Abstract
Study Objectives:
To determine whether fixed-pressure or variable-pressure CPAP was preferred by patients and gave better outcomes in patients with the obstructive sleep apnea/hypopnea syndrome (OSAHS).
Design:
Randomized blinded cross-over trial with 6 weeks of fixed and 6 weeks of variable-pressure CPAP
Setting:
Sleep center
Patients:
200 consecutive consenting CPAP naive patients with daytime sleepiness and >15 apneas + hypopneas/h after an attended auto-CPAP titration night.
Interventions:
CPAP therapy using the same device (Autoset Spirit) set for 6 weeks in fixed pressure mode and for 6 weeks in variable pressure mode, the order of therapies being randomized.
Measurements and Results:
All measurements were recorded at the end of each limb by a researcher blind to treatment. These included symptoms, Epworth Score, CPAP usage, objective sleepiness by modified Osler test, vigilance and health related quality of life. A total of 181 of 200 patients completed the study. At the end of the study, patients expressed no significant difference in the primary outcome, patient preference, 72 patients preferring fixed and 69 preferring variable-pressure CPAP. Epworth score was lower on variable (9.5, SEM 0.4) than fixed-pressure CPAP (10.0, SEM 0.3; P = 0.031). Mean CPAP use was higher on variable (4.2, SEM 0.2 h/night) than fixed-pressure CPAP (4.0, SEM 0.2 h/night; P = 0.047). There were no other significant differences between treatments.
Conclusions
This study shows no difference in patient preference and only a marginal benefit of variable over fixed-pressure CPAP in OSAHS in terms of subjective sleepiness and CPAP use. The clinical value of this difference remains to be determined.
Clinical Trial Information:
Variable-pressure versus fixed-pressure continuous positive airway pressure (CPAP) treatment for patients with obstructive sleep apnoea/hypopnoea syndrome (OSAHS); Registration # ISRCTN43085025; http://www.controlled-trials.com/ISRCTN43085025
Citation:
Vennelle M; White S; Riha RL; Mackay T; Engleman HM; Douglas NJ. Randomized controlled trial of variable-pressure versus fixed-pressure continuous positive airway pressure (CPAP) treatment for patients with obstructive sleep apnea/hypopnea syndrome (OSAHS). SLEEP 2010;33(2):267-271.
Keywords: Variable pressure, fixed pressure, obstructive sleep apnea/hypopnea syndrome
THE OBSTRUCTIVE SLEEP APNEA/HYPOPNEA SYNDROME (OSAHS) CAUSES DAYTIME SLEEPINESS ASSOCIATED WITH LOUD SNORING IN APPROXIMATELY 4% of middle-aged men and 2% of middle aged women. Patients with OSAHS are at increased risk of road traffic accidents1,2 have increased blood pressure3–5 and an increased risk of cardiovascular complications such as strokes and myocardial infarction.6
The treatment of choice for obstructive sleep apnea/hypopnea syndrome (OSAHS) is continuous positive airway pressure (CPAP) which initially delivered a preset pressure determined on an overnight titration study. More recently CPAP devices which can vary the pressure delivered during the night have become available. Such variable pressure devices have the theoretical advantages of being able to cope with changes in pressure requirements due to both short term (posture, alcohol, nasal congestion) and long term (weight change, ageing) effects. Variable-pressure variable pressure devices tend to be more expensive. Anecdotally some patients have reported preference for variable pressure devices and others for fixed pressure devices.
When the study was initiated a meta-analysis showed no clear evidence whether variable-pressure devices give better outcomes than fixed pressure devices in the average patient with OSAHS.7 However even this inconclusive meta-analysis included only 282 patients, and averaged data from 9 studies and 6 manufacturers' differing variable-pressure CPAP devices, both factors which may have decreased the clarity of any difference. In addition there is evidence that in some sub-groups of patients, including those requiring a higher CPAP pressure > 10 cm H2O8 and those with high within-night pressure variability,9 variable pressure devices may deliver better patient outcomes,8 but this cannot be generalized to other patient populations. We therefore performed a blinded, randomized controlled crossover trial in 200 consecutive patients across a range of severities of OSAHS to determine whether 6 weeks of treatment with variable-pressure CPAP produced better outcomes than 6 weeks of treatment with fixed-pressure CPAP.
METHODS
Patients
Eligible patients with a diagnosis of obstructive sleep apnea/hypopnea syndrome (OSAHS) were identified during the Department of Sleep Medicine's weekly clinical review of all new cases where full case notes and investigations were available to ascertain inclusion and exclusion criteria. Consecutive eligible patients were approached with information on the study and asked to consent to participation until 200 patients were recruited. All participants gave written informed consent to the study, which was approved by the local IRB before commencement. Those agreeing to participate were randomized into the study on the morning after CPAP titration night.
Inclusion Criteria
Patients had to have all of
Epworth Sleepiness Score10≥ 10 or history of troublesome sleepiness when driving
AHI ≥ 15 on polysomnograph with Profusion PSG2 (Compumedics, Australia) or ≥ 25 apneas + hypopneas/h in bed11 on a limited sleep study using Hypno PTT (Tyco Healthcare, Gosport, Hampshire). Apneas were defined by cessation of airflow for > 10 sec12 and hypopneas as a 50% reduction in thoraco-abdominal movement for > 10 sec12,13
Age between 18 and 70 years of age
No previous CPAP use.
Exclusion criteria
Severe neurological deficit sufficient to compromise CPAP usability or understanding.
Significant comorbidity (severe or unstable respiratory, neurological, metabolic or cardiac disease) such as severe COPD, stroke, unstable diabetes, or active angina.
Coexisting narcolepsy or periodic limb movement syndrome
Contraindications to CPAP use including recent pneumothorax
Protocol
Consecutive consenting patients received treatment with the same CPAP device (AutoSet Spirit, ResMed, Poway, CA) for 2 periods of 6 weeks, attending for assessment on the last day of each treatment. During one period, the CPAP machine was set in fixed-pressure mode at the pressure determined during overnight in-lab CPAP titration, performed using our standard technique of attended in-lab auto-titration without PSG,14 and during the other 6 weeks it was set in variable-pressure mode. There was no gap between the 2 limbs, as it was not considered ethical to withhold treatment. In lieu of a washout period, no data from the first 2 weeks of each limb were included in the analysis.
Randomization
Patients were randomized to fixed- or variable-pressure CPAP as their first treatment, using a randomization schedule of balanced blocks, predetermined by a worker otherwise uninvolved in the trial. Any subject who withdrew was replaced by the next available eligible patient.
Blinding
Patients.
Patients were informed that 2 different methods of giving CPAP were to be assessed, but were not told which was the new method.
Staff.
None of the staff involved in data acquisition or analysis were aware of the mode of treatment the patient was receiving. A separate worker issued the appropriate CPAP type. All management of technical problems with CPAP during the trial was handled by nursing staff separate from the blinded research staff. The blinded staff member conducted the follow-up assessments unaware of the type of CPAP the patient was using at the time of assessment. The individual providing the patient with support and CPAP trouble-shooting during the trial was able to access which mode of therapy was being used. The number of times that support was requested by the patients on each limb of treatment was recorded.
Baseline Assessment, CPAP Titration, and CPAP Commencement
Consenting patients received CPAP education and mask-fitting as per our usual practice.15 Attended CPAP titration was performed in the sleep laboratory using Spirit units.16 (Data were reviewed by certified sleep technologists and any periods of poor quality or doubtful data were identified. The therapeutic pressure for fixed-pressure CPAP determined using the automated 95th centile of pressure profile unless poor quality of doubtful data had been identified, by the sleep technologist, in which case the 95th centile pressure was estimated from the valid data. After the titration study, all patients were issued with a Spirit unit set in the appropriate treatment mode (fixed- or variable-pressure CPAP) for home use over the first 6 week treatment limb.
Post-treatment Assessment
At the end of each 6 week treatment limb, patients were asked to attend with their Spirit CPAP units for a 3-h session of testing, during which tests of objective sleepiness by modified OSLER17 using 2 wakefulness trials,18 vigilance using Psychomotor Vigilance Test [PVT],19 and quality of life by Short Form 36 (SF-36)20 were performed.
Follow-up outcome tests were carried out at the same time of day after each treatment limb to avoid circadian effects. At the last session patients were also asked ”Did you prefer the first or second treatment”
The a priori primary outcome measure was whether the patients preferred fixed or variable pressure CPAP. The a priori secondary outcome measures were whether there were differences in CPAP use and Epworth sleepiness score on the different CPAP types.
Analysis
The statistical analysis of the primary outcome variable was by χ2 test. For ordinal data, Wilcoxon rank sum tests, and paired t-tests were used as appropriate to test differences between treatments with analysis of variance with general linear modeling using SPSS (SPSS Inc, Chicago, IL) to evaluate order effects. Results are quoted as mean and standard error of the mean (SEM) unless otherwise stated.
Power
The study was designed to have a 90% power to detect a 60% to 40% difference in patient preference at the 5% level. It also had a 94% power to detect a 1 unit difference in Epworth score at the 5% level based on the data of Massie et al.8
This study is registered as a clinical trial with number ISRCTN43085025
RESULTS
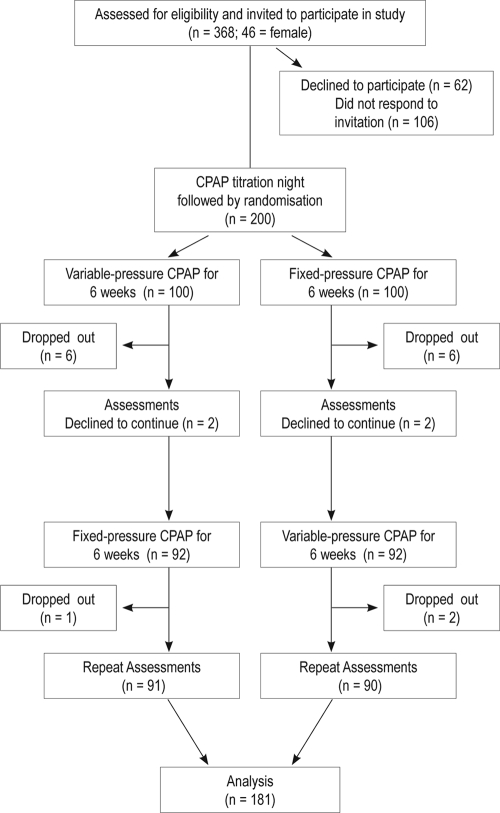
A total of 368 patients with OSAHS were invited to participate in the study (Figure 1), and 200 patients (46 F) were recruited (mean age 50 SD ± 10 y; BMI 34.5 ± 7.8 kg/m2; Epworth Score 14 ± 3). One hundred twenty-three patients had polysomnography; mean AHI was 33 ± 18. An additional 77 had a limited sleep study, with mean A+H/h 49 ± 20). The patients who declined to participate were not different from the participants in terms of age, Epworth score, or breathing during sleep (P > 0.2). Nineteen patients (4 female) did not complete the study; at the time of dropout 9 of these were receiving fixed and 10 variable pressure CPAP; 11 dropped out during the first limb. One patient died from unrelated and nonvascular causes during the first limb.
Figure 1.
Randomised controlled trial of variable-pressure versus fixed-pressure continuous positive airway pressure (CPAP) treatment for patients with obstructive sleep apnoea/hypopnoea syndrome (OSAHS)
There was no significant difference in the primary outcome, patient preference, with 72 patients preferring fixed pressure CPAP and 69 preferring variable pressure CPAP (χ2 = 0.8), and 40 expressing no preference.
Epworth sleepiness score was lower on variable (9.5, SEM 0.4) than fixed pressure CPAP (10.0, SEM 0.3; P = 0.031). Mean CPAP use was higher on variable (4.2, SEM 0.2 h/night) than fixed pressure CPAP (4.0, SEM 0.2 h/night; P = 0.047). There was no difference between treatments in objective sleepiness as judged by the limited Osler test (variable 36 min, SEM 0.6; fixed 35 min, SEM 0.6; P = 0.43), and no difference in vigilance (variable mean response time 291.9 msec, SEM 13.2; fixed mean response time 302.8 msec, SEM 18.9; P = 0.137), quality of life (variable 58, SEM 0.1; fixed 58, SEM 0.1; P = 0.9), SF-36 vigilance or in any daytime or night time symptoms (Table 2). The number of times patients sought help from the sleep center was 25 during fixed treatment and 13 on variable CPAP (P = 0.7)
Table 1.
Measurements made at end of each limb
| Domain | Instrument |
|---|---|
| Objective sleepiness | Two 40-min OSLER tests16,17 at 10:00 and 12:00 (sleep resistance task) |
| Subjective sleepiness | Epworth sleepiness scale |
| Vigilance | Psychomotor vigilance test [PVT]18 |
| Symptom ratings | Nocturnal and daytime symptoms |
| Health-related quality of life | Short-form-36&19 |
| CPAP side effects | Edinburgh side-effects checklist |
| CPAP use and efficacy | Spirit CPAP units' memory (final 4 wks of each 6 wk limb) |
| CPAP use | |
| CPAP pressure | |
| Mask leak | |
| Residual AHI on CPAP |
Table 2.
Results of study expressed as mean ± SEM
| Variable Treatment (Mean ± SEM) | Fixed Treatment (Mean ± SEM) | P value | |
|---|---|---|---|
| CPAP use (h/night) | 4.2 ± 0.2 | 4.0 ± 0.2 | 0.047 |
| Epworth Sleepiness Scale | 9.5 ± 0.4 | 10.0 ± 0.3 | 0.031 |
| Mean CPAP pressure | 10.7 ± 0.16 | 10.6 ± 0.13 | > 0.5 |
| Residual A+H/h on CPAP | 6.7 ± 0.4 | 6.3 ± 0.4 | 0.17 |
| OSLER (min) | |||
| Test 1 | 36.9 ± 0.6 | 36.6 ± 0.6 | > 0.5 |
| Test 2 | 34.6 ± 0.7 | 34 ± 0.8 | > 0.3 |
| Mean | 35.7 ± 0.6 | 35.3 ± 0.6 | > 0.4 |
| PVT (msec) | |||
| Mean response time | 292 ± 13 | 302.8 ± 19 | 0.14 |
| Median response time | 263.4 ± 5 | 273.7 ± 11 | 0.2 |
| Lapses | 2.9 ± 0.5 | 3.8 ± 0.8 | 0.14 |
| SF-36 | |||
| Health transition | 3.0 ± 0.1 | 2.9 ± 0.1 | > 0.3 |
| Physical Health | 42.5 ± 0.9 | 42.1 ± 1.0 | > 0.9 |
| Mental Health | 48.7 ± 0.8 | 48.8 ± 0.8 | > 0.7 |
| Quality of Life | 57.7 ± 0.1 | 57.7 ± 0.1 | > 0.9 |
During the fixed limb patients who preferred fixed pressure used the machine more than those who preferred variable (fixed preference 4.5, SEM 0.3 h/night; variable preference 3.5, SEM 0.3 h/night; P = 0.015), however there was no difference in use during the variable treatment (fixed preference 4.4, SEM 0.3 h/night; variable preference 4.2, SEM 0.3 h/night; P = 0.5)
There were significant order effects shown on the analysis of variance, with 40 of the 100 patients who received variable pressure CPAP on the first limb preferring variable pressure compared to 29 preferring fixed pressure CPAP, whereas of those receiving fixed pressure first 46 preferred fixed and 26 variable pressure CPAP at the end of the study (P = 0.009). CPAP use did not vary with order (variable setting first 4.4, SEM 0.3 h/night, variable second 4.0, SEM 0.2 h/night; fixed pressure first 4.0, SEM 0.3 h/night, fixed pressure second 4.0, SEM 0.2 h/night; P = 0.458), whereas ESS was significantly different (variable setting first 10.6, SEM 0.5; variable second 8.5, SEM 0.4; fixed pressure first 10.1, SEM 0.5; fixed pressure second 9.95, SEM 0.4; P = 0.033).
DISCUSSION
The primary result of the study was that after 6 weeks treatment with each form of therapy, patients with OSAHS expressed no preference between fixed-pressure and variable-pressure CPAP. Overall there was greater CPAP use and patients reported being less sleepy when on variable pressure CPAP than on fixed pressure CPAP but there were no significant differences between the treatments in terms of objective sleepiness or quality of life. There was a significant time order effect in preference, more patients preferring the first treatment they received.
Although variable pressure CPAP produced better outcomes in terms of Epworth Sleepiness score and CPAP use, the advantages were marginal. The difference in Epworth scores between the treatments was 0.6 and the difference in CPAP use was only 0.2 h/night (5%) over the 4 week period studied on each treatment. Whether these differences are sufficient to influence choice of therapy will depend on the healthcare system and the differences in CPAP machine prices locally. The fact that there were no significant differences in objective sleepiness, vigilance, quality of life or nocturnal symptoms indicates there is no compelling advantage of variable over fixed pressure CPAP in unselected patients.
There have been several smaller or shorter term studies comparing the outcomes following fixed and variable pressure CPAP.9,21–30 Overall these have shown no major benefits for variable over fixed devices. This study adds to these previous studies by using rigorous methodology in a significantly larger number of patients and by using cross-over design which removes the variance in response to CPAP resulting from differing severities of OSAHS31 by comparing differences within patients. Our study contains data on 181 patients completing both limbs of a crossover study compared with the previous largest study of 52 patients28 included in the recent Cochrane Review.32 That review reported a data of a total of 450 patients in 18 crossover studies and 444 patients in 10 parallel limb studies on 6 different manufacturers' devices. Thus our study is by far the largest and statistically the most powerful so far. It broadly confirms the results of the Cochrane Review by showing a small benefit of dubious clinical value from variable-pressure as opposed to fixed-pressure CPAP therapy but we also showed no difference in terms of patient preference.
One study33 has suggested that fixed pressure CPAP might have a greater effect on cardiovascular risk including blood pressure than variable CPAP. However that study did not perform the appropriate analysis, which would have been to directly compare the blood pressures after fixed as opposed to variable pressure. It merely showed that in a small number of patients (15), variable pressure CPAP did not significantly reduce blood pressure, which may reflect the lack of power of that component of the study. This study should be repeated in larger numbers with improved analysis.
In the review process it was suggested that analysis should be performed of the residual AHI as recorded by the CPAP device during the study limbs. This was not originally planned as the accuracy and equivalence of this measure has not been determined. The post hoc analysis showed that the residual AHI was higher on variable than fixed CPAP (variable median 5.0, IQR 3.2-8.8; fixed 4.7, 2.8-7.7/h; P = 0.03). However the clinical significance of this small but statistically significant difference is unclear. This also has to be seen in the context of marginally (0.2 h/night) greater CPAP use on variable CPAP, so that apneas and hypopneas occurring during these unrecorded 12 min (on average) would not have been recorded by the CPAP machine in fixed pressure mode.
Limitations of this study include the fact that 10% of the patients enrolled in the study dropped out. Dropout rates were similar between the 2 devices and this is therefore unlikely to have skewed the findings of the study. Dropouts are inevitable with CPAP, and the rate we observed in this study is not unusual. Another limitation is the relatively short battery of tests that could be fitted in at follow up while minimizing patient inconvenience. The shortened Osler test might have masked a real difference had more sleep opportunities been studied. Another limitation is that unselected patients requiring CPAP were recruited, not subgroups who may have particularly benefited from variable pressure CPAP. Massie7 showed greater CPAP use and vitality on variable pressure but no difference in sleepiness on variable pressure CPAP in patients requiring a high CPAP pressure (> 10 cm H2O). Noseda et al9 found an improved Epworth score on variable-pressure devices in 24 patients with high within-night variability in CPAP pressure requirements. In a post hoc analysis, Hukins21 reported greater CPAP use with variable pressure devices in those reporting side effects from CPAP treatment. An attribute of our study is that it was a single-center well-controlled trial, thus minimizing discrepancies of definitions and patient characteristics that can occur in multicenter studies. However it must be stressed that our results reflect our patient population and will not be generalizable to all settings. Similarly they were obtained on a single CPAP device and cannot be extended to other devices.
The marked order effect with greater benefit from the first form of CPAP used not only complicated the analysis but also may be of real concern in clinical practice. Eighty-six patients preferred the first type of CPAP they received, compared to 55 who preferred the second form of CPAP. Some centers have adopted a practice of titrating CPAP by giving patients variable devices for a week or more at home, reading the level of CPAP pressure required, and then issuing cheaper fixed-pressure devices at that pressure. The current study raises concerns that such practice might result in worse outcomes and possibly lower CPAP use on the subsequent fixed-pressure CPAP compared with those put on fixed pressure CPAP immediately after an overnight titration with a variable device.
DISCLOSURE STATEMENT
This study was supported by a grant from ResMed, Poway, CA. Dr. Douglas is a shareholder in ResMed. The other authors have indicated no additional conflicts of interest. The study was proposed, designed and all analysis performed solely by the authors.
References
- 1.George CF, Boudreau AC, Smiley A. Simulated driving performance in patients with obstructive sleep apnoea. Am J Respir Crit Care Med. 1996;154:175–81. doi: 10.1164/ajrccm.154.1.8680676. [DOI] [PubMed] [Google Scholar]
- 2.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J Cooperative Group Burgos-Santander. The association between sleep apnea and the risk of traffic accidents. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 3.Faccenda JF, Mackay TW, Boon NA, et al. Randomized placebo-controlled trial of continuous positive airway pressure on blood pressure in the sleep apnea-hypopnea syndrome. Am J Respir Crit Care Med. 2001;163:344–8. doi: 10.1164/ajrccm.163.2.2005037. [DOI] [PubMed] [Google Scholar]
- 4.Pepperell JC, Davies RJ, Stradling JR. Systemic hypertension and obstructive sleep apnoea. Sleep Med Rev. 2002;6:157–173. doi: 10.1053/smrv.2001.0189. [DOI] [PubMed] [Google Scholar]
- 5.Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359:204–10. doi: 10.1016/S0140-6736(02)07445-7. [DOI] [PubMed] [Google Scholar]
- 6.Marin JM, Carrizo SJ, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 7.Ayas NT, Patel SR, Malhotra A, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep. 2004;27:249–53. doi: 10.1093/sleep/27.2.249. [DOI] [PubMed] [Google Scholar]
- 8.Massie CA, McArdle N, Hart RW, et al. Comparison between automatic and fixed positive airway pressure therapy in the home. Am J Respir Crit Care Med. 2003;167:20–3. doi: 10.1164/rccm.200201-022OC. [DOI] [PubMed] [Google Scholar]
- 9.Noseda A, Kempenaers C, Kerkhofs M, Braun S, Linkowski P, Jann E. Constant vs auto-continuous positive airway pressure in patients with sleep apnea hypopnea syndrome and a high variability in pressure requirement. Chest. 2004;126:31–7. doi: 10.1378/chest.126.1.31. [DOI] [PubMed] [Google Scholar]
- 10.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 11.Whittle AT, Finch SP, Mortimore IL, MacKay TW, Douglas NJ. Use of home sleep studies for the diagnosis of the sleep apnoea/ hypopnoea syndrome. Thorax. 1997;52:1068–73. doi: 10.1136/thx.52.12.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Academy of Sleep Medicine. Sleep-related breathing disorders in adults: recommendations for syndrome of definition and measurement techniques in clinical research: the report of an American Academy of Sleep Medicine task force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 13.Gould GA, Whyte KF, Rhind GB, et al. The sleep hypopnea syndrome. Am Rev Respir Dis. 1988;137:895–8. doi: 10.1164/ajrccm/137.4.895. [DOI] [PubMed] [Google Scholar]
- 14.Cross MD, Mills NL, Al-Abri M, et al. Continuous positive airway pressure improves vascular function in obstructive sleep apnoea/ hypopnoea syndrome: a randomised controlled trial. Thorax. 2008;63:578–83. doi: 10.1136/thx.2007.081877. [DOI] [PubMed] [Google Scholar]
- 15.Hoy CJ, Vennelle M, Kingshott RN, et al. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159:1096–1100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 16.Cross MD, Vennelle M, Engleman HM, et al. Comparison of CPAP titration at home or the sleep laboratory in the sleep apnea hypopnea syndrome. Sleep. 2006;29:1451–5. doi: 10.1093/sleep/29.11.1451. [DOI] [PubMed] [Google Scholar]
- 17.Bennett LS, Stradling JR, Davies RJ. A behavioural test to assess daytime sleepiness in obstructive sleep apnoea. J Sleep Res. 1997;6:142–5. doi: 10.1046/j.1365-2869.1997.00039.x. [DOI] [PubMed] [Google Scholar]
- 18.Smith LA, Vennelle M, Gardner RS, et al. Auto-titrating continuous positive airway pressure therapy in patients with chronic heart failure and obstructive sleep apnoea: a randomized placebo-controlled trial. Eur Heart J. 2007;28:1221–7. doi: 10.1093/eurheartj/ehm131. [DOI] [PubMed] [Google Scholar]
- 19.Lamond N, Dawson D, Roach GD. Fatigue assessment in the field: validation of a hand-held electronic psychomotor vigilance task. Aviat Space Environ Med. 2005;76:486–9. [PubMed] [Google Scholar]
- 20.Flemons WW, Reimer MA. Development of a disease specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med. 1998;158:494–503. doi: 10.1164/ajrccm.158.2.9712036. [DOI] [PubMed] [Google Scholar]
- 21.Hukins C. Comparative study of autotitrating and fixed-pressure CPAP in the home: a randomized, single-blind crossover trial. Sleep. 2004;15(27):1512–7. doi: 10.1093/sleep/27.8.1512. [DOI] [PubMed] [Google Scholar]
- 22.Marrone O, Resta O, Salvaggio A, Giliberti T, Stefano A, Insalaco G. Preference for fixed or automatic CPAP in patients with obstructive sleep apnea syndrome. Sleep Med. 2004;5:221–51. doi: 10.1016/j.sleep.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Resta O, Carratú P, Depalo A, et al. Effects of fixed compared to automatic CPAP on sleep in obstructive sleep apnoea syndrome. Monaldi Arch Chest Dis. 2004;61:153–6. doi: 10.4081/monaldi.2004.694. [DOI] [PubMed] [Google Scholar]
- 24.Nussbaumer Y, Bloch KE, Genser T, Thurnheer R. Equivalence of autoadjusted and constant continuous positive airway pressure in home treatment of sleep apnea Chest. 2006;129:638–43. doi: 10.1378/chest.129.3.638. [DOI] [PubMed] [Google Scholar]
- 25.Mulgrew AT, Cheema R, Fleetham J, Ryan CF, Ayas NT. Efficacy and patient satisfaction with auto-adjusting CPAP with variable expiratory pressure versus standard CPAP: a randomized crossover trial. Sleep Breath. 2007;11(1):31–7. doi: 10.1007/s11325-006-0078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nolan GM, Doherty LS, McNicholas WT. Auto-adjusting versus fixed positive pressure therapy in mild to moderate obstructive sleep apnoea. Sleep. 2007;30:189–94. doi: 10.1093/sleep/30.2.189. [DOI] [PubMed] [Google Scholar]
- 27.Hudgel DW, Fung C. A long-term randomized, cross-over comparison of auto-titrating and standard nasal continuous airway pressure. Sleep. 2000;23:645–8. [PubMed] [Google Scholar]
- 28.Randerath WJ, Schraeder O, Galetke W, Feldmeyer F, Ruhle KH. Autoadjusting CPAP therapy based on impedance efficacy, compliance and acceptance. Am J Respir Crit Care Med. 2001;163:652–7. doi: 10.1164/ajrccm.163.3.2006168. [DOI] [PubMed] [Google Scholar]
- 29.Senn O, Brack T, Matthews F, Russi EW, Bloch KE. Randomized short-term trial of two autoCPAP devices versus fixed continuous positive airway pressure for the treatment of sleep apnea. Am J Respir Crit Care Med. 2003;168:1506–11. doi: 10.1164/rccm.200304-542OC. [DOI] [PubMed] [Google Scholar]
- 30.Hussain SF, Love L, Burt H, Fleetham JA. A randomized trial of auto-titrating CPAP and fixed CPAP in the treatment of obstructive sleep apnea-hypopnea. Respir Med. 2004;98:330–3. doi: 10.1016/j.rmed.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Kingshott RN, Vennelle M, Hoy CJ, Engleman HM, Deary IJ, Douglas NJ. Predictors of improvements in daytime function outcomes with CPAP therapy. Am J Respir Crit Care Med. 2000;161:866–71. doi: 10.1164/ajrccm.161.3.9905053. [DOI] [PubMed] [Google Scholar]
- 32.Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2009. doi: 10.1002/14651858.CD003531.pub3. CD003531. [DOI] [PubMed] [Google Scholar]
- 33.Patruno V, Aiolfi S, Costantino G, et al. Fixed and autoadjusting continuous positive airway pressure treatments are not similar in reducing cardiovascular risk factors in patients with obstructive sleep apnea. Chest. 2007;131:1393–9. doi: 10.1378/chest.06-2192. [DOI] [PubMed] [Google Scholar]