data for sleep duration from all analyses (Figure 1). The distribution of hours of self-reported sleep duration by employment status is shown in Figure 2. For each group except employed workers, the highest proportion of respondents reported sleeping an average of 8 h/day. The highest proportion of employed workers reported sleeping an average of 7 h/day. The overall weighted prevalence of short sleep duration (≤ 6 h/day) was 28.3%, and ranged from 16.1% among respondents with unknown employment status to 29.9% among employed workers.
Figure 1.
Establishment of sample for analysis of self-reported sleep duration, National Health Interview Survey, 2004-2007
Figure 2.
Self-reported sleep duration by employment status, 2004-2007: National Health Interview Survey
Employment status in the week prior to interview
Employed = Working for pay at a job or business or with a job or business but not at work
Unemployed = Looking for work
Unpaid = Working, but not for pay, at a job or business
Non-workers = Not working at a job or business and not looking for work
N = 107,587 (2,835 respondents with missing data on sleep duration or employment status excluded)
The remainder of the analyses focused on employed civilian workers (N = 66,099; representing ∼137 million workers per year). The overall weighted prevalence of short sleep duration within this group was lower in 2007 than in 2004, 2005, or 2006 (Table 1). The lowest prevalence of short sleep duration occurred among the oldest age group (> 65 years), followed by the youngest age group (18-25 years); and the highest prevalence occurred between the ages of 46 and 55. Females had a lower prevalence of short sleep duration than males; Whites had a lower prevalence of short sleep duration than Blacks or persons of other races; Hispanics had a lower prevalence than non-Hispanics; and married persons had a lower prevalence than non-married persons. Smoking, heavy alcohol use, and obesity were associated with an increased prevalence of short sleep duration. Workers who reported no leisure time physical activity had a decreased prevalence of short sleep duration compared to workers who were physically active during their leisure time. Workers who reported fair or poor health status had a much higher prevalence of short sleep duration than workers with excellent, very good, or good health status. Workers with more than one job and workers who worked > 40 h in the last week had an increased prevalence of short sleep duration compared to other workers.
Table 1.
Estimated population prevalence (%) of short sleep duration* among employed civilian US workers, 2004–2007
| Variable | Unweighted sample Size | Estimated annual population (in millions) | Estimated annual cases (in millions) | Weighted prevalence (%, SE†) | PR | 95% CI |
|---|---|---|---|---|---|---|
| Total | 66,099 | 136.8 | 40.9 | 29.9 (0.3) | ||
| 2004 | 18,667 | 133.1 | 40.9 | 30.7 (0.4) | 1.08 | 1.03–1.13 |
| 2005 | 18,875 | 136.6 | 41.2 | 30.2 (0.4) | 1.06 | 1.01–1.12 |
| 2006 | 14,601 | 138.1 | 42.1 | 30.5 (0.5) | 1.08 | 1.03–1.13 |
| 2007 | 13,956 | 139.3 | 39.5 | 28.4 (0.5) | Ref. | |
| By Demographic Characteristics | ||||||
| Sex | ||||||
| Male | 32,956 | 73.9 | 22.6 | 30.7 (0.3) | 1.06 | 1.03–1.09 |
| Female | 33,143 | 62.9 | 18.3 | 29.0 (0.3) | Ref. | |
| Age category | ||||||
| 18–25 y | 8,751 | 21.0 | 5.4 | 25.9 (0.6) | 1.04 | 0.95–1.15 |
| 26–35 y | 15,455 | 30.7 | 9.1 | 29.8 (0.5) | 1.20 | 1.10–1.31 |
| 36–45 y | 16,679 | 33.8 | 10.7 | 31.7 (0.5) | 1.28 | 1.17–1.40 |
| 46–55 y | 14,989 | 31.7 | 10.1 | 31.9 (0.5) | 1.28 | 1.17–1.40 |
| 56–65 y | 7,965 | 15.7 | 4.5 | 28.9 (0.6) | 1.16 | 1.06–1.28 |
| > 65 y | 2,260 | 3.9 | 1.0 | 24.8 (1.0) | Ref. | |
| Race | ||||||
| White | 52,058 | 118.2 | 36.0 | 28.8 (0.3) | Ref. | |
| Black | 9,733 | 15.4 | 5.8 | 37.2 (0.7) | 1.29 | 1.24–1.35 |
| Other | 4,308 | 8.7 | 2.8 | 31.5 (0.9) | 1.10 | 1.03–1.16 |
| Ethnicity | ||||||
| Non-Hispanic | 53,860 | 118.2 | 36.0 | 30.5 (0.3) | 1.15 | 1.10–1.20 |
| Hispanic | 12,239 | 18.6 | 4.9 | 26.4 (0.6) | Ref. | |
| Marital Status | ||||||
| Married | 35,022 | 87.8 | 25.5 | 29.0 (0.3) | Ref. | |
| Not married | 30,841 | 48.6 | 15.4 | 31.6 (0.4) | 1.09 | 1.06–1.12 |
| Education | ||||||
| < 16 y | 26,066 | 52.9 | 16.0 | 30.3 (0.4) | 1.02 | 0.99–1.05 |
| 16 y or more | 39,556 | 82.9 | 24.7 | 29.8 (0.3) | Ref. | |
| By Health Behaviors | ||||||
| Current smoker | ||||||
| Yes | 14,116 | 29.2 | 10.4 | 35.7 (0.6) | 1.26 | 1.22–1.31 |
| No | 51,190 | 105.9 | 29.9 | 28.3 (0.3) | Ref. | |
| Heavy alcohol user§ | ||||||
| Yes | 15,229 | 32.8 | 10.6 | 32.2 (0.5) | 1.11 | 1.07–1.15 |
| No | 50,077 | 102.3 | 29.8 | 29.1 (0.3) | Ref. | |
| Physically inactive¶ | ||||||
| Yes | 22,793 | 44.4 | 13.1 | 29.5 (0.4) | 0.98 | 0.95–1.01 |
| No | 42,513 | 90.7 | 27.3 | 30.1 (0.3) | Ref. | |
| Obese** | ||||||
| Yes | 15,972 | 32.7 | 11.9 | 36.2 (0.5) | 1.30 | 1.26–1.34 |
| No | 49,334 | 102.4 | 28.5 | 27.9 (0.3) | Ref. | |
| By Self-reported health status | ||||||
| Excellent/very good/good | 61,878 | 129.0 | 37.7 | 29.2 (0.3) | Ref. | |
| Fair/poor | 4,206 | 7.7 | 3.3 | 42.2 (1.0) | 1.45 | 1.38–1.51 |
| By Work Characteristics | ||||||
| Number of current jobs | ||||||
| 1 | 60,410 | 124.8 | 36.6 | 29.3 (0.3) | Ref. | |
| > 1 | 5,303 | 11.2 | 4.1 | 37.0 (0.8) | 1.26 | 1.20–1.32 |
| Weekly work hours | ||||||
| ≤ 40 | 46,872 | 95.8 | 26.0 | 27.1 (0.3) | Ref. | |
| > 40 | 18,434 | 39.3 | 14.4 | 36.6 (0.4) | 1.35 | 1.31–1.39 |
Short sleep duration defined as ≤ 6 h/24-h period
Standard error estimated by SUDAAN (v9.0)
Heavy alcohol use defined as having had 5 or more drinks in 1 day in the past year
Physically inactive defined as never engaging in any moderate or vigorous leisure-time physical activity
Obese defined as a body mass index ≥ 30
The analysis of short sleep duration by industry excluded respondents with missing data for age, sex, race/ethnicity, education, marital status, industry and/or occupation, for a final sample of 62,871 workers (Figure 1, Table 2). Among industry categories, the weighted prevalence of short sleep duration was greatest for management of companies and enterprises (40.5%), followed by transportation and warehousing (37.1%), manufacturing (34.8%), and public administration (33.5%). These prevalences represent approximately 38,000 workers in the management of companies and enterprises industry group, 2 million workers in the transportation and warehousing industry group, 5 million workers in the manufacturing industry group, and 2 million workers in the public administration industry group experiencing short sleep duration each year. The lowest prevalence of short sleep duration (23.1%) occurred among the agriculture, forestry, fishing, and hunting industries (Table 2).
Table 2.
Estimated prevalence (%) of short sleep duration* by industry sectors, United States, 2004–2007
| Industry sector (NAICS 2002) | Unweighted sample size | Estimated population(in 1000s) | Estimated number of workers with short sleep duration (in 1000s) | Weighted prevalence (%, SE†) | Model 1:industry + demographicsPR (95% CI) § | Model 2:industry + demographics+ health behaviorsPR (95% CI)¶ | Model 3:industry + demographics+ health behaviors +health statusPR (95% CI)** | Model 4:industry + demographics+ health behaviors +health status +job characteristicsPR (95% CI)‡ |
|---|---|---|---|---|---|---|---|---|
| Management of companies and enterprises (55) | 41 | 93.34 | 37.80 | 40.5 (9.4) | 1.30 (0.82-2.04) | 1.22 (0.73-2.03) | 1.24 (0.74-2.06) | 1.27 (0.79-2.05) |
| Transportation and warehousing (48-49) | 2,696 | 5565.43 | 2064.92 | 37.1 (1.2) | 1.15 (1.07-1.24) | 1.13 (1.05-1.21) | 1.13 (1.05-1.21) | 1.11 (1.03-1.20) |
| Manufacturing (31-33) | 7,026 | 15162.27 | 5276.06 | 34.8 (0.7) | 1.11 (1.04-1.18) | 1.11 (1.04-1.17) | 1.11 (1.04-1.18) | 1.09 (1.03-1.16) |
| Public administration (92) | 3,201 | 6508.39 | 2179.68 | 33.5 (1.1) | 1.05 (0.98-1.14) | 1.05 (0.98-1.13) | 1.05 (0.98-1.13) | 1.07 (1.03-1.11) |
| Information (51) | 1,589 | 3367.48 | 1056.76 | 31.4 (1.7) | 1.01 (0.90-1.13) | 1.02 (0.91-1.14) | 1.02 (0.92-1.14) | 1.03 (0.93-1.15) |
| Health care and social assistance (62) | 8,310 | 16065.03 | 5012.83 | 31.2 (0.6) | 1.02 (0.96-1.08) | 1.02 (0.96-1.08) | 1.02 (0.96-1.08) | 1.03 (0.97-1.09) |
| Administrative support, waste management, and remediation services (56) | 2,737 | 3395.09 | 1651.37 | 30.6 (1.1) | 0.99 (0.91-1.07) | 0.98 (0.90-1.06) | 0.97 (0.90-1.06) | 0.98 (0.91-1.06) |
| Utilities (22) | 527 | 1201.86 | 368.07 | 30.6 (2.3) | 0.97 (0.83-1.13) | 0.96 (0.83-1.12) | 0.97 (0.83-1.13) | 0.99 (0.85-1.15) |
| Accommodation and food service (72) | 3,837 | 7600.49 | 2306.50 | 30.4 (0.9) | 1.02 (0.95-1.10) | 1.01 (0.94-1.09) | 1.01 (0.93-1.09) | 1.01 (0.94-1.09) |
| Retail trade (44-45) | 6,447 | 13821.80 | 4163.28 | 30.1 (0.7) | 1.00 | 1.00 | 1.00 | 1.00 |
| Arts, entertainment, and recreation (71) | 1,199 | 2485.33 | 742.06 | 29.9 (1.7) | 0.98 (0.87-1.10) | 0.99 (0.88-1.11) | 0.99 (0.88-1.11) | 0.99 (0.89-1.13) |
| Wholesale trade (42) | 1,898 | 4162.37 | 1196.70 | 28.8 (1.3) | 0.93 (0.84-1.02) | 0.92 (0.84-1.02) | 0.93 (0.84-1.03) | 0.91 (0.82-1.00) |
| Mining (21) | 252 | 605.70 | 170.87 | 28.2 (3.2) | 0.91 (0.72-1.15) | 0.90 (0.71-1.13) | 0.90 (0.72-1.14) | 0.85 (0.67-1.08) |
| Construction (23) | 4,778 | 10507.84 | 2947.89 | 28.1 (0.9) | 0.90 (0.84-0.98) | 0.90 (0.83-0.97) | 0.90 (0.83-0.97) | 0.91 (0.84-0.98) |
| Finance and insurance (52) | 3,001 | 6233.08 | 1747.40 | 28.0 (1.0) | 0.92 (0.84-1.00) | 0.93 (0.85-1.02) | 0.93 (0.86-1.02) | 0.94 (0.86-1.02) |
| Professional, scientific, and technical service (54) | 3,811 | 8272.35 | 2270.22 | 27.4 (0.9) | 0.89 (0.83-0.96) | 0.91 (0.85-0.98) | 0.91 (0.85-0.97) | 0.91 (0.85-0.98) |
| Real estate, rental, and leasing (53) | 1,369 | 2856.26 | 778.01 | 27.2 (1.5) | 0.89 (0.80-1.00) | 0.89 (0.79-1.00) | 0.89 (0.80-1.00) | 0.89 (0.80-1.00) |
| Other services, except public administration (81) | 3,251 | 6582.17 | 1772.49 | 26.9 (0.9) | 0.88 (0.81-0.96) | 0.89 (0.82-0.96) | 0.88 (0.81-0.96) | 0.88 (0.81-0.95) |
| Education services (61) | 6,092 | 12488.11 | 3330.99 | 26.7 (0.7) | 0.88 (0.82-0.94) | 0.90 (0.85-0.97) | 0.91 (0.85-0.97) | 0.92 (0.86-0.98) |
| Agriculture, forestry, fishing, and hunting (11) | 809 | 1673.39 | 387.17 | 23.1 (1.8) | 0.78 (0.66-0.91) | 0.78 (0.66-0.91) | 0.78 (0.67-0.91) | 0.74 (0.63-0.86) |
| Total | 62,871 | 130647.79 | 39461.06 | 30.2 (0.3) | ||||
Short sleep duration defined as ≤ 6 h/24-h period
Standard error estimated by SUDAAN (v9.0).
In Model 1, prevalence ratios (PR) are adjusted for demographic covariates (age, sex, race, ethnicity, marital status, and education).
In Model 2, prevalence ratios (PR) are adjusted for demographic covariates and health behaviors (smoking, alcohol consumption, physical inactivity, and obesity)
In Model 3, prevalence ratios (PR) are adjusted for demographic covariates, health behaviors, and health status
In Model 4, prevalence ratios (PR) are adjusted for demographic covariates, health behaviors, health status, and job characteristics (long work hours and multiple jobs)
The retail trade industry ranked 10th out of the 20 industry groups in prevalence of short sleep duration (30.1%), and was used as a reference group for calculation of prevalence ratios. Compared to workers in the retail trade industry, workers in the transportation and warehousing (Model 1 PR = 1.15; 95% CI 1.07-1.24) and manufacturing (Model 1 PR = 1.11; 95% CI 1.04-1.18) industries were significantly more likely to report short sleep duration. The significant findings for the prevalence of short sleep duration by industry were the same across the 4 models, with the exception that the PR for public administration became significant in the fourth model (i.e., the PRs for the transportation and manufacturing industries remained elevated across all 4 models). The magnitude of the elevated PRs was slightly attenuated with the addition of heath behaviors, health status, and job characteristics to the models (Table 2).
Within the transportation/warehousing, manufacturing, and public administration industry groups, the prevalence of short sleep duration was calculated by occupational group, and the 5 occupational groups with the highest prevalence within each of these industry groups are shown in Table 3. Of the industry-occupation pairs examined, the weighted prevalence of short sleep duration was highest for production occupations in the transportation and warehousing industry (44.9%; representing 37,000 workers with short sleep duration annually), followed by installation, maintenance, and repair occupations in the transportation and warehousing industry (43.4%; representing 124,000 workers with short sleep duration annually) and transportation and material moving occupations in the public administration industry (43.0%; representing 43,000 workers with short sleep duration annually). Among the industry-occupation pairs examined, the largest numbers of workers with short sleep duration annually were found in production workers within the manufacturing industry (2.6 million) and transportation and material moving occupations within the transportation and warehousing industry group (∼960,000).
Table 3.
Estimated prevalence (%) of short sleep duration* by occupation within high-prevalence industries United States, 2004–2007
| Industry Sector (NAICS 2002) / Occupation | Unweighted sample size | Estimated population(in 1000s) | Estimated number of workers with short sleep duration (in 1000s) | Weighted prevalence (%, SE†) | PR§ | 95 % CI |
|---|---|---|---|---|---|---|
| Transportation and Warehousing (48-49) | ||||||
| Production occupations | 41 | 82.68 | 37.09 | 44.9 (9.2) | 1.45 | 0.94–2.23 |
| Installation, maintenance, and repair occupations | 127 | 285.20 | 123.87 | 43.4 (4.9) | 1.35 | 1.08–1.69 |
| Management occupations | 186 | 413.82 | 168.46 | 40.7 (4.4) | 1.28 | 1.03–1.58 |
| Building and grounds cleaning and maintenance occupations | 31 | 48.21 | 18.05 | 37.4 (9.9) | 1.29 | 0.77–2.16 |
| Transportation and material moving occupations | 1,231 | 2576.64 | 962.14 | 37.3 (1.8) | 1.12 | 1.00–1.25 |
| Manufacturing (31-33) | ||||||
| Installation, maintenance, and repair occupations | 289 | 683.90 | 281.20 | 41.1 (3.3) | 1.25 | 1.06–1.48 |
| Production occupations | 3,319 | 6881.85 | 2606.11 | 37.9 (1.0) | 1.20 | 1.12–1.29 |
| Building and grounds cleaning and maintenance occupations | 88 | 179.74 | 65.23 | 36.3 (6.1) | 1.16 | 0.83–1.61 |
| Transportation and material moving occupations | 599 | 1363.29 | 485.12 | 35.6 (2.4) | 1.12 | 0.97–1.29 |
| Architecture and engineering occupations | 401 | 888.45 | 291.67 | 32.8 (3.1) | 1.02 | 0.85–1.23 |
| Public Administration (92) | ||||||
| Transportation and material moving occupations | 47 | 100.36 | 43.12 | 43.0 (9.4) | 1.37 | 0.93–2.01 |
| Protective service occupations | 781 | 1671.53 | 639.11 | 38.2 (2.1) | 1.16 | 1.03–1.31 |
| Healthcare practitioners and technical occupations | 104 | 200.53 | 76.34 | 38.1 (5.1) | 1.18 | 0.91–1.52 |
| Architecture and engineering occupations | 77 | 175.90 | 65.93 | 37.5 (6.8) | 1.30 | 0.93–1.82 |
| Computer and mathematical occupations | 116 | 256.67 | 90.93 | 35.4 (5.9) | 1.16 | 0.83–1.62 |
Short sleep duration defined as ≤ 6 h/24-h period
Standard error estimated by SUDAAN (v9.0)
Prevalence ratios (PR) are adjusted for demographic covariates (age, sex, race, ethnicity, marital status, and education), health behaviors (smoking, alcohol consumption, physical inactivity, and obesity), health status, and job characteristics (long work hours and multiple jobs); reference group = all workers employed in retail sales industry
In the combined sample from 1985 and 1990, 24.2% (SD = 0.3%) of workers reported short sleep duration, significantly less than the overall prevalence of short sleep duration among workers in 2004-2007 of 30.1% (SD = 0.3%; P < 0.0001). Differences between the 2 time periods were significant for each of the 8 NORA sectors except mining (Table 4). In 1985/1990, health care was the industry with the highest prevalence of short sleep duration (28.1%). However, in 2004-2007 it ranked third (31.7%) and was exceeded by transportation, warehousing and utilities (36.0%), and manufacturing (34.7%).
Table 4.
Estimated prevalence of short sleep duration by NORA industry sector, United States, 1985 and 1990 compared to 2004–2007
| 1985 and 1990 |
2004–2007 |
P-value F for short sleep duration‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Unweighted sample size (NHIS) | Weighted prevalence (%) of short sleep duration (SE*) | Mean weekly work hours (weighted; from CPS, 1990†) | Prevalence (%) of shift work; (from CPS, 1985§) | Unweighted sample size (NHIS) | Weighted prevalence (%) of short sleep duration (SE*) | Mean weekly work hours (weighted; from NHIS, 2004–2007¶) | Prevalence (%) of shift work; (from CPS, 2004**) | ||
| Agriculture, forestry, fishing, and hunting | 1,222 | 16.9 (1.4) | 44.7 | 10.6a | 826 | 23.1 (1.8) | 45.7 | 9.5 | 0.0025 |
| Mining | 336 | 25.5 (2.7) | 45.9 | 21.9 | 252 | 28.2 (3.2) | 49.3 | 31.5 | 0.4328 |
| Construction | 2,567 | 22.2 (1.0) | 40.9 | 2.5 | 4,832 | 28.0 (0.9) | 42.1 | 2.8 | < 0.0001 |
| Manufacturing | 8,572 | 27.0 (0.6) | 42.4 | 17.9 | 7,108 | 34.7 (0.7) | 43.6 | 17.7 | < 0.0001 |
| Transportation, Warehousing and utilities | 3,129 | 27.3 (1.0) | 42.8 | 20.6 | 3,252 | 36.0 (1.0) | 43.2 | 27.8 | < 0.0001 |
| Wholesale and retail trade | 8,058 | 23.4 (0.6) | 39.9 | 26.3b | 8,423 | 29.7 (0.6) | 39.6 | 22.0 | < 0.0001 |
| Services | 17,291 | 22.7 (0.4) | 39.9 | 38.4c | 32,011 | 28.8 (0.3) | 39.0 | 36.1c | < 0.0001 |
| Health care | 3,871 | 28.1 (0.9) | 39.1 | 27.0d | 6,915 | 31.7 (0.7) | 38.8 | 19.0 | 0.0012 |
| Total | 45,046 | 24.2 (0.3) | 40.7 | 15.9 | 63,619 | 30.1 (0.3) | 40.2 | 17.7 | < 0.0001 |
Standard error estimated by SUDAAN (v9.0).
CPS data obtained from the website of the National Bureau of Economic Research (http://www.nber.org/data/cps_basic.html)
Reference: Mellor EF. Shift work and flexitime: how prevalent are they? Monthly Labor Review. 1986; November:14-21.
Excludes 1,391 respondents without valid data for mean weekly work hours.
Reference: McMenamin TM. A time to work: Recent trends in shift work and flexible schedules. Monthly Labor Review 2007; December:3-15.
Compares the prevalence of short sleep duration between 1985, 1990 and 2004-2007 using the Wald χ2 test.
Excludes forestry and fishing workers.
Excludes wholesale trade workers
Based on all workers in service occupations, including health care workers; data for all service industries not available
Hospital workers only
The average work hours for each sector, based on 2004-2007 NHIS data are also shown in Table 4. Work hour data were not collected in the NHIS in 1985 or 1990, but work hour data from the 1990 CPS are shown for comparison. Work hours do not appear substantially different between the 2 time periods overall or within most sectors, but caution is advised when comparing these data from 2 different surveys. Although data on shifts worked are not available from the NHIS, previously published data on the prevalence of shift work by industry from supplements to the CPS in 198545 and 200446 are shown in Table 4 as a reference.
DISCUSSION
To the best of our knowledge, this is the first paper to estimate the prevalence of short sleep duration (defined as ≤ 6 h of self-reported sleep per day) by occupational category in the US and by industry category in any country. We found that self-reported short sleep duration among US workers currently affects approximately 30% of the working population, approximately 40 million workers annually. Furthermore, we found evidence that the prevalence of short sleep duration among workers has increased over the past two decades, even though the average number of hours worked per week may have decreased slightly.
We found modestly increased prevalence ratios for short sleep duration among workers in certain industry and occupational groups compared to workers in an industry group with an average (median) prevalence of short sleep duration. Although the PRs were all less than 1.5, they represent substantial numbers of workers with short average sleep duration, who may be at risk for both morbidity and mortality related to short sleep duration and for workplace injuries and impaired work performance. In addition, we found several industry groups (e.g., agriculture, forestry, and fishing; education services; mining) with prevalences of short sleep duration well below the median, suggesting that much better sleep patterns are possible. Differences by industry remained after adjustment for health behaviors, health status, work hours, and multiple jobs.
Among workers currently employed in the civilian sectors, we found the highest prevalence of short sleep duration within the industry group “Management of companies and enterprises,” but the prevalence ratio for this group compared to the median prevalence group (retail industry) was not significantly elevated which may be due to the small sample size (N = 41). This category represents a sector newly added to the 1997 version of NAICS (sector 55), and comprises: 1) business establishments that hold the securities of companies for the purpose of owning a controlling interest or influencing management decisions; and 2) establishments that administer, oversee, and manage their overall company or enterprise (e.g., corporate offices, head offices, and centralized administrative offices which achieve economies of scale by consolidating these services from across other establishments of the company). It has been suggested that this sector is underrepresented because survey respondents tend not to provide the kind of information needed to distinguish workers in the management establishment of a larger corporation or enterprise from those that work in the production or service-providing establishments of the same company.47 Our study suggests a need for further study of the health habits and needs of this group of workers.
The industry groups with prevalences of short sleep duration significantly above the median (transportation and warehousing, manufacturing, and public administration) appear to be industries likely to operate on a 24-h/day schedule based on working shifts. A 2004 supplement to the Bureau of Labor Statistics' Current Population Survey found that wage and salary workers in food services, transportation and warehousing, and nondurable goods manufacturing were among the groups most likely to usually work an alternate (other than regular daytime) shift.46
The effects of such work shifts on sleep duration may be exacerbated by excessive work hours in some groups. According to the 2004-2007 NHIS data (Table 4), workers in the manufacturing and transportation industries averaged some of the highest weekly work hours, after mining and agriculture and related industries.
Adverse impacts of long work hours and insufficient sleep and other sleep problems on workplace safety and job performance have been described for truck drivers, medical interns, and Japanese workers in small and medium-scale (mostly manufacturing) enterprises.13–15 Specifically, truck drivers had significantly less sleep (measured by actigraghy) prior to critical incidents (crashes, near-crashes, and crash-relevant conflicts)13; medical interns exhibited both decreased sleep and increased attentional failures (validated by electrooculography and polysomnography) during periods with extended work shifts14; and, Japanese workers who reported insufficient sleep and other sleep problems were more likely to report any occupational injuries in the past year.15 Because the consequences of exhaustion and fatigue among truck drivers and railroad workers, and among health care workers may adversely impact public health and safety, there have been efforts to regulate extreme working hours in these two industries.31 (See http://www.ntsb.gov/publictn/1999/SR9901.pdf and http://www.govtrack.us/congress/bill.xpd?bill=h110-2095 for more information on transportation workers and http://www.acgme.org/DutyHours/dutyhoursummary2003-04.pdf for information on medical residents). There is evidence that truck drivers' average sleep duration has increased since stricter regulations were promulgated in 2003,13 and at least one clinical trial has suggested that reducing work hours has increased sleep duration, as well as decreased attentional failures, among medical interns.14
Interestingly, within the transportation and warehousing industry group, we found higher prevalences of short sleep duration among production and installation, maintenance, and repair occupations than among transportation and material moving occupations; but the prevalence of short sleep duration among transportation and material moving occupations in the transportation and warehousing industry was also significantly higher than among the median worker group, suggesting that despite the regulations, both truck drivers and other workers in the transportation industry may continue to experience insufficient sleep.
Early morning start times, night shifts, and rotating shifts may also be a factor in explaining short sleep duration. Unfortunately, the NHIS did not collect data on workers' shift schedules, but other studies, such as the Helsinki Heart Study and the 2004 CPS supplement, have found a high prevalence of irregular schedules among traffic and transportation workers.26,46
We found the lowest prevalence of short sleep duration in the agriculture, forestry, fishing, and hunting industry category. Although farmers and others in these categories often work long hours and start working early in the morning, it seems logical that since their work schedules are more attuned to natural light-dark cycles, and may be more flexible compared to the schedules of other workers, work may interfere less with natural sleep habits. According to CPS supplements that measured shift work, approximately 10% of agricultural workers report working non-standard shifts, which is considerably lower than manufacturing or transportation workers, but much higher than construction workers, who were more likely to report short sleep duration in our study.46 Consistent with the present estimate of 23.1% prevalence of short sleep duration among farmers and related workers, Spengler et al found a prevalence of short sleep duration (≤ 6 h of self-reported daily sleep) among part-time Kentucky farmers of 24.3%.48
Most previous studies in which sleep duration or quality were determined by occupation have used very broad categories, compared to the categories presented here.49,50 Two exceptions are a Finnish study published in 1984, in which differences in the prevalence of difficulty falling asleep, frequent nighttime wakening, and early wakening among workers in 40 occupational groups were assessed51 and a recent Norwegian study in which sleep duration was compared among 7 occupational categories.52 Some of our findings regarding variation in prevalence of short sleep duration by industry and occupation are consistent with findings from these studies, although the former study only addressed sleep quality, and our study only addressed sleep quantity. Specifically, Partinen et al51 found the highest frequency of complaints of difficulty falling asleep among male bus drivers and the highest frequency of complaints of frequent awakening among male laborers (who might have been similar to production workers in our study). Ursin et al found that craft workers, plant operators, and drivers slept less than their reference group of “leaders” (legislators, senior officials, and managers)52 Furthermore, Ursin et al found that occupational groups had effects on sleep duration independent of the effects of shift work.
Interestingly, the increase in the prevalence of short sleep duration among workers from 1985/1990 to 2004-2007 does not appear to be explained by substantial increases in work hours nor by changes in shift work. Our analyses and previous analyses of CPS data indicate that average weekly work hours have slightly declined during this time period, while CPS data indicate that the proportion of workers engaged in shift work has increased.33 Furthermore, few of the industry sectors with the highest mean weekly work hours or the highest prevalence of shift work in either time period were among the industry groups with the highest prevalence of short sleep duration, suggesting that the relationship between work hours, shift work and sleep duration may vary by industry sector. Before indulging in speculation about possible predictors of short sleep duration across different industry sectors, we plan to perform more detailed analyses by hours worked, commuting times, other job characteristics, and industry sector.
Limitations
The large sample size and nationally representative sample design of this study allowed reliable estimates of the prevalence of short sleep duration for various industries and occupations. On the other hand, the NHIS provides data on quantity, but not quality of sleep, which may be a limitation; however, duration of sleep has been associated with many aspects of the quality of sleep in other studies that assessed both duration and quality of sleep.3,29,53 For example, Japanese workers who reported symptoms of insomnia (i.e., non-refreshing sleep, difficulty falling asleep, frequent sleep disruption, and early morning arousal) reported significantly shorter average sleep durations29; and clinically diagnosed primary insomniacs have been found to have significantly reduced total sleep time (measured by polysomnography) compared to healthy controls.53
Other limitations to the NHIS data are that sleep duration is self-reported, with no distinction made between sleep duration on weekdays (work days) vs. weekends (non-work days), reported average sleep time is rounded to the nearest hour, and there are no data on work shifts. Self-reported habitual sleep duration has been found to have a modest correlation with sleep duration measured by actigraphy, with higher subjective estimates of sleep duration and variation in the accuracy of self-reported sleep duration by health, sociodemographic, and sleep characteristics.54
We analyzed data by simple NCHS industry and occupation recodes rather than detailed recodes to limit problems caused by small numbers. Trend analyses were further limited by the fact that no data on sleep hours were collected by the NHIS between 1990 and 2004, and industry and occupation recode categories changed between 1990 and 2004; thus comparisons could only be made within broad industry categories.
Finally, the present study was not designed to determine how the differential in the distribution of short sleep duration is related to many specific job characteristics (e.g., job stress, irregular or rotating shifts) or to examine how work and non-work demands/activities (e.g. internet, TV, video games) compete for sleep. Differences in the prevalence within broad industry and occupation categories may be due to changes in not only the nature of jobs but also the composition of jobs within these categories. The present analysis did not reveal the reason(s) driving the increase in the number of workers who are not getting enough sleep.
Furthermore, the differences in sleep duration between industry/occupation groups may be influenced by self-selection of job according to sleep needs, which could not be assessed with this cross-sectional study. People who need a lot of regular sleep might avoid jobs that have irregular schedules and night shifts.
Conclusions
We found a high prevalence of short sleep duration among workers in the transportation/warehousing, manufacturing, and public administration industries, and identified specific occupational groups within these industries with the highest prevalence of short sleep duration. Additionally, analyses suggest that average sleep duration has generally declined among workers over the last two decades. Further explorations of the relationship between work and sleep and development of targeted interventions (i.e., protective legislation or other policy interventions, education and training materials) for specific industry/occupation groups are needed.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors wish to thank Marie Haring-Sweeney, PhD, Thomas Balkin, PhD, Claire Caruso, PhD, Jana Price, PhD, and anonymous reviewers for their review and comments on previous drafts; and Jia Li, PhD, for sharing her statistical expertise.
REFERENCES
- 1.US Department of Health and Human Services, National Center on Sleep Disorders Research. National Sleep Disorders Research Plan. 2003. Available at http://www.nhlbi.nih.gov/health/prof/sleep/res_plan/sleep-rplan.pdf.
- 2.Centers for Disease Control and Prevention. QuickStats: Percentage of Adults Aged > 18 Years Who Reported an Average of < 6 Hours of Sleep per 24-Hour Period, by Sex and Age Group --- National Health Interview Survey, United States, 1985 and 2006. MMWR. 2008;57:209. [Google Scholar]
- 3.National Sleep Foundation. Sleep in America Poll: Summary of Findings. 2008. Available at http://www.sleepfoundation.org/atf/cf/%7Bf6bf2668-a1b4-4fe8-8d1a-a5d39340d9cb%7D/2008%20POLL%20SOF.PDF.
- 4.Bureau of Labor Statistics. American Time Use Survey—2006 Results. Available at http://www.bls.gov/news.release/pdf/atus.pdf.
- 5.Hammond EC. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am J Public Health Nations Health. 1964:11–23. doi: 10.2105/ajph.54.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gangwisch JE, Heymsfield SB, Boden-Albala, et al. Sleep duration associated with mortality, but not middle-aged adults in a large US sample. Sleep. 2008;31:1087–96. [PMC free article] [PubMed] [Google Scholar]
- 7.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: Analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 8.Gottleib DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the sleep heart health study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 9.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 10.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30:1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166:1689–92. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 12.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanowski RJ, Hickman J, Fumero MC, Olson RL, Dingus TA. The sleep of commercial vehicle drivers under the 2003 hours-of-service regulations. Accid Anal Prev. 2007;39:1140–5. doi: 10.1016/j.aap.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 14.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 15.Nakata A, Ikeda T, Takahashi M, et al. Sleep-related risk of occupational injuries in Japanese small and medium-scale enterprises. Ind Health. 2005;43:89–97. doi: 10.2486/indhealth.43.89. [DOI] [PubMed] [Google Scholar]
- 16.Patel SR. Social and demographic factors related to sleep duration. Sleep. 2007;30:1077–8. doi: 10.1093/sleep/30.9.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basner MB, Fomberstein KM, Razavi FM, et al. American Time Use Survey: Sleep time and its relationship to waking activities. Sleep. 2007;30:1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hale L. Who has time to sleep? J Public Health. 2005;27:205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 20.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 21.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: Results of the National Health Interview Survey. J Natl Med Assoc. 2008;100:317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 22.John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with sleep duration in an adult general population sample. J Psychiatr Res. 2005;39:577–83. doi: 10.1016/j.jpsychires.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Schoenborn CA, Adams PF. Sleep duration as a correlate of smoking, alcohol use, leisure-time physical inactivity, and obesity among adults: United States, 2004–2006. NCHS Health E-Stats May 2008. Available at http://www.cdc.gov/nchs/products/pubs/pubd/hestats/sleep04-06/sleep04-06.htm.
- 24.Tucker P, Smith L, Macdonald I, Folkard S. The impact of early and late shift changeovers on sleep, health, and well-being in 8- and 12- hour shift systems. J Occup Health Psychol. 1998;3:265–75. doi: 10.1037//1076-8998.3.3.265. [DOI] [PubMed] [Google Scholar]
- 25.Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23:155–63. [PubMed] [Google Scholar]
- 26.Harma M, Tenkanen L, Sjoblom T, Alikoski T, Heinsalmi P. Combined effects of shift work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scand J Work Environ Health. 1998;24:300–7. doi: 10.5271/sjweh.324. [DOI] [PubMed] [Google Scholar]
- 27.Tachibana H, Izumi T, Honda S, Takemoto TI. The prevalence and pattern of insomnia in Japanese industrial workers: relationship between psychosocial stress and type of insomnia. Psychiatry Clin Neurosci. 1998;52:397–402. doi: 10.1046/j.1440-1819.1998.00407.x. [DOI] [PubMed] [Google Scholar]
- 28.Nakata A, Haratani T, Takahashi M, et al. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc Sci Med. 2004;59:1719–30. doi: 10.1016/j.socscimed.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Ota A, Masue T, Yasuda N, Tsutsumi A, Mino Y, Ohara H. Association between psychosocial job characteristics and insomnia: an investigation using two relevant job stress models—the demand-control-support (DCS) model and the effort-reward imbalance (ERI) model. Sleep Med. 2005;6:353–8. doi: 10.1016/j.sleep.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Burgard S, Ailshire J. Putting work to bed: Stressful experiences on the job and sleep quality. Population Studies Center Research Report 08-652. 2008. Jul, Available at http://www.psc.isr.umich.edu/pubs/pdf/rr08-652.pdf. [DOI] [PMC free article] [PubMed]
- 31.Johnson JV, Lipscomb J. Long working hours, occupational health and the changing nature of work organization. Am J Ind Med. 2006;49:921–9. doi: 10.1002/ajim.20383. [DOI] [PubMed] [Google Scholar]
- 32.Rones PL, Ilg RE, Gardner JM. Trends in hours of work since the mid-1970s. Monthly Labor Review. 1997 Apr;:3–14. [Google Scholar]
- 33.Kirkland K. On the decline in average weekly hours worked. Monthly Labor Review. 2000 Jul;:26–31. [Google Scholar]
- 34.Kuhn PJ, Lozano FA. The Expanding Workweek? Understanding Trends in Long Work Hours among U.S. Men, 1979–2004. J Labor Econ. 2008;26:311–43. [Google Scholar]
- 35.Rajaratnam SMW, Arendt J. Health in a 24-h Society. Lancet. 2001;358:999–1005. doi: 10.1016/S0140-6736(01)06108-6. [DOI] [PubMed] [Google Scholar]
- 36.Dijk DJ, Duffy JF, Riel E, Shanahan TL, Czeisler CA. Ageing and the circadian and homeostatic regulation of human sleep during forced desynchrony of rest, melatonin and temperature rhythms. J Physiol. 1999;516:611–27. doi: 10.1111/j.1469-7793.1999.0611v.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Czeisler CA, Weitzman ED, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: its duration and organization depend on its circadian phase. Science. 1980;210:1264–7. doi: 10.1126/science.7434029. [DOI] [PubMed] [Google Scholar]
- 38.Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, Roth T. Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiology. 2003;38:979–87. doi: 10.1111/1469-8986.3860979. [DOI] [PubMed] [Google Scholar]
- 39.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 40.Fowler FJ. The redesign of the National Health Interview Survey. Public Health Rep. 1996;111:508–11. [PMC free article] [PubMed] [Google Scholar]
- 41.National Center for Health Statistics. National Health Interview Survey: Research for the 1995–2004 redesign. Vital Health Stat 2(126) 1999 [PubMed] [Google Scholar]
- 42.Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–95. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.VanderWeele T. On the relative nature of overadjustment and unnecessary adjustment. Epidemiology. 2009;20:496–9. doi: 10.1097/EDE.0b013e3181a82f12. [DOI] [PubMed] [Google Scholar]
- 44.Research Triangle Institute. SUDAAN Language Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2004. [Google Scholar]
- 45.Mellor EF. Shift work and flexitime: how prevalent are they. Monthly Labor Review. 1986 Nov;:14–21. [Google Scholar]
- 46.McMenamin TM. A time to work: Recent trends in shift work and flexible schedules. Monthly Labor Review. 2007 Dec;:3–15. [Google Scholar]
- 47.Scopp TS, U.S. Census Bureau The Relationship between the 1990 Census and Census 2000 Industry and Occupation Classification Systems: Technical Paper #65. 2003. [Published October 30, 2003]. http://www.census.gov/hhes/www/ioindex/pdfio/techpaper2000.pdf.
- 48.Spengler SE, Browning SR, Reed DB. Sleep deprivation and injuries in part-time Kentucky farmers: Impact of self reported sleep habits and sleep problems on injury risk. AAOHN J. 2004;52:373–82. [PubMed] [Google Scholar]
- 49.Kronholm E, Harma M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006;15:276–90. doi: 10.1111/j.1365-2869.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- 50.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. Sleep. 2006;29:206–16. doi: 10.1093/sleep/29.2.206. [DOI] [PubMed] [Google Scholar]
- 51.Partinen M, Eskelinen L, Tuomi K. Complaints of insomnia in different occupations. Scand J Work Environ Health. 1984;10:467–9. doi: 10.5271/sjweh.2297. [DOI] [PubMed] [Google Scholar]
- 52.Ursin R, Baste V, Moen BE. Sleep duration and sleep-related problems in different occupations in the Hordaland Health Study. Scand J Work Environ Health. 2009;35:193–202. doi: 10.5271/sjweh.1325. [DOI] [PubMed] [Google Scholar]
- 53.Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Reimann D. Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety. 2003;17:162–72. doi: 10.1002/da.10101. [DOI] [PubMed] [Google Scholar]
- 54.Lauderdale DA, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]