Abstract
Study Objectives:
A lapse during the psychomotor vigilance task (PVT) is usually defined as a response longer than 500 ms; however, it is currently unknown what psychobiological phenomena occur during a lapse. An assessment of what a participant is doing during a lapse may depict varying levels of “disengagement” during these events and provide more insight into the measurement of both a lapse and sleepiness.
Design:
Repeated measures
Setting:
Participants underwent extended 30-min PVT sessions twice, at 22:00 and 04:00, under: (i) typical non-distractive laboratory conditions, and (ii) an additional distractive condition.
Participants:
Twenty-four healthy young adults (mean age: 23.2 y ± 2 y; range 21-25 y [12 m; 12 f]) without any sleep or medical problems and without any prior indication of daytime sleepiness.
Interventions:
One night of sleep loss. Distraction comprised a TV located at 90° in the visual periphery showing a popular TV program. For the non-distraction condition, the TV was turned off.
Measurements and Results:
Video data (bird's-eye and frontal view) were used to classify each lapse (≥500 ms) as occurring with eyes open (EO), eyes closed (EC), or due to a head turn (HT). EO lapses were more prevalent, with all lapses (EO, EC, and HT) increasing with sleepiness. There was a significant effect of distraction for HT lapses which was exacerbated when sleepy. For lapse duration there was little effect of sleepiness for EO lapses but a significant effect for EC and HT. The 95% confidence intervals for lapse duration and associated behavior showed those lapses greater than 2669 ms were 95% likely to be EC, whereas those 500-549 ms were 95% likely to be EO. Response times of 1217 ms had a 50:50 probability of being EO:EC.
Conclusions:
Discriminating the varying causes of lapses whether due to visual inattention (eyes open), microsleep (eyes closed), or distraction (head turn) may provide further insight into levels of disengagement from the PVT and further insight into developing sleepiness.
Citation:
Anderson C; Wales AWJ; Horne JA. PVT lapses differ according to eyes open, closed or looking away. SLEEP 2010;33(2):197-204.
Keywords: Lapse, PVT, sleepiness, distraction, behavior
NUMEROUS STUDIES HAVE SUGGESTED VIGILANCE AND SELECTIVE ATTENTION TO BE THE MOST SENSITIVE MECHANISMS TO ACCOUNT FOR THE detrimental effects of sleep deprivation. Relying on the ability to sustain attention and respond to an unprepared stimulus in a timely fashion, the psychomotor vigilance task (PVT) is the most widely used performance task used to assess sleepiness, and has been validated for sensitivity to various forms of sleep loss,1–5 circadian variation6–10 and subjective ratings of sleepiness.11 Whilst decreased reaction times, increased response time variability and increased false alarms are PVT outcome variables,12,13 the key sign of impairment is the lapse,14 often thought to be a “microsleep.”15–17 Since the 1980s, a lapse on the PVT has been defined as a response > 500 ms, yet while this cutoff has been used successfully to discriminate varying levels of sleepiness,1–5 making it a hallmark of the sleep deprived state, the neurobehavioral factors that account for “why” a lapse occurs is poorly understood.
Several early studies18–21 pre-empted the lapse hypothesis, with the most notable being Bills' “blocks.”19 Bills arbitrarily defined “blocks” as a “pause in the responses equivalent to the time of two or more average responses”19 which increased in duration and frequency with increasing fatigue. In 1949 Bjerner20 defined blocks more in terms of “lapses” which became the accepted terminology with the ensuing, influential lapse hypothesis proposed by Williams et al.22 and later shaped by Kjellberg.23 Wilkinson further refined this area of research,24–28 but, curiously, did not measure lapses or blocks. The general acceptance of the arbitrary definition of the lapse being a doubling of the subject's baseline RT remained until the late 1980s, when Dinges introduced the PVT29 and labelled the lapse as a response > 500 ms.29–31 This 500-ms criterion has become widely accepted as the key indicator of performance impairment on the PVT.
The > 500-ms lapse is undoubtedly highly sensitive to the effects of sleep deprivation, showing clear dose-response effects of prior sleep.1,2 Lapses during the waking state have been seen to be caused by state instability,4 which posits that performance during sleep deprivation is variable due to competing sleep initiating and endogenous wake promoting factors (i.e., effort to remain awake and vigilant). When prior sleep is inadequate and/or circadian pressure for sleep is high, the pressure to sleep, overcoming the will to stay awake, is manifested as a momentary (3-15 sec) protrusion of sleep into the waking state.6
The common belief that a lapse was synonymous with a microsleep15–17 resulting in an inability to respond to stimuli,32 is characterized by a predominance of EEG theta (4-7 Hz) activity without eye blinks.33 However, while the microsleep is certainly responsible for some lapses, it cannot be attributed to all lapses, since participants in a well-rested state occasionally lapse on the PVT (with the eyes open). Recent work using a simple reaction time test (Johns Test of Vigilance-JTV) indicated that sleep deprived individuals can lapse with their eyes open.34,35 Further research shows that some lapses are due to distraction36 caused by looking at irrelevant peripheral stimuli. Thus, not all lapses may be the same, and an assessment of what a participant is doing during a lapse may depict varying levels of “disengagement” during these events, i.e., (1) eye open (visual inattention) versus (2) eyes closed (microsleeps) versus (3) eyes open, gaze diverted (distraction). Accordingly, establishing different characteristics of a PVT lapse may reveal fundamental differences in terms of frequency and duration of lapses, and/or sensitivity to sleep loss, for lapses occurring due to different phenomena.
Changes to eye activities with increasing sleepiness include: percentage of eye closure,37 forced eye closures,38 blink duration,39 pendular motions,40 and saccade velocities.41 Sleep deprivation can cause some eyes open lapses, whether due to an inability to disengage from the current focal spot42 at a slower rate,43,44 a simultaneous blink delaying the response,45 a failure to disengage or inhibit the “default network” to engage in a voluntary response,46 or a global slowing of responses beyond the lapse threshold.26 Nevertheless, an eyes-closed lapse probably reflects a greater degree of task disengagement, as it is likely due to a microsleep and reflected by a slower response time.
While PVT lapses correlate with slow eyelid closures,47–49 no study has systematically assessed PVT lapses in relation to the associated behavior. Despite the well-documented PVT lapse in sleep deprivation literature, surprisingly, no study has as yet characterized what the lapse is. The question of whether subjects are not looking (eyes closed), looking but not seeing (eyes open), or looking but not paying attention (head turn), in addition to whether these also vary in terms of frequency, duration, and sensitivity to sleep loss is unknown. The determination of these factors may well reveal more insight into developing sleepiness and provide a useful categorization of PVT lapse types.
Using a novel experimental protocol whereby lapses are time-framed to video footage, we distinguish between lapses occurring with eyes open (visual inattention), eyes closed (microsleep) and eyes open, with the gaze diverted (distraction) and describe how these evolve in terms of frequency and duration with increasing sleepiness in both normal sterile laboratory environments and with a competing distraction.
METHODS
Participants
Twenty-four healthy, young adults (23.2 ± 2y [mean ± standard deviation]), equal men and women, with no complaint of daytime sleepiness (ESS ≤ 10)50 and reporting sleeping 7-8 h/night, were recruited following interviews, and further screened to exclude those who smoked, had an average intake of alcohol > 4 units (1 unit = 10 mL ethanol) per day, had any sleep or medical problems (other than minor illnesses), or who were on any medication liable to cause daytime sleepiness. To check for stable sleep patterns actiwatches (Cambridge Neurotechnology Ltd., Cambridge, UK) were worn for an initial screening week. Those who slept 8 h ± 1 h per night, and with consistent bed/rise times, were included. The study was approved by Loughborough University's Ethical Advisory Committee. All procedures were fully explained, informed consent given, and participants were paid for their involvement.
Design and Procedure
Participants underwent a single night of sleep loss with testing at 22:00 and 04:00 and under 2 conditions (distraction and no distraction). Each condition lasted for 30 min with a 5-min interim break (total: 65 min). These were counterbalanced across participants.
Subjective sleepiness scales at each time period showed significant effects of sleepiness between the testing periods (correlation between sleepiness and lapses: r = 0.67), so we classified the 22:00 testing period as ALERT and the 04:00 testing period as SLEEPY. For one week previously, participants slept normally at home and were monitored via actigraphy. On the day of the study, they woke up at 08:00 (verified by actigraphy and time-logged phone calls to the laboratory) and went about normal activities. They abstained from alcohol and caffeinated beverages for the remainder of the day. At 18:00 they arrived at the laboratory where saliva (for caffeine), breath (for alcohol), and urine (for recreational drugs [6 drug MultiTest 1; SureScreen Diagnostics]) samples were taken. Participants remained in the laboratory overnight, supervised by 2 experimenters to ensure no sleep episodes. Between testing sessions, they remained in a lounge area and were allowed to read, watch, DVDs or play card/board games. They had a light meal at 03:00, and had free access to non-caffeinated drinks. Participants were taken home by taxi the following day at 06:30.
Distraction versus No Distraction
For distraction condition, a TV showing a popular TV show was shown in the periphery (90° to field of vision); and for no distraction condition, the TV was switched off. On each occasion, the participant was asked to attend fully to the PVT task.
PVT Testing
Participants were seated at a computer screen in a sound attenuated, sterile cubicle with their preferred finger on a response button, with which they responded when a millisecond counter appeared in a small red rectangle box on the screen. Random interstimulus intervals ranged from 2-12 seconds. Task duration was extended from the more typical 10 min to 30 min, in order to maximize sensitivity.
Subjective Sleepiness
Participants rated their subjective sleepiness using the Karolinska Sleepiness Scale before and after each PVT test. This is a 9-point scale ranging from extremely alert (1) to extremely sleepy, fighting sleep (9).
Video Data
During the PVT session, participants were observed, especially during lapses (≥ 500 ms). Two miniature cameras monitored, respectively, a frontal face view and a bird's eye view. Video data were later assessed by 2 independent experimenters blind to the time of day of each recording. These data were time-locked to PVT lapses and each lapse was identified as:
Eyes open (EO), participant staring at the screen
Eyes closed (EC), participant facing toward the screen
Head turn (HT).
A total of 2754 lapses were logged and visually analyzed. Of these, 68.0% (n = 1871) were EO; 25.1% (n = 692) were EC; and 6.9% (n = 191) due to HT.
Statistical Analysis
To normalize the data, the number of lapses were transformed for statistical analysis ((√n) + (√n+1)).15 Repeated measures analyses of variance (ANOVAs) were utilized with Tukey post hoc tests. Two-way ANOVAs assessed differences between “sleepiness” (22:00 vs. 04:00) and “distraction” (Nil Distraction vs. Distraction) for each lapse type. For duration of lapse, a 2*2*3 mixed model ANOVA was used with sleepiness, distraction, and lapse type as factors. Tukey HSD post hoc tests were used to identify contributing factors to main effects. Repeated measures t-tests were used to assess differences in sleepiness ratings, and Pearson r correlation for any correlational analyses.
RESULTS
As expected, subjective sleepiness was significantly greater at 04:00 than 22:00 (t = 6.14, df 1, 23, P < 0.0005 one-tailed), and reflected increased PVT lapses (r = 0.61, P < 0.0005). For all lapses, irrespective of cause, there was a significant main effect of sleepiness (F = 49.8, df 1, 23, P < 0.0005) but no main effect of distraction (P = 0.25). However, there was a significant interaction in that lapses increased in a distractive environment, which was exacerbated when sleepy (F = 3.782, df 1, 23, P < 0.04).
Number of Lapses (≥ 500 ms): Sleepiness x Distraction
For all 2754 lapses (RT ≥ 500 ms): when ALERT, 24.1% of lapses occurred with EO (n = 663), 3.5% (n = 96) with EC, and 2.1% (n = 58) occurred with a HT. When SLEEPY, 43.9% (1208) occurred with EO, 21.6% (n = 596) occurred with EC, and 4.8% (n = 133) with HT. For both ALERT conditions (distraction combined), 92% of subjects (n = 22) exhibited EO lapses, 29% (n = 7) exhibited EC lapses, and 29% (n = 7) exhibited HT lapses. When SLEEPY, all participants exhibited at least one EO lapse, 67% (n = 16) an EC lapse, and 42% (n = 10) a HT lapse.
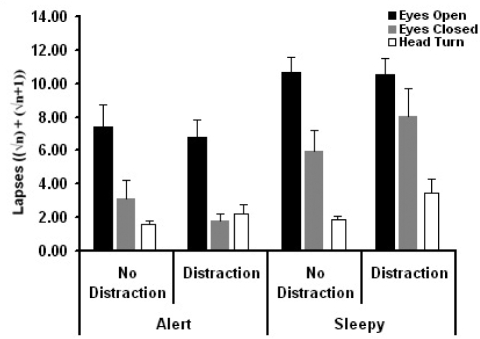
Overall, for number of lapses, there was a significant effect of lapse type (F = 25.38, df 2, 60.39, P < 0.0005). Tukey post hoc tests confirmed that there were more EO lapses than both EC (P < 0.0005) and HT lapses (P < 0.0005). There was a trend for more EC than HT lapses, but this was just above the acceptable level of significance (P = 0.057). As seen in Figure 1, for EO there was a significant effect of sleep (F = 25.27, df 1, 23, P < 0.0005) but no effect of distraction (P = 0.326) nor any interaction (P = 0.619). For EC, there was a significant effect of sleep (F = 18.57, df 1, 23, P < 0.0005) and a sleep*distraction interaction (F = 5.21, df 1, 23, P < 0.04). For EC lapses, there was no main effect of distraction (P = 0.951). For HT, there were significant main effects of sleep (F = 6.47, df 1, 23, P < 0.02) and distraction (F = 4.39, df 1, 23, P < 0.05), and sleep*distraction interaction (F = 4.38, df 1, 23, P < 0.05).
Figure 1.
Frequency of lapses for each condition: A Comparison of eyes open, eyes closed, and head turn lapses. Eyes open lapses were more frequent than all others (P < 0.0005). Eyes open and eyes closed lapses increased when sleepy (P < 0.00005), and lapses caused by distraction (head turn) increased when sleepy which was exacerbated by distraction (P < 0.05).
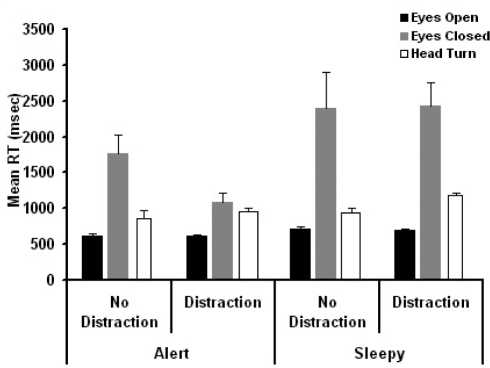
Mean RT for Lapses (≥ 500 ms): Sleepiness x Distraction
Mean reaction times for each lapse type (EO, EC, and HT) was computed for each individual. However, because of the low prevalence of eyes closed lapses and head turn lapses under alert and non-distraction conditions, a 2 * 2 * 3 mixed model analysis was used (Sleep * Distraction * Lapse Type), which accommodates missing data points. For lapse duration, and as seen in Figure 2, there was a significant main effect of sleep (F = 22.01, df 1, 21, P < 0.0005, η2 = 0.51), and lapse type (F = 60.87, df 1, 21, P < 0.0005, η2 = 0.85). There was also a significant sleep*lapse type interaction (F = 16.77, df 2, 21, P < 0.0005, η2 = 0.61), and distraction*lapse type interaction (F = 5.86, df 2, 21, P < 0.009, η2 = 0.36). Tukey post hoc tests for lapse type show EC lapses were longer in duration than both EO (706 ms vs. 3894 ms: P < 0.005) and HT lapses (1270 ms vs. 3894 ms: P < 0.005). When sleepy, eyes closed lapses were exacerbated (2202 ms vs. 4140 ms: P < 0.04).
Figure 2.
Mean reaction time of lapses for each condition: A Comparison of eyes open, eyes closed, and head turn lapses. Eyes closed lapses were longer in duration than lapses occurring with the eyes open (P < 0.0005) and head turns (P < 0.002); they also increased when sleepy (P < 0.0005). Eyes open lapses did not increase in duration when sleepy.
Time on Task—Effect of Lapse Type
The task was split into three 10-min blocks to assess any time on task effect. A 2*2*3 repeated measures ANOVA, with factors sleepiness, distraction and time, was computed. Results are not reported for main effects of distraction or sleep (as these are presented above). For EO and EC lapses, there was a significant effect of time (EO: F = 14.94, df 2, 22, P < 0.0005, η2 = 0.58; EC: F = 5.52, df 2, 22, P < 0.01, η2 = 0.33). There was no significant interaction between time and sleepiness or distraction. For HT lapses, there was no effect of time or any interactions (P > 0.1).
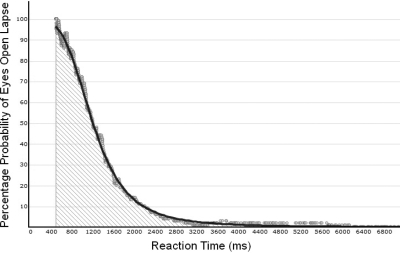
Shift in EO vs. EC as a function of RT
Lapses due to a head turn were removed from this analysis in order to assess the likelihood of the eyes being open or closed as a function of RT. All of the reaction time lapses (≥ 500 ms) in all conditions were first sorted in ascending order with their corresponding behavioral correlates (i.e. 500 ms – EO, 501 ms – EO, etc). Then, a 100-point moving average technique51 was fitted using the following protocol to calculate the x coordinates for Figure 3:
Figure 3.
Example of relationship between mean RT and likelihood of the eyes being open. All lapses were ranked in duration, with each then expressed as percentage of the preceding 100 for EO, creating a 100-point moving average. Using a least squares function fit, the percent of lapses with eyes open (y) for any given lapse duration (x) is shown. A power law function curve was the best fit for the data (r2=0.99) and the resultant formula gives the percentage probability of the eyes being open (y) for any given lapse duration (x). After 7000 ms, the % probability tails off as all lapses had a < 1% chance of occurring with the eyes open.
Where RTx is the reaction time at a given position in the ordered reaction time list (i.e. the 600th data point would be RT600), n is the resolution of the graph (chosen as 100 data points for this study in a sample of over 2,700 data points), and i is the current reaction time position in the iteration sum of reaction times. For the first 100 data points, n is the sum of the first 100 points, which occurred within 7ms from the first to the hundredth point. However, if x = 1500 for example, the sum of reaction times (i) from the 1400th fastest to the 1500th fastest would be divided by 100 to obtain the average, and this would form the 1500th data point on Figure 3. To calculate the corresponding y coordinate data points for each x the following equation is used:
Where EOy is the percentage probability of an eyes-opened lapse occurring at a given y-point (which corresponds with an x-point at the same position such that there is the same number of x-y pairs), n is the resolution of the graph (100), i is the current iteration in the sum, EOi and ECi are the count of lapses within the given n that are attributable to the eyes being either opened or closed. This formula can be expressed as “the previous percentage of lapses that occurred with the eyes open for a given reaction time within a defined bound of 100-lapses.”
As an example of this formula's usage, to calculate the 1500th data point the formulas would be:
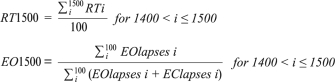 |
While it is possible with a larger sample of data points to increase n to achieve even greater confidence in the estimates, using n = 100 ensured that the ordinate (y-coordinate) would be within a 1% resolution and thus clearly reflect the changing behavior with increasing response times. This can be seen in Figure 3, which shows the percentage chance of a specific reaction time (y) occurring with either EO or EC. A best fitting least squares curve was fitted to the data (power law function - r2 = 0.99) and group means for specific points can be seen in Table 1.
Table 1.
Percentage chance of lapses occurring with eyes open or eyes closed as a function of lapse duration
| Lapse Duration (ms) | Description | % Chance Eyes Open | % Chance Eyes Closed |
|---|---|---|---|
| 549 | 5th Percentile | 95 | 5 |
| 2669 | 95th Percentile | 5 | 95 |
| 907 | Lower Quartile | 75 | 25 |
| 1217 | MIDPOINT | 50 | 50 |
| 1632 | Upper Quartile | 25 | 75 |
| 500-907 | All other lapses | Av. 94.1 | Av. 5.9 |
The resultant formula from the power law curve ([y = (99.8*3.8e11*x^(1-4.75))/(1 + 3.8e11*x^(1-4.75)) for x ≥ 500 where x is RT) was applied to each individual to determine whether the relationship held at an individual level, or whether it was only applicable at the group level. As seen in Table 2, mean RTs falling below the midpoint or 50% level (e.g., 1217 ms) and occurring with EO can be predicted with 85% accuracy. At the 95% level, lapses that occur with a mean RT ' 2669 ms occurring with eyes closed can be predicted with 93% accuracy.
Table 2.
Individual predictability of the decaying power law function model for all subjects applied to individuals.
| Probability Level |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| 50% |
95% |
||||||||
| Ss | EO | No | EC | No | EO | No | EC | No | Individual |
| 1 | 0.84 | 129 | 0.96 | 189 | 0.93 | 56 | 0.99 | 140 | 1156 |
| 2 | 0.84 | 116 | 0.90 | 67 | 0.96 | 48 | 1.00 | 29 | 1012 |
| 3 | 0.93 | 177 | 0.93 | 134 | 0.99 | 67 | 1.00 | 70 | 1290 |
| 4 | 0.97 | 68 | - | 1 | 0.95 | 43 | - | 1 | 1610 |
| 5 | 0.84 | 97 | 0.75 | 16 | 0.98 | 57 | 1.00 | 4 | 932 |
| 6 | 0.99 | 222 | 0.29 | 65 | 1.00 | 118 | 0.43 | 21 | 5458 |
| 7 | 0.96 | 28 | - | 1 | 0.95 | 20 | - | 1 | 910 |
| 8 | 0.48 | 23 | - | 2 | 0.38 | 8 | - | 0 | 923 |
| 9 | 0.98 | 126 | - | 3 | 1.00 | 79 | - | 0 | 1478 |
| 10 | 0.97 | 62 | 0.69 | 13 | 1.00 | 34 | - | 1 | 1392 |
| 11 | 0.64 | 45 | 0.94 | 34 | 0.88 | 16 | 1.00 | 11 | 940 |
| 12 | 0.87 | 106 | 0.75 | 8 | 0.95 | 57 | - | 1 | 943 |
| 13 | 0.50 | 102 | - | 0 | 0.50 | 78 | - | 0 | 907 |
| 14 | 0.79 | 34 | - | 0 | 1.00 | 12 | - | 0 | 867 |
| 15 | 0.63 | 63 | 0.95 | 56 | 0.85 | 27 | 0.96 | 28 | 960 |
| 16 | 1.00 | 22 | 0.57 | 7 | 1.00 | 11 | - | 28 | 1469 |
| 17 | 0.77 | 43 | 0.96 | 52 | 0.95 | 20 | 0.93 | 1 | 898 |
| 18 | 1.0 | 55 | - | 1 | 1.00 | 44 | - | 28 | 1100 |
| 19 | 0.95 | 153 | 0.85 | 13 | 1.00 | 102 | - | 0 | 883 |
| 20 | 0.75 | 183 | 0.91 | 58 | 0.95 | 95 | 0.90 | 0 | 839 |
| 21 | 0.96 | 52 | - | 3 | 1.00 | 40 | - | 10 | 984 |
| 22 | 0.81 | 70 | 0.85 | 13 | 1.00 | 34 | - | 2 | 1612 |
| 23 | 0.96 | 54 | - | 0 | 1.00 | 41 | - | 0 | - |
| 24 | 0.83 | 18 | - | 0 | 1.00 | 13 | - | 0 | 629 |
| Average | 0.85 | 0.81 | 0.93 | 0.91 | 1078.82 | ||||
| SD | 0.15 | 0.19 | 0.16 | 0.19 | 238.97 | ||||
The probability of a lapse being EO when under 1217 ms (50%) is shown for each individual with an average accuracy of 85%. The 95% confidence limits were highly predictive of EC and EO lapses in that lapses occurring above the 95 percentile (2669 ms) were likely to be EC with an average accuracy of 97%. The final column shows the midpoint in milliseconds where the probability of an EC lapse exceeds that of EO for each subject.
Subject six is removed from the average of the individual midpoints due to being an outlier.
DISCUSSION
Despite the PVT lapse being well-documented in the sleep research literature, our study is the first study to examine what occurs during a lapse, to show more clearly that some lapses are caused by participants looking but not seeing (eyes open–visual inattention), not seeing due to the eyes being shut (eyes closed–microsleep), or due to the eyes being open, but the gaze being diverted elsewhere (head turn-distraction). While EO lapses were overall more frequent (n = 1871) than both EC (n = 692) and HT lapses (n = 191), they were less sensitive to the effects of sleepiness. As expected, EC lapses occurred more frequently when SLEEPY than when ALERT (ratio 1:6.21), as did HT lapses (1:2.29). This increased occurrence of lapses when sleepy was less apparent for EO lapses (1:1.82), despite all three lapse types showing a significant effect of increasing sleepiness. Both EO and EC lapses increase as a function of time, whereas distraction lapses remained stable over time.
In a distractive environment, EO lapses also showed little effect of distraction. The ratio of lapses for no distraction vs distraction for EO was 1:0.95, whereas for EC this was 1:1.3. HT lapses showed a dramatic effect of distraction given the ratio between no distraction conditions: 1:9.05. As most studies of sleepiness and performance are undertaken in the sterile laboratory environment, a 9.05-fold increase in lapses in attention caused by distraction is considerable given that working environments are full of potential distracters. Moreover, while distraction results in a 7.25 increase in HT lapses, this further rises to 16.25 when SLEEPY. Our results indicate that HT lapses significantly increase when distracted, but more importantly, this is exacerbated when SLEEPY.
While there is a clear difference in the frequency of EO, EC, and HT lapses, of greater interest is the difference in duration for these lapse types. EO lapses averaged 706 ms in duration compared with 3894 ms for EC and 1270 ms for HT. More specifically, EC lapses were delayed by a further 1938 ms when SLEEPY (2202 ms vs 4140 ms) whereas EO lapses remained unaffected by increasing sleepiness, lengthening only by 30 ms (685 ms vs 715 ms). Although previous work describes the incidence of microsleeps occurring with the eyes open,52 only a few EO lapses were considered long enough in duration to reflect this phenomenon (i.e. EO lapses > 1 second or > 2 seconds = 8.65%, and 1.28%, respectively). Future work should focus on these longer duration EO lapses in order to assess simultaneous signs of an EEG-defined microsleep32,33.
We wanted to assess the impact of a distractive environment on lapses, compared with the more sterile and unrealistic conditions usually adopted for the PVT. Following our previous findings36 of increased lapses and head turns in a distractive environment, here, we assessed whether lapses were caused by head turns per se. Consistent with our previous findings (looking at afternoon sleepiness following a night of restricted sleep), here we report increased lapses irrespective of cause and an increase in head turns when distracted. Of interest, and for lapses overall, compared to ALERT no distraction, there was a 17% reduction in lapses when ALERT but distracted, despite head turns increasing by 294%. Thus, not all head turns resulted in a lapse when ALERT. In contrast, when SLEEPY, the distractive environment increased head turns by 452% and lapses by 246%, indicating more head turns lead to a lapse when SLEEPY. Based on video data, when ALERT it appeared that participants engaged in a strategy to enable them to be distracted but retain performance: participants glanced at the TV screen during the PVT stimulus interval and looked back pre-empting the next stimulus. Due to the partial predictability (i.e., 2-12 sec) of the inter-stimulus interval, this strategic incorporation of distraction was possible, however, when SLEEPY, distraction not only occurred more often but also for longer periods, thus any strategy to incorporate distraction without impairing performance was lost.
It is often assumed that a lapse (RT ≥ 500 ms) is indicative of “long blinks” or eye closure. However, we have shown, albeit specific to our database, that unless the lapse exceeds about 1217 ms at least half of them appear with the EO, with the participant staring at the screen. What underlies these EO lapses remains unclear, but may center on a process termed “blink suppression,”53 a period of 200-250 ms prior to, during, and following a blink that is associated with a general lowering of awareness and characterized by a reduction of activity in the frontal and parietal cortex.53 As such, any stimulus that occurs prior to, during, or immediately following a blink will be delayed.53–55 As blink rate typically averages 15-20 per minute56 this may account for our observed higher frequency of EO lapses. As blink rate is also known to increase with sleepiness,57–60 possibly due to it being controlled in the orbitofrontal cortex,61 this would also be consistent with our findings of an increase in the frequency in EO lapses when SLEEPY (1.82-fold increase). Given a lack of response for c500 ms per blink, blinking on average 20 times per minute, the ability to respond in a timely manner (i.e. < 500ms) even when in an alert state occurs only about 85% of the time, which supports our findings of an elevated number of EO lapses when ALERT, compared with EC or HT. As the lapse is defined as a response greater than 500 ms, some of these particular EO lapses might be captured and may well appear as sleepiness. Future research along these line should capture eye blink data prior to or during EO lapses, by utilizing better techniques than employed here, such as eye scan technologies.
Neuroimaging data suggest that PVT lapses correspond to larger responses in the medial frontal, superior frontal, and ventral anterior cingulated gyrus,46 often referred to as the “default network.”62 This network needs to be inhibited or suspended to actively engage in a goal directed behavior, such as a responding to a stimulus. During sleep loss, this process of disengagement is delayed, thus resulting in a PVT lapse. Lapses occurring with the EO may reflect this delay of allocating cognitive resources to the task, although the extent to which this reflects lapses occurring with EC is unknown, as the neuroimaging study by Drummond et al.46 compared all lapses > 500 ms versus all other reaction times, irrespective of cause.
Our EC lapse is more characteristic of a slow eye movement (SEM) commonly reported during the drowsy state, with a duration of 0.25 Hz6,63,64 and distinct from long eye blinks.65 Given the longer duration of a SEM compared to a long eye blink, the duration of an EC lapse will be longer than an EO lapse. Cajochen et al.6 reported increased SEMs within ~2 h of the onset of melatonin secretion, which would account for our increase in EC lapses at 04:00. Interestingly, these authors described how blink rate closely mirrored the time course of the circadian drive for wakefulness or the alerting signal from the SCN peaking late in the evening. While our study is unable to disentangle the homeostatic/circadian modulation of SEMs/EC lapses, further work may find EC lapses and EO lapses not only respond differently to the homeostatic drive for sleep, as seen here, but also to the circadian drive for sleep and wakefulness.
Whilst we clearly find differences in EO, EC, and HT lapses, further classification of lapses may provide yet further information of what occurs during performance decrements related to drowsiness. Although we find lapses with EO, we are unable to provide information as to exactly “where” the eye was looking except from at the screen (any head turn was classed as distraction and not included in the EO analysis). Although some EO lapses may be due to simultaneous blinks, others may be due to looking elsewhere on the screen, or even looking directly at the stimulus yet having a delayed response. With emerging eye tracking technologies, further important information may be gained from the simple PVT to provide even further insight into developing sleepiness, especially in relation to EO lapses.
Due to time or financial constraints, not all studies are able to utilize eye tracking or camera technologies to identify lapse types. However, given the strong relationship between lapse duration and EO/EC behavior, mean lapse duration may provide further insight than merely frequency of lapses. Although prior work14 has shown that the average number of PVT lapses is highly correlated with lapse duration, this association is only clear for extreme levels of sleep loss (i.e., 88 h TSD, 4-h time in bed for 2 weeks14) and probably reflects more lapses due to SEMs (EC). We found no clear link between number of lapses and lapse duration for EO lapses, whereas this was more evident for EC lapses. As 33% of our data comprised lapses of duration 500-600 ms, with most of these (99%) being EO, this gives a different insight into sleepiness (i.e., increased blink rate), and may hide other important variables due to its prevalence (i.e., more extreme duration lapses associated with EC). Most studies assessing the frequency of PVT lapses may not reveal the extent of impairment, as we indicate that shorter lapses that occur with EO do not reflect sleepiness per se. Numerous studies have shown that subjective sleepiness does not reflect PVT lapses, with most concluding that sleepy people are unable to introspect about their sleepiness. If such studies were to assess EC lapses, this relationship may become more meaningful. By assessing lapse duration, and in particular the frequency or duration of more extreme lapses (beyond 1 s), this may result in a greater association between PVT lapses and EEG66 or PVT lapses and real-world performance.67
Under real-world conditions, such an extended failure to respond due to the eyes being closed, worsening with increasing sleepiness, or with head turns becoming more frequent with increasing distraction, these are clearly more hazardous than an EO lapse. For example, given the lapse duration described here, an EO lapse averaging 659 ms would extend a vehicle's braking distance by 10.98 meters (36 feet) when travelling at 60 kph (37.3 mph), compared with 53.4 m (175 ft) for an EC lapse (average 3199 ms) and 18.5 m (61 ft) for a HT lapse (average 1111 ms). In these respects EC lapses could be described as “major” lapses and EO lapses as more “minor.”
Our data came from two time periods, one later in the evening prior to bedtime, and the other early morning during the sleep period. We also utilized distraction under two conditions. While this provided for a range of sleepiness and lapses, our results regarding the exact RT associated with percentage chance of eye closure should be viewed with caution. Using only one of these time periods, for instance, would have shifted the distributions of EO/EC in one or the other direction. With respect to our findings on the likelihood of EO vs EC lapses, it is likely that other laboratories would also find a decaying power or exponential curve although this would vary with the protocol used, range of sleepiness, surroundings, participant sample etc. More varied and extensive protocols are required to examine the EO vs EC relationships with RTs. Irrespective of this caveat, our findings do highlight that not all lapses are the same, and simply looking at frequency of lapses may mask the contribution of attentional impairment caused by SEMs versus non-sleepy inattention, eye blinks etc. With respect to our 50:50 probability of EO/EC at 1217 ms, this will vary according to experimental circumstances, but we believe that with similar young adults this criterion represents a common psychobiological phenomenon whereby EO lapses are distinct from longer EC lapses. Based on our novel but exploratory findings, we propose that not all PVT lapses above 500 ms should carry the same “sleepiness weighting,” and further discrimination of lapse type and/or lapse duration may reveal important information on performance decrements associated with a loss of sleep.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was funded by the UK Economic and Social Sciences Research Council (ESRC)–grant No. RES-000-23-1583. We would like to thank Katherine Jones for help with data collection.
REFERENCES
- 1.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioural functions and sleep physiology from chronic sleep restriction and total deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 2.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep-dose-response study. J. Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 3.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 4.Doran SM, Van Dongen HP, Dinges DF. Sustained attention performance during sleep deprivation: evidence of state instability. Arch Ital Biol. 2001;139:253–67. [PubMed] [Google Scholar]
- 5.Rogers NL, Dorrian J, Dinges DF. Sleep, waking and neurobehavioural performance. Front Biosci. 2003;8:s1056–s1067. doi: 10.2741/1174. [DOI] [PubMed] [Google Scholar]
- 6.Cajochen C, Khalsa SBS, Wyatt JK, Czeisler CA, Dijk DJ. EEG and ocular correlates of circadian melatonin phase and human performance decrements during sleep loss. Am J Physiol Regul Intergr Comp Physiol. 1999;277:R640–R649. doi: 10.1152/ajpregu.1999.277.3.r640. [DOI] [PubMed] [Google Scholar]
- 7.Graw P, Kräuchi K, Knoblauch V, Wirz-Justice A, Cajochen C. Circadian and wake-dependent modulation of fastest and slowest response times during the psychomotor vigilance task. Physiol Behav. 2004;80:695–701. doi: 10.1016/j.physbeh.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Wyatt JK, Ritz-de Cecco A, Czeisler CA, Dijk DJ. Circadian temperature and melatonin rhythms, sleep, and neurobehavioral function in humans living on a 20-hour day. Am J Physiol Regul Intergr Comp Physiol. 1999;244:R1152–R1163. doi: 10.1152/ajpregu.1999.277.4.r1152. [DOI] [PubMed] [Google Scholar]
- 9.Van Dongen HPA, Dinges DF. Circadian rhythms in fatigue, alertness and performance. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 3rd ed. Philadelphia: WB Saunders; 2000. pp. 391–9. [Google Scholar]
- 10.Cajochen C, Blatter K, Wallach D. Circadian and sleep–wake dependent impact on neurobehavioral function. Psychol Belg. 2004;44:59–80. [Google Scholar]
- 11.Frey DJ, Badia P, Wright KP. Inter- and intra-individual variability in performance near the circadian nadir during sleep deprivation. J Sleep Res. 2004;13:305–15. doi: 10.1111/j.1365-2869.2004.00429.x. [DOI] [PubMed] [Google Scholar]
- 12.Doran SM, Van Dongen HPA, Dinges DF. Sustained attention performance during sleep deprivation: evidence of state instability. Arch Ital Biol. 2001;139:253–67. [PubMed] [Google Scholar]
- 13.Roehrs TA, Carskadon MA, Dement WC, Roth T. Daytime sleepiness and alertness. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 3rd ed. Philadelphia: WB Saunders; 2000. pp. 43–52. [Google Scholar]
- 14.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann NY Acad Sci. 2008;1129:305–22. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 15.Dinges DF, Kribbs NB. Performing while sleepy: effects of experimentally-induced sleepiness. In: Monk TH, editor. Sleep, sleepiness and performance. Chichester, U.K: Wiley; 1991. pp. 97–128. [Google Scholar]
- 16.Williams HL, Lubin A, Goodnow JJ. Impaired performance with acute sleep loss. Psychol Monogr: Gen Appl. 1959;73:1–26. [Google Scholar]
- 17.Horne JA. Oxford University Press; 1988. Why we sleep. [Google Scholar]
- 18.Patrick GTW, Gilbert JA. Studies from the Psychological Laboratory of the University of IOWA. Psychol Rev. 1896;3:468–83. [Google Scholar]
- 19.Bills AG. Blocking: A new principle in mental fatigue. Am J Psychol. 1932;43:230–45. [Google Scholar]
- 20.Bjerner B. Alpha depression and lowered pulse rate during delayed actions in a serial reaction test: a study in sleep deprivation. Acta Physiol Scand. 1949;19:65. [Google Scholar]
- 21.Kleitman N. Sleep and wakefulness. 2nd ed. Chicago: University of Chicago Press; 1963. [Google Scholar]
- 22.Williams HL, Lubin A, Goodnow JJ. Impaired performance with acute sleep loss. Psychol Monogr. 1959;73:1–26. [Google Scholar]
- 23.Kjellberg A. Sleep deprivation, arousal and performance. In: Mackie RR, editor. Vigilance theory, operational performance and physiological correlates. New York: Plenum Press; 1977. pp. 529–35. [Google Scholar]
- 24.Wilkinson RT. Interaction of lack of sleep with knowledge of results, repeated testing and individual differences. J Exp Psychol. 1961;62:263–71. doi: 10.1037/h0048787. [DOI] [PubMed] [Google Scholar]
- 25.Wilkinson RT. Evoked response and reaction time. Acta Psychologica. 1967;27:235–45. doi: 10.1016/0001-6918(67)90064-9. [DOI] [PubMed] [Google Scholar]
- 26.Wilkinson RT, Allison S. Age and simple reaction time: decade differences for 5,325 subjects. J Gerontol. 1989;44:29–35. doi: 10.1093/geronj/44.2.p29. [DOI] [PubMed] [Google Scholar]
- 27.Wilkinson RT. Sleep deprivation: Performance tests for partial and selective sleep deprivation. In: Abt LE, Reiss BF, editors. Progress in clinical psychology: Dreams and dreaming. New York: Grune & Stratton; 1968. pp. 28–98. [Google Scholar]
- 28.Wilkinson RT. Interaction of lack of sleep with knowledge of results, repeated testing, and individual differences. J Exp Psychol. 1961;62:263–71. doi: 10.1037/h0048787. [DOI] [PubMed] [Google Scholar]
- 29.Dinges DF, Powell JW. Microcomputer analysis of performance on a portable, simple visual RT task sustained operations. Behavioral Research Methods, Instrumentation, and Computers. 1985;17:652–5. [Google Scholar]
- 30.Dinges DF, Whitehouse WG, Orne EC, Orne MT. The benefits of a nap during prolonged work and wakefulness. Work Stress. 1988:139–53. [Google Scholar]
- 31.Dinges DF, Orne MT, Whitehouse WG, Orne EC. Temporal placement of a nap for alertness: contributions of circadian phase and prior wakefulness. Sleep. 1987;10:313–29. [PubMed] [Google Scholar]
- 32.Tirunahari VL, Zaidi SA, Sharma R, Skurnick J, Ashtyani H. Microsleep and sleepiness: a comparison of multiple sleep latency test and scoring of microsleep as a diagnostic test for excessive daytime sleepiness. Sleep Med. 2003;4:63–7. doi: 10.1016/s1389-9457(02)00250-2. [DOI] [PubMed] [Google Scholar]
- 33.Priest B, Brichard C, Aubert G, Liistro G, Rodenstein DO. Microsleep during a simplified maintenance of wakefulness test. A validation study of the OSLER test. Am J Respir Crit Care Med. 2001;163:1517–9. doi: 10.1164/ajrccm.163.7.2007028. [DOI] [PubMed] [Google Scholar]
- 34.Johns MW, Tucker A, Chapman R, Crowley K, Michael N. Monitoring eye and eyelid movements by infra-red reflectance oculography to measure drowsiness in drivers. Somnologie. 2007;11:234–42. [Google Scholar]
- 35.Chapman R, Johns MW, Crowley K. In the drowsy state, errors of omission in a visual reaction time test occur with eyes open or closed. Sleep. 2007;29(Suppl):A364. [Google Scholar]
- 36.Anderson C, Horne JA. Sleepiness enhances distraction during a monotonous task. Sleep. 2006;29:573–6. doi: 10.1093/sleep/29.4.573. [DOI] [PubMed] [Google Scholar]
- 37.Dinges DF, Mallis MM, Maislin G, Powell JW. Evaluation of techniques for ocular measurement as an index of fatigue and as the basis for alertness management. Report no. DOT HS 808 762. 1998:42–47. [Google Scholar]
- 38.Wierwille WW, Ellisworth LA. Evaluation of driver drowsiness by trained raters. Accid Anal Prev. 1994;26:571–81. doi: 10.1016/0001-4575(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 39.Caffier PP, Erdmann U, Ullsperger P. Experimental evaluation of eye-blink parameters as a drowsiness measure. Eur J Appl Physiol. 2003;89:319–25. doi: 10.1007/s00421-003-0807-5. [DOI] [PubMed] [Google Scholar]
- 40.Maulsby RL. Electroencephalogram during orbital flight. Aerospace Med. 1966;37:1022–6. [PubMed] [Google Scholar]
- 41.Van Orden KF, Jung T, Makeig S. Combined eye activity measures accurately estimate changes in sustained visual task performance. Biol Psychol. 2000;51:221–40. doi: 10.1016/s0301-0511(99)00043-5. [DOI] [PubMed] [Google Scholar]
- 42.Bocca M-L, Denise P. Total sleep deprivation effect on disengagement of spatial attention as assessed by saccadic eye movements. Clin Neurophysiol. 2006;117:894–9. doi: 10.1016/j.clinph.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 43.De Gennaro L, Ferrara M, Urbani L, Bertini M. Oculomotor impairment after 1 night of total sleep deprivation: a dissociation between measures of speed and accuracy. Clin Neurophysiol. 2000;11:1771–8. doi: 10.1016/s1388-2457(00)00393-x. [DOI] [PubMed] [Google Scholar]
- 44.De Gennaro L, Ferrara M, Curcio G, Bertini M. Visual search performance across 40 h of continuous wakefulness: measures of speed and accuracy and relation with oculomotor performance. Physiol Behav. 2001;74:197–204. doi: 10.1016/s0031-9384(01)00551-0. [DOI] [PubMed] [Google Scholar]
- 45.Volkmann FC, Riggs LA, Moore RK. Eyeblinks and visual suppression. Science. 1980;207:900–2. doi: 10.1126/science.7355270. [DOI] [PubMed] [Google Scholar]
- 46.Drummond SPA, Bischoff-Grethe A, Dinges DF, Ayalon L, Mednick SC, Meloy MJ. The neural basis of the psychomotor vigilance task. Sleep. 2005;28:1059–68. [PubMed] [Google Scholar]
- 47.Dinges DF, et al. Evaluation of techniques for ocular measurements and index of fatigue and the basis for alertness management. Final report for the U.D. Department of Transportation, national Highway Traffic Safety Administration. 1998:1–112. [Google Scholar]
- 48.Dinges DF, et al. Wierwille WW, et al., editors. Prospective laboratory revalidation of ocular-based drowsiness detection technologies and countermeasures. NHTSA Drowsy driver detection and interface projects. 2002 DTNH-22-00-D-07007. [Google Scholar]
- 49.Price NJ, Maislin G, Powell JW, et al. Unobtrusive detection of drowsiness-induced PVT lapses using infra-red retinal reflectance of sloe eyelid closures. Sleep. 2003;26:A177. [Google Scholar]
- 50.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 51.Fox J. Applied regression analysis, linear models, and related methods. Sage. 1997 [Google Scholar]
- 52.Torsvall L, Åkerstedt T. Sleepiness on the job: continuously measured EEG in train drivers. Electroenceph Clin Neurophysiol. 1987;66:502–11. doi: 10.1016/0013-4694(87)90096-4. [DOI] [PubMed] [Google Scholar]
- 53.Volkmann FC, Riggs LA, Moore RK. Eyeblinks and visual suppression. Science. 1980;207:900–2. doi: 10.1126/science.7355270. [DOI] [PubMed] [Google Scholar]
- 54.Burr D. Vision: in the blink of an eye. Curr Biol. 2005;15:R554–R556. doi: 10.1016/j.cub.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 55.Ridder WH, Tonlinson A. A comparison of saccadic and blink suppression in normal observers. Vision Res. 1997;37:3171–9. doi: 10.1016/s0042-6989(97)00110-7. [DOI] [PubMed] [Google Scholar]
- 56.Leigh RJ, Zee DS. Oxford: Oxford University press; 2006. The neurology of eye movements. [Google Scholar]
- 57.Tucker A, Johns MW. The duration of eyelid movements during blinks: changes with drowsiness. Sleep. 28:A122. [Google Scholar]
- 58.Crevits L, Simons B, Wildenbeest J. Effects of sleep deprivation on saccades and eyelid blinking. Eur Neurol. 2003;50:176–80. doi: 10.1159/000073060. [DOI] [PubMed] [Google Scholar]
- 59.Morris TL, Miller JC. Electrooculographic and performance indices of fatigue during simulated flight. Biol Psychol. 1996;42:343–60. doi: 10.1016/0301-0511(95)05166-x. [DOI] [PubMed] [Google Scholar]
- 60.Lobb ML, Stern JA. Pattern of eyelid motion predictive of decision errors during drowsiness: oculomotor indices of altered states. Int J Neurosci. 1986;30:17–22. doi: 10.3109/00207458608985650. [DOI] [PubMed] [Google Scholar]
- 61.Tsubota K, Kwong KH, Lee T-Y, Makamura J, Cheng H-M. Functional MRI of brain activation by eye blinking. Exp Eye Res. 1999;69:1–7. doi: 10.1006/exer.1999.0660. [DOI] [PubMed] [Google Scholar]
- 62.Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98:676–82. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.kerskedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52:29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 64.Maulsby RL, Kellaway P, Graham M, et al. National Aeronautic and Space Administration. 1968. The normative electroencephalographic data reference library; p. p. 172. [Google Scholar]
- 65.Santamaria J, Chiappa KH. The EEG of drowsiness in young adults. J. Clin Neurophysiol. 1987;4:327–82. doi: 10.1097/00004691-198710000-00002. [DOI] [PubMed] [Google Scholar]
- 66.Caldwell JA, Prazinko B, Caldwell JL. Body posture affects electroencephalographic activity and psychomotor vigilance performance in sleep-deprived subjects. Clin Neurophysiol. 2003;114:23–31. doi: 10.1016/s1388-2457(02)00283-3. [DOI] [PubMed] [Google Scholar]
- 67.Baulk SD, Biggs SN, Reid KJ, van den Heuvel CJ, Dawson D. Chasing the silver bullet: Measuring driver fatigue using simple and complex tasks. Accid Anal Prev. 2008;40:396–402. doi: 10.1016/j.aap.2007.07.008. [DOI] [PubMed] [Google Scholar]